Abstract
Introduction
Germany is experiencing the second COVID-19 pandemic wave. The intensive care unit (ICU) bed capacity is an important consideration in the response to the pandemic. The purpose of this study was to determine the costs and benefits of maintaining or expanding a staffed ICU bed reserve capacity in Germany.
Methods
This study compared the provision of additional capacity to no intervention from a societal perspective. A decision model was developed using, e.g. information on age-specific fatality rates, ICU costs and outcomes, and the herd protection threshold. The net monetary benefit (NMB) was calculated based upon the willingness to pay for new medicines for the treatment of cancer, a condition with a similar disease burden in the near term.
Results
The marginal cost-effectiveness ratio (MCER) of the last bed added to the existing ICU capacity is €21,958 per life-year gained assuming full bed utilization. The NMB decreases with an additional expansion but remains positive for utilization rates as low as 2%. In a sensitivity analysis, the variables with the highest impact on the MCER were the mortality rates in the ICU and after discharge.
Conclusions
This article demonstrates the applicability of cost-effectiveness analysis to policies of hospital pandemic preparedness and response capacity strengthening. In Germany, the provision of a staffed ICU bed reserve capacity appears to be cost-effective even for a low probability of bed utilization.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40258-020-00632-2.
Key Points for Decision Makers
| As Germany is experiencing the second COVID-19 pandemic wave, intensive care unit (ICU) bed capacity is an important consideration. |
| In Germany, the provision of ICU bed reserve capacity appears to be cost-effective even for a low probability of bed utilization. |
Introduction
In view of the second severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic wave, the German federal government and the federal states are pursuing a strategy of COVID-19 mitigation [1]. This strategy includes a bundle of measures such as a partial shutdown of businesses, social distancing, tracking, testing, public mask wearing, and quarantine orders [1]. An important goal of this strategy is to control COVID-19 outbreaks or postpone them (‘flatten the curve’) and thus avoid overstretching intensive care unit (ICU) capacity at the time of peak demand (cf. [2]). Given the high number of transmissions in the German population at the time of writing this manuscript (14,054 new COVID-19 cases and 4257 ICU cases on December 8, 2020) [3], the German federal government and the German federal states have extended (on November 25, 2020) the additional measures, which have been in force since November, until January 10, 2021 [4]. There is hope that these measures will also reduce the incidence of infections with the influenza virus, which shows similar routes of transmission. This would avoid a double burden on hospital capacities in the forthcoming months [5].
Data from 2010/11 indicate that Germany has the highest number of ICU plus immediate care unit beds on a per-capita basis in Europe [6]. Germany’s leading position in terms of the number of ICU beds was recently confirmed in a report by the Organisation for Economic Co-operation and Development [7]. During the first SARS-CoV-2 pandemic wave, ICUs in Germany were not overwhelmed [8]. At the peak of the first wave in Germany (on April 18, 2020), 12,336 ICU beds (or 41% of the available ICU bed capacity) were still vacant [9].
In general, COVID-19 response measures can be categorized based upon the three levels of prevention: primary, secondary, and tertiary prevention [10]. Primary prevention aims to reduce the incidence of COVID-19. Secondary prevention screens for infected asymptomatic and symptomatic patients with COVID-19. At the same time, secondary prevention of infected individuals is primary prevention of potential contacts. Tertiary prevention aims to prevent sequelae of COVID-19. While the COVID-19 mitigation strategy currently pursued by the German government emphasizes primary and secondary prevention, adding ICU bed capacity is an example of tertiary prevention. The German government had pursued the latter strategy, with approximately 7000 beds added as of April 27, 2020 [11], but thereafter recommended to redeploy part of the available hospital capacity for treating non-COVID-19 patients [8]. An alternative tertiary prevention strategy that is still under investigation is medical treatment of COVID-19. Currently, there is great hope for future COVID-19 treatments by repurposing drugs that are already approved for other diseases and demonstrate acceptable safety profiles (cf. [12]).
It is possible that the current COVID-19 mitigation strategy in Germany may turn out to be insufficient in flattening the second SARS-CoV-2 pandemic wave. This strategy may also become unsustainable in terms of affordability, psychological burden, or violation of civil rights. Given the current high number of COVID-19 transmissions, the ICU bed capacity becomes an important consideration again [13]. The ICU bed capacity includes potential ICU beds (‘surge beds’) that could be supported by current staff in the event of a surge. Surge capacity is a broader term that encompasses not only potential beds but also “available space in which patients may be triaged, managed, vaccinated, decontaminated, or simply located; available personnel of all types; necessary medications, supplies and equipment; and even the legal capacity to deliver healthcare under situations which exceed authorized capacity” [14]. Little has been published on the cost effectiveness of building surge capacity for infectious and other diseases.
The purpose of this study is to evaluate the costs and benefits of maintaining or expanding a staffed ICU reserve capacity (surge beds) in Germany during the second pandemic wave and in preparation for further pandemic waves. Results of this study allow comparing the health benefits and cost effectiveness of maintaining/extending the ICU bed capacity with those of life-extending COVID-19 treatments.
Methods
General
I conducted a cost-effectiveness analysis on COVID-19 patients who have an indication for ICU care. The analysis used life-years gained as a measure of health benefits. The time horizon was the remaining lifetime. By comparing the costs and health benefits of different levels of ICU bed capacity, I calculated marginal cost-effectiveness ratios (MCERs). In addition, I performed net benefit and return on investment (ROI) calculations.
