Abstract
Background
Fatigue is frequently reported in inflammatory bowel disease (IBD) and impacts on health-related quality of life (HRQoL). HRQoL has not been systematically reviewed in IBD fatigue.
Aim
To investigate what impact IBD fatigue has on HRQoL in adults with IBD.
Methods
Systematic searches (CINAHL, EMBASE, PsychINFO, Medline) were conducted on 25 September 2018, restricted to ‘human’, ‘adult’, ‘primary research’ and ‘English language’. Search terms encompassed concepts of ‘fatigue’, ‘IBD’ and ‘HRQoL’. A 5-year time limit (2013–2018) was set to include the most relevant publications. Publications were screened, data extracted and quality appraised by two authors. A narrative synthesis was conducted.
Results
Eleven studies were included, presenting data from 2823 participants. Fatigue experiences were significantly related to three HRQoL areas: symptom acceptance, psychosocial well-being and physical activity. Patients reporting high fatigue levels had low symptom acceptance. Psychosocial factors were strongly associated with both fatigue and HRQoL. Higher social support levels were associated with higher HRQoL. Physical activity was impaired by higher fatigue levels, lowering HRQoL, but it was also used as a means of reducing fatigue and improving HRQoL. Quality appraisal revealed methodological shortcomings in a number of studies. Notably, use of multiple measures, comparison without statistical adjustment and fatigue and HRQoL assessment using the same tool were some of the methodological shortcomings.
Conclusion
Psychosocial factors, symptom management and acceptance and physical activity levels have significant impact on HRQoL. Results support application of psychosocial or exercise interventions for fatigue management. Further exploration of HRQoL factors in IBD fatigue is required, using validated fatigue and HRQoL measures.
PROSPERO registration number
CRD42018110005.
Keywords: inflammatory bowel disease, Crohn’s disease, ulcerative colitis, fatigue, health related quality of life
Significance of this study.
What is already known on this topic
Fatigue is frequently reported in inflammatory bowel disease (IBD) and has been identified as one of the most burdensome symptoms.
IBD fatigue has been reported as multidimensional and complex, impacting individual’s activities of daily living and reducing health-related quality of life (HRQoL).
The subjective nature of fatigue and poor understanding means it is often underestimated by clinicians.
What this study adds
This work identified the experiences of fatigue were significantly related to three HRQoL linked themes: symptom acceptance and management, psychosocial well-being and management and physical activity.
Psychosocial factors were strongly associated with both fatigue and HRQoL.
Physical activity was impaired by higher fatigue levels, lowering HRQoL, but it was also used as a means of reducing fatigue and improving HRQoL.
Significance of this study.
How might it impact on clinical practice in the foreseeable future
Better understanding of the impact of IBD fatigue will help patients and clinicians better manage fatigue, for individuals with IBD this has the potential to improve HRQoL, reduce costs to the National Health Service and allow patients to feel a sense of control over their treatment through effective self-management.
This review has identified areas for possible further research with use of validated fatigue and HRQoL measures and clearer characterisation of disease activity to define a diagnostic cut-off for IBD fatigue.
Introduction
Fatigue related to inflammatory bowel disease (IBD) and other long-term conditions (LTCs) is defined as an ‘extreme and persistent sense of tiredness, weakness or exhaustion,’1 which can be physical, mental or both and is not easily resolved by sleep or rest.2 Fatigue can be attributed to both physical and mental exertion3 4 or as the outcome of pathological processes.3 4 The International Classification of Diseases code presents fatigue as an assortment of physical, cognitive and emotional symptoms affecting undertaking of daily tasks.5 It is not known whether fatigue in a given disease is a result of being chronically ill or whether it represents a specific symptom of that disease.6
The prevalence of IBD fatigue is reported as 41%–48% for patients in remission and 71%–86% in patients with active disease.7 8 The most frequently experienced symptoms of IBD are pain, urgency and fatigue.9–15 IBD fatigue is one of the top five research priorities highlighted by the nurses European Crohn’s and Colitis Organisation (N-ECCO) due to its pervasiveness and negative impact on health-related quality of life (HRQoL).12 16 The symptom of fatigue in LTCs has received greater attention as part of overall HRQoL.6 However, to date, there has been no thorough appraisal of the impact of IBD fatigue on an individual’s HRQoL.
