Abstract
Context: Trunk impairment among non-ambulatory individuals with spinal cord injury (SCI) reduces the ability to maintain a functional sitting position and perform activities of daily living. Measuring functional sitting balance is complex and difficult in a clinical setting. The function in sitting test (FIST) is a clinical measure that includes the assessment of all the components of sitting balance. The purpose of this study is to assess the reliability and validity of the 14-item FIST among non-ambulatory individuals with SCI.
Participants: Twenty-six individuals with chronic SCI.
Outcome measures: Participants were evaluated with the FIST, the modified Functional Reach Test (lateral and forward mFRT) and a posturography assessment (virtual time to contact – VTC). The FIST was re-assessed during a second study visit 12 weeks later. Test-retest reliability was evaluated using intraclass coefficient correlation (ICC), the minimal detectable change (MDC) was calculated and the internal consistency reliability was assessed using Cronbach's coefficient-α. Concurrent validity of the FIST was also tested with the mFRT and the VTC.
Results: Test-retest reliability was found to be excellent (ICC = 0.95) with a MDC of 4. The internal consistency was satisfactory (0.81). Moreover, the FIST correlates with the lateral mFRT (r = 0.64, P = 0.001) but not with the forward mFRT and the VTC.
Conclusion: These observations provide evidence that the FIST is a reliable clinical measure with partially established validity for non-ambulatory individuals with SCI. Further studies are needed to strengthen the validity of the FIST and explore this measure in a larger sample.
Keywords: Spinal cord injury, Reliability, Sitting balance, Validity
Introduction
It is estimated that more than 282,000 individuals with spinal cord injury (SCI) are living in the United States and about 60–80% of them use a wheelchair to complete daily mobility activities.1 Individuals with SCI often present with poor sitting balance due to trunk motor and sensory impairments. Depending on the level of injury, the ability to sit unsupported varies greatly among this population.2
The ability to sit unsupported to perform daily activities is an important skill for wheelchair users with SCI to increase independence. More than 60% of individuals with tetraplegia rated trunk and arm/hand function as priorities to improve functional independence and quality of life.3 The importance of trunk stability and dynamism to facilitate performance of functional activities is also well documented among able-body individuals4,5 as well as for individuals with neurological diseases such as brain injury,6 stroke,7,8 and SCI.9 Among individuals with SCI, trunk control has been shown to be an important determinant contributing to reduced sitting stability when compared to able-bodied individuals.10 Impairment of trunk muscles due to paralysis after SCI reduces the performance of reaching and transfer activities.11–13 As part of a kinematic chain, there is an important interaction between the trunk with the upper extremities (UE) and the head.14 This interaction is essential in and out of the wheelchair to perform functional sitting activities among non-ambulatory individuals. For example, transfers to/from a bed, car, toilet, tub as well as daily living activities that commonly involve transfers, such as dressing, bathing often done out the wheelchair require a certain amount of trunk stability. Therefore, trunk impairment may have consequences on activity execution and performance in a sitting position.14 Gagnon et al. demonstrated that trunk and UE strength are key determinants of wheelchair mobility which is also essential for functional independence among non-ambulatory individuals with SCI.15 Hence, to improve the performance of functional activities, it is essential to consider the key role of the trunk in sitting balance.10,14
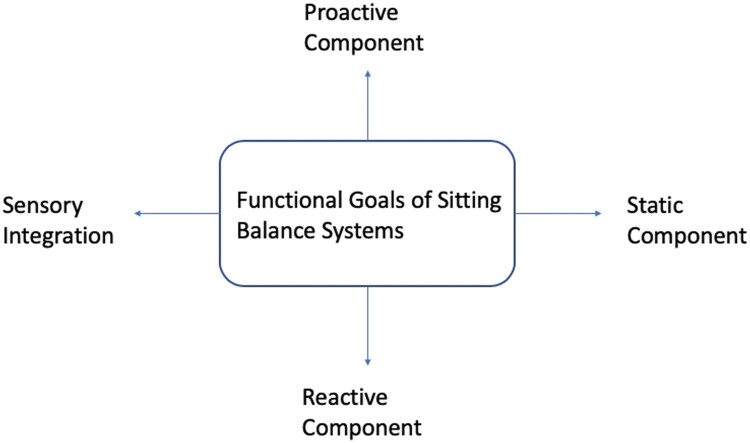
The assessment of sitting balance to plan and monitor treatment strategies and for discharge planning is of high importance in clinical settings. In a research laboratory, several complex systems are used to assess sitting balance among individuals with SCI including force platforms16,17 and movement analysis systems18,19 which are considered the “gold standard.” Among these laboratory tools, the measures of the center of pressure (COP) has been commonly used to quantify sitting balance as well as the effect of UE support.10,20,21 These systems allow for accurate and objective quantification of movement underlying sitting balance. However, the equipment used in a laboratory setting is relatively costly and requires expertise to analyze and interpret the data which is not suitable for clinical settings. A sitting balance assessment is complex and requires an evaluation of the functional goals of sitting balance components. The functional goals imply the maintenance of a specific postural alignment (static), the facilitation of voluntary movement or movement transitions between postures (proactive) and the reactions that recover equilibrium to external disturbances (reactive).22 In addition to these systems, sensory integration also plays a key role during sitting balance assessment (see Fig. 1).23 A recent systematic review by Abou et al investigated clinical measures to assess sitting balance among individuals with SCI and concluded that there is a need for clinical measures with the ability to assess all the underlying sitting balance systems.24 The lack of appropriate clinical measures reduces the ability to design, test and implement rehabilitation interventions to improve seated posture among non-ambulatory individuals with SCI.
