Abstract
High-flow oxygen inhalation is one of the most effective acute treatments for cluster headache. The therapy was first described for the treatment of cluster headache in 1952 by Horton, and has exhibited some advantages and efficacy compared to other acute medicines. The mechanism is not very clear, but some evidence has demonstrated its relationship to the trigeminovascular system and neuroinflammation. High-flow oxygen inhalation via a non-rebreather mask during cluster headache attacks has been widely recommended. Patients with frequent attacks and/or intolerance to drugs may prefer the oxygen treatment.
Keywords: cluster headache, oxygen, acute treatment, hyperbaric oxygen, pathophysiology, clinical research, experimental research, primary headache
INTRODUCTION
Cluster headache (CH) is a severe primary headache of trigeminal autonomic cephalalgia with severe and strictly unilateral attacks, lasting 15–180 minutes, and occurring up to eight times a day.1 Because of the frequency and severity of attacks, acute abortive treatment is very important. High flow oxygen has been recommended for alleviating acute attacks of CH, and is one of the first-line acute treatments in the international guidelines.2,3 Compared to other acute medicines, such as sumatriptan and zolmitriptan, oxygen causes very few side effects or long-term harm.4,5,6 Although pure oxygen inhalation is recognized as the first-line treatment, the underlying pathophysiology is still unclear. It has been observed that vasodilation is accompanied with CH attacks and studies have suggested oxygen aborted headaches by contracting the cerebral vessels.7,8,9,10 Recently, animal experiments have revealed that oxygen can inhibit dural plasma protein extravasation in rats,11 and the improvement of neurogenic inflammation may explain why oxygen works for the treatment of CH.
Studies have shown that 100% oxygen inhalation at a flow rate of 6–15 L/min has a better effect.7,12,13 Petersen et al.14 investigated the different curative effects of three mask types, and found that the demand valve oxygen or O2ptimask maybe better choices compared to the simple mask. Although high flow oxygen inhalation is effective, it is not available worldwide; a survey conducted by the International Headache Society found that oxygen for CH acute treatment is reimbursed in 50% of all involved countries.6
To date, there have been few studies that have systematically reviewed the history, oxygen inhalation mode, and mechanisms by which oxygen can alleviate the symptoms of CH. Therefore, we aim to provide a comprehensive evaluation of oxygen treatment, and to explore a more effective oxygen regimen for CH.
HISTORY OF OXYGEN IN CLUSTER HEADACHE
The use of oxygen for the treatment of headaches was first described by Alvarez and Mason15 in 1940, who used a nasal mask to deliver oxygen at a flow rate between 6 and 8 L/min, and found it effective for the treatment of typical migraines. The treatment was first used for CH in 1952 by Horton.16 In 1955, Horton17 described the successful treatment of CH with oxygen in a population of 1176 patients with histamine cephalalgia. However, it was not a systematic study, and was only based on his experience in the clinic. Horton did not disclose why he chose oxygen as the treatment and why it worked until 1961, when he raised the vasoconstrictive effect of oxygen.7 In 1981, Kudrow18 published the first systematic study of the use of oxygen as a treatment for CH, and found that oxygen delivered at 7 L/min for 15 minutes and sublingual ergotamine administration were both effective in reducing CH attacks. Oxygen aborted more than 7 out of 10 attacks in 82% of the patients, and ergotamine in 70%. On the other hand, the study also found a rebound effect in oxygen users. A study published in 1985 by Fogan12 found that using oxygen at 6 L/min was more effective than using room air in reducing headaches, and there was a statistically significant difference between the two groups. Fogan’s study revealed that 56% of patients who used oxygen experienced relief in over 80% of attacks, compared with 7% of patients who used room air.12 In 2009, a study published in JAMA by Cohen et al.19 found that a higher oxygen flow rate of 12 L/min also was effective for the treatment of CH, compared to an oxygen flow rate of 7 L/min.