Increasing life expectancy has highlighted the need for other measures of health, capturing the quality of the years someone lives. Traditional markers for population health, such as life expectancy and causes of death, do not offer information regarding the quality of the physical, mental and social domains of life. The concept of QoL is not a new one, in 1995 WHO recognised the importance of improving peoples’ QoL.17 When QoL in considered in the context of health and disease, it is commonly referred to as HRQoL to differentiate from other aspects of QoL. Health is a multidimensional concept, HRQoL is also multidimensional and incorporates areas related to physical, mental and social functioning.18 HRQoL goes beyond the direct measures of health and focuses on the QoL consequences of health status. HRQoL represents the functional effect of an illness and its consequent therapy on a patient, as perceived by the patient. It encompasses several dimensions of life, including physical functioning, psychosocial functioning, role functioning, mental health and general health perceptions. HRQoL is determined by sociodemographic, clinical and psychological and treatment-related determinants.19 20
Studies to date have rarely measured IBD fatigue as a primary outcome and there has been limited literature focused on the impact of IBD fatigue on HRQoL. The aim of this review is to synthesise the existing body of knowledge on IBD fatigue and its impact on HRQoL. This work is essential in order to better define the research streams needed to improve HRQoL in people with IBD fatigue.
Methods
The review question ‘What is the impact of IBD fatigue on the HRQoL of adults with IBD?’ was developed using the format: population, exposure, outcome.
The final search of literature was performed on 25 September 2018. Databases searched were EMBASE, CINAHL, PsychINFO and Medline. These databases were selected as they were likely to provide a broad combination of medical and healthcare allied papers related to the topic of interest.21 To increase the reference retrieval, the medical subject headings (MeSH) and free-text searching were employed, and each database was individually searched.22 Grey literature searching was used to maximise the number of publications retrieved.23 24 This was conducted by searching Google Scholar, reference lists of included publications and registered controlled trial registers.
Search terms were determined through consideration of previously reviewed literature and scoping searches of Google Scholar (table 1).9 25–27
Table 1.
Search terms
| Fatigue | IBD | Quality of life |
| Fatigue (MeSH) | Inflammatory Bowel Disease* | Quality of Life |
| Fatigue* | IBD | Health related quality of life* |
| Lethargy (MeSH) | Ulcerative Colitis* | Life Quality |
| Lethargy | UC | HRQoL |
| Low energy* | Crohn’s Disease* | |
| Vigour* | CD | |
| Vitality* | ||
| Exhaustion* |
*free search term for truncation.
Searches were performed with the ‘suggested search terms’ and ‘explode’ selection. The Boolean operator ‘OR’ was used within each facet to maximise the searches, with the operator ‘AND’ used between facets to combine terms. Searches were restricted to ‘human’, ‘adult’, ‘primary research’ and ‘English language’ publications. Studies of any design published in English were considered for the review if IBD fatigue was mentioned in the abstract. Commentary papers and literature reviews were excluded. A time limit of 5 years (2013–2018) was set to ensure inclusion of only the most up-to-date information. Due to limited number of publications related to IBD fatigue, no studies were excluded from the review based on study quality, however quality was considered when reviewing study findings. Studies that did not meet the inclusion criteria were retained, if relevant, for background information.
Quality appraisal and data extraction
Quality of studies was assessed and data were extracted by two independent reviewers (SJR and JMcG), using forms specific to study design from the Joanna Briggs Institute to allow for comparison of quality across study types.28 The data extracted includes specific details about populations, context, culture, geographical location, study methods and the phenomena of IBD fatigue relevant to the review question. Due to the time constraints, all papers were read in full, but only data reflecting the aims of the review were extracted. For several of the studies, information and analysis regrading HRQoL was limited, but present, therefore deemed important to include given the comprehensive and systematic nature of the review.
Data analysis
Thematic analysis was used to analyse data. The analysis included three phases: open coding, creating categories and abstraction. The open coding phase relies on the research question driving the coding process so that only valid data are highlighted and further examined.29–31 Open coding involved highlighting the text when reading, later the highlighted sections were grouped and categorised. During categorisation, each category was named and combined into larger themes. The larger themes were analysed for subthemes through analysis of the coding.
The abstraction phase involved conveying a general description of the topic being researched to the themes identified.
