Abstract
The purpose of this study was to identify patients at higher risk of deep venous thrombosis (DVT) in the uninjured lower extremity both preoperatively and postoperatively in patients with lower extremity fractures. We collected the clinical data of patients with lower extremities fractures who presented at Xi’an Honghui Hospital between 1 July, 2015 and 31 October, 2017. Doppler ultrasonography was used to diagnose the DVT. Patients were examined pre- and postoperatively. The patients were divided into thrombosis group and no thrombosis group according to the preoperative and postoperative ultrasonography results. The thrombosis group was defined as patients with DVT in the uninjured lower extremity and the no thrombosis group was defined as patients without DVT in the uninjured lower extremity. This study enrolled 1454 patients who met the inclusion criteria. The incidence of preoperative DVT in the uninjured lower extremity was 9.63% whereas the postoperative incidence was 20.29%. Age (OR = 0.965, 95 CI%: 0.954-0.977; P ≤ 0.001) and female (OR = 0.667, 95% CI: 0.451-0.986, P = 0.042) were independent risk factors for preoperative DVT in the uninjured lower extremity. Blood loss (OR = 0.997, 95 CI%: 0.995-1.000; P = 0.020), D-dimer level at admission (OR = 0.941, 95 CI%: 0.887-0.999; P = 0.045), and postoperative day 5 D-dimer level (OR = 0.889, 95 CI%: 0.819-0.965; P = 0.005), were independent risk factors for postoperative DVT in the uninjured lower extremity. For the patients with lower extremity fractures, age and female were associated with the preoperative DVT in the uninjured lower extremity. Blood loss, D-dimer at admission and postoperative day 5 D-dimer were associated with the postoperative DVT in the uninjured lower extremity.
Keywords: deep vein thrombosis, lower extremity fractures, ultrasonography, uninjured lower extremity
Introduction
Deep vein thrombosis (DVT) occurs frequently in orthopedic patients. It can increase the length of the hospital stay and associated costs, affect the recovery process of patients, and potentially cause fatal pulmonary embolism.1
Previous studies have shown that the incidence rate of postoperative DVT ranged from 40% to 60%.2–4 These incidences were observed in injured lower extremity. Decker and Weaver demonstrated that the DVT could occur in both the injured and uninjured leg with a trend for higher incidences in the injured leg.5 Song et al. reported that 29.4% of preoperative patients had DVT in either the uninjured or injured lower extremity and that percentage has increased to 32.8% postoperatively.6 Even though previous studies have shown that DVT can occur not only in the injured lower extremity but also in the uninjured lower extremity,7,8 the incidence of DVT in uninjured lower extremity has not been reported or analyzed in detail. There are only a few studies that directly identify the incidence and importance of DVT in the uninjured lower extremity in patients with lower extremity fractures. Only Mok et al. reported that the incidence of DVT in uninjured lower extremities is 14.3%.9
On the basis of these factors, this study aimed to retrospectively analyze the data of patients with lower extremity fractures to investigate the incidence of DVT and identify patients at higher risk of DVT in the uninjured lower extremity.
Patients and Methods
Ethical Statement
The study was approved by the Institutional Review Board (IRB) of Xi’an Jiaotong University.
Included and Excluded Criterion
Inclusion criteria: a) age ≥ 16 years, b) recent lower extremity fractures requiring surgical treatment, c) hospital stay > 48 h, d) availability of results of preoperative and postoperative ultrasonography. Exclusion criteria: a) delayed lower extremity fractures, defined as injuries without surgical treatment within 3 weeks of injury, b) open soft tissue fractures c) serious medical problems without tolerating surgery, d) poor compliance patients, e) patients with contraindications to pharmacological thromboprophylaxis: at high risk of stroke or bleeding.
Methods
The consecutive patients with lower extremity fractures admitted to the hospital were routinely assessed using the risk assessment profile for thromboembolism score (RAPT) to determine the risk of thromboembolism.10 We also assessed patients for contraindications for using of low-molecular-weight heparin (LMWH). For patients without contraindications, LMWH (3800 IU/0.4 mL once per day, Fraxiparine; Glaxo Wellcome Production, GlaxoSmithKline) was injected subcutaneously to prevent DVT when admitted to hospital. Mechanical thromboprophylaxis (foot intermittent pneumatic compression sleeve, 20 minutes twice a day) was used to prevent DVT. Blood samples were collected within 2 hours after admission, 1 day preoperatively, 1 day postoperatively, and 5 days postoperatively.
