Abstract
Background
The COVID-19 pandemic is caused by a severe acute respiratory syndrome coronavirus which emerged in Wuhan. Recently this virus has rapidly spread throughout Ethiopia. The current preventive measure practices and knowledge have gaps. Therefore this study aimed to assess COVID-19 preventive measure practices and knowledge of pregnant women in Guraghe Zone hospitals.
Methods and Materials
This cross-sectional study was conducted from July 27–August 27, 2020 among pregnant women in Guraghe zone hospitals. Systematic random sampling technique were employed to select 403 participants. Data were checked manually for completeness, cleaned, and stored in Epi Data and exported to SPSS for further analysis. Variables which have a P-value less than 0.25 on bivariate analysis were taken to multivariate analysis. A P-value of less than 0.05 and 95% confidence level was used as a cut-off point for presence of association in multivariate analysis.
Results
COVID-19 preventive measure practice and knowledge of pregnant women visiting Guraghe Zone hospitals was 76.2% and 54.84%, respectively. Those aged 20–24 (AOR=1.22, 95% CI=1.15–22.24), 25–29 (AOR=1.32, 95% CI=1.20–20.25), and 30–34 (AOR=2.57, 95% CI–2.32–43.38) were more likely to practice COVID-19 preventive measures. Those residing in urban area (AOR=2.16, 95% CI=1.24–3.77) and perceiving that COVID-19 is worst for people with chronic disease (AOR=5.12, 95% CI=1.73–15.17) were more likely to practice COVID-19 preventive measures.
Conclusion
COVID-19 preventive measure practices and knowledge were low. Age, residence, and perception of COVID-19 on chronic disease were independent factors associated with preventive measure practices. Pregnant women aged ≥35 need to be counseled on practices of preventing COVID-19 by their healthcare providers.
Keywords: COVID-19, Guraghe Zone, pregnant women, 2020
Introduction
In December 2019 a coronavirus (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged in Wuhan, China.1–5 The first cases were then reported from Thailand, Japan, and the Republic of Korea, and then devastating all over the world.6 On January 30, 2020 the Director‑General of WHO declared the 2019‑nCoV outbreak a public health emergency of international concern.7–10
COVID-19, as of June 2, 2020 had 6,403,439 cases and 378,113 deaths in the world, and 1,344 cases and 14 deaths in Ethiopia were recorded.11 The case fatality rate of SARS-CoV infection among pregnant women is up to 25%.12 COVID-19 mortality rate among pregnant mothers has been lower than that of SARS and MERS.13
The COVID-19 pandemic is causing huge stress on the healthcare system of all countries in the world, putting on both social and economic distresses.14–17 Despite the large and rapidly rising number of COVID-19 and resulting deaths, there are limited data about the clinical characteristics of pregnant women with the disease.2,–18–21 Although pregnant women do not seem to have an increased susceptibility to COVID−19 or more severe complications than non-pregnant adults, the available studies suggest that they may have the risk of adverse pregnancy outcomes.22,23
A study conducted in New York City shows more than one in eight asymptomatic patients who were admitted to the labor and delivery unit were positive for SARS-CoV-2.1 A case study conducted in the USA reports a high-risk pregnant woman who developed respiratory failure associated with COVID-19, possible vertical transmission of COVID-19 infection in this case.24 Pregnant women at all gestational ages, the gravida in labor, and the acutely ill parturient are at risk of this virus.1,25,26
Pregnancy is a physiological state that predisposes women to viral respiratory infection due to the physiological changes in the immune and cardiopulmonary systems.3,–27–29 Therefore, pregnant women and household members should be educated about personal hygiene, basic Infection Prevention and Control (IPC) measures, and how to care as safely as possible for the person suspected of having COVID−19 to prevent the infection from spreading to household contacts.6,13,14,30
Recently COVID-19 has rapidly spread throughout Ethiopia. New data are being collected every day. It is important to provide healthcare workers with the most updated information about COVID-19 in pregnant women. This information will help to answer the numerous questions that future mothers may have in the current situation and to prevent obstetrical complications. Since pregnant women, especially in rural areas, have a limited information route, and scarcity of resources, this virus will have a severe impact. Therefore, this study is aimed to assess CoVID-19 preventive measure practices and knowledge of pregnant women in Guraghe zone hospitals.