Calculation of Health Benefits
A decision model was constructed using a previously developed and validated model as a basis [15]. The latter model determines the loss of life years when no ICU bed capacity is left to treat COVID-19 patients. It is based on a life-table model that summarizes the age-specific mortality impact of the SARS-CoV-2 pandemic. To account for the age distribution of the population, the model weighs age-specific life-expectancy changes by age-specific population sizes. This paper extends the previous model based on the following conceptual idea: the clinical value of an additional ICU bed is equivalent to the marginal loss of life years in the absence of an additional ICU bed, i.e. when the demand for ICU beds exceeds the available capacity by one ICU bed. Following this principle, I calculated the weighted-average loss of life years when the demand exceeds the available ICU bed capacity by one bed, with weights reflecting the portions of patients (1) admitted to the ICU and (2) refused admission. These weights were multiplied by the average per-capita loss of life years in the German population (compared with non-crisis mortality rates) when all patients with ICU indications were admitted to the ICU and refused admission. This conceptual idea is formalized as follows:
| 1 |
where denotes lost life years, refers to admission, and denotes the currently available bed capacity. The difference in this weighted average loss of life years compared with the loss of life years with a sufficient ICU bed capacity presents the value (health benefit ) of an additional ICU bed. This is formalized as follows:
| 2 |
When sequentially adding an m number of beds, I applied the same marginal calculation. The value of each additional ICU bed diminishes which can be formally shown by taking the first derivative of Eq. (1) with respect to :
| 3 |
The negative quadratic term indicates the diminishing impact of another ICU bed on lost life years. For a given demand level, adding one bed to 1000 beds at the baseline is thus more valuable than adding one bed to 10,000 beds.
Given that this calculation relates the addition of beds to the existing national capacity, it was conducted at the population level. For this reason, I multiplied the clinical value of an additional ICU bed by the population size. I conservatively assumed that the benefits of the ICU bed capacity would only last for 12 months, thus accounting for the expected time to develop, approve, and distribute COVID-19 vaccines [16].
Presuming a harvesting effect in a sensitivity analysis, I assumed for age groups with excess mortality associated with COVID-19 (the difference between observed and pre-pandemic mortality rates) that except for COVID-19, there are no other causes of death in the forthcoming 12 months [15].
In addition to the above calculation, which yields the clinical value of an ICU bed in terms of life-years gained, I also determined its value in terms of reduction of mortality. To this end, I followed the same methodological approach but applied, as weights, mortality of patients admitted to the ICU and refused admission.
Cost Analysis
For the cost analysis, I took a societal viewpoint. To calculate medical costs, I considered the initial ICU stay, rehospitalizations occurring in the first year after discharge from the ICU, hospital copayments, as well as future consumption and unrelated care during added life years. To determine the hospital costs of treating COVID-19 patients, I considered both the operating and infrastructure costs. To calculate the operating costs, I assumed an average patient trajectory. I applied the corresponding diagnosis-related group (DRG) codes plus additional tariffs on top of the DRG payments (“Zusatzentgelt”). Furthermore, I accounted for nursing staff costs (“Pflegeentgelt”) regardless of the degree of bed utilization. Moreover, I considered extra payments by the German government for both personal protective equipment and nursing care (on top of the “Pflegeentgelt”) in treating COVID-19 patients.
To identify the appropriate DRG codes for COVID-19 cases admitted to the ICU, I followed the guidance of the German Interdisciplinary Association for Intensive Care and Emergency Medicine [17]. Specifically, I applied DRG codes that reflect the average length of stay (LOS) with and without mechanical ventilation. I purposely used conservative cost estimates, i.e. I selected higher-cost DRGs in the presence of several coding options, thus biasing against the value of an additional ICU bed. To arrive at the final cost estimate for treating a COVID-19 patient in the ICU, the costs of patients with and without mechanical ventilation were weighted by their respective shares.
To arrive at the costs of infrastructure, I accounted for the opportunity costs of capital. To calculate the latter, I considered the weighted average cost of capital (WACC). Strictly speaking, the WACC only applies to private hospitals, which account for 36% of all German hospitals, based on 2016 data [18]. However, during the coronavirus crisis, government funds covered a portion of the capital costs resulting from the expansion of ICU capacity, i.e. €50,000 per additional ICU bed [19]. Hence, the WACC for private hospitals needs to be adjusted for this portion (cf. [20]). In contrast, when public hospitals expand their capacity, they receive interest-free loans from the federal states without any obligation to pay them back. Nevertheless, only half of the infrastructure investments are currently covered by the federal states [21]. The overall opportunity cost of capital was thus calculated as a weighted average of the WACC and a zero cost of capital, with the weights representing shares of private and public funding, respectively.
To determine the future unrelated medical costs incurred during added life years, I determined the cumulative probability of an individual at age of surviving until age (i.e. the product of age-specific survival probabilities up to age ) using the life table embedded in the previously published decision model [15]. I multiplied the cumulative probability of surviving until age by health expenditures at age , took the sum over all ages , and thus obtained the remaining health expenditures for an individual at age . By comparing the remaining health expenditures for different levels of ICU bed capacity, I calculated the life-extension costs. To account for the age distribution of the population, I weighted the age-specific life-extension costs by age-specific population sizes. I performed all calculations for men and women separately and then aggregated the results.
Moreover, a societal perspective requires considering expenses for primary needs such as food, shelter, and clothing as their satisfaction contributes to life extension [22]. That is, as the denominator of the MCER captures the benefits of the resources used to satisfy primary needs, the costs of these resources also need to be included for consistency reasons [22]. To determine these types of consumption costs during added life years, I used the same calculation as for health expenditures outlined in the above paragraph.
Net Benefit and ROI Calculation
The monetary value of an additional life year was borrowed from new, innovative oncological drugs as cancer reflects a condition with a similar morbidity and mortality burden in the general population in the short term as COVID-19 [15]. To calculate the net monetary benefit (NMB) of an additional bed, I subtracted the cost of an additional bed from the monetary value created. By dividing the monetary value of an additional bed by its additional cost, I also determined the ROI.
Discounting
In the base-case analysis, I did not discount costs or health benefits, as the reported survival benefits from cancer treatment [23], which were used to determine the economic value of a life year, were undiscounted as well. In a sensitivity analysis, I discounted both costs and effects.