We used Doppler ultrasonography to diagnose the DVT. The diagnostic criteria was the presence of a constant intraluminal filling defect. Patients were examined pre-and postoperatively. All patients were underwent ultrasonography of the double lower extremities on the day before the scheduled surgery and between the third and fifth day after surgery. DVTs were classified into 3 types: central (femoral and iliac veins), peripheral (calf muscle, fibular, anterior/posterior tibial and popliteal veins), and mixed thrombosis (both central and peripheral thrombosis).11
Based on the results of the ultrasonography, the patients were divided into 2 groups: thrombosis group and no thrombosis group. The thrombosis group was defined as patients suffering DVT in the uninjured lower extremity and the no thrombosis group was defined as patients without DVT in the uninjured lower extremity. For patients without thrombosis, LMWH (3800 IU/0.4 mL once per day, Fraxiparine; Glaxo Wellcome Production, GlaxoSmithKline) was continuously injected subcutaneously to prevent DVT. For patients with thrombosis, LMWH (3800 IU/0.4 mL, twice per day) was injected subcutaneously to treat the DVT. When preoperative ultrasonography results showed a central or mixed thrombosis, an inferior vena cava filter was used to prevent the risk of pulmonary embolism. The thromboprophylaxis was stopped 12 hours before surgery and restarted again 24 hours after surgery. When the patients were discharged, the protocol was changed to rivaroxaban for 35 days after operation.
Statistics Analysis
Statistical analysis was performed using the SPSS Version 19.0 (SPSS Inc., Chicago, Illinois, USA). The measurement data was analyzed to determine if the data is normally distributed. The statistical analysis utilized the independent sample t-test if it is normally distribution. Non-normally distributed variables were shown as median and interquartile range and rank sum test was used to compare the differences. For the enumeration data, chi-square test was used. Multivariate analysis was used to detect the risk factors. The difference was statistically significant if P < 0.05.
Results
Patient Characteristics
In total, 1454 patients suffering a lower extremity fracture were screened. Totally, there were 334 patients suffering DVT in uninjured lower extremity. Of these patients, there were 269 fractures above the knee, 37 fractures around the knee and 28 fractures below the knee. All 1454 the patients received operation. All patients were treated with LMWH at admission. No fatal bleeding events or pulmonary embolism was found in the study.
The Incidence Preoperative DVT in Uninjured Lower Extremity
The preoperative DVT in the uninjured lower extremity was shown in Table 1. There were 140 patients with thrombosis in uninjured lower extremity (9.63%) and 1314 patients without thrombosis in uninjured lower extremity (90.37%). There were 9.01% peripheral DVT, 0.07% central DVT, and 0.55% mixed DVT. Peripheral DVT constituted 93.57% (131/140) of all DVTs.
Table 1.
Patient Characteristics According to Preoperative Ultrasound.
| Thrombosis | No thrombosis | Overall | P | |
|---|---|---|---|---|
| Number | 140 | 1314 | 1454 | |
| Age | 72.42 ± 13.57 | 60.98 ± 19.38 | 62.09 ± 19.19 | <0.001 |
| Gender | ||||
| Female (%) | 98(70.00) | 694(52.82) | 792 | <0.001 |
| Male (%) | 42(30.00) | 620(47.18) | 662 | |
| Unilateral or bilateral | ||||
| Left fracture right thrombosis (%) | 22(15.71) | – | 22 | |
| Right fracture left thrombosis (%) | 34(24.29) | – | 34 | |
| Left fracture bilateral thrombosis (%) | 50(35.71) | – | 50 | |
| Right fracture bilateral thrombosis (%) | 34(24.29) | – | 34 | |
| Only affected limb thrombosis (%) | – | 333(25.34) | 333 | |
| No lower extremities thrombosis (%) | – | 981(74.66) | 981 | |
