Abstract
Background
Countries have restricted international arrivals to delay the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). These measures carry a high economic and social cost, and might have little effect on COVID-19 epidemics if there are many more cases resulting from local transmission compared with imported cases. Our study aims to investigate the extent to which imported cases contribute to local transmission under different epidemic conditions.
Methods
To inform decisions about international travel restrictions, we calculated the ratio of expected COVID-19 cases from international travel (assuming no travel restrictions) to expected cases arising from internal spread, expressed as a proportion, on an average day in May and September, 2020, in each country. COVID-19 prevalence and incidence were estimated using a modelling framework that adjusts reported cases for under-ascertainment and asymptomatic infections. We considered different travel scenarios for May and September, 2020: an upper bound with estimated travel volumes at the same levels as May and September, 2019, and a lower bound with estimated travel volumes adjusted downwards according to expected reductions in May and September, 2020. Results were interpreted in the context of local epidemic growth rates.
Findings
In May, 2020, imported cases are likely to have accounted for a high proportion of total incidence in many countries, contributing more than 10% of total incidence in 102 (95% credible interval 63–129) of 136 countries when assuming no reduction in travel volumes (ie, with 2019 travel volumes) and in 74 countries (33–114) when assuming estimated 2020 travel volumes. Imported cases in September, 2020, would have accounted for no more than 10% of total incidence in 106 (50–140) of 162 countries and less than 1% in 21 countries (4–71) when assuming no reductions in travel volumes. With estimated 2020 travel volumes, imported cases in September, 2020, accounted for no more than 10% of total incidence in 125 countries (65–162) and less than 1% in 44 countries (8–97). Of these 44 countries, 22 (2–61) had epidemic growth rates far from the tipping point of exponential growth, making them the least likely to benefit from travel restrictions.
Interpretation
Countries can expect travellers infected with SARS-CoV-2 to arrive in the absence of travel restrictions. Although such restrictions probably contribute to epidemic control in many countries, in others, imported cases are likely to contribute little to local COVID-19 epidemics. Stringent travel restrictions might have little impact on epidemic dynamics except in countries with low COVID-19 incidence and large numbers of arrivals from other countries, or where epidemics are close to tipping points for exponential growth. Countries should consider local COVID-19 incidence, local epidemic growth, and travel volumes before implementing such restrictions.
Funding
Wellcome Trust, UK Foreign, Commonwealth & Development Office, European Commission, National Institute for Health Research, Medical Research Council, and Bill & Melinda Gates Foundation.
Introduction
COVID-19 is an illness caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which was first detected in Wuhan, China, in late 2019. Since then, it has been spread by travellers to almost every country in the world, and was declared a pandemic by WHO on March 22, 2020.1 In the absence of effective pharmaceutical measures for prevention and treatment, governments have imposed a range of response measures to delay the spread of SARS-CoV-2, and hence enable health systems to cope with the expected sharp rise in health-care demand.
One such intervention that has been widely used is international travel restrictions. Early travel restrictions focused on countries with early outbreaks (such as China, Iran, and Italy), but as SARS-CoV-2 spread to more countries, the number of origin countries on travel restriction lists has grown. The World Tourism Organization reports that every country in the world had imposed some form of COVID-19-related travel restriction by April 20, 2020, marking the most extensive travel restrictions in history.2 However, the restrictions implemented differ from country to country and include border closures, flight suspensions, and quarantine and self-isolation for travellers. Measures can also be applied indiscriminately or targeted at specific places of origin.
Research in context.
Evidence before this study
Countries are at different stages of COVID-19 epidemics, and many have implemented policies to minimise the risk of importing cases via international travel. Such policies include border closures, flight suspensions, and quarantine and self-isolation on international arrivals. Searching PubMed and medRxiv using the search term (“covid” OR “coronavirus” OR “SARS-CoV-2”) AND (“travel” OR “restrictions” OR “flight” OR “flights” OR “border”) for articles published in any language from Jan 1 to July 10, 2020, returned 118 and 84 studies, respectively, of which 39 were relevant to our study. These studies either concentrated in detail on the risk of importation to specific countries or used a single epidemiological or travel dataset to estimate risk. Most of them focused on the risk of COVID-19 introduction from China or other countries that had cases early in 2020. No study combined country-specific travel data, prevalence estimates, and incidence estimates to assess the global risk of importation relative to current local transmission within countries.
Added value of this study
Our study considers the risk of case importation across 162 countries, in the context of local epidemic growth rates. Producing estimates on a global scale allows the complex relationship between the prevalence of COVID-19, traveller volume, and incidence locally to be combined, producing a simple, digestible metric. This allows decision makers to determine where travel restriction policies make large contributions to slowing local transmission, and where they have very little overall effect.
Implications of all the available evidence
In many countries, imported cases would make a relatively small contribution to local transmission, so travel restrictions would have very little effect on epidemics. Countries where travel restrictions would have a large effect on local transmission are those with strong travel links to countries with high COVID-19 prevalence or countries that have successfully managed to control their local outbreaks.