Results
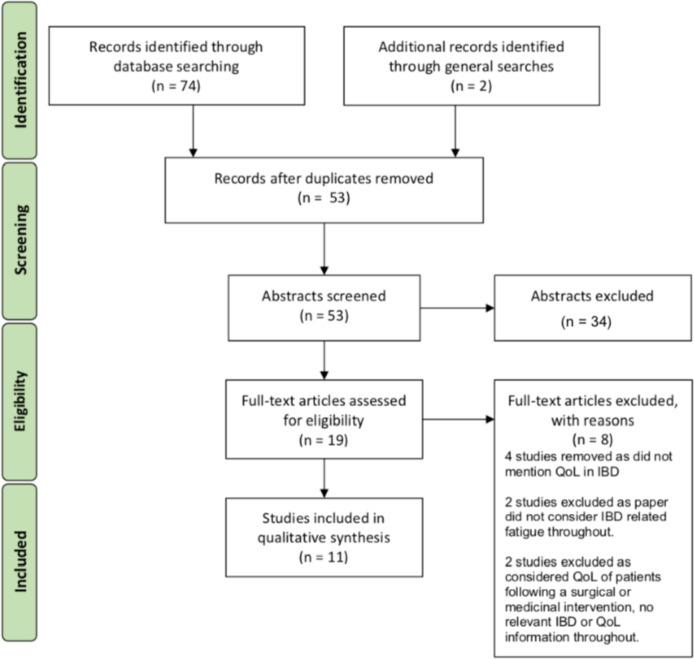
Searches yielded 76 publications overall, with 11 studies meeting inclusion criteria (figure 1). A summary of the included papers and data extracted is shown in table 2.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart of literature search and selection. IBD, inflammatory bowel disease; QoL, quality of life.
Table 2.
Summary of data extracted from the reviewed literature (in ascending chronological order)
| Study | Year | Geographic location | Study design | Sample size and characteristics | Disease activity | Fatigue questionnaires and measurements | HRQoL questionnaires and measurements | Study findings | Quality |
| Castillo-Cejas, et al 39 | 2013 | Spain | Cross-sectional | Two-part study: part 1/99 (55 CD, 44 UC); part 2/137 (70 CD, 67 UC) | Active CD; 49%. Active UC; 46% | DFIS, FSS, MFI | EQ-5D-5L, IBDQ-9 | High levels of disease activity related to high levels of fatigue. High levels of fatigue related to low HRQoL. | High |
| Czuber-Dochan, et al 7 | 2013 | UK | Qualitative | 46 (28 CD, 18 UC) selected from online database | Not disclosed | No questionnaires used, focus group study | Five themes identified: experience, causes, management, consequences and seeking support. Participants described fatigue in terms of how it affected life. High levels of fatigue affected physical and cognitive abilities, impacting on everyday life. | High | |
| Viazis, N. et al 32 | 2013 | Greece | Qualitative | 1181 (827 online questionnaire, 354 outpatient clinic questionnaires) (642 CD, 539 UC) | Not disclosed | Survey of authors’ own design (unvalidated) | 60% of patients felt depressed, 25% felt angry because of IBD fatigue. IBD fatigue interfered with social life in more than half of cases also affecting working capability. Respondents report good social support from family and friends. | Low | |
| Cohen, B. L. et al 35 | 2014 | USA | Prevalence | 220 (125 CD, 95 UC) from disease registry | Active CD; fatigued 44%, non-fatigued 18%. Active UC; fatigued 38%, non-fatigued 22% | FACIT-F scale | SF-36, EuroQoL EQ-5D-5L, IBDQ-32 | Patients with fatigue reported having problems with their usual daily activities, except for self-care. The association of fatigue and impairment were strongest for usual activities. Patients with fatigue had worse valuations of current health status. | High |
| Devlen, J. et al 33 | 2014 | USA | Qualitative | 27 participants (four focus groups), 10 1:1 interviews) (21 UC, 6 CD) | Active disease; 22% (CD/UC not specified) | No questionnaires used, focus group study | 21/27 participants were in disease remission. Patient reported key burdens of IBD fatigue were impact on lifestyle, impact on daily activities, impact on relationships and psychological impact. | Medium | |
| Opheim, R. et al 38 | 2014 | Norway | Cross-sectional | 428 (238 CD, 190 UC) adult IBD outpatients | Active CD; fatigued 73% non-fatigued 45%. Active UC; fatigued 85%, non-fatgued 58% | FSS | Nil | 43% CD and 33% UC reported severe fatigue, 39% reported fatigue severely interfered with daily life. Those with higher education status, working and higher income were less likely to report high fatigue interference. 43% CD and 33% UC reported severe fatigue interference with everyday life. | Medium |
| Van Langenberg, D.R. and Gibson, P.R.8 | 2014 | Australia | Cross-sectional | 379 (181 CD, 113 UC, 85 controls) | Active disease: CD 51%, CD follow-up group 47%, UC 67% | FIS | Nil | Patients with IBD reported significantly higher scores on all global and dimensional fatigue indices compared with controls. Improved physical fatigue was associated with establishing a regular exercise routine. Improvement was seen in cognitive fatigue when immunomodulator therapy ceased. | High |