Methods and Materials
Study Area, Design, and Period
Guraghe zone is one of the administrative zones in Southern nation nationalities and peoples region (SNNPR) of Ethiopia. It has 13 districts and two town administrations. Wolkite town is the capital of Guraghe zone, found 153 km southwest to Addis Ababa, the capital of Ethiopia. According to Wikipedia, Guraghe zone has a total population of 1,279,646, of which 657,568 are women.31
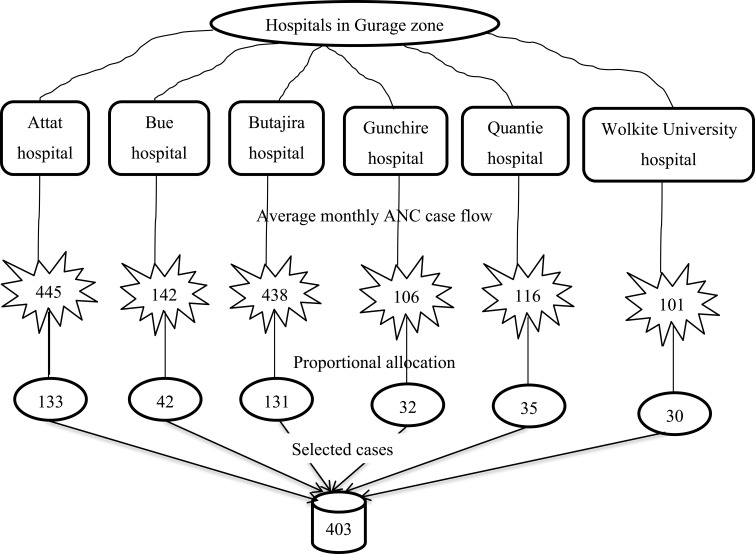
There are six hospitals in Guraghe zone: Attat primary hospital with an annual Antenatal Care (ANC) case flow of 5,342, Bue primary hospital with an annual ANC case flow of 1,700, Butajira general hospital with an annual ANC case flow of 5,254, Gunchire primary hospital with annual ANC case flow of 1,275, Quantie primary hospital with an annual ANC case flow of 1,396, and Wolkite university specialized referral hospital with an annual ANC case flow of 1,216 serving the total population in the zone. All hospitals provide comprehensive emergency obstetric care services. Moreover, there are 72 health centers which provide basic emergency obstetric care services in Guraghe zone. All the six hospitals in Guraghe zone were involved in this study and an institution-based crossectional study was conducted from July 27–August 27, 2020.
Study Subjects
All pregnant women visiting those six hospitals in Guraghe zone were the source population of this study. Women who had come to the hospital for ANC follow-up in the study period were included. However, pregnant women who were either admitted to the inpatient department for gynecologic, medical, or surgical cases or treated in the out-patient department were excluded.
Sample Size Determination, Sampling Technique, and Procedure
The required sample size was calculated using OpenEpi statistics software version 3.03. An assumption of 95% confidence level, 5% margin of error, and a proportion of 60.9%32 from a study done in Nigeria on knowledge and practice of preventive measures against COVID-19 infection among pregnant women in a low-resource African setting is considered. This makes a sample size of 366, adding a 10% contingency to account for non-response rate, which yielded a final sample size of 403.
The total sample size was deployed proportionally to each hospital according to their case flow. A systematic random sampling technique was employed in this study. The intervals for subjects to be selected were calculated for each hospital in accordance with their case flow (Figure 1).
Figure 1.
Sampling procedures of COVID-19 preventive measure practices and knowledge of pregnant women in Guraghe zone hospitals, Wolkite, September 2020 (N=403).
Professionals who were on routine service were data collectors on their respective hospitals. Two data collectors who were working in ANC and have a Bachelor of Science (BSc) degree in midwifery were selected. Two supervisors who have a degree in midwifery and instructors of Wolkite University were recruited. One day training for supervisors and data collectors in each hospital was given on how to conduct data collection. The training discloses the possible benefit and purpose of the study to the study participants before the start of data collection.
Orders of interview and intervals of selection were according to their ANC clinic entry. The objective of the study, how they are selected, and voluntary participation was clarified. The interview was conducted after routine services were given in ANC.
Data Collection Tools and Technique
An interviewer-administered based questionnaire on the practice and knowledge of coronavirus infection preventive measures were used for data collection. The questionnaires were developed following a review of the literature and WHO recommendations on the measures to prevent human-to-human transmission of COVID-19 infection.
The questionnaires have an 8-item scale for knowledge assessment questions and an 8-item scale for practice questions. The scoring system of women’s knowledge and practice of preventive measures were either 1 (for correct answer) or 0 (for incorrect answer). The minimum score was 0, whereas the maximum score was 8 for each of knowledge and practice component of the questionnaire. The reliability of the questionnaire was checked by conducting a pretest among pregnant women in Saint Lukas hospital antenatal clinic, by taking 20 clients, which was 5% of the total sample size.
Variables
COVID-19 preventive measure practice and knowledge were the dependent variables, and socio-demographic characteristics (age, parity, marital status, permanent residence, occupation, participant’s level of education, and husband’s level of education) and media exposure to access information about the coronavirus infection pandemic (Radio, Television, Smart phone for social media, route for broacher and tracts) were the independent variables.
Operational Definitions
Good practice: Women who scored 100% on the practice of COVID-19 preventive measures questionnaire, and poor practice: Women who scored <100% on the practice of COVID-19 preventive measures questionnaire.32 Adequate knowledge: Participants who scored ≥65% on knowledge of COVID-19 preventive measures questionnaire, and inadequate knowledge: Women who scored <65% on knowledge of COVID-19 preventive measures questionnaire.32
Data Quality Control
The principal investigators checked the completeness and consistency of questionnaires filled by the data collectors to ensure the quality of data. To check the clarity, skipping pattern and order of questions, the questionnaire will be pre-tested before the start of the actual data collection.
After pre-test, questions have revised, edited, and those found to be unclear have been modified. The questionnaire was prepared in English language and then translated to Amharic and Guragigna (local) languages by native speakers of the languages. Two trained midwives who can speak both Amharic and Guragigna language have been participated in the data collection in each hospital. Guragigna and Amharic questionnaires were used for data collection and have been used according to the skills of the clients. The questionnaire will then be refined accordingly for final use.