International travel restrictions carry a high economic and social cost. Much of global tourism, trade, business, education, and labour mobility relies on cross-border movement of people. The UN Conference on Trade and Development estimates that the world's tourism sector will lose value worth 1·6–2·8% of global gross domestic product as a result of COVID-19.3 This excludes the value of lost non-tourism travel, which is difficult to estimate. Additionally, the Organisation for Economic Co-operation and Development (OECD) estimates that complete travel restrictions could increase service trade costs by 12%.4 The social cost comes in the form of lost opportunities for family and friend reunion, international education, and career development. According to the 2005 International Health Regulations, travel restrictions “shall not be more restrictive of international traffic and not more invasive or intrusive to persons than reasonably available alternatives that would achieve the appropriate level of health protection”.5 Hence, there are strong economic, humanitarian, and legal reasons to impose international travel restrictions only when the benefits outweigh the costs.
Some studies have looked at the impact of international travel restrictions on the spread of COVID-19 globally. Most of these studies focused on the initial phase of the COVID-19 spread, when the epidemic was mainly concentrated in Wuhan, China;6, 7, 8, 9 these studies modelled the effect of flight restrictions from Wuhan or mainland China more generally. Chinazzi and colleagues6 also used a dynamic metapopulation model to estimate the extent to which the restrictions might have delayed or prevented epidemics in target countries. All of these studies found that travel restrictions in the early part of the epidemic helped to delay the spread of COVID-19 but could not completely prevent it due to cases having left China before the onset of these restrictions. However, these studies do not address the current issue of whether travel restrictions are still justified at a time when there are outbreaks in most countries. A further study10 looked at retrospective travel data up to late April, 2020, to examine the main international pathways that led to spread across the world. It concluded that travel bans from hotspots (such as China) were insufficient to control global spread completely, since epidemics had spread to many other countries by the time travel restrictions were imposed.
Travel restrictions have clear benefits when there are zero or few cases in the destination country. For instance, restrictions on travellers from Wuhan, or China more generally, in early 2020 might have contributed to slowing the global spread of SARS-CoV-2.6, 9 However, once case numbers within a country are sufficiently large that local outbreaks have been established and are self-sustaining, travel restrictions become less effective. For instance, the ban on European travellers to the USA on March 12, 2020, was too late to prevent a large epidemic in New York already seeded mainly by European travellers.11 Countries with established epidemics attempting to reduce COVID-19 incidence through stringent physical distancing measures such as lockdowns might impose travel restrictions to accelerate the reduction of new cases. However, this would only be effective if the number of cases being imported from international travellers contributes substantially to overall incidence. Hence, decisions around travel restrictions are complex; they need to take into account local transmission, COVID-19 prevalence in source countries of travellers, and the volume of travel from those countries.
As of November, 2020, almost all countries have reported COVID-19 cases, but they differ in the stage of the pandemic they are in. Many countries in east Asia and Australasia are well past peak incidence, with some having reduced incidence to very low levels.12 Conversely in other countries, incidence remains high, with some countries experiencing second waves of cases and a handful experiencing a third. Therefore, recommendations about international travel restrictions cannot be applied uniformly, but instead need to take into account country circumstances.
In this Article, we provide information about the potential benefit of international travel restrictions when countries are experiencing different epidemic conditions, by comparing the number of cases resulting from international travel to those resulting from local transmission in 162 countries. In the absence of effective vaccines and antiviral drugs for prevention and treatment, governments have imposed a range of non-pharmaceutical measures to reduce transmission of SARS-CoV-2 to a level that does not overburden the capacity of health systems.
Methods
Case under-ascertainment, incidence, and prevalence estimates
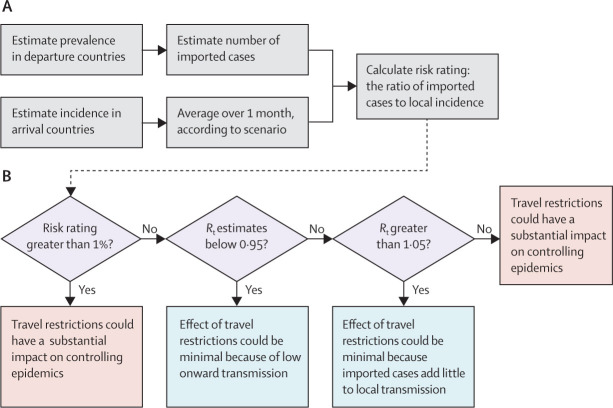
Our analysis combines estimates of SARS-CoV-2 prevalence and incidence for countries in May and September, 2020, with detailed flight data, to produce risk ratings for each country (ie, the ratio of imported cases to total incidence, expressed as a proportion). Total incidence was inferred from deaths occurring in a country, so would include cases arising from local transmission as well as imported cases, since they would also presumably contribute to COVID-19 deaths in that country. We chose September as it was the month with the most up-to-date data available at the time of our analysis, and compared this scenario with May, when countries with large internal epidemics were also experiencing high volumes of outgoing travellers, thus representing a potential worst-case scenario of transmission related to travel. Our methodological framework is outlined in figure 1 .
