Abstract
There is an ongoing revolution in psychology and psychiatry that will likely change how we conceptualize, study and treat psychological problems. Many theorists now support viewing psychopathology as consisting of continuous dimensions rather than discrete diagnostic categories. Indeed, recent papers have proposed comprehensive taxonomies of psychopathology dimensions to replace the DSM and ICD taxonomies of categories. The proposed dimensional taxonomies, which portray psychopathology as hierarchically organized correlated dimensions, are now well supported at phenotypic levels. Multiple studies show that both a general factor of psychopathology at the top of the hierarchy and specific factors at lower levels predict different functional outcomes. Our analyses of data on a large representative sample of child and adolescent twins suggested the causal hypothesis that phenotypic correlations among dimensions of psychopathology are the result of many familial influences being pleiotropic. That is, most genetic variants and shared environmental factors are hypothesized to non‐specifically influence risk for multiple rather than individual dimensions of psychopathology. In contrast, person‐specific experiences tend to be related to individual dimensions. This hierarchical causal hypothesis has been supported by both large‐scale family and molecular genetic studies. Current research focuses on three issues. First, the field has not settled on a preferred statistical model for studying the hierarchy of causes and phenotypes. Second, in spite of encouraging progress, the neurobiological correlates of the hierarchy of dimensions of psychopathology are only partially described. Third, although there are potentially important clinical implications of the hierarchical model, insufficient research has been conducted to date to recommend evidence‐based clinical practices.
Keywords: Psychopathology, dimensions, hierarchical approach, general factor of psychopathology, internalizing, externalizing, bifactor model, second‐order model
Although the dominant view in psychiatry and psychology conceptualizes psychopathology as consisting of discrete diagnostic categories of mental disorders, some scholars have argued since at least the 1960s that psychopathology is better conceptualized as consisting of continuous dimensions of maladaptive behaviors, emotions and cognitions1, 2, 3, 4. More recently, a cross‐disciplinary movement has forcefully argued for abandoning categorical diagnoses and replacing them with an entirely dimensional taxonomy of psychopathology5, 6, 7, 8.
This international movement is fueled by three key issues. First, there are inherent advantages to dimensional measures of psychopathology that make them both more reliable and more valid9, 10, 11. Second, an important tenet of the movement is that all dimensions of psychopathology are positively correlated to varying degrees, and that the patterns of correlations are as important as the dimensions themselves12, 13, 14. Third, there is no empirical justification for not including all symptoms of both previously distinguished clinical and personality disorders in the same dimensional taxonomy6, 15.
The proposed hierarchical taxonomies of phenotypic dimensions of psychopathology have garnered considerable empirical support, but our understanding of these dimensions at this time requires extrapolation from limited evidence. In particular, we are hampered by the current absence of a comprehensive dimensional measure of psychopathology that includes all symptoms. This makes efforts to develop such a measure a top priority; we cannot comprehensively define the dimensions of psychopathology until we can study all of the symptoms that define the universe of psychopathology at the same time and in the same way.
DIFFERENCES AMONG STATISTICAL MODELS OF THE HIERARCHY OF PSYCHOPATHOLOGY DIMENSIONS
Several theorists have argued that the patterns of correlations among the first‐order dimensions of psychopathology (e.g., generalized anxiety, depression) can be organized into a hierarchy6, 14, 16. In meaningfully different ways, these theorists have posited that the hierarchy consists of a broad general factor of psychopathology that reflects positive correlations among all symptoms – also referred to as the p factor – and two or more specific factors of psychopathology (e.g., internalizing, externalizing)6, 14, 16, 17, 18, 19.
There are similarities among the several proposed hierarchical taxonomies, but an important unresolved issue concerns the statistical models used by different theorists. Some authors have used a simple series of exploratory principal component or factor analyses in which increasing numbers of factors are specified in each analysis. That is, one factor is extracted in the first analysis (i.e., the general factor), two factors in the second analysis (e.g., internalizing and externalizing factors), and so on until the largest number of specific factors that the data will justify have been extracted. These successive factor analyses describe a hierarchy from more general to more specific dimensions 20 , but they do not constitute or imply a specific and comprehensive statistical model of the hierarchy.
Other theorists have used second‐order models to describe the hierarchy of dimensions of psychopathology 21 . In these models, every symptom (or first‐order dimension of symptoms) loads on one of several correlated lower‐order factors and these lower‐order factors load, in turn, on a second‐order general factor (Figure 1). This operationalizes the hierarchy in a single integrated model, but the general factor and the lower‐order factors are not statistically independent, making their unique correlates impossible to parse.
Figure 1.