Figure 1.
Model summarizing systems underlying sitting balance assessment (Adapted from the BESTest model by Horak et al.23).
Therefore, a clinical instrument appropriate for non-ambulatory individuals with SCI that is easy to apply, quick and simple to analyze and included all the sitting balance systems is necessary. One potential measurement is the function in sitting test (FIST).25 The FIST was originally developed to assess functional sitting balance among adults with stroke25 and has been validated for non-ambulatory individuals with Multiple Sclerosis.26 The FIST quantifies static, proactive, reactive and sensory integration of sitting balance systems during 14 everyday functional activities and describes sitting balance at the activity level of the International Classification of Functioning, Disability and Health (ICF).25,27 Activities included in the FIST comprise, but are not limited to, quiet sitting with eyes open and closed for 30 s, self-initiated activities, and reactive nudges.25 The FIST administration is quick, taking less than 10 min, simple, low cost and requires minimal training.26
Therefore, the aim of this study is to evaluate the reliability and validity of the FIST among non-ambulatory individuals with SCI. The following hypotheses were set:
The FIST will present with good to excellent test-retest reliability and internal consistency for non-ambulatory individuals with SCI.
Given that the FIST assesses various aspects of sitting balance control, we do not expect a strong correction between the FIST and unidimensional sitting balance measures.
Methods
Participants
This study is a secondary analysis of data collected as part of an investigation of a fall prevention intervention in non-ambulatory individuals with SCI. The local institutional review board approved the experimental procedures, and all participants provided written informed consent before data collection.
Participants were recruited from the community via posting of flyers in areas frequented by individuals with SCI and word of mouth. Individuals were invited to participate in the study if they met the following eligibility criteria: A self-reported history of SCI; at least 1-year post onset of SCI; over 18 years old; self-reported full-time wheelchair user (use a wheelchair > 40 h per week); self-reported inability to ambulate outside of the home and a self-reported ability to transfer with moderate assistance or less (participant is able to perform 50–100% of the effort).28 Participants were classified into 3 groups of self-reported SCI levels: cervical injuries (between cervical 1 and cervical 8), high thoracic injuries (between thoracic 1 and thoracic 8) and low thoracic injuries (below thoracic 8).
Assessment protocol
The assessment protocol used in this study is similar to the protocol described and explained, in-depth, elsewhere.26 All the assessments were administered by a trained researcher. The same researcher re-administered the FIST during the second study visit. The modified Functional Reach Test (mFRT) and the posturography assessment (the Virtual Time to Contact – VTC) were performed to test the concurrent validity of the FIST. Briefly, the FIST was administered by a trained researcher to 26 non-ambulatory individuals with SCI using the standardized protocol established by Gorman et al.25 Participants sat on a height adjustable mat table without backrest with their hips and knees flexed at 90° and their feet supported on the floor. A small stool was used for positioning and foot support when necessary. Participants sat with approximately ½ of the length of their thighs in contact with the mat table as indicated in the protocol25 The items of the FIST were administered once in the same order for all participants. Standardized instructions were used to explain the test to the participants before performing each item. The items of the FIST as developed by Gorman et al. include anterior, posterior and lateral nudges; static sitting for 30 s; shake “no”, closed eyes for 30 s, lift foot; pick up object from behind and from the floor; forward and lateral reach; anterior, posterior and lateral scooting.25 Each of the 14 items on the FIST is scored on a scale from 0 to 4. Participants score 0 when they are unable to complete the sitting task even with assistance, 1 indicates that they need a physical assistance, and 2 indicates that they use UE assistance to complete the task. Participants score 3 when they need verbal cues or more time and 4 when they complete the task independently. A total score ranging from 0 to 56 is obtained, where 0 equates to the inability to perform any of the sitting tasks, and 56 equates to the full ability to perform all of the tasks.25 No sub-score is calculated for the test. The FIST was re-administered to 22 participants by the same rater following the same protocol adopted in the first assessment after 12 weeks without intervention in between the assessments as the participants were part of a control group for an interventional study. The mFRT, a common clinical sitting balance test, was also administered at baseline after completion of the FIST to assess concurrent validity of the FIST.29 The positioning protocol used for the FIST assessment was also adopted to assess the mFRT. Participants sat on the same height adjustable mat table without backrest with their hips and knees flexed at 90° and their feet supported on the floor. Participants were asked to reach forward without losing balance and to the side with their dominant arm as far as possible. Participants were allowed to reach once for familiarization. Participants were instructed to be sure to get all their weight off the opposite side of their bottom and keep their feet on the floor. The distance reached was measured from the initial and the final position of the styloid process of the radius with a tape measure placed horizontally at participant’s acromion level. The forward and lateral mFRT were repeated twice each. The mean performances for the repetitions were used in the analysis. The assessments were not video recorded.