Figure 1.
Our methodology: the modelling procedure and our policy recommendations
A descriptive schematic of the modelling process used to arrive at the overall risk ratios is shown (A), with a flow-chart outlining the necessary conditions that determine our policy recommendations (B). Rt=reproduction number.
Prevalence and incidence estimates were derived by use of statistical modelling methods described elsewhere13 and summarised here. First, the level of case ascertainment in each country was estimated as the ratio of a delay-adjusted country-specific case–fatality ratio to an assumed baseline case–fatality ratio (derived from published estimates).14 Then, temporal variation in under-ascertainment was inferred using a Gaussian process: a non-parametric Bayesian framework, suited for statistically robust estimates of time-dependent functions. Finally, these temporal under-ascertainment estimates were used to adjust the confirmed case time series.12 The adjusted case data represent the estimated true number of symptomatic individuals in each country, which is typically substantially larger than the confirmed case number.13, 15
To estimate incidence of destination countries, we first inferred a time-varying ascertainment rate for each country, following the methods of Russell and colleagues.13 We then adjusted the confirmed case numbers from the European Centre for Disease Prevention and Control12 with our ascertainment estimates, with the use of an estimated delay distribution from confirmation to death.16 Once the case numbers had been adjusted for temporally varying under-ascertainment, we took the mean case incidence over the month in question for the corresponding scenario (May, 2020, for scenarios A and B, and September, 2020, for scenarios C and D).
Prevalence of source countries (ie, countries where travellers are departing from) on each day was estimated as the sum of the new cases over the 10 most recent days (ie, assuming an infectious period of 10 days).16, 17, 18, 19 This was then converted to a proportion by dividing by the country's population. We restricted our analysis to countries that had reported at least ten confirmed COVID-19 deaths in total at least 10 days earlier, to estimate prevalence and incidence using the methods from Russell and colleagues;13 the estimated 95% credible intervals (CrIs) would be too wide to be informative otherwise. Details of the inference framework employed, computation of the incidence and prevalence estimates, and the limitations of our methods are shown in the appendix (pp 2–5).
As a final step, we adjusted both the prevalence and incidence estimates for the number of infections that are asymptomatic. We did so by assuming a wide plausible range of all infections (10–70%), reflecting the still-present uncertainty surrounding such estimates, with a median estimate of 50%. However, it is important to note that both the prevalence and incidence estimates are adjusted in precisely the same fashion and therefore the resulting risk ratings are unchanged when the proportion of asymptomatic infections is varied. This implies the conclusions of our analysis are robust to changes in the estimates of the proportion of asymptomatic infections.
Our under-ascertainment estimates, described in a previous study,13 form the basis of our incidence and prevalence estimates. They are calculated in a Bayesian modelling framework, and as such, we report a median (95% CrI) over time for each country. This 95% CrI includes the uncertainty in the hospitalisation-to-death distribution. The incidence 95% CrIs include the 95% CrI from the under-ascertainment estimates and the assumed wide range of asymptomatic infections. However, uncertainty in the other distributions used (table ) is captured only in the prevalence estimates, as they require two additional calculation steps compared with the incidence estimates (appendix pp 3–4). Scenarios A and B used incidence and prevalence estimates from May, 2020, and scenarios C and D used incidence and prevalence estimates from September, 2020. We combined the sources of parameter uncertainty in country prevalence and incidence estimates in a Bayesian inference framework. The model's cumulative incidence estimates were validated against seroprevalence estimates in the original publication13 that develops the model employed here.
Table.
Summary of the time delay distributions used in our model and their sources
| Description | Value | Source | |
|---|---|---|---|
| Incubation period | Time from exposure to onset of symptoms | Gamma (μ=5·5, σ2=6·5) distribution; median 5·1 days (95% CI 4·5–5·8), with 97·5% of symptomatic cases developing symptoms within 11·5 days | Lauer et al (2020)18 |
| Time to infectiousness, for symptomatic cases* | Time after exposure (and before symptom onset) from which pre-symptomatic transmission can occur | Median: 3·4 days (IQR 2·3–4·9; 95% CI 0·9–8·6) | Derived from He et al (2020)17 |
| Infectious period, for symptomatic cases* | Time after incubation period during which case is able to infect others | Median 7·1 days (IQR 5·7– 8·5; 95% CI 2·5–11·6) | Derived from Wölfel et al (2020)19 |
| Hospitalisation to death | Time between being admitted to hospital and dying for severe cases | Median 13·0 days (95% CI 8·7–20·9) | Linton et al (2020)16 |
95% CIs are calculated using bootstrapping.
