Abstract
Ninety percent of health care systems now offer patient portals to access electronic health records (EHRs) in the United States, but only 15% to 30% of patients use these platforms. Using PubMed, the authors identified 53 studies published from September 2013 to June 2019 that informed best practices and priorities for future research on patient engagement with EHR data through patient portals, These studies mostly involved outpatient settings and fell into 3 major categories: interventions to increase use of patient portals, usability testing of portal interfaces, and documentation of patient and clinician barriers to portal use. Interventions that used one-on-one patient training were associated with the highest portal use. Patients with limited health or digital literacy faced challenges to portal use. Clinicians reported a lack of workflows to support patient use of portals in routine practice. These studies suggest that achieving higher rates of patient engagement through EHR portals will require paying more attention to the needs of diverse patients and systematically measuring usability as well as scope of content. Future work should incorporate implementation science approaches and directly address the key role of clinicians and staff in promoting portal use.
Electronic health records (EHRs) were developed to manage clinical information, not to engage patients. However, patient access to their EHR data through online portals or mobile applications represents a potential tool for improving patient engagement (1). As the landscape expands with the growth of application programming interfaces to increase bidirectional data flow with patients (2) and greater patient access to medical data, such as clinical notes (3), the potential impact of patient engagement with these platforms will grow in parallel.
Currently, approximately 90% of U.S. health care systems and providers offer patients online portal access to their EHR data (4), largely supported by the over $30 billion in financial incentives from the meaningful use program (5). Common features of online patient portals include the ability to view visit summaries, test results, and immunization and allergy lists, in addition to secure messaging, appointment scheduling, and medication renewals (6). Despite a robust patient portal infrastructure across many U.S. health care systems, only 15% to 30% of patients use even a single portal feature (4), and portal use is largely confined to a specific setting, such as outpatient care in integrated delivery systems (7).
To date, there is limited evidence linking clinical outcomes to portal use (8), but there is substantial demand from patients and their caregivers to access EHR data and communicate electronically with health systems. The strongest evidence supporting the importance of portal use is related to extremely high patient interest (8) and potential to improve patient satisfaction, convenience, and self-management (9).
We examined recent studies of patient engagement with EHR data through patient portals to identify research priorities and best practices.
Methods
Adhering to the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses) recommendations for scoping reviews (10), we searched PubMed from 1 September 2013 through 4 June 2019 to identify published studies on use of online patient portals (Appendix Table 1, available at Annals.org). Search terms represented the constructs of self-management, engagement, and uptake of patient portals. We searched only PubMed because of the specific biomedical and health care focus of papers published on online portal use and our focus on implementation in U.S. settings. The beginning search date was chosen to exclude studies before meaningful use requirements, when the absence of regulation made the functionality of these systems very heterogeneous.
We excluded articles in which no original data were presented (for example, reviews, protocols, commentaries), reported studies were done outside the United States, and reports focused on stakeholder or clinician perspectives without patient input.
Two coauthors (C.R.L. and A.G.C.) completed all data extraction and conducted full-text review of all articles that met initial selection criteria; this was because studies on portal implementation were not always evident in the abstract alone. Full-text review enabled us to identify and exclude studies that did not examine an intervention or program to engage patients in portal use, and studies that did not examine portal use or barriers to use as a primary outcome. A third coauthor (U.S.) reviewed a subset of the full-text results to ensure reliability in the final inclusion process. We did not hand-search the reference list of included papers to find additional studies, but we did determine whether any of the included studies evaluated the same inter vention or program, combining studies in our summarization as appropriate.
We chose to exclude observational portal use and outcome studies that did not have an interventional component because of the well-established body of literature examining patterns of portal use by patient age (11, 12), race/ethnicity (10, 13, 14), socioeconomic status (12), language (14, 15) presence of chronic health conditions (12), digital literacy or access (13, 16), and provider influence or recommendation (10, 12). These observational studies do not shed light on implementation issues that may explain why some patient subgroups use portals less than others.
We grouped included articles according to the major purpose of the research, to separate studies focused on usability or barriers to portal use from studies of interventions aimed to evaluate or increase portal use. We abstracted information from each study on the methods and sample, primary objective and intervention, and major findings reported.
We used the RE-AIM (reach, effectiveness, adoption, implementation, and maintenance) framework (17) to specifically note whether an included study provided relevant findings related to implementation and dissemination and, qualitatively, identified exemplar interventional studies. RE-AIM is an evaluation framework used in implementation science to promote wider adoption and sustained implementation of effective programs and interventions. Specifically, we examined included studies by using the explicit RE-AIM framework domains of reach (proportion and representativeness of patients using the portal or responding to a specific engagement approach), adoption (proportion and representativeness of the sites offering portals or portal engagement strategies), implementation (consistency, costs, and barriers in patient engagement approaches), and maintenance (the ability to sustain the portal engagement strategies over time). We did not focus on the effectiveness domain of RE-AIM because other recent review articles have specifically focused on portal use and subsequent effectiveness on clinical or behavioral outcomes (18, 19).
Results
Of 283 articles initially identified, 53 met inclusion criteria (Appendix Figure, available at Annals.org). We evaluated 3 major categories of articles separately: studies on use and outcomes, usability studies, and studies on barriers to use.
Use and Outcomes Studies
Twenty-four articles described a type of portal intervention or program, either delivery of an intervention through a portal (20–27) or evaluation of a program to increase portal use (28–43) (Appendix Table 2, available at Annals.org). The majority (18 studies) targeted adults in outpatient primary or specialty care, and 6 evaluated portal enrollment and use among pediatric patients and their parents or caregivers (26, 29, 31, 35, 40, 41). Only 7 studies examined portal use among inpatients, often engaging caregivers in use of the portal (28, 31, 34, 38, 39, 42, 43). Overall, there was low to moderate uptake of portal use in most studies.
Among the 8 studies that delivered interventions via an existing portal, the type of intervention varied widely. For example, studies prompted patients to complete such tasks as advance care planning (21) and cancer screening decision-making modules (22, 27) on the portal before a visit. Other studies examined tasks (such as patient-reported outcome completion) after office visits (20), and others were subgroup analyses of broader programs in which portals were only one component of an intervention (23, 24). Overall, the studies with lowest rates of use passively delivered the intervention via the portal without a broader engagement plan.
Of the 15 studies that evaluated specific interventions or programs to increase portal use, the types of outcome measures assessed included portal enrollment and registration (30, 32, 33, 35, 41, 42); portal logins immediately after training (28, 31, 34, 39); sustained portal use postintervention over a follow-up period (36–38, 40); and use of specific features, such as secure messaging within the portal (28, 31, 39). Five were randomized trials or quasi-experimental designs; the remainder were pre–post or cross-sectional analyses. Among the randomized and quasi-experimental studies, 48% to 81% of patients used the portal postintervention (34, 36, 37, 39, 42). The pre–post or cross-sectional studies generally evaluated broader system-or clinic-wide quality improvement efforts to increase portal use and reported more variation in rates of portal use ranging from 8% to 77% of patients (22, 30, 32, 33, 38). Of note, the studies with high rates of use often employed dedicated staff to enroll and assist patients.
Usability Studies
Twelve usability studies evaluated the functionality of portal systems related to design, layout, format, and content (Appendix Table 3, available at Annals.org). These studies included 10 observational approaches or pilots of existing platforms (44–53) and 2 user surveys assessing ease of use, usefulness, usability, and satisfaction (54, 55). The studies covered the overall functionality of the portal (such as having participants complete multiple tasks in sequence) as well as more focused testing (such as improving test result reporting in an iterative manner).