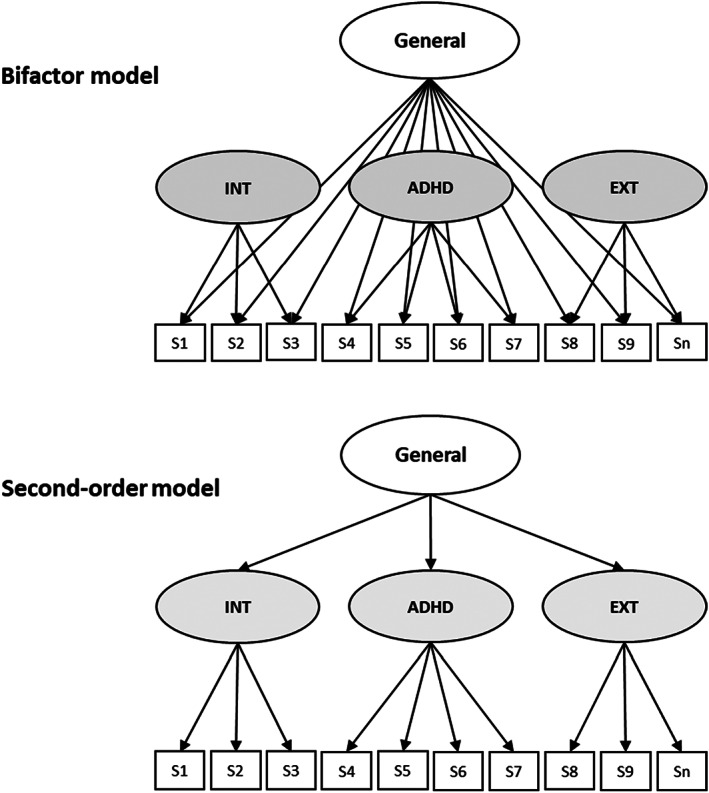
Illustrations of the different structure of bifactor and second‐order models for defining general and specific factors of psychopathology. INT – internalizing, ADHD – attention‐deficit/hyperactivity disorder, EXT – externalizing, S – symptom (or first‐order dimension of symptoms)
The bifactor model22, 23, 24 defines the hierarchy of general and specific dimensions of psychopathology proposed by Lahey et al14, 16, 17 and Caspi et al18, 19. In a bifactor model (Figure 1), each symptom (or first‐order dimension of symptoms) loads both on the general factor and on one (and only one) of some specific factors. Thus, the general factor is defined by residual correlations among all items when accounting for the correlations among items that load on each specific factor. Conversely, the specific factors are defined solely by residual correlations among symptoms within each domain when accounting for the correlations that define the general factor22, 23.
On the surface, bifactor and second‐order factor models are similar in defining general and specific factors of psychopathology, but they actually differ in important ways 23 . Tests of associations of factor scores with external variables – such as clinical outcomes, risk factors and neurobiological variations – of the two models are necessarily different in form and meaning.
In bifactor models, all of the general and specific factors are orthogonal, meaning that they are not correlated with one another. Thus, using a bifactor model, one can regress an independently defined and measured external variable on all of the general and specific factors simultaneously to determine if each of these factors accounts for unique variance in that variable.
In contrast, the factors in second‐order models are not statistically independent. Although one can regress an external variable on the general factor, the lower‐order factors cannot be included in the same regression model, because the general factor is defined by their loadings. Conversely, one can regress an external variable on lower‐order factors, but the general factor cannot be included because it is not independent of them. That is, the lower‐order and general factors are perfectly collinear in second‐order models. This means that determining the unique correlates of the lower‐level factors when controlling for the general factor is impossible. This limits the use of second‐order models in attempting to discover the unique causes and mechanisms of each general and specific factor. Even if the general factor were included in predictive models with only one specific factor at a time, thereby avoiding the perfect collinearity, the results would be uninterpretable, because the lower‐order factors are part of the very definition of the general factor.
In contrast to the above issues with the second‐order models, the bifactor model is optimal for testing unique effects simultaneously, because all of the general and specific factors are orthogonal.
There are both similarities and differences among the factors defined in bifactor and second‐order models. The general factors defined in bifactor and second‐order models are actually very highly correlated and, for some purposes, can be used interchangeably6, 25. In contrast, the specific factors defined in these two statistical models are quite different and only moderately correlated 25 . For instance, in one study of adults testing the bifactor model, first‐order dimensions capturing all types of phobias had lower loadings on the general factor than the first‐order dimensions of generalized anxiety and depression 26 . This means that the specific internalizing factor in a bifactor model reflects fears more, and generalized anxiety and depression less, than the internalizing factor in a second‐order model.
CONCERNS ABOUT BIFACTOR MODELS
The discriminant validity of general and specific factors of psychopathology using bifactor models has been supported in several studies with large samples. These studies have shown that, over and above the prediction from specific factors such as externalizing and internalizing, the general factor of psychopathology predicts independently measured adverse functional outcomes, such as psychoactive drug prescriptions, incarceration, poor academic progress, suicidal behavior, and self‐harm27, 28, 29, 30, 31.