Time to infectiousness and infectious period are summed to arrive at prevalence estimates.
A mathematical model is required to estimate both prevalence and incidence, as the available case data do not necessarily reflect the true number of infections in many places.13, 20 Furthermore, serological estimates are not available for enough countries for them to be used for a global analysis such as this.21
International travellers
International travel has decreased greatly since the COVID-19 pandemic began2 because of travel restrictions, but also owing to individual self-exclusion due to fear of infection and reduced business and tourism opportunities. Hence, we considered four scenarios for international travel in the hypothetical case of there being no travel restrictions: one each for the months May and September, both in 2019 and in 2020. Travel restrictions are defined for the purposes of this study as any measure that completely or almost completely prevents international arrivals from contributing to local transmission, such as entry bans and compulsory 14-day facility-based quarantines. Two scenarios (A and C) are upper-bound scenarios to illustrate the situation in which traveller volumes returned to levels seen in 2019 in the absence of travel restrictions; whereas the two remaining scenarios (B and D) are lower-bound scenarios using projected traveller volumes in 2020, which might underestimate the level of international travel in the absence of travel restrictions. Scenarios A and B used travel data from May, 2020, and scenarios C and D used travel data from September, 2020.
For scenario A, the number of travellers between each country was estimated using the number of passengers booked on flights with data from the Official Aviation Guide in May, 2019. For scenario B, we used the OpenSky database,22 which provides data on the number of flights each day between pairs of countries. We adjusted the number of international travellers between countries downwards using the ratio of the number of flights in the OpenSky database in May, 2019, and May, 2020. This gave a mean reduction of 63% (range 0–99) across countries. For scenario C, the number of travellers between each country was estimated using the number of passengers booked on flights with data from the Official Aviation Guide in September, 2019. For scenario D, we adjusted the number of international travellers between countries downwards using the ratio of the number of flights in the OpenSky database in September, 2019, and September, 2020. This gave a mean reduction of 48% (range 0·5–100) across countries. For scenarios B and D, where data were not available, we applied the mean reduction across pairs of countries with data.
We found large reductions in travel volumes across countries regardless of their level of travel restrictions in both May and September, 2020 (appendix pp 7–8), meaning scenarios B and D might be closest to the plausible range for travel volumes during the pandemic without travel restrictions.
Imported cases
The number of cases imported from a source country to a destination country on a particular date was estimated as the product of the prevalence on that date in the source country multiplied by the number of travellers from that country to the destination country on a single day in May, 2019 or 2020 (scenarios A and B, respectively) or September, 2019 or 2020 (scenarios C and D, respectively), where the 2020 estimates were downscaled using OpenSky data. The total number of imported cases on that date was then estimated by summing the cases imported from all countries that had travellers to the destination country. We then calculated the ratio of the mean number of imported cases to mean total incidence, with both means averaged over the month in question.
For countries where imported cases were predicted to account for more than 1% of total incidence, we estimated the proportion of incoming travellers that needed to be averted to bring this proportion below 1%. We focused on the 1% threshold as it is a simple threshold at which the reduction to overall incidence due to travel restrictions would be arguably undetectable. We illustrate this by applying three thresholds (0·1%, 1%, and 10%) to the incidence over the course of an epidemic parameterised to match the key characteristics of COVID-19. Relaxing travel restrictions in countries where imported cases acount for 10% of local transmission leads to a minimal change in the resulting epidemic, and if imported cases account for less than 1% of local transmission, changes to incidence are virtually undetectable (pp 23–24). We assumed that incoming travellers would be averted in order of COVID-19 prevalence in their countries of origin (ie, averting travellers from the country with the highest prevalence first).
Reproduction number estimates
Even a small change in infected cases can be consequential if a local epidemic is at the tipping point between slow exponential growth and decline. Hence, travel restrictions are more effective if they can prevent a country's local epidemic from transitioning from slow exponential decline to slow exponential growth, or if they can revert such a growth to a decline. To examine this, we used publicly available country-specific reproduction number (R t) estimates from EpiForecasts23 (the full list of R t estimates can be found in the appendix [pp 10–16]). We then enumerate the countries that are close to the tipping point of their local epidemic (R t between 0·95 and 1·05), even though they might have risk ratings below 1% (figure 1).
Sensitivity analyses
We did sensitivity analyses to examine whether our results would be affected by different rates of mortality under-ascertainment and using data from different timepoints of the pandemic. As the completeness of COVID-19 death reporting has been questioned in low-income and middle-income settings, we examined the possibility that COVID-19 deaths might be under-reported by 50% or 80% in low-income and middle-income countries, as classified by the OECD, in scenario D, which has the most similar travel volumes to current levels.24 We also tested whether the conclusions of our analysis change at different timepoints of the pandemic by using prevalence and incidence estimates from July, 2020. Finally, we did a sensitivity analysis on flight volumes, as it has been estimated by the International Air Transport Association that aircraft occupancy has decreased by 50·6% in 2020 compared with 2019.25 For simplicity, we assumed reductions of 50% and 80%. All analyses were done in R (version 4.0.2).