| Types of fracture | ||||
| Above the knee (%) | 109(77.86) | 812(61.80) | 921 | 0.001 |
| Around the knee (%) | 14(10.00) | 264(20.09) | 278 | |
| Below the knee (%) | 17(12.14) | 238(18.11) | 255 | |
| Types of thrombosis | ||||
| Central (%) | 1(0.71) | 8(2.40) | 9 | <0.001 |
| Peripheral (%) | 131(93.58) | 289(86.79) | 420 | |
| Mixed (%) | 8(5.71) | 36(10.81) | 44 | |
| Medical morbidity | ||||
| Hypertension (%) | 46 (32.86) | 288 (21.91) | 334 | 0.003 |
| Diabetes (%) | 18 (12.86) | 106 (8.07) | 124 | 0.054 |
| Coronary heart disease (%) | 46 (32.86) | 286 (21.76) | 332 | 0.003 |
| Arrhythmia (%) | 19 (13.57) | 142 (10.81) | 161 | 0.322 |
| Stroke (%) | 12 (8.57) | 76 (5.78) | 88 | 0.189 |
| Associated trauma (%) | 14 (10.00) | 167 (12.71) | 181 | 0.356 |
| BMI | 21.15 ± 7.64 | 22.41 ± 5.31 | 22.28 ± 5.58 | 0.331 |
| Days between fracture and hospitalization (days) | 0.00[0.00, 12.00] | 0.00[0.00, 13.00] | 0.00[0.00, 13.00] | 0.087 |
| Days between fracture and operation (days) | 5.00[0.00, 14.00] | 5.00[0.00, 15.00] | 5.00[0.00, 15.00] | 0.256 |
| ASA classification | ||||
| 1 (%) | 10(7.14) | 245(18.65) | 255 | 0.005 |
| 2 (%) | 88(62.86) | 766(58.30) | 854 | |
| 3 (%) | 41(29.29) | 299(22.75) | 340 | |
| 4 (%) | 1(0.71) | 4(0.30) | 5 | |
| Serum markers | ||||
| D-Dimer at admission (mg/L) | 9.48[0.60, 86.96] | 5.47[0.20, 247.32] | 5.73[0.20, 247.32] | 0.147 |
| D-Dimer at preoperation (mg/L) | 4.44[0.70, 45.50] | 3.24 [0.30, 74.18] | 3.46[0.30, 74.18] | 0.263 |
| CRP at admission (mg/L) | 5.39[0.04, 137.53] | 5.76[0.00, 209.60] | 5.72[0.00, 209.60] | 0.597 |
ASA, American Society of Anesthesiologists; CRP, C-reactive protein; BMI, Body Mass Index.
Importantly, there were 50 patients with a left lower extremity fracture who suffered a DVT in both lower extremities (3.44%), 22 with a left lower extremity fracture who suffered a right lower extremity DVT (1.51%), 34 with a right lower extremity fracture who suffered a left lower extremity DVT(2.34%) and 34 with right lower extremity fractures who suffered a DVT in both lower extremities (2.34%).
Univariate Analysis of Preoperative DVT in Uninjured Lower Extremity
There were no statistically significant differences between the 2 groups in medical morbidity excluding hypertension or coronary heart disease, Body Mass Index, days between fracture and hospitalization, days between fracture and operation, D-dimer at admission, preoperative D-dimer, or CRP at admission. However, in the thrombosis group, female patients, patients with a fracture located above the knee, and patients classified as stage Ⅱ of American Society of Anesthesiologists Physical Status Classification System (ASA) were statistically different than the no thrombosis group. In addition, there were more patients in the thrombosis group suffered hypertension (32.86% vs. 21.91%, P = 0.003) and coronary heart disease (32.86% vs. 21.76%, P = 0.003) than no thrombosis group. Age (72.42 ± 13.57 vs. 60.98 ± 19.38, P < 0.001) was found to be another vital factor contributing to thrombosis (Table 1).
Multivariate Analysis of Preoperative DVT in Uninjured Lower Extremity
Multivariate analysis was used to detect the risk factors by entering age, sex, types of fracture, hypertension, coronary heart disease and ASA classification. The results showed that age (OR = 0.965, 95 CI%: 0.954-0.977; P≤0.001) and female (OR = 0.667, 95% CI: 0.451-0.986, P = 0.042) were independent risk factors for preoperative DVT.
The Incidence of Postoperative DVT in Uninjured Lower Extremity
There were 295 patients with thrombosis in uninjured lower extremity (20.29%) and 1159 patients without thrombosis in uninjured lower extremity (79.71%). There were 19.33% peripheral DVT, 0.21% central DVT, 7.57% mixed DVT. Peripheral DVT constituted 95.25% (281/295) of all DVTs (Table 2).
Table 2.
