Abstract
The current management of patients with primary psychosis worldwide is often remarkably stereotyped. In almost all cases an antipsychotic medication is prescribed, with second‐generation antipsychotics usually preferred to first‐generation ones. Cognitive behavioral therapy is rarely used in the vast majority of countries, although there is evidence to support its efficacy. Psychosocial interventions are often provided, especially in chronic cases, but those applied are frequently not validated by research. Evidence‐based family interventions and supported employment programs are seldom implemented in ordinary practice. Although the notion that patients with primary psychosis are at increased risk for cardiovascular diseases and diabetes mellitus is widely shared, it is not frequent that appropriate measures be implemented to address this problem. The view that the management of the patient with primary psychosis should be personalized is endorsed by the vast majority of clinicians, but this personalization is lacking or inadequate in most clinical contexts. Although many mental health services would declare themselves “recovery‐oriented”, it is not common that a focus on empowerment, identity, meaning and resilience is ensured in ordinary practice. The present paper aims to address this situation. It describes systematically the salient domains that should be considered in the characterization of the individual patient with primary psychosis aimed at personalization of management. These include positive and negative symptom dimensions, other psychopathological components, onset and course, neurocognition and social cognition, neurodevelopmental indicators; social functioning, quality of life and unmet needs; clinical staging, antecedent and concomitant psychiatric conditions, physical comorbidities, family history, history of obstetric complications, early and recent environmental exposures, protective factors and resilience, and internalized stigma. For each domain, simple assessment instruments are identified that could be considered for use in clinical practice and included in standardized decision tools. A management of primary psychosis is encouraged which takes into account all the available treatment modalities whose efficacy is supported by research evidence, selects and modulates them in the individual patient on the basis of the clinical characterization, addresses the patient’s needs in terms of employment, housing, self‐care, social relationships and education, and offers a focus on identity, meaning and resilience.
Keywords: Primary psychosis, schizophrenia, personalization of treatment, psychosocial interventions, recovery, positive dimension, negative dimension, neurocognition, social cognition, social functioning, psychiatric antecedents, psychiatric comorbidities, physical comorbidities, family history, obstetric complications, environmental exposures, protective factors, resilience, practical needs, internalized stigma
Primary psychoses represent a heterogeneous group of mental disorders that: a) are characterized by delusions and/or hallucinations, along with other clinical manifestations such as disorganized thinking, grossly disorganized or abnormal motor behavior, and negative symptoms (i.e., affective blunting, alogia, asociality, anhedonia or avolition); b) are not due to the effects of a substance or a medication on the central nervous system, and are not secondary to another medical condition (e.g., a brain tumor or an autoimmune disease) or a mood disorder (depression or mania).
Our current diagnostic systems, the DSM‐51 and the ICD‐11 2 , include several categories that fulfill the above definition, but neither the list of these categories nor their definition is consistent between the two systems.
In the DSM‐5, primary psychoses include schizophrenia, schizophreniform disorder, brief psychotic disorder, schizoaffective disorder, delusional disorder, “other specified schizophrenia spectrum and other psychotic disorder”, and “unspecified schizophrenia spectrum and other psychotic disorder”. In the ICD‐11, primary psychoses (the expression “primary psychotic disorders” is explicitly used in this system) include schizophrenia, acute and transient psychotic disorder, schizoaffective disorder, delusional disorder, and “other primary psychotic disorder”.
In the DSM‐5, the definition of schizophrenia requires that “continuous signs of the disturbance persist for at least six months”, whereas this requirement is absent in the ICD‐11 (it is only stated that “symptoms must be present most of the time for a period of one month or more”). As a consequence of this, the DSM‐5 category of schizophreniform disorder (marked by a duration of the disorder of at least one month but less than six months) does not appear in the ICD‐11. People with a diagnosis of schizophreniform disorder according to the DSM‐5 will be diagnosed as having schizophrenia according to the ICD‐11.
Furthermore, social dysfunction is an integral part of the diagnostic criteria for schizophrenia in the DSM‐5 (“for a significant portion of the time since the onset of the disturbance, level of functioning in one or more major areas, such as work, interpersonal relations, or self‐care, is markedly below the level achieved prior to the onset”) 1 , whereas this element is absent in the ICD‐11 definition. In the “additional features” subsection of the section on schizophrenia of the ICD‐11 diagnostic guidelines, it is indeed specified that “distress and psychosocial impairment are not requirements for a diagnosis of schizophrenia” 2 .
The symptomatological criterion for the diagnosis of schizophrenia lists, in both the DSM‐5 and ICD‐11, delusions, hallucinations, negative symptoms, disorganized thinking, and grossly disorganized behavior. However, the ICD‐11 also includes “experiences of influence, passivity or control” (subsumed under the heading of delusions in the DSM‐5), and “psychomotor disturbances” (which are part of the item “grossly disorganized or catatonic behavior” in the DSM‐5).
Schizoaffective disorder is defined quite differently in the two diagnostic systems. In fact, the longitudinal criterion (“delusions or hallucinations for two or more weeks in the absence of a major mood episode (depressive or manic) during the lifetime duration of the illness”) is absent in the ICD‐11, in which the disorder is just defined by the concurrent fulfillment of the definitional requirements for schizophrenia and a mood episode for at least one month. So, a number of patients will receive a diagnosis of schizoaffective disorder according to the ICD‐11 but not the DSM‐5.
There are also significant differences in the DSM‐5 definition of brief psychotic disorder vs. the ICD‐11 characterization of acute and transient psychotic disorder. In particular, the presence of negative symptoms is excluded in the definition of the latter but not the former disorder, and the duration of symptoms is required to be “less than one month” in the DSM‐5, while it “does not exceed three months” in the ICD‐11. Furthermore, the requirement that “symptoms change rapidly, both in nature and intensity, from day to day or even within a single day” is present in the ICD‐11 definition but not in the DSM‐5 criteria.
Also due to the above discrepancies, that were already present in the previous editions of the two diagnostic systems, there is no clarity about the prevalence of the individual primary psychotic disorders either in the general population or in clinical settings. What can certainly be argued is that there is a predominant focus on schizophrenia both in research and in clinical practice. For instance, research on neurocognitive impairment has been conducted almost exclusively in patients with a post‐DSM‐III diagnosis of schizophrenia 3 , and its results may not be generalizable to all patients with an ICD‐11 diagnosis of schizophrenia or to patients with ICD‐11 “other primary psychotic disorder”.
On the other hand, the awareness that the term schizophrenia has been traditionally associated with the notion of a poor outcome, and has acquired in ordinary language a derogatory connotation 4 , is leading many clinicians and researchers to use the generic term “psychosis” as a synonym for schizophrenia or as equivalent to the expression “primary psychosis”. This is generating confusion in the field – e.g., obscuring the need for the differentiation between primary psychosis and substance induced psychosis.
Of note, one of the few comprehensive population‐based epidemiological studies available in this area (which used DSM‐IV criteria, that are very close to DSM‐5 ones) 5 found the lifetime prevalence of all primary psychotic disorders to be 1.94%, while that of schizophrenia was 0.87% (so, according to this study, schizophrenia accounts for just 43.8% of cases of primary psychotic disorder). The lifetime prevalence was 0.32% for schizoaffective disorder, 0.07% for schizophreniform disorder, 0.18% for delusional disorder, 0.05% for brief psychotic disorder, and 0.45% for psychotic disorder not otherwise specified. The lifetime prevalence of affective psychoses was 0.59%, that of substance induced psychotic disorder was 0.42%, and that of psychotic disorder due to a general medical condition was 0.21% (so that schizophrenia accounted for only 26.9% of all cases of psychotic disorder) 5 .
The current approach to schizophrenia (or to “psychosis”) in routine clinical practice worldwide is often remarkably stereotyped. In almost all cases an antipsychotic medication is prescribed, with second‐generation antipsychotics usually preferred to first‐generation ones 6 . Cognitive behavioral therapy (CBT) is rarely used in the vast majority of countries, even though there is evidence to support its efficacy 7 . Psychosocial interventions are often provided, especially in patients with chronic illness, but those applied are frequently not validated by research 8 . Evidence‐based family interventions 9 and supported employment programmes 10 are seldom implemented in ordinary practice. The notion that patients with schizophrenia (or “psychosis”) are at increased risk for several physical diseases and that their life expectancy is dramatically reduced is now widely shared, but it is not frequent that appropriate measures be implemented to address this problem as part of the management plan 11 .
The view that the management of a patient with schizophrenia (or “psychosis”) should be personalized is endorsed by the vast majority of clinicians, but the awareness that this would require a comprehensive assessment of the patient, beyond the mere diagnosis, is not equally shared, and personalization of management is actually lacking or inadequate in most clinical contexts worldwide 12 .
Finally, although many mental health services would declare themselves “recovery‐oriented”, in practice a resilience‐promoting environment is rarely provided, and a focus on the skills that people with primary psychosis need to learn in order to live a fulfilling life despite persistent disabilities is not common 13 .
The present paper, which has been produced in parallel with a similar one focusing on depression 14 , aims to address the situation we have just described. Its main objectives are: a) to reinforce the emerging awareness of the need to personalize the management of patients with primary psychosis, taking into account all the available treatment modalities whose efficacy is supported by research evidence; b) to help in the identification of the salient domains to be considered in the characterization of the individual patient with primary psychosis aimed at personalization of management (see Table 1); c) to help in the selection of simple assessment instruments that can already be considered for use in clinical practice today, and can be included in comprehensive batteries of measures to be tested in large observational studies in order to guide the development of standardized decision tools 15 ; and d) to encourage a clinical practice that is recovery‐oriented as well as evidence‐based.
Table 1.
Salient domains to be considered in the clinical characterization of a patient with a diagnosis of primary psychosis
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
On the basis of the above discussion, we will preferentially use the expression “primary psychosis” throughout the paper, except in those cases in which the available research evidence specifically refers to patients with a post‐DSM‐III diagnosis of schizophrenia.
We are fully aware that a significant effort is ongoing to identify biological measures or markers that may help in the personalization of the management plan in patients with primary psychosis. However, since none of these measures or markers is currently ready for use in clinical practice, we do not consider them in this paper. On the other hand, we do believe that biological research can benefit from a systematic characterization of patients with primary psychosis, since this is likely to facilitate the identification of more homogeneous subtypes within this group of disorders.
POSITIVE DIMENSION
The conceptualization of the positive dimension as the core of primary psychosis has continuously evolved over the last four decades. There is common agreement that this dimension includes delusions (persistent false beliefs based on an incorrect inference about reality, that are firmly maintained despite obvious contrary evidence, and are not shared by others with a similar cultural background) and hallucinations (perception‐like experiences with the clarity and impact of a true perception but without the external stimulation of the relevant sensory organ). Other symptoms – i.e., disorganized thinking (covered in another section of this paper) and self‐disturbances – are sometimes regarded as part of this dimension.
Self‐disturbances are alterations in the sense of self as the subject of one’s experience and agent of one's actions 16 . They have been hypothesized by some authors to represent the “core Gestalt” of schizophrenia 17 . Empirically, there is evidence for the validity and relevance of self‐disturbances from studies using the Examination of Anomalous Self‐Experience (EASE) 18 : EASE scores are increased in people with a diagnosis of schizophrenia compared to those with other mental disorders 19 . Anomalous self‐experiences have been reported to be among the most common symptoms in the prodromal phase of primary psychosis, and scores on the Inventory of Psychotic‐Like Anomalous Self‐Experiences (IPASE)20, 21, a self‐report measure of minimal self‐disturbances, have been found to correlate with those for subclinical positive symptoms as assessed by the Comprehensive Assessment of At Risk Mental States (CAARMS) 22 and the Community Assessment of Psychic Experiences (CAPE) 23 .
In the ICD‐112 (but not in the DSM‐5 1 ), “experiences of influence, passivity or control” are regarded as a separate symptom from delusions. If these experiences are explained in a delusional manner, then the presence of both these experiences and delusions should be recorded.
The ICD‐11 and DSM‐5 provide a dimensional assessment of positive symptoms beyond the categorical classification. The ICD‐11 enables clinicians to indicate the severity of positive symptoms in patients with primary psychosis using a symptom qualifier, with scores ranging from “0 ‐ not present” to “3 ‐ present and severe”, based on patient report or observer rating during the last week. This qualifier combines hallucinations, delusions, disorganized thinking and behavior, and experiences of influence, passivity and control to an overall score indicating the severity of the positive dimension. The ICD‐11 also specifies degrees of severity for each of those four symptoms. The DSM‐5 contains dimensions of psychosis symptom severity covering hallucinations, delusions and disorganized speech (each rated on a 5‐point scale). These measures help to improve clinical decision‐making beyond the diagnostic categories and allow the monitoring of course and outcome.
The positive scale of the Positive and Negative Syndrome Scale (PANSS) 24 is the most widely used instrument for the assessment of positive symptoms. The PANSS allows clinicians to rate the severity of seven positive symptoms (delusions, conceptual disorganization, hallucinations, excitement, grandiosity, suspiciousness/persecution, and hostility), each on a 7‐point scale ranging from “1 ‐symptom not at all present” to “7 ‐ symptom extremely severe”. For these ratings, information from a clinical interview and, if available, other sources (e.g., family members) is used. There is a large body of evidence indicating good reliability, validity and sensitivity of the PANSS 25 , which is available in several languages. However, the scale contains items that are not clearly part of the positive dimension of primary psychosis (e.g., hostility and excitement).
The PANSS‐6 26 , an abbreviated version of the PANSS that could be more suitable for use in routine clinical practice, contains a subscale including three items that refer to the positive dimension of primary psychosis: delusions, hallucinations and conceptual disorganization.
Across different instruments and classification systems, clinicians should resort to different sources of information to assess positive symptoms in primary psychosis (i.e., self‐report, clinical observations, information provided by care staff or family members). Integrating these sources is particularly necessary when information about longer time periods is required (e.g., to assess whether a person meets the time criterion of six months for schizophrenia according to the DSM‐5).
Depending on the illness stage, people with primary psychosis are usually able to reliably report positive symptoms 27 . The assessment of these symptoms may be more problematic in patients lacking insight, where it can be facilitated by the technique of “Socratic questioning” 28 , a form of cooperative argumentative dialogue based on asking and answering questions to stimulate critical thinking and to draw out ideas and underlying presuppositions.
The presence of positive symptoms has immediate consequences for an integrated management plan. On the pharmacological side, antipsychotic drug treatment is strongly recommended for people with acute positive symptoms. Although there may be differences among the various antipsychotic drugs regarding their efficacy on positive symptoms 29 , these are not sufficiently clear to guide the clinician’s choice in the individual case, which is usually based essentially on issues concerning possible side effects. The assessment of the severity of positive symptoms over time, using one of the above‐mentioned tools, is crucial to monitor their evolution and to lead, if treatment resistance emerges 30 , to the prescription of clozapine.
In patients with a diagnosis of schizophrenia, antipsychotic maintenance treatment (i.e., continuous treatment with the lowest effective dose of oral or long‐acting antipsychotic medication) is recommended to prevent relapse 31 , although there is not a consensus about how long this treatment should be continued32, 33, due to the lack of randomized controlled trials beyond the second year following the first psychotic episode.
Particularly in acute stages with limited judgement, delusional loss of reality control, and lack of coping with everyday life, positive symptoms may require inpatient care. Close monitoring of positive symptoms and a corresponding adjustment of medication or inpatient admission is always required, in the framework of a person‐oriented, individualized and human‐rights respecting approach of evidence‐based treatment and care.
CBT, in addition to antipsychotic medication, can produce further improvement in positive symptomatology for people with primary psychosis 7 . Considering the type and severity of positive symptoms is crucial to tailor the psychotherapeutic approach accordingly, for example in the presence of disorganized thinking 34 . There are also effective psychotherapeutic interventions for specific positive symptoms (e.g., cognitive therapy for command hallucinations) 35 . Family interventions, including illness education and crisis intervention, can lower the levels of distress and burden associated with positive symptoms in primary psychosis 9 .
Positive symptoms have been reported to be associated with cognitive biases, which can be addressed in psychoeducation and may be targeted in CBT. The Cognitive Biases Questionnaire for psychosis (CBQp) 36 measures five specific cognitive biases: jumping‐to‐conclusions (making firm decisions based on little evidence), intentionalizing (interpreting events or behaviors as deliberate), catastrophizing (worst‐case‐scenario thinking), emotional reasoning, and dichotomous (i.e., “black or white”) thinking.
NEGATIVE DIMENSION
Negative symptoms have long been conceptualized as a core aspect of primary psychosis, especially schizophrenia37, 38, and their treatment is increasingly recognized as an important unmet need. They play a key role in the functional outcome of the disorder39, 40, and largely contribute to the burden that the disorder poses on affected people, their relatives and the society 41 . Unfortunately, so far, most available treatments have shown a limited impact on these symptoms, especially when they are primary and persistent.
According to recent studies and expert opinions41, 42, 43, 44, negative symptoms include five domains, also known as the 5 As: affective blunting, alogia, asociality, anhedonia and avolition.
Affective blunting, more often referred to as blunted affect, is a reduction in the expression of emotion and reactivity to events. It is assessed during the clinical interview by inspecting spontaneous or elicited changes in facial and vocal expressions, as well as the amount of expressive gestures. In the assessment of blunted affect, clinicians should avoid a quite common mistake, i.e. the tendency to include the subjective experience of decreased emotional range or a general decrease in spontaneous movements, as these aspects are non‐specific and more relevant to depression.
Alogia refers to a reduction in the quantity of spoken words and the amount of information spontaneously given when answering a question. The person with alogia provides very short answers, with few words strictly needed to answer the question. The poverty of content of speech in the presence of a normal quantity of spoken words is not included in the alogia construct, but is part of the disorganization dimension.
Asociality is a reduction in social interactions and initiative due to indifference or lack of desire for them. The clinician should investigate both the behavioral aspect (e.g., the reduction of interpersonal relationships) and the decreased interest in social bonds.
Anhedonia should be further characterized as consummatory or anticipatory. The former is a reduction in the experience of pleasure during pleasurable activities. The latter involves a reduction in the anticipation of pleasure for future pleasurable activities.
Avolition, also referred to as amotivation or apathy, refers to a poor engagement in any activity due to a lack of interest and motivation. It is important that the examiner evaluates both subject’s behavior and internal experience. The clinician can be confident about the presence of avolition when behavior shows poor engagement in activities and the subject does not miss or feel the need to participate in those activities.
From a clinical standpoint, it is important to distinguish primary from secondary negative symptoms. Currently, this distinction remains a major challenge. Suggestions provided hereafter are meant to support clinicians in this effort.
Primary negative symptoms are supposed to stem from the pathophysiological process underlying psychosis. They are often persistent across the different stages of the disorder 45 , and do not show a substantial improvement with most treatments available so far. The only head‐to‐head study supporting the superiority of an antipsychotic drug to treat primary negative symptoms compared cariprazine with risperidone and found the former to be more effective 46 . However, the study was sponsored by the manufacturer and no independent replication is available so far. Results provided by trials exploring the efficacy of drugs with mechanisms different from D2 antagonism or D2/D3 partial agonism (e.g., glutamatergic or dopamine agonists) remain inconclusive 41 .
When signs and symptoms resembling negative symptoms are due to other illness dimensions, in particular positive symptoms, depression, extrapyramidal symptoms, sedation, environmental deprivation, or substance use, they are referred to as secondary negative symptoms. In this case, they can improve when the underlying factors are correctly identified and adequately treated.
In case of negative symptoms secondary to positive symptoms, patients may be reluctant to talk and interact with the examiner. They (or others) may report an asocial behavior due to persecutory delusions and/or difficulties in initiating and persisting in goal‐directed activities due to engagement in delusional thinking or abnormal perceptions. If this is the case, clinicians should treat positive symptoms aiming at their remission, by using adequate doses of antipsychotics, improving adherence to treatment, and prescribing clozapine in case of failure with at least two other antipsychotics. When treatment leads to an improvement of psychotic symptoms, negative symptoms often improve as well.
Depression may also underlie secondary negative symptoms, such as a reduced range of emotional expression, diminished amount of speech, social withdrawal, anhedonia and lack of motivation. The co‐occurrence of sadness, feelings of guilt, and suicidal ideation or attempts strongly suggests that these features are due to depression. In this case, treatment with second‐generation antipsychotics should be preferred to first‐generation medications, which could worsen depression, and add‐on treatment with antidepressants should be considered.
Side effects of antipsychotic drugs, in particular high doses of first‐generation antipsychotics, may also produce secondary negative symptoms: akinesia or bradykinesia, for instance, can result in reduced expression and amotivation, due to reduced dopaminergic transmission. The presence of other extrapyramidal side effects (tremor or rigidity, gate instability) can confirm this interpretation and indicate the need to reduce the doses or change the class of antipsychotics (e.g., switching from first‐ to second‐generation drugs or to a D2/D3 partial agonist).
Among non‐pharmacological interventions for negative symptoms, preliminary evidence of beneficial effects of social skills training, CBT and cognitive training is available. In particular, there is evidence of superior efficacy of social skills training vs. treatment as usual and active comparators47, 48. The evidence for CBT is weaker, and trials in large samples of patients with severe negative symptoms, based on CBT approaches specific for those symptoms, are needed47, 49. Cognitive training, although primarily aimed to treat cognitive dysfunctions, seems to have small to moderate beneficial effects on negative symptoms too 50 . However, a certain degree of overlap between cognitive dysfunctions and negative symptoms does remain, and makes it difficult to draw clear conclusions on the efficacy of this intervention for negative symptoms.
Available evidence also suggests that repetitive transcranial magnetic stimulation (rTMS) of the left prefrontal region may possibly be an effective treatment for patients with negative symptoms that do not improve with other interventions 51 .
The relevance of the above non‐pharmacological treatments to primary and persistent negative symptoms remains to be tested in controlled trials.
The most widely used instruments for the assessment of negative symptoms are the PANSS 24 and the Scale for the Assessment of Negative Symptoms (SANS) 52 . However, the use of these tools is problematic, due to the inappropriate inclusion of symptoms that are not relevant to the negative dimension (e.g., difficulty in abstract thinking and stereotyped thinking in the PANSS).
Two state‐of‐the‐art instruments, the Brief Negative Symptom Scale (BNSS) 53 and the Comprehensive Assessment of Negative Symptoms (CAINS) 54 , are increasingly used in research settings, but unfortunately their dissemination to clinical practice is still limited. Neither scale contains irrelevant items; both focus on inner experience in addition to behavioral aspects, and allow the assessment of anticipatory and consummatory anhedonia. For both instruments, training is advisable and can be conducted online.