Data Entry and Analysis
Data were checked manually for completeness. Data marked as complete were entered in to Epi Data version 3.1 software. For further analysis the data were exported to the statistical package for social sciences version 24.0 software. Descriptive statistics were carried out as a frequency and percentage. Bivariate and multivariate analysis were used to see the effect of independent variable over COVID-19 preventive measure practice and knowledge. Variables which will be significant on bivariate analysis at a P-value less than 0.25 were taken to multivariate analysis. The fitness of model have been checked by Hosmer and Lemeshow test with the value 0.11. In multivariate analysis P-value of less than 0.05 and 95% confidence level was used as a cut-off point for the presence of association. Finally, results were compiled and presented using tables, graphs, charts, and texts.
Results
A total of 403 study subjects participated in this study making the response rate of 100%. In this study the maximum age of the participant was 41 and the minimum age was 18 with the mean and standard deviation of 27.11±5.24. From the participants more than two thirds of the participants were multipara and most of them have married status (Table 1).
Table 1.
Socio-Demographic Characteristics of COVID-19 Preventive Measure Practices and Knowledge of Pregnant Women in Guraghe Zone Hospitals, Wolkite, September 2020 (N=403)
| Socio-Demographic Characteristics | |||
|---|---|---|---|
| Variables | Category | Frequency | Percent |
| Age | ≤19 | 48 | 11.9 |
| 20–24 | 140 | 34.7 | |
| 25–29 | 127 | 31.5 | |
| 30–34 | 64 | 15.9 | |
| ≥35 | 24 | 6 | |
| Religion | Orthodox | 156 | 38.7 |
| Muslim | 205 | 50.9 | |
| Protestant | 33 | 8.2 | |
| Catholic | 9 | 2.2 | |
| Parity | Primipara | 115 | 28.5 |
| Multipara | 249 | 61.8 | |
| Grand-multipara | 39 | 9.7 | |
| Marital status | Married | 380 | 94.3 |
| Single | 10 | 2.5 | |
| Divorced | 9 | 2.2 | |
| Widowed | 4 | 1 | |
| Place of residence | Urban | 252 | 62.5 |
| Rural | 151 | 37.5 | |
| Occupation | House wife | 208 | 51.6 |
| Civil servant | 86 | 21.3 | |
| Personal business | 81 | 20.1 | |
| Unemployed | 28 | 6.9 | |
| Educational status | No formal education | 99 | 24.6 |
| Primary | 156 | 38.7 | |
| Secondary | 91 | 22.6 | |
| College and above | 57 | 14.1 | |
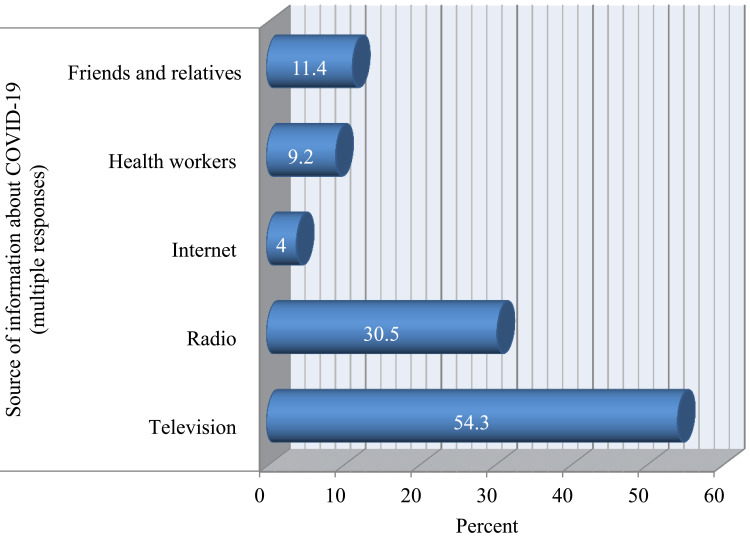
COVID-19 Preventive Measure Information Source of the Participants
From the total participants 312 (77.4%) have television or radio in their home, whereas 91 (22.6) of them have no television or radio. On the other hand, about 109 (27%) of the participants have access to print media and 294 (73%) of them have not. Similarly 102 (25.3%) have access to the internet and 301 (74.7%) have not. More than half of the participants have heard about COVID-19 on television (Figure 2).
Figure 2.
Source of information about COVID-19 preventive measure practices and knowledge of pregnant women in Guraghe zone hospitals, Wolkite, September 2020 (N=403).