| Artom, M. et al 40 | 2017 | UK | Cross-sectional | 182 (116 CD, 60 UC) from tertiary care | Those without stoma—active disease 26%, remission 74% (CD/UC not specified) | MFI, IBD-F | IBDQ-32 | There was a significant difference in fatigue and HRQoL according to employment, education, marital and smoking status. Negative fatigue perceptions, 'all-or-nothing' and avoidance behaviours were significantly associated with worse HRQoL. | High |
| Habibi, F. et al 41 | 2017 | Iran | Cross-sectional | 71 (46 UC, 25 CD) | Those with severe disease omitted. Further disease activity data not given | Nil | IBDQ-32 | 44% of sample reported poor sleep quality, linked to daytime sleepiness and fatigue which decreases HRQoL. Higher fatigue level correlated with poorer HRQoL. | Medium |
| Skrautvol, K. and Naden, D34 | 2017 | Norway | Qualitative | 13 (7 CD, 6 UC) | Not disclosed | No questionnaires used, face-to-face interview study | Participants reported tolerance limits might be reflected in a lack of energy. Participants reported the importance of balancing regular physical activity with regular rest. | Medium | |
| Villoria, A. et al 36 | 2017 | Spain | Prevalence | 177 (127 CD, 50 UC) | Not disclosed | FACIT-F scale | IBDQ-9 | Patients with fatigue had higher scores for depression, sleep disturbance and anxiety than those without fatigue. A strong negative correlation was seen between HRQoL and fatigue. Those patients with more severe IBD fatigue had worse anxiety and depression and worse quality of life. | Medium |
CD, Crohn's disease; DFIS, Daily Fatigue Impact Scale; EQ-5D-5L, EuroQual 5-dimension questionnaire (five level); FACIT-F scale, Functional Assessment of Chronic Illness Therapy-Fatigue; FSS, Fatigue Severity Scale; IBD, inflammatory bowel disease; IBD-F, Inflammatory Bowel Disease-Fatigue scale; IBDQ-9/IBDQ-32, Inflammatory Bowel Disease Questionnaire 9(shortened)/32; MFI, multidimensional fatigue inventory; SF-36, 36-item Short Form survey; UC, ulcerative colitis.
Sample characteristics
Eleven studies have been included in the review, four qualitative,7 32–34 two prevalence35 36 and five cross-sectional studies.37–41 Geographical locations of the research studies included the UK,7 40 the USA,33 42 Norway34 38 and Spain,36 39 with one study each from Australia,37 Iran41 and Greece.32 All are considered to be high-income countries with good quality healthcare.
The current review presents data from a total of 2823 adults. Study sample sizes ranged from n=13 to 1181, and 54% of the sample were female. Most settings were outpatient departments, however there was also use of online participation and interview/focus group data collection. One study combined results from inpatient and outpatient areas. A total of 1550 participants studied had Crohn’s disease (CD) (54.9%), 1182 had ulcerative colitis (UC) (41.9%), 85 healthy volunteers (3%) and 6 with IBD-unclassified (0.2%). Reported fatigue prevalence ranged between 26.4% and 54%. All studies reported data from mixed disease states (active or quiescent).
Through the processes of data extraction and thematic analysis, three themes developed as aspects of IBD fatigue that have the greatest influence on HRQoL; symptom acceptance and management, psychosocial well-being and physical activity. Table 3 displays the distribution and frequency of the main themes throughout the reviewed studies.