Sensitivity Analysis
Using one-way deterministic analyses, I assessed the parameter uncertainty by varying the input parameters that are subject to variation one at a time. In addition, I conducted threshold sensitivity analyses that determined the break-even points of additional ICU bed capacity, government subsidies for ICU bed provision, and the ICU bed utilization rate.
Cost Data
The model input data are listed in Table 1. For COVID-19 patients receiving mechanical ventilation, LOS in the ICU has been estimated to be between 11 and 20 days [30–32]. Among the DRGs that are applicable in this range, I made conservative choices. Of note, in the German DRG system, age-specific DRG codes are usually limited to children and thus played no role in assigning DRG codes. Specifically, for ICU patients receiving mechanical ventilation, I chose the DRG code E40A [40], which is the only DRG code with a specific reference to ARDS. It has a case-mix index of 3.406 and allows for an additional payment of €18.21 (code ZE162). For ICU patients who do not receive mechanical ventilation, I applied the DRG code E77B, which entails a slightly shorter LOS (15.1 vs 17.1 days) with a case-mix index of 2.090 and allows for an additional payment of €34.48 (code ZE163). Each case-mix index was multiplied by the national base price [39].
Table 1.
Input data used in the base case and the sensitivity analysis
| Input | Mean (range) | References |
|---|---|---|
| Epidemiological and clinical data | ||
| Probability of death by age and gender in Germany | See reference | [24] |
| Population size by age | See reference | [25] |
| CFR in the ICU | 0.23 (0.21–0.52) | [26–28] |
| CFR 1 year post-ICU discharge | 0.59 (0.47–0.73) | [29] |
| Proportion of cases admitted to the ICU | 0.065 (0.04–0.08) | [30] |
| False-positive ICU admissions | 0.1 (0.1–0.2) | [30] |
| ICU beds available for COVID-19 on October 26, 2020 | 9765 | [28] |
| Proportion of ICU patients with mechanical ventilation | 0.46 | [28] |
| ICU length of stay | 14 (11–20) | [30–32] |
| Cost data | ||
| Healthcare expenditure by age | See reference | [33] |
| Consumption costs per year, primary needs (€) | [34] | |
| Adult | 11,580 | |
| Child | 3984 | |
| ICU bed, infrastructural cost (€) | 85,000 (85,000–100,000) | [35–37] |
| Weighted average cost of capital (%) | 0.06 | [38] |
| ICU costs per admission (with mechanical ventilation) (€) | 12,551 | [39, 40] |
| ICU costs per admission (without mechanical ventilation) (€) | 7725 | [39, 40] |
| Hospital copayment per day (€) | 10 | [41] |
| Nursing care payment per patient per day (€) | 185 | [19] |
| Personal protective equipment per patient (€) | 50 | [19] |
CFR case fatality rate, ICU intensive care unit, IFR infection fatality rate
In terms of the infrastructure costs of ICU beds, the estimates range between €85,000 and €100,000 [35–37]. In the base case, I applied an estimate provided by the German Hospital Federation, which was €85,000 [36]. This estimate includes the costs of ventilators and monitoring equipment associated with ICU bed provision [42]. While the acquisition costs of ventilators plus monitoring equipment is around €35,000 [42] and therefore less than €85,000, the calculated difference (€50,000) may be seen as a reflection of opportunity costs because a bed with or without a ventilator could be used otherwise to generate revenues for the hospital. A societal perspective as chosen in this study mandates the inclusion of opportunity costs.
In terms of the infrastructure costs, I accounted for nursing staff costs by multiplying the nursing care case-mix pertaining to the relevant DRG codes by the national base price and the number of days (365).
To estimate the costs of rehospitalizations occurring in the first year after discharge from the ICU, I used the results of a published cohort study of 396 ICU survivors with ARDS. The study was conducted between September 2014 and April 2016 in 61 German hospitals [43]. The study reported a median number of rehospitalizations of 2 (interquartile range 1–3). The LOS was 16 days on average (interquartile range 10–25). Of note, rehospitalizations included stays in rehabilitation facilities as well as admissions for medical conditions unrelated to ARDS. The data did not differentiate between different types of rehospitalizations or admissions to ICUs and normal wards. Given the latter, I applied the costs of the initial ICU stay, thus conservatively assuming that all rehospitalized patients would be admitted to the ICU.
As outlined in the cost analysis section, for ICU survivors I determined both future (unrelated) medical and consumption costs during added life years. To account for the former, I used the healthcare expenditures in the general population, which were available for four age categories based on 2015 data [33] and explicitly referred to national (societal) costs and not to social health insurance costs. The data on the private consumption costs were from 2017 [34]. The categories of the private consumption costs were available for adults and children but not according to age. To narrow down the consumption costs to those for primary needs, I considered the per capita private consumption costs on food and nonalcoholic beverages, clothing and shoes, housing (including maintenance), and energy.
The capital costs, which served as an input to the cost of infrastructure of private hospitals, were based on the whole healthcare and pharmaceutical industry [38]. All costs were inflated to 2020 euros based on the general German Consumer Price Index.
Other Data
Patients who require an ICU bed were considered true positives and true positives were assumed to die otherwise. I assumed a 10% rate of inappropriate (false positive) ICU admissions in the base case. A rate above 0% seems plausible given that “good clinical practice demands that greater emphasis be placed on patient safety by limiting false negatives” [44]. This strategy comes at the risk of excessive use of ICU facilities. Nevertheless, even a rate of 10% has been considered “exceptionally low” in a non-COVID-19 setting [44]. Therefore, I increased the rate to 20% in a sensitivity analysis.
The willingness to pay for an additional life year (€101,493 per life-year gained) was obtained by dividing incremental costs of new, innovative cancer drugs (€39,751) by the incremental survival benefit (0.39 life years) [15].
Given the lack of official guidance on the discount rates for the costs and health benefits from a societal perspective in Germany, I applied a 3% discount rate for the costs based on the social rate of time preference derived from the Ramsey equation [45]. For health benefits, I applied a 2% discount rate, reflecting a 1% expected growth rate of the consumption value of health in Germany (cf. [46]).