Direct observation studies demonstrated that patients with limited health literacy and numeracy skills, along with those without extensive previous computer experience and older adults, faced substantial barriers in using the portal interfaces (46, 49–51, 53, 54). However, despite these observed challenges in usability, several self-report studies noted that patients rated the systems highly and expressed strong interest in using portals (45, 46). These observations highlight the differences in usability when outcomes are direct observations versus patient ratings. Studies also underscored the need for better functionality of the platforms, with specific needs for simplified log-ins, consistency across platforms, and greatly improved navigation (50, 53, 55). In addition, acceptability to patients appeared to be better in studies that used audiovisual features or improved graphical representations of the portal content (47, 48, 52).
Barriers to Use
Seventeen studies specifically outlined barriers to portal use (Appendix Table 4, available at Annals.org). Six of these studies included clinicians in their sample along with patients (56–61), whereas the remaining studies focused on patients or caregivers (62–72). Ten of the studies were qualitative, and 7 studies used quantitative approaches.
The most common concerns or barriers among patients centered on the need for support in understanding the medical content presented (44, 56, 59, 60, 63, 64, 66, 69, 71) and the need for improved digital skills and confidence (62, 66, 67, 69, 70). Other barriers included preferences for and satisfaction with current in-person communication (66–69), security/privacy concerns (62, 68, 70, 72), and desire for more ways to contribute their own feedback or data back into the EHR (59, 63). Included studies focusing on clinicians identified concerns about overwhelming patients with information (34, 59), EHR information creating patient anxiety (56, 59), and the potential time burden of secure messaging due to a lack of existing workflows to support electronic communication in their practices (34, 59, 61).
Exemplar Studies of Implementation
Many studies documented low use of portals across various health care settings, but several studies went further in addressing the RE-AIM concept of reach (extent to which the intervention reached the intended population). For example, Arcia (45) examined real-world portal uptake by documenting a tailored portal outreach program, completing the work in both English and Spanish and using the prenatal care period to deliver educational content. Similarly, Ramsey and colleagues (35) outlined an outreach program that utilized medical students to meet adolescent patients before their visits to review the purpose of the portal and assist with enrollment, and collected patient surveys to understand current digital use and preferences for electronic health care communication.
Other studies highlighted findings related to the implementation domain of RE-AIM. McCleary and associates (33) and Kamo and coworkers (30) targeted patients and clinicians or staff simultaneously to promote portal use. For example, Kamo and coworkers adapted their telephone triage system to complement patient portal use in their setting and expended substantial effort to develop workflows that could deliver secure messages sent via the portal to the appropriate staff member (in a team-based rather than physician-focused approach). McCleary and associates developed staff educational programming about patient portal use and rolled out programs to support staff with patient portal enrollment.
Less evidence was provided on comparing different portal outreach approaches across clinics or sites, or long-term implementation approaches. Therefore, available evidence reveals little about the adoption and maintenance constructs of the RE-AIM framework.
Discussion
Available studies generally found low to modest uptake of patient portals. Studies that used broader implementation strategies to engage patients, caregivers, clinicians, or staff generated higher rates of patient engagement. In addition, studies that directly addressed usability of these systems by diverse users shed light on functionality challenges that could be improved to achieve broader portal uptake. Patient-facing digital health technology encounters barriers to uptake and sustained engagement (73, 74), so our findings have relevance beyond patient portals.
Current evidence suggests 4 best practices for future research studying patient use of EHRs and portals (Table).
Table.
Summary Recommendations on Research and Reporting for Understanding Patient Engagement in Their Health Care Using Electronic Health Records
| Research | Examples |
|---|---|
| Measure patients’ skills and interests in using digital health tools. | Understanding health and digital literacy oftarget users is critical to interpreting study results. |
| Use mixed-methods studies to determine usability and uptake. | User-centered design of portals will require gathering qualitative data about perceived barriers as well as observational evidence of navigational challenges. |
| Tailor portal interface and outreach to reach broad groups of patients, families, and caregivers. | Consider using audiovisual formats for data presentation to improve comprehension across literacy levels; translate tools into languages other than English. |
| Study the combination of digital tools with human support. | Initial in-person training and ongoing support can increase digital tool use; greater integration into existing provider and staff workflows will also reinforce patient support in using the tools. |
| Reporting | |
| Incorporate implementation frameworks. | Frameworks such as RE-AIM may be particularly suited to understand processes and contextual factors that influence patient and caregiver use as well as provider and staff use. |
| Emphasize external validity alongside internal validity. | Report how and whether the approach could be tested in new or different populations. |
| Report effectiveness and use from multiple viewpoints. | Consider investigating a broader set of stakeholders in digital health research, including caregivers, peers, providers, staff, and system leadership. |
RE-AIM = reach, effectiveness, adoption, implementation, and maintenance.
1. Studies of patient engagement via EHR portals should directly measure patient skills and interest, including digital health literacy, digital access, health literacy, and numeracy.
Available studies identify patient subgroups that face barriers to portal use. Paying attention to digital literacy, device ownership, and broadband access—along with health literacy and numeracy—is critical to improving engagement via patient portals. Not only do these factors influence portal use, but they also often coexist with increased health needs (75). Some studies suggest a correlation between health literacy and digital literacy (49, 51) and underscore the growing evidence that a digital divide persists among a sizable proportion of the U.S. population, in particular for low-income and older adults (76). Research examining portal use, or delivering interventions via the portal, should explicitly measure these factors.
2. Interventions to promote patient engagement via EHR portals should be designed to address the usability barriers identified to date.
Available studies, particularly those examining usability and barriers to use, highlight the need for greatly improved usability of portal platforms, almost all of which appeared to be vendor-designed portals without many modifications. Cumbersome, fragmented, and complex interfaces dampen the enthusiasm of new users and disadvantaged patients who struggle to find relevant information and might never return to the platform.
Future research should incorporate audiovisual and improved graphical representation of medical data, because studies that used these features reported better patient uptake and satisfaction (47, 48). Only 2 studies recruited non–English speakers (45, 58), suggesting a need to study portal-based interventions available in languages other than English. Finally, future studies should consider combining quantitative use or survey data with direct observation of portal use. Studies reporting observation provided a richer understanding of patient experiences by uncovering underlying beliefs, concerns, and gaps in functionality.
3. Interventions to promote patient engagement via EHR portals should incorporate in-person support for patients.
We observed more favorable portal uptake in studies that incorporated in-person enrollment and training for patients (28, 36). This suggests an opportunity in future research to combine technological outreach (such as communication delivered via portals) with human support, which is a burgeoning area of investigation. Studies that use adaptive designs to understand the best combination of technological and human interaction could be fruitful, especially if we can automate certain processes while systematically investigating the best timing for human follow-up, support, and reinforcement.
The role of caregivers, family, friends, and peers remains a critically underutilized and underevaluated aspect of patient engagement that warrants much more attention in future studies. Some patients cannot use portals themselves, but their care partners or proxy may be able and willing to do this for them (28).
4. Studies of patient engagement via EHR portals should use the principles of implementation science.
Patient engagement problems represent implementation problems. Using RE-AIM, as well as other implementation frameworks, can promote standard ways to report on portal use that take key stakeholders into account. Several of the studies in this review dealt critically with the construct of reach to understand who was offered and currently using portals (including the representativeness of the user groups). Future work should shift more to the adoption, implementation, and maintenance components to spread best practices. This will include understanding key steps in a patient’s health care journey and specific health behaviors for which portal engagement is most relevant (combined with appropriate, established behavioral change approaches [77]), and understanding and designing workflows for clinicians and staff to support patients’ use (78).