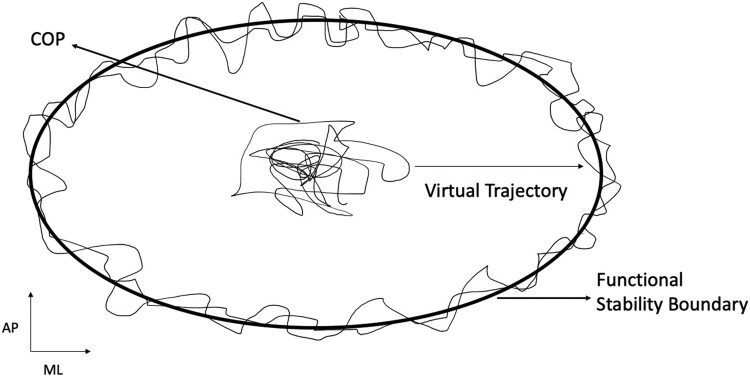
Next, to further assess concurrent validity, a posturography assessment was performed following a protocol previously established.10 Participants sat with their feet and back unsupported, and arms across their chest on a force platform (Model FP4060-05; Bertec Inc., Columbus, Ohio, USA) that was placed on a custom-built height adjustable table. Participants also sat with approximately ½ of the length of their thighs in contact with the force plate. Two trials were performed to quantify seated postural control. In the first trial, participants sat quietly with their eyes open for 30 s. Then, the participants were instructed to lean in all directions as far as possible by pivoting at the waist in a circular motion without losing their balance for 30 s. This test allowed for the determination of the seated functional stability boundary indicating the previously established virtual time to contact (VTC).16,17 CoP displacement collected from the force plate was sampled at 100 Hz and processed with a fourth order, low pass Butterworth filter at a cutoff frequency of 5 Hz. All data were processed using a custom MATLAB script (Mathworks Inc., Natick, MA) to calculate the VTC to the functional stability boundary as described by Slobounov et al.30 (See Fig. 2). The virtual time taken by the CoP, following a virtual path (ρi), to move from its position to the functional boundaries was used to calculate the VTC using the following equation:
Figure 2.
Visual representation of the functional stability boundary, center of pressure (COP) sway, and virtual trajectory. AP, anteroposterior; ML, mediolateral.
where r is the instantaneous initial position; v is the velocity; a is the acceleration.
Higher VTC values correspond to an increased functional sitting stability.16
Statistical analysis
Descriptive statistics of the demographic data were calculated to characterize the sample. A Shapiro–Wilk test indicated the data analyzed in this study (FIST visits 1 and 2, VTC, lateral mFRT, and forward mFRT) were normally distributed. Test-retest reliability of the FIST was calculated using the Intraclass Coefficient Correlation (ICC). The ICC is considered fair to good between 0.40 and 0.75 and excellent more than 0.75.31 The standard error measurement (SEM) of the FIST was estimated using the following formula: SEM = where indicates the standard deviation of the FIST (first visit).32,33 In addition, the minimal detectable change (MDC) of the FIST was calculated using the following formula: MDC = 1.96*SEM.32,33 The internal consistency reliability of the individual FIST items was evaluated using Cronbach’s Coefficient-α. For clinical application, this coefficient is considered excellent when it is higher than 0.9, satisfactory between 0.7 and 0.9, and acceptable between 0.6 and 0.7.34 Pearson’s Product-Moment Correlation Coefficient was used to examine the concurrent validity of the FIST with the mFRT and the VTC. The correlation coefficient was considered high between 0.8 and 1, moderately high between 0.6 and 0.79, moderate between 0.4 and 0.59, low between 0.2 and 0.39, and no relationship between 0 and 0.19.35 In addition, a Kruskal–Wallis H test was used to determine the ability of the FIST to distinguish the self- reported injury levels: discriminant validity. Cervical injury, high thoracic injury, and low thoracic injury levels were used as sub-groups for the discriminant validity analysis. All statistical analyses were carried out using SPSS version 21.0 (SPSS Inc., Chicago, Illinois USA). The significance level was set, a priori, at P < 0.05.
Results
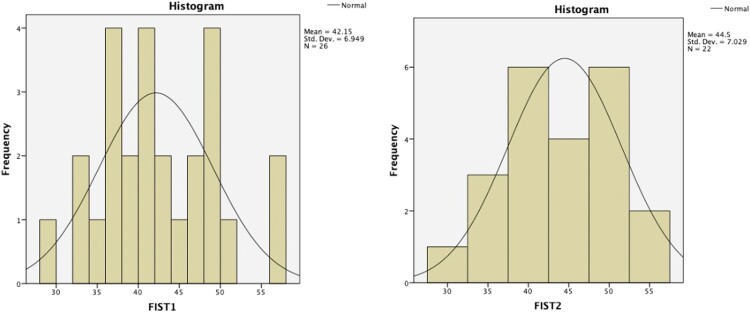
Data from a total of 26 individuals with SCI were analyzed for this study. The sample included 16 women and 10 men. Age ranged from 20 to 72 years, with an average age of 39 ± 15 years. Time since SCI ranged from 2 to 66 years, with an average of 21 ± 18 years since injury. Self-reported level of injury ranged from C4 to L3. Three participants presented with a cervical level injury, 10 high thoracic (between T1–T8) and 13 low thoracic (below T8). Nine participants were considered an “A” on the American Spinal Injury Association Impairment Scale (AIS), 2 AIS B, 10 AIS C, 1 AIS D and 4 unknowns. Basic demographic characteristics are summarized in Table 1. The mean performance scores of the FIST for visit 1 and visit 2 were 42 ± 7 and 44.5 ± 7, respectively (see Fig. 3), the VTC mean score was 1.2 ± 0.32 while the mean performance of the forward mFRT was 10.8 ± 4.6 cm and lateral mFRT was 6.3 ± 4.2 cm.