Nonetheless, the use of bifactor models in hierarchical approaches to psychopathology has been controversial. Some of the controversy stems from the fact that fit indices sometimes favor bifactor models over second‐order models when they conceptually should not 32 . This is a valid concern, but not a telling issue. One should not choose among well‐fitting but substantively different statistical models only on the basis of the model fit in any case. Rather, one should choose among well‐fitting models on the basis of their validity and utility 32 .
A second concern raised about bifactor models focuses on the replicability of the specific factors in those models. The H index uses cross‐sectional data to estimate how replicable a latent factor may be. One study raised a concern about bifactor models by reporting adequate H for the general and externalizing factors, but unacceptable H values for the internalizing factor 33 . However, other studies using stronger samples and measures have reported acceptable H values for both the general and all specific factors in bifactor models21, 25, 34.
Moreover, rather than trying to estimate the replicability of the general and specific factors of psychopathology from a single analysis of cross‐sectional data, it is far more informative to conduct longitudinal studies in which these factors are independently estimated in the same persons. When this has been done, both general and specific factors of psychopathology defined in bifactor models have proven to be replicable in the same persons over multiple years34, 35, 36, 37, 38, 39. Thus, although estimates of the replicability of specific factors as indexed by H in single assessments warrant attention, there is strong evidence from longitudinal studies that all factors of psychopathology are replicable over time.
CAUSAL VS. PHENOTYPIC HIERARCHICAL MODELS
It is important to note that the hierarchical taxonomies of psychopathology that have been proposed to date all necessarily include a descriptive model of dimensional phenotypes. The most extensive hierarchical phenotypic model has been offered by the group operating under the name of Hierarchical Taxonomy of Psychopathology (HiTOP)6, 15. The HiTOP has advanced a comprehensive taxonomy based on the existing empirical literature on phenotypic structure and advocated for the utility of applying such a model to psychopathology in both research and clinical practice.
We have offered a complementary approach that addresses both the hierarchy of phenotypes and the causes that create the hierarchy of phenotypes 14 . In one of our studies, we collected data on psychopathology dimensions from a large and representative sample of child and adolescent twins 17 . Based on differences in correlations among these phenotypic dimensions in monozygotic and dizygotic twin pairs, genetic and environmental correlations among the phenotypic dimensions were estimated and then each analyzed in bifactor models. The results suggested the causal hypothesis that phenotypic correlations among all dimensions of psychopathology captured by the general factor are largely the result of the same familial factors. That is, many genetic variants and environmental factors shared by family members appear to non‐specifically influence risk for manifesting psychopathology of some sort, but not specific dimensions of psychopathology. On the contrary, other genetic and environmental influences, particularly person‐specific experiences, play the largest role in determining the specific dimensions of psychopathology that will be exhibited 17 .
Thus, we hypothesized a hierarchy of causal influences, from the most non‐specific to the most specific, that gives rise to the hierarchy of phenotypes 14 . This hypothesized hierarchy of genetic and environmental influences has been confirmed in a large sample of siblings in Sweden 40 . Moreover, molecular genetic research has supported the hypothesis that the hierarchy of correlated phenotypes results partly from highly pleiotropic genetic variants that non‐specifically increase the risk for many or all forms of psychopathology41, 42, 43.
Members of the HiTOP group have recently proposed that their hierarchical, dimensional and data‐driven classification system provides a more effective approach to identifying genes that underlie mental disorders, and to studying psychiatric etiology, than current diagnostic categories. Specifically, genes are expected to operate at different levels of the HiTOP hierarchy, with some highly pleiotropic genes influencing higher‐order psychopathology (e.g., the general factor), whereas other genes confer more specific risk for individual spectra (e.g., internalizing), sub‐factors (e.g., fear disorders), or narrow symptoms (e.g., mood instability) 44 .
We strongly agree that this is the hypothesis that we should be testing. Indeed, this hypothesis has already received considerable empirical support. We would only add that family level environmental influences may also be highly non‐specific, while person‐specific experiences more likely play a role in determining which specific symptoms a person exhibits at each point in time. We note in this context that the bifactor model is optimized to test such general versus specific hypotheses, whereas second‐order models are not.
NATURE OF GENERAL AND SPECIFIC FACTORS DEFINED IN BIFACTOR MODELS
A great deal has been learned in a short amount of time about the nature of the hypothesized general and specific factors of psychopathology from the bifactor model. Here we focus on several issues, including the stability of the hierarchy of factors of psychopathology over time, the correlated psychobiological processes, and the neurobiological mechanisms.
Stability over time
To what extent do persons’ scores on the general and specific factors of psychopathology change or remain the same? Across 1‐2 years in childhood and adolescence, several studies have found that each general and specific factor of psychopathology significantly predicted itself primarily or exclusively in the next assessment, revealing moderate to strong stability over time34, 35, 36, 39.
In a study of a representative sample of 43,000 adults, the general and all specific factors of psychopathology predicted only themselves over 3 years, with the exception of a specific distress factor defined by major depression, dysthymia, and generalized anxiety disorder 37 . In contrast, a study of 499 persons assessed in childhood or adolescence and then evaluated again 12 years later in adulthood found that general factor scores were significantly stable over time, but specific internalizing and externalizing factors were not stable over this long interval 38 .