The BNSS consists of 13 items covering the five domains of blunted affect, alogia, asociality, anhedonia and avolition. The scale has been found to have an excellent inter‐rater and test‐retest reliability and a strong internal consistency 53 . The CAINS also has 13 items, loading on two modestly correlated subscales: expression and motivation/pleasure. The former has been found to be related to independent living and family functioning, while the latter has been related to all aspects of functioning. The inter‐rater and test‐retest reliability of the tool has been documented 54 .
Clinicians often express the desire for an instrument specifically designed for clinical assessment, and taking less time than either BNSS (about 20 min) or CAINS (about 35 min). Unfortunately, for the time being, no tool is available that provides an accurate and at the same time shorter assessment of negative symptoms.
OTHER PSYCHOPATHOLOGICAL COMPONENTS
Psychopathological components of primary psychosis other than positive and negative symptoms include disorganization, motor disturbances, mood states, and lack of insight.
The disorganization component of primary psychosis comprises positive formal thought disorders (thought disorganization), bizarre behavior, and inappropriate affect. From a network perspective, disorganization has been reported to be the most central and interconnected domain of psychotic disorders 55 . It is strongly related to neurocognition and represents an integral link in cognitive pathways 56 , although this association may be due to some conceptual overlap with neuropsychological constructs such as abstraction and attention. Formal thought disorders appear to be the psychotic symptoms whose contribution to everyday functioning is most significant 57 .
There is a lack of specific instruments for assessing the various subcomponents of disorganization, yet they can be reliably derived from wide‐ranging scales such as the Comprehensive Assessment of Symptoms and History (CASH) 58 and the Manual for Assessment and Documentation of Psychopathology (AMDP) 59 . Formal thought disorders, the core manifestations of disorganization, are reliably evaluated by the positive formal thought disorder subscale from the CASH and, more comprehensively, by the Thought, Language and Communication (TLC) rating scale 60 .
Disorganization symptoms tend to co‐vary with positive symptoms during acute psychotic episodes, and with negative symptoms in chronic schizophrenia. There is no specific pharmacological treatment for these symptoms, although they respond well to antipsychotic medication during the acute phases of primary psychosis. In chronic stages, disorganization symptoms appear to be better addressed by psychosocial rehabilitation programs, although controlled trials thereof are lacking.
Motor abnormalities comprise a broad array of manifestations that are usually subdivided into two overlapping subdomains: catatonia and extrapyramidal signs (EPS). EPS are usually linked with side effects of antipsychotics; however, they may also be an indigenous feature of primary psychosis, the so‐called spontaneous EPS, which are tied to the underlying pathophysiology of the illness. Spontaneous EPS are observed in 15‐25% of drug‐naïve subjects with schizophrenia spectrum disorders; hence, it would be useful to assess motor abnormalities before and after starting antipsychotic medication, to disentangle their primary or secondary origin. Such a differentiation, however, may be challenging even for experienced clinicians. Currently, a balanced view of motor signs in subjects on antipsychotics is that they result from an interaction between medication and illness‐related factors 61 .
Motor signs are poorly represented in the assessment instruments for psychosis; thus, it is necessary to make use of specific tools. For catatonia, the Bush‐Francis Catatonia Rating Scale 62 is preferred for routine use, because of its validity, reliability and ease of administration. For dyskinesia and parkinsonism, the most commonly used instruments are the Abnormal Involuntary Movement Scale 63 and the Simpson‐Angus Scale 64 , respectively. The St. Hans Rating Scale for Extrapyramidal Syndromes 65 rates comprehensively all EPS, including dyskinesia, parkinsonism, akathisia and dystonia.
Acute and severe catatonia is best managed using electroconvulsive therapy, although less severe catatonia symptoms may respond to benzodiazepines or second‐generation antipsychotics. Established drug‐induced EPS should be managed by reducing or changing antipsychotic medication, particularly in subjects treated with first‐generation antipsychotics. In this regard, clozapine and quetiapine are among the second‐generation antipsychotics with the lowest risk of producing neurological side effects 66 .
Major mood symptoms are found in about 30% of cases of primary psychosis during an index episode, and their prevalence rate reaches 70% when lifetime mood ratings are considered 67 .
A frequent diagnostic problem during an acute episode is the differentiation between mood disorders with psychotic features and primary psychosis 68 . In this regard, examining the temporal pattern of the association between psychotic and mood syndromes, and using specific mood rating scales that do not include psychotic symptoms, are highly desirable. The Calgary Depression Scale for Schizophrenia 69 is the best option for assessing depression in the context of psychotic symptoms. Unfortunately, a similar instrument does not exist for mania, since all available mania rating scales also include psychotic symptoms to some degree. The mania subscale from the CASH 58 may be reliably used. The relevance of mood symptoms for the management plan in primary psychosis is discussed elsewhere in this paper.
Lack of insight is a hallmark feature of primary psychosis, entailing three relatively overlapping subcomponents: awareness of symptoms, awareness of illness, and collaboration with treatment. Poor insight is strongly related to reality distortion and disorganization symptoms; in contrast, higher cognitive ability and depressive symptoms are associated with better insight. Poor insight has important clinical and management implications, since it is associated with a number of interrelated factors, including longer duration of untreated psychosis, poor collaboration with treatment, and aggressiveness, all of which result in poor outcomes 70 .
The standard instrument for assessing clinical insight is the Scale to Assess Unawareness of Mental Disorder 71 . This scale, however, may be too time‐consuming for use in routine clinical practice. An alternative option is to use the three AMDP 59 items covering the insight domains referred to above.
Recently, a distinction has been made between clinical insight and cognitive insight, the latter describing the subject’s flexibility towards his/her beliefs, judgments and experiences. The self‐report Beck Cognitive Insight Scale 72 examines two subcomponents of cognitive insight: self‐certainty (i.e., overconfidence in the validity of one's beliefs) and self‐reflectiveness (i.e., capacity and willingness to observe one's mental productions and to consider alternative explanations). These two distinct but related aspects of cognitive insight in psychosis appear to be differentially associated with clinical insight, symptoms and functioning.
During an acute episode, improvement of insight co‐varies with improvement of psychotic symptoms. However, in a substantial proportion of subjects with chronic schizophrenia, lack of insight may represent a major therapeutic challenge. Insight‐focused CBT is often recommended, although research findings are conflicting about its efficacy. Metacognitive reflection and insight therapy (MERIT), an individual psychotherapy seeking to enhance the reflective capacity necessary for people who have experienced severe mental illness to form a complex and integrated sense of self and others, has been proposed as an alternative 70 .
Depressive symptoms and the presence of insight are associated with a higher risk for suicide in patients with primary psychosis. Being young, male and with a high level of education, prior suicide attempts, active hallucinations and delusions, a family history of suicide, and comorbid substance abuse are also positively associated with later suicide, while the only consistent protective factor is delivery of and adherence to effective treatment 73 . The Columbia‐Suicide Severity Rating Scale 74 is a validated tool for the assessment of suicide risk, whose administration requires a specific training that is available online.
Sleep disturbances, in particular insomnia, are common in persons with primary psychosis 75 , and can have a significant impact on their quality of life 76 . Their presence should be explored in the clinical characterization of the individual patient, because they can be targeted in CBT and considered in the choice of the antipsychotic medication. Furthermore, obstructive sleep apnea has been reported to be more frequent in these patients than in the general population, and can be related to the dosage of the antipsychotic medication 77 .
ONSET AND COURSE
The onset of primary psychosis usually occurs in adolescence or early adulthood 78 . On average, men are diagnosed in their late teens to early twenties, whilst women tend to get diagnosed in their late twenties to early thirties.
Onset of primary psychosis should be distinguished from the expression of premorbid developmental alterations in the domains of cognition, motor function and social adjustment. Follow‐back studies indicate that the first changes often involve affective and negative symptoms, appearing years before diagnosis. Positive symptoms emerge later and typically trigger contact with mental health services. Indicators of social disability appear 2‐4 years before onset. Cannabis use is associated with an earlier onset of psychosis.
Onset can be considered as a three‐stage process, consisting of: a) a prodrome, in which a period of non‐specific “unease” precedes “non‐diagnostic” symptoms in the form of disturbances of perceptions, beliefs, cognition, affect and behavior; b) first expression of psychotic symptoms; and c) increase in characteristic symptoms resulting in a definite diagnosis. The prodrome can be absent or not identifiable in several patients.
The Nottingham Onset Schedule (NOS) is a short guided interview and rating schedule to assess onset in psychosis, defined as the time between the first changes in mental state and behavior to the appearance of psychotic symptoms 79 . Other instruments providing comparable onset assessment are the CASH 58 and the Symptom Onset in Schizophrenia (SOS) inventory 80 .
The International Pilot Study of Schizophrenia 81 categorized mode of onset into three groups: a) acute (psychotic symptoms appear within hours, one week or one month since first noticeable behavioral change); b) gradual (psychotic symptoms appear within one to six months since first noticeable behavioral change); and c) insidious (psychotic symptoms appear incrementally over a period of six months or greater since first noticeable behavioral change). There is some evidence that the insidious mode of onset is associated with poorer and the acute onset with better outcome.
The course of primary psychosis after onset is highly variable both within and between patients. There is a broad range of possible course patterns, ranging from complete recovery to continuous unremitting psychopathology, cognitive alterations and social disability. Between such extremes, a substantial number of patients present with multiple episodes of psychosis interspersed with partial remission 82 . On average, within the primary psychosis syndrome, patients with a diagnosis of schizophrenia have the poorest outcome, with schizoaffective patients occupying an intermediate position between schizophrenia and affective psychosis 83 . Patients diagnosed using a broad definition of schizophrenia generally have better outcomes than those diagnosed with narrowly defined (post‐DSM‐III) schizophrenia.
The Life Chart Schedule 84 was designed to assess the course of psychotic disorder in four key domains (symptoms, treatment, residence and work) over several time periods. Course type can be rated as episodic (no episode longer than six months), continuous (no remission longer than six months), neither episodic nor continuous, and not psychotic in this period. Type of remission can be coded as “mainly complete”, “mainly incomplete” and “mixed”. A “usual severity of symptoms” rating is made to indicate the symptomatic level of the patient during most of the period under observation. Ratings are “severe”, “moderate”, “mild” and “recovered”. The amount of time spent in a psychotic state is also rated, as are parasuicidal acts and instances of assault. A rating is also given as to whether there was clear evidence of negative symptoms over the period under observation. In addition, the life chart rates the proportion of the period spent unemployed (time in institutions not counted; full‐time students and housewives rated as employed), living independently, in hospital, in prison, or without accommodation. In addition, treatment variables over time (hospitalization, use of antipsychotic medication, other interventions) are recorded.
In a given patient with a given length of illness, the assessment of preceding course is essential, because it allows for the formation of hypotheses about the effectiveness of treatment across different outcome domains to date. The first five years of the illness are considered “critical”, referring to the hypothesis that early energetic treatment may causally impact on the later course of the syndrome. After the first episode, around 90% of patients will experience a remission of symptoms. After five years, however, 80% will have experienced one or more relapses. With each episode, a small proportion of patients will develop a continuous illness course, displaying a mix of persistent positive and negative symptoms, cognitive difficulties and catatonia. Over the course of five years, around 40% of patients with primary psychosis can be expected to show “good” outcome (with 15% showing complete recovery), 20% “poor” outcome, and 40% “intermediate” outcome 85 . Thus, assessment of course to date is necessary to place the patient at the right position on dimensions of illness episodicity and inter‐episode recoverability, thus informing continued clinical management.
After the first ten years after onset, the illness course tends to plateau. Cross‐sectional outcome measures of psychopathology do not differ substantially according to study duration, suggesting that there is no clear pattern of deterioration or “progression”, although this may occur in a subgroup of patients. Careful assessment of course over time in a patient with long duration of illness can reveal signs of progression and possible reasons thereof.
Course and outcome cannot be defined unidimensionally. For patients, the most important outcome, apart from societal participation (education, work, housing, relationships), is restoration of perspective, in the sense of feeling that life is meaningful and worth living (existential recovery) 86 . The Recovery Assessment Scale can be used to evaluate the course of existential recovery over the period preceding the assessment 87 . This evaluation is essential, as it provides information on the causes of variation and the possible role of the health system herein, including unintended iatrogenic hopelessness, antipsychotic polypharmacy, and post‐traumatic stress after admission. These may be counteracted by facilitating peer‐supported interventions focusing on hope, connectedness, identity, meaning and empowerment.
Over time, patients (and their environment) learn about their mental vulnerability, the relativity of formal diagnosis, the limitations of treatment, the gaps in knowledge, and the weak spots in local service provision. As a result, they become more involved in and opinionated about treatment and services 88 , so that the process of shared decision‐making becomes even more essential. It is therefore important to assess, before planning the clinical management, the preceding course of decision‐making about diagnosis and treatment, and the experience to date in being able to experiment with dosing and even discontinuation of antipsychotic treatment, to engage in alternative therapies and in general to take risks in pursuit of life goals.
In order to be able to deal with an intense mental vulnerability, characterized by an often unpredictable waxing and waning expression over time, a long‐term therapeutic relationship of trust and mutual commitment is essential. Assessment of course, therefore, should include the quality and level of therapeutic continuity over time, and its impact on outcome to date.
NEUROCOGNITION
Neurocognitive alterations have been identified as a key component of schizophrenia since the clinical observations of Bleuler and Kraepelin, but they have gained much more clinical and research attention in recent years3, 89. These alterations are present in many cases years before the first psychotic episode 90 , persist into clinical remission 91 , and may be present in a milder form in first‐degree relatives of patients 92 .
As the role of neurocognitive alterations in predicting and influencing everyday functioning in people with schizophrenia became more widely recognized 93 , the US National Institute of Mental Health promoted the development of a consensus on the major dimensions of this neurocognitive impairment, their measurement in clinical trials, and the design of trials to evaluate potential treatments 94 . This initiative, Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS), led to the identification of seven major dimensions: speed of processing, attention/vigilance, working memory, verbal learning and memory, visual learning and memory, reasoning and problem solving, and verbal comprehension 95 .
Speed of processing refers to the speed with which simple perceptual and motor tasks can be performed, which is believed to reflect the pace of cognitive processing. Attention/vigilance refers to sustaining a focus on relevant information over a prolonged period of time. Working memory involves temporary maintenance and manipulation of information in consciousness, usually over a few seconds. Verbal learning and memory refers to the initial encoding and later recognition and recall of words and other information involving language. Visual learning and memory involves similar encoding, recognition and recall processes for visuospatial information such as shape, color, spatial orientation, and movement.
Reasoning and problem solving refers to processes of strategic and logical thinking, planning, formation and maintenance of goals, and coordinating these processes flexibly over time. Reasoning and problem‐solving abilities are sometimes also called executive processes. Finally, verbal comprehension refers to verbal information that is accumulated over many years and stored in a widely distributed neural network, such as vocabulary and common shared information in a culture.
While all of these dimensions are impaired in schizophrenia, the MATRICS Neurocognition Committee concluded that verbal comprehension is not likely to be impacted to a notable degree by pharmacological or psychosocial interventions and is therefore less relevant as a focus for clinical trial or clinical practice assessment.
The typical person with a post‐DSM‐III diagnosis of schizophrenia scores between 0.75 and 2.00 standard deviations below community samples of similar age and gender on each of these neurocognitive domains 96 , which corresponds to a percentile between 2% and 24%. Thus, the cognitive alterations, on average, are large and generalized across cognitive domains, with perhaps larger alterations in speed of processing than in other domains 97 . While the overall picture is one of a generalized impairment across neurocognitive domains, there is also notable heterogeneity in the profile of alterations from one patient to the next, which may to some extent also be due to a different impact of interfering factors such as disturbances in motivation and emotion3, 98. The variability in neurocognitive performance is likely to be even higher in patients fulfilling the broader ICD‐10/ICD‐11 definition of schizophrenia and in those with ICD‐10/ICD‐11 “other primary psychotic disorder”, although no research evidence is available in this respect. The clinical importance of these domains of neurocognitive impairment is very clear, as each one is significantly related to the level of work/school and social recovery that a patient is able to achieve99, 100.
In clinical practice, the options for assessing neurocognitive alterations fall into three categories: comprehensive cognitive performance assessment, brief cognitive performance assessment, and interview‐based measures of cognition.
Comprehensive cognitive performance assessment batteries allow the clinician to identify the individual profile across the six neurocognitive domains, and to plan tailored interventions and clinical management accordingly. The MATRICS Consensus Cognitive Battery (MCCB) was developed through a systematic expert consensus process, and measures each of the domains with tests that are reliable, repeatable and sensitive to change 101 . It requires about 65 min to administer and yields standardized scores for each cognitive domain and for a neurocognitive composite across domains 102 . Other well‐developed comprehensive batteries include the Cambridge Neuropsychological Test Automated Battery (CANTAB) 103 and the CogState 104 , both of which consist of reliable, repeatable measures of most or all MATRICS neurocognitive domains.
The disadvantages of these comprehensive batteries for clinical practice are that they are relatively lengthy and require adequate professional training for administration and interpretation. An alternative would be to complete one of these batteries at initial assessment and then choose one to three of their tests for tracking change based on the initial profile of neurocognitive alterations.
Brief cognitive performance assessments have the advantage of being less time‐consuming, while still allowing changes in at least overall cognitive performance to be evaluated over time. The Brief Assessment of Cognition in Schizophrenia (BACS) 105 involves six tests and 35 min for administration, while the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) 106 covers five cognitive domains in about 30 min. Both yield reliable and valid measures of global cognitive functioning that correlate well with overall scores from comprehensive batteries, as well as some information about the pattern of alterations.
Even shorter cognitive screening measures include the 15‐min Brief Cognitive Assessment 107 and the 10‐min Brief Cognitive Assessment Tool for Schizophrenia (B‐CATS) 108 . Both of these brief tools yield a global cognitive score that correlates well with comprehensive battery composite scores, but they do not allow any pattern of alterations to be evaluated. All of these measures still require professional training, but less than the comprehensive batteries.
Finally, interview‐based measures of cognition are intuitively attractive for ordinary practice, as clinicians are accustomed to interview formats and can more easily adapt to their administration. The Cognitive Assessment Interview (CAI) 109 requires 15 min to administer, and has high test‐retest reliability and moderate relationships to performance‐based cognitive measures and everyday functioning. The Schizophrenia Cognition Rating Scale (SCoRS) 110 also takes about 15 min per interview, has good test‐retest reliability, and moderate relationships with cognitive performance measures and everyday functioning. The SCoRS yields stronger relationships when an informant is used rather than solely a patient interview.
Both these interview‐based measures of cognition require some training. While both yield an overall cognitive score, the relationship of these scores to cognitive performance measures is weaker than the interrelationship of cognitive performance measures to each other. They also do not provide a reliable pattern of alterations across cognitive domains.
Given the clear influence of neurocognitive alterations on everyday functioning in primary psychosis, the importance of treatment plans that address these alterations is increasingly recognized. Although attempts to develop cognition‐enhancing adjunctive medications have promise for the future, so far cognitive remediation 111 , aerobic exercise 112 , and perhaps their combination 113 are most relevant for clinical practice.
Aerobic exercise has thus far been shown to improve overall neurocognition and specifically attention/vigilance and working memory 112 . Cognitive remediation produces moderate gains in overall cognition and several cognitive domains, with larger neurocognitive and everyday functioning improvements being achieved when it is implemented in the context of active rehabilitation programs 111 . Emerging evidence indicates that forms of cognitive remediation that emphasize perceptual processes vs. higher‐level executive processes impact on different neurophysiological mechanisms 114 . Furthermore, perceptual training may be beneficial only for patients with initial perceptual processing impairments 115 .
Thus, beyond assessment of the level of overall cognitive impairment, identifying neurocognitive domains with particularly severe alterations is becoming of increasing importance in the clinical characterization of the patient with primary psychosis.
SOCIAL COGNITION
Social cognition refers to mental operations needed to perceive, interpret and process information for adaptive social interactions. The term encompasses a very broad range of domains. In the context of primary psychosis, most of the attention has focused on four aspects of social cognition: emotion identification, mentalizing, social perception, and attributional bias3, 116.
Emotion identification includes one’s ability to perceive emotion in faces, voice intonation, gestures or gait. Mentalizing refers to the ability to infer intentions or beliefs of others, such as whether they are being sincere, sarcastic or deceptive. Social perception refers to the ability to identify social roles, social rules and social contexts from various cues. Individuals with a post‐DSM‐III diagnosis of schizophrenia have alterations on all three of these aspects of social cognition based on performance‐based measures 117 , although this notion may not be generalizable to all patients fulfilling the broader ICD‐11 definition of schizophrenia or to those with ICD‐11 “other primary psychotic disorder”.
Attributional bias refers to how individuals typically infer the causes of particular positive and negative events (e.g., having a tendency to attribute hostile intentions to others). Unlike the other social cognitive areas, people with schizophrenia do not consistently show differences in attributional bias compared with healthy individuals117, 118.
Social cognition is relevant to the management of primary psychosis because it is associated with functional outcome 100 . Consistent associations between social cognitive domains and community functioning have been reported in schizophrenia, with mentalizing showing the strongest relationship in one meta‐analysis 100 . Further, social cognition explained more variance in community functioning than did nonsocial cognition (16% vs. 6%). Thus, social cognition is a key correlate and determinant of functional outcome in primary psychosis, and can help clinicians to form realistic expectations for how the individual patient might integrate in the community, or how much additional support he/she may need to do so.
Given its relevance for functional outcome, there have been considerable efforts, and some encouraging progress, in developing psychosocial training interventions for social cognition in primary psychosis. These interventions are typically interactive and group‐based, and include a variety of visual, auditory and video stimuli depicting social stimuli. Recently, individual computerized interventions have also been developed 119 . One meta‐analysis of 16 studies 120 found improvements of large effect sizes in facial affect identification (d=.84), mentalizing (d=.70), and social perception (d=1.29). The impact of these interventions on functional outcome has been encouraging, though not consistent across studies 121 .
Beyond psychosocial training interventions, there are considerable efforts to examine the impact of intranasal oxytocin (using single or repeated administration strategies) on social cognitive tasks. Here, however, the results in patients with a diagnosis of schizophrenia have been mixed, with both positive and negative findings 122 . Another approach has been to examine oxytocin as an augmentation during social cognitive training programs, and again the results have been mixed 123 .