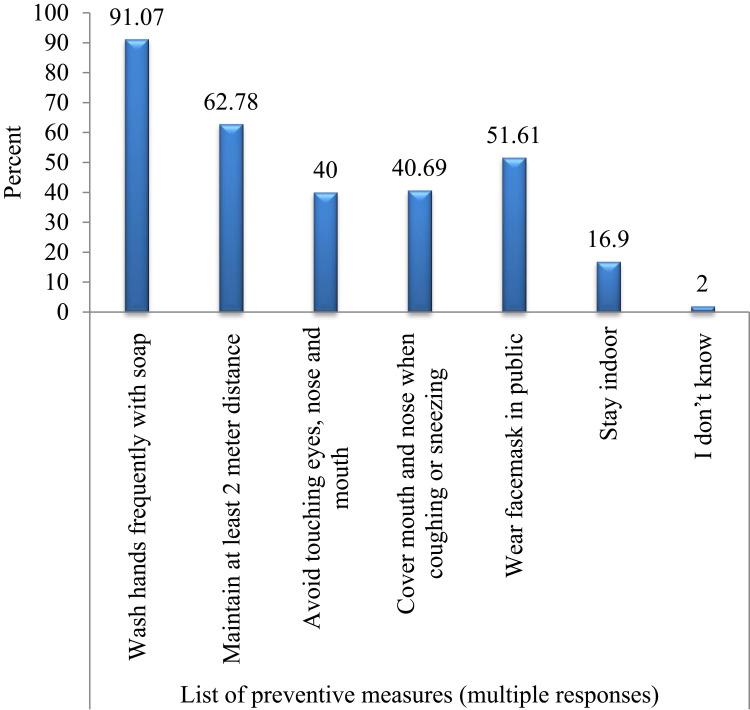
COVID-19 Preventive Measure Knowledge of the Participants
From the total participant almost all of the participants were aware of COVID-19 except 18 (4.5%) of them. In the same manner, 28 (6.9%) participants were responding that this virus have vaccine (Table 2). Most of the participants listed washing hands with soap and water as a preventive measure (Figure 3).
Table 2.
Knowledge Assessment on COVID-19 Preventive Measure Practices and Knowledge of Pregnant Women in Guraghe Zone Hospitals, Wolkite, September 2020 (N=403)
| Variables | Category | Frequency | Percent |
|---|---|---|---|
| Aware of ongoing COVID-19 | Yes | 396 | 98.3 |
| No | 7 | 1.7 | |
| COVID-19 is contagious | Yes | 385 | 95.5 |
| No | 18 | 4.5 | |
| Symptoms of COVID-19 (multiple responses) | Fever | 357 | 88.58 |
| Cough | 340 | 84.37 | |
| Difficulty of breathing | 132 | 32.84 | |
| Headache | 224 | 55.58 | |
| I do not know | 2 | 0.5 | |
| Measures, if there are symptoms (multiple responses) | Stay at home | 133 | 33 |
| Wear face mask | 97 | 24.07 | |
| Visit health facility | 327 | 81.1 | |
| I do not know | 14 | 3.5 | |
| Worst on older people | Yes | 365 | 90.6 |
| No | 38 | 9.4 | |
| Worst on people with chronic disease | Yes | 356 | 88.3 |
| No | 47 | 11.7 | |
| Vaccine available | Yes | 28 | 6.9 |
| No | 375 | 93.1 |
Figure 3.
Participants knowledge on list of COVID-19 preventive measure practices and knowledge of pregnant women in Guraghe zone hospitals, Wolkite, September 2020 (N=403).
From the total participants, 221 (54.84%) of them have adequate knowledge (Figure 3). Almost all of the participants have awareness of the ongoing pandemic (Table 3). Knowledge assessment questions with multiple responses were categorized as correct response if they respond above or equal to the mean of listed answers (Table 3).
Table 3.
Categorized Knowledge Assessment on COVID-19 Preventive Measure Practices and Knowledge of Pregnant Women in Guraghe Zone Hospitals, Wolkite, September 2020 (N=403)
| Variables | Category | Frequency | Percent | Correct Response | Correct Percent |
|---|---|---|---|---|---|
| Aware of ongoing COVID-19 | No | 7 | 1.7 | Yes | 98.3 |
| Yes | 396 | 98.3 | |||
| COVID-19 is contagious | No | 18 | 4.5 | Yes | 95.5 |
| Yes | 385 | 95.5 | |||
| List symptoms answered more than mean | No | 205 | 50.9 | Yes | 49.1 |
| Yes | 198 | 49.1 | |||
| List actions answered more than mean | No | 256 | 63.5 | Yes | 36.5 |
| Yes | 147 | 36.5 | |||
| List preventive measure answered more than mean | No | 150 | 37.2 | Yes | 62.8 |
| Yes | 253 | 62.8 | |||
| Worst on older people | No | 38 | 9.4 | Yes | 90.6 |
| Yes | 365 | 90.6 | |||
| Worst on people with chronic disease | No | 47 | 11.7 | Yes | 88.3 |
| Yes | 356 | 88.3 | |||
| Vaccine available | No | 28 | 6.9 | No | 6.9 |
| Yes | 375 | 93.1 |
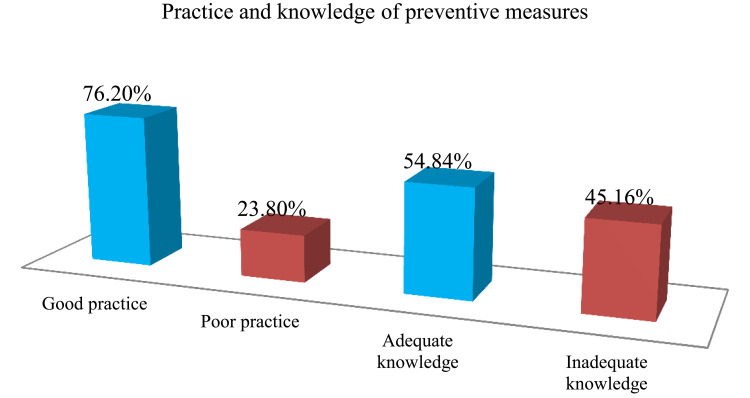
COVID-19 Preventive Measure Practices of the Participants
From the total participants, 307 (76.2%) of them have good practice on prevention of COVID-19 (Figure 4). Most of the participants (365, 90.6%) are obeying government restrictions due to the pandemic (Table 4).