Results
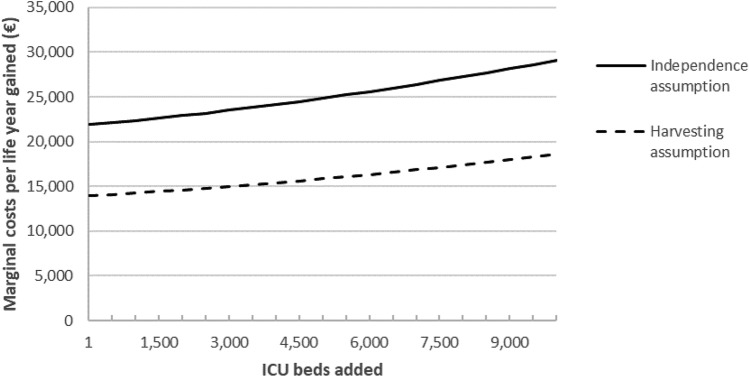
The last staffed bed added to the existing ICU bed capacity yields an MCER of €21,958 per life-year gained and an ROI of 4.6 in the base case assuming full bed utilization. A bed utilization of 1.1% yields a break-even ROI of 1. The low utilization necessary to break even results from the low share of infrastructure costs. The cost-effectiveness and ROI diminish with additional increases in ICU bed capacity (Fig. 1). This trend holds because when the demand for ICU beds exceeds the available capacity, the clinical value of an additional bed diminishes (see Eq. 3).
Fig. 1.
Marginal costs per life-year gained by adding intensive care unit (ICU) bed capacity
Based on the harvesting assumption, the cost effectiveness of supplying an additional ICU bed improves (to €14,003) because COVID-19 patients who are saved from death in the presence of an additional bed are assumed to represent a healthier subgroup of ICU patients than those who unavoidably die.
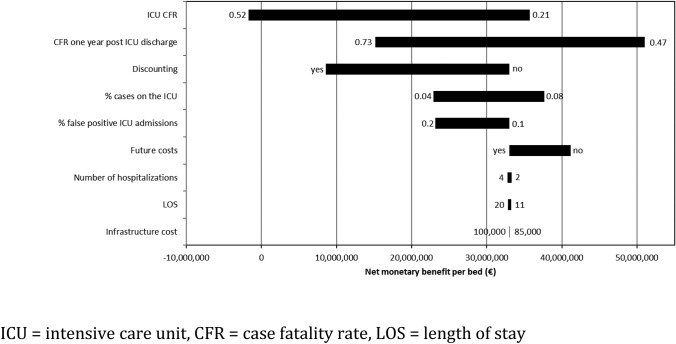
As shown in the sensitivity analysis (see Fig. 2), the variables with the greatest impact on NMB were the mortality rates in the ICU and after discharge. Ceteris paribus, higher mortality rates reduce the NMB of an additional ICU bed.
Fig. 2.
Tornado diagram demonstrating the results of the one-way sensitivity analysis. The variables are ordered by the impact on the net monetary benefit of the provision of additional ICU bed capacity versus no intervention. The numbers indicate the upper and lower bounds
Expanding staffed ICU bed capacity by another 10,000 beds or 102% of the available capacity (9765 beds on October 26, 2020) is projected to increase societal costs by €50 billion. The resulting decrease in the mortality of ICU candidates is 24% compared with no intervention (Fig. 3). While the ROI diminishes with the expansion of capacity, it remains above three for the ten thousandth bed added.
Fig. 3.
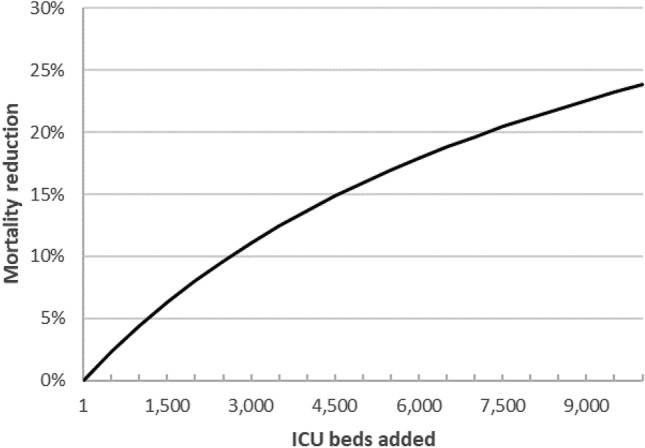
Mortality reduction of intensive care unit (ICU) candidates by increasing ICU bed capacity compared with no increase
Threshold sensitivity analysis shows that negative returns do not appear even with a 16.4-fold increase in ICU bed capacity. Similarly, a government subsidy or bonus of €7.5 million per ICU bed still yields a positive NMB for the ten thousandth bed added.
Discussion
Facing the second SARS-CoV-2 pandemic wave, the German government has imposed stricter measures. However, the current strategy may turn out to be insufficient in preventing overstretching of ICU capacity at the time of peak demand. Therefore, the ICU bed capacity is still a relevant consideration. As shown in this analysis, the pre-existing staffed ICU bed capacity is cost effective even for a utilization rate as low as 2%.
Further extending the existing ICU bed capacity seems acceptable based on the MCER but also from a budgetary perspective. That is, extending capacity by more than 100% is forecast to result in a one-time increase in healthcare expenditure [47] of 13%, which amounts to 1.5% of the gross domestic product (GDP) in Germany [48].
As a word of caution, cost effectiveness of ICU bed expansion is based on the assumption of a positive probability of utilizing the additional ICU bed capacity. If, however, the additional capacity remains entirely unused, the value of investment becomes negative due to the presence of fixed costs. However, it is reassuring that even a vacancy rate of 98% still allows for a positive return due to the low share of infrastructure costs. This is equivalent to a 2% probability of having full utilization. Hence, the additional beds are best characterized as surge beds, which could potentially be used in the event of a surge but may remain vacant.