Patient Characteristics According to Postoperative Ultrasound.
| Thrombosis | No thrombosis | Overall | P | |
|---|---|---|---|---|
| Number | 295 | 1159 | 1454 | |
| Age | 71.76 ± 13.42 | 59.62 ± 19.66 | 62.09 ± 19.19 | <0.001 |
| Gender | ||||
| Female | 191(64.74) | 601(51.86) | 792 | <0.001 |
| Male | 104(35.26) | 558(48.14) | 662 | |
| Unilateral or bilateral | ||||
| Left fracture right thrombosis | 25(8.47) | – | 25 | |
| Right fracture left thrombosis | 33(11.19) | – | 33 | |
| Left fracture bilateral thrombosis | 127(43.05) | – | 127 | |
| Right fracture bilateral thrombosis | 110(37.29) | – | 110 | |
| Only affected limb thrombosis | – | 433(37.36) | 433 | |
| No lower extremities thrombosis | – | 726(62.64) | 726 | |
| Types of fracture | ||||
| Above the knee | 240(81.35) | 681(58.76) | 921 | <0.001 |
| Around the knee | 34(11.53) | 244(21.05) | 278 | |
| Below the knee | 21(7.12) | 234(20.19) | 255 | |
| Types of thrombosis | ||||
| Central | 3(1.02) | 10(2.31) | 13 | <0.001 |
| Peripheral | 281(95.25) | 377(87.07) | 658 | |
| Mixed | 11(3.73) | 46(10.62) | 57 | |
| Medical morbidity | ||||
| Hypertension (%) | 85 (28.81) | 249 (21.48) | 334 | 0.009 |
| Diabetes (%) | 32 (10.85) | 92 (7.94) | 124 | 0.120 |
| Coronary heart disease (%) | 87 (29.49) | 245 (21.14) | 332 | 0.003 |
| Arrhythmia (%) | 41 (13.90) | 120 (10.35) | 161 | 0.091 |
| Stroke (%) | 27 (9.15) | 61 (5.26) | 88 | 0.017 |
| Associated trauma (%) | 34 (11.53) | 147 (12.68) | 181 | 0.588 |
| BMI | 21.90 ± 6.58 | 22.38 ± 5.30 | 22.28 ± 5.58 | 0.516 |
| Length of hospital | 9.76 ± 3.84 | 9.54 ± 4.26 | 9.58 ± 4.18 | 0.429 |
| Days between fracture and hospitalization (days) | 0.00[0.00, 12.00] | 0.00[0.00, 13.00] | 0.00[0.00, 13.00] | 0.251 |
| Days between fracture and operation (days) | 5.00[0.00, 14.00] | 5.00[0.00, 15.00] | 5.00[0.00, 15.00] | 0.209 |
| ASA classification | ||||
| 1 | 21(7.12) | 234(20.19) | 255 | <0.001 |
| 2 | 183(62.03) | 671(57.89) | 854 | |
| 3 | 89(30.17) | 251(21.66) | 340 | |
| 4 | 2(0.68) | 3(0.26) | 5 | |
| Duration of operation (mins) | 109.39 ± 57.43 | 113.68 ± 73.00 | 112.81 ± 70.12 | 0.349 |
| Blood loss (ml) | 200.00[10.00, 3000.00] | 200.00[10.00, 2600.00] | 200.00[10.00, 3000.00] | <0.001 |
| Liquid transfusion (ml) | 1730.61 ± 623.94 | 1739.41 ± 557.11 | 1737.62 ± 5 71.12 | 0.814 |
| Serum markers | ||||
| D-Dimer at admission (mg/L) | 9.84[0.44, 273.42] | 4.91[0.20, 207.80] | 5.73[0.20, 247.32] | <0.001 |
| D-Dimer at preoperation (mg/L) | 4.40[0.35, 45.50] | 4.00[0.30, 74.18] | 3.46[0.30, 74.18] | 0.058 |
| D-Dimer at postoperative 1 day (mg/L) | 7.04[0.97, 59.25] | 3.93[0.33, 57.50] | 4.44[0.33, 59.25] | <0.001 |
| D-Dimer at postoperative 3 day (mg/L) | 6.10[0.57, 52.74] | 3.96[0.32, 85.00] | 4.22[0.32, 85.00] | <0.001 |
| D-Dimer at postoperative 5 day (mg/L) | 8.41[1.23, 34.90] | 4.94[0.60, 39.98] | 5.50[0.60, 39.98] | <0.001 |
| CRP at admission (mg/L) | 5.77[0.04, 137.53] | 5.66[0.00, 209.60] | 5.72[0.00, 209.60] | 0.663 |
| CRP at postoperative 5 day (mg/L) | 25.73[0.05, 146.33] | 12.25[0.00, 345.99] | 13.40[0.00, 345.99] | 0.115 |
ASA, American Society of Anesthesiologists; CRP, C-reactive protein; BMI, Body Mass Index.