Figure 4.
COVID-19 preventive measure practices and knowledge of pregnant women in Guraghe zone hospitals, Wolkite, September 2020 (N=403).
Table 4.
COVID-19 Preventive Measure Practices of Pregnant Women in Guraghe Zone Hospitals, Wolkite, September 2020 (N=403)
| Questions | Responses | Correct Responses | Percent Correct | |||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| N | % | N | % | |||
| Are you obeying government restriction on COVID-19 prevention strategies? | 365 | 90.6 | 38 | 9.4 | Yes | 90.6 |
| Have you stop going to public or crowded place after the COVID-19 pandemic confirmed in Ethiopia? | 346 | 85.9 | 57 | 14.1 | Yes | 85.9 |
| Did you wash your hands frequently with soap and water or alcohol-based sanitizers? | 373 | 92.6 | 30 | 7.4 | Yes | 92.6 |
| Did you maintaining at least 2 meter distance between yourself and others? | 369 | 91.6 | 34 | 8.4 | Yes | 91.6 |
| Did you avoid touching eyes, nose, and mouth with hands? | 351 | 87.1 | 52 | 12.9 | Yes | 87.1 |
| Did you wear face mask in public? | 355 | 88.1 | 48 | 11.9 | Yes | 88.1 |
| Did you stay in-door if it is not must to get out? | 354 | 87.8 | 49 | 12.2 | Yes | 87.8 |
| In order to prevent contracting and spreading COVID-19 do you avoid handshaking, hugging and kissing? | 344 | 85.4 | 59 | 14.6 | Yes | 85.4 |
Factors Associated with COVID-19 Preventive Measure Practices
On bivariate analysis age, place of residence, educational status, presence of television/radio at home, access to internet, worst on older people, worst on people with chronic disease, and vaccine available were candidates for multivariate analysis. On multivariate analysis, age, place of residence, and worst on people with chronic disease were statistically significant (Table 5).
Table 5.
Factors Associated with COVID-19 Preventive Measure Practices of Pregnant Women in Guraghe Zone Hospitals, Wolkite, September 2020 (N=403)
| Variables | Category | Prevention Practice | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Good N (%) | Poor N (%) | ||||
| Age category | ≤19 | 40 (13) | 8 (8.3) | 1.00 (0.27–3.72) | 1.02 (0.75–16.06) |
| 20–24 | 110 (35.8) | 30 (31.2) | 1.36 (0.43–4.29) | 1.22 (1.15–22.24)* | |
| 25–29 | 99 (32.2) | 28 (29.2) | 1.41 (0.45–4.45) | 1.32 (1.20–20.25)* | |
| 30–34 | 38 (12.4) | 26 (27.1) | 3.42 (1.05–11.18) | 2.57 (2.32–43.38)** | |
| ≥35 | 20 (6.5) | 4 (4.2) | 1 | 1 | |
| Place of residence | Urban | 209 (68.1) | 43 (44.8) | 2.63 (1.65–4.19) | 2.16 (1.24–3.77)** |
| Rural | 98 (31.9) | 53 (55.2) | 1 | 1 | |
| Educational status | No formal education | 69 (22.5) | 30 (31.2) | 2.32 (1.01–5.32) | 0.74 (0.25–2.19) |
| Primary | 121 (39.4) | 35 (36.5) | 1.54 (0.69–3.45) | 0.52 (0.18–1.46) | |
| Secondary | 69 (22.5) | 22 (22.9) | 1.70 (0.72–4.01) | 1.12 (0.42–2.99) | |
| College and above | 48 (15.6) | 9 (9.4) | 1 | 1 | |
| Have television/radio | Yes | 244 (79.5) | 68 (70.8) | 1.59 (0.95–2.68) | 0.73 (0.37–1.45) |
| No | 63 (20.5) | 28 (29.2) | 1 | 1 | |
| Have access to internet | Yes | 89 (29) | 13 (13.5) | 2.61 (1.38–4.92) | 2.24 (0.99–5.13) |
| No | 218 (71) | 83 (86.5) | 1 | 1 | |
| Worst on older | Yes | 293 (95.4) | 72 (75) | 6.97 (3.44–14.16) | 2.27 (0.71–7.23) |
| No | 14 (4.6) | 24 (25) | 1 | 1 | |
| Worst on people with chronic disease | Yes | 290 (94.5) | 66 (68.8) | 7.75 (4.04–14.89) | 5.12 (1.73–15.17)** |
| No | 17 (5.5) | 30 (31.2) | 1 | 1 | |
| Vaccine available | Yes | 18 (5.9) | 10 (10.4) | 0.54 (0.24–1.20) | 0.72 (0.26–1.99) |
| No | 289 (94.1) | 86 (89.6) | 1 | 1 | |
Notes: *P≤0.05, **P≤0.05, bold = statistically significant.