Moreover, patient subgroups with the greatest barriers to use could be specifically targeted by using implementation science approaches with a goal of increasing health equity. In particular, high-cost, high-need patients are those with the most to gain from more regular health care communication and information about their conditions, and yet most systems have not targeted portal engagement efforts on the basis of their potential impact.
To directly address some of these recommendations, promising work is currently under way. With respect to usability, tools have been developed that can be overlaid or integrated with the EHR to improve the comprehensibility of medical content, such as hyperlinks to plain-language descriptions and tailored educational materials (7, 75, 79). In addition, to specifically address the health and digital literacy barriers of diverse patients, a growing body of work is linking patients to community-based resources, such as libraries and nonprofit organizations, to foster digital inclusion (80).
Finally, related to the need for greater attention to implementation strategies, efforts are under way that have generated knowledge about patient engagement tied to learning health system approaches (81, 82) and implementation of comprehensive marketing and promotion of patient portals (83).
Our study has limitations. First, our search terms could have excluded relevant articles that used different key words, as well as articles published in journals not indexed in PubMed. Second, we were unable to combine outcome measures or directly compare the quality of the findings across articles in a systematic way because of the heterogeneous nature of the included studies. Third, we did not focus on the clinical impact of portal use because there are existing review articles on that topic. Finally, small sample sizes for certain types of studies, such as those engaging both families and caregivers, precluded us from making more specific recommendations in some areas.
In conclusion, available studies suggested low patient use of portals made available to them and identified barriers to use. Moving forward, research on improving patient engagement using EHR portals should measure a broader array of patient skills, access, and interest; address usability barriers identified to date; incorporate in-person support for patients; and apply the principles of implementation science. Widespread adoption and routine use of EHR portals by patients and caregivers will require multifaceted approaches to encourage uptake.
Grant Support:
By grant R01LM013045, Creating Community Driven, Personalized Health Maps for Patients with Diabetes, Mapping to Amplify the Vitality of Engaged Neighborhoods (MAVEN), from the National Library of Medicine to Dr. Lyles and grant K24CA212294, Improving Survivorship Care for Diverse Cancer Patients Cared for in Safety-net Settings, from the National Cancer Institute and grant P30HS023558, Building an Ambulatory Patient Safety Learning Laboratory for Diverse Populations: The San Francisco Ambulatory Safety CEnter for iNnovaTion (ASCENT), from the Agency for Healthcare Research and Quality to Dr. Sarkar.
Appendix Figure 1.
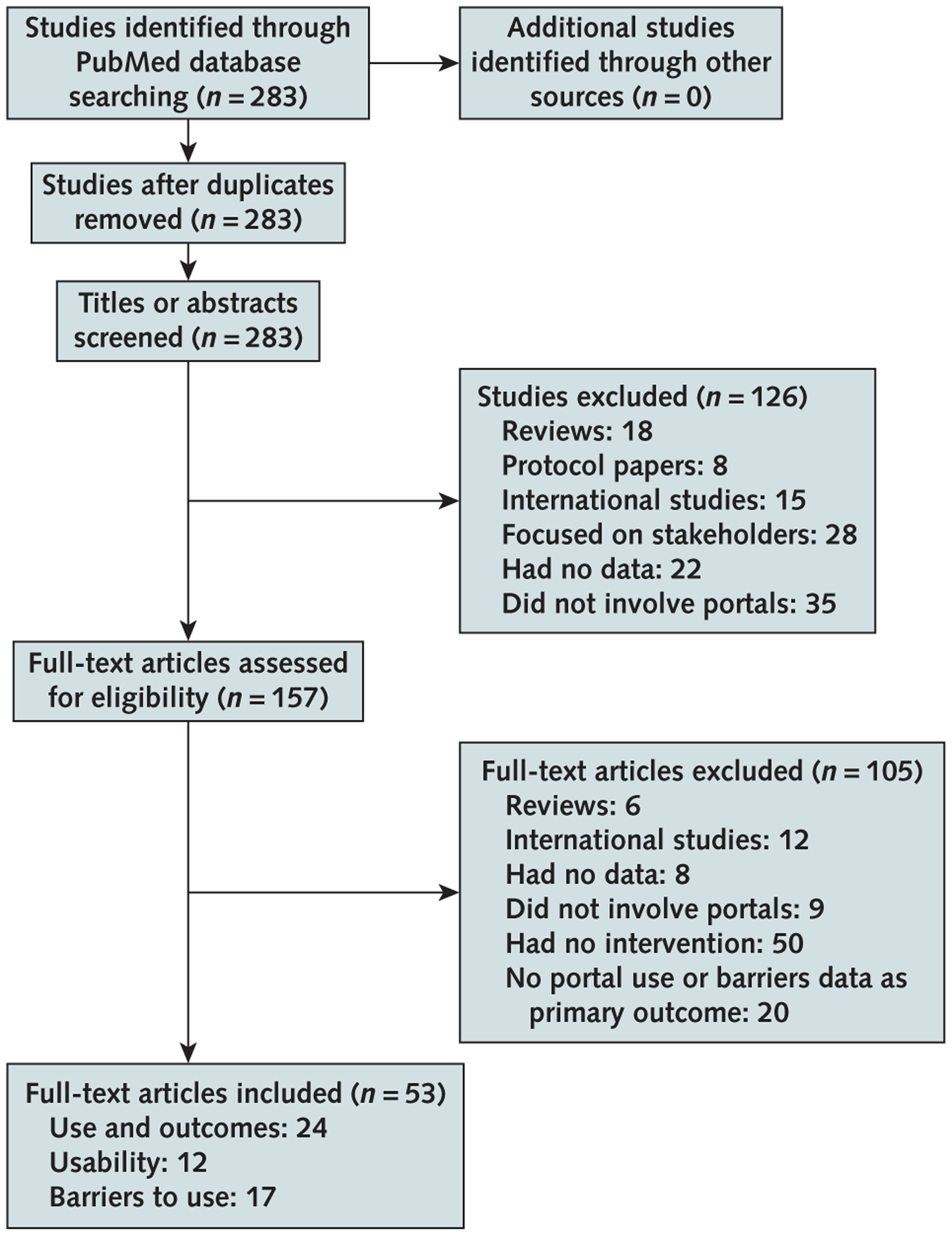
Study flow diagram.
Appendix Table 1.
Search Strategy
| Date | Database Searched | Search Strategy | Results, n |
|---|---|---|---|
| 1 September 2013 to 4 June 2019 | PubMed | (“self management”[tiab] OR engaged[tiab] OR engagement[tiab] OR engages[tiab] OR engage[tiab] OR engaging[tiab] OR “user uptake”[tiab] OR “self help”[tiab] OR “Patient Participation”[Mesh]) AND (“patient portal”[tiab] OR “patient portals”[tiab] OR “portal use”[tiab] OR “online portal”[tiab] OR “online portals”[tiab]) AND (“2013/09/01”[PDat] : “2019/06/04”[PDat]) |
283 |
Appendix Table 2.