How does this finding fit into the virus mitigation strategy currently pursued by the German government, which aims to control the number of new infections? A strategy of supplying additional ICU beds becomes cost effective once there is a 2% probability that the virus mitigation strategy is not successful or is abandoned because it is too expensive or burdensome for society or because a vaccine is not distributed in time. Hence, an economic justification for a bed expansion strategy requires a positive probability of viral spread in the population, potentially leading to herd immunity by natural infection, regardless of whether this is actively sought by the government. Although an overload of the intensive care bed capacity may still seem unlikely at the time of writing this manuscript (December 8, 2020), mean values are less relevant than extreme values in disaster control. Instead, the so-called fat tail risk, that is, a non-negligible probability that a catastrophe will occur, is an important consideration. Indeed, such a thick end of the distribution has been observed in “major epidemic and pandemic diseases of history” [49].
Of note, there are different ways of providing the additional ICU capacity. These approaches not only include the construction of new buildings but also freeing up existing capacity, e.g. deferring elective procedures, moving non-COVID-19 patients to alternative sites, and using step-down care more aggressively. In addition, ICU units and beds may be converted from existing capacity, such as operating, recovery, procedure and treatment rooms; ambulatory surgery centers; unstaffed floors; physical therapy space; outpatient facilities; and nonhealthcare facilities [50, 51]. In the short term, freeing up existing capacity may, in fact, be the only feasible approach. However, to meet a potential increase in future demand for ICU beds, the construction of new buildings and the conversion of existing capacity may be unavoidable.
Creating surge capacity also requires recruiting additional personnel (e.g. ICU nurses) as well as purchasing additional materials, supplies (e.g. protective clothing), and equipment (e.g. ventilators). However, even before the SARS-CoV-2 pandemic the healthcare environment in Germany has been characterized by labor shortages, particularly ICU nurses [52]. In 2018, the German government initiated steps to improve short- and long-term nursing staff numbers [53]. In general, short-term strategies to address a shortage of labor in the ICU include accelerated training for ICU nurses; contacting former nurses with ICU experience and other recently retired staff; and redeploying anesthesiologists, other physicians, other nurses, respiratory therapists, other allied health professionals and other staff with appropriate skills to work in a critical-care environment [50, 54, 55]. In fact, during the first pandemic wave in Germany, former nurses responded to COVID-19 calls to return to service. Assuming that altruistic motives played a major role, attractive sign-on bonuses may enable recruitment of an additional cohort of former nurses with stronger financial motives. What this study shows is that sign-on bonuses for former nurses can be quite high given the large societal NMB of a filled ICU bed. Based on the model, a sign-on bonus of, say, €20,000 per ICU nurse or equivalent staff member, plus the cost of a refresher course, would lead to a negligible increase in the required probability of full utilization.
Strategies to create surge capacity can lead to opportunity costs. If ICU labor and bed capacity is expanded, say, by cancelling or postponing unrelated treatments (e.g. elective surgeries), this would increase the minimum acceptable bed utilization rate. Therefore, a strategy of supplying additional ICU beds requires careful planning.
Recently, dexamethasone was shown to lower the 28-day mortality among hospitalized COVID-19 patients receiving respiratory support [56]. Expanding ICU bed capacity and life-prolonging treatments of COVID-19 become complementary interventions if life-prolonging treatments have a label for ICU patients. In that case, ICU bed expansion becomes an enabling strategy for life-prolonging treatments and creates option value (cf. [57]). Both interventions applied together, thus form a combination therapy. This is also confirmed in the sensitivity analysis of this paper, implying an improved cost effectiveness of ICU bed expansion when accounting for a lower ICU mortality. Of note, the absolute mortality reduction demonstrated by dexamethasone (12%) is already achieved by an ICU capacity expansion of 3500 beds (assuming full capacity utilization), thus emphasizing the clinical significance of ICU bed expansion.
If expanding ICU bed capacity and providing life-prolonging treatments of COVID-19 are complementary approaches, but ICU bed capacity is a limiting factor, life-prolonging treatments may not be applicable unless they are prescribed on-label or off-label before ICU admission. In that case, life-prolonging treatments can be regarded as a substitute for expanding ICU bed capacity. Similarly, if life-prolonging treatments have a label for hospitalized patients without mechanical ventilation and are able to reduce ICU admissions, they become a substitute for expanding ICU bed capacity.
The limitations of this study need to be acknowledged. First, there are reasons why the base-case analysis underestimates the MCER and overestimates the NMB. Some of these reasons were already captured in the sensitivity analysis and include high mortality in the ICU and post-discharge. As shown, a high CFR in the ICU even leads to a negative NMB. One reason for a higher CFR in the ICU exists when rationing decisions in the absence of an ICU bed disfavor patients with less prospect of survival. Thus, patients who are not admitted to the ICU are likely to be older and at higher risk. Furthermore, this study did not include direct nonmedical costs, such as time and transportation costs, which are mandated by the societal perspective adopted in this paper. Moreover, given the funding challenges of the coronavirus crisis for the German healthcare system, stepping up surge capacity may create increasing opportunity costs. The latter would be accounted for by a decreasing willingness to pay for an additional life year. Nevertheless, as in this analysis, MCERs are far below the willingness to pay threshold over a large increment of beds, a diminishing willingness to pay would only matter for extreme expansions.
On the other hand, there are reasons to believe that the base case underestimates the NMB, i.e. overestimates the MCER. First, by including future medical costs along with the costs of hospitalizations in the first year after ICU discharge, some double counting of hospitalization costs may result. Furthermore, the DRG rates may not reflect true hospital costs and may yield a positive profit margin for ventilated patients [58]. Moreover, the productivity gains resulting from a reduction in mortality were not included due to the age distribution of averted deaths (the median age is 82 years) and the difficulty of disentangling deaths in relevant age groups (e.g. in the age group 50–69 years). Finally, an additional reserve capacity may also prevent deaths from other infectious disease outbreaks and public health emergencies. Some of the biases mentioned in this and the previous paragraph may cancel each other out.