Being aged 20–24 (AOR=1.22, 95% CI=1.15–22.24), 25–29 (AOR=1.32, 95% CI=1.20–20.25), and aged 30–34 (AOR=2.57, 95% CI=2.32–43.38) were more likely to practice COVID-19 preventive measures practices compared to participants age greater or equal to 35. Residing in an urban area (AOR=2.16, 95% CI=1.24–3.77) were more likely to practice COVID-19 preventive measures compared rural residence. Perceiving COVID-19 have a poor prognosis on people with chronic disease (AOR=5.12, 95% CI=1.73–15.17) were more likely to practice COVID-19 preventive measures compared to those who perceive chronic disease as having no difference on the prognosis (Table 5).
Discussion
This study presents COVID-19 preventive measure practices and knowledge of pregnant women, visiting hospitals in Guraghe Zone, Southern Ethiopia. Factors which have a significant effect on COVID-19 preventive measure were identified using multivariate logistic regression analysis. On the multivariate analysis only three variables were found to be statistically significant from the eight variables that were significant in bivariate analysis. Those factors statistically significant in the final model were discussed accordingly in comparison with other studies and possible authors’ justification on the nature of this specific study.
This study shows that 54.84% (95% CI=50.1–59.6) of the participants have adequate knowledge. Result of this study on knowledge of COVID-19 preventive measure were lower than studies conducted in Ghana which state that knowledge of women following antenatal care were 62.7%,33 in Uganda knowledge of COVID-19 among mothers following antenatal care were 69%,34 and in Nigeria knowledge of pregnant women visiting medical centers were 60.9%.35
Contrarily, this result was higher than a study done in Debre Tabor town (46.8%).36 Moreover, knowledge of preventive measure among Jimma university medical center visitors was 41.3%.37
This difference might be due to the time of the studies conducted in which information delivery and awareness creation programs about the pandemic are ongoing and improving from time to time. For this reason practices were expected to be low in the beginning of the pandemic. The other reason might be those who have better information source and urban residencies were intended to practice prevention methods than their counterparts.
In the other hand this study shows that COVID-19 preventive measure practices were 76.2% (95% CI=72.0–80.4). A study in southern Ethiopia reports that 47.6% of the participants have good practice.36
This difference might be due to effective interventions measures taken by the government and health institution; which was accepted by the healthcare provider to carry out the rules and regulations. Because of this, practices of the community on the preventive measure were increasing. Since this disease could not be defeated without efficiently sticking with preventive measure practices, the results of this study are not good enough. Pregnant women visiting hospitals in Guraghe Zone are expected to practice more than the stated value. Therefore it’s not conclusive to state practices of COVID-19 preventive measures among those women were higher.
Participants aged 20–24, 25–29, and 30–34 were more likely to practice COVID-19 preventive measures practice compared to participants whose age was greater or equal to 35. Consistently, a study conducted in Debre Tabor town shows that participants aged 15–24 were more likely to practice COVID-19 preventive measures.38
This might be due to information access to younger participants being better. This study also shows most younger participants have access to print media, internet, television, and radio. In another way younger participants have a better educational level, and another study has shown participants with a higher level of education have better preventive practices.38 Results of this study also showthat younger participants have a better educational status when compared to older participants.
Urban residents were more likely to practice COVID-19 preventive measures compared to rural residents. Consistently a study conducted in India shows urban residents was more likely to practice COVID-19 preventive measures.39
This might be due to urban residents in Ethiopia having better access to different types of communication media carrying messages about the pandemic. Additionally peoples living in an urban area of Ethiopia were relatively surrounded by educated people who would have the chance to obtain information informally like in transport, in neighborhood, and informal social meetings.
Participants who perceive that COVID-19 has a poor prognosis on people with chronic disease were more likely to practice COVID-19 preventive measures compared to those who perceive that COVID-19 has no difference on people with chronic diseases. Consistently, a study conducted in Addis Zemen Hospital, Northwest Ethiopia reports that participants practicing better on preventive measures responded that the pandemic was worst among people with chronic diseases.40
This might be due to those peoples having better knowledge on the characteristics of COVID-19 because they were responding to the right answer, unlike their counterparts. Similarly clients with chronic disease have the chance to visit health service facilities during their follow-up appointment, and could get information from their health provider to develop their knowledge about the pandemic in relation with their disease.
Conclusion
COVID-19 preventive measure practice and knowledge among mothers in Guraghe zone hospitals were low compared to other studies.
Participants aged 20–24, 25–29, and 30–34 were more likely to practice COVID-19 preventive measures practices compared to participants age greater or equal to 35. Residence of urban area was more likely to practice COVID-19 preventive measures compared rural residence. Those perceiving COVID-19 has a poor prognosis on people with chronic disease were more likely to practice COVID-19 preventive measures compared to those who perceive chronic disease to have no difference on the prognosis.
Therefore:
COVID-19 preventive measure practices and knowledge among pregnant women in the rural part of Guraghe zone needs to be supported by Guraghe zone health office.
Pregnant women aged ≥35 in Guraghe zone hospitals need to be counseled by the healthcare providers about the preventive measures practices.