More needs to be learned, but it appears that all factors of psychopathology defined in bifactor models are stable over time during childhood and adolescence, but some of the specific factors may be less stable during adulthood or from adolescence into adulthood.
Correlated psychobiological processes
What is the nature of the general factor in psychological and biological terms? Because the general factor is simply a statistical construct, it is very important for us to understand the processes that it reflects to gain the greatest theoretical leverage on psychopathology. A growing amount of replicated data already reveals something of the psychobiological nature of the general factor defined in bifactor models.
Negative emotionality
It is well known that individual differences in negative emotionality (neuroticism) are robustly and positively associated with every form of psychopathology 45 . Thus, it is not surprising that multiple studies have found negative emotionality to be associated with the general factor defined in bifactor models34, 46, 47.
In nearly all of these studies, the measure of negative emotionality was also significantly associated with specific internalizing psychopathology. In one study, it was also associated with externalizing psychopathology 47 . Thus, the individual differences in the experience of negative emotions captured by measures of negative emotionality appear to be at the heart of the general factor, but are also related to more specific dimensions of psychopathology.
Cognitive abilities, including executive functions
A number of studies have also consistently reported significant associations of the general factor of psychopathology with both intelligence 19 and global and specific measures of the executive functions18, 25, 48, 49, 50. The term executive functions refers to a related set of highly heritable cognitive processes that are believed to regulate attention and foster adaptive goal‐directed behavior 51 . Much remains to be learned, but it is possible that deficits in executive functions are one of the psychobiological processes that underlie the general factor of psychopathology 52 .
It is important to note that both twin and molecular genetic studies suggest that the general factor of psychopathology is moderately heritable53, 54. Furthermore, two twin studies have determined that both measures of negative emotionality 47 and of executive functions 55 share their genetic influences with the general factor of psychopathology in children and adolescents. These findings strengthen the view that high negative emotionality and deficits in executive functions are at least part of what constitutes the non‐specific tendency to develop psychopathology that is captured by the general factor.
Impulsive responsivity to positive and negative emotions
Johnson et al 56 have argued that impulsive responding to both positive and negative emotions is a key factor underlying all dimensions of psychopathology through the general factor 57 . Thus, they posit that it is the cognitive control of emotion that is important, and argue that deficits in controlling both negative emotions and exuberant positive emotions are involved in psychopathology.
We recently used data from the large Adolescent Brain Cognitive Development (ABCD) Study to examine associations between the general factor of psychopathology in children and self‐report measures of dispositions, including the positive urgency and negative urgency scales of a short form of the UPPS impulsivity measure 58 . Consistent with the above hypothesis, these scales, which tap impulsive responding to positive and negative emotions, were both positively associated with the general factor of psychopathology defined in a bifactor model 25 .
Disordered thinking
Caspi and Moffitt 19 have added another hypothesis regarding the underlying psychobiological nature of the general factor of psychopathology. They suggest that the general factor is partly the result of disordered thought processes common to essentially all dimensions of psychopathology.
They defined disordered thought as “thought processes [that] are illogical, unfiltered, tangential, and reality‐distorted and ‐distorting” 19 . This refers broadly to the altered cognitions revealed in difficulty making decisions, misattributions, body image disturbances, irrational fears, dissociative states, depersonalization and derealization, beliefs that there will be terrible consequences if a logically unrelated action is not performed, and delusions and hallucinations.
This new hypothesis is cogent, plausible and intriguing. One difficulty is that reliable and valid measures of the full breadth of disordered cognition referred to by Caspi and Moffitt do not exist at this time. This means that only piecemeal tests of their hypothesis are currently possible.
Neurobiological mechanisms
We have only begun to map the biological correlates of the general and specific factors of psychopathology defined in bifactor models. This research is vitally important to understand the mechanisms that link causes and symptoms and, fortunately, is continuing at a rapid pace 59 .
A recent review of this research literature stated that the general factor “has been associated with a number of neurobiological measures in youths, including reduced gray matter volume60, 61, reduced activity in executive regions 62 , elevated resting‐state cerebral blood flow 63 , reduced fractional anisotropy 64 , and delay in connectome distinctiveness”65, 66.
Replications of some findings have already been published, including associations between the general factor of psychopathology and atypical white matter development67, 68, 69, atypicalities in the cerebellum and its connections70, 71, 72, and lack of typical segregation between the default mode and executive networks during rest 73 . Thus, we may not be far from an understanding of at least some of the neurobiological mechanisms related to the general factor of psychopathology.
CLINICAL IMPLICATIONS
There are several ways in which hierarchical dimensional models of psychopathology are important in clinical settings. The most immediate implication of these models is a change in how we conceptualize psychopathology. There is a continuous relationship between dimensions of symptoms and adverse outcomes. This relationship between gradually more symptoms and greater impairment begins well below diagnostic thresholds, which argues against limiting care to only those who meet binary diagnostic thresholds74, 75, 76, 77, 78. Similarly, the extensive changes in symptoms over time – heterotypic continuity – refutes the view of mental disorders as enduring discrete conditions 79 .