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
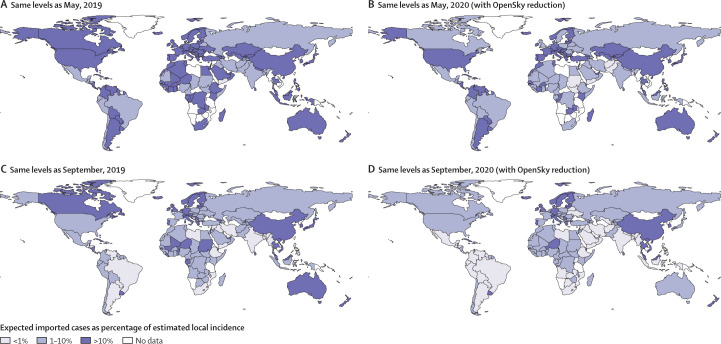
136 countries were included for the May scenarios (A and B) and 162 for the September scenarios (C and D), as fewer countries in May, 2020, had reported at least ten COVID-19 deaths. Figure 2 shows the risk rating for each country, based on the ratio of imported cases to total incidence, for different scenarios about passenger reductions in both May, 2020, and September, 2020. For May, 2020, in the worst-case scenario of no change in travel patterns compared with May, 2019, travel restrictions are likely to have made a large difference to COVID-19 epidemics in most countries, with imported cases exceeding 10% of total incidence in 102 (95% CrI 63–129) of 136 countries. Even so, this means imported cases would have contributed to no more than 10% of total incidence in 34 countries (7–73) and to less than 1% of total incidence in four countries (4–16; figure 2A). If we assume that travel volumes were reduced by the proportions seen in OpenSky data for May, 2020, compared with May, 2019, imported cases would have contributed to more than 10% of total incidence in 74 countries (33–114) and no more than than 10% of total incidence in 62 countries (22–103), and to less than 1% in eight countries (4–39; figure 2B).
Figure 2.
Risk rating by country, in the absence of international travel restrictions, in each of the four scenarios about international travellers in May and September, 2020
(A) Travel assumed to be at the same levels as in May, 2019. (B) Travel estimated to be at the same levels as in May, 2020, by downscaling the May, 2019, levels by flight path-specific reduction factors calculated by using the ratio of the OpenSky datasets for May, 2019, and May, 2020. (C) Travel assumed to be at the same levels as in September, 2019. (D) Travel estimated to be at the same levels as in September, 2020, by downscaling the September, 2019, levels by flight path-specific reduction factors calculated using the ratio of the OpenSky datasets for September, 2019, and September, 2020. See appendix for the full list of results (p 22) and for the lower and upper 95% credible intervals of our results (pp 17–18).
By September, 2020, travel restrictions are likely to have had a smaller impact on local epidemics compared with May, 2020. Assuming no change in travel patterns compared with September, 2019, we find that imported cases would have accounted for more than 10% of total incidence in 56 (95% CrI 22–112) of 162 countries and no more than 10% of total incidence in 106 countries (50–140), and to less than 1% in 21 countries (4–71; figure 2C). With reductions in travel volumes, imported cases accounted for more than 10% of total incidence in 37 countries (8–85) and no more than 10% of total incidence in 125 countries (65–162), and to less than 1% in 44 countries (8–97; figure 2D).
Of the 44 countries with risk ratings below 1% in September, 2020, 22 countries (6–61) had risk ratings below 1% but R t estimates not close to their tipping point (ie, <0·95 or >1·05) in scenario D; when assuming September, 2019, travel volumes, the number was reduced to 13 countries (4–40). Equivalent numbers for other scenarios are presented in the appendix (p 22). These are the countries in which we are the most confident that lifting travel restrictions would have been very unlikely to cause outbreaks.
Individual country results are shown in the appendix (pp 9–16), alongside 95% lower and upper CrIs for each flight scenario (appendix pp 17–18). Assuming high rates of mortality under-ascertainment in the 143 low-income and middle-income countries included in our analysis does not change this picture substantially, since most of these countries do not contribute greatly to international travel volumes (appendix p 20). The conclusions are also largely unchanged when prevalence estimates from July, 2020, are used instead of May or September, 2020 (appendix p 21).