Measurement of social cognition in primary psychosis has been a daunting challenge. The measurement problems apply to both clinical trials and ordinary practice. Regarding clinical trials, there is no consensus on a battery of social cognition outcome measures, or even a set of social cognitive domains. A highly diverse range of outcome measures have been used in treatment studies, and they often have poor or unknown psychometric properties.
Considering the lack of psychometric information on potential social cognitive endpoints for clinical trials of psychosis, the US National Institute of Mental Health supported two method‐development projects. One project focused on evaluation of social cognitive measures that were in current use in psychopathology 124 , while the other adapted measures from social neuroscience and evaluated their application to people with psychosis 125 . Both projects produced a rich data set and a series of recommendations for endpoints in clinical trials. Despite these efforts, there is no widely‐used battery for measurement of social cognition in clinical trials.
The absence of such standardization means that results from trials vary depending on the specific outcome measure 126 . For example, the majority of studies that found treatment effects for mentalizing used very simple tasks or questionnaires. However, a more challenging and ecologically valid test is The Awareness of Social Inference Test (TASIT) 127 , which has good psychometric properties. This test uses video vignettes, and participants are asked to detect lies and sarcasm. Studies using this test have generally failed to find treatment effects. A similar pattern was seen for the domain of social perception. If more challenging and psychometrically stronger measures tend to show smaller or negative findings, this raises questions about the strength of treatment effects for certain domains.
In contrast, other aspects of social cognition, such as facial affect perception, show treatment effects regardless of the specific outcome measure. Attributional bias presents a different measurement issue: there are very few available measures for this domain, and the current ones do not have strong psychometric properties 124 .
The situation for the assessment of social cognition in clinical practice is similarly problematic. In contrast to nonsocial cognition, social cognition does not have a long history of clinical evaluation with standardized and highly reliable measures. Partly due to this historical lack of emphasis, it is rarely evaluated in routine cognitive or neuropsychological assessments.
This situation is going to change. Some innovative and interpretable tests of emotion processing are emerging, including an emotion processing battery with a large normative sample, the Mayer‐Salovey‐Caruso Emotional Intelligence Test (MSCEIT) 128 . Also, some social cognitive domains lend themselves to brief assessments that do not require expertise in test administration. For example, there are a large number of tests for facial or vocal emotion perception that are easy to administer and do not depend on language (i.e., could be used cross‐nationally) 129 .
Nonetheless, at the current time, measurement remains the Achilles’ heel of social cognition. Social cognition is an important and functionally meaningful aspect in primary psychosis, but it has not yet moved into broad clinical application.
NEURODEVELOPMENTAL INDICATORS
The neurodevelopmental understanding of primary psychosis has evolved along the decades, from Kraepelin’s remarks 130 on the developmental differences in children who as adults would manifest dementia praecox; to the contributions of Fish 131 , who recognized a continuity between infant development and risk of early psychosis; Weinberger 132 , who postulated an early genetic or environmental insult to the developing brain interacting with normal adolescent development; and Murray and Lewis 133 , who proposed a subtype of schizophrenia being a long‐term sequela of obstetric injury.
Subsequently, evidence has accrued with epidemiological research using prospective information, particularly from birth cohorts and population registers, to support wide‐ranging manifestations of neurodevelopmental effects in primary psychosis. Indeed, the incidence of primary psychosis peaks between puberty and the mid‐twenties, an epoch of renewed grey and white matter changes and a sensitive period for psychosocial development.
Earlier neurodevelopmental indicators in primary psychosis are highly relevant to clinical practice. They include a history of delayed or reduced acquisition of early childhood motor and language skills, atypical age‐appropriate social interaction, and lower IQ and school attainment throughout childhood and adolescence134, 135, 136, 137. Furthermore, soft neurological signs have a prevalence of 50‐65% in people with a diagnosis of schizophrenia (compared with 5% in healthy controls) 138 . All these elements offer a window on neurodevelopment, as well as informing clinical management and prognosis.
Soft neurological signs include dysgraphaesthesia (the inability to recognize writing on the skin through touch alone), diminished motor coordination, and problems with complex motor sequencing (such as dysdiadochokinaesia, an impairment in rapid alternating movements). They also encompass persistence of infantile (primitive) reflexes such as the palmomental response (reflex contraction of the mentalis muscle leading to pouting of the lower lip when the palm is scratched), increased blink rate, and a positive glabellar tap (no habituation of blinking when the glabella is tapped).
Soft neurological signs are readily understandable in terms of distributed or circuit dysfunction rather than a localized lesion. They are present from early in development and most likely share the same underlying network‐based mechanisms as the pandysmaturation reported in genetically high‐risk children 139 and the early motor and language milestone delays seen more broadly in primary psychosis.
Minor physical anomalies (i.e., dysmorphic features representing subtle alterations in the development of somatic structures) have also been observed in some patients with a diagnosis of schizophrenia, with high‐arched palate being particularly common (20‐25% of patients) 140 .
Consideration of neurodevelopmental indicators is important in the clinical assessment of a patient with primary psychosis. Their presence helps to confirm the diagnosis where other phenomenology is scant (e.g., presentations with catatonia or mutism) or where a secondary psychosis is a realistic differential. They can be seen as direct precursors of negative symptoms such as alogia, affective blunting and asociality, and of cognitive alterations. These aspects are challenging to manage clinically, and presage poorer outcome.
The identification of neurodevelopmental markers may support a causal formulation in an individual patient, particularly where there has been obvious obstetric mishap or early trauma such as pre‐ or neonatal infection. They also illuminate an individual patient’s psychosocial life history whereby developmental differences from childhood peers is likely to have created an altered social microenvironment during development and a cascade of abnormal experiences 134 , something that needs accommodation in a management plan aiming at functional recovery.
It is also important to assess whether neurodevelopmental indicators are present to such an extent that an alternative diagnosis is more appropriate, such as psychotic phenomena in the context of an autistic spectrum disorder or a learning disability syndrome, particularly where the psychosis itself is similar to a primary syndrome 141 but is treatment resistant 142 . These classical neurodevelopmental disorders may remain undiagnosed into early adulthood and present atypically.
Further investigations, including evaluation by a clinical geneticist, may be required where there are multiple minor physical anomalies or when, collectively, they suggest a specific genetic condition such as velocardiofacial syndrome. Even where the observed picture does not meet diagnostic criteria for a neurodevelopmental disorder, advice from clinicians experienced in these fields can be useful, given the transdiagnostic occurrence of psychotic and neurodevelopmental features 143 .
The evaluation of soft neurological signs should be part of the full neurological examination required in every patient with primary psychosis 144 , but there are scales intended for both clinical and research practice that can be helpful. The Cambridge Neurological Inventory 145 was developed for the full range of psychiatric conditions and is applicable to primary psychosis. In this inventory, the second part focuses on soft sign examination (primitive reflexes, repetitive sequential motor execution, and sensory integration). The longer Neurological Evaluation Scale 146 focuses on schizophrenia. It includes 26 items, clustered into three subscales (sensory integration, motor coordination, and sequencing of complex motor acts).
The systematic assessment of childhood neurodevelopmental indicators presents a particular challenge in primary psychosis. Effects seen in research using prospective data may be subtle (standing, walking or speech delayed by four to six weeks) and would have been barely noticeable at the time, given the wide range of normal experience, or may simply have been forgotten, even by parents. Contemporary health or school records may be sought, if available. Despite these caveats, inquiry into the developmental history is important.
The Premorbid Adjustment Scale (PAS)147, 148 evaluates the level of functioning in four major areas (social accessibility ‐ isolation, peer relationships, ability to function outside the nuclear family, and capacity to form intimate socio‐sexual ties) at each of four periods of the subject’s life: childhood (up to 11 years), early adolescence (12‐15 years), late adolescence (16‐18 years), and adulthood (19 years and beyond). The final section contains items estimating the highest level of functioning that the subject achieved before becoming ill. The scale is intended to measure only “premorbid” functioning, and its questions have been updated to discount the entire year before the first psychiatric contact, in order to accommodate contemporary focus on early detection and intervention 148 . Ratings are based on reports from family members or clinical records. When it is felt that the patient is reliable, a personal interview may be conducted to complete the ratings. The scoring for each item ranges from “0”, corresponding to the healthiest end of the adjustment range, to “6”, corresponding to the least healthy end. Asking informants to compare and contrast with the patient's siblings is often helpful.
Overall, consideration of neurodevelopmental indicators can be useful to obtain a more complete characterization of the patient with primary psychosis, help in differential diagnosis, and contribute to the formulation of a more comprehensive and targeted management plan.
SOCIAL FUNCTIONING, QUALITY OF LIFE AND UNMET NEEDS
Impairments of social functioning in schizophrenia have been described since the time of Kraepelin 130 . Social functioning is a broad term, which includes milestones such as marriage or equivalent relationships, social interactions such as friendships, as well as social skills and social motivation. Further, social functioning is related to quality of life, the definition and assessment of which have been complex and occasionally obscured in research on primary psychosis.
Impairments of social functioning in patients with a post‐DSM‐III diagnosis of schizophrenia have several features. People with this disorder are much less likely than the general population to experience marriage or equivalent milestones 149 . They also have smaller social networks, and are likely to nominate a clinician as the person who knows them best 110 . The generalizability of these findings to all patients fulfilling the broader ICD‐11 definition of schizophrenia or to those with ICD‐11 “other primary psychotic disorder” remains uncertain.
Social anhedonia is the phenomenon whereby people with schizophrenia experience less pleasure from social interactions and manifest reduced interest in these interactions. In fact, many of them rarely leave their homes, being home as much as 70% or more of the time 150 . It is a complex phenomenon, because there is evidence that individuals with schizophrenia enjoy social activities as much as healthy individuals at the time of the experience, but have challenges in recalling this enjoyment in order to motivate later interactions 151 .
Another feature of social functioning in schizophrenia is an impairment in social skills or social competence. Many people with this disorder have reduced ability to interact with others and may make socially inappropriate statements or gestures 152 . These problems make interactions challenging and may reduce the willingness of others to engage with them.
In addition to data on current social functioning, the assessment needs to consider motivation to engage in social activities, the level of social competence, and the individuals’ evaluation of their ability compared to objective information (social milestones). Understanding the level of social motivation will be critical for the development of treatment strategies, as social skills training will not improve social outcomes in people who have no plans to engage in social activities 153 , and targeted treatment aimed at negative symptoms associated with poor social outcomes is now proven effective 154 .
Several social functioning scales are available, and most are very easy to use in practice. The Specific Levels of Functioning (SLOF) has been found to be the rating scale wherein informant reports are most consistently correlated with objective data from performance‐based assessments 155 . This 31‐item scale has three subscales (vocational, social, and everyday activities). It is easily completed and requires no special training.
The Personal and Social Performance Scale (PSP) 156 also collects data on social and everyday activities. Also amenable to informant report, this scale generates both domain and total scores. The domains are socially useful activities (including work and school), personal and social relationships, self‐care, and disturbing and aggressive behavior. Impairments in the four domains are rated on a 6‐point scale (from “absent” to “very severe”), with a global score ranging from 0 to 100. As functional impairments in primary psychosis are relatively uncorrelated across domains, consideration of domain scores instead of a total score is highly recommended.
For the critical assessment of motivation to engage in social activities, there are several possibilities. Self‐reported measures include the Temporal Experience of Pleasure Scale (TEPS) 157 , which captures the level of enjoyment in pleasurable activities (consummatory pleasure) and the anticipation of pleasure in these activities (anticipatory pleasure). A similar assessment of sensitivity to pleasurable activities is the Motivation and Pleasure Scale ‐ Self‐Report (MAP‐SR) 158 . This scale is designed to be a self‐report measure that parallels the widely used negative symptoms assessment by the CAINS 54 . All of these scales capture subjective motivation, which has been found to correlate quite strongly with actual social outcomes measured by an independent rater, by‐passing the need for a structured interview procedure.
Problems in social competence are usually treated with social skills training, while recent treatments aimed at motivational impairment have used technology‐based interventions such as the Personalized Real‐time Intervention for Motivational Enhancement (PRIME) 159 . This is a mobile application which first assesses the participant’s level of engagement with others and in activities and then uses those assessment data to make suggestions regarding possible activities to engage in: “Why don't you try to visit someone in your family today?”. Cognitive behavioral interventions have shown efficacy for improvement of social skills and concurrent reduction of socially relevant negative symptoms 154 .
Quality of life in primary psychosis is multi‐faceted and only partially overlapping with social functioning. Objective quality of life indicators include the milestones noted above, as well as employment, independence in living, and other elements of maintenance of normal adult autonomy. Subjective quality of life is the report of both activities performed and the individuals’ subjective response to these activities. It has been widely confirmed that overlap between objective and subjective quality of life indices is reduced in people with schizophrenia, with evidence of under‐estimation of level of impairment found objectively160, 161.
In terms of subjective quality of life, several scales are readily available. It is important to capture patient quality of life reports, even if divergent from objective information, because patients’ motivation to engage in multiple different treatments will be based on their perception of their current level of functioning.
The World Health Organization Quality of Life Scale (WHO‐QOL) 162 has been widely used to assess subjective quality of life. This scale has the benefit of being self‐administered. It examines quality of life in the domains of physical and mental health, social relationships, and the environment.
A rater‐administered scale, the Quality of Well‐Being scale (QWB) 163 , captures subjective illness burden and has the advantage of providing norms across different illnesses, including psychiatric and physical conditions. This is a more challenging assessment which requires training to administer.
A main driver of quality of life in persons with primary psychosis is represented by the dimension of unmet needs 164 . Unmet needs are frequently found in the areas of daytime activities, information, company, intimate relationships and sexual expression. In many parts of the world, housing, employment and social benefits also represent frequent unmet needs in people with primary psychosis 165 .
Including these elements in the clinical assessment framework is important for several reasons. First, a perspective of needs is humanizing and normalizing. There is, in fact, a widely recognized universal hierarchy of human needs as defined by Maslow 166 : physiological, safety, love and belonging, esteem, and self‐actualization needs. Second, the concept of need recognizes the service user’s experience and preference, given that assessment requires his/her perspective on what is “unmet”.
Assessment of needs thus becomes an active process of exploration, listening and understanding on the part of the clinician, often requiring a degree of negotiation between clinician and patient, which in turn will enhance the likelihood of shared decision‐making. This is important, as better staff‐patient agreement on needs makes a significant additional contribution in predicting treatment outcomes 167 , and staff with an active and shared decision‐making style has more impact on reducing unmet needs over time 168 .
Third, the assessment of needs automatically takes into account the level of contextual influences, such as the impact of friends, family and informal help, in making a need met or unmet. This enhances the sensitivity of the mental health service to the role of informal carers and other resources in the network. Finally, there is evidence that systematic monitoring of patient needs may result in better outcomes and is cost‐effective169, 170, 171.
The Camberwell Assessment of Need (CAN)172, 173, available in 26 languages, is a widely used and practical instrument to assess needs in clinical care. Its reliability and validity have been tested extensively. It is comprehensive, assessing a full range of 22 health and social needs, including housing, food, cleaning, self‐care, daily activities, physical health, psychotic symptoms, treatment or illness information, psychological distress, personal security, social security, security of others, alcohol, drugs, social relationships, emotional relationships, sexual life, care of children, education, financial tasks, use of telephone/computer, and use of public transportation. Clinicians can choose to add further needs, for example religion/spirituality. This instrument separately assesses the perspective of staff, service users and family members, identifying areas of agreement and disagreement about whether a need is present, which supports negotiation and shared decision‐making.
The assessment of the patient’s practical needs is essential for the formulation of a comprehensive management plan. For patients who express an interest in supported employment, the Individual Placement and Support (IPS) model has been found to be significantly more effective than other types of vocational assistance in many randomized trials conducted internationally 174 . Among the basic principles of the IPS model are eligibility based on client's choice, focus on competitive employment, integration of mental health and employment services, attention to the client's preferences, and individualized job supports 174 .
CLINICAL STAGING
Staging was developed in clinical medicine as a strategy to add precision to diagnosis and treatment selection and also to prognosis and prediction of outcome175, 176. A transdiagnostic approach is essential for staging in psychiatry. This approach acknowledges the fluid and dynamic nature of the onset and early stages of mental ill‐health, during which microphenotypes ebb and flow, and either fade or evolve into a more stable syndrome or more commonly syndromes (Figure 1). Primary psychosis is one of these syndromes, one that typically emerges from earlier stages which already display a need for care, and attracts additional comorbid syndromes and functional impairment 177 .
Figure 1.
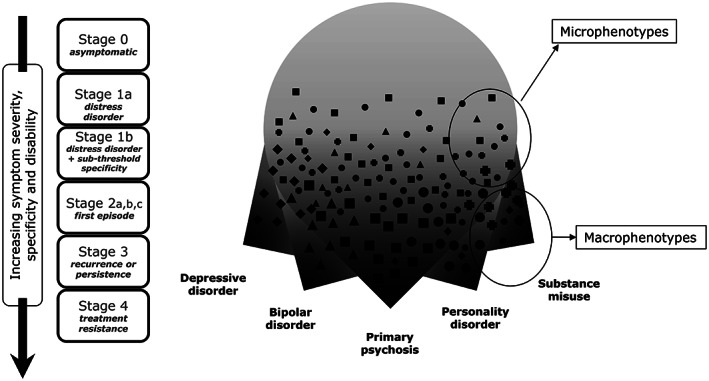
Clinical staging model showing the emergence of undifferentiated microphenotypes that may progress to macrophenotypes such as primary psychosis
While the idea of staging had been raised initially for common mental disorders 178 , the early intervention paradigm in psychosis created the ideal conditions for clinical staging to be formulated. First episode psychosis was the fulcrum around which this began, and an evidence‐based case was steadily made that the content of treatment for such cases was very different from what was appropriate for later stages of illness.
An earlier clinical stage, the ultra/clinical high risk state (corresponding to stage 1b in Figure 1), was defined, covering the period prior to the threshold for a first episode of psychosis being reached, and this has become an intense focus for research and intervention 179 . The validity of this earlier stage was supported by its manifestly different treatment needs, and ultimately overwhelming evidence that progression could be delayed at least, and early trajectories of illness significantly improved180, 181. While some critics remain unconvinced 182 , the mindset of the psychosis field has moved from deterministic “doomed from the womb” thinking to a more preventive, recovery‐oriented approach180, 183.
In this earlier clinical stage, in which psychotic symptoms are present though still attenuated, but there is a need for care, the treatment consists of psychosocial interventions influenced by CBT, and a focus on treatable comorbid syndromes such as anxiety and depression, alleviating stress, strengthening coping and minimizing illicit drug use. At this stage, antipsychotic medications are not indicated.
When new perceptual experiences and/or delusional ideas cluster and persist, reaching a threshold of frequency and severity that causes distress and functional impairment, a diagnosis of first episode psychosis (stage 2) can be made.
Patients with first episode psychosis respond much better to all treatments if the duration of untreated psychosis (DUP) is reduced to a minimum. There is varying evidence on the exact window of time, but some of it suggests that delays of even a few weeks may make a significant difference to treatment response184, 185. This suggests that first episode psychosis might be better considered as a stage with substages within it.
In fact, with a much shorter DUP now achievable in early intervention services, it may be possible for a small subgroup of patients to remit without antipsychotic medication if provided with intensive psychosocial interventions alone 186 , although further evidence is needed in this respect. This might be termed stage 2a.
In all other cases of first episode psychosis (stage 2b), research evidence indicates that low doses of antipsychotic medications are often effective and must be rigorously adhered to if adverse experiences are to be minimized and engagement maximized 187 . Shared decision‐making has a crucial place here. The imperative to prevent weight gain and metabolic consequences means that medications least likely to produce these effects must be first line.
A subgroup of patients who fail to respond to dopamine antagonists and reveal early treatment resistance can be reclassified as a further substage of stage 2 (stage 2c), or alternatively as having rapidly progressed to stage 4. Here the benefit‐risk ratio changes sharply and, while clozapine has a number of adverse effects which mean it should not be used as first line, the evidence strongly mandates its use if early treatment resistance or stage 4 is reached 188 .
Psychosocial treatments, notably supported vocational programmes such as IPS and family interventions, have to be adapted to the stage of illness, and are much more effective at stage 2 189 .
Beyond the first episode (stage 2), patients may enter stage 3 (recurrence or persistence) or 4 (treatment resistance). Stage 3 intervention involves the prevention of relapse and efforts to treat comorbidity and persistent subthreshold or residual symptoms of psychosis and other associated syndromes. Long‐acting injectable antipsychotics can be seen as a preventive strategy. However, dose reduction and even discontinuation are possible for a subgroup of patients 190 , so a personalized approach with substages and subgroups reflects a heterogeneity within stage 3.
Late stage 3 patients who appear to have stabilized, but with continuing symptoms and functional impairment, can be offered a different suite of psychosocial interventions which may greatly improve their quality of life. This may involve meaningful activity, including part‐time work, strength‐based strategies, social engagement within community to combat loneliness, family support, financial support, and expert medical care to respond to the greatly increased risk of medical illnesses.
For stage 4 (treatment resistant) patients, the use of clozapine, as mentioned above, is mandated.
A contributing life is possible for most people with primary psychosis. The “soft bigotry of low expectations” is a consequence of poorly resourced systems of care and antiquated diagnostic thinking, which is not informed by the opportunities that new models of care and high fidelity implementation can now deliver. Such approaches, which of course need to be supported by scientifically valid data, depend on congruent mindsets and conceptual frameworks, and a much more educated and supportive wider community.
ANTECEDENT AND CONCOMITANT PSYCHIATRIC CONDITIONS
The diagnosis of schizophrenia was previously considered in a hierarchical framework, wherein comorbid psychiatric conditions were viewed as diverse manifestations of the psychotic process and were not considered or addressed. Antipsychotic medications were expected to impact on a wide array of psychopathology, whereas they largely target only psychotic symptoms.
We now recognize that the majority of persons with primary psychosis have other antecedent or concomitant psychiatric syndromes or subthreshold conditions. This is unsurprising given the large overlap of common gene variants for multiple psychiatric conditions and the association of many environmental exposures with diverse psychiatric disorders. Addressing comorbid conditions, even those that are subthreshold with respect to categorical diagnoses, and considering antecedent conditions in the treatment plan, can significantly improve the patient’s functional outcome and his/her quality of life.