Table 1. Demographic characteristics of the participants.
| Age in years [mean ± SD] (range) | [39 ± 15] (20–72) | |
| Sex [n (%)] | Male = 10 (38.5) | |
| Female = 16 (61.5) | ||
| Type of injury [n (%)] | AIS A = 9 (34.6) | |
| AIS B = 2 (7.7) | ||
| AIS C = 10 (38.5) | ||
| AIS D = 1 (3.8) | ||
| Missing = 4 (15.4) | ||
| Level of injury (n) | C = 3 | |
| HT = 10 | ||
| LT = 13 | ||
| FIST 1 (mean ± SD) | 42 ± 7 (29–56) | |
| C | 37 ± 6 (33–41) | |
| HT | 42 ± 3 (38–48) | |
| LT | 45 ± 8 (33–56) | |
| FIST 2 (mean ± SD) | 44 ± 7 (30–56) | |
| VTC (mean ± SD) | 1.2 ± 0.32 (0.51–1.68) | |
| Forward mFRT in cm (mean ± SD) | 10.8 ± 4.6 (0–20) | |
| Lateral mFRT in cm (mean ± SD) | 6.3 ± 4.2 (0–16) | |
Notes: AIS, American Spinal Injury Association Impairment Scale; C, cervical; HT, high thoracic; LT, low thoracic; FIST 1 = function in sitting test (first assessment); FIST 2 = (second assessment); mFRT, modified functional reach test; VTC, virtual time to contact.
Figure 3.
Histograms with the distribution of the participants for the function in sitting test, visit 1 (FIST 1) and visit 2 (FIST 2), respectively.
Reliability
An analysis of the test-retest reliability for the FIST showed an excellent Intraclass Coefficient Correlation ICC = 0.95, P < 0.001. In addition, the FIST presented a SEM = 1.45 and a MDC = 4. The SEM and the MDC ensure the level of reproducibility of the FIST.
The Internal Consistency was analyzed based on the following specificity. All participants scored the maximum (score 4) for the first three items which are: “static sitting for 30 s”, “shake no: left and right” and “sitting eyes closed for 30 s”. These items presented a ceiling effect, and consequently, the variance of these items was zero. The percentage of a ceiling effect for the items is evaluated at 21% of the total items of the FIST. Based on this, the 3 items were automatically excluded from the internal consistency analysis. The results showed that Cronbach’s coefficient-α for the internal consistency reliability was 0.81.
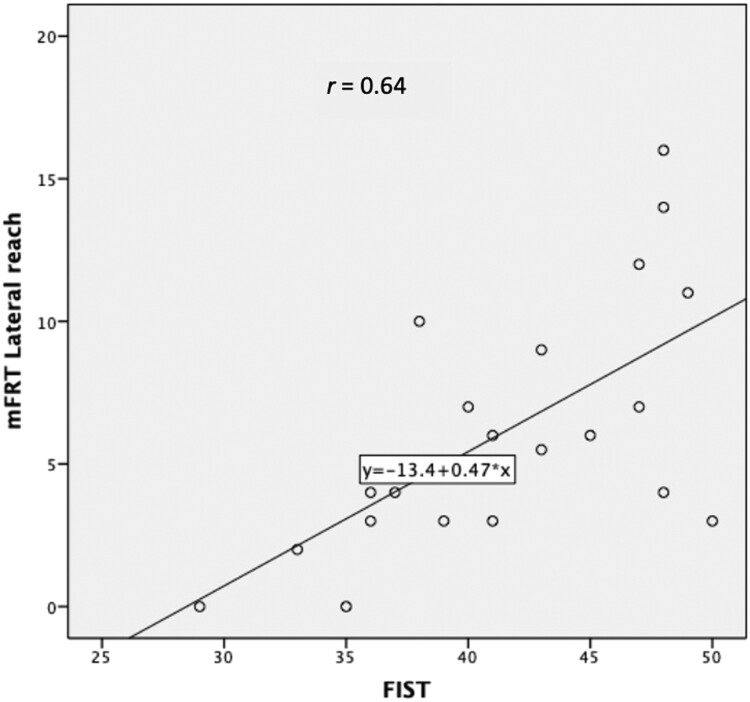
Validity
The correlation analyzed between the FIST and the lateral mFRT was moderate and significant (r = 0.64, P < 0.001) (see Fig. 4). The FIST did not correlate either with the forward mFRT (r = 0.16, P = 0.42) nor with the VTC (r = 0.23, P = 0.25).