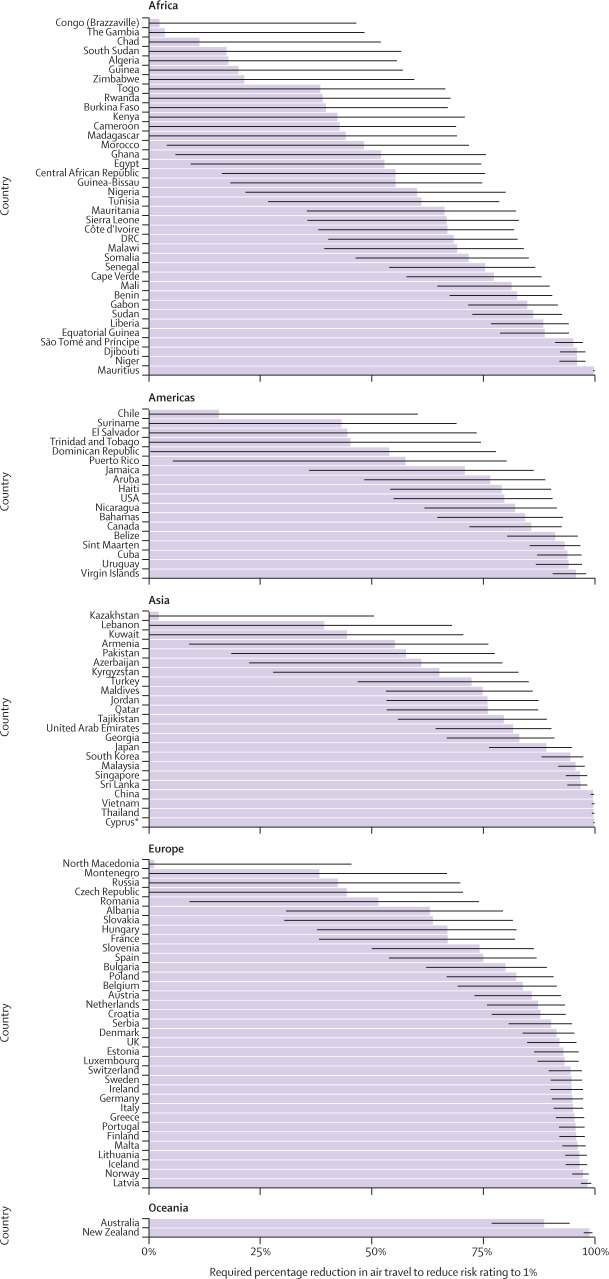
Figure 3 shows the proportion by which international arrivals need to be averted to bring imported cases to less than 1% of total incidence in countries where it is at least 1% in scenario D. At this level, imported cases will make an almost undetectable contribution to epidemic size (appendix pp 23–24). Most of these countries would need to avert the majority of their international arrivals, although there are a few that might be able to bring imported cases to below 1% of total incidence by averting less than a quarter of arrivals. The relationship between imported cases and local outbreak size is shown in the appendix (p 9). Most countries cluster, given that high expected numbers of imported cases increase the probability of the seeding of outbreaks. However, several countries are outliers from the cluster, as they either have large outbreaks (the USA) or very small outbreaks with high numbers of expected imported cases (China).
Figure 3.
Percentage reduction in passenger numbers required for countries to bring proportion of total incidence due to imported cases to less than 1%
Figure shows 118 countries in scenario D where imported cases account for at least 1% of total incidence. Error bars represent the lower and upper 95% credible intervals of our expected number of imported cases estimates. Countries are grouped by UN region. *Geographically part of Asia.
Discussion
Using estimated COVID-19 prevalence in 162 countries together with international travel data between countries, we categorised countries according to the extent to which imported cases might contribute to local transmission under different epidemic conditions, in the absence of travel restrictions. In May, 2020, imported cases would have contributed to more than 10% of total incidence in the majority of countries without travel restrictions, and hence such restrictions appear to have been justified. However, by September, 2020, even without travel restrictions, imported cases would have exceeded 10% of total incidence in 56 countries when using September, 2019, travel volumes and in only 37 countries when using estimated travel volumes in September, 2020. Additionally, we found that some countries (13 when using 2019 travel volumes and 22 when using estimated 2020 travel volumes) fell into the most stringent category of having imported cases contribute less than 1% of total incidence and R t either lower than 0·95 or higher than 1·05 in September, 2020. These are countries in which we are most confident that travel restrictions in September would have had little epidemiological benefit, as the countries either had low onwards transmission that was not approaching exponential growth or imported cases will have been contributing little to existing high rates of local transmission.
Furthermore, in most of the countries where the proportion of imported cases is greater than 1%, it can be brought to less than 1% with selective restrictions imposed only on travellers from the highest-prevalence countries. However, a few countries would have to prevent entry by almost all international travellers to reach this threshold. These are generally countries where control of local epidemics has been achieved. For instance, in September, 2020, both New Zealand and China had low enough total incidence that the expected number of imported cases (six and 55, respectively) was close to the total incidence (ten and 45, respectively), meaning that imported cases could pose a real risk of triggering a second local epidemic wave (appendix pp 9–16).