In some settings, the Structured Clinical Interview for DSM‐5 (SCID‐5) 191 or other semi‐structured assessments are employed to explore other psychopathological domains. However, these instruments are designed to detect categorical diagnoses, rated only as present or absent, and do not identify subthreshold conditions which might nonetheless inform clinical approaches. Continuous scales can detect symptoms and be useful in monitoring treatment. DSM‐5's Section III includes a cross‐cutting symptom measure 1 which may be used as a screening tool to identify the presence of other symptom domains in a patient with a diagnosis of primary psychosis.
Depressive symptoms are common even in persons with non‐affective psychoses. They are highly confusable with negative symptoms, particularly social withdrawal, anhedonia, avolition, and reduced emotional expression. So, information on enduring versus episodic presentations of such symptoms, as well as on alterations in appetite, sleep and concentration, and the presence of guilt and hopelessness, is essential to elicit. The Calgary Depression Scale for Schizophrenia 69 can be used to disentangle negative and depressive symptoms.
Persisting depression despite antipsychotic treatment limits recovery and well‐being and is associated with increased suicide risk 192 . Adjunctive antidepressant medications may be needed. On the other hand, subsyndromal or premorbid manic symptoms may suggest the practicability of a lithium trial, especially when there is a family history of bipolar disorder.
Social anxiety is also highly prevalent in primary psychosis. It is likewise distinct from negative symptoms and predicts poor functioning. As social anxiety is readily addressed through psychotherapy or medication, it should not be overlooked or confused with paranoia. The Liebowitz Social Anxiety Scale 193 can be used for this purpose.
The common finding of antecedent obsessive‐compulsive disorder (OCD) or traits in persons with primary psychosis is notable, as this subgroup demonstrates an earlier age of psychosis onset, worse psychotic and negative symptoms, and more depressive symptoms and suicide attempts, resulting in higher hospitalization rates and a worse prognosis overall 194 . This component can be explored in patients with a diagnosis of primary psychosis by using the Yale‐Brown Obsessive Compulsive Scale (Y‐BOCS) 195 .
The treatment of comorbid OCD and psychosis is complex. Newer atypical antipsychotics are sometimes associated with de novo occurrence or worsening of OCD phenomena that can be managed by medication changes, but persons with premorbid and persisting OCD require other interventions, including CBT and, if that is not ameliorative, adjunctive antidepressant treatment targeting the OCD symptoms.
Post‐traumatic stress disorder (PTSD) is commonly comorbid with primary psychosis, requiring specific interventions and possibly heralding treatment resistance. Treatment‐refractory psychotic symptoms with relatively preserved intellectual function are also reported in persons who experienced premorbid eating disorders several years before psychosis was manifest, found to be as many as 10% of schizophrenia cases in a recent series 196 . These cases and those with PTSD may require higher doses of antipsychotics. Attention‐deficit/hyperactivity disorder (ADHD) in childhood also confers a greater risk of subsequent psychosis, but does not appreciably alter the illness expression 197 .
Psychotic symptoms frequently present in association with substance use, particularly chronic cannabis abuse, but also use of amphetamines, cocaine, hallucinogens, opioids, phencyclidine, sedatives/hypnotics and alcohol. If the hallucinations and delusions exceed those that are typically observed in the setting of substance intoxication or withdrawal, then a diagnosis of substance induced psychosis will have to be considered.
Many individuals who are already at high risk for psychosis use substances, and their psychotic symptoms do not abate when intoxication or withdrawal is resolved, indicating a primary psychotic disorder. Evidence of prior psychiatric symptoms can shed light on the differentiation of substance induced versus primary psychosis.
Persons with psychosis have a more than 4‐fold increase in substance use compared to the general population, with an even greater relative risk for nicotine addiction 198 . Interventions for substance use and abuse are frequently essential components of the treatment plan.
Psychotic symptoms occurring in the context of global developmental delay, communication disorders of childhood onset, or autism spectrum disorder are not considered to be primary psychotic disorders, unless prominent delusions or hallucinations emerge that persist for at least one month, or for a lesser duration if they are successfully treated. Psychotic symptoms in persons with developmental disorders appear to be resistant to antipsychotic treatment 142 , possibly having distinct underpinnings. Additional studies are needed that may define the characteristics of those with developmental disorders who do respond to different medications for precision treatment approaches.
Finally, although the vast majority of persons with primary psychosis are far more likely to be victims than aggressors, there is a small increase in the risk for antisocial traits among these persons. This comorbidity is rarely considered, but it should be assessed and inform treatment planning. Antisocial traits are not revealed by prior contact with the criminal justice system, which is sadly quite common among persons with psychosis. A history of antisocial traits in childhood and demonstrated callous indifference towards others can be elicited using the Hare Psychopathy Checklist‐Revised 199 .
PHYSICAL COMORBIDITIES
People with primary psychosis suffer excess morbidity and mortality from physical conditions, particularly cardiometabolic diseases, leading to a drastically reduced life expectancy 11 . Although this is partly due to the metabolic side effects of antipsychotic medication, unhealthy lifestyle behaviors further increase the risk of physical complications/disorders. Despite numerous calls to take their physical health seriously, the screening, assessment and management of physical health aspects in people with primary psychosis remain poor, even in high‐income countries. Physical health improvement in these patients is therefore essential, and physical health considerations should be paramount in the choice of antipsychotic medication11, 200, 201, 202, 203.
One third of people with primary psychosis develop metabolic syndrome 204 , characterized by the simultaneous occurrence of several metabolic abnormalities (abdominal obesity, glucose intolerance or insulin resistance, dyslipidemia and hypertension) 201 . Meta‐analytic data show that, compared with the general population, these people have a 1.9 times higher risk of developing the syndrome 204 .
Primary psychosis is also a risk factor for cardiovascular diseases and type 2 diabetes mellitus205, 206. According to a large‐scale meta‐analysis, a diagnosis of schizophrenia increases the risk for coronary heart disease by 1.5‐1.6 times 207 . The risk for type 2 diabetes mellitus is two times higher in people with schizophrenia compared to the general population 206 .
As the individual components of metabolic syndrome are critical in predicting the occurrence of cardiovascular diseases, type 2 diabetes mellitus, cancer and other related diseases, they should be checked at baseline, taken into account in the choice of medication, and measured regularly during treatment 208 . Among second‐generation antipsychotics, clozapine and olanzapine are associated with the highest cardiometabolic risks, while the lowest risk is with aripiprazole, ziprasidone, lurasidone and amisulpride 207 .
Clinicians should monitor the weight of each patient at every visit. Central/abdominal obesity correlates more strongly with insulin resistance, and places people with primary psychosis at higher risk for developing type 2 diabetes mellitus and cardiovascular diseases, than does total body weight or body mass index. Waist circumference, therefore, is the best measurement to assess these risks, and can easily be done with a simple tape measure placed around the waist. This parameter should be measured at midpoint between the last rib and the iliac crest. Cutoff points for increased obesity‐related health risks are 94 cm for men and 90 cm for women (these cutoff values, however, are somewhat lower for Asians and South and Central Americans) 208 .
Hypertension increases the risk for a variety of cardiovascular diseases. Although differences in the definition of hypertension between guidelines exist, any systolic blood pressure >120 mmHg is associated with an increased cardiovascular risk. Blood pressure monitoring, therefore, should become part of the routine health assessment in patients with primary psychosis. A checklist for accurate measurement of blood pressure is provided by the American College of Cardiology/American Heart Association (ACC/AHA) 209 . Importantly, repeated measurements separated by 1‐2 min intervals, as well as out‐of‐office‐based measurements, are required to confirm the diagnosis of elevated blood pressure/hypertension. At the first visit, blood pressure should be recorded at both arms. Thereafter, one should use the arm that gives the higher reading 209 .
It is also important to calculate and manage the overall cardiovascular risk of a patient. Several institutions and consensus health panels, including the World Health Organization (WHO) and the Joint British Societies (JBS), have published online tools to calculate patients’ cardiovascular disease risk, based on several clinical parameters such as age, gender, blood pressure, smoking status, total cholesterol, and presence or absence of diabetes mellitus210, 211, 212. The value of such predictions is to help communicate risk, so that patients can receive advice (and treatment if necessary) appropriate to their risk level.
Identifying and managing all modifiable cardiovascular risk factors in people with primary psychosis – such as smoking, an unhealthy diet, obesity, sedentary lifestyle, alcohol consumption, diabetes mellitus, and dyslipidemia – are as important as managing hypertension in lowering overall cardiovascular risk213, 214. Evidence has shown that people with schizophrenia have significantly higher rates of current smoking, heavy smoking, and nicotine dependence, and have significantly higher food intake and poorer diet quality than the general population 203 . Moreover, more than half of people with schizophrenia (55%) do not meet physical activity guidelines and are sedentary for more than 8 hours per day203, 215. One in five patients have or have had alcohol use disorder 203 .
As a general rule, every patient should have an electrocardiogram measurement before prescribing antipsychotic drugs that have been associated with QT prolongation. Moreover, these drugs should not be prescribed for patients with known heart disease, a personal history of syncope, a family history of sudden cardiac death at an early age (especially if both parents had sudden cardiac death), or congenital long QT syndrome 208 .
Regardless of age and presence of other risk factors, periodic monitoring of patients with primary psychosis to prevent hyperglycemia is critical, and testing should be considered early in the course of treatment. Finger prick tests, giving an instant reading or snapshot of the glucose level in the blood, should be carried out at baseline, after three months to capture early cases of hyperglycemia, and annually thereafter 208 . These monitoring intervals are, however, suggestions which need to be modified with regard to the administered antipsychotic. Ideally, blood glucose should be assessed in the fasting state, because this is the most sensitive measurement for the detection of developing glucose abnormalities. Conventional tests for screening hyperglycemia are the fasting plasma glucose test, the oral glucose tolerance test, and the glycosylated hemoglobin (HbA1c) test. As adherence in this patient population may be an issue, the HbA1c test may be preferable to a fasting glucose level as a screening test 216 .
Lipid parameters, especially triglycerides and high density lipoprotein (HDL)‐cholesterol, should also be assessed at baseline and at three months, with 12‐monthly assessments thereafter. More frequent screening is unnecessary, unless in case of abnormal values 206 . Fasting is not routinely required for the determination of a lipid profile.
Individual lifestyle counseling and psychoeducation interventions focused on promoting a healthy lifestyle should be considered as first‐line strategies for the prevention and management of physical comorbidities in patients with primary psychosis203, 216, 217, 218. Patients should be advised to engage in at least 30 min of moderate‐intensity physical activity for a minimum of five days per week 215 . An e‐learning tool from the National Centre for Smoking Cessation is now freely available online for clinicians to acquire core knowledge and skills to deliver effective behavioral support for smoking cessation 203 .
When lifestyle interventions for physical comorbidities are not effective, medication may be indicated 208 . Metformin is the leading pharmacological option for managing weight gain during antipsychotic treatment, and has the additional advantage of reducing the incidence of type 2 diabetes in patients with hyperglycemia. Growing evidence also suggests that metformin has cardioprotective effects beyond its hypoglycemic effects 219 . Bupropion and varenicline have proven their effectiveness for smoking cessation in individuals with primary psychosis220, 221.
In cases where physical health problems – such as hyperglycemia, hyperlipidemia or hyperprolactinemia – are secondary to antipsychotic medication, dose reduction or switching to an antipsychotic with a lower risk profile should be considered, if safe and feasible202, 208. Patients treated with clozapine need a special monitoring, because the adverse drug reactions related to physical health that can be induced by this medication (agranulocytosis, myocarditis and cardiomyopathy, cardiometabolic diseases) are a major concern 202 .
Prevention of physical health problems in people with primary psychosis by promoting a healthy lifestyle is likely to be more efficient than intervening after significant changes in clinical or biological markers are found during cardiometabolic screening 222 . Emerging evidence indicates that mHealth, i.e. the use of digital technology (such as smartphone apps and fitness trackers) in health care delivery, can play an important role in preventing physical comorbidities 223 , although its feasibility and clinical utility in patients with primary psychosis remains to be proved.
FAMILY HISTORY
In schizophrenia spectrum psychosis, family history of the disorder is one the strongest known risk factors. According to a meta‐analysis, having an affected parent is associated with a 7.5‐fold higher risk for schizophrenia in the offspring 224 .
Only a minority of people with a diagnosis of schizophrenia, however, have a positive family history of that disorder. A simulation study of complex polygenic diseases estimated that 83‐90% of persons with schizophrenia in typical families (with an average of two children) do not have any affected first‐, second‐, or third‐degree relatives 225 . This large proportion of sporadic cases is expected under the polygenic model, considering the low prevalence rate of the disorder 225 .
The clinical assessment of family history in a patient with primary psychosis should not only focus on schizophrenia. Clinically diagnosed schizophrenia may be associated with the presence of several different mental disorders in first‐degree relatives, and more schizophrenia in the population can be attributed to a family history of a non‐schizophrenia disorder than to a family history of schizophrenia itself 226 . These findings echo those of molecular genetic studies, showing that two thirds of genetic associations are common to schizophrenia, bipolar disorder and major depressive disorder, and overlaps also exist with genetic variants contributing to autism, ADHD and intellectual disabilities227, 228. Therefore, the clinical assessment of family history in patients with primary psychosis should consider the entire spectrum of mental disorders. Given the high lifetime rates of mental disorder, a positive family history, broadly defined, may be expected in a sizeable proportion of patients.
The clinical interpretation of the presence of family history is complex and goes beyond “genetic load”. Schizophrenia polygenic risk scores appear to mediate less than 20% of the effect of family history 229 . This is likely in part explained by the fact that particularly parental family history also reflects environmental influences, such as higher rates of birth and pregnancy complications230, 231, growing up in an unfavorable home environment 232 , out‐of‐home placement 233 , elevated divorce rate, alterations in parental communication 234 , and poor school performance 235 . The sizeable impact of growing up with a parent with severe mental illness on psychological and social development has been recently reviewed 236 . Therefore, a positive family history should be accompanied by an examination of the developmental impact of parental psychopathology and the clinical needs associated with this.
Family history is also of direct clinical relevance, as the first episode of primary psychosis typically occurs when patients are still dependent on and/or living with their parents. The presence of parental psychopathology may indicate reduced family resilience and increased need for family support 236 .
In a patient with primary psychosis, the family history of mental disorders can be assessed using either structured interviews or screening instruments. Most structured interviews, such as the Family Interview for Genetic Studies 237 and the Diagnostic Interview for Genetic Studies 238 , can take several hours to complete. In clinical practice, shorter questionnaires or screens are more suitable for use.
The Family History Screen (FHS) 239 collects information on 15 lifetime mental disorders as well as on suicide attempts. It is administered to a family informant, who reports about himself/herself and other biological relatives (parents, siblings and offspring). The screen starts with general questions about symptoms, treatment and impairment, followed by more specific questions about psychopathology. The FHS takes about 5 to 20 min to administer, as each question is posed only once about all family members as a group.
Family history needs to be re‐assessed over time, as not all relatives of the index patient may have passed through their period of risk for each mental disorder. Also, new information may arise that previously had remained undetected due to recall difficulties or lack of knowledge.
There is some evidence that a family history of psychosis may affect prognosis. For example, this history was associated with worse outcomes of the disorder in several meta‐analyses, especially regarding negative symptoms 240 and occupational and global outcome 241 . Effect sizes, however, were relatively small. Younger age of onset has also been associated with family history 240 , which is clinically relevant since this variable is associated with poorer clinical and social outcome 242 . There is no evidence that gender moderates the influence of family history on outcome. However, it has been noticed that, although men typically display more negative symptoms than women, this may not be the case among those with a family history 242 .
In the recent Swedish National Register and Genomic Study 243 , family history was found to be associated with a higher risk for treatment resistance in patients with schizophrenia. In a subset of cases with genomic data, there was no significant association between the genetic risk scores of four mental disorders and treatment resistance. However, further research is needed to explore if genetic risk scores are associated with clinical outcome, alone or when combined with family history data.
In summary, broadly defined family history of mental illness may impact psychosocial development of patients and alter family resilience in a clinically relevant fashion. Family history can be reliably assessed in patients with primary psychosis in routine clinical practice using short screening instruments. The presence of a family history of the disorder is associated with an earlier age at onset and may have an effect on outcome.
OBSTETRIC COMPLICATIONS
Obstetric complications are among the best replicated environmental risk factors for psychosis in the schizophrenia spectrum. They include a number of different variables which present a hazard to the normal development of the baby’s brain.
The significance of the association between birth complications and schizophrenia was established by the work of Scandinavian researchers244, 245 from the 1970s onwards. Indeed, their findings contributed to the thinking behind the formulation in 1987 of the neurodevelopmental model of schizophrenia133, 246.
The topic was comprehensively reviewed by Cannon et al 247 . Their meta‐analysis of prospective population‐based studies revealed that three groups of complications were significantly associated with later schizophrenia: a) complications of pregnancy (bleeding, diabetes, Rh incompatibility, pre‐eclampsia); b) abnormal foetal growth and development (low birthweight, congenital malformations, reduced head circumference), and c) complications of delivery (uterine atony, asphyxia, emergency caesarean section). However, estimates of effect sizes were generally less than 2.
Very recently, Davies et al 248 carried out a meta‐analysis of pre‐ and perinatal factors for psychosis as a whole, largely confirming Cannon’s findings. Both meta‐analyses concluded that foetal hypoxia and anoxia‐related factors, where the developing brain is deprived of oxygen, are among those most consistently implicated.
In clinical practice, one should always enquire of patients if they know whether they were subject to any obstetric events. A minority of patients may know about this, particularly if the events were severe or life‐threatening (e.g., prematurity, emergency caesarean section, being “blue” or in an incubator). However, more likely than not, the patient will not know about this aspect of his/her life.
This lack of information cannot be taken as meaning that such events did not occur. Therefore, wherever possible, it is wise to ask a parent, particularly the mother, about pregnancy and the patient's birth. The evidence is that mothers remember major events that occurred (e.g., pre‐eclampsia, forceps delivery), although they may have forgotten more minor events (e.g., antenatal haemorrhage) 249 . Fathers are much less reliable.
The Lewis‐Murray checklist246, 250 can be used for rating information obtained from maternal interviews. It covers 16 complications: rubella and syphilis during pregnancy, Rh incompatibility, antepartum haemorrhage, severe pre‐eclampsia, premature rupture of membranes, labour >36 hours, complicated twin birth, cord prolapse, gestational age <37 weeks or >42 weeks, emergency caesarean section, breech or abnormal presentation, mid to high forceps, birth weight ≤2 kg, incubator >4 weeks. Each of these complications is rated. Thresholds are given rating them as “definite” or “equivocal” 250 .
If it is very important to establish the facts and mother is vague, then the ideal approach is to obtain the original birth records. The Lewis‐Murray checklist can be applied to these. However, the McNeil‐Sjöström scale 251 is more comprehensive and was specifically designed for use with birth records. It takes longer to complete but gives much more detailed information. Therefore, it is generally used in research rather than clinical practice.
Prospective studies have examined the overall long‐term consequences to babies of being exposed to obstetric complications252, 253. These have demonstrated that early brain hazards, especially those which cause periventricular haemorrhage, are associated to vulnerability not only to psychosis but also to neurodevelopmental disorders such as ADHD and autism. Cognitive problems are common (including lower IQ), as well as neurological deficits ranging from soft signs to cerebral palsy. Neuroimaging studies have shown that, when babies who suffered periventricular bleeds reach adult life, they show an excess of brain structural abnormalities such as ventricular enlargement and cortical thinning, as well as dopaminergic abnormalities, reminiscent of those found in patients with schizophrenia253, 254.
If one elicits a history of a major obstetric event, then what relevance does this have to the patient? It may have none, as the vast majority of babies exposed to such events develop entirely normally; the psychosis may be coincidental. However, the event is particularly likely to be significant if the patient has shown evidence of soft neurological signs or developmental problems in childhood (e.g., late milestones, lower IQ than siblings, childhood psychiatric or behavioral problems, especially ADHD).
Should any of these be present, then further investigation is warranted. In particular, structural magnetic resonance imaging (MRI) may be useful to ascertain if there is any evidence of early brain damage: larger ventricles, small hippocampi or cortical thinning may point to significance. Neuropsychological testing may be useful to establish overall intellectual functioning or any specific alterations. For some unknown reason, the male foetus or baby is more susceptible to long‐term neuropsychiatric consequences of early brain insults.
Does the presence of an obstetric event which seems to be significant make any difference to the patient’s care? Not directly, but it does obviously contribute to the characterization of the individual case. It may have caused developmental delays in childhood as well as other behavioral problems long before the onset of the psychosis; it may also explain cognitive alterations and MRI abnormalities. Furthermore, it may help parents to understand why their son or daughter has developed the psychosis, and prevent them worrying about whether they may have caused the illness through some fault in their parenting.
Of course, one should keep in mind that risk factors for psychosis seldom act alone, and obstetric events may be a contributory cause acting on top of genetic predisposition or together with other environmental risk factors such as migration or cannabis use.
EARLY ENVIRONMENTAL EXPOSURES
Epidemiological evidence suggests that an adverse environment during the neurodevelopmentally sensitive period is associated with an increased risk for primary psychosis in later life. The meta‐analytical effect size estimates of primary psychosis risk vary for the different exposures, that include childhood adversities (e.g., parental death, abuse, neglect and bullying) as well as urban environment, migration and ethnic minority (that are likely to act through increased socio‐environmental adversities)255, 256, 257.
The effects of early exposures appear to be complex, dynamic and interactive 258 . Childhood adversity represents the epitome of the complex etiology of primary psychosis. For instance, childhood sexual abuse, in addition to primary psychosis, is associated with a wide range of mental and physical health outcomes, from obesity to depression to substance misuse 259 , which are also individually linked to increased risk for psychosis and poor outcomes among individuals with psychosis.
The detrimental impact of childhood adversities also appears to be additive 260 . In this regard, there may be various causal and non‐causal paths between childhood adversities and primary psychosis, such that the link between adversities and psychosis may also be partly dependent on the widespread detrimental impact on well‐being. Further, evidence suggests a gene‐environment interplay, as the association between childhood adversities and primary psychosis increases as a function of high genetic vulnerability 261 .