Figure 4.
Scatter plot of the relationship among the function in sitting test (FIST) and the modified functional reach test (mFRT) lateral reach.
A Kruskal–Wallis H test between injury level groups (cervical, high-thoracic and low-thoracic) showed that there is a significant difference between-group effect of level of injury on the FIST scores χ2(2) = 7, P = 0.03.
Discussion
The purpose of this study was to investigate whether the FIST is a reliable and valid measure to assess sitting balance among non-ambulatory individuals with SCI. The original version of the FIST, validated for individuals with stroke and multiple sclerosis, is feasible to be utilized for individuals with SCI regardless of the type of injury (AIS A, B, C, and D), and level of injury (cervical, high thoracic and low thoracic). The FIST provides an assessment with functional tasks analyzing which specific underlying sitting balance systems are affected and may be managed in rehabilitation. None of the clinical sitting balance measures (the trunk control test, sitting balance measure, and the set of assessment tools) suggested by Abou et al. is able to evaluate all the sitting balance systems.24 In addition, none of the items of the suggested balance measures assesses the sensory integration with the sitting balance systems as provided by the items of the FIST. Our study found satisfactory internal consistency of the FIST, excellent test-retest reliability and discriminant validity. In addition, the SEM and a MDC of the FIST were determined. The FIST correlated with the lateral mFRT but not with the forward mFRT and the VTC. Thus, our findings indicate that the FIST is a reliable clinical measure with a partially established validity to assess sitting balance among non-ambulatory individuals with SCI. Further studies are required to improve the FIST to objectively document clinical sitting balance among non-ambulatory individuals with SCI.
The study showed an ICC of 0.95 indicating excellent test-retest reliability of the FIST for use in a clinical setting and research context to assess functional sitting balance among non-ambulatory individuals with SCI. This finding is similar to the previous results of studies investigating the test-retest reliability of the FIST in individuals with stroke (ICC = 0.97, confidence interval 0.85–0.99)27 and with multiple sclerosis (ICC = 0.92, confidence interval 0.68–0.98).26 This test-retest result ensures stability of the FIST to measure sitting balance over time. In addition, the SEM estimation indicates that the FIST has a measurement error of 2 points and the MDC indicates that the smallest change in the FIST score that can be detected objectively is 4 points. A change score on the FIST of 4 points ensures that the change is greater than the measurement error.
In addition to the test-retest reliability, the results showed a satisfactory internal consistency of the FIST. The internal consistency analysis in our study was based on 11 of the 14 items because the first 3 items “static sitting for 30 s”, “shake no: left and right” and “sitting eyes closed for 30 s”, presented a variance of zero, indicating a ceiling effect. This may be due to the fact that the 3 items are not challenging enough for the majority of the participants in our study. Also, all the participants with motor-complete injury (AIS A and B) scored 0 for the item “sitting, lift foot”. Our results suggest that robust analyses, such as RASH analyses, are required to determine the contribution of each item of the FIST. A robust analysis will determine which items need to be removed or adapted depending on the level of injury (tetraplegia and paraplegia) and/or on the type of injury (motor-complete and incomplete) to improve the specificity of the FIST. For example, individuals with motor-complete SCI (AIS A and B) independent of the level of injury are likely to score 0 for the item “sitting, lift foot” due to complete lower limb paralysis. We suggest adding a “unable to perform” option that would not be included in the final score.
The results also showed a correlation between the FIST and the lateral mFRT (r = 0.64) indicating a concurrent validity of the FIST. The mFRT is a widely used clinical measure among ambulatory and non-ambulatory individuals with SCI29,36,37 and other various neurological individuals including stroke,38 Parkinson’s disease,39 and multiple sclerosis40 to evaluate sitting and standing balance. It has been suggested that longer reaching distance without losing balance is associated with greater stability. Gagnon et al. reported that seated reaching capacity is a strong predictor of wheelchair mobility among non-ambulatory individuals with SCI.15 In addition, it has been suggested that ambulatory individuals with SCI with a forward reaching distance more than 20 cm are at a greater risk of multiple falls.36 Among non-ambulatory individuals with SCI, there is no data available on prediction of falls. Acknowledging that forward reaching is not equal to lateral reaching, based on the correlation found in our study between the FIST and the lateral mFRT; we hypothesize that a refined version of the FIST may be able to predict falls and should be explored in future studies.
The FIST did not correlate with the forward mFRT and the VTC. This result was expected since the forward mFRT and the VTC probably do not assess the same construct as the FIST. In fact, the mFRT and the VTC only assess the dynamic limits of stability of sitting balance without hands support while the FIST assessment integrates all the sitting balance components rating the amount of hands support. A possible explanation for these results may also be the heterogeneity of the sample regarding the type of injury and the small number of participants included in the study. In addition, the nature of the assessments and the methods used may explain the absence of correlation between these measures. Although all participants were guarded by a trained research assistant, non-ambulatory individuals with SCI may feel more confident reaching to the side due to the presence of a physical support surface (mat table) under the direction in which they were asked to reach than reaching forward and pivoting at the waist in a circular motion (forward mFRT and VTC respectively) in which limited physical support was available under the direction they were asked to reach/shift weight. Another explanation may be the fact that we did not make any adjustments of the trunk length and that the head-arm-trunk segment weight was not estimated in our assessments.