Furthermore, the robust correlations among dimensions of psychopathology tell us that meeting diagnostic criteria for a categorical diagnosis does not imply that a person has a distinct mental disorder. The ubiquitous correlations among symptoms and dimensions mean that people do not fit neatly into diagnostic categories. People exhibit widely varying patchworks of symptoms from multiple dimensions, even if they meet criteria for a single diagnosis.
In considering the implications of the hierarchical taxonomy of psychopathology for clinical practice, it is essential to understand that the general factor of psychopathology is not being proposed as a new “kind” of psychopathology. It is certainly not being proposed as the basis for a new diagnosis. Nonetheless, bifactor models that include a general factor do give us an opportunity to view dimensions of psychopathology through a new lens.
In simple terms, the general factor reflects a “weighted average” of some aspects of all symptoms exhibited by each person at that point in time. Symptoms that are more correlated with all other symptoms – controlling for correlations among symptoms captured by more specific second‐order factors, such as internalizing or externalizing – contribute more to the general factor score. Conversely, specific factor scores, such as internalizing, reflect only the residual correlations among just a subset of symptoms after controlling for the widespread correlations among all symptoms.
The general factor score may prove to have particular value in improving prognosis in clinical practice and in targeted prevention programs. Although much remains to be learned, it appears that youth with higher general factor scores experience greater serious functional impairment over time, independent of the specific symptoms they exhibit. As noted above, this includes greater risk for incarceration, suicidal behavior, and non‐suicidal self‐harm27, 28, 29, 30, 31.
The difficulty is that there currently is no comprehensive standard measure of the general and specific factors of psychopathology that is ready for clinical use to improve prognosis. One group has used a large set of psychopathology items administered to a large sample of children and adolescents to develop a computer‐administered measure of general and specific factors of psychopathology that may eventually be useful in clinical settings 80 . The psychometric properties of this measure are encouraging, but it has not been replicated and validated enough to be ready for clinical application.
These replications and tests would need to be conducted in large samples representing a variety of geographic locations, cultures and languages before they can be widely usable. Such measures may not be available in the near future, which means that no evidence‐based practices can be recommended even for improving prognosis. On a commonsense basis, it seems reasonable for clinicians to suspect that persons with simply more symptoms from across multiple domains are at higher risk for serious adverse outcomes. However, we do not have enough evidence at this point to be confident in that practice.
The hierarchical model is likely to play an important role in treatment research. At least one clinical research study used the hierarchical taxonomy of psychopathology to measure changes associated with randomly assigned interventions to better understand the general and specific effects of treatment 81 . Other researchers are developing and testing new treatment methods that are designed to remediate the processes, e.g. negative emotionality, that all dimensions of psychopathology appear to share82, 83. Tests of these new treatments may not only lead to better treatments with more widespread benefits, but will help us understand what underlies the general and specific factors of psychopathology.
ACKNOWLEDGEMENTS
This paper was supported by grants from the US National Institute of Drug Abuse (UG3‐DA045251), the US National Institute of Mental Health (R01‐MH098098 and R01‐MH117014), the US National Institutes of Health (UL1‐TR000430 and UL1‐TR000445), the Lifespan Brain Institute of the University of Pennsylvania, and the Children’s Hospital of Philadelphia.
REFERENCES
- 1. Achenbach TM. Classification of children’s psychiatric symptoms: a factor analytic study. Psychol Monogr 1966;80:1‐37. [DOI] [PubMed] [Google Scholar]
- 2. Achenbach TM, Conners CK, Quay HC et al. Replication of empirically derived syndromes as a basis for taxonomy of child and adolescent psychopathology. J Abnorm Child Psychol 1989;17:299‐323. [DOI] [PubMed] [Google Scholar]
- 3. Quay HC. Classification In: Quay HC, Werry JS. (eds). Psychopathological disorders of childhood, 3rd ed. New York: Wiley, 1986:1‐42. [Google Scholar]
- 4. Quay HC, Quay LC. Behavior problems in early adolescence. Child Develop 1965;36:215‐20. [PubMed] [Google Scholar]
- 5. Conway CC, Forbes MK, Forbush KT et al. A hierarchical taxonomy of psychopathology can transform mental health research. Perspect Psychol Sci 2019;14:419‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kotov R, Krueger RF, Watson D et al. The hierarchical taxonomy of psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol 2017;126:454‐77. [DOI] [PubMed] [Google Scholar]