Acknowledgment
When the world is in terrible planning to be a part of solution is remarkable decision. Wolkite University was in charge of this decision, and those who facilitate conditions accordingly in hierarchy of their position to conduct research need to be acknowledged. This work would not beas good as it is now without friends, whose support and advice made this article viable, thank you for your time. My wife, you are kind, patient, and closest friend ever, I see you can hear me even when I am silent; thank you my sweet and I love you. My subjects, pregnant womenvisiting hospitals in Guraghe zone who were included in this study; this research couldn't have happened without you, many thanks dear clients.
Funding Statement
This research was supported by Wolkite University, but the University has no role on this manuscript.
Ethical Considerations
Ethical clearance was obtained from Wolkite University College of medicine and health science institutional review board (IRB) with a reference number RCSUILC043/2013. Permission was obtained from Guraghe zone health office and each hospital medical directors office; oral informed consent, which was approved by IRB of Wolkite University, was obtained from participants, and this study was conducted in accordance with the Declaration of Helsinki. Confidentiality and anonymity were ensured, and participants were informed that their participation was voluntary.
Author Contributions
All authors have substantial contributions to conception, study design, acquisition of data, analysis, and interpretation of data. YF have drafted and YF, AY, TM, MM, WA, MA critically reviewed the article. All authors have agreed on the journal to which the article will be submitted. We have reviewed and agreed on all versions of the article before submission, during revision, the final version accepted for publication, and any significant changes introduced at the proofing stage. YF agree to take responsibility and be accountable for the contents of the article.
Disclosure
The authors declare that there is no conflict of interest.
References
- 1.Sutton D, Fuchs K, D’Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. 2020;382(22):2163–2164. doi: 10.1056/nejmc2009316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goyal P. Correspondence clinical characteristics of Covid-19 in China. NEJM. 2020;1–3. doi: 10.1056/NEJMc2005203 [DOI] [Google Scholar]
- 3.Muchinsky PM. Maternal psychological distress during Covid-19. Psychol Appl to Work an Introd to Ind Organ Psychol Tenth Ed Paul. 2020;53:1689–1699. [Google Scholar]
- 4.Muldoon KM, Fowler KB, Pesch MH, et al. 2020 Elsevier has created a COVID-19 resource centre with free information in english and mandarin on the novel coronavirus COVID- 19. The COVID-19 resource centre is hosted on Elsevier Connect, the company ’ s public news and information. J Obstet Gynaecol Canada. 2020. [Google Scholar]
- 5.Denis M, Vandeweerd V, Verbeke R, Version DV. COVID-19 overview of information available to support the development of medical countermeasures and interventions against COVID-19. Transdiscipl Insights. 2020;1–157. [Google Scholar]
- 6.WHO. Home Care for Patients with Suspected Novel Coronavirus (Ncov) Infection Presenting with Mild Symptoms and Management of Contacts. 2020. [Google Scholar]
- 7.WHO. Clinical Management of COVID-19. 2020. [Google Scholar]
- 8.WHO. DRAFT Landscape of COVID-19 Candidate Vaccines. 2020. [Google Scholar]
- 9.WHO. Maintaining a Safe and Adequate Blood Supply During the Pandemic Outbreak of Coronavirus Disease (COVID-19). 2020. [Google Scholar]
- 10.WHO. Strategic Preparedness. 2020. [Google Scholar]
- 11.Worldo meter. Corona virus daily report. 2020. Available from: https://www.worldometers.info/coronavirus/. Accessed December15, 2020.
- 12.Poon LC, Yang H, Kapur A, et al. Global interim guidance on coronavirus disease 2019 (COVID-19) during pregnancy and puerperium from FIGO and allied partners: information for healthcare professionals. Int J Gynecol Obstet. 2020;149(3):273–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beheshtkhoo N, Alipour MH, Nemati R, et al. A review of COVID-19: the main ways of transmission and some prevention solutions, clinical symptoms, more vulnerable human groups, risk factors, diagnosis, and treatment. J Environmental Treat Tech. 2020;8:884–893. [Google Scholar]
- 14.Ashokka B, Loh M-H, Tan CH, et al. Care of the pregnant woman with coronavirus disease 2019 in labor and delivery: anesthesia, emergency cesarean delivery, differential diagnosis in the acutely ill parturient, care of the newborn, and protection of the healthcare personnel. Am J Obstet Gynecol. 2020;223(1):66–74.e3. doi: 10.1016/j.ajog.2020.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.FMOH, E. Covid19 Management Handbook. 2020. [Google Scholar]
- 16.Watch G. Covid-19 and pregnancy. BMJ. 2020;369:1–2. [DOI] [PubMed] [Google Scholar]
- 17.Vivanti AJ, Deruelle P, Picone O, et al. Follow-up for pregnant women during the COVID-19 pandemic: french national authority for health recommendations. J Gynecol Obstet Hum Reprod. 2020;101804. doi: 10.1016/j.jogoh.2020.101804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jiang H, Jin L, Qian X, et al. Evidence of accessing antenatal care information via social media platforms supports mental wellbeing in COVID-19 epidemic. Bull World Health Organ. 2020. doi: 10.2471/BLT.20.255489 [DOI] [Google Scholar]