The FIST also discriminates injury levels. Our results showed that there is a statistically significant difference between injury levels based on the FIST assessment. This difference is probably between individuals with cervical injury and individuals with low thoracic injury. Individuals with a low thoracic injury or below T8 impairment level have intact abdominal muscle innervation and would be expected to perform better on the FIST than individuals with a cervical level injury. A similar result has been reported regarding the ability of the mFRT to distinguish between cervical injuries and low thoracic injury.29 However, unlike the FIST which evaluates all the sitting balance systems, the mFRT only assesses the proactive system of sitting balance. The discriminant evidence of the FIST is not strong due to the small sample included in the comparison’s groups. We only had 3 participants in the cervical reported level of injury which limits the statistical power of the comparison.
Overall, the FIST is suitable for application to non-ambulatory individuals with SCI independent of the type and level of injury constituting a critical starting point for a clinical measure to be explored in research. The existing sitting balance measures provide less relevant clinical information compared to the FIST on the sitting balance systems that need to be targeted for rehabilitation. However, due to SCI-specific characteristics and groups, this version of the FIST may not be specific enough to precisely assess the needs of all individuals with SCI. Also, some items may not be challenging enough. For example, based on our findings, it is likely that individuals with lower motor-incomplete SCI will often obtain the maximum score on the item “Static sitting with eyes open” showing a ceiling effect. Indeed, for the internal consistency reliability, we detected a 21% ceiling effect. The results of this investigation confirm the feasibility of the FIST among non-ambulatory individuals with SCI, however, several item modifications may be necessary with further robust analyses to provide a precise assessment of functional sitting balance. Such an assessment is essential to plan and monitor interventions to improve functional independence among non-ambulatory individuals with SCI.
This study has limitations that should be taken into consideration. First, other important measurement properties are lacking in our study such as inter and intra-rater reliability as well as criterion validity. In addition, the sample size was relatively small taking into consideration the heterogeneity of the participants included in our study. Also, only the comparison of reported levels of injury is not enough to establish the discriminant ability of the FIST since the type of injury (AIS A, B, C, D or E) is an important factor that also may increase the variability of function. The discriminant validity of the FIST needs to be further explored since we had a very small sample for comparisons between groups. Participant’s trunk length was not measured in our protocol. Therefore, adjustments of the trunk length in the assessments of the reaching tests and the VTC may also affect the results. However, the study shows that a clinical measure including functional activities and all sitting balance systems can be used for all types of SCI independent of the type of injury and level of injury. Further research is warranted using more robust analysis such as RASH analysis to refine and improve the measurement properties of the FIST to allow the use of this measure in clinical studies such as randomized clinical trials.
Clinical relevance
The relevant components of sitting balance assessment among non-ambulatory individuals with SCI in clinical settings can be documented with the FIST which may help physical and occupational therapists to design specific task-based balance training programs accordingly. The measure provides a simple and objective assessment of the tasks which cannot be performed due to poor sitting balance and which specific components of balance are affected. This is a good starting point for a future objective sitting balance measure for non-ambulatory individuals with SCI.
Conclusion
On the basis of the results of our study, the FIST was found to be a reliable tool with partially established validity to assess sitting balance among non-ambulatory individuals with SCI in a clinical setting. Overall, the FIST demonstrated excellent test-retest reliability and satisfactory internal consistency. In addition, the FIST correlated with the lateral mFRT and was able to distinguish between levels of injury. The FIST, however, did not correlate with the forward mFRT and VTC. The measure is easy to apply and score, low cost and quick to administer which is essential for clinicians. However, due to the various levels and types of injury, further analyses are required to improve the measurement properties of the FIST to perform a more precise sitting balance assessment. Refining the FIST may improve the specificity of this measure to assess sitting balance among non-ambulatory individuals with SCI.
Disclaimer statements
Disclosure Libak Abou, JongHun Sung, Jacob J Sosnoff, and Laura A. Rice have nothing to disclose in relation to this article.
Conflicts of interest The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding Statement
This study was supported by the Craig H. Neilsen Foundation, Psychosocial Research Grants, 323277.