Importantly, there were 127 patients with a left lower extremity fracture who suffered a DVT in both lower extremities (8.73%), 25 with a left lower extremity fracture who suffered a DVT in the right lower extremity (1.72%), 33 with a right lower extremity fracture who suffered a DVT in the left lower extremity (2.27%) and 110 with a right lower extremity fracture who suffered a DVT in both lower extremities (7.56%).
Univariate Analysis of Postoperative DVT in Uninjured Lower Extremity
In 2 groups, there was no statistically significant difference in the medical morbidity excluding hypertension or coronary heart disease or stroke, Body Mass Index, length of hospital stay, days between fracture and hospitalization, days between fracture and operation, duration of operation, liquid transfusion, preoperative D-dimer values, C-reactive protein at admission and at postoperative day 5. However, in the thrombosis group, there were more female (P < 0.001), fracture above the knee (P < 0.001), and ASA stage Ⅱ (P < 0.001) compared to the no thrombosis group. Similar to the preoperative ultrasound data, age is a contributing factor to postoperative thrombosis (71.76 ± 13.42 vs. 59.62 ± 19.66, P < 0.001). Coronary heart disease, stroke, and hypertension were also important factors contributing to postoperative thrombosis (P = 0.003, P = 0.017, P = 0.009). In addition, blood loss was another factor that contributed to postoperative thrombosis (P < 0.001). In the serum markers, D-dimer at admission, at postoperative day 1, at postoperative day 3, at postoperative day 5 were higher in the thrombosis group (Table 2).
Multivariate Analysis of Postoperative DVT in Uninjured Lower Extremity
Multivariate analysis was used to detect the risk factors by entering age, gender, types of fracture, hypertension, coronary heart disease, stroke, ASA classification, blood loss, D-dimer at admission, D-dimer at postoperative day 1, D-dimer at postoperative day 3 and at D-dimer at postoperative day 5. The results show that D-dimer at admission (OR = 0.941, 95 CI%: 0.887-0.999; P = 0.045), D-dimer at postoperative 5 day (OR = 0.889, 95 CI%: 0.819-0.965; P = 0.005), and blood loss (OR = 0.997, 95 CI%: 0.995-1.000; P = 0.020) were independent risk factors for postoperative DVT.
The Preoperative to Postoperative Changes of DVT in Uninjured Lower Extremity
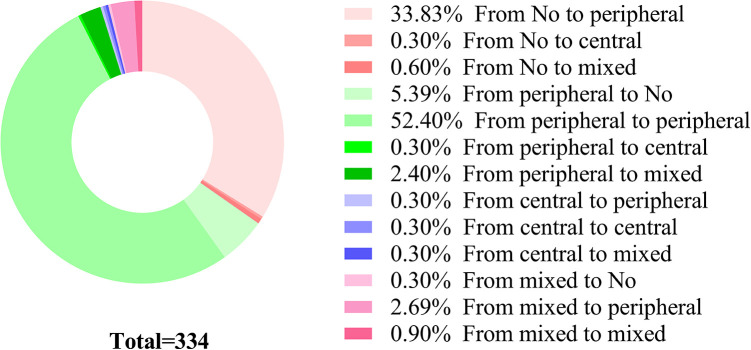
There were 334 patients suffering DVT in uninjured lower extremity in all 1454 patients. There was a total of 53.60% (0.90%, 52.40%, 0.30%) patients without changes during the hospital stay. There were 5.39% of patients who went from having a preoperative peripheral DVT to no thrombosis postoperatively. Conversely, 34.73% (33.83%, 0.30%, 0.60%) of patients changed from having no preoperative thrombosis to developing a peripheral, central, or mixed DVT postoperatively (Figure 1).
Figure 1.
The dynamic changes of DVT in uninjured lower extremity before and after operation.