A recent meta‐analysis shows that childhood adversity is associated with poorer treatment outcomes among individuals diagnosed with psychotic disorders (OR=1.51, 95% CI: 1.08‐2.10) 262 . Childhood adversity is also linked to reduced service engagement and medication adherence 263 . Notwithstanding the scarcity of higher‐quality evidence from prospective studies in large samples, these findings indicate that it is important to acknowledge the presence of childhood adversity when forecasting the course of illness and formulating a management plan. Therefore, childhood adversity should be routinely assessed in individuals with primary psychosis.
However, the assessment of childhood adversities is challenging, even for an experienced mental health practitioner. First, the retrospective collection may be prone to recall bias. Second, acknowledging subjective experience, including perception and meaning assigned to adversity, is as much important as, if not more important than, the objective evaluation of an adverse event. Third, sociocultural background and personality influence appraising, reporting and disclosing of early adversities, and should therefore be considered during the assessment. Finally, a thorough assessment, taking into account the timing, duration, severity, frequency and type of childhood adversity, will yield better results, but may be considered time‐consuming in a hectic clinical setting.
Of numerous self‐report and clinician‐rated instruments for screening or more definitive appraisal of exposure to childhood adverse events, the Childhood Trauma Questionnaire (CTQ) 264 and the Childhood Experiences of Care and Abuse (CECA) 265 are the most commonly used.
The CTQ is a self‐report instrument, supported by robust psychometric data collected from different populations in diverse settings across the world. A total of 70 items (28 items for the CTQ‐Short Form) are rated on a 5‐point Likert scale (from “1 ‐ never” to “5 ‐ very often”), to assess five domains of childhood adversity: emotional neglect, physical neglect, emotional abuse, physical abuse, and sexual abuse.
With easy and quick administration (10 to 15 min), the CTQ may serve as a useful screening tool that covers a relatively broad range of childhood adversities. This simple questionnaire can be integrated into routine electronic health records to provide a basic perspective of the history of early exposures 266 .
The CECA offers the most detailed and contextualized formal assessment of childhood adversities, measuring the frequency, pervasiveness and intensity of physical and sexual abuse, maternal and paternal antipathy, and neglect. However, this tool requires at least an hour‐long interview and a specific training of the interviewer.
The Retrospective Bullying Questionnaire measures the frequency, intensity and duration of physical, emotional and relational victimization during elementary and middle/high school period 267 .
It should be noted that these instruments have been designed to collect information in a research context, and evidence on their clinical utility remains limited 268 . Further, childhood adversities, although largely unvarying in essence, may change in form over time (e.g., cyberbullying). These emerging forms of early adversities need to be addressed as well.
A meta‐analysis of 12 studies showed that trauma‐focused CBT (e.g., gradual imaginal exposure, cognitive restructuring) and eye‐movement desensitization reprocessing therapy result in a small improvement in positive symptoms immediately after treatment (g=0.31, 95% CI: 0.55‐0.06), but not at follow‐up, while having no effect on negative, depressive or anxiety symptoms 269 . A more inclusive systematic review failed to show converging high‐quality evidence for the effectiveness of trauma‐informed psychotherapeutic interventions in patients with psychotic symptoms 263 .
Given the limited benefit of current trauma‐focused psychotherapeutic interventions, and the need for further studies with low risk of bias, these interventions cannot be routinely recommended for patients with primary psychosis who present with a history of early adversities, particularly in a limited resource mental health setting. However, they should certainly be considered on a case‐by‐case basis.
Trauma‐focused psychotherapies should be tailored to the needs of individuals with primary psychosis. Randomized controlled trials are required to find the optimal duration and intensity for an effective intervention. Further, research is needed to help inform health care strategies to identify individuals most likely to benefit from these interventions.
From a public health perspective, early adversities are modifiable factors contributing to the global burden of mental disorders, including primary psychosis. Therefore, the ultimate goal should be to promote a nurturing environment for optimal childhood development 270 .
RECENT ENVIRONMENTAL EXPOSURES
Major stressful life events, i.e. situations that bring about a very significant positive or negative change in personal circumstances and/or involve an element of threat, may operate close to the onset or relapse of psychosis.
A meta‐analysis reported an association of major stressful life events with psychotic disorder and subclinical psychotic experiences, with an odds ratio of around 3 271 . However, the methodological quality of the majority of included studies was low. Moreover, a part of the association may be explained by a shared underlying genetic propensity, increasing the risk for psychosis as well as exposure to major life events 272 .
From a clinical point of view, stressful life events may be particularly important when preceded by childhood adversity. A study found that 47% of the effect of childhood abuse was mediated by adverse events in adulthood, particularly events involving violence 273 . Moreover, some studies reported that exposure to childhood adversity may also increase the impact of stressful life events 274 , suggesting stress sensitization.
For assessment purposes, the semi‐structured interview Life Events and Difficulties Schedule (LEDS) is considered the gold standard, as it takes account of factors such as timing, severity and independence of events 275 . It is, however, time‐consuming to administer and rate. Alternatively, questionnaires such as the Social Readjustment Rating Scale (SRRS) 276 , the Psychiatric Epidemiology Research Interview (PERI) Life Events Scale 277 , and the Questionnaire of Stressful Life Events (QSLE) 278 , can be used.
In addition to stressful life events, the subjective feeling of being overwhelmed by, or unable to control, the demands of the environment seems to be a further factor linking stress experience to psychosis. At the population level, a study among 177,000 individuals found consistent evidence for a link between perceived stress and psychotic experiences 279 . Data again suggest that the impact of perceived stress is stronger in individuals previously confronted with childhood adverse events 280 .
While it should be appreciated that perceived stress is not an independent environmental factor, but arises in interaction with the subjective experience of the individual, its assessment may be of considerable clinical relevance, given its close correlation with 279 , as well as future prediction of 281 , psychotic symptom levels. This can be done using instruments such as the Perceived Stress Scale 282 or the Psychological Stress Index 283 .
Ecological momentary assessments, which measure symptoms, feelings and context multiple times per day during the course of several days, may even be more suited to assess daily life stress and the person’s sensitivity to it 284 . Novel e‐health approaches, such as apps, may help to implement these assessments in standard clinical practice 284 .
There are evidence‐based approaches that can help to reduce the impact of both stressful life events and daily life stress in psychotic patients, such as CBT for psychosis (CBTp), physical exercise, mindfulness, and acceptance and commitment therapy.
Another environmental exposure exerting its effect close to the onset or relapse of psychosis is the use of illegal substances, particularly cannabis. Meta‐analyses report a 2‐ to 3‐fold increased risk of psychosis in frequent users, with clear evidence for a dose‐response relationship 285 . This risk may be higher at a younger age at onset of use, in case of a family history of psychosis, or when cannabis strains with high levels of tetrahydrocannabinol are consumed 286 . Individuals with a history of severe childhood exposure to traumatic events also seem to be more sensitive to the psychosis‐inducing effects of cannabis 286 .
A systematic review concluded that around one third of psychotic patients had clinically significant cannabis use at their first episode, and the time between first use and the first psychotic break was on average about six years. During the first ten years after the first episode, around half of the previous users quit smoking cannabis. Those who continue to use it have higher relapse rates, longer hospital admissions and more severe psychotic symptoms than individuals who discontinue use or are non‐users 287 . Part of this effect may be mediated by worse medication adherence in cannabis users 288 . Importantly, quitting cannabis use may improve psychotic symptoms to the level of non‐using patients 288 .
Cannabis use can be assessed using the most updated version of the Cannabis Experience Questionnaire 289 . Unfortunately, treatment of cannabis use in patients with psychotic disorders remains a challenge: a meta‐analysis indicated no evidence of effect on frequency of use for any intervention, but there was some evidence for a decrease of quantity of use and positive symptoms associated with motivational intervention, either with or without CBTp 290 . There is, as yet, no compelling evidence to suggest that pharmacological substitution is effective.
PROTECTIVE FACTORS / RESILIENCE
In primary psychosis, personal and social protective factors and the individual’s levels of resilience can be mediators of the relationship between illness factors, such as cognitive impairment and negative symptom severity, and outcomes such as work and school functioning.
Protective factors include good coping capacity and problem solving skills, higher education, social and emotional support, participation in community activities, and economic/financial security40, 291, 292, 293, 294. Resilience refers to the ability to positively adapt to psychosocial adversity. Aspects of resilience include positive self‐image, self‐control, cognitive flexibility, social competence, emotional self‐regulation, self‐efficacy, and optimism293, 295, 296, 297, 298.
Given that no protective factor or aspect of resilience emerges as a “primary” contributor to functioning in persons with psychosis, consideration of several factors is important for understanding their relative contribution296, 299. Some factors can have a direct effect on functioning, while others act as mediators of the relationship between one illness factor and daily functioning. For example, positive coping and resilience partly mediate the relationship between negative symptoms and disability in primary psychosis99, 100, 298.
The assessment of protective factors and characteristics of resilience in an individual with primary psychosis is an important step in the formulation of a targeted management plan. The number of protective and resilience variables is relatively large. Individual patients might be deficient in some, but not all factors. Although there is no one gold‐standard assessment for protective factors or characteristics of resilience, there are several tools from which the clinician can choose. The analysis of total scores or individual items from these assessment measures can be used to personalize the treatment approach.
The Brief Cope (BC) 300 is a self‐report 14‐subscale/28‐item questionnaire composed of two items per subscale. A higher score indicates greater use of a specific coping strategy. The BC contains items assessing “adaptive” coping (e.g., “I’ve been taking action to try to make the situation better” and “I've been getting emotional support from others”), and “maladaptive” coping (e.g., “I've been using alcohol or other drugs to make myself feel better” and “I've been criticizing myself”).
The Simplified Coping Style Questionnaire (SCSQ) 301 is a 20‐item self‐report questionnaire with two categories: positive coping styles (items 1‐12) and negative coping styles (items 13‐20). The SCSQ items assess “appraisal” coping (e.g., “I try to see the positive side of the situation”) and “behavioral methods” of coping (e.g., “I make compromises”). The participants can rate each item from “0 ‐ never” to “3 ‐ often”, based on the frequency with which they used a given strategy when addressing a stressful situation or problem. This scale can be used to identify the coping style most often adopted by the patient. Low scores on specific items or low total scores indicate that an intervention to improve coping skills is needed.
The Social Network Questionnaire (SNQ) 302 can be used to assess structural and qualitative aspects of patients’ social network. This self‐administered questionnaire includes 15 items rated on a 4‐point scale (from “1 ‐ never" to “4 ‐ always"), organized into four factors: quality and frequency of social contacts, practical social support, emotional support, and quality of an intimate relationship. If family tension and criticism is high and family support is a potential protective factor that needs to be improved, then empirically‐based approaches such as family psychoeducation and family therapy would be indicated.
Resilience can be assessed using the Resilience Scale for Adults (RSA) 303 , a 33‐item self‐administered scale that examines intra‐ and inter‐personal factors thought to facilitate adaptation when a patient is facing psychosocial adversity. Items are organized into six factors: perception of self, perception of the future, structured style, social competence, family cohesion, and social resources. The RSA total score can be used as a global index of resilience, with higher scores reflecting higher resilience.
The Connor‐Davidson Resilience Scale (CD‐RISC) 304 is a 25‐item, 5‐point Likert‐type scale ranging from “0 ‐ not true at all” to “4 ‐ true all the time”. Patients rate each item based on how they felt over the previous month. The total score ranges from 0 to 100, with higher scores representing greater resilience. The 3‐factor structure comprises tenacity, strength and optimism, all of which have adequate internal reliability.
The Recovery Style Questionnaire (RSQ) 305 , a 39‐item self‐report measure, is designed to assess two distinct recovery styles, termed “integration” and “sealing over”. Integration (i.e., trying to understand and put one’s illness into perspective) has been associated with better outcomes, lower levels of depression, and better self‐evaluation, as compared to a “sealing over” style, in which individuals try to cover‐up, deny, or downplay the seriousness of a psychotic episode.
The relationship of protective factors and resilience to real‐life functioning highlights the importance of working in collaboration with patients when defining life goals and designing treatment programs. A resilience‐promoting mental health service should offer hope, optimism, empowerment, a focus on identity (the process of having to reinvent oneself after the onset of psychosis) and meaning (relationship with symptoms, illness and others) 306 , and foster the ability to absorb suffering307, 308. Peer‐run recovery colleges aim to facilitate these processes 309 .
INTERNALIZED STIGMA
Internalized stigma has been defined as “the devaluation, shame, secrecy and withdrawal triggered by applying negative stereotypes to oneself” 310 .
Surveys of people with schizophrenia have found that such experiences are either common or usual. A cross‐national study in 14 European countries reported that 43% of patients with this diagnosis had moderate or high levels of internalized stigma 311 . In a study conducted in rural settings in China, internalized stigma was found among 95% of people with severe mental illness 312 .
A wide range of factors have been associated with the experience of internalized stigma. Perhaps the most consistent finding is the close link with low self‐esteem. Higher internalized stigma was also shown to be connected to lower quality of life and lower levels of social functioning. There is evidence, as the name implies, that internalized stigma is associated with, and may often be a consequence of, experienced discrimination by others. There are also clinical associations, with connections between internalized stigma and symptoms of depression. A further implication of this line of reasoning is that higher internalized stigma may confer a greater risk of suicidality.
Further contextual and environmental factors also appear to play a role in internalized stigma, including how mental disorders are portrayed in the media, as well as cultural explanatory models of mental illness, with supernatural accounts being found to be more common among people with higher rates of internalized stigma. This stigma is also positively associated with psychiatric symptom severity and negatively associated with treatment adherence 313 .
Several important sequelae of internalized stigma have been identified. Higher rates are associated with lower rates of help‐seeking, and this may be especially the case among some minority ethnic groups and among older people. A mediation analysis has suggested that help‐seeking may be especially impaired among people with both higher levels of internalized stigma and depression 313 .
Internalized stigma can also be a potent barrier to seeking employment, as the anticipation of rejection deters people from applying for work 314 . More broadly, the literature suggests that internalized stigma is a powerful obstacle to recovery among people with severe mental illness, and can impair forming intimate partner relationships and social functioning.
For formal assessment of internalized stigma, the most commonly used measure is the Internalized Stigma of Mental Illness (ISMI) scale 315 . This scale was developed in collaboration with people with mental disorders, and contains 29 items with a score from “1 ‐ disagree” to “4 ‐ strongly agree”. It has high internal consistency and test‐retest reliability. Construct validity was supported by comparisons against scales measuring related constructs with the same methodology.
The ISMI score has positive correlations with measures of depressive symptoms, and negative correlations with measures of self‐esteem, empowerment and recovery orientation315, 316. There are now versions available in 47 languages, and adaptations for people with various mental disorders as well as for their parents and caregivers, and for people of different ethnicity. Evaluations of these versions of the scale have shown their reliability and validity across a wide range of languages and cultures, although not all psychometric properties have been assessed in all the scale versions.
Internalized stigma has several key implications for clinical practice. First, mental health practitioners need to recognize that internalized stigma among patients with a diagnosis of primary psychosis, in particular schizophrenia, is likely to be common and may be disabling. It is therefore necessary to ask patients directly about their understanding of their diagnosis of psychosis and their views about the implications of having such a condition. This will often lead to a detailed discussion to help the patient correct common misunderstandings, for example that psychosis is always a chronic and progressively disabling condition, or that psychosis means never being able to work or marry. Such discussions are often also necessary with family members to convey a realistic prospect of recovery from a psychotic episode, with an emphasis upon supporting advocacy, self‐esteem and empowerment 317 .
The verified presence of internalized stigma may have significant implications for the formulation of the management plan. Stigmatizing contacts with health professionals can worsen internalized stigma, and therefore interventions to reduce stigma among health care staff will contribute to reduction in internalized stigma. Advocacy groups and peer support may act to reduce the stigma 318 . There are now well‐established methods to reduce experienced stigma 319 , and there is emerging evidence that group therapeutic interventions can have a favorable impact, with psychoeducation being the most effective intervention element 320 .
DISCUSSION
The current practice of the management of patients with primary psychosis worldwide is often characterized by an oversimplification at several different levels.
The first level is that of diagnosis. Most treatment research and practice guidelines focus on schizophrenia, but this condition, as defined by the DSM‐III and its successors, accounts for only less than one half of cases of primary psychotic disorder, and about one quarter of all cases of psychosis 5 . So, it is not appropriate to generalize to all patients with primary psychotic disorder what research has documented in people with a post‐DSM‐III diagnosis of schizophrenia (i.e., concerning neurocognition, social cognition and social functioning), nor is it correct to regard all patients with “psychosis” (a term that is often used today as a synonym for either schizophrenia or primary psychosis) as having the same treatment needs.
Furthermore, even if the diagnosis is made according to one of current diagnostic systems, which is not the case in many clinical settings worldwide 321 , we cannot ignore that the definitions of all primary psychotic disorders, and in particular that of schizophrenia, differ in some significant respects between the DSM‐5 and the ICD‐11, so that the research evidence collected in samples of patients with a post‐DSM‐III diagnosis of schizophrenia is not necessarily generalizable to all patients receiving this diagnosis according to the ICD‐10 or ICD‐11.
A second level of oversimplification is that of psychopathological evaluation. It is widely acknowledged that schizophrenia, however diagnosed, is a heterogeneous entity. Both the DSM‐5 criteria and the ICD‐11 clinical description of that syndrome are polythetic, so that a patient presenting with only positive symptoms, minimal social and neurocognitive impairment and an episodic course, with little or no residual symptomatology in the intervals between the episodes, will receive the same diagnosis as a patient with prominent positive, negative and disorganization symptoms, a significant social and neurocognitive impairment and a continuous course. In the absence of a more focused clinical assessment beyond the mere diagnosis, these patients are likely to receive the same management, although their treatment needs may be very different.
Moreover, treatment needs in a given patient may change significantly depending on the current stage of the illness. Nonetheless, clinical staging is very rarely applied in ordinary practice, as is a detailed assessment of the course of the illness up to that moment.
A third level of oversimplification is that of history taking. The fact that schizophrenia (or “psychosis”) is clearly a heterogeneous condition, with a multitude of underlying genetic and environmental vulnerability and protective factors, which are involved to a different degree in the individual patient, should prompt a comprehensive assessment of the history of each patient, with respect to the best validated of those vulnerability factors, such as family history, history of obstetric complications, early and recent environmental exposures, as well as to the personal and social protective factors that have been supported by research evidence. This assessment can influence in several respects the choice and the modulation of the various components of the management plan. Unfortunately, it is very rare that this evaluation is implemented in ordinary clinical practice.
A fourth level of oversimplification can be identified in the choice of the treatment modality. Although every clinician and researcher would agree that the management of schizophrenia (or “psychosis”) must be “integrated” and consist of several components, the reality in many clinical contexts worldwide is that the patient will just receive an antipsychotic medication plus some psychosocial support that will likely not be evidence‐based. CBT is very seldom used in the vast majority of clinical settings worldwide, although there is evidence to support its efficacy in primary psychosis 7 .
The fifth level of oversimplification is that of the choice of the specific intervention within a given treatment modality. In the case of pharmacotherapy, although there seem to be differences among the various available drugs with respect to their efficacy on positive and negative symptoms 29 , it is true that these differences are not so clear at the moment as to guide the choice of medication in the individual patient. However, it is also true that there are major differences among the available drugs in terms of tolerability, which makes the characterization of the individual patient with respect to physical health and physical comorbidities absolutely needed in order to guide the choice of medication207, 322. Unfortunately, this is a principle upon which all clinicians would agree, but which is not consistently translated into routine clinical practice worldwide 11 .
Concerning psychosocial interventions, a significant body of research has accumulated in the past few decades, and we have a somewhat clear idea of what “works” in populations of patients with schizophrenia (or “psychosis”) 323 , and also, to some extent, of the features in the individual patient that could guide the choice and tailoring of a given intervention (see, for instance, the section on social functioning of the present paper). The reality, however, is that the psychosocial intervention in patients with schizophrenia (or “psychosis”) is often stereotyped (i.e., not adapted to the characteristics and needs of the individual patient in the specific stage of his/her illness) and not evidence‐based (the social skills training, cognitive remediation and family interventions that are validated by research are certainly not the most frequently used worldwide).
The sixth level of oversimplification can be recognized in the translation into ordinary practice of some principles upon which the vast majority of clinicians and researchers would agree: that the management of primary psychosis should be recovery‐oriented; that it should take into account the patient’s practical needs; and that the management plan will have to be agreed upon between the clinician(s) and the patient. It is indeed not common that a resilience‐promoting therapeutic environment and a focus on empowerment, identity, meaning and resilience is ensured in ordinary practice; that patients’ needs in terms of employment, housing, self‐care, social relationships and education are taken into account in the management plan; and that negotiation and shared decision‐making are really implemented 13 .
So, it could be argued that the availability of biological markers which can guide us in the choice of the most appropriate medication in an individual patient, so frequently emphasized in the literature, is only one of the unmet needs that we have today concerning the management of patients with primary psychosis. Further unmet needs are: a) an approach to management that considers the various treatment modalities found to be effective by research, and that incorporates the general principles of care agreed upon by the vast majority of clinicians; and b) the personalization of management on the basis of a clinical characterization of the individual patient beyond the mere diagnosis, which might become more systematic through the development of standardized decision tools.
The present paper represents an attempt to address these latter unmet needs. We describe the salient domains to be covered in the clinical characterization of the individual patient with primary psychosis aimed at personalization of management. We identify, within each domain, simple assessment instruments that can already be considered for use in ordinary clinical practice, and that can be included in comprehensive batteries of measures to be tested in large observational studies in order to guide the development of standardized decision tools 15 . Finally, we encourage a clinical practice taking into account all the available treatment modalities validated by research evidence, addressing the patient’s practical needs, and offering a focus on identity, meaning and resilience.
One could argue that clinicians do not like to use standardized assessment instruments in their routine practice, and that they often do not even use formal diagnostic systems in that practice. However, as we already pointed out in the paper on the clinical characterization of the patient with a diagnosis of depression 14 , our experience with the above diagnostic systems is very telling in this respect. Although those systems are seldom formally used in routine practice, several elements of their description of major mental disorders have been incorporated by most clinicians in their personal prototypes of those disorders, so that the reliability of psychiatric diagnosis has become today, although certainly far from optimal, much better than it was in the 1970s. Something similar may happen with respect to the clinical characterization of the patient with psychosis or depression: although only a minority of clinicians will formally adopt the standardized decision tools to be developed, it is likely that many of them will incorporate several elements of those tools in their ordinary practice, which may make the patient characterization more reliable and clinically useful than it is today.