Studies of Patient Portal Use and Related Outcomes
| Study, Year (Reference) | Design (Sample Size)* | Setting and Population | Intervention | Findings |
|---|---|---|---|---|
| Interventions delivered via the portal | ||||
| Bell et al, 2018 (20) | Quantitative (n = 17 133) EHR and use data |
Single multispecialty academic, adult orthopedic practice in Philadelphia | Portal utilization: patient-reported outcomes | Use 82% of patients logged in at least once during the 30-mo study period Intervention participation 42% to 52% completed patient-reported outcomes, and 30% sent at least one message Lower uptake among older patients, but improved uptake in all age groups on mobile platform versus browser |
| Bose-Brill et al, 2018 (21) | Quantitative (n = 419) Prospective, quasi-experimental analysis of EHR and use data |
Older patients (≥50 y) in 2 Columbus, Ohio, clinics | Portal utilization: advanced care planning module | Intervention participation 20% of intervention patients responded, one half of whom then had advance care planning documentation rates and improved quality at follow up (significantly higher than control group) |
| Krist et al, 2017 (22); Woolf et al, 2018 (27) | Quantitative (n = 11 458) EHR and use data |
12 primary care practices in northern Virginia | Portal utilization: cancer screening modules | Use About one fifth of the unique portal users had to make a decision about 1 of the 3 selected screenings Intervention participation 21% started the module, and 8% of these patients completed the decision module 41% of them felt the module made their appointment more productive Lower use among women, those without prior cancer screening, Hispanic patients, Asian patients, non-English-speaking patients, and uninsured patients |
| Pecina et al, 2017 (23) | Quantitative (n = 1769) Subgroup analysis of larger collaborative care intervention EHR and use data |
Large, academic medical center in Minnesota | Portal utilization: communication with depression care providers | Use Higher use among younger, married, and female users Intervention participation 15% of patients analyzed used the portal to communicate with their care managers Portal users were more likely to complete the depressive screening at 6 mo (76% vs. 66%) |
| Quinn et al, 2018 (24) | Quantitative Subgroup analysis of RCT (107 patients with diabetes) Qualitative Secure messages (4109 messages) |
26 primary care clinics in Maryland | Portal utilization: secure messaging with diabetes educator | Intervention participation 77% of intervention group participants messaged during the intervention period Many messages were about glucose monitoring and self-care Other outcomes Better glycemic control among those sending messages versus those who did not |
| Raghu et al, 2015 (25) | Quantitative (n = 18 702) EHR and use data |
Large outpatient clinics in Arizona | Portal utilization: updating medication lists via secure message | Intervention participation Around 50% responded to either telephone or secure message requests, but demographic patterns of who was using portals differed |
| Thompson et al, 2018 (26) | Quantitative (n = 257) Surveys: patients with visits to clinic |
Academic clinic in Florida primarily serving adolescents with Medicaid | Portal utilization: survey delivered via portal | Intervention participation Only 3 participants fully completed either survey, but more than one quarter of both groups read the survey e-mail |
| Programs to improve portal use | ||||
| Dalal et al, 2016 (28) | Quantitative Use data (120 patient-caregiver dyads; 239 total) System usability and satisfaction survey (10 patients and 8 caregivers) Qualitative Patients’ goals, preferences, concerns and content of secure messages |
Inpatient MICU and oncology unit (patients and caregivers) Large academic hospital in Boston |
Portal education (inpatient) and portal implementation evaluation | Use 66% of participants used the goal setting and/or the secure messaging features Other outcomes Positive usability and satisfaction ratings Specific suggestions for portal functionality improvement (e.g., highlight abnormal test results and increase clinician portal knowledge) Digital and logistical barriers to adoption |
| Dykes et al, 2017 (43) | Quantitative (2105 admissions [1030at baseline, 1075 during intervention]) EHR and use data |
MICU patients at a large tertiary care center | Portal education and implementation evaluation (inpatient) | Use 18% of patients admitted during the intervention enrolled onto the portal Other outcomes Higher enrollment among patients who were white, younger, and privately insured Aggregate rate of adverse events decreased by 29% during the intervention period Patient satisfaction increased from 72% to 93% Care partner satisfaction increased from 84% to 90% |
| Fiks et al, 2016 (29) | Quantitative Use data (n = 237) Monthly surveys via portal Qualitative Interviews (n = 22) Focus groups (n = 10) |
Pediatric (6–12 years) asthma patients’ parents/guardians 20 primary care sites in 11 states |
Portal implementation evaluation | Use 2.6% of invited families used the portal, most because of a mailed letter invitation Other outcomes Use of portal was associated with more medication changes and primary care visits at follow-up |
| Greysen et al, 2018 (39) | Quantitative Prospective, randomized intervention Use data, observations, and patient satisfaction (n = 97) |
Adult patients admitted to hospitalist service at large academic medical center in San Francisco | Patient education (inpatient randomization to usual care vs. brief training) and assistance with registration/log-in via tablets at the bedside | Use 58% logged into the portal at least once within 7 d of discharge; no differences between study groups Other outcomes Observed ability to view provider messaging higher in training group (92% vs. 77%) 88% were satisfied or very satisfied |
| Kamo et al, 2017 (30) | Quantitative Use data and cohort analysis (n = 189 723) Patient satisfaction surveys (n = 465) |
Integrated urban health care delivery system in the Pacific Northwest | Portal implementation evaluation | Use 39% of patients seen within a 12-mo period had enrolled onto the portal Other outcomes Patient portal enrollees were likely to be urban, white, younger, female patients 41% of survey respondents rated their portal experience as excellent |
| Kelly et al, 2017 (31) | Quantitative Use data (n = 296) Parent survey (n = 90) |
Preteen inpatients and their families at a tertiary children’s hospital inWisconsin | Portal implementation evaluation (inpatient) | Use 90% of parents offered the acute care portal used it 176 requests (29% of patients) and 36 messages (5% of patients) Other outcomes 89% of survey respondents felt the portal reduced errors in their child’s health care 60% said the portal improved communications with their child’s provider |
| Kidwell et al, 2018 (40) | Quantitative Use data (n = 44) Qualitative Patient ratings of ease of use and usefulness |
Adolescents and young adults with sickle cell disease in clinics throughout the Midwest | Portal education program (homework for patients to complete via portal over time) |
Use All patient logged on at least once, with 46% continuing to use the portal after 2 mo Other outcomes 90% rated portal as high quality, 77% rated it as very easy to use, and 81% agreed it was useful or very useful No clear effects on portal use on medical decision making or patient-provider communication |
| Krist et al, 2014 (32) | Quantitative Use data (n = 28 910) Clinician and patient surveys Qualitative Staff training session transcripts (n = 7) Exit interviews |
Eight primary care practices in Virginia | Portal implementation evaluation | Use 26% of patients seen within the study period created a portal account, with consistent rates across all clinic sites after broad implementation efforts Higher uptake among older patients and patients with multiple comorbidities, and lower uptake among underrepresented minorities Other outcomes Clinicians’ and staffs’ previous negative experiences with informatics tools were a barrier to implementing the portal successfully |
| McCleary et al, 2018 (33) | Quantitative Patient surveys (n = 1019) Qualitative Focus groups with patients and staff (n = 25) |
Ambulatory oncology practices at academic cancer treatment center in Boston | Portal implementation evaluation and staffing education/support | Use Intervention increased patient portal enrollment by 6% to 53% over 2 mo Other outcomes Barriers reported in terms of computer access, difficulty signing up, and lack of awareness of the benefits |
| O’Leary et al, 2016 (34) | Quantitative Site-randomized portal intervention Use data (100 intervention participants and 102 control participants) Patient satisfaction questionnaires Qualitative Structured patient and provider interviews (n = 100) |
Large academic hospital in Chicago | Portal education (inpatient) and effectiveness evaluation | Use 57% used the portal more than once daily Other outcomes A higher percentage of intervention unit patients could identify their care team and roles than the control group No difference in knowledge about procedures, tests, or medications No difference in patient activation Patients often allow surrogates to use their portal account |
| Ramsey et al, 2018 (35) | Quantitative Survey data (n = 96) |
Adolescent practice in urban Maryland | Portal implementation evaluation | Use 88% of approached patients enrolled in the patient portal High enrollment rates among black patients that reflect the overall clinic population |
| Ratliff-Schaub and Valleru, 2017 (41) | Quantitative Pre-post analysis (total clinicsize, 1700 children annually) |
Pediatric clinic serving patients with chronic illness in Columbus, Ohio | Portal implementation evaluation (targeting staff commitment, workflow, and family awareness) | Use Percentage of patient visits increased from 2% to 30% over the quality improvement cycle work and was maintained for 16 months |
| Shaw et al, 2017 (38) | Quantitative Utilization survey data at 3 points in time (n = 14) |
Admitted patients undergoing a cardiac procedure | Portal education program with training delivered by nurse navigators |
Use 36% of patients self-reported using a portal feature Almost one fifth of patients watched an assigned health video via the portal |
| Sorondo et al, 2016 (36) | Quantitative Prospective, quasi-experimental analysis (n = 96) |
5 primary care sites in eastern Maine | Portal education and effectiveness evaluation | Use 79% of enrolled patients used the portal during the follow-up study period Other outcomes No change in self-efficacy or health perceptions, but potential improvement in functional status and emergency visits |
| Stein et al, 2018 (42) | Quantitative Prospective, randomized analysis intervention of portal education on subsequent portal use (n = 70) |
Public hospital in Seattle | Portal education to train hospitalized patients to access discharge summaries | Use 48% of trained patients and 11% of the control group registered for the portal Other outcomes Only 43% of eligible patients had working e-mail addresses to be able to be included in this study 80% to 85% of patients in both study groups preferred hospitals with access to an online patient portal |
| Toscos et al, 2016 (37) | Quantitative Prospective, quasi-experimental analysis (n = 200) |
Large cardiology practice in Indiana | Portal education and effectiveness evaluation | Use 81% of patients logged in ≥4 times over 12 mo Other outcomes No change in patient activation between groups High portal users had lower hemoglobin A1c values at follow-up |
EHR = electronic health record; MICU = medical intensive care unit; RCT = randomized controlled trial.