Furthermore, the number of life years as an outcome measure may be criticized for lacking a consideration of health-related quality of life unlike quality-adjusted life years (QALYs). QALYs diminish the health benefits obtained from additional survival by accounting for a quality-of-life decrement of ICU survivors. As the QALY metric thus discriminates against the elderly and the disabled, it has been considered ethically controversial [59]. There also exists a methodological concern with regard to QALYs when the quality of life of ICU survivors is reduced to a degree that they do not want to go on living. This so-called maximum endurable time invalidates the QALY metric [60] (as a word of caution, the presence of a maximum endurable time would also question the appropriateness of using life-years gained or even lives saved as measures of health benefit but rather for ethical than for methodological reasons). For these reasons, QALYs have not been used so far in Germany for the purpose of reimbursing and pricing new, innovative medicines (cf. [61]). As another counterpoint, the public debate on COVID-19 in Germany has mainly focused on mortality as an endpoint and the number of life-years lost by the elderly who die from COVID-19. In summary, there is not a straightforward answer to the question of which outcome measure best reflects the value of expanded ICU capacity. Life-years gained may serve as a compromise between the use of unweighted lives saved and QALYs gained.
In terms of the transferability of the results and conclusions of this study to other countries, the usual caveats apply. The reasons for caution include between-country differences in clinical and epidemiological data, costs, and the willingness to pay for health benefits.
This article demonstrates the applicability of cost-effectiveness analysis to strengthening hospital pandemic preparedness and response capacity. For data collection in the forthcoming months of the crisis, policymakers should pay particular attention to mortality data, as the MCERs and ROIs forecasted in this study were shown to be particularly sensitive to these data.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
I would like to thank Rolf Bartkowski and Rainer Sibbel for their valuable comments on the hospital cost calculation. In addition, I thank the three anonymous reviewers for their insight full comments on the manuscript. Any remaining errors are, of course, my responsibility.
Declarations
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest
AG declares that he has no conflict of interest.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
All data are contained within the manuscript.
Code availability
Not applicable.
References
- 1.Bundesregierung. Coronavirus in Deutschland. https://www.bundesregierung.de/breg-de/themen/coronavirus. Accessed 27 Dec 2020.
- 2.Bundesregierung. Drittes Bevölkerungsschutzgesetz: Kriterien für Pandemiebekämpfung präzisiert. https://www.bundesregierung.de/breg-de/themen/buerokratieabbau/bevoelkerungsschutzgesetz-1805062. Accessed 27 Dec 2020.
- 3.Robert Koch Institut. Daily Situation Report of the Robert Koch Institute. 08/12/2020. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Dez_2020/2020-12-08-en.pdf?__blob=publicationFile. Accessed 27 Dec 2020.
- 4.Bundesregierung, Corona-Regeln: Das gilt an Weihnachten und Silvester. November 25, 2020. https://www.bundesregierung.de/breg-de/themen/coronavirus/corona-weihnachten-1825108. Accessed 27 Dec 2020.
- 5.WHO Regional Office for Europe . Health system considerations: when influenza meets COVID-19—preparedness and response measures when COVID-19, influenza and acute respiratory infections coincide in the WHO European Region. Copenhagen: WHO Regional Office for Europe; 2020. [Google Scholar]
- 6.Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38(10):1647–1653. doi: 10.1007/s00134-012-2627-8. [DOI] [PubMed] [Google Scholar]
- 7.Organisation for Economic Co-operation and Development . Beyond Containment: Health systems responses to COVID-19 in the OECD. Paris: OECD; 2020. [Google Scholar]
- 8.Bundesministerium für Gesundheit. Ein neuer Alltag auch für den Klinikbetrieb in Deutschland. April 27, 2020. https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/C/Coronavirus/Faktenpapier_Neuer_Klinikalltag.pdf. Accessed 27 Dec 2020.
- 9.Robert Koch Institut. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/2020-04-18-de.html. Accessed 27 Dec 2020.
- 10.Fletcher R, Fletcher SW. Clinical epidemiology: the essentials. 5. Philadelphia: Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 11.Bundesamt für Soziale Sicherung. Zahlungen des BAS aufgrund der COVID-19-Pandemie. October 27, 2020. https://www.bundesamtsozialesicherung.de/de/themen/covid-19-krankenhausentlastungsgesetz/auszahlungsbetraege/.
- 12.Naveja JJ, Madariaga-Mazón A, Flores-Murrieta F, Granados-Montiel J, Maradiaga-Ceceña M, Alaniz VD, Maldonado-Rodriguez M, García-Morales J, Senosiain-Peláez JP, Martínez-Mayorga K. Union is strength: antiviral and anti-inflammatory drugs for COVID-19. Drug Discov Today. 2020 doi: 10.1016/j.drudis.2020.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DW. Corona-Pandemie: Intensivstationen nähern sich offenbar der Belastungsgrenze. December 6, 2020. https://www.dw.com/de/intensivstationen-nähern-sich-offenbar-der-belastungsgrenze/a-55835947. Accessed 27 Dec 2020.
- 14.Joint Commission on Accreditation of Healthcare Organizations. Health care at the crossroads health care at the crossroads strategies for creating and sustaining community-wide emergency preparedness systems. 2003. https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/topics-library/emergency_preparednesspdf.pdf?db=web&hash=91EF71C40DB61C83B34368560B7DD52C. Accessed 27 Dec 2020.
- 15.Gandjour A. The clinical and economic value of a successful shutdown during the SARS-CoV-2 pandemic in Germany. Q Rev Econ Finance. 2020 doi: 10.1016/j.qref.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CNN. Fauci says we may not get back to our normal lives until the end of 2021. September 11, 2020. https://edition.cnn.com/world/live-news/coronavirus-pandemic-09-11-20-intl/h_429c94d4d63f9ab3a1b632ef081c1e15.