- 19.Liang H, Acharya G. Novel corona virus disease (COVID-19) in pregnancy: what clinical recommendations to follow? Acta Obstet Gynecol Scand. 2020;99(4):439–442. doi: 10.1111/aogs.13836 [DOI] [PubMed] [Google Scholar]
- 20.Lopez M, Meler Bcnatal E, Jafet R, Portilla M, Palacio L. COVID-19 in pregnancy: a clinical management protocol and considerations for practice short title: COVID-19 in pregnancy: a clinical management protocol fetal cardiology view project development of a LLDP porometer able to characterize NF membranes view. 2020. doi: 10.13140/RG.2.2.29732.83840. [DOI]
- 21.Marinelli KA. International perspectives concerning donor milk banking during the SARS-CoV-2 (COVID-19) pandemic. J Hum Lact. 2020;00:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Type I, Library NH, Evidence KS, Executive HS. Evidence summary: in pregnant women who have tested positive for COVID-19 is there any evidence in relation to the safest mode of delivery — caesarean or vaginal — for the woman, her baby and those caring for her? Irish Health Repos. 2020. [Google Scholar]
- 23.Thomas B. Maternal and perinatal outcomes and pharmacological management of Covid-19 infection in pregnancy: a systematic review protocol. BMC. 2020;1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mehta H, Ivanovic S, Cronin A, et al. Novel coronavirus-related acute respiratory distress syndrome in a patient with twin pregnancy: a case report. Case Rep Womens Health. 2020;27:e00220. doi: 10.1016/j.crwh.2020.e00220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yassa M, Birol P, Yirmibes C, Usta C, Haydar A. Near-term pregnant women’s attitude toward, concern about and knowledge of the COVID-19 pandemic. J Matern Fetal Neonatal Med. 2020;33(22):3827–3834. doi: 10.1080/14767058.2020.1763947 [DOI] [PubMed] [Google Scholar]
- 26.Kurdoğlu M, Khaki A. What is the current state of knowledge about the novel coronavirus infection during pregnancy? Int J Womens Health Reprod Sci 2020;8:110–111. [Google Scholar]
- 27.Rochelson B, Nimaroff M, Combs A, et al. The care of pregnant women during the COVID-19 pandemic – response of a large health system in metropolitan New York. J Perinat Med. 2020;48(5):453–461. doi: 10.1515/jpm-2020-0175 [DOI] [PubMed] [Google Scholar]
- 28.Poon LC, Yang H, Lee JC, et al. ISUOG Interim Guidance on 2019 novel coronavirus infection during pregnancy and puerperium: information for healthcare professionals. Ultrasound Obstet Gynecol. 2020. doi: 10.1002/uog.22013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mullins E, Evans D, Viner R, O’Brien P, Morris E. Coronavirus in pregnancy and delivery: rapid review and expert consensus. medRxiv. 2020;4–13. [DOI] [PubMed] [Google Scholar]
- 30.Abdollahpour S, Khadivzadeh T. Improving the quality of care in pregnancy and childbirth with coronavirus (COVID-19): a systematic review. J Matern Neonatal Med. 2020;1–9. [DOI] [PubMed] [Google Scholar]
- 31.Wikipedia, the free encyclopedia. Gurage zone. 2020. Available from: https://en.wikipedia.org/wiki/Gurage_people. Accessed December15, 2020.
- 32.Nwafor JI, Aniukwu JK, Anozie BO, Ikeotuonye AC. Knowledge and practice of preventive measures against COVID-19 infection among pregnant women in a low-resource African setting. medRxiv. 2020;2020:04.15.20066894. doi: 10.1101/2020.04.15.20066894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Serwaa D, Lamptey E, Appiah AB, Senkyire EK, Ameyaw JK. Knowledge, risk perception and preparedness towards coronavirus disease-2019 (COVID-19) outbreak among Ghanaians: a quick online cross-sectional survey. Pan Afr Med J. 2020;35:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olum R, Bongomin F. Coronavirus disease-2019: knowledge, attitude, and practices of health care workers at Makerere University Teaching Hospitals. Front Public Health. 2020;8:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nwafor JI 1, Aniukwu JK 2, Anozie BO 1, Ikeotuonye AC. Knowledge and practice of preventive measures against COVID-19 infection among pregnant women in a low-resource African setting. medRxiv Prepr. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Policy H. Knowledge and precautionary behavioral practice toward COVID-19 among health professionals working in public University Hospitals in Ethiopia: a web-based survey. Risk Manag Healthc Policy. 2020;13:1327–1334. doi: 10.2147/RMHP.S267261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Id YK, Yitayih Y, Birhanu Z, Mekonen S. Knowledge, perceptions and preventive practices towards COVID-19 early in the outbreak among Jimma university medical center visitors, Southwest Ethiopia. PLoS One. 2020;77:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ayele AD, Mihretie GN, Belay HG, Teffera AG, Kassa BG, Amsalu BT. Knowledge and practice to prevent against corona virus disease (COVID-19) and its associated factors among pregnant women in Debre Tabor Town Northwest Ethiopia: a community based Cross-Sectional Study. Res Sq. 2020;1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pal R, Yadav U, Grover S, et al. Knowledge, attitudes and practices towards COVID-19 among young adults with type 1 diabetes mellitus amid the nationwide lockdown in India: a cross-sectional survey. Diabetes Res Clin Pract. 2020;166:108344. doi: 10.1016/j.diabres.2020.108344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hospital AZ. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at. Infect Drug Resist. 2020;1949–1960. doi: 10.2147/IDR.S258736 [DOI] [PMC free article] [PubMed] [Google Scholar]