Unless otherwise specified, sample sizes are the number of patients.
Appendix Table 3.
Studies of Portal Usability
| Study, Year (Reference) | Design (Sample Size) | Setting and Population | Intervention | Findings |
|---|---|---|---|---|
| Observational testing or piloting | ||||
| Alpert et al, 2016 (44) | Qualitative Recall interviews with patients (n = 31) Two provider focus groups (n = 13) |
2 primary care practices in Virginia | Overall portal evaluation | 73% of recalled incidents were negative Negative patient findings: lack of personalization, need for more functionality, need for more knowledge to understand laboratory data Provider negative findings: lack of feedback, increase on workload, inappropriate patient use Patients liked instant and clear information, and providers liked potential for patient empowerment and increased efficiency |
| Arcia, 2017 (45) | Quantitative Use data (n = 12) Usability/satisfaction surveys (n = 16) Qualitative 4 focus groups (n = 16) |
Safety-net clinics in New York City Spanish-speaking and English-speaking pregnant women enrolled in Medicaid |
Secure messages with educational content | Use 75% of participants had logged into the portal during the 4-mo study period Portal feedback Satisfaction and usability were rated highly Spanish speakers needed more assistance in navigating e-mail, logging in Participants overall desired easier portal log-in without passwords |
| Czaja et al, 2015 (46) | Observational interviews (n = 54) | 3 safety-net clinics in New York City | Overall portal evaluation; 3 different platforms | Diverse patients faced barriers to using the system, especially in terms of complex navigation and medical terminology for those with limited health literacy High ratings and interest in portals overall |
| Martinez et al, 2018 (52) | Observational interviews (n = 14 over 3 rounds) | Vanderbilt University adult primary care clinic | Design and evaluation of a diabetes dashboard embedded within the portal | Computer system usability improved from initial to final prototype rounds Specific changes included examples such as increasing font size, as well as adding reminders and star ratings to the dashboard for personalization |
| Morrow et al, 2017 (47) | Observational interviews (n = 12 and n = 24 in 2 rounds) | Older adults patients in Indiana | Secure message content displaying laboratory results | Patients understood video messages well and were satisfied with synthetic voice used to deliver test result information |
| Nystrom et al, 2018 (48) | Observational interviews and usability questionnaires (n = 14) | Participants recruited via e-mail (location not specified) | Laboratory test displays | Iterative rounds of feedback on test result graphical displays (such as out-of-range lipid levels), with corresponding changes in system usability scale with design changes Final version had improved clickability and navigation, along with simpler/less confusing layout related to normal versus abnormal results |
| Portz et al, 2019 (53) | Observational interviews (n = 24, 15 of which were portal users and 9 were nonusers) | Older adults with multiple chronic conditions at Kaiser Permanente Colorado | Overall portal evaluation | Observed barriers to portal tasks Overall digital literacy anxiety and lack of awareness of features Nonusers identified problems with font size and colors Users identified problems with registration, logging in, and scheduling appointments |
| Taha et al, 2014 (51) | Observational interviews and questionnaire (n = 51) | Community sample of older adults in Miami | Overall portal evaluation | Observed barriers to many portal tasks, especially for those with limited numeracy and lack of previous Internet experience |
| Tieu et al, 2017 (49) | Observational interviews and usability questionnaire (n = 25) | San Francisco primary care public health care setting | Overall portal evaluation | Those with limited health literacy were significantly more likely to need assistance in completing portal tasks and faced basic computer barriers High interest in portals was expressed by patients overall |
| Yen et al, 2018 (50) | Observational interviews (n = 19) | Midwestern academic medical center with 6 hospitals | Overall portal evaluation | Most difficulty in exiting a specific section of the Web site and finding the right tab with the appropriate medical information Highest number of errors among the oldest participants |
| Patient reports | ||||
| Mackert et al, 2016 (54) | Surveys (n = 4974) | Online national sample of respondents from an existing research platform | Assessed ease of use and usefulness of apps, trackers, and portals | Patients with limited health literacy associated with decreased use and lower ease of use and usefulness of portals, along with higher misperceptions about privacy |
| Nazi et al, 2018 (55) | Surveys (n = 200 624) | Veterans Affairs patients using the portal nationwide | Assessed current user experiences with pop-up survey | Patients liked tracking of prescription refills, but did not like lack of session time-out warnings and overall poor navigation Future decisions under way to increase proxy portal access |
Appendix Table 4.