MECHANISM OF OXYGEN IN CLUSTER HEADACHE
As previously mentioned, it is still unclear why oxygen exhibits such good efficacy in the treatment of CH. The vasoconstrictive theory was prevalent in the early 20th century until Wolff et al. found that ergotamine constricted external carotid arteries and simultaneously relieved migrainous headaches.20 Therefore, they proposed that headache is caused by vasodilation rather than vasoconstriction. The study was published in 1938 and overturned the past theory.20 In 1961, Horton7 proposed that histamine cephalalgia was caused by the vasodilatation of extracranial vessels, and that oxygen was a vasoconstriction factor. If the vasoconstrictive effect of oxygen exists, oxygen therapy should be effective for both migraine and CH. However, the oxygen treatment is only effective for CH. In the 1980s, some studies reported a decrease of cerebrospinal flui in patients after breathing 100% oxygen as compared to breathing room air.21 Since then, animal model studies have demonstrated the protective, anti-inflammatory role of hyperoxia in microcirculatory inflammation. In 2006, Schuh-Hofer et al.11 demonstrated that hyperoxia can inhibit dural plasma protein extravasation in rats. Recent studies have suggested that CH is associated with some brain structures, including the trigeminovascular system, the cranial autonomic system, and the hypothalamus. The activation of the trigeminovascular system is thought to play an important role in the pathophysiology of CH. Goadsby and Edvinsson22 attempted to demonstrate the associations between hyperoxia and neuropeptides, and the results indicated that a significant reduction of calcitonin gene related peptide concentration in the jugular vein after oxygen treatment occurred, which suggests a possible effect of hyperoxia on trigeminal afferents. However, animal experiments have shown that oxygen does not directly act on trigeminal afferents, but appears to play a key role at the parasympathetic pathways.23 At present, studies assume that oxygen may act as a terminating factor in CH attacks. More research is needed to clarify the specific mechanisms of oxygen treatment for CH.
Table 1.
The history of oxygen used for cluster headache
| Study | Year | Findings |
|---|---|---|
| Alvarez et al.15 | 1940 | First use of oxygen for headache at a flow rate between 6 and 8 L/min. |
| Horton16 | 1952 | First description of oxygen used for histamine cephalalgia. |
| Horton17 | 1955 | Oxygen treatment in 1176 patients with histamine cephalalgia. |
| Horton7 | 1961 | He raised the vasoconstrictive effect of oxygen in histamine cephalalgia. |
| Kudrow et al.18 | 1981 | First systematic study on oxygen used for cluster headache. |
| Fogan et al.12 | 1985 | Crossover study found that oxygen was more effective than room air. |
| Cohen et al.19 | 2009 | Oxygen at 12 L/min, as well as at 7 L/min, was effective. |
Figure 1.
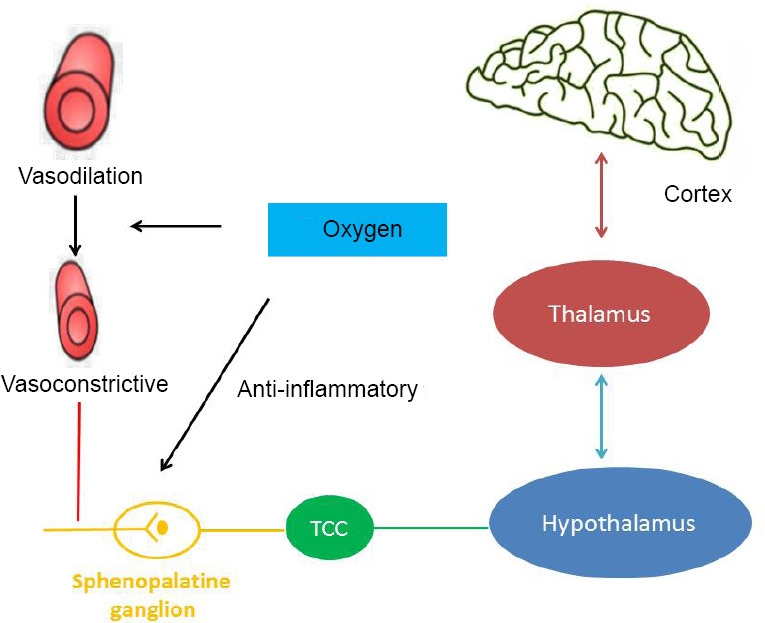
The possible mechanism of oxygen in cluster headache.
Note: TCC: Trigeminal cervical complex.