- 17.Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin (DIVI). Kodierung der Coronavirus-Krankheit-2019 [COVID-19]. March 24, 2020. https://www.divi.de/joomlatools-files/docman-files/publikationen/covid-19-dokumente/Kodierung_Coronavirus_2020_03_24.pdf.
- 18.Bundesverband Deutscher Privatkliniken. Krankenhäuser nach Trägerschaft. Stand: 2016. https://www.bdpk.de/positionen/statistiken/krankenhaeuser5/allgemeine-krankenhaeuser-nach-traegerschaft.
- 19.Bundesregierung. 2020. Covid19-Krankenhausentlastungsgesetz: Kliniken und Praxen werden gestärkt. March 27, 2020. https://www.bundesregierung.de/breg-de/themen/coronavirus/covid19-krankenhaus-gesetz-1733614.
- 20.Zapp W, Haubrock M. Kennzahlen im Krankenhaus. Lohmar: Josef Eul Verlag; 2010. [Google Scholar]
- 21.GKV-Spitzenverband. Investitionsbedarf der Krankenhäuser—aktuelle Auswertung bestätigt Unterfinanzierung durch die Bundesländer. March 28, 2018. https://www.gkv-spitzenverband.de/gkv_spitzenverband/presse/pressemitteilungen_und_statements/pressemitteilung_680448.jsp. .
- 22.Gandjour A. Consumption costs and earnings during added years of life—a reply to Nyman. Health Econ. 2006;15(3):315–317. doi: 10.1002/hec.1065. [DOI] [PubMed] [Google Scholar]
- 23.Storm A, Greiner W, Witte J. AMNOG-Report 2017: Nutzenbewertung von Arzneimitteln in Deutschland. DAK-Gesundheit; 2017.
- 24.Bundesamt S. Allgemeine Sterbetafel. Wiesbaden: Statistisches Bundesamt; 2019. [Google Scholar]
- 25.Statistisches Bundesamt. Vorausberechneter Bevölkerungsstand. Moderate Entwicklung der Geburtenhäufigkeit, Lebenserwartung und Wanderung (G2L2W2). Wiesbaden: Statistisches Bundesamt; 2020.
- 26.Adlhoch C, Gomes Dias J, Bonmarin I, Hubert B, Larrauri A, Oliva Domínguez JA, Delgado-Sanz C, Brytting M, Carnahan A, Popovici O, Lupulescu E. Determinants of fatal outcome in patients admitted to intensive care units with influenza, European Union 2009–2017. Open Forum Infect Dis. 2019;6(11):ofz462. doi: 10.1093/ofid/ofz462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, Lee M. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323(16):1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robert Koch Institut. https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Okt_2020/2020-10-26-de.pdf?__blob=publicationFile. Accessed 27 Dec 2020.
- 29.Damuth E, Mitchell JA, Bartock JL, Roberts BW, Trzeciak S. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(7):544–553. doi: 10.1016/S2213-2600(15)00150-2. [DOI] [PubMed] [Google Scholar]
- 30.KSTA. Grippe oder Covid-19? Diese Symptome sprechen für eine Infektion mit dem Coronavirus. March 27, 2020. https://www.ksta.de/ratgeber/gesundheit/grippe-oder-covid-19--diese-symptome-sprechen-fuer-eine-infektion-mit-dem-coronavirus-36470456. Accessed 27 Dec 2020.
- 31.Stang A, Stang M, Jöckel KH. Estimated use of intensive care beds due to COVID-19 in Germany over time. Dtsch Arztebl Int. 2020;117:329–335. doi: 10.3238/arztebl.2020.0329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.SWR. Coronavirus—so werden Covid-19-Patienten auf Intensivstation behandelt. April 1, 2020. https://www.swr.de/wissen/coronavirus-so-werden-schwerstkranke-covid-19-patienten-auf-intensivstation-behandelt-100.html. Accessed 27 Dec 2020.
- 33.Statistisches Bundesamt. Krankheitskosten: Krankheitsklassen und Alter in Euro je Einwohner der jeweiligen Altersgruppe. 2015. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Krankheitskosten/Tabellen/krankheitsklassen-alter.html;jsessionid=B0F2B949894388182E44014F74A76084.internet8722. Accessed 27 Dec 2020.
- 34.Statistisches Bundesamt. Einkommen, Konsum, Lebensbedingungen. Statistisches Jahrbuch 2019. Wiesbaden: Statistisches Bundesamt; 2019.
- 35.Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin (DIVI). Pressemitteilung. March 22, 2020. https://www.divi.de/presse/pressemeldungen/pm-corona-pandemie-das-gesetzesvorhaben-zur-finanzierung-der-covid-19-behandlungen-ist-so-nicht-akzeptabel. Accessed 27 Dec 2020.
- 36.Deutsche Krankenhausgesellschaft. DKG zum Gesetz zur Finanzierung der Krankenhäuser im Ausnahmezustand. March 21, 2020. https://www.dkgev.de/dkg/presse/details/das-ist-kein-schutzschirm-das-ist-ein-fataler-politischer-fehler-des-ministers/. Accessed 27 Dec 2020.
- 37.ZEIT. Krankenhaeuser: Leere Betten, leere Kassen. April 15, 2020. https://www.zeit.de/2020/17/krankenhaeuser-coronavirus-deutschland-kliniken-finanzkrise. Accessed 27 Dec 2020.
- 38.PricewaterhouseCoopers. Kapitalmarktdaten Gesundheitswesen & Pharma. https://pwc-tools.de/kapitalkosten/kapitalmarktdaten-gesundheitswesen-pharma/. Accessed 27 Dec 2020.
- 39.GKV-Spitzenverband. Bundesbasisfallwert (BBFW). https://www.gkv-spitzenverband.de/krankenversicherung/krankenhaeuser/budgetverhandlungen/bundesbasisfallwert/bundesbasisfallwert.jsp. Accessed 27 Dec 2020.