- 7. Wright AGC, Krueger RF, Hobbs MJ et al. The structure of psychopathology: toward an expanded quantitative empirical model. J Abnorm Psychol 2013;122:281‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Krueger RF, Kotov R, Watson D et al. Progress in achieving quantitative classification of psychopathology. World Psychiatry 2018;17:282‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Markon KE, Chmielewski M, Miller CJ. The reliability and validity of discrete and continuous measures of psychopathology: a quantitative review. Psychol Bull 2011;137:856‐79. [DOI] [PubMed] [Google Scholar]
- 10. Helzer JE, Kraemer HC, Krueger RF. The feasibility and need for dimensional psychiatric diagnoses. Psychol Med 2006;36:1671‐80. [DOI] [PubMed] [Google Scholar]
- 11. Widiger TA, Samuel DB. Diagnostic categories or dimensions? A question for the diagnostic and statistical manual of mental disorders ‐ fifth edition. J Abnorm Psychol 2005;114:494‐504. [DOI] [PubMed] [Google Scholar]
- 12. Angold A, Costello EJ. Nosology and measurement in child and adolescent psychiatry. J Child Psychol Psychiatry 2009;50:9‐15. [DOI] [PubMed] [Google Scholar]
- 13. Krueger RF, Markon KE. Reinterpreting comorbidity: a model‐based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol 2006;2:111‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lahey BB, Krueger RF, Rathouz PJ et al. A hierarchical causal taxonomy of psychopathology across the life span. Psychol Bull 2017;143:142‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kotov R, Krueger RF, Watson D. A paradigm shift in psychiatric classification: the Hierarchical Taxonomy Of Psychopathology (HiTOP). World Psychiatry 2018;17:24‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lahey BB, Applegate B, Hakes JK et al. Is there a general factor of prevalent psychopathology during adulthood? J Abnorm Psychol 2012;121:971‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lahey BB, Van Hulle CA, Singh AL et al. Higher‐order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Arch Gen Psychiatry 2011;68:181‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Caspi A, Houts RM, Belsky DW et al. The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin Psychol Sci 2014;2:119‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Caspi A, Moffitt TE. All for one and one for all: mental disorders in one dimension. Am J Psychiatry 2018;175:831‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Michelini G, Barch DM, Tian Y et al. Delineating and validating higher‐order dimensions of psychopathology in the Adolescent Brain Cognitive Development (ABCD) study. Transl Psychiatry 2019;9:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sunderland M, Forbes MK, Mewton L et al. The structure of psychopathology and association with poor sleep, self‐harm, suicidality, risky sexual behaviour, and low self‐esteem in a population sample of adolescents. Dev Psychopathol (in press). [DOI] [PubMed] [Google Scholar]
- 22. Reise SP. The rediscovery of bifactor measurement models. Multivar Behav Res 2012;47:667‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mansolf M, Reise SP. When and why the second‐order and bifactor models are distinguishable. Intelligence 2017;61:120‐9. [Google Scholar]
- 24. Holzinger KJ, Swineford F. The bi‐factor method. Psychometrika 1937;2:41‐54. [Google Scholar]
- 25. Moore TM, Kaczkurkin AN, Durham EL et al. Criterion validity and relationships between alternative hierarchical dimensional models of general and specific psychopathology. J Abnorm Psychol (in press). [DOI] [PMC free article] [PubMed]
- 26. Lahey BB, Zald DH, Perkins SF et al. Measuring the hierarchical general factor model of psychopathology in young adults. Int J Methods Psychiatr Res 2018;27:e1593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pettersson E, Lahey BB, Lundström S et al. Criterion validity and utility of the general factor of psychopathology in childhood: predictive associations with independently measured severe adverse mental health outcomes in adolescence. J Am Acad Child Adolesc Psychiatry 2018;57:372‐83. [DOI] [PubMed] [Google Scholar]
- 28. Lahey BB, Rathouz PJ, Keenan K et al. Criterion validity of the general factor of psychopathology in a prospective study of girls. J Child Psychol Psychiatry 2015;4:415‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sallis H, Szekely E, Neumann A et al. General psychopathology, internalising and externalising in children and functional outcomes in late adolescence. J Child Psychol Psychiatry 2019;60:1183‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Haltigan JD, Aitken M, Skilling T et al. “P” and “DP”: examining symptom‐level bifactor models of psychopathology and dysregulation in clinically referred children and adolescents. J Am Acad Child Adolesc Psychiatry 2018;57:384‐96. [DOI] [PubMed] [Google Scholar]
- 31. Hoertel N, Franco S, Wall MM et al. Mental disorders and risk of suicide attempt: a national prospective study. Mol Psychiatry 2015;20:718‐26. [DOI] [PubMed] [Google Scholar]
- 32. Bonifay W, Lane SP, Reise SP. Three concerns with applying a bifactor model as a structure of psychopathology. Clin Psychol Sci 2017;5:184‐6. [Google Scholar]
- 33. Watts AL, Poore HE, Waldman ID. Riskier tests of the validity of the bifactor model of psychopathology. Clin Psychol Sci 2019;7:1285‐303. [Google Scholar]