CLINICAL STUDIES OF OXYGEN IN CLUSTER HEADACHE
CH is usually called suicide headache because of the intense pain, so the acute analgesic treatment is important. Although oxygen therapy is recommended as the first-line treatment, there exist some patients who cannot benefit from it. Clinical trials and questionnaires indicate that the effectiveness of oxygen for CH attacks ranges between 56% and 82%.6,24 The largest CH survey, which included 3251 subjects, found that 13% of patients experienced a complete remission with the oxygen treatment, and that it was very effective in 41% of patients, moderately effective in 27%, minimally effective in 12%, and completely ineffective in 7%.6 Though most patients respond to high flow oxygen, approximately 20% of cases do not experience headache relief with 100% oxygen. Some studies attempted to explore the factors that can predict the response to oxygen treatment. Backx et al.25 found that shorter attacks and a lack of interictal pain were positively associated with oxygen responsiveness, while some accompanying symptoms, such as photophobia or phonophobia, nausea and vomiting, or restlessness during an attack, were negatively associated with it. Additionally, the study identified three predictors of poor oxygen response, namely no past history of smoking, interictal headache, and a longest attack period of more than 180 minutes. Previous studies also found different results for predictors of poor efficacy, such as age, sex, and history of smoking.6
Compared with other acute medicines, like triptans or ergotamine, high flow oxygen is effective for the treatment of CH and has few side effects, though triptans have shown similar effects and are more available. Considering safety, oxygen is a good option for patients who have multiple attacks per day, as well as those who are pregnant or breastfeeding. As previously mentioned, oxygen given at a rate between 6 and 15 L/min shows efficacy. Some studies have attempted to compare the effects between different flow rates for the treatment of CH attacks. Dirkx and Haane26 found that patients preferred a rate of 12 L/min to 7 L/min, but there were no significant differences in effects between flow rates. A recent study14 investigated the differences in the effects of different types of masks that deliver oxygen. The trial compared the effects of three types of masks (demand valve oxygen, O2ptimask, or a simple mask), and found that oxygen inhalation via O2ptimask and demand valve oxygen decreased the need for rescue medication.14
Previous studies have shown that different oxygen therapy regimens have different effects. The influence factors include the oxygen flow rate, different masks for oxygen inhalation, and individual variation. However, few studies have focused on the right timing of oxygen supply. To fully understand all the symptoms inpatients before, during, and after the onset of CH, Snoer et al.27 collected data on 500 CH attacks and found that preictal and postictal symptoms are very common in CH, which suggests that CH patients not just experience present headache period. Although the pathogenic mechanism triggering CH is not clear, studies of preictal and postictal symptoms may contribute to the understanding of CH pathophysiology and enlighten early abortion treatment strategies.27 We therefore would like to study whether receiving oxygen therapy during the preictal period is more effective than during the headache attack, and this will be a future research direction.
In conclusion, high-flow oxygen is recommended as a more effective treatment for CH that has few complications, but the choice of suitable cases and oxygen flow rate or tools, as well as the appropriate time for oxygen inhalation, require more exploration in the future.
Footnotes
Conflicts of interest
The authors have no conflicts of interests to declare.
Financial support
None.
Copyright license agreement
The Copyright License Agreement has been signed by all authors before publication.
Plagiarism check
Checked twice by iThenticate.
Peer review
Externally peer reviewed.
REFERENCES
- 1.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders. 3rd edition. Vol. 38. Cephalalgia; 2018. pp. 1–211. [DOI] [PubMed] [Google Scholar]
- 2.May A, Leone M, Afra J, et al. EFNS guidelines on the treatment of cluster headache and other trigeminal-autonomic cephalalgias. Eur J Neurol. 2006;13:1066–1077. doi: 10.1111/j.1468-1331.2006.01566.x. [DOI] [PubMed] [Google Scholar]
- 3.Robbins MS, Starling AJ, Pringsheim TM, Becker WJ, Schwedt TJ. Treatment of cluster headache: The American Headache Society Evidence-Based Guidelines. Headache. 2016;56:1093–1106. doi: 10.1111/head.12866. [DOI] [PubMed] [Google Scholar]
- 4.May A, Schwedt TJ, Magis D, Pozo-Rosich P, Evers S, Wang SJ. Cluster headache. Nat Rev Dis Primers. 2018;4:18006. doi: 10.1038/nrdp.2018.6. [DOI] [PubMed] [Google Scholar]