Studies of Barriers to Portal Use
| Study, Year (Reference) | Design (Sample Size)* | Setting and Population | Intervention | Participant Concerns and Desires |
|---|---|---|---|---|
| Studies assessing patient experiences | ||||
| Colorafi et al, 2018 (62) | 40 patients Quantitative Survey Qualitative Visit observation Interviews |
Older adults from 2 urban cardiac clinics in Arizona | Discussion of AVS | Digital literacy and access Privacy and security |
| Giardina et al, 2015 (64) | Qualitative Interviews (n = 13) |
Patients and caregivers in the Houston VA system | Discussion of abnormal test results | Support to interpret medical information Timeliness of information |
| Gerard et al, 2017 (63) | Qualitative Open-ended responses within online platform (n = 260) |
Primary care patients at an academic hospital system in Boston | Discussion of visit note and care plan | Want to contribute own data and share data with others |
| Haun et al, 2017 (65) | Qualitative (n = 48) Focus groups Simulations |
Patients and caregivers from the VA health systems in Bedford, Massachusetts, and Tampa, Florida | Discussion of the overall VA HIT system | New features Virtual visits Better functionality and standardization Security and privacy More education and training needed |
| Hefner et al, 2019 (71) | Qualitative Three focus groups (n = 17) |
Patients with a cardiopulmonary condition at a large academic medical center in the Midwest | Discussion of experiences using portal secure messaging | Digital literacy/access More education/training needed Concern about provider engagement |
| Irizarry et al, 2017 (66) | Quantitative Surveys (n = 100) Qualitative 4 focus groups (n = 23) |
Community-based sample in Pittsburgh with varying health literacy and portal use experience | Discussion on overall portal interest and usefulness | Digital literacy and access Preference for in-person communication More education/training needed |
| Kim and Fadem, 2018 (69) | Qualitative Focus groups (n = 17) |
Convenience sample of older adults in New Jersey | Discussion on overall portal interest and specific features | Preference for in-person communication More education/training needed Concern about provider engagement |
| Mishuris et al, 2015 (67) |
n = 19 Qualitative In-depth interviews Quantitative Survey |
Home-based primary care patients, caregivers, and staff in the Boston VA system | Discussion on overall portal interest and usefulness | Digital literacy and access More education/training needed Satisfied with current care delivery methods Want to share data with others |
| Price-Haywood et al, 2017 (72) | Quantitative Cross-sectional survey (n = 247) |
Older adults with hypertension or diabetes at a large, integrated health delivery system | Discussion on overall interest and experiences with portals | Digital literacy/access Need for simpler interface Need for increased awareness |
| Sadasivaiah et al, 2019 (70) | Mixed methods (n = 16 507) Overall interest in portal registration (yes/no) Documentation and coding of specific reasons for noninterest |
Inpatients at a large public hospital in San Francisco | Specific documentation of interest and noninterest in portal use documented in the EHR among nurses | Low interest Digital literacy and access Physical or mental barriers Security and privacy |
| Tieu et al, 2015 (68) | Qualitative In-depth interviews (n = 16) |
Patients and caregivers in the San Francisco safety-net system | Discussion on overall portal interest and usefulness | Digital literacy and access Health literacy Security and privacy Preference for in-person communication Want to share data with others Better functionality and standardization |
| Studies assessing patient and provider experiences | ||||
| Alpert et al, 2018 (56) | Qualitative Interviews (35 patients and 13 oncologists) |
National Cancer Center in central Virginia | Participants provide feedback about portal usefulness and communication practices | Digital literacy and access Health literacy |
| Black et al, 2015 (57) | Qualitative Interviews (10 patients) 6 focus groups (21 patients and 13 providers) |
Asthma clinics in urban Philadelphia | Participants review AVS features and portal | More education/training needed Better functionality and standardization Digital access and literacy |
| Ochoa et al, 2017 (58) | Quantitative Surveys (400 patients and 59 providers) |
Safety-net health care system in Los Angeles | Participants provide feedback about portal adoption | Digital access and literacy (among a subset) Limited interest from providers |
| O’Leary et al, 2016 (59) | Qualitative Interviews (18 patients) 3 focus groups (21 providers) |
Large academic hospital in Chicago | Participants provide feedback about portal usefulness | Digital access and literacy Need for new features |
| Pillemer et al, 2016 (60) | Quantitative Use data Surveys (n = 6368) Qualitative Interviews (13 patients) |
Large, integrated delivery system in Western Pennsylvania | Participants provide feedback about their experience with the portal | Increased patient anxiety |
| Sieck et al, 2017 (61) | Qualitative Interviews (29 patients and 13 providers) |
Primary care offices at a large academic medical center in Ohio | Participants provide feedback about portal usefulness | More education and training are needed |
AVS = after-visit summary; EHR = electronic health record; HIT = health information technology; VA = Veterans Affairs.
Unless otherwise specified, sample sizes are the number of patients.
Footnotes
Disclosures: Dr. Nelson reports stock from QDM outside the submitted work. Authors not named here have disclosed no conflicts of interest. Disclosures can also be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M19-0876.
References
- 1.Tang PC, Ash JS, Bates DW, et al. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006. Mar-Apr;13:121–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mandel JC, Kreda DA, Mandl KD, et al. SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. J Am Med Inform Assoc. 2016;23:899–908. doi: 10.1093/jamia/ocv189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Delbanco T, Walker J, Darer JD, et al. Open notes: doctors and patients signing on. Ann Intern Med. 2010;153:121–5. doi: 10.7326/0003-4819-153-2-201007200-00008 [DOI] [PubMed] [Google Scholar]
- 4.U.S. Government Accountability Office. Health information technology: HHS should assess the effectiveness of its efforts to enhance patient access to and use of electronic health information. Washington, DC: U.S. Government Accountability Office; March 2017. Accessed at www.gao.gov/products/GAO-17-305?utm_source=blog&utm_medium=social&utm_campaign=watchblog on 28 September 2019. [Google Scholar]
- 5.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010;363:501–4. doi: 10.1056/NEJMp1006114 [DOI] [PubMed] [Google Scholar]
- 6.Holden RJ, Kulanthaivel A, Purkayastha S, et al. Know thy eHealth user: development of biopsychosocial personas from a study of older adults with heart failure. Int J Med Inform. 2017;108:158–67. doi: 10.1016/j.ijmedinf.2017.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grossman LV, Choi SW, Collins S, et al. Implementation of acute care patient portals: recommendations on utility and use from six early adopters. J Am Med Inform Assoc. 2018;25:370–9. doi: 10.1093/jamia/ocx074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dhanireddy S, Walker J, Reisch L, et al. The urban underserved: attitudes towards gaining full access to electronic medical records. Health Expect. 2014;17:724–32. doi: 10.1111/j.1369-7625.2012.00799.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ralston JD, Hirsch IB, Hoath J, et al. Web-based collaborative care for type 2 diabetes: a pilot randomized trial. Diabetes Care. 2009;32: 234–9. doi: 10.2337/dc08-1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lyles CR, Harris LT, Jordan L, et al. Patient race/ethnicity and shared medical record use among diabetes patients. Med Care. 2012;50:434–40. doi: 10.1097/MLR.0b013e318249d81b [DOI] [PubMed] [Google Scholar]
- 11.Coughlin SS, Carbone LD, Heboyan V, et al. Use of My Healthe-Vet patient web portal among veterans seen for diabetes mellitus at a medical center in the southeastern United States. Mhealth. 2017;3: 50. doi: 10.21037/mhealth.2017.10.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenberg AJ, Falisi AL, Finney Rutten LJ, et al. Access to electronic personal health records among patients with multiple chronic conditions: a secondary data analysis. J Med Internet Res. 2017;19: e188. doi: 10.2196/jmir.7417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Graetz I, Gordon N, Fung V, et al. The digital divide and patient portals: internet access explained differences in patient portal use for secure messaging by age, race, and income. Med Care. 2016;54: 772–9. doi: 10.1097/MLR.0000000000000560 [DOI] [PubMed] [Google Scholar]