- 34. Castellanos‐Ryan N, Briere FN, O’Leary‐Barrett M et al. The structure of psychopathology in adolescence and its common personality and cognitive correlates. J Abnorm Psychol 2016;125:1039‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. McElroy E, Belsky J, Carragher N et al. Developmental stability of general and specific factors of psychopathology from early childhood to adolescence: dynamic mutualism or p‐differentiation? J Child Psychol Psychiatry 2018;59:667‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Snyder HR, Young JF, Hankin BL. Strong homotypic continuity in common psychopathology‐, internalizing‐, and externalizing‐specific factors over time in adolescents. Clin Psychol Sci 2017;5:98‐110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Greene AL, Eaton NR. The temporal stability of the bifactor model of comorbidity: an examination of moderated continuity pathways. Compr Psychiatry 2017;72:74‐82. [DOI] [PubMed] [Google Scholar]
- 38. Class QA, Rathouz PJ, Van Hulle CA et al. Socioemotional dispositions of children and adolescents predict general and specific second‐order factors of psychopathology in early adulthood across informants: a 12‐year prospective study. J Abnorm Psychol 2019;128:574‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Olino TM, Bufferd SJ, Dougherty LR et al. The development of latent dimensions of psychopathology across early childhood: stability of dimensions and moderators of change. J Abnorm Child Psychol 2018;46:1373‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pettersson E, Larsson H, Lichtenstein P. Common psychiatric disorders share the same genetic origin: a multivariate sibling study of the Swedish population. Mol Psychiatry 2016;21:717‐21. [DOI] [PubMed] [Google Scholar]
- 41. Selzam S, Coleman JRI, Caspi A et al. A polygenic p factor for major psychiatric disorders. Transl Psychiatry 2018;8:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Grotzinger AD, Cheung AK, Patterson MW et al. Genetic and environmental links between general factors of psychopathology and cognitive ability in early childhood. Clin Psychol Sci 2019;7:430‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Smoller JW, Andreassen OA, Edenberg HJ et al. Psychiatric genetics and the structure of psychopathology. Mol Psychiatry 2019;24:409‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Waszczuk MA, Eaton NR, Krueger RF et al. Redefining phenotypes to advance psychiatric genetics: implications from Hierarchical Taxonomy of Psychopathology. J Abnorm Psychol 2020;129:143‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lahey BB. Public health significance of neuroticism. Am Psychol 2009;64:241‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Olino TM, Dougherty LR, Bufferd SJ et al. Testing models of psychopathology in preschool‐aged children using a structured interview‐based assessment. J Abnorm Child Psychol 2014;42:1201‐11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Tackett JL, Lahey BB, Van Hulle CA et al. Common genetic influences on negative emotionality and a general psychopathology factor in childhood and adolescence. J Abnorm Psychol 2013;122:1142‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Martel MM, Pan PM, Hoffmann MS et al. A general psychopathology factor (p factor) in children: structural model analysis and external validation through familial risk and child global executive function. J Abnorm Psychol 2017;126:137‐48. [DOI] [PubMed] [Google Scholar]
- 49. Shields AN, Reardon KW, Brandes CM et al. The p factor in children: relationships with executive functions and effortful control. J Res Personality 2019;82:103853. [Google Scholar]
- 50. Bloemen AJP, Oldehinkel AJ, Laceulle OM et al. The association between executive functioning and psychopathology: general or specific? Psychol Med 2018;48:1787‐94. [DOI] [PubMed] [Google Scholar]
- 51. Friedman NP, Miyake A, Young SE et al. Individual differences in executive functions are almost entirely genetic in origin. J Exp Psychol Gen 2008;137:201‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. McTeague LM, Goodkind MS, Etkin A. Transdiagnostic impairment of cognitive control in mental illness. J Psychiatr Res 2016;83:37‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Waldman ID, Poore HE, van Hulle C et al. External validity of a hierarchical dimensional model of child and adolescent psychopathology: tests using confirmatory factor analyses and multivariate behavior genetic analyses. J Abnorm Psychol 2016;125:1053‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Neumann A, Pappa I, Lahey BB et al. SNP heritability of a general psychopathology factor in children. J Am Acad Child Adolesc Psychiatry 2016;55:1038‐45. [DOI] [PubMed] [Google Scholar]
- 55. Harden KP, Engelhardt LE, Mann FD et al. Genetic associations between executive functions and a general factor of psychopathology. J Am Acad Child Adolesc Psychiatry 2020;59:749‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Johnson SL, Elliott MV, Carver CS. Impulsive responses to positive and negative emotions: parallel neurocognitive correlates and their implications. Biol Psychiatry 2020;87:338‐49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Carver CS, Johnson SL, Timpano KR. Toward a functional view of the p factor in psychopathology. Psychol Sci 2017:5:880‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Zapolski TCB, Stairs AM, Settles RF et al. The measurement of dispositions to rash action in children. Assessment 2010;17:116‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Zald DH, Lahey BB. Implications of the hierarchical structure of psychopathology for psychiatric neuroimaging. Biol Psychiatry Cogn Neurosci Neuroimaging 