References
- 1.NSCICS . National spinal cord injury statistical center, Facts and Figures at a Glance. Birmingham: University of Alabama at Birmingham; 2016. [Google Scholar]
- 2.Maynard FM, Bracken MB, Creasey G, Ditunno JF, Donovan WH, Ducker TB, et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord. 1997;35(5):266–274. doi: 10.1038/sj.sc.3100432 [DOI] [PubMed] [Google Scholar]
- 3.Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma. 2004;21(10):1371–1383. doi: 10.1089/neu.2004.21.1371 [DOI] [PubMed] [Google Scholar]
- 4.Dean C, Shepherd R, Adams R.. Sitting balance I: trunk-arm coordination and the contribution of the lower limbs during self-paced reaching in sitting. Gait Posture. 1999;10(2):135–146. doi: 10.1016/S0966-6362(99)00026-0 [DOI] [PubMed] [Google Scholar]
- 5.Dean CM, Shepherd RB, Adams RD.. Sitting balance II: reach direction and thigh support affect the contribution of the lower limbs when reaching beyond arm's length in sitting. Gait Posture. 1999;10(2):147–153. doi: 10.1016/S0966-6362(99)00027-2 [DOI] [PubMed] [Google Scholar]
- 6.Black K, Zafonte R, Millis S, Desantis N, Harrison-Felix C, Wood D, et al. Sitting balance following brain injury: does it predict outcome? Brain Inj. 2000;14(2):141–152. doi: 10.1080/026990500120808 [DOI] [PubMed] [Google Scholar]
- 7.Sandin KJ, Smith BS.. The measure of balance in sitting in stroke rehabilitation prognosis. Stroke. 1990;21(1):82–86. doi: 10.1161/01.STR.21.1.82 [DOI] [PubMed] [Google Scholar]
- 8.Kwakkel G, Wagenaar RC, Kollen BJ, Lankhorst GJ.. Predicting disability in stroke – a critical review of the literature. Age Ageing. 1996;25(6):479–489. doi: 10.1093/ageing/25.6.479 [DOI] [PubMed] [Google Scholar]
- 9.Chen CL, Yeung KT, Bih LI, Wang CH, Chen MI, Chien JC.. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil. 2003;84(9):1276–1281. doi: 10.1016/S0003-9993(03)00200-4 [DOI] [PubMed] [Google Scholar]
- 10.Milosevic M, Masani K, Kuipers MJ.. Trunk control impairment is responsible for postural instability during quiet sitting in individuals with cervical spinal cord injury. Clin Biomech. 2015;30(5):507–512. doi: 10.1016/j.clinbiomech.2015.03.002 [DOI] [PubMed] [Google Scholar]
- 11.Gauthier C, Gagnon D, Grangeon M, Jacquemin G, Nadeau S, Masani K, et al. Comparison of multidirectional seated postural stability between individuals with spinal cord injury and able-bodied individuals. J Rehabil Med. 2013;45(1):47–54. doi: 10.2340/16501977-1066 [DOI] [PubMed] [Google Scholar]
- 12.Gagnon D, Nadeau S, Noreau L, Eng JJ, Gravel D.. Trunk and upper extremity kinematics during sitting pivot transfers performed by individuals with spinal cord injury. Clin Biomech. 2008;23(3):279–290. doi: 10.1016/j.clinbiomech.2007.09.017 [DOI] [PubMed] [Google Scholar]
- 13.Desroches G, Gagnon D, Nadeau S, Popovic M.. Magnitude of forward trunk flexion influences upper limb muscular efforts and dynamic postural stability requirements during sitting pivot transfers in individuals with spinal cord injury. J Electromyogr Kinesiol. 2013;23(6):1325–1333. doi: 10.1016/j.jelekin.2013.09.003 [DOI] [PubMed] [Google Scholar]
- 14.Peeters LHC, de Groot IJM, Geurts ACH.. Trunk involvement in performing upper extremity activities while seated in neurological patients with a flaccid trunk – a review. Gait Posture. 2018;62:46–55. doi: 10.1016/j.gaitpost.2018.02.028 [DOI] [PubMed] [Google Scholar]
- 15.Gagnon DH, Roy A, Gabison S, Duclos C, Verrier MC, Nadeau S.. Effects of seated postural stability and trunk and upper extremity strength on performance during manual wheelchair propulsion tests in individuals with spinal cord injury: an exploratory study. Rehabil Res Pract. 2016;2016:6842324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shin S, Sosnoff JJ.. Spinal cord injury and time to instability in seated posture. Arch Phys Med Rehabil. 2013;94(8):1615–1620. doi: 10.1016/j.apmr.2013.02.008 [DOI] [PubMed] [Google Scholar]
- 17.Janssen-Potten YJ, Seelen HA, Drukker J, Spaans F, Drost MR.. The effect of footrests on sitting balance in paraplegic subjects. Arch Phys Med Rehabil. 2002;83(5):642–648. doi: 10.1053/apmr.2002.32437 [DOI] [PubMed] [Google Scholar]
- 18.Kukke SN, Triolo RJ.. The effects of trunk stimulation on bimanual seated workspace. IEEE Trans Neural Syst Rehabil Eng. 2004;12(2):177–185. doi: 10.1109/TNSRE.2004.827222 [DOI] [PubMed] [Google Scholar]
- 19.Allison GT, Singer KP.. Assisted reach and transfers in individuals with tetraplegia: towards a solution. Spinal Cord. 1997;35(4):217–222. doi: 10.1038/sj.sc.3100393 [DOI] [PubMed] [Google Scholar]