Although group‐based comparisons constitute the scientific basis underlying academic psychiatry and psychology, the fact remains that individual patients are more likely to “escape” group‐based predictions than to behave in accordance. Clinicians are faced with individuals with largely unique combinations of symptoms, unique needs and unique treatment responses. Leaving this individual heterogeneity unaccounted for exposes patients and carers to disappointment and confusion as group‐based predictions do not materialize.
Furthermore, the assessment and management of primary psychosis is not a linear guideline affair, but an iterative process of “finding it out together”, requiring a solid therapeutic relationship characterized by genuine interest and curiosity, a caring attitude, and the ability to project trust and stimulate motivation. There is evidence that shared decision‐making results in a better patient‐clinician relationship and better outcomes in mental health settings162, 163, 324. Quality of care is something dynamic, plural and relational, which is established in a continuing collaborative process between patient and clinician.
We hope that the present paper will contribute to make the management of the patient with primary psychosis, in the real world, less stereotyped and more personalized, in the broadest sense of this latter word. We are open to comments and additions, which may be incorporated in a future updated version of the article.
ACKNOWLEDGEMENTS
Johan Detraux and Davy Vancampfort (University Psychiatric Centre KU Leuven, Kortenberg, Belgium) contributed to the section on physical comorbidities. Erika Jääskeläinen (University of Oulu, Finland) and John McGrath (Aarhus University, Denmark, and University of Queensland, St. Lucia, Australia) contributed to the section on family history.
REFERENCES
- 1. American Psychiatric Association . Diagnostic and statistical manual of mental disorders, 5th ed. Arlington: American Psychiatric Association, 2013. [Google Scholar]
- 2. World Health Organization . ICD‐11 guidelines. https://gcp.network/en/.
- 3. Green MF, Horan WP, Lee J. Nonsocial and social cognition in schizophrenia: current evidence and future directions. World Psychiatry 2019;18:146‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sartorius N, Chiu H, Heok KE et al. Name change for schizophrenia. Schizophr Bull 2014;40:255‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Perälä J, Suvisaari J, Saarni SI et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry 2007;64:19‐28. [DOI] [PubMed] [Google Scholar]
- 6. Verdoux H, Tournier M, Bégaud B. Antipsychotic prescribing trends: a review of pharmaco‐epidemiological studies. Acta Psychiatr Scand 2010;121:4‐10. [DOI] [PubMed] [Google Scholar]
- 7. Bighelli I, Salanti G, Huhn M et al. Psychological interventions to reduce positive symptoms in schizophrenia: a systematic review and network meta‐analysis. World Psychiatry 2018;17:316‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Drake RE, Essock SM. The science‐to‐service gap in real‐world schizophrenia treatment: the 95% problem. Schizophr Bull 2009;35:677‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. McFarlane WR. Family interventions for schizophrenia and the psychoses: a review. Family Process 2016;55:460‐82. [DOI] [PubMed] [Google Scholar]
- 10. Bond GR, Becker DR, Drake RE et al. Implementing supported employment as an evidence‐based practice. Psychiatr Serv 2001; 52:313‐22. [DOI] [PubMed] [Google Scholar]
- 11. De Hert M, Detraux J. Reversing the downward spiral for people with severe mental illness through educational innovations. World Psychiatry 2017;16:41‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fleischhacker WW, Arango C, Arteel P et al. Schizophrenia – time to commit to policy change. Schizophr Bull 2014;40(Suppl. 3):S165‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pincus HA, Spaeth‐Rublee B, Grant S et al. A review of mental health recovery programs in selected industrialized countries. Int J Ment Health Syst 2016;10:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Maj M, Stein DJ, Parker G et al. The clinical characterization of the adult patient with depression aimed at personalization of management. World Psychiatry 2020;19:269‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kessler RC. The potential of predictive analytics to provide clinical decision support in depression treatment planning. Curr Opin Psychiatry 2018;31:32‐9. [DOI] [PubMed] [Google Scholar]
- 16. Sass LA. Self‐disturbance and schizophrenia: structure, specificity, pathogenesis (current issues, new directions). Schizophr Res 2014;152:5‐11. [DOI] [PubMed] [Google Scholar]
- 17. Parnas J. The core Gestalt of schizophrenia. World Psychiatry 2012;11:67‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Parnas J, Møller P, Kircher T et al. EASE: Examination of Anomalous Self‐Experience. Psychopathology 2005;38:236‐58. [DOI] [PubMed] [Google Scholar]
- 19. Nordgaard J, Parnas J. Self‐disorders and the schizophrenia spectrum: a study of 100 first hospital admissions. Schizophr Bull 2014;40:1300‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cicero DC, Neis AM, Klaunig MJ et al. The Inventory of Psychotic‐Like Anomalous Self‐Experiences (IPASE): development and validation. Psychol Assess 2017;29:13‐25. [DOI] [PubMed] [Google Scholar]
- 21. Nelson B, Li E, Cicero DC et al. The construct validity of the Inventory of Psychotic‐Like Anomalous Self‐Experiences (IPASE) as a measure of minimal self‐disturbance: preliminary data. Early Interv Psychiatry 2019;13:686‐91. [DOI] [PubMed] [Google Scholar]
- 22. Yung AR, Yuen HP, McGorry PD et al. Mapping the onset of psychosis: the Comprehensive Assessment of At‐Risk Mental States. Aust N Z J Psychiatry 2005;39:964‐71. [DOI] [PubMed] [Google Scholar]
- 23. Konings M, Bak M, Hanssen M et al. Validity and reliability of the CAPE: a self‐report instrument for the measurement of psychotic experiences in the general population. Acta Psychiatr Scand 2006;114:55‐61. [DOI] [PubMed] [Google Scholar]
- 24. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 1987;13:261‐76. [DOI] [PubMed] [Google Scholar]
- 25. Kay SR, Opler RA, Fiszbein A. The Positive and Negative Syndrome Scale (PANSS) manual. Toronto: Multi‐Health Systems Inc., 2000. [Google Scholar]
- 26. Ostergaard SD, Lemming OM, Mors O et al. PANSS‐6: a brief rating scale for the measurement of severity in schizophrenia. Acta Psychiatr Scand 2016;133:436‐44. [DOI] [PubMed] [Google Scholar]
- 27. Lincoln TM, Ziegler M, Lüllmann E et al. Can delusions be self‐assessed? Concordance between self‐ and observer‐rated delusions in schizophrenia. Psychiatry Res 2010;178:249‐54. [DOI] [PubMed] [Google Scholar]
- 28. Carey TA, Mullan RJ. What is Socratic questioning? Psychother Theor Res Pract Train 2004;41:217‐26. [Google Scholar]
- 29. Huhn M, Nikolakopoulou A, Schneider‐Thoma J et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi‐episode schizophrenia: a systematic review and network meta‐analysis. Lancet 2019;394:939‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Howes OD, McCutcheon R, Agid O et al. Treatment‐resistant schizophrenia: Treatment Response and Resistance in Psychosis (TRRIP) Working Group consensus guidelines on diagnosis and terminology. Am J Psychiatry 2017;174:216‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gaebel W, Stricker J, Riesbeck M. The long‐term antipsychotic treatment of schizophrenia: a selective review of clinical guidelines and clinical case examples. Schizophr Res (in press). [DOI] [PubMed] [Google Scholar]
- 32. Correll CU, Rubio JM, Kane JM. What is the risk‐benefit ratio of long‐term antipsychotic treatment in people with schizophrenia? World Psychiatry 2018;17:149‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Murray RM, Quattrone D, Natesan S et al. Should psychiatrists be more cautious about the long‐term prophylactic use of antipsychotics? Br J Psychiatry 2016;209:361‐5. [DOI] [PubMed] [Google Scholar]
- 34. Palmier‐Claus J, Griffiths R, Murphy E et al. Cognitive behavioural therapy for thought disorder in psychosis. Psychosis 2017;9:347‐57. [Google Scholar]
- 35. Trower P, Birchwood M, Meaden A et al. Cognitive therapy for command hallucinations: randomised controlled trial. Br J Psychiatry 2004;184:312‐20. [DOI] [PubMed] [Google Scholar]
- 36. Peters ER, Moritz S, Schwannauer M et al. Cognitive Biases Questionnaire for psychosis. Schizophr Bull 2014;40:300‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bleuler E. Dementia praecox oder Gruppe der Schizophrenien. Leipzig: Deuticke, 1911. [Google Scholar]
- 38. Jackson JH. Selected writings. London: Hodder and Stoughton, 1931. [Google Scholar]
- 39. Harvey PD, Strassnig M. Predicting the severity of everyday functional disability in people with schizophrenia: cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry 2012;11:73‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Galderisi S, Rossi A, Rocca P et al. The influence of illness‐related variables, personal resources and context‐related factors on real‐life functioning of people with schizophrenia. World Psychiatry 2014;13:275‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Galderisi S, Mucci A, Buchanan RW et al. Negative symptoms of schizophrenia: new developments and unanswered research questions. Lancet Psychiatry 2018;5:664‐77. [DOI] [PubMed] [Google Scholar]
- 42. Kirkpatrick B, Fenton WS, Carpenter WT Jr et al. The NIMH‐MATRICS consensus statement on negative symptoms. Schizophr Bull 2006;32:214‐19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Strauss GP, Esfahlani FZ, Galderisi S et al. Network analysis reveals the latent structure of negative symptoms in schizophrenia. Schizophr Bull 2019;45:1033‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Marder SR, Galderisi S. The current conceptualization of negative symptoms in schizophrenia. World Psychiatry 2017;16:14‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mucci A, Merlotti E, Üçok A et al. Primary and persistent negative symptoms: concepts, assessments and neurobiological bases. Schizophr Res 2017;186:19‐28. [DOI] [PubMed] [Google Scholar]
- 46. Krause M, Zhu Y, Huhn M et al. Antipsychotic drugs for patients with schizophrenia and predominant or prominent negative symptoms: a systematic review and meta‐analysis. Eur Arch Psychiatry Clin Neurosci 2018;268:625‐39. [DOI] [PubMed] [Google Scholar]
- 47. Lutgens D, Gariepy G, Malla A. Psychological and psychosocial interventions for negative symptoms in psychosis: systematic review and meta‐analysis. Br J Psychiatry 2017;210:324‐32. [DOI] [PubMed] [Google Scholar]
- 48. Turner DT, McGlanaghy E, Cuijpers P et al. A meta‐analysis of social skills training and related interventions for psychosis. Schizophr Bull 2018;44:475‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Velthorst E, Koeter M, van der Gaag M et al. Adapted cognitive‐behavioural therapy required for targeting negative symptoms in schizophrenia: meta‐analysis and meta‐regression. Psychol Med 2015;45:453‐65. [DOI] [PubMed] [Google Scholar]
- 50. Cella M, Preti A, Edwards C et al. Cognitive remediation for negative symptoms of schizophrenia: a network meta‐analysis. Clin Psychol Rev 2017;52:43‐51. [DOI] [PubMed] [Google Scholar]
- 51. Kennedy NI, Lee WH, Frangou S. Efficacy of non‐invasive brain stimulation on the symptom dimensions of schizophrenia: a meta‐analysis of randomized controlled trials. Eur Psychiatry 2018;49:69‐77. [DOI] [PubMed] [Google Scholar]
- 52. Andreasen NC, Olsen S. Negative vs positive schizophrenia. Definition and validation. Arch Gen Psychiatry 1982;39:789‐94. [DOI] [PubMed] [Google Scholar]
- 53. Kirkpatrick B, Strauss GP, Nguyen L et al. The brief negative symptom scale: psychometric properties. Schizophr Bull 2011;37:300‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Kring AM, Gur RE, Blanchard JJ et al. The Clinical Assessment Interview for Negative Symptoms (CAINS): final development and validation. Am J Psychiatry 2013;170:165‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Peralta V, Gil‐Berrozpe G, Librero J et al. The symptom and domain structure of psychotic disorders: a network analysis approach. Schizophr Bull Open (in press).
- 56. Minor KS, Lysaker PH. Necessary, but not sufficient: links between neurocognition, social cognition, and metacognition in schizophrenia are moderated by disorganized symptoms. Schizophr Res 2014;159:198‐204. [DOI] [PubMed] [Google Scholar]
- 57. Rocca P, Galderisi S, Rossi A et al. Disorganization and real‐world functioning in schizophrenia: results from the multicenter study of the Italian Network for Research on Psychoses. Schizophr Res 2018;201:105‐12. [DOI] [PubMed] [Google Scholar]
- 58. Andreasen NC, Flaum M, Arndt S. The Comprehensive Assessment of Symptoms and History (CASH). An instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry 1992;49:615‐23. [DOI] [PubMed] [Google Scholar]
- 59. Broome MR, Bottlender R, Rossler M. et al (eds). The AMDP System. Manual for assessment and documentation of psychopathology in psychiatry, 9th ed Boston: Hogrefe, 2018. [Google Scholar]
- 60. Andreasen NC. Scale for the assessment of thought, language, and communication (TLC). Schizophr Bull 1986;12:473‐82. [DOI] [PubMed] [Google Scholar]
- 61. Peralta V, Cuesta MJ. Motor abnormalities: from neurodevelopmental to neurodegenerative through "functional" (neuro)psychiatric disorders. Schizophr Bull 2017;43:956‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bush G, Fink M, Petrides G et al. Catatonia. I. Rating scale and standardized examination. Acta Psychiatr Scand 1996;93:129‐36. [DOI] [PubMed] [Google Scholar]
- 63. Guy W. ECDEU assessment manual for psychopharmacology, revised. Rockville: US Department of Health, Education and Welfare, 1976. [Google Scholar]
- 64. Simpson GM, Angus JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand 1970;45(Suppl. 212):11‐9. [DOI] [PubMed] [Google Scholar]
- 65. Gerlach J, Korsgaard S, Clemmesen P et al. The St. Hans Rating Scale for extrapyramidal syndromes: reliability and validity. Acta Psychiatr Scand 1993;87:244‐52. [DOI] [PubMed] [Google Scholar]
- 66. Martino D, Karnik V, Osland S et al. Movement disorders associated with antipsychotic medication in people with schizophrenia: an overview of Cochrane reviews and meta‐analysis. Can J Psychiatry 2018;63:730‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Peralta V, Cuesta MJ. Characterization of affective domains within the nonaffective psychotic disorders. Schizophr Res 2009;111:61‐9. [DOI] [PubMed] [Google Scholar]
- 68. Gonzalez‐Pinto A, Gutierrez M, Mosquera F et al. First episode in bipolar disorder: misdiagnosis and psychotic symptoms. J Affect Disord 1998;50:41‐4. [DOI] [PubMed] [Google Scholar]
- 69. Addington D, Addington J, Maticka‐Tyndale E et al. Reliability and validity of a depression rating scale for schizophrenics. Schizophr Res 1992;6:201‐8. [DOI] [PubMed] [Google Scholar]
- 70. Lysaker PH, Pattison ML, Leonhardt BL et al. Insight in schizophrenia spectrum disorders: relationship with behavior, mood and perceived quality of life, underlying causes and emerging treatments. World Psychiatry 2018;17:12‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Amador XF, Strauss DH, Yale SA et al. Assessment of insight in psychosis. Am J Psychiatry 1993;150:873‐9. [DOI] [PubMed] [Google Scholar]
- 72. Beck AT, Baruch E, Balter JM et al. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr Res 2004;68:319‐29. [DOI] [PubMed] [Google Scholar]
- 73. Hor K, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol 2010; 24(Suppl. 4):81‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Posner K, Brown GK, Stanley B et al. The Columbia‐Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 2011;168:1266‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Breslau N, Roth T, Rosenthal L et al. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry 1996;39:411‐8. [DOI] [PubMed] [Google Scholar]
- 76. Xiang YT, Weng YZ, Leung CM et al. Prevalence and correlates of insomnia and its impact on quality of life in Chinese schizophrenia patients. Sleep 2009;32:1059. [PMC free article] [PubMed] [Google Scholar]
- 77. Alam A, Chengappa KR, Ghinassi F. Screening for obstructive sleep apnea among individuals with severe mental illness at a primary care clinic. Gen Hosp Psychiatry 2012;34:660‐4. [DOI] [PubMed] [Google Scholar]
- 78. van Os J, Reininghaus U. The clinical epidemiology of schizophrenia In: Kaplan B, Sadock J, Sadock V. et al (eds). Kaplan & Sadock’s comprehensive textbook of psychiatry, 10th ed London: Lippincott Williams & Wilkins, 2017. [Google Scholar]
- 79. Singh SP, Cooper JE, Fisher HL et al. Determining the chronology and components of psychosis onset: the Nottingham Onset Schedule (NOS). Schizophr Res 2005;80:117‐30. [DOI] [PubMed] [Google Scholar]
- 80. Perkins DO, Leserman J, Jarskog LF et al. Characterizing and dating the onset of symptoms in psychotic illness: the Symptom Onset in Schizophrenia (SOS) inventory. Schizophr Res 2000;44:1‐10. [DOI] [PubMed] [Google Scholar]
- 81. Sartorius N, Shapiro R, Kimura M et al. WHO International Pilot Study of Schizophrenia. Psychol Med 1972;2:422‐5. [DOI] [PubMed] [Google Scholar]
- 82. Johnstone EC, Frith CD, Crow TJ et al. The Northwick Park ’Functional' Psychosis Study: diagnosis and outcome. Psychol Med 1992;22:331‐46. [DOI] [PubMed] [Google Scholar]
- 83. Tsuang MT, Dempsey GM. Long‐term outcome of major psychoses. II. Schizoaffective disorder compared with schizophrenia, affective disorders, and a surgical control group. Arch Gen Psychiatry 1979;36:1302‐4. [DOI] [PubMed] [Google Scholar]
- 84. Susser E, Finnerty M, Mojtabai R et al. Reliability of the Life Chart Schedule for assessment of the long‐term course of schizophrenia. Schizophr Res 2000;42:67‐77. [DOI] [PubMed] [Google Scholar]
- 85. Menezes NM, Arenovich T, Zipursky RB. A systematic review of longitudinal outcome studies of first‐episode psychosis. Psychol Med 2006;36:1349‐62. [DOI] [PubMed] [Google Scholar]
- 86. Llewellyn‐Beardsley J, Rennick‐Egglestone S, Callard F et al. Characteristics of mental health recovery narratives: systematic review and narrative synthesis. PLoS One 2019;14:e0214678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Corrigan PW, Salzer M, Ralph RO et al. Examining the factor structure of the Recovery Assessment Scale. Schizophr Bull 2004;30:1035‐41. [DOI] [PubMed] [Google Scholar]
- 88. Carter L, Read J, Pyle M et al. The impact of causal explanations on outcome in people experiencing psychosis: a systematic review. Clin Psychol Psychother 2017;24:332‐47. [DOI] [PubMed] [Google Scholar]
- 89. Nuechterlein KH, Green MF, Kern R. Schizophrenia as a cognitive disorder: recent approaches to identifying its core cognitive components to aid treatment development In: Gattaz WF, Busatto G. (eds). Advances in schizophrenia research 2009. New York: Springer, 2009:267‐82. [Google Scholar]
- 90. Cornblatt B, Obuchowski M, Roberts S et al. Cognitive and behavioral precursors of schizophrenia. Dev Psychopathol 1999;11:487‐508. [DOI] [PubMed] [Google Scholar]
- 91. Nuechterlein KH, Dawson ME, Gitlin M et al. Developmental processes in schizophrenic disorders: longitudinal studies of vulnerability and stress. Schizophr Bull 1992;18:387‐425. [DOI] [PubMed] [Google Scholar]
- 92. Snitz BE, MacDonald AW 3rd, Carter CS. Cognitive deficits in unaffected first‐degree relatives of schizophrenia patients: a meta‐analytic review of putative endophenotypes. Schizophr Bull 2006;32:179‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 1996;153:321‐30. [DOI] [PubMed] [Google Scholar]
- 94. Marder SR, Fenton W. Measurement and Treatment Research to Improve Cognition in Schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schizophr Res 2004;72:5‐9. [DOI] [PubMed] [Google Scholar]
- 95. Nuechterlein KH, Barch DM, Gold JM et al. Identification of separable cognitive factors in schizophrenia. Schizophr Res 2004;72:29‐39. [DOI] [PubMed] [Google Scholar]
- 96. Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: a quantitative review of the evidence. Neuropsychology 1998;12:426‐45. [DOI] [PubMed] [Google Scholar]
- 97. Kern RS, Gold JM, Dickinson D et al. The MCCB impairment profile for schizophrenia outpatients: results from the MATRICS psychometric and standardization study. Schizophr Res 2011;126:124‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Grant PM, Best MW, Beck AT. The meaning of group differences in cognitive test performance. World Psychiatry 2019;18:163‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Green MF, Kern RS, Braff DL et al. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull 2000;26:119‐36. [DOI] [PubMed] [Google Scholar]
- 100. Fett AKJ, Viechtbauer W, Dominguez MG et al. The relationship between neurocognition and social cognition and functional outcomes in schizophrenia: a meta‐analysis. Neurosci Biobehav Rev 2011;35:573‐88. [DOI] [PubMed] [Google Scholar]
- 101. Nuechterlein KH, Green MF, Kern RS et al. The MATRICS Consensus Cognitive Battery, part 1: Test selection, reliability, and validity. Am J Psychiatry 2008;165:203‐13. [DOI] [PubMed] [Google Scholar]
- 102. Nuechterlein KH, Green MF. MATRICS Consensus Cognitive Battery Manual, 3rd ed. Los Angeles: MATRICS Assessment, Inc., 2016. [Google Scholar]
- 103. Robbins TW, James M, Owen AM et al. Cambridge Neuropsychological Test Automated Battery (CANTAB): a factor analytic study of a large sample of normal elderly volunteers. Dementia 1994;5:266‐81. [DOI] [PubMed] [Google Scholar]
- 104. Pietrzak RH, Olver J, Norman T et al. A comparison of the CogState Schizophrenia Battery and the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) Battery in assessing cognitive impairment in chronic schizophrenia. J Clin Exp Neuropsychol 2009;31:848‐59. [DOI] [PubMed] [Google Scholar]
- 105. Keefe RSE, Goldberg TE, Harvey PD et al. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res 2004;68:283‐97. [DOI] [PubMed] [Google Scholar]
- 106. Randolph C, Tierney MC, Mohr E et al. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): preliminary clinical validity. J Clin Exp Neuropsychol 1998;20:310‐9. [DOI] [PubMed] [Google Scholar]
- 107. Velligan DI, DiCocco M, Bow‐Thomas CC et al. A brief cognitive assessment for use with schizophrenia patients in community clinics. Schizophr Res 2004;71:273‐83. [DOI] [PubMed] [Google Scholar]