- 14.Bush RA, Richardson AC, Cardona-Grau D, et al. Patient portal usage in pediatric urology: is it meaningful use for everyone? Urol Pract. 2018;5:279–85. doi: 10.1016/j.urpr.2017.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mook PJ, Trickey AW, Krakowski KE, et al. Exploration of portal activation by patients in a healthcare system. Comput Inform Nurs. 2018;36:18–26. doi: 10.1097/CIN.0000000000000392 [DOI] [PubMed] [Google Scholar]
- 16.Woods SS, Forsberg CW, Schwartz EC, et al. The association of patient factors, digital access, and online behavior on sustained patient portal use: a prospective cohort of enrolled users. J Med Internet Res. 2017;19:e345. doi: 10.2196/jmir.7895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goldzweig CL, Orshansky G, Paige NM, et al. Electronic patient portals: evidence on health outcomes, satisfaction, efficiency, and attitudes: a systematic review. Ann Intern Med. 2013;159:677–87. doi: 10.7326/0003-4819-159-10-201311190-00006 [DOI] [PubMed] [Google Scholar]
- 19.Kruse CS, Bolton K, Freriks G. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res. 2015;17:e44. doi: 10.2196/jmir.3171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bell K, Warnick E, Nicholson K, et al. Patient adoption and utilization of a web-based and mobile-based portal for collecting outcomes after elective orthopedic surgery. Am J Med Qual. 2018. Nov-Dec;33:649–56. doi: 10.1177/1062860618765083 [DOI] [PubMed] [Google Scholar]
- 21.Bose-Brill S, Feeney M, Prater L, et al. Validation of a novel electronic health record patient portal advance care planning delivery system. J Med Internet Res. 2018;20:e208. doi: 10.2196/jmir.9203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krist AH, Woolf SH, Hochheimer C, et al. Harnessing information technology to inform patients facing routine decisions: cancer screening as a test case. Ann Fam Med. 2017;15:217–24. doi: 10.1370/afm.2063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pecina J, North F, Williams MD, et al. Use of an on-line patient portal in a depression collaborative care management program. J Affect Disord. 2017;208:1–5. doi: 10.1016/j.jad.2016.08.034 [DOI] [PubMed] [Google Scholar]
- 24.Quinn CC, Butler EC, Swasey KK, et al. Mobile diabetes intervention study of patient engagement and impact on blood glucose: mixed methods analysis. JMIR Mhealth Uhealth. 2018;6:e31. doi: 10.2196/mhealth.9265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raghu TS, Frey K, Chang YH, et al. Using secure messaging to update medications list in ambulatory care setting. Int J Med Inform. 2015;84:754–62. doi: 10.1016/j.ijmedinf.2015.06.003 [DOI] [PubMed] [Google Scholar]
- 26.Thompson LA, Mercado R, Martinko T, et al. Novel interventions and assessments using patient portals in adolescent research: confidential survey study. J Med Internet Res. 2018;20:e101. doi: 10.2196/jmir.8340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Woolf SH, Krist AH, Lafata JE, et al. Engaging patients in decisions about cancer screening: exploring the decision journey through the use of a patient portal. Am J Prev Med. 2018;54:237–47. doi: 10.1016/j.amepre.2017.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dalal AK, Dykes PC, Collins S, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: a preliminary evaluation. J Am Med Inform Assoc. 2016;23: 80–7. doi: 10.1093/jamia/ocv093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fiks AG, DuRivage N, Mayne SL, et al. Adoption of a portal for the primary care management of pediatric asthma: a mixed-methods implementation study. J Med Internet Res. 2016;18:e172. doi: 10.2196/jmir.5610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kamo N, Bender AJ, Kalmady K, et al. Meaningful use of the electronic patient portal – Virginia Mason’s journey to create the perfect online patient experience. Healthc (Amst). 2017;5:221–6. doi: 10.1016/j.hjdsi.2016.09.003 [DOI] [PubMed] [Google Scholar]
- 31.Kelly MM, Hoonakker PL, Dean SM. Using an inpatient portal to engage families in pediatric hospital care. J Am Med Inform Assoc. 2017;24:153–61. doi: 10.1093/jamia/ocw070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krist AH, Woolf SH, Bello GA, et al. Engaging primary care patients to use a patient-centered personal health record. Ann Fam Med. 2014. Sep-Oct;12:418–26. doi: 10.1370/afm.1691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCleary NJ, Greenberg TL, Barysauskas CM, et al. Oncology patient portal enrollment at a comprehensive cancer center: a quality improvement initiative. J Oncol Pract. 2018;14:e451–61. doi: 10.1200/JOP.17.00008 [DOI] [PubMed] [Google Scholar]
- 34.O’Leary KJ, Lohman ME, Culver E, et al. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. J Am Med Inform Assoc. 2016;23: 159–65. doi: 10.1093/jamia/ocv058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramsey A, Lanzo E, Huston-Paterson H, et al. Increasing patient portal usage: preliminary outcomes from the MyChart genius project.JAdolescHealth.2018;62:29–35. doi: 10.1016/j.jadohealth.2017.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sorondo B, Allen A, Fathima S, et al. Patient portal as a tool for enhancing patient experience and improving quality of care in primary care practices. EGEMS (Wash DC). 2016;4:1262. doi: 10.13063/2327-9214.1262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Toscos T, Daley C, Heral L, et al. Impact of electronic personal health record use on engagement and intermediate health outcomes among cardiac patients: a quasi-experimental study. J Am Med Inform Assoc. 2016;23:119–28. doi: 10.1093/jamia/ocv164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shaw CL, Casterline GL, Taylor D, et al. Increasing health portal utilization in cardiac ambulatory patients: a pilot project. Comput Inform Nurs. 2017;35:512–9. doi: 10.1097/CIN.0000000000000361 [DOI] [PubMed] [Google Scholar]
- 39.Greysen SR, Harrison JD, Rareshide C, et al. A randomized controlled trial to improve engagement of hospitalized patients with their patient portals. J Am Med Inform Assoc. 2018;25:1626–33. doi: 10.1093/jamia/ocy125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kidwell KM, Peugh J, Westcott E, et al. Acceptability and feasibility of a disease-specific patient portal in adolescents with sickle cell disease. J Pediatr Hematol Oncol. 2018. doi: 10.1097/MPH.0000000000001341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ratliff-Schaub K, Valleru J. Increasing patient portal activation in a pediatric subspecialty clinic. Pediatr Qual Saf. 2017. Nov-Dec;2: e049. doi: 10.1097/pq9.0000000000000049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stein JN, Klein JW, Payne TH, et al. Communicating with vulnerable patient populations: a randomized intervention to teach inpatients to use the electronic patient portal. Appl Clin Inform. 2018;9: 875–83. doi: 10.1055/s-0038-1676333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dykes PC, Rozenblum R, Dalal A, et al. Prospective evaluation of a multifaceted intervention to improve outcomes in intensive care: the Promoting Respect and Ongoing Safety Through Patient Engagement Communication and Technology Study. Crit Care Med. 2017;45:e806–13. doi: 10.1097/CCM.0000000000002449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Alpert JM, Krist AH, Aycock RA, et al. Applying multiple methods to comprehensively evaluate a patient portal’s effectiveness to convey information to patients. J Med Internet Res. 2016;18:e112. doi: 10.2196/jmir.5451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arcia A. Time to push: use of gestational age in the electronic health record to support delivery of relevant prenatal education content. EGEMS (Wash DC). 2017;5:5. doi: 10.13063/2327-9214.1281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Czaja SJ, Zarcadoolas C, Vaughon WL, et al. The usability of electronic personal health record systems for an underserved adult population. Hum Factors. 2015;57:491–506. doi: 10.1177/0018720814549238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Morrow D, Hasegawa-Johnson M, Huang T, et al. A multidisciplinary approach to designing and evaluating electronic medical record portal messages that support patient self-care. J Biomed Inform. 2017;69:63–74. doi: 10.1016/j.jbi.2017.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nystrom DT, Singh H, Baldwin J, et al. Methods for patient-centered interface design of test result display in online portals. EGEMS (Wash DC). 2018;6:15. doi: 10.5334/egems.255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tieu L, Schillinger D, Sarkar U, et al. Online patient websites for electronic health record access among vulnerable populations: portals to nowhere? J Am Med Inform Assoc. 2017;24:e47–54. doi: 10.1093/jamia/ocw098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yen PY, Walker DM, Smith JMG, et al. Usability evaluation of a commercial inpatient portal. Int J Med Inform. 2018;110:10–8. doi: 10.1016/j.ijmedinf.2017.11.007 [DOI] [PubMed] [Google Scholar]