2017;2:310‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kaczkurkin AN, Park SS, Sotiras A et al. Evidence for dissociable linkage of dimensions of psychopathology to brain structure in youths. Am J Psychiatry 2019;176:1000‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Snyder HR, Hankin BL, Sandman CA et al. Distinct patterns of reduced prefrontal and limbic gray matter volume in childhood general and internalizing psychopathology. Clin Psychol Sci 2017;5:1001‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Shanmugan S, Wolf DH, Calkins ME et al. Common and dissociable mechanisms of executive system dysfunction across psychiatric disorders in youth. Am J Psychiatry 2016;173:517‐26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Kaczkurkin AN, Moore TM, Calkins ME et al. Common and dissociable regional cerebral blood flow differences associate with dimensions of psychopathology across categorical diagnoses. Mol Psychiatry 2018;23:1981‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Riem MME, van Hoof MJ, Garrett AS et al. General psychopathology factor and unresolved‐disorganized attachment uniquely correlated to white matter integrity using diffusion tensor imaging. Behav Brain Res 2018;359:1‐8. [DOI] [PubMed] [Google Scholar]
- 65. Kaufmann T, Alnaes D, Doan NT et al. Delayed stabilization and individualization in connectome development are related to psychiatric disorders. Nat Neurosci 2017;20:513‐5. [DOI] [PubMed] [Google Scholar]
- 66. Kaczkurkin AN, Moore TM, Sotiras A et al. Approaches to defining common and dissociable neurobiological deficits associated with psychopathology in youth. Biol Psychiatry 2020;88:51‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Vanes LD, Moutoussis M, Ziegler G et al. White matter tract myelin maturation and its association with general psychopathology in adolescence and early adulthood. Hum Brain Mapp 2020;41:827‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Hinton KE, Lahey BB, Villalta‐Gil V et al. White matter microstructure correlates of general and specific second‐order factors of psychopathology. Neuroimage Clin 2019;22:101705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Neumann A, Muetzel RL, Lahey BB et al. White matter microstructure and the general psychopathology factor in children. J Am Acad Child Adolesc Psychiatry 2020;59:1285‐96. [DOI] [PubMed] [Google Scholar]
- 70. Elliott ML, Romer A, Knodt AR et al. A connectome‐wide functional signature of transdiagnostic risk for mental illness. Biol Psychiatry 2018;84:452‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Hariri AR. The emerging importance of the cerebellum in broad risk for psychopathology. Neuron 2019;102:17‐20. [DOI] [PubMed] [Google Scholar]
- 72. Romer AL, Knodt AR, Sison ML et al. Replicability of structural brain alterations associated with general psychopathology: evidence from a population‐representative birth cohort. Mol Psychiatry (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Xia CH, Ma ZM, Ciric R et al. Linked dimensions of psychopathology and connectivity in functional brain networks. Nat Commun 2018;9:3003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Bosman RC, ten Have M, de Graaf R et al. Prevalence and course of subthreshold anxiety disorder in the general population: a three‐year follow‐up study. J Affect Disord 2019;247:105‐13. [DOI] [PubMed] [Google Scholar]
- 75. Costanzo M, Jovanovic T, Norrholm SD et al. Psychophysiological investigation of combat veterans with subthreshold post‐traumatic stress disorder symptoms. Mil Med 2016;181:793‐802. [DOI] [PubMed] [Google Scholar]
- 76. Fergusson DM, Horwood LJ, Ridder EM et al. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry 2005;62:66‐72. [DOI] [PubMed] [Google Scholar]
- 77. Rosengard RJ, Malla A, Mustafa S et al. Association of pre‐onset subthreshold psychotic symptoms with longitudinal outcomes during treatment of a first episode of psychosis. JAMA Psychiatry 2019;76:61‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Lahey BB, Class QA, Zald DH et al. Prospective test of the developmental propensity model of antisocial behavior: from childhood and adolescence into early adulthood. J Child Psychol Psychiatry 2018;59:676‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Lahey BB, Zald DH, Hakes JK et al. Patterns of heterotypic continuity associated with the cross‐sectional correlational structure of prevalent mental disorders in adults. JAMA Psychiatry 2014;71:989‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Moore TM, Calkins ME, Satterthwaite TD et al. Development of a computerized adaptive screening tool for overall psychopathology (“p”). J Psychiatr Res 2019;116:26‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Wade M, Fox NA, Zeanah CH et al. Effect of foster care intervention on trajectories of general and specific psychopathology among children with histories of institutional rearing: a randomized clinical trial. JAMA Psychiatry 2018;75:1137‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Meier MA, Meier MH. Clinical implications of a general psychopathology factor: a cognitive‐behavioral transdiagnostic group treatment for community mental health. J Psychother Integration 2018;28:253‐68. [Google Scholar]
- 83. Farchione TJ, Fairholme CP, Ellard KK et al. Unified protocol for transdiagnostic treatment of emotional disorders: a randomized controlled trial. Behav Ther 2012;43:666‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]