Discussion
There are few studies that directly identify the incidence and importance of DVT in the uninjured lower extremity in patients with lower extremity fractures. Most previous research analyzed the distribution of DVT in the injured lower extremity across the different fractures,12 or risk factors contributing to a DVT in the injured lower extremity during the hospital stay.13 In order to explore the DVT in the uninjured lower extremity, we retrospectively investigated the changes in preoperative and postoperative DVTs in this study. We have found: a. the incidence of preoperative DVT in the uninjured side is 9.63% and increases to 20.29% postoperatively, b. peripheral DVT constitutes 93.57% of all preoperative and 95.25% of postoperative uninjured lower extremity DVTs.
The dynamic changes in preoperative and postoperative uninjured lower extremity DVT are obvious. There were 116 new postoperative DVTs in the uninjured lower extremity, primarily peripheral DVTs. Peripheral DVTs are likely to occur in calf muscle veins.14 The DVTs in 298 patients were stable peripheral thrombosis from pre-operation to post-operation. The result is similar to DVT in the injured lower extremity. The majority of patients diagnosed with a postoperative DVT had suffered a preoperative DVT in the uninjured lower extremity.6
In this study, the incidence of DVT in the uninjured lower extremity is high, increasing from 9.63% preoperatively to 20.29% postoperatively. Mok et al9 calculated the incidence of DVT in uninjured lower extremity is 14.3% after proximal femur fracture in Hong Kong Chinese.9 Previous study report that the incidence is lower than that in our study but the reasons are various.9 First, we have calculated the incidences independently according to preoperative and postoperative time-points. Second, some studies reported symptomatic DVT but ignored asymptomatic DVT. In fact, Sun and Chen et al. reported that 11.2% of DVTs are asymptomatic.15 Third, the median of days between fracture and surgery is 5.00 days in our study. However, other studies have shown the preoperative incidence of injured lower extremity DVT to be between 54% and 62% for patients with acute fracture whose surgery was delayed by >48 hours.16,17 Most of the patients in this study received the operation in a few days after the fracture occurred. The delay may result from preoperative medical evaluation and optimization or transfer from community hospitals to tertiary hospital. Elderly patients tend to be sicker on admission and therefore more likely to require more time for preoperative preparation.13,15 The delays in surgical intervention may predispose patients to developing thromboembolic problems and may be related to the DVT in uninjured lower extremity. Fourth, thrombosis could be detected by ultrasonography, venography, and multidetector computed tomographic venography.13,18 The diagnostic sensitivity and the specificity is different for each modality and thus, these factors may be contributing to the high incidence of DVT.18
There are many factors contributing to the formation of thrombosis after trauma, including the fracture and surgical intervention.6,19–21 In this study, we found that age and gender were independent risk factors for preoperative DVT in uninjured lower extremity and that D-dimer at admission and at postoperative day 5 and blood loss were independent risk factors for postoperative DVT. Knudson and Gomez et al. found that age is an independent risk factor for thrombosis in adult patients with trauma.22 As for gender, some scholars believe that gender does not affect the incidence of DVT.23 Furthermore, blood loss is another factor promoting the hypercoagulability states.24 In the multivariate analysis of postoperative DVT, blood loss is an independent risk factor (OR = 5.430, P = 0.020). Blood loss in thrombosis group is higher than in the no thrombosis group (Table 2); however, there is no difference in liquid transfusion. The hypercoagulation states, one factor that increases the thrombosis risk, may be the main reason contributing to this phenomenon. Meissner et al. and Selby et al. have proved that the hypercoagulability state will persist for a long time after injury.25,26 In addition, the surgical intervention itself is the introducing factor for hypercoagulability states.27,28 Thus, DVT in uninjured lower extremity and the increased incidence of DVT are easy to comprehend.
It is worth noting that there are several potential limitations in this study. Firstly, the results may be biased by our case-control study design itself. Secondly, there were many other factors affecting the formation of DVT, but we did not completely collect these indicators, such as the use of statins. Therefore, a multicentre prospective study with a large sample size will help explore the role of DVT in the uninjured lower extremity in patients with lower extremity fractures.
In conclusion, the incidence of DVT in the uninjured lower extremity after fracture may currently be underestimated and should be pay more attention. For the patients with lower extremity fractures, age and female were associated with the preoperative DVT in the uninjured lower extremity. Blood loss, D-dimer levels at admission and postoperative day 5 D-dimer were associated with the postoperative DVT in the uninjured lower extremity.
Abbreviations
DVT: Deep vein thrombosis; LMWH: Low-molecular-weight heparin; BMI: Body mass index; ASA: American Society of Anesthesiologists; OR: Odds ratio
Acknowledgments
We thank all our colleagues working in the Department of Orthopedic Trauma, Honghui Hospital, Xi’an Jiaotong University.