- 51.Taha J, Sharit J, Czaja SJ. The impact of numeracy ability and technology skills on older adults’ performance of health management tasks using a patient portal. J Appl Gerontol. 2014;33:416–36. doi: 10.1177/0733464812447283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martinez W, Threatt AL, Rosenbloom ST, et al. A patient-facing diabetes dashboard embedded in a patient web portal: design sprint and usability testing. JMIR Hum Factors. 2018;5:e26. doi: 10.2196/humanfactors.9569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Portz JD, Bayliss EA, Bull S, et al. Using the technology acceptance model to explore user experience, intent to use, and use behavior of a patient portal among older adults with multiple chronic conditions: descriptive qualitative study. J Med Internet Res. 2019; 21:e11604. doi: 10.2196/11604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mackert M, Mabry-Flynn A, Champlin S, et al. Health literacy and health information technology adoption: the potential for a new digital divide. J Med Internet Res. 2016;18:e264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nazi KM, Turvey CL, Klein DM, et al. A decade of veteran voices: examining patient portal enhancements through the lens of user-centered design. J Med Internet Res. 2018;20:e10413. doi: 10.2196/10413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Alpert JM, Morris BB, Thomson MD, et al. Identifying how patient portals impact communication in oncology. Health Commun. 2018: 1–9. doi: 10.1080/10410236.2018.1493418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Black H, Gonzalez R, Priolo C, et al. True “meaningful use”: technology meets both patient and provider needs. Am J Manag Care. 2015;21:e329–37. [PubMed] [Google Scholar]
- 58.Ochoa A 3rd, Kitayama K, Uijtdehaage S, et al. Patient and provider perspectives on the potential value and use of a bilingual online patient portal in a Spanish-speaking safety-net population. J Am Med Inform Assoc. 2017;24:1160–4. doi: 10.1093/jamia/ocx040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.O’Leary KJ, Sharma RK, Killarney A, et al. Patients’ and healthcare providers’ perceptions of a mobile portal application for hospitalized patients. BMC Med Inform Decis Mak. 2016;16:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pillemer F, Price RA, Paone S, et al. Direct release of test results to patients increases patient engagement and utilization of care. PLoS One. 2016;11:e0154743. doi: 10.1371/journal.pone.0154743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sieck CJ, Hefner JL, Schnierle J, et al. The rules of engagement: perspectives on secure messaging from experienced ambulatory patient portal users. JMIR Med Inform. 2017;5:e13. doi: 10.2196/medinform.7516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Colorafi K, Greenes RA, Kates M. Preferences of older adults and their families for meaningful use clinical summaries. Mhealth. 2018; 4:8. doi: 10.21037/mhealth.2018.03.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gerard M, Fossa A, Folcarelli PH, et al. What patients value about reading visit notes: a qualitative inquiry of patient experiences with their health information. J Med Internet Res. 2017;19:e237. doi: 10.2196/jmir.7212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Giardina TD, Modi V, Parrish DE, et al. The patient portal and abnormal test results: an exploratory study of patient experiences. Patient Exp J. 2015;2:148–54. [PMC free article] [PubMed] [Google Scholar]
- 65.Haun JN, Chavez M, Nazi K, et al. Veterans’ preferences for exchanging information using Veterans Affairs health information technologies: focus group results and modeling simulations. J Med Internet Res. 2017;19:e359. doi: 10.2196/jmir.8614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Irizarry T, Shoemake J, Nilsen ML, et al. Patient portals as a tool for health care engagement: a mixed-method study of older adults with varying levels of health literacy and prior patient portal use. J Med Internet Res. 2017;19:e99. doi: 10.2196/jmir.7099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mishuris RG, Stewart M, Fix GM, et al. Barriers to patient portal access among veterans receiving home-based primary care: a qualitative study. Health Expect. 2015;18:2296–305. doi: 10.1111/hex.12199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tieu L, Sarkar U, Schillinger D, et al. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Internet Res. 2015;17: e275. doi: 10.2196/jmir.4847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kim S, Fadem S. Communication matters: exploring older adults’ current use of patient portals. Int J Med Inform. 2018;120:126–36. doi: 10.1016/j.ijmedinf.2018.10.004 [DOI] [PubMed] [Google Scholar]
- 70.Sadasivaiah S, Lyles CR, Kiyoi S, et al. Disparities in patient-reported interest in web-based patient portals: survey at an urban academic safety-net hospital. J Med Internet Res. 2019;21:e11421. doi: 10.2196/11421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hefner JL, MacEwan SR, Biltz A, et al. Patient portal messaging for care coordination: a qualitative study of perspectives of experienced users with chronic conditions. BMC Fam Pract. 2019;20:57. doi: 10.1186/s12875-019-0948-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Price-Haywood EG, Harden-Barrios J, Ulep R, et al. EHealth literacy: patient engagement in identifying strategies to encourage use of patient portals among older adults. Popul Health Manag. 2017;20: 486–94. doi: 10.1089/pop.2016.0164 [DOI] [PubMed] [Google Scholar]
- 73.Perez S. Nearly 1 in 4 people abandon mobile apps after only one use. TechCrunch. 31 May 2016. Accessed at https://techcrunch.com/2016/05/31/nearly-1-in-4-people-abandon-mobile-apps-after-only-one-use on 21 June 2019. [Google Scholar]
- 74.Zweig M, Shen J, Jug L. Healthcare consumers in a digital transition. Rock Health. 2018. Accessed at https://rockhealth.com/reports/healthcare-consumers-in-a-digital-transition on 21 June 2019. [Google Scholar]
- 75.Dykes PC, Stade D, Chang F, et al. Participatory design and development of a patient-centered toolkit to engage hospitalized patients and care partners in their plan of care. AMIA Annu Symp Proc. 2014;2014:486–95. [PMC free article] [PubMed] [Google Scholar]
- 76.Anderson M, Perrin A, Jiang J. 10% of Americans don’t use the internet. Who are they? Fact Tank: Pew Research Center; 2018. Accessed at www.pewresearch.org/fact-tank/2019/04/22/some-americans-dont-use-the-internet-who-are-they on 21 June 2019. [Google Scholar]
- 77.Yardley L, Spring BJ, Riper H, et al. Understanding and promoting effective engagement with digital behavior change interventions. Am J Prev Med. 2016;51:833–42. doi: 10.1016/j.amepre.2016.06.015 [DOI] [PubMed] [Google Scholar]
- 78.Ackerman SL, Sarkar U, Tieu L, et al. Meaningful use in the safety net: a rapid ethnography of patient portal implementation at five community health centers in California. J Am Med Inform Assoc. 2017;24:903–12. doi: 10.1093/jamia/ocx015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Ancker JS, Mauer E, Hauser D, et al. Expanding access to high-quality plain-language patient education information through context-specific hyperlinks. AMIA Annu Symp Proc. 2016;2016:277–284. [PMC free article] [PubMed] [Google Scholar]
- 80.National Health Service. Transforming digital health. 2018. Accessed at www.nhsx.nhs.uk/key-information-and-tools/apps-and-tools on 21 September 2018.
- 81.Nelson EC, Dixon-Woods M, Batalden PB, et al. Patient focused registries can improve health, care, and science. BMJ. 2016;354: i3319. doi: 10.1136/bmj.i3319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lindblad S, Ernestam S, Van Citters AD, et al. Creating a culture of health: evolving healthcare systems and patient engagement. QJM. 2017;110:125–9. doi: 10.1093/qjmed/hcw188 [DOI] [PubMed] [Google Scholar]
- 83.Yamin CK, Emani S, Williams DH, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med. 2011;171:568–74. doi: 10.1001/archinternmed.2011.34 [DOI] [PubMed] [Google Scholar]