- 108. Hurford IM, Marder SR, Keefe RS et al. A brief cognitive assessment tool for schizophrenia: construction of a tool for clinicians. Schizophr Bull 2011;37:538‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Ventura J, Reise SP, Keefe RS et al. The Cognitive Assessment Interview (CAI): reliability and validity of a brief interview‐based measure of cognition. Schizophr Bull 2013;39:583‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Keefe RS, Poe M, Walker TM et al. The Schizophrenia Cognition Rating Scale: an interview‐based assessment and its relationship to cognition, real‐world functioning, and functional capacity. Am J Psychiatry 2006;163:426‐32. [DOI] [PubMed] [Google Scholar]
- 111. Wykes T, Huddy V, Cellard C et al. A meta‐analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am J Psychiatry 2011;168:472‐85. [DOI] [PubMed] [Google Scholar]
- 112. Firth J, Stubbs B, Rosenbaum S et al. Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta‐analysis. Schizophr Bull 2017;43:546‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Nuechterlein KH, Ventura J, McEwen SC et al. Enhancing cognitive training through aerobic exercise after a first schizophrenia episode: theoretical conception and pilot study. Schizophr Bull 2016;42(Suppl. 1):S44‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Best MW, Milanovic M, Iftene F et al. A randomized controlled trial of executive functioning training compared with perceptual training for schizophrenia spectrum disorders: effects on neurophysiology, neurocognition, and functioning. Am J Psychiatry 2019;176:297‐306. [DOI] [PubMed] [Google Scholar]
- 115. Medalia A, Saperstein AM, Qian M et al. Impact of baseline early auditory processing on response to cognitive remediation for schizophrenia. Schizophr Res 2019;208:397‐405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Green MF, Penn DL, Bentall R et al. Social cognition in schizophrenia: an NIMH workshop on definitions, assessment, and research opportunities. Schizophr Bull 2008;34:1211‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Savla GN, Vella L, Armstrong CC et al. Deficits in domains of social cognition in schizophrenia: a meta‐analysis of the empirical evidence. Schizophr Bull 2013;39:979‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Healey KM, Bartholomeusz CF, Penn DL. Deficits in social cognition in first episode psychosis: a review of the literature. Clin Psychol Rev 2016;50:108‐37. [DOI] [PubMed] [Google Scholar]
- 119. Nahum M, Fisher M, Loewy R et al. A novel, online social cognitive training program for young adults with schizophrenia: a pilot study. Schizophr Res Cogn 2014;1:e11‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Kurtz MM, Gagen E, Rocha NBF et al. Comprehensive treatments for social cognitive deficits in schizophrenia: a critical review and effect‐size analysis of controlled studies. Clin Psychol Rev 2016;43:80‐9. [DOI] [PubMed] [Google Scholar]
- 121. Horan WP, Dolinsky M, Lee J et al. Social cognitive skills training for psychosis with community‐based training exercises: a randomized controlled trial. Schizophr Bull 2018;44:1254‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Burkner PC, Williams DR, Simmons TC et al. Intranasal oxytocin may improve high‐level social cognition in schizophrenia, but not social cognition or neurocognition in general: a multilevel Bayesian meta‐analysis. Schizophr Bull 2017;43:1291‐303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Davis MC, Green MF, Lee J et al. Oxytocin‐augmented social cognitive skills training in schizophrenia. Neuropsychopharmacology 2014;39:2070‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Pinkham AE, Penn DL, Green MF et al. Social cognition psychometric evaluation: results of the Initial Psychometric Study. Schizophr Bull 2016;42:494‐504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Kern RS, Penn DL, Lee J et al. Adapting social neuroscience measures for schizophrenia clinical trials, part 2: Trolling the depths of psychometric properties. Schizophr Bull 2013;39:1201‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Horan WP, Green MF. Treatment of social cognition in schizophrenia: current status and future directions. Schizophr Res 2019;203:3‐11. [DOI] [PubMed] [Google Scholar]
- 127. McDonald S, Flanagan S, Rollins J. The Awareness of Social Inference Test. Suffolk: Thames Valley Test Company, 2002. [Google Scholar]
- 128. Mayer JD, Salovey P, Caruso DR. Mayer‐Salovey‐Caruso Emotional Intelligence Test (MSCEIT) user’s manual. Toronto: MHS Publishers, 2002. [Google Scholar]
- 129. Bryson G, Bell M, Lysaker P. Affect recognition in schizophrenia: a function of global impairment or a specific cognitive deficit. Psychiatry Res 1997;71:105‐13. [DOI] [PubMed] [Google Scholar]
- 130. Kraepelin E. Psychiatrie. Ein Lehrbuch für Studirende und Aerzte. Fünfte, vollständig umgearbeitete Auflage. Leipzig: Barth, 1896. [Google Scholar]
- 131. Fish B. The detection of schizophrenia in infancy: a preliminary report. J Nerv Ment Dis 1957;125:1‐24. [DOI] [PubMed] [Google Scholar]
- 132. Weinberger DR. Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry 1987;44:660‐9. [DOI] [PubMed] [Google Scholar]
- 133. Murray RM, Lewis SW. Is schizophrenia a neurodevelopmental disorder? BMJ 1987;295:681‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Jones P, Rodgers B, Murray R et al. Child development risk factors for adult schizophrenia in the British 1946 birth cohort. Lancet 1994;344:1398‐402. [DOI] [PubMed] [Google Scholar]
- 135. Isohanni M, Jones PB, Moilanen K et al. Early developmental milestones in adult schizophrenia and other psychoses. A 31‐year follow‐up of the Northern Finland 1966 Birth Cohort. Schizophr Res 2001;52:1‐19. [DOI] [PubMed] [Google Scholar]
- 136. Cannon M, Caspi A, Moffitt TE et al. Evidence for early‐childhood, pan‐developmental impairment specific to schizophreniform disorder: results from a longitudinal birth cohort. Arch Gen Psychiatry 2002;59:449‐56. [DOI] [PubMed] [Google Scholar]
- 137. Khandaker GM, Barnett JH, White IR et al. A quantitative meta‐analysis of population‐based studies of premorbid intelligence and schizophrenia. Schizophr Res 2011;132:220‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Heinrichs DW, Buchanan RW. Significance and meaning of neurological signs in schizophrenia. Am J Psychiatry 1988;145:11‐8. [DOI] [PubMed] [Google Scholar]
- 139. Fish B, Marcus J, Hans SL et al. Infants at risk for schizophrenia: sequelae of a genetic neurointegrative defect. Arch Gen Psychiatry 1992;49:221‐35. [DOI] [PubMed] [Google Scholar]
- 140. Green MF, Satz P, Christenson C. Minor physical anomalies in schizophrenia patients, bipolar patients, and their siblings. Schizophr Bull 1994;20:433‐40. [DOI] [PubMed] [Google Scholar]
- 141. Larson FV, Wagner AP, Jones PB et al. Psychosis in autism: comparison of the features of both conditions in a dually affected cohort. Br J Psychiatry 2017;210:269‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Downs JM, Lechler S, Dean H et al. The association between comorbid autism spectrum disorders and antipsychotic treatment failure in early‐onset psychosis: a historical cohort study using electronic health records. J Clin Psychiatry 2017;78:e1233‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Khandaker GM, Stochl J, Zammit S et al. A population‐based longitudinal study of childhood neurodevelopmental disorders, IQ and subsequent risk of psychotic experiences in adolescence. Psychol Med 2014;44:3229‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Sanders RD, Keshavan MS. The neurologic examination in adult psychiatry: from soft signs to hard science. J Neuropsychiatry Clin Neurosci 1998;10:395‐404. [DOI] [PubMed] [Google Scholar]
- 145. Chen EY, Shapleske J, Luque R et al. The Cambridge Neurological Inventory: a clinical instrument for assessment of soft neurological signs in psychiatric patients. Psychiatry Res 1995;56:183‐204. [DOI] [PubMed] [Google Scholar]
- 146. Buchanan RW, Heinrichs DW. The Neurological Evaluation Scale (NES): a structured instrument for the assessment of neurological signs in schizophrenia. Psychiatry Res 1989;27:335‐50. [DOI] [PubMed] [Google Scholar]
- 147. Cannon‐Spoor H, Potkin S, Wyatt R. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull 1982;8:470‐84. [DOI] [PubMed] [Google Scholar]
- 148. Van Mastrigt S, Addington J. Assessment of premorbid function in first‐episode schizophrenia: modifications to the Premorbid Adjustment Scale. J Psychiatry Neurosci 2002;27:92‐101. [PMC free article] [PubMed] [Google Scholar]
- 149. Leung WW, Bowie CR, Harvey PD. Functional implications of neuropsychological normality and symptom remission in older outpatients diagnosed with schizophrenia: a cross‐sectional study. J Int Neuropsychol Soc 2008;14:479‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Granholm E, Holden JL, Mikhael T et al. What do people with schizophrenia do all day? Ecological momentary assessment of real‐world functioning in schizophrenia. Schizophr Bull 2020;46:242‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Gard DE, Kring AM, Gard MG et al. Anhedonia in schizophrenia: distinctions between anticipatory and consummatory pleasure. Schizophr Res 2007;93:253‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Sitzer DI, Twamley EW, Patterson TL et al. Multivariate predictors of social skills performance in middle‐aged and older out‐patients with schizophrenia spectrum disorders. Psychol Med 2008;38:755‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Robertson BR, Prestia D, Twamley EW et al. Social competence versus negative symptoms as predictors of real world social functioning in schizophrenia. Schizophr Res 2014;160:136‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Granholm E, Holden J, Link PC et al. Randomized clinical trial of cognitive behavioral social skills training for schizophrenia: improvement in functioning and experiential negative symptoms. J Consult Clin Psychol 2014;82:1173‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Harvey PD, Raykov T, Twamley EW et al. Validating the measurement of real‐world functional outcomes: phase I results of the VALERO study. Am J Psychiatry 2011;168:1195‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Morosini PL, Magliano L, Brambilla L et al. Development, reliability and acceptability of a new version of the DSM‐IV social and occupational functioning assessment scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand 2000;101:323‐9. [PubMed] [Google Scholar]
- 157. Gard DE, Gard MG, Kring AM et al. Anticipatory and consummatory components of the experience of pleasure: a scale development study. J Res Pers 2006;40:1086‐102. [Google Scholar]
- 158. Llerena K, Park SG, McCarthy JM et al. The Motivation and Pleasure Scale‐Self‐Report (MAP‐SR): reliability and validity of a self‐report measure of negative symptoms. Compr Psychiatry 2013;54:568‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Schlosser DA, Campellone TR, Truong B et al. Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia. Schizophr Bull 2018;44:1010‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Tolman AW, Kurtz MM. Neurocognitive predictors of objective and subjective quality of life in individuals with schizophrenia: a meta‐analytic investigation. Schizophr Bull 2012;38:304‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Durand D, Strassnig M, Sabbag S et al. Factors influencing self‐assessment of cognition and functioning in schizophrenia: implications for treatment studies. Eur Neuropsychopharmacol 2015;25:185‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.World Health Organization. The World Health Organization Quality of Life (WHOQOL). www.who.int.
- 163. Button B. Quality of Well‐Being (QWB) Scale In: Michalos AC. (eds). Encyclopedia of quality of life and well‐being research. Dordrecht: Springer, 2016. [Google Scholar]
- 164. Slade M, Leese M, Ruggeri M et al. Does meeting needs improve quality of life? Psychother Psychosom 2004;73:183‐9. [DOI] [PubMed] [Google Scholar]
- 165. Drukker M, van Dillen K, Bak M et al. The use of the Camberwell Assessment of Need in treatment: what unmet needs can be met? Soc Psychiatry Psychiatr Epidemiol 2008;43:410‐7. [DOI] [PubMed] [Google Scholar]
- 166. Maslow AH. Toward a psychology of being. Princeton: Van Nostrand, 1962. [Google Scholar]
- 167. Lasalvia A, Bonetto C, Tansella M et al. Does staff‐patient agreement on needs for care predict a better mental health outcome? A 4‐year follow‐up in a community service. Psychol Med 2008;38:123‐33. [DOI] [PubMed] [Google Scholar]
- 168. Puschner B, Becker T, Mayer B et al. Clinical decision making and outcome in the routine care of people with severe mental illness across Europe (CEDAR). Epidemiol Psychiatr Sci 2016;25:69‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Drukker M, Joore M, van Os J et al. The use of a cumulative needs for care monitor for individual treatment v. care as usual for patients diagnosed with severe mental illness, a cost‐effectiveness analysis from the health care perspective. Epidemiol Psychiatr Sci 2012;21:381‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Drukker M, van Os J, Dietvorst M et al. Does monitoring need for care in patients diagnosed with severe mental illness impact on psychiatric service use? Comparison of monitored patients with matched controls. BMC Psychiatry 2011;11:45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Drukker M, van Os J, Bak M et al. Systematic monitoring of needs for care and global outcomes in patients with severe mental illness. BMC Psychiatry 2010;10:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Slade M, Phelan M, Thornicroft G et al. The Camberwell Assessment of Need (CAN): comparison of assessments by staff and patients of the needs of the severely mentally ill. Soc Psychiatry Psychiatr Epidemiol 1996;31:109‐13. [DOI] [PubMed] [Google Scholar]
- 173. Phelan M, Slade M, Thornicroft G et al. The Camberwell Assessment of Need: the validity and reliability of an instrument to assess the needs of people with severe mental illness. Br J Psychiatry 1995;167:589‐95. [DOI] [PubMed] [Google Scholar]
- 174. Bond GR, Drake RE, Becker DR. An update on Individual Placement and Support. World Psychiatry 2020;19:390‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. McGorry PD, Hickie IB. (eds). Clinical staging in psychiatry: making diagnosis work for research and treatment. Cambridge: Cambridge University Press, 2019. [Google Scholar]
- 176. McGorry PD, Hickie IB, Yung AR et al. Clinical staging of psychiatric disorders: a heuristic framework for choosing earlier, safer and more effective interventions. Aust N Z J Psychiatry 2006;40:616‐22. [DOI] [PubMed] [Google Scholar]
- 177. Shah JL, Scott J, McGorry PD et al. Transdiagnostic clinical staging in youth mental health: a first international consensus statement. World Psychiatry 2020;19:233‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Fava GA, Kellner R. Staging: a neglected dimension in psychiatric classification. Acta Psychiatr Scand 1993;87:225‐30. [DOI] [PubMed] [Google Scholar]
- 179. McGorry PD, Hartmann JA, Spooner R et al. Beyond the “at risk mental state” concept: transitioning to transdiagnostic psychiatry. World Psychiatry 2018;17:133‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. McGorry PD, Ratheesh A, O’Donoghue B. Early intervention – an implementation challenge for 21st century mental health care. JAMA Psychiatry 2018;75:545‐6. [DOI] [PubMed] [Google Scholar]
- 181. Correll CU, Galling B, Pawar A et al. Comparison of early intervention services vs treatment as usual for early‐phase psychosis: a systematic review, meta‐analysis, and meta‐regression. JAMA Psychiatry 2018;75:555‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Frances A. Saving normal: an insider’s revolt against out‐of‐control psychiatric diagnosis, DSM‐5, big pharma, and the medicalization of ordinary life. New York: Morrow, 2013. [Google Scholar]
- 183. Insel TR. The arrival of preemptive psychiatry. Early Interv Psychiatry 2007;1:5‐6. [DOI] [PubMed] [Google Scholar]
- 184. Hegelstad WT, Larsen TK, Auestad B et al. Long‐term follow‐up of the TIPS early detection in psychosis study: effects on 10‐year outcome. Am J Psychiatry 2012;169:374‐80. [DOI] [PubMed] [Google Scholar]
- 185. Kane JM, Robinson DG, Schooler NR et al. Comprehensive versus usual community care for first‐episode psychosis: 2‐year outcomes from the NIMH RAISE Early Treatment Program. Am J Psychiatry 2016;173:362‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Francey S, O’Donoghue B, Nelson B et al. Psychosocial intervention with or without antipsychotic medication for first episode psychosis: a randomized noninferiority clinical trial. Schizophr Bull Open (in press). [Google Scholar]
- 187. Orygen . Australian clinical guidelines for early psychosis, 2nd ed Melbourne: Orygen, The National Centre of Excellence in Youth Mental Health, 2016. [DOI] [PubMed] [Google Scholar]
- 188. Thien K, Bowtell M, Eaton S et al. Clozapine use in early psychosis. Schizophr Res 2018;199:374‐9. [DOI] [PubMed] [Google Scholar]
- 189. Killackey E, Allott K, Jackson HJ et al. Individual placement and support for vocational recovery in first‐episode psychosis: randomised controlled trial. Br J Psychiatry 2019;214:76‐82. [DOI] [PubMed] [Google Scholar]
- 190. Wunderink L, Nieboer RM, Wiersma D et al. Recovery in remitted first‐episode psychosis at 7 years of follow‐up of an early dose reduction/discontinuation or maintenance treatment strategy: long‐term follow‐up of a 2‐year randomized clinical trial. JAMA Psychiatry 2013;70:913‐20. [DOI] [PubMed] [Google Scholar]
- 191. First MB, Williams JBW, Karg RS et al. Structured Clinical Interview for DSM‐5 – Research Version. Arlington: American Psychiatric Association, 2015. [Google Scholar]
- 192. Upthegrove R, Marwaha S, Birchwood M. Depression and schizophrenia: cause, consequence, or trans‐diagnostic issue? Schizophr Bull 2017;43:240‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Heimberg RG, Horner KJ, Juster HR et al. Psychometric properties of the Liebowitz Social Anxiety Scale. Psychol Med 1999;29:199‐212. [DOI] [PubMed] [Google Scholar]
- 194. Sharma LP, Reddy YCJ. Obsessive‐compulsive disorder comorbid with schizophrenia and bipolar disorder. Indian J Psychiatry 2019;61(Suppl. 1):S140‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Goodman WK, Price LH, Rasmussen SA et al. The Yale‐Brown Obsessive Compulsive Scale: I. Development, use, and reliability. Arch Gen Psychiatry 1989;46:1006‐11. [DOI] [PubMed] [Google Scholar]
- 196. Malaspina D, Walsh‐Messinger J, Brunner A et al. Features of schizophrenia following premorbid eating disorders. Psychiatry Res 2019;278:275‐80. [DOI] [PubMed] [Google Scholar]
- 197. Peralta V, de Jalón EG, Campos MS et al. The meaning of childhood attention‐deficit hyperactivity symptoms in patients with a first‐episode of schizophrenia‐spectrum psychosis. Schizophr Res 2011;126:28‐35. [DOI] [PubMed] [Google Scholar]
- 198. Hartz SM, Pato CN, Medeiros H et al. Comorbidity of severe psychotic disorders with measures of substance use. JAMA Psychiatry 2014;71:248‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Hare RD. The Hare Psychopathy Checklist‐Revised. North Tonawanda: Multi‐Health Systems, 1991. [Google Scholar]
- 200. Oakley P, Kisely S, Baxter A, et al. Increased mortality among people with schizophrenia and other non‐affective psychotic disorders in the community: a systematic review and meta‐analysis. J Psychiatr Res 2018;102:245‐53. [DOI] [PubMed] [Google Scholar]
- 201. De Hert M, Correll CU, Bobes J et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 2011;10:52‐77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Correll CU, Detraux J, De Lepeleire J et al. Effects of antipsychotics, antidepressants and mood stabilizers on risk for physical diseases in people with schizophrenia, depression and bipolar disorder. World Psychiatry 2015;14:119‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Firth J, Siddiqi N, Koyanagi A et al. The Lancet Psychiatry Commission: a blueprint for protecting physical health in people with mental illness. Lancet Psychiatry 2019;6:675‐712. [DOI] [PubMed] [Google Scholar]
- 204. Vancampfort D, Stubbs B, Mitchell AJ et al. Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta‐analysis. World Psychiatry 2015;14:339‐47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. De Hert M, Detraux J, Vancampfort D. The intriguing relationship between coronary heart disease and mental disorders. Dialogues Clin Neurosci 2018;20:31‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Vancampfort D, Correll CU, Galling B et al. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta‐analysis. World Psychiatry 2016;15:166‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Correll CU, Solmi M, Veronese N et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large‐scale meta‐analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry 2017;16:163‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. De Hert M, Cohen D, Bobes J et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry 2011;10:138‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018;138:e426‐83. [DOI] [PubMed] [Google Scholar]
- 210. Garg N, Muduli SK, Kapoor A et al. Comparison of different cardiovascular risk score calculators for cardiovascular risk prediction and guideline recommended statin uses. Indian Heart J 2017;69:458‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. WHO CVD Risk Chart Working Group . World Health Organization cardiovascular disease risk charts: revised models to estimate risk in 21 global regions. Lancet Glob Health 2019;7:e1332‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Hippisley‐Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 2017;357:j2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Yusuf S, Joseph P, Rangarajan S et al. Modifiable risk factors, cardiovascular disease, and mortality in 155,722 individuals from 21 high‐income, middle‐income, and low‐income countries (PURE): a prospective cohort study. Lancet 2020;395:795‐808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Rosengren A, Hawken S, Ounpuu S et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case‐control study. Lancet 2004;364:953‐62. [DOI] [PubMed] [Google Scholar]