- 5.Tepper D. Oxygen for cluster headache. Headache. 2017;57:1493–1494. doi: 10.1111/head.13085. [DOI] [PubMed] [Google Scholar]
- 6.Pearson SM, Burish MJ, Shapiro RE, Yan Y, Schor LI. Effectiveness of oxygen and other acute treatments for cluster headache: results from the Cluster Headache Questionnaire, an international survey. Headache. 2019;59:235–249. doi: 10.1111/head.13473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horton BT. Histaminic cephalgia (Horton’s headache or syndrome) Md State Med J. 1961;10:178–203. [PubMed] [Google Scholar]
- 8.Steinberg A, Wiklund NP, Brundin L, Remahl AI. Levels of nitric oxide metabolites in cerebrospinal fluid in cluster headache. Cephalalgia. 2010;30:696–702. doi: 10.1177/0333102409351799. [DOI] [PubMed] [Google Scholar]
- 9.D’Andrea G, Bussone G, Di Fiore P, et al. Pathogenesis of chronic cluster headache and bouts: role of tryptamine, arginine metabolism and alpha1-agonists. Neurol Sci. 2017;38:37–43. doi: 10.1007/s10072-017-2862-4. [DOI] [PubMed] [Google Scholar]
- 10.Mitsikostas DD, Edvinsson L, Jensen RH, et al. Refractory chronic cluster headache: a consensus statement on clinical definition from the European Headache Federation. J Headache Pain. 2014;15:79. doi: 10.1186/1129-2377-15-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schuh-Hofer S, Siekmann W, Offenhauser N, Reuter U, Arnold G. Effect of hyperoxia on neurogenic plasma protein extravasation in the rat dura mater. Headache. 2006;46:1545–1551. doi: 10.1111/j.1526-4610.2006.00447.x. [DOI] [PubMed] [Google Scholar]
- 12.Fogan L. Treatment of cluster headache A double-blind comparison of oxygen v air inhalation. Arch Neurol. 1985;42:362–363. doi: 10.1001/archneur.1985.04060040072015. [DOI] [PubMed] [Google Scholar]
- 13.Rozen TD. High oxygen flow rates for cluster headache. Neurology. 2004;63:593. doi: 10.1212/01.wnl.0000133405.80679.4b. [DOI] [PubMed] [Google Scholar]
- 14.Petersen AS, Barloese MC, Lund NL, Jensen RH. Oxygen therapy for cluster headache A mask comparison trial A single-blinded, placebo-controlled, crossover study. Cephalalgia. 2017;37:214–224. doi: 10.1177/0333102416637817. [DOI] [PubMed] [Google Scholar]
- 15.Alvarez WC, Mason AY. Results obtained in the treatment of headache with the inhalation of pure oxygen. Mayo Clin Proc. 1940;15:616–618. [Google Scholar]
- 16.Horton B. Histamine cephalalgia. Lancet. 1952;72:92–98. [Google Scholar]
- 17.Horton BT. Histaminic cephalgia: differential diagnosis and treatment. Bull Tufts N Engl Med Cent. 1955;1:143–156. [PubMed] [Google Scholar]
- 18.Kudrow L. Response of cluster headache attacks to oxygen inhalation. Headache. 1981;21:1–4. doi: 10.1111/j.1526-4610.1981.hed2101001.x. [DOI] [PubMed] [Google Scholar]
- 19.Cohen AS, Burns B, Goadsby PJ. High-flow oxygen for treatment of cluster headache: a randomized trial. JAMA. 2009;302:2451–2457. doi: 10.1001/jama.2009.1855. [DOI] [PubMed] [Google Scholar]
- 20.Graham JR, Wolff HG. Mechanism of migraine headache and action of ergotamine tartrate. Arch Neurol Psychiatry. 1938;39:737–763. [Google Scholar]
- 21.Nelson RF, du Boulay GH, Marshall J, Russell RW, Symon L, Zilkha E. Cerebral blood flow studies in patients with cluster headache. Headache. 1980;20:184–189. doi: 10.1111/j.1526-4610.1980.hed2004184.x. [DOI] [PubMed] [Google Scholar]
- 22.Goadsby PJ, Edvinsson L. Human in vivo evidence for trigeminovascular activation in cluster headache Neuropeptide changes and effects of acute attacks therapies. Brain. 1994;117:427–434. doi: 10.1093/brain/117.3.427. [DOI] [PubMed] [Google Scholar]
- 23.Akerman S, Holland PR, Lasalandra MP, Goadsby PJ. Oxygen inhibits neuronal activation in the trigeminocervical complex after stimulation of trigeminal autonomic reflex, but not during direct dural activation of trigeminal afferents. Headache. 2009;49:1131–1143. doi: 10.1111/j.1526-4610.2009.01501.x. [DOI] [PubMed] [Google Scholar]
- 24.Lademann V, Jansen JP, Evers S, Frese A. Evaluation of guideline-adherent treatment in cluster headache. Cephalalgia. 2016;36:760–764. doi: 10.1177/0333102415612774. [DOI] [PubMed] [Google Scholar]
- 25.Backx AP, Haane DY, De Ceuster L, Koehler PJ. Cluster headache and oxygen: is it possible to predict which patients will be relieved A retrospective cross-sectional correlation study. J Neurol. 2010;257:1533–1542. doi: 10.1007/s00415-010-5569-5. [DOI] [PubMed] [Google Scholar]
- 26.Dirkx THT, Haane DYP, Koehler PJ. Oxygen treatment for cluster headache attacks at different flow rates: a double-blind, randomized, crossover study. J Headache Pain. 2018;19:94. doi: 10.1186/s10194-018-0917-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Snoer A, Lund N, Beske R, Hagedorn A, Jensen RH, Barloese M. Cluster headache beyond the pain phase: A prospective study of 500 attacks. Neurology. 2018;91:e822–e831. doi: 10.1212/01.wnl.0000542491.92981.03. [DOI] [PubMed] [Google Scholar]