Authors’ Note: Shuang-Wei Qu and Yu-Xuan Cong contributed equally to this work. Conceptualization: ZY, ZK. Data curation: FC, LZ, YK, KC, and HH. Formal analysis: ZBF and QSW. Roles/Writing-original draft: QSW, CYX and ZBF. The survey was implemented by Xi’an Honghui Hospital. According to relevant regulations, the data could not be shared. The study was approved by the ethical board of Xi’an JiaoTong University (No. 2014026).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Social Development Foundation of Shaanxi Province (grant numbers 2017ZDXM-SF-009), the Natural Science Basic Research Plan in Shaanxi Province of China (2020JQ-961).
ORCID iDs: Chen Fei  https://orcid.org/0000-0003-4390-1469
https://orcid.org/0000-0003-4390-1469
Yan Zhuang  https://orcid.org/0000-0002-6816-3071
https://orcid.org/0000-0002-6816-3071
Bin-Fei Zhang  https://orcid.org/0000-0002-1135-6972
https://orcid.org/0000-0002-1135-6972
References
- 1. Brill JB, Badiee J, Zander AL, et al. The rate of deep vein thrombosis doubles in trauma patients with hypercoagulable thromboelastography. J Trauma Acute Care Surg. 2017;83(3):413–419. [DOI] [PubMed] [Google Scholar]
- 2. Tang Y, Wang K, Shi Z, Yang P, Dang X. A RCT study of rivaroxaban, low-molecular-weight heparin, and sequential medication regimens for the prevention of venous thrombosis after internal fixation of hip fracture. Biomed Pharmacother. 2017;92:982–988. [DOI] [PubMed] [Google Scholar]
- 3. Deitelzweig SB, Johnson BH, Lin J, Schulman KL. Prevalence of clinical venous thromboembolism in the USA: current trends and future projections. Am J Hematol. 2011;86(2):217–220. [DOI] [PubMed] [Google Scholar]
- 4. Godzik J, McAndrew CM, Morshed S, Kandemir U, Kelly MP. Multiple lower-extremity and pelvic fractures increase pulmonary embolus risk. Orthopedics. 2014;37(6):e517–e524. [DOI] [PubMed] [Google Scholar]
- 5. Decker S, Weaver MJ. Deep venous thrombosis following different isolated lower extremity fractures: what is known about prevalences, locations, risk factors and prophylaxis? Eur J Trauma Emerg Surg. 2013;39(6):591–598. [DOI] [PubMed] [Google Scholar]
- 6. Song K, Yao Y, Rong Z, Shen Y, Zheng M, Jiang Q. The preoperative incidence of deep vein thrombosis (DVT) and its correlation with postoperative DVT in patients undergoing elective surgery for femoral neck fractures. Arch Orthop Trauma Surg. 2016;136(10):1459–1464. [DOI] [PubMed] [Google Scholar]
- 7. Weiss ES, Hayanga AJ, Efron DT, Noll K, Cornwell EE, III, Haut ER. Laterality of deep venous thrombosis among trauma patients: are we screening our patients adequately? J Surg Res. 2007;141(1):68–71. [DOI] [PubMed] [Google Scholar]
- 8. Torholm C, Broeng L, Jorgensen PS, et al. Thromboprophylaxis by low-molecular-weight heparin in elective hip surgery. A placebo controlled study. J Bone Joint Surg Br. 1991;73(3):434–438. [DOI] [PubMed] [Google Scholar]
- 9. Mok CK, Hoaglund FT, Rogoff SM, Chow SP, Ma A, Yau AC. The incidence of deep vein thrombosis in Hong Kong Chinese after hip surgery for fracture of the proximal femur. Br J Surg. 1979;66(9):640–642. [DOI] [PubMed] [Google Scholar]
- 10. Greenfield LJ, Proctor MC, Rodriguez JL, Luchette FA, Cipolle MD, Cho J. Posttrauma thromboembolism prophylaxis. J Trauma. 1997;42(1):100–103. [DOI] [PubMed] [Google Scholar]
- 11. Liu XC, Chen XW, Li ZL, Wang SC, Chen C. Anatomical distribution of lower-extremity deep venous thrombosis in patients with acute stroke. J Stroke Cerebrovasc Dis. 2020;29(7):104866. [DOI] [PubMed] [Google Scholar]