Table 3.
Main themes from the reviewed literature
| Reviewed studies | Year published | Main themes | ||
| Symptom acceptance and management | Psychosocial well-being | Physical activity | ||
| Castillo-Cejas, M. et al 39 | 2013 | x | ||
| Czuber-Dochan, et al 7 | 2013 | x | x | x |
| Viazis, N. et al 32 | 2013 | x | x | |
| Cohen, B. L. et al 35 | 2014 | x | x | x |
| Devlen, J. et al 33 | 2014 | x | x | x |
| Opheim, R. et al 38 | 2014 | x | x | x |
| Van Langenberg, D.R. and Gibson, P.R.37 | 2014 | x | ||
| Artom, M. et al 40 | 2017 | x | x | x |
| Habibi, F. et al 41 | 2017 | x | x | |
| Skrautvol, K. and Naden, D.34 | 2017 | x | x | x |
| Villoria, A. et al 36 | 2017 | x | ||
Symptom acceptance and management
Ability to accept diagnoses and IBD symptoms can depend on the care patients receive from healthcare professionals. This was particularly highlighted in those of a younger age.33 One study reports 31% of participants were informed about disease advances, however only 30% of those obtained information from healthcare professionals.32 The same study reports 26% of participants do not discuss their treatment with healthcare professionals, with 40% feeling like healthcare professionals are unsupportive of patients making decisions about their own healthcare.7 32
Participants who report feelings of not having control over IBD symptoms experience higher levels of fatigue than those who feel like they have good levels of control.40 41 Altered self-image and fears about stigma caused participants to hold back sharing their diagnosis with friends, family, colleagues and employers.7 32–34 40 Negative fatigue perceptions were associated with greater negative impact on daily activities.40
‘Normalising behaviours’ were described in terms of the participants incorporating their management techniques into their daily lives in order to reduce the negative impact that fatigue has on daily functioning. Those patients who used self-help techniques, such as complementary or herbal therapies, were more likely to report higher levels of fatigue than those who engaged in traditional healthcare.38 Participants using poor methods of fatigue management, such as task avoidance and ‘all or nothing’ behaviours, experienced higher level of fatigue and worse HRQoL than those who did not.40 41 Understanding one’s own physical and cognitive tolerance limits and being able to adjust lifestyle to manage symptoms were highlighted as important steps for some participants.34 Higher levels of IBD-related distress, namely a lack of symptom acceptance or ability to manage symptoms, have been shown to be associated with diminished HRQoL.40
Psychosocial well-being
Anxiety and depression were the factors most frequently associated with high levels of fatigue,7 32 34–37 39–41 contributing to higher psychological distress.36 Patients reported low mood (60%) or anger (25%) because of IBD and symptoms interfering with their social life.32 Both, UC and CD patient populations affected by fatigue exhibit higher anxiety and depression and lower HRQoL than those without IBD.41 42
Fatigue burden was frequently reported by study participants as a reason for limited or missed social interactions.7 32 33 Family and friends have been presented as being supportive, however others, such as employers or colleagues, were reported as lacking in understanding of IBD fatigue.34 Participants reported that they were mindful about depending heavily on family support while also recounting they would feel more supported if the people around them were better informed about IBD fatigue.7 Support from family and friends may compensate for the gaps in support from healthcare professionals as reported by participants.32
Interestingly, none of the studies considered the impact of fatigue on intimate relationships. Only one study touched on the subject of personal relationships, with participants feeling unable to disclose IBD to a new partner for the fear of stigma related to symptoms.33 Two studies reported participants views regarding children; fatigue has impacted their decisions to delay having any children, having more children or not to have children at all.7 33
IBD fatigue was found to interfere with working capability in 40% of study participants, with more than half taking time off work for IBD-related reasons.32 Patients report not progressing in their careers at the same rate as colleagues without IBD fatigue. Participants report choosing not to take on more responsibility or reducing the working hours due to IBD fatigue.7 33–35
Physical activity
Participants reported IBD fatigue impacted on their daily living by increasing absence from work or school, cancelling trips or events and avoiding undertaking certain activities such as sports or travelling.33 Avoidance and ‘all or nothing’ behaviours associated with high levels of fatigue, such as decisions regarding not being in employment, were linked to the negative impact on HRQoL.7 40
High levels of physical fatigue impacted participants’ ability to have a fulfilling life.7 Patients with IBD fatigue reported having problems undertaking usual daily activities when compared with those without fatigue.42 Very few participants reported issues with self-care regardless of fatigue level.42 Patients who commenced a regular exercise programme had greater improvement in the fatigue scores than those who did not.37 Improvements in physical fatigue associated with the introduction of regular exercise were also associated with reduction of depression scores.37 Establishing a regular routine between activity and rest helped some participants establish physical fatigue limits.34 Introducing a healthy average amount of daily activity was important to participants.34
Discussion
The symptom of fatigue across long-term conditions all share characteristics; persistent, reduced energy and reduced muscle strength which is disproportionate to the level of activity, impacting daily physical and cognitive functioning and leading to impaired HRQoL.1 43–49 IBD fatigue has been shown to have a predominantly negative impact on every aspect of an individual’s life.34 50–54
The well-established link between increased disease activity and increased levels of fatigue is presented in many of the included studies.7 32 34–37 39–41 However, disease activity cannot independently explain the presence, or severity, of fatigue as IBD fatigue is also reported in disease remission.55–57 This is also true in other long-term conditions.