Some countries with fairly large local epidemics in May, 2020—eg, Brazil and Mexico—still have a moderate level of risk associated with imported cases under the worst-case traveller volume scenario (scenario A), because of their strong connectedness to other high-prevalence countries. Imported cases in these countries might be insufficient to drive local epidemics on their own, but could become important in driving epidemics that have already started if countries succeed in reducing local reproduction numbers close to 1, the level at which each new generation of infected cases is smaller than the last.
One example illustrating where more effective travel restrictions could have prevented outbreaks is the second wave of infections in Victoria, Australia. The wave began in June, when travellers under hotel quarantine infected hotel staff due to shortcomings in infection control procedures.26 We used our model to retroactively estimate the risk rating for Australia at that time, in an attempt to validate our model as a tool for policy makers. We estimated that the risk rating in June (mean daily contribution of imported cases to total incidence) was 264% (95% CrI 230–294), based on estimated mean daily number of imported cases of 111 (95% CrI 50–235) and mean daily total incidence of 42·1 cases (21·8–80·4). We can therefore conclude that our modelling framework provides evidence for the value of effective travel restrictions at that time.
Our estimates involve simplifying assumptions. We assume that international arrivals in a country have the same probability of being infected as any other person selected at random from the source country. In practice, the risk of infected arrivals is likely to be lower because symptomatic cases are less likely to travel as they might be recuperating at home or in hospital. For those who do attempt to travel, they might be detected during exit screening in the source country or entry screening in the destination country. For those in their incubation period at the time of travel, they might develop symptoms during the course of their journey and be detected or self-declare illness upon arrival. We also did not consider the effect of outbound travellers on local transmission. Travel restrictions would also prevent infected travellers from leaving their source country, which would reduce the number of cases locally and hence mitigate the impact of infected inbound travellers. All these limitations result in overestimating the number of COVID-19 importations that would occur without travel restrictions. However, a limitation in the opposite direction is that we assume that all international travel occurs through flights, so our analysis might not accurately capture the risk of importation between countries that normally have a high volume of land traffic (such as rail and road travel between countries in continental Europe). Also, OpenSky flight data do not inform about a traveller's final destination if a stopover flight is taken,22 so our travel volume estimates in scenarios B and D might be imprecise.
Our prevalence and incidence estimates are approximate and might overestimate incidence in countries with younger overall population structures and underestimate it in countries with older populations.13 Furthermore, countries with very low case numbers are excluded from our analysis, as it is not possible to accurately estimate incidence and prevalence estimates for such countries. Similarly, estimates of time-varying reproduction numbers are approximate; the limitations of the EpiForecast estimates have been previously documented.23
Lastly, there are several sources of uncertainty in our analysis (appendix pp 3–4). However, the risk categorisation of countries remained broadly stable over sensitivity analyses around both country prevalence and incidence estimates (appendix pp 17–18, 21), international travel patterns (appendix pp 27–28), and assumed levels of under-ascertainment of COVID-19 deaths (appendix p 20). Only very extreme scenarios (such as prevalence at the upper 95% CrI or travel volumes unchanged from 2019) substantially increased the number of countries where imported cases might contribute to more than 10% of local cases. Even in these unlikely scenarios, there are many countries where travel appears to make little difference to local COVID-19 epidemiology. Our study considered only international travel restrictions. However, the same methodology could be applied to examine the impact of internal travel restrictions (such as between states in the USA).
These results indicate that strict untargeted travel restrictions are probably unjustified in many countries, other than those that have both good international travel connections and very low local COVID-19 incidence. Governments needing to make detailed decisions about travel restrictions or quarantine white lists can use the methods presented here combined with the most current and accurate local data available.
Data sharing
Acknowledgments
Acknowledgments
MJ was partly funded by the Bill & Melinda Gates Foundation (INV-003174) and by the National Institute for Health Research (NIHR) using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the UK Department of Health and Social Care. MJ and WJE have received funding from the European Union's Horizon 2020 research and innovation programme—project EpiPose (101003688). This project was funded by the Wellcome Trust (AJK: 206250/Z/17/Z; SC: 208812/Z/17/Z). We acknowledge the OpenSky website and database for their publicly available, detailed data on total numbers of flights between airports, which were used to inform our analysis.
Editorial note: the Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations
Contributors
MJ and TWR conceived the study. TWR, JTW, and MJ compiled, analysed and verified the data. TWR, AJK, and WJE estimated country COVID-19 prevalence and incidence. TWR, SC, and MJ designed the model and conducted the analyses. All authors had access to all the data in the study, contributed to manuscript writing, and approved the final version.
Declaration of interests
We declare no competing interests.
The confirmed COVID-19 data used in this analysis are publicly available case and death time series data, available from the European Centre for Disease Control. The flight reduction scaling factors are calculated using publicly available data from the OpenSky database. We encourage analysts to use our code to re-run calculations with updated data that might be available locally. The code used for the analysis in this paper is available on a GitHub repository, as is the script used for the literature review can also be found at the first GitHub repository. The repository includes functions for users to input their own data, as well as instructions for using the premade script to run the analysis with a different dataset. The code used to produce under-reporting estimates, which form the basis for the country-specific prevalence and incidence estimates, is also available online.