- 40.Institut für das Entgeltsystem im Krankenhaus (InEK). Fallpauschalen-Katalog 2020. Siegburg: InEK; 2020.
- 41.Bundesministerium für Gesundheit. Zuzahlungsregelungen der gesetzlichen Krankenversicherung. Informationsblatt Nr. 223-06. Februar 13, 2018. https://www.bundesgesundheitsministerium.de/fileadmin/Dateien/3_Downloads/A/Arzneimittelversorgung/Zuzahlungsregelungen_GKV.pdf. Accessed 27 Dec 2020.
- 42.Ärzteblatt. Coronakrise: Länder unterstützen Krankenhäuser unterschiedlich. August 14, 2020. https://www.aerzteblatt.de/nachrichten/115516/Coronakrise-Laender-unterstuetzen-Krankenhaeuser-unterschiedlich. Accessed 27 Dec 2020.
- 43.Brandstetter S, Dodoo-Schittko F, Brandl M, Blecha S, Bein T, Apfelbacher C, DACAPO Study Group Ambulatory and stationary healthcare use in survivors of ARDS during the first year after discharge from ICU: findings from the DACAPO cohort. Ann Intensive Care. 2019;9(1):70. doi: 10.1186/s13613-019-0544-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Abers MS, Musher DM. Clinical prediction rules in community-acquired pneumonia: lies, damn lies and statistics. QJM. 2014;107(7):595–596. doi: 10.1093/qjmed/hcu096. [DOI] [PubMed] [Google Scholar]
- 45.Ramsey FP. A mathematical theory of saving. Econ J. 1928;38(152):543–559. doi: 10.2307/2224098. [DOI] [Google Scholar]
- 46.John J, Koerber F, Schad M. Differential discounting in the economic evaluation of healthcare programs. Cost Eff Resour Alloc. 2019;17(17):29. doi: 10.1186/s12962-019-0196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Statistisches Bundesamt. Gesundheitsausgaben im Jahr 2018 um 4 % gestiegen. Pressemitteilung Nr. 164 vom 12. Mai 2020. Wiesbaden: Statistisches Bundesamt; 2020.
- 48.Statistisches Bundesamt. Bruttoinlandsprodukt im 1. Quartal 2020 um 2,2 % niedriger als im Vorquartal. Pressemitteilung Nr. 169 vom 15. Mai 2020. Wiesbaden: Statistisches Bundesamt; 2020.
- 49.Cirillo P, Taleb NN. Tail risk of contagious diseases. Nat Phys. 2020;16:606–613. doi: 10.1038/s41567-020-0921-x. [DOI] [Google Scholar]
- 50.Government of Alberta. COVID-19 Modelling. April 8, 2020. https://www.alberta.ca/assets/documents/covid-19-case-modelling-projection.pdf. Accessed 27 Dec 2020.
- 51.Singhal S, Reddy P, Dash P, Weber K. From “wartime” to “peacetime”: Five stages for healthcare institutions in the battle against COVID-19. April 2020. https://healthcare.mckinsey.com/wartime-peacetime-five-stages-healthcare-institutions-battle-against-covid-19. Accessed 27 Dec 2020.
- 52.Deutsche Gesellschaft für Internistische Intensivmedizin und Notfallmedizin Intensivmedizinische Versorgung in den kommenden Jahren erheblich gefährdet. Med Klin Intensivmed Notfmed. 2019;114:276–279. doi: 10.1007/s00063-019-0574-7. [DOI] [Google Scholar]
- 53.Bundesministerium für Gesundheit. Bundestag beschließt Pflegepersonal-Stärkungsgesetz. November 9, 2018. https://www.bundesgesundheitsministerium.de/presse/pressemitteilungen/2018/4-quartal/ppsg-pflegepersonal-staerkungsgesetz.html. Accessed 27 Dec 2020.
- 54.CNBC. Regulations slow urgent hiring of doctors and nurses amid coronavirus outbreak, staffing firms say. March 28, 2020. https://www.cnbc.com/2020/03/28/coronavirus-regulations-slow-hiring-of-doctors-and-nurses-staffing-firms-say.html#close. Accessed 27 Dec 2020.
- 55.Deutsche Gesellschaft für Anästhesiologie und Intensivmedizin. Empfehlungen der DGAI zu Schulungen von medizinischen Helfenden bei Einsatz während der COVID-19-Pandemie. https://www.dgai.de/aktuelles/coronavirus-covid-19/informationen-der-verbaende-2.html. Accessed 27 Dec 2020.
- 56.Recovery Collaborative Group. Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with Covid-19—preliminary report [published online ahead of print, 2020 Jul 17] N Engl J Med. 2020 doi: 10.1056/NEJMoa2021436. [DOI] [Google Scholar]
- 57.Garrison LP, Jr, Kamal-Bahl S, Towse A. Toward a broader concept of value: identifying and defining elements for an expanded cost-effectiveness analysis. Value Health. 2017;20(2):213–216. doi: 10.1016/j.jval.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 58.Welt. „Mit künstlicher Beatmung wird richtig viel Geld gemacht“. April 20, 2020. https://www.welt.de/politik/deutschland/article207311157/Corona-Mit-kuenstlicher-Beatmung-wird-richtig-viel-Geld-gemacht.html. Accessed 27 Dec 2020.
- 59.Ubel PA, Richardson J, Prades JL. Life-saving treatments and disabilities. Are all QALYs created equal? Int J Technol Assess Health Care. 1999;15(4):738–748. doi: 10.1017/S0266462399154138. [DOI] [PubMed] [Google Scholar]
- 60.Stalmeier PF, Chapman GB, de Boer AG, van Lanschot JJ. A fallacy of the multiplicative QALY model for low-quality weights in students and patients judging hypothetical health states. Int J Technol Assess Health Care. 2001;17(4):488–496. doi: 10.1017/S026646230110704X. [DOI] [PubMed] [Google Scholar]
- 61.Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen. General methods: version 5.0. Cologne, Germany; 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.