Symptom acceptance and management
Patients with IBD often feel it is important to remain ‘in control’ of their health.34 52 58
Unpredictability and uncertainty concerning IBD relapses, treatment options and possible side effects contribute to low HRQoL.52 On the contrary, a diagnosis of a long-term condition can, after time, build an individual’s resilience and can sometimes be a relief, such as eventually getting an answer to questions regarding symptoms.59 60 Symptoms are reported more frequently when the patient has difficulty in coping with the demands of the disease.26 61 Acceptance of IBD and using effective coping strategies, such as task management and pacing, seem to have positive impact on symptom activity and higher levels of HRQoL, whereas negative attitude and ineffective strategies, such as task avoidance, worsens HRQoL.26 58 61 62
Psychosocial support
Stigma is found to be independent of level of disease activity and seems to affect the lives of patients with IBD in multiple ways.63 Stigma related to ill-health has been shown to be connected with the perceived views of employers, coworkers and friends.52 63 In the case of IBD fatigue, like in other long-term conditions, stigma results from perceived physical weakness, cognitive limitations, reduced social activity and the inability to fulfil certain roles within an individuals personal and professional life.64–68
Lack of support from colleagues negatively impacts on an individual’s HRQoL.52 53 Often the steps taken to adjust the work environment to accommodate IBD symptoms can lead to feelings of loneliness, such as adjusting the working day to accommodate more frequent rest breaks.52 62 Patients in full-time work experience significantly higher HRQoL, than those in part-time work, unemployed or absent due to sickness.62 69 Sick leave and work absence was reported to reduce HRQoL.7 32 33 35 38 53 69 This could be attributed to enhanced interaction in those individuals who work or are in education, consequently improving HRQoL.70
A study in multiple sclerosis showed a cycle of depression; social isolation leading to a reduction in social support, contributing to increased depression.71 Similar cycle has been also observed in IBD fatigue.26 57 Social support has been found to be important to individuals and help encourage good coping strategies, while disengagement from social activity had negative affect on HRQoL.26 52 54 62 It is reported that 68% of patients with IBD have experienced social constraint in some way, such as an inability to undertake hobbies or leisure activities.52–54 62 Patients worry that their fatigue restricts their own, and their families’ social activities.52 Close relationships with friends and social support groups are evidenced to positively impact on HRQoL by improving fatigue management.54 58 IBD fatigue has been reported to be a daily concern of 66% of patients; however, only 44% of family and friends and 36% of healthcare professionals demonstrated agreement with the patients’ perceived fatigue levels.72 This kind of discrepancy may result in patients feeling misunderstood and isolated, leading to under-reporting of symptoms. Family and friends occasionally express disbelief that symptoms of IBD are real, causing feelings of hurt and anger in patients.52 62 Some healthcare professionals consider some IBD symptoms as psychological in nature, causing emotional distress among patients due to feelings of lack of support and understanding.62 This is echoed in other long-term conditions, such as chronic fatigue syndrome, where there has been converse viewpoints regarding the origins of fatigue from healthcare professionals and patients.2
Physical activity
There is very little evidence regarding exercise or physical activity in IBD fatigue. The benefit of exercise on an individual level of fatigue was identified in a recent randomised controlled trial.73 The pilot study compared exercise advice, dietary advice, dietary supplementation of omega-3 fatty acids and placebo. It was found that fatigue was considerably reduced in the exercise group.73 Evidence from the review demonstrates that those who commenced a regular exercise programme generally had greater improvement in fatigue scores than those who did not undertake regular exercise.37 This is supported in the wider literature, where introducing regular exercise was associated with more positive feelings, improved HRQoL and better functioning by patients with long-term conditions, such as cancer or multiple sclerosis.74–76
Limitations
There are potential limitations to this work. The use of thematic analysis may be limited by the subjective nature of the reviewer, influencing the repeatability of data analysis. This may introduce an element of interobserver variability, which might limit the reliability of the themes chosen. Thematic analysis may as well be overly reductive and emphasise on less important themes. To increase reliability of this work, the categories and subcategories were reached through discussion with multiple authors.