- 20.Grangeon M, Gagnon D, Gauthier C, Jacquemin G, Masani K, Popovic MR.. Effects of upper limb positions and weight support roles on quasi-static seated postural stability in individuals with spinal cord injury. Gait Posture. 2012;36(3):572–579. doi: 10.1016/j.gaitpost.2012.05.021 [DOI] [PubMed] [Google Scholar]
- 21.Milosevic M, Gagnon DH, Gourdou P, Nakazawa K.. Postural regulatory strategies during quiet sitting are affected in individuals with thoracic spinal cord injury. Gait Posture. 2017;58:446–452. doi: 10.1016/j.gaitpost.2017.08.032 [DOI] [PubMed] [Google Scholar]
- 22.Mancini M, Horak FB.. The relevance of clinical balance assessment tools to differentiate balance deficits. Eur J Phys Rehabil Med. 2010;46(2):239–248. [PMC free article] [PubMed] [Google Scholar]
- 23.Horak FB, Wrisley DM, Frank J.. The balance evaluation systems test (BESTest) to differentiate balance deficits. Phys Ther. 2009;89(5):484–498. doi: 10.2522/ptj.20080071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abou L, de Freitas GR, Palandi J, Ilha J.. Clinical Instruments for measuring unsupported sitting balance in subjects with spinal cord injury: a systematic review. Top Spinal Cord Inj Rehabil. 2018;24(2):177–193. doi: 10.1310/sci17-00027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gorman SL, Radtka S, Melnick ME, Abrams GM, Byl NN.. Development and validation of the function in sitting test in adults with acute stroke. J Neurol Phys Ther. 2010;34(3):150–160. doi: 10.1097/NPT.0b013e3181f0065f [DOI] [PubMed] [Google Scholar]
- 26.Sung J, Ousley CM, Shen S, Isaacs ZJ, Sosnoff JJ, Rice LA.. Reliability and validity of the function in sitting test in nonambulatory individuals with multiple sclerosis. Int J Rehabil Res. 2016;39(4):308–312. doi: 10.1097/MRR.0000000000000188 [DOI] [PubMed] [Google Scholar]
- 27.Gorman SL, Rivera M, McCarthy L.. Reliability of the function in sitting test (FIST). Rehabil Res Pract. 2014;2014:593280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dodds TA, Martin DP, Stolov WC, Deyo RA.. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74(5):531–536. doi: 10.1016/0003-9993(93)90119-U [DOI] [PubMed] [Google Scholar]
- 29.Lynch SM, Leahy P, Barker SP.. Reliability of measurements obtained with a modified functional reach test in subjects with spinal cord injury. Phys Ther. 1998;78(2):128–133. doi: 10.1093/ptj/78.2.128 [DOI] [PubMed] [Google Scholar]
- 30.Slobounov SM, Slobounova ES, Newell KM.. Virtual time-to-collision and human postural control. J Mot Behav. 1997;29(3):263–281. doi: 10.1080/00222899709600841 [DOI] [PubMed] [Google Scholar]
- 31.Shrout PE, Fleiss JL.. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi: 10.1037/0033-2909.86.2.420 [DOI] [PubMed] [Google Scholar]
- 32.Streiner DL, Norman GR.. Health measurement scales: a practical guide to their development and use. 3rd ed. New York: Oxford University Press Inc; 2003. [Google Scholar]
- 33.de Vet HC, Terwee CB, Knol DL, Bouter LM.. When to use agreement versus reliability measures. J Clin Epidemiol. 2006;59(10):1033–1039. doi: 10.1016/j.jclinepi.2005.10.015 [DOI] [PubMed] [Google Scholar]
- 34.Bland JM, Altman DG.. Cronbach's alpha. Br Med J. 1997;314(7080):572. doi: 10.1136/bmj.314.7080.572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Safrit M, Wood T.. Introduction to measurement in physical education and exercise science. 3rd ed. St. Louis: Times Mirrow/Mosby; 1995. [Google Scholar]
- 36.Srisim K, Saengsuwan J, Amatachaya S.. Functional assessments for predicting a risk of multiple falls in independent ambulatory patients with spinal cord injury. J Spinal Cord Med. 2015;38(4):439–445. doi: 10.1179/2045772313Y.0000000186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boswell-Ruys CL, Sturnieks DL, Harvey LA, Sherrington C, Middleton JW, Lord SR.. Validity and reliability of assessment tools for measuring unsupported sitting in people with a spinal cord injury. Arch Phys Med Rehabil. 2009;90(9):1571–1577. doi: 10.1016/j.apmr.2009.02.016 [DOI] [PubMed] [Google Scholar]
- 38.Duncan PW, Weiner DK, Chandler J, Studenski S.. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192–M197. doi: 10.1093/geronj/45.6.M192 [DOI] [PubMed] [Google Scholar]
- 39.Behrman AL, Light KE, Flynn SM, Thigpen MT.. Is the functional reach test useful for identifying falls risk among individuals with Parkinson's disease? Arch Phys Med Rehabil. 2002;83(4):538–542. doi: 10.1053/apmr.2002.30934 [DOI] [PubMed] [Google Scholar]
- 40.Kalron A, Fonkatz I, Frid L, Baransi H, Achiron A.. The effect of balance training on postural control in people with multiple sclerosis using the CAREN virtual reality system: a pilot randomized controlled trial. J Neuroeng Rehabil. 2016;13:13. doi: 10.1186/s12984-016-0124-y [DOI] [PMC free article] [PubMed] [Google Scholar]