Supplementary Material
References
- 1.WHO WHO Director-General's opening remarks at the media briefing on COVID-19. March 11, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020
- 2.World Tourism Organization COVID-19 related travel restrictions. a global review for tourism. Second report. April 28, 2020. https://www.unwto.org/covid-19-travel-restrictions
- 3.UN Conference on Trade and Development (UNCTAD) Covid-19 and tourism: assessing the economic consequences. July 1, 2020. https://unctad.org/en/PublicationsLibrary/ditcinf2020d3_en.pdf
- 4.Benz S, Gonzales F, Mourougane A. Organisation for Economic Co-operation and Development; Paris: 2020. The impact of COVID-19 international travel restrictions on services-trade costs. OECD Trade Policy Papers. [Google Scholar]
- 5.Habibi R, Burci GL, de Campos TC. Do not violate the International Health Regulations during the COVID-19 outbreak. Lancet. 2020;395:664–666. doi: 10.1016/S0140-6736(20)30373-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chinazzi M, Davis JT, Ajelli M. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368:395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hossain MP, Junus A, Zhu X. The effects of border control and quarantine measures on the spread of COVID-19. Epidemics. 2020;32 doi: 10.1016/j.epidem.2020.100397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pullano G, Pinotti F, Valdano E, Boëlle P-Y, Poletto C, Colizza V. Novel coronavirus (2019-nCoV) early-stage importation risk to Europe, January 2020. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.4.2000057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wells CR, Sah P, Moghadas SM. Impact of international travel and border control measures on the global spread of the novel 2019 coronavirus outbreak. Proc Natl Acad Sci USA. 2020;117:7504–7509. doi: 10.1073/pnas.2002616117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang C, Qian L-X, Hu J-Q. COVID-19 pandemic with human mobility across countries. J Oper Res Soc China. 2020 doi: 10.1007/s40305-020-00317-6. published online Aug 3. [DOI] [Google Scholar]
- 11.Gonzalez-Reiche AS, Hernandez MM, Sullivan MJ. Introductions and early spread of SARS-CoV-2 in the New York City area. Science. 2020;369:297–301. doi: 10.1126/science.abc1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.European Centre for Disease Prevention and Control Daily update of new reported cases of COVID-19 by country worldwide. Oct 26, 2020. https://www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide
- 13.Russell TW, Golding N, Hellewell J. Reconstructing the early global dynamics of under-ascertained COVID-19 cases and infections. BMC Med. 2020;18:332. doi: 10.1186/s12916-020-01790-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verity R, Okell LC, Dorigatti I. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020;20:669–677. doi: 10.1016/S1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li R, Pei S, Chen B. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science. 2020;368:489–493. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linton NM, Kobayashi T, Yang Y. Incubation period and other epidemiological characteristics of 2019 novel coronavirus infections with right truncation: a statistical analysis of publicly available case data. J Clin Med. 2020;9:538. doi: 10.3390/jcm9020538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He X, Lau EHY, Wu P. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672–675. doi: 10.1038/s41591-020-0869-5. [DOI] [PubMed] [Google Scholar]
- 18.Lauer SA, Grantz KH, Bi Q. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020;172:577–582. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wölfel R, Corman VM, Guggemos W. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581:465–469. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 20.Li R, Pei S, Chen B. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science. 2020;368:489–493. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arora RK, Joseph A, Wyk JV. SeroTracker: a global SARS-CoV-2 seroprevalence dashboard. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30631-9. published online Aug 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schäfer M, Strohmeier M, Lenders V, Martinovic I, Wilhelm M. IPSN-14 Proceedings of the 13th International Symposium on Information Processing in Sensor Networks. Institute of Electrical and Electronics Engineers; New York, NY: 2014. Bringing up OpenSky: a large-scale ADS-B sensor network for research; pp. 83–94. [Google Scholar]
- 23.Abbott S, Hellewell J, Thompson RN. Estimating the time-varying reproduction number of SARS-CoV-2 using national and subnational case counts. Wellcome Open Res. 2020;5:112. [Google Scholar]
- 24.OECD DAC list of ODA recipients. Effective for reporting on 2018, 2019, and 2020 flows. 2018. https://www.oecd.org/dac/financing-sustainable-development/development-finance-standards/DAC_List_ODA_Recipients2018to2020_flows_En.pdf
- 25.International Air Transport Association Economic performance of the airline industry. June 9, 2020. https://www.iata.org/en/iata-repository/publications/economic-reports/airline-industry-economic-performance-june-2020-report
- 26.Smith P. Covid-19 in Australia: most infected health workers in Victoria's second wave acquired virus at work. BMJ. 2020;370 doi: 10.1136/bmj.m3350. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.