Multiple databases were searched, and only relevant publications considered. Each publication was discussed by at least two researchers, with a third or fourth being consulted if there were any discrepancies. The outcomes represent an accurate response to the research question. Continuous conversations between authors occurred throughout to ensure a unanimous decision regarding article searches and quality appraisal criteria, thus limiting any potential bias.
The scope of background information collected, disease activity levels, depth of data relating to types and magnitude of fatigue and its effects appears to vary vastly between studies.
Contribution to knowledge
This is the first systematic review considering the impact of IBD fatigue on HRQoL. This review has highlighted the areas of HRQoL identified by individuals with IBD, to be most impacted by IBD fatigue. Uncovering these compounding factors of HRQoL has identified areas for further research and has begun a pathway to better understanding of the patient’s experience of living with IBD fatigue.
Clinical implications
The clinical implications of this work include permitting healthcare professionals to better understand the lived patient experience of IBD fatigue. Healthcare professionals will be better able to consider IBD fatigue holistically taking into consideration factors that have be raised throughout this review. Researchers will be more efficient in designing and conducting targeted research for interventions for both IBD fatigue and IBD-related HRQoL.
Conclusion
This work identified the experiences of fatigue were significantly related to three HRQoL linked themes: symptom acceptance and management, psychosocial well-being and management and physical activity. Individuals with IBD fatigue who exhibit better coping and management mechanisms were shown to have higher levels of HRQoL than those with IBD fatigue who adopted maladaptive behaviours.
Good social support from friends, family and colleague was found to be important to individuals with IBD fatigue and was shown to meaningfully impact on HRQoL. Findings from the review suggest that patients who are more physically active have higher levels of HRQoL than those who are comparatively sedentary.
This would suggest that a psychosocial and/or exercise intervention for fatigue management would be beneficial. Further exploration of the impact of IBD fatigue on HRQoL is warranted in order to better understand patient experiences. There is a need for prospective long-term studies with serial measures of IBD fatigue alongside other key measures, such as HRQoL, anxiety and depression, physical activity, disease activity and measures of disease burden. Exploring this information would allow better understanding of IBD fatigue. Further work with use of validated fatigue and HRQoL measures, and clearer characterisation of disease activity is needed to define a diagnostic cut-off for IBD fatigue that requires an intervention.
Footnotes
Twitter: @Shellie_Jean
Contributors: SJR: whole manuscript preparation, literature searching, data appraisal and extraction, analysis and write up. JMcG: literature searching, data appraisal and extraction and analysis. WC-D: review of manuscript and supervision of data extraction and analysis. GM: whole manuscript review, supervision of data extraction and analysis.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article.