- 12. Schick MA, Pacifico L. Deep venous thrombosis (DVT), lower extremity In: StatPearls edn StartPearls Publishing; 2017. [PubMed] [Google Scholar]
- 13. Shin WC, Woo SH, Lee SJ, Lee JS, Kim C, Suh KT. Preoperative prevalence of and risk factors for venous thromboembolism in patients with a hip fracture: an indirect multidetector CT venography Study. J Bone Joint Surg Am. 2016;98(24):2089–2095. [DOI] [PubMed] [Google Scholar]
- 14. Henry JC, Satiani B. Calf muscle venous thrombosis: a review of the clinical implications and therapy. Vasc Endovascular Surg. 2014;48(5-6):396–401. [DOI] [PubMed] [Google Scholar]
- 15. Sun Y, Chen D, Xu Z, et al. Incidence of symptomatic and asymptomatic venous thromboembolism after elective knee arthroscopic surgery: a retrospective study with routinely applied venography. Arthroscopy. 2014;30(7):818–822. [DOI] [PubMed] [Google Scholar]
- 16. Zahn HR, Skinner JA, Porteous MJ. The preoperative prevalence of deep vein thrombosis in patients with femoral neck fractures and delayed operation. Injury. 1999;30(9):605–607. [DOI] [PubMed] [Google Scholar]
- 17. Hefley FG, Jr, Nelson CL, Puskarich-May CL. Effect of delayed admission to the hospital on the preoperative prevalence of deep-vein thrombosis associated with fractures about the hip. J Bone Joint Surg Am. 1996;78(4):581–583. [DOI] [PubMed] [Google Scholar]
- 18. Terao M, Ozaki T, Sato T. Diagnosis of deep vein thrombosis after operation for fracture of the proximal femur: comparative study of ultrasonography and venography. J Orthop Sci. 2006;11(2):146–153. [DOI] [PubMed] [Google Scholar]
- 19. Park MS, Perkins SE, Spears GM, et al. Risk factors for venous thromboembolism after acute trauma: a population-based case-cohort study. Thromb Res. 2016;144:40–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Park SJ, Kim CK, Park YS, Moon YW, Lim SJ, Kim SM. Incidence and factors predicting venous thromboembolism after surgical treatment of fractures below the hip. J Orthop Trauma. 2015;29(10):e349–e354. [DOI] [PubMed] [Google Scholar]
- 21. Chen F, Xiong JX, Zhou WM. Differences in limb, age and sex of Chinese deep vein thrombosis patients. Phlebology. 2015;30(4):242–248. [DOI] [PubMed] [Google Scholar]
- 22. Knudson MM, Gomez D, Haas B, Cohen MJ, Nathens AB. Three thousand seven hundred thirty-eight posttraumatic pulmonary emboli: a new look at an old disease. Ann Surg. 2011;254(4):625–632. [DOI] [PubMed] [Google Scholar]
- 23. Anderson FA, Jr, Spencer FA. Risk factors for venous thromboembolism. Circulation. 2003;107(23 Suppl 1):I9–I16. [DOI] [PubMed] [Google Scholar]
- 24. Riha GM, Kunio NR, Van PY, et al. Uncontrolled hemorrhagic shock results in a hypercoagulable state modulated by initial fluid resuscitation regimens. J Trauma Acute Care Surg. 2013;75(1):129–134. [DOI] [PubMed] [Google Scholar]
- 25. Selby R, Geerts W, Ofosu FA, et al. Hypercoagulability after trauma: hemostatic changes and relationship to venous thromboembolism. Thromb Res. 2009;124(3):281–287. [DOI] [PubMed] [Google Scholar]
- 26. Meissner MH, Chandler WL, Elliott JS. Venous thromboembolism in trauma: a local manifestation of systemic hypercoagulability? J Trauma. 2003;54(2):224–231. [DOI] [PubMed] [Google Scholar]
- 27. Kupcinskiene K, Trepenaitis D, Petereit R, et al. Monitoring of hypercoagulability by thromboelastography in bariatric surgery. Med Sci Monit. 2017;23:1819–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wilson D, Cooke EA, McNally MA, Wilson HK, Yeates A, Mollan RA. Changes in coagulability as measured by thrombelastography following surgery for proximal femoral fracture. Injury. 2001;32(10):765–770. [DOI] [PubMed] [Google Scholar]