- 215. Vancampfort D, Firth J, Schuch FB et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: a global systematic review and meta‐analysis. World Psychiatry 2017;16:308‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Annamalai A, Tek C. An overview of diabetes management in schizophrenia patients: office based strategies for primary care practitioners and endocrinologists. Int J Endocrinol 2015;2015:969182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Vancampfort D, Firth J, Correll CU et al. The impact of pharmacological and non‐pharmacological interventions to improve physical health outcomes in people with schizophrenia: a meta‐review of meta‐analyses of randomized controlled trials. World Psychiatry 2019;18:53‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Tumiel E, Wichniak A, Jarema M et al. Nonpharmacological interventions for the treatment of cardiometabolic risk factors in people with schizophrenia – a systematic review. Front Psychiatry 2019;10:566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Luo F, Das A, Chen J et al. Metformin in patients with and without diabetes: a paradigm shift in cardiovascular disease management. Cardiovasc Diabetol 2019;18:54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. McGinty EE, Baller J, Azrin ST et al. Interventions to address medical conditions and health risk behaviors among persons with serious mental illness: a comprehensive review. Schizophr Bull 2016;42:96‐124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Shawen AE, Drayton SJ. Review of pharmacotherapy for smoking cessation in patients with schizophrenia. Ment Health Clin 2018;8:78‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Gates J, Killackey E, Phillips L et al. Mental health starts with physical health: current status and future directions of non‐pharmacological interventions to improve physical health in first‐episode psychosis. Lancet Psychiatry 2015;2:726‐42. [DOI] [PubMed] [Google Scholar]
- 223. Torous J, Andersson G, Bertagnoli A et al. Towards a consensus around standards for smartphone apps and digital mental health. World Psychiatry 2019;18:97‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Rasic D, Hajek T, Alda M et al. Risk of mental illness in offspring of parents with schizophrenia, bipolar disorder, and major depressive disorder: a meta‐analysis of family high‐risk studies. Schizophr Bull 2014;40:28‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Yang J, Visscher PM, Wray NR. Sporadic cases are the norm for complex disease. Eur J Hum Genet 2010;18:1039‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Mortensen PB, Pedersen MG, Pedersen CB. Psychiatric family history and schizophrenia risk in Denmark: which mental disorders are relevant? Psychol Med 2010;40:201‐10. [DOI] [PubMed] [Google Scholar]
- 227. Cross‐Disorder Group of the Psychiatric Genomics Consortium , Lee SH, Ripke S et al. Genetic relationship between five psychiatric disorders estimated from genome‐wide SNPs. Nat Genet 2013;45:984‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Cross‐Disorder Group of the Psychiatric Genomics Consortium , Genetic Risk Outcome of Psychosis Consortium. Identification of risk loci with shared effects on five major psychiatric disorders: a genome‐wide analysis. Lancet 2013;381:1371‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Agerbo E, Sullivan PF, Vilhjalmsson BJ et al. Polygenic risk score, parental socioeconomic status, family history of psychiatric disorders, and the risk for schizophrenia: a Danish population‐based study and meta‐analysis. JAMA Psychiatry 2015;72:635‐41. [DOI] [PubMed] [Google Scholar]
- 230. Vigod SN, Kurdyak PA, Dennis CL et al. Maternal and newborn outcomes among women with schizophrenia: a retrospective population‐based cohort study. BJOG 2014;121:566‐74. [DOI] [PubMed] [Google Scholar]
- 231. Zhong QY, Gelaye B, Fricchione GL et al. Adverse obstetric and neonatal outcomes complicated by psychosis among pregnant women in the United States. BMC Pregnancy Childbirth 2018;18:120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Gantriis DL, Thorup AAE, Harder S et al. Home visits in the Danish High Risk and Resilience Study ‐ VIA 7: assessment of the home environment of 508 7‐year‐old children born to parents diagnosed with schizophrenia or bipolar disorder. Acta Psychiatr Scand 2019;140:126‐34. [DOI] [PubMed] [Google Scholar]
- 233. Simoila L, Isometsa E, Gissler M et al. Maternal schizophrenia and out‐of‐home placements of offspring: a national follow‐up study among Finnish women born 1965‐1980 and their children. Psychiatry Res 2019;273:9‐14. [DOI] [PubMed] [Google Scholar]
- 234. de Sousa P, Varese F, Sellwood W et al. Parental communication and psychosis: a meta‐analysis. Schizophr Bull 2014;40:756‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Ranning A, Laursen T, Agerbo E et al. School performance from primary education in the adolescent offspring of parents with schizophrenia and bipolar disorder – a national, register‐based study. Psychol Med 2018;48:1993‐2000. [DOI] [PubMed] [Google Scholar]
- 236. Kallquist A, Salzmann‐Erikson M. Experiences of having a parent with serious mental illness: an interpretive meta‐synthesis of qualitative literature. J Child Fam Stud 2019;28:2056‐68. [Google Scholar]
- 237. NIMH Genetics Initiative. Family Interview for Genetic Studies (FIGS). Rockville: National Institute of Mental Health, 1992. [Google Scholar]
- 238. Nurnberger JI Jr, Blehar MC, Kaufmann CA et al. Diagnostic interview for genetic studies. Rationale, unique features, and training. NIMH Genetics Initiative. Arch Gen Psychiatry 1994;51:849‐59. [DOI] [PubMed] [Google Scholar]
- 239. Weissman MM, Wickramaratne P, Adams P et al. Brief screening for family psychiatric history: the Family History Screen. Arch Gen Psychiatry 2000;57:675‐82. [DOI] [PubMed] [Google Scholar]
- 240. Esterberg ML, Trotman HD, Holtzman C et al. The impact of a family history of psychosis on age‐at‐onset and positive and negative symptoms of schizophrenia: a meta‐analysis. Schizophr Res 2010;120:121‐30. [DOI] [PubMed] [Google Scholar]
- 241. Kakela J, Panula J, Oinas E et al. Family history of psychosis and social, occupational and global outcome in schizophrenia: a meta‐analysis. Acta Psychiatr Scand 2014;130:269‐78. [DOI] [PubMed] [Google Scholar]
- 242. Immonen J, Jaaskelainen E, Korpela H et al. Age at onset and the outcomes of schizophrenia: a systematic review and meta‐analysis. Early Interv Psychiatry 2017;11:453‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. Kowalec K, Lu Y, Sariaslan A et al. Increased schizophrenia family history burden and reduced premorbid IQ in treatment‐resistant schizophrenia: a Swedish National Register and Genomic Study. Mol Psychiatry (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Mirdal GKM, Mednick SA, Schulsinger F et al. Perinatal complications in children of schizophrenic mothers. Acta Psychiatr Scand 1974;50:553‐6. [DOI] [PubMed] [Google Scholar]
- 245. McNeil TF, Kaij L. Obstetric factors in the development of schizophrenia: complications in the birth of preschizophrenics and in reproduction by schizophrenic parents In: Wynne LC, Cromwell RL, Matthysse S. (eds). The nature of schizophrenia. New York: Wiley, 1978:401‐29. [Google Scholar]
- 246. Lewis SW, Murray RM. Obstetric complications, neurodevelopmental deviance, and risk of schizophrenia. J Psychiatr Res 1987;21:413‐21. [DOI] [PubMed] [Google Scholar]
- 247. Cannon M, Jones PB, Murray RM. Obstetric complications and schizophrenia: historical and meta‐analytical review. Am J Psychiatry 2002;159:1080‐92. [DOI] [PubMed] [Google Scholar]
- 248. Davies C, Segre G, Estradé A et al. Prenatal and perinatal risk factors for psychosis: a meta‐analysis. Lancet Psychiatry 2020;7:399‐41. [DOI] [PubMed] [Google Scholar]
- 249. Walshe M, McDonald C, Boydell J et al. Long‐term maternal recall of obstetric complications in schizophrenia research. Psychiatry Res 2011;187:335‐40. [DOI] [PubMed] [Google Scholar]
- 250. Lewis SW, Murray RM, Owen MJ. Obstetric complications in schizophrenia: methodology and mechanisms In: Schulz SC, Tamminga CA. (eds). Schizophrenia: scientific progress. New York: Oxford University Press, 1989:56‐68. [Google Scholar]
- 251. McNeil TF, Sjöström K. A comprehensive scale for assessing obstetric complications. Malmo: Lund University, 1994. [Google Scholar]
- 252. Breeman LD, Jaekel J, Baumann N et al. Preterm cognitive function into adulthood. Pediatrics 2015;136:415‐23. [DOI] [PubMed] [Google Scholar]
- 253. Karolis VR, Froudist‐Walsh S, Kroll J et al. Volumetric grey matter alterations in adolescents and adults born very preterm suggest accelerated brain maturation. Neuroimage 2017;163:379‐89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Froudist‐Walsh S, Bloomfield MA, Veronese M et al. The effect of perinatal brain injury on dopaminergic function and hippocampal volume in adult life. eLife 2017;6:e29088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255. Radua J, Ramella‐Cravaro V, Ioannidis JP et al. What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry 2018;17:49‐66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256. Belbasis L, Köhler C, Stefanis N et al. Risk factors and peripheral biomarkers for schizophrenia spectrum disorders: an umbrella review of meta‐analyses. Acta Psychiatr Scand 2018;137:88‐97. [DOI] [PubMed] [Google Scholar]
- 257. Morgan C, Knowles G, Hutchinson G. Migration, ethnicity and psychoses: evidence, models and future directions. World Psychiatry 2019;18:247‐58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. Guloksuz S, Rutten BP, Pries L‐K et al. The complexities of evaluating the exposome in psychiatry: a data‐driven illustration of challenges and some propositions for amendments. Schizophr Bull 2018;44:1175‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Hailes HP, Yu R, Danese A et al. Long‐term outcomes of childhood sexual abuse: an umbrella review. Lancet Psychiatry 2019;6:830‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Pries L‐K, Guloksuz S, Ten Have M et al. Evidence that environmental and familial risks for psychosis additively impact a multidimensional subthreshold psychosis syndrome. Schizophr Bull 2018;44:710‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Guloksuz S, Pries L‐K, Delespaul P et al. Examining the independent and joint effects of molecular genetic liability and environmental exposures in schizophrenia: results from the EUGEI study. World Psychiatry 2019;18:173‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262. Thomas S, Höfler M, Schäfer I et al. Childhood maltreatment and treatment outcome in psychotic disorders: a systematic review and meta‐analysis. Acta Psychiatr Scand 2019;140:295‐312. [DOI] [PubMed] [Google Scholar]
- 263. Bloomfield MA, Yusuf FN, Srinivasan R et al. Trauma‐informed care for adult survivors of developmental trauma with psychotic and dissociative symptoms: a systematic review of intervention studies. Lancet Psychiatry 2020;7:449‐62. [DOI] [PubMed] [Google Scholar]
- 264. Bernstein DP, Fink L, Handelsman L et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry 1994;151:1132‐6. [DOI] [PubMed] [Google Scholar]
- 265. Bifulco A, Brown GW, Harris TO . Childhood Experience of Care and Abuse (CECA): a retrospective interview measure. J Child Psychol Psychiatry 1994;35:1419‐35. [DOI] [PubMed] [Google Scholar]
- 266. Weissman MM, Pathak J, Talati A. Personal life events – a promising dimension for psychiatry in electronic health records. JAMA Psychiatry 2020;77:115‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267. Schäfer M, Korn S, Smith PK et al. Lonely in the crowd: recollections of bullying. Br J Dev Psychol 2004;22:379‐94. [Google Scholar]
- 268. Thabrew H, de Sylva S, Romans S. Evaluating childhood adversity In: Fava GA, Sonino N, Wise TN. (eds). The psychosomatic assessment. Basel: Karger, 2012:35‐57. [DOI] [PubMed] [Google Scholar]
- 269. Brand RM, McEnery C, Rossell S et al. Do trauma‐focussed psychological interventions have an effect on psychotic symptoms? A systematic review and meta‐analysis. Schizophr Res 2018;195:13‐22. [DOI] [PubMed] [Google Scholar]
- 270. Britto PR, Lye SJ, Proulx K et al. Nurturing care: promoting early childhood development. Lancet 2017;389:91‐102. [DOI] [PubMed] [Google Scholar]
- 271. Beards S, Gayer‐Anderson C, Borges S et al. Life events and psychosis: a review and meta‐analysis. Schizophr Bull 2013;39:740‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272. Shakoor S, Zavos HMS, Haworth CMA et al. Association between stressful life events and psychotic experiences in adolescence: evidence for gene‐environment correlations. Br J Psychiatry 2018;208:532‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Bhavsar V, Boydell J, McGuire P et al. Childhood abuse and psychotic experiences – evidence for mediation by adulthood adverse life events. Epidemiol Psychiatr Sci 2017;28:300‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Lataster J, Myin‐Germeys I, Lieb R et al. Adversity and psychosis: a 10‐year prospective study investigating synergism between early and recent adversity in psychosis. Acta Psychiatr Scand 2012;125:388‐99. [DOI] [PubMed] [Google Scholar]
- 275. Brown G, Harris T. Life events and illness. New York: Guilford, 1989. [Google Scholar]
- 276. Holmes TH, Rahe RH. The Social Readjustment Rating Scale. J Psychosom Res 1967;11:213‐8. [DOI] [PubMed] [Google Scholar]
- 277. Dohrenwend BS, Askenasy AR, Krasnoff L et al. Exemplification of a method for scaling life events: the PERI Life Events Scale. J Health Soc Behav 1978;19:205‐29. [PubMed] [Google Scholar]
- 278. Butjosa A, Gómez‐Benito J, Myin‐Germeys I et al. Development and validation of the Questionnaire of Stressful Life Events (QSLE). J Psychiatr Res 2017;95:213‐23. [DOI] [PubMed] [Google Scholar]
- 279. DeVylder JE, Koyanagi A, Unick J et al. Stress sensitivity and psychotic experiences in 39 low‐ and middle‐income countries. Schizophr Bull 2016;42:1353‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Rauschenberg C, van Os J, Cremers D et al. Stress sensitivity as a putative mechanism linking childhood trauma and psychopathology in youth’s daily life. Acta Psychiatr Scand 2017;136:373‐88. [DOI] [PubMed] [Google Scholar]
- 281. DeVylder JE, Ben‐David S, Schobel SA et al. Temporal association of stress sensitivity and symptoms in individuals at clinical high risk for psychosis. Psychol Med 2012;43:259‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24:385‐96. [PubMed] [Google Scholar]
- 283. Tso IF, Grove TB, Taylor SF. Self‐assessment of psychological stress in schizophrenia: preliminary evidence of reliability and validity. Psychiatry Res 2012;195:39‐44. [DOI] [PubMed] [Google Scholar]
- 284. Myin‐Germeys I, Kasanova Z, Vaessen T et al. Experience sampling methodology in mental health research: new insights and technical developments. World Psychiatry 2018;17:123‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285. Marconi A, Di Forti M, Lewis CM et al. Meta‐analysis of the association between the level of cannabis use and risk of psychosis. Schizophr Bull 2016;42:1262‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286. van Winkel R, Kuepper R. Epidemiological, neurobiological, and genetic clues to the mechanisms linking cannabis use to risk for nonaffective psychosis. Annu Rev Clin Psychol 2014;10:767‐91. [DOI] [PubMed] [Google Scholar]
- 287. Large M, Mullin K, Gupta P et al. Systematic meta‐analysis of outcomes associated with psychosis and co‐morbid substance use. Aust N Z J Psychiatry 2014;48:418‐32. [DOI] [PubMed] [Google Scholar]
- 288. Schoeler T, Petros N, Di Forti M et al. Poor medication adherence and risk of relapse associated with continued cannabis use in patients with first‐episode psychosis: a prospective analysis. Lancet Psychiatry 2017;4:627‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289. Di Forti M, Quattrone D, Freeman TP et al. The contribution of cannabis use to variation in the incidence of psychotic disorder across Europe (EU‐GEI): a multicentre case‐control study. Lancet Psychiatry 2019;6:427‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290. Hjorthoj CR, Baker A, Fohlmann A et al. Intervention efficacy in trials targeting cannabis use disorders in patients with comorbid psychosis systematic review and meta‐analysis. Curr Pharm Des 2014;20:2205‐11. [DOI] [PubMed] [Google Scholar]
- 291. Rossi A, Galderisi S, Rocca P et al. Personal resources and depression in schizophrenia: the role of self‐esteem, resilience and internalized stigma. Psychiatry Res 2017;256:359‐64. [DOI] [PubMed] [Google Scholar]
- 292. Rossi A, Galderisi S, Rocca P et al. The relationships of personal resources with symptom severity and psychosocial functioning in persons with schizophrenia: results from the Italian Network for Research on Psychoses study. Eur Arch Psychiatry Clin Neurosci 2017;267:285‐94. [DOI] [PubMed] [Google Scholar]
- 293. Tian CH, Feng XJ, Yue M et al. Positive coping and resilience as mediators between negative symptoms and disability among patients with schizophrenia. Front Psychiatry 2019;10:641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294. Meyer B. Coping with severe mental illness: relations of the Brief COPE with symptoms, functioning, and well‐being. J Psychopathol Behav Assess 2001;23:265‐77. [Google Scholar]
- 295. Ventura J, Subotnik KL, Ered A et al. The relationship of attitudinal beliefs to negative symptoms, neurocognition, and daily functioning in recent‐onset schizophrenia. Schizophr Bull 2014;40:1308‐18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Mizuno Y, Wartelsteiner F, Frajo‐Apor B. Resilience research in schizophrenia: a review of recent developments. Curr Opin Psychiatry 2016;29:218‐23. [DOI] [PubMed] [Google Scholar]
- 297. Hofer A, Mizuno Y, Frajo‐Apor B et al. Resilience, internalized stigma, self‐esteem, and hopelessness among people with schizophrenia: cultural comparison in Austria and Japan. Schizophr Res 2016;171:86‐91. [DOI] [PubMed] [Google Scholar]
- 298. Ventura J, Nuechterlein KH, Subotnik KL et al. Self‐efficacy and neurocognition may be related to coping responses in recent‐onset schizophrenia. Schizophr Res 2004;69:343‐52. [DOI] [PubMed] [Google Scholar]
- 299. Harris K, Gooding P, Haddock G et al. Factors that contribute to psychological resilience to suicidal thoughts and behaviours in people with schizophrenia diagnoses: qualitative study. BJPsych Open 2019;5:e79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300. Carver CS. You want to measure coping but your protocol’s too long: consider the Brief COPE. Int J Behav Med 1997;4:92‐100. [DOI] [PubMed] [Google Scholar]
- 301. Xie Y. Reliability and validity of the simplified Coping Style Questionnaire. Chinese J Clin Psychol 1998;6:114‐5. [Google Scholar]
- 302. Magliano L, Fadden G, Madianos M et al. Burden on the families of patients with schizophrenia: results of the BIOMED I study. Soc Psychiatry Psychiatr Epidemiol 1998;33:405‐12. [DOI] [PubMed] [Google Scholar]
- 303. Friborg O, Hjemdal O, Rosenvinge JH et al. A new rating scale for adult resilience: what are the central protective resources behind healthy adjustment? Int J Methods Psychiatr Res 2003;12:65‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304. Connor KM, Davidson JR. Development of a new resilience scale: the Connor‐Davidson resilience scale (CD‐RISC). Depress Anxiety 2003;18:76‐82. [DOI] [PubMed] [Google Scholar]
- 305. Drayton M, Birchwood M, Trower P. Early attachment experience and recovery from psychosis. Br J Clin Psychol 1998;37:269‐84. [DOI] [PubMed] [Google Scholar]
- 306. Leamy M, Bird V, Le Boutillier C et al. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. Br J Psychiatry 2011;199:445‐52. [DOI] [PubMed] [Google Scholar]
- 307. Stuart SR, Tansey L, Quayle E. What we talk about when we talk about recovery: a systematic review and best‐fit framework synthesis of qualitative literature. J Mental Health 2017;26:291‐304. [DOI] [PubMed] [Google Scholar]
- 308. Slade M, Blackie L, Longden E. Personal growth in psychosis. World Psychiatry 2019;18:29‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309. Whitley R, Shepherd G, Slade M. Recovery colleges as a mental health innovation. World Psychiatry 2019;18:141‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310. Corrigan PW. The impact of stigma on severe mental illness. Cogn Behav Pract 1998;5:201‐22. [Google Scholar]
- 311. Brohan E, Elgie R, Sartorius N et al. Self‐stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN‐Europe study. Schizophr Res 2010;122:232‐8. [DOI] [PubMed] [Google Scholar]
- 312. Ran MS, Zhang TM, Wong IY et al. Internalized stigma in people with severe mental illness in rural China. Int J Soc Psychiatry 2018;64:9‐16. [DOI] [PubMed] [Google Scholar]
- 313. Zhang TM, Wong IY, Yu YH et al. An integrative model of internalized stigma and recovery‐related outcomes among people diagnosed with schizophrenia in rural China. Soc Psychiatry Psychiatr Epidemiol 2019;54:911‐8. [DOI] [PubMed] [Google Scholar]
- 314. Clement S, Schauman O, Graham T et al. What is the impact of mental health‐related stigma on help‐seeking? A systematic review of quantitative and qualitative studies. Psychol Med 2015;45:11‐27. [DOI] [PubMed] [Google Scholar]
- 315. Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res 2003;121:31‐49. [DOI] [PubMed] [Google Scholar]
- 316. Boyd JE, Adler EP, Otilingam PG et al. Internalized Stigma of Mental Illness (ISMI) scale: a multinational review. Compr Psychiatry 2014;55:221‐31. [DOI] [PubMed] [Google Scholar]
- 317. Slade M. Recovery research: the empirical evidence from England. World Psychiatry 2012;11:162‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318. Sorsdahl KR, Kakuma R, Wilson Z et al. The internalized stigma experienced by members of a mental health advocacy group in South Africa. Int J Soc Psychiatry 2012;58:55‐61. [DOI] [PubMed] [Google Scholar]
- 319. Thornicroft G, Mehta N, Clement S et al. Evidence for effective interventions to reduce mental‐health‐related stigma and discrimination. Lancet 2016;387:1123‐32. [DOI] [PubMed] [Google Scholar]
- 320. Tsang HW, Ching SC, Tang KH et al. Therapeutic intervention for internalized stigma of severe mental illness: a systematic review and meta‐analysis. Schizophr Res 2016;173:45‐53. [DOI] [PubMed] [Google Scholar]
- 321. Reed GM, Mendonça Correira J, Esparza P et al. The WPA‐WHO Global Survey of Psychiatrists’ Attitudes Towards Mental Disorders Classification. World Psychiatry 2011;10:118‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322. Kishimoto T, Hagi K, Nitta M et al. Long‐term effectiveness of oral second‐generation antipsychotics in patient with schizophrenia and related disorders: a systematic review and meta‐analysis of direct head‐to‐head comparisons. World Psychiatry 2019;18:208‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323. Dixon LB, Dickerson F, Bellack AS et al. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull 2010;36:48‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324. Stovell D, Morrison AP, Panayiotou M et al. Shared treatment decision‐making and empowerment‐related outcomes in psychosis: systematic review and meta‐analysis. Br J Psychiatry 2016;209:23‐28. [DOI] [PubMed] [Google Scholar]