References
- 1. Dittner AJ, Wessely SC, Brown RG. The assessment of fatigue: a practical guide for clinicians and researchers. J.Psychosom.Res 2004;56:157–70. [DOI] [PubMed] [Google Scholar]
- 2. Arnett SV, Clark IA. Inflammatory fatigue and sickness behaviour — lessons for the diagnosis and management of chronic fatigue syndrome. J Affect Disord 2012;141:130–42. 10.1016/j.jad.2012.04.004 [DOI] [PubMed] [Google Scholar]
- 3. Pawlikowska T, Chalder T, Hirsch SR, et al. Population based study of fatigue and psychological distress. BMJ 1994;308:763–6. 10.1136/bmj.308.6931.763 10.1136/bmj.308.6931.763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. van't Leven M, Zielhuis GA, van der Meer JW, et al. Fatigue and chronic fatigue syndrome-like complaints in the general population. Eur J Public Health 2010;20:251–7. 10.1093/eurpub/ckp113 [DOI] [PubMed] [Google Scholar]
- 5. Haney E, Smith MEB, McDonagh M, et al. Diagnostic methods for myalgic Encephalomyelitis/Chronic fatigue syndrome: a systematic review for a national Institutes of health pathways to prevention workshop. Ann Intern Med 2015;162:834–53. 10.7326/M15-0443 [DOI] [PubMed] [Google Scholar]
- 6. Swain MG. Fatigue in chronic disease. Clin Sci 2000;99:1–8. 10.1042/cs0990001 10.1042/cs0990001 [DOI] [PubMed] [Google Scholar]
- 7. Czuber-Dochan W, Dibley LB, Terry H, et al. The experience of fatigue in people with inflammatory bowel disease: an exploratory study. J Adv Nurs 2013;69:1987–99. 10.1111/jan.12060 [DOI] [PubMed] [Google Scholar]
- 8. Van Langenberg DR, Gibson PR. Systematic review: fatigue in inflammatory bowel disease. Aliment Pharmacol Ther 2010;32:131–43. 10.1111/j.1365-2036.2010.04347.x [DOI] [PubMed] [Google Scholar]
- 9. de Rooy E, et al. Concerns of patients with inflammatory bowel disease: results from a clinical population. Am J Gastroenterol 2001;96:1816–21. 10.1016/S0002-9270(01)02440-6 [DOI] [PubMed] [Google Scholar]
- 10. Drossman DA, Patrick DL, Mitchell CM, et al. Health-Related quality of life in inflammatory bowel disease. Dig Dis Sci 1989;34:1379–86. 10.1007/BF01538073 [DOI] [PubMed] [Google Scholar]
- 11. Casati J, Toner BB. Psychosocial aspects of inflammatory bowel disease. Biomed Pharmacother 2000;54:388–93. 10.1016/S0753-3322(01)80006-8 [DOI] [PubMed] [Google Scholar]
- 12. Dibley L, Bager P, Czuber-Dochan W, et al. Identification of research priorities for inflammatory bowel disease nursing in Europe: a Nurses-European Crohn's and colitis organisation Delphi survey. J Crohns Colitis 2017;11:353–9. 10.1093/ecco-jcc/jjw164 [DOI] [PubMed] [Google Scholar]
- 13. Stjernman H, Tysk C, Almer S, et al. Worries and concerns in a large unselected cohort of patients with Crohn's disease. Scand J Gastroenterol 2010;45:696–706. 10.3109/00365521003734141 [DOI] [PubMed] [Google Scholar]
- 14. Czuber-Dochan W, Ream E, Norton C. Review article: description and management of fatigue in inflammatory bowel disease. Aliment Pharmacol Ther 2013;37:505–16. 10.1111/apt.12205 [DOI] [PubMed] [Google Scholar]
- 15. Hart AL, Lomer M, Verjee A, et al. What are the top 10 research questions in the treatment of inflammatory bowel disease? A priority setting partnership with the James Lind alliance. J Crohns Colitis 2017;11:204–11. 10.1093/ecco-jcc/jjw144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mowat C, Cole A, Windsor A, et al. Guidelines for the management of inflammatory bowel disease in adults. Gut 2011;60:571–607. 10.1136/gut.2010.224154 [DOI] [PubMed] [Google Scholar]
- 17. The world Health organization quality of life assessment (WHOQOL): position paper from the world Health organization. Soc. Sci. Med 1995. [DOI] [PubMed] [Google Scholar]
- 18. Lipscomb J, Gotay CC, Snyder C, Definitions and conceptual models of quality of life Outcomes assessment in cancer: Measures, methods, and applications. Cambridge University Press, 2005. [Google Scholar]
- 19. Cohen RD. The quality of life in patients with Crohn's disease. Aliment Pharmacol Ther 2002;16:1603–9. 10.1046/j.1365-2036.2002.01323.x [DOI] [PubMed] [Google Scholar]
- 20. Peyrin-Biroulet L. What Is the Patient’s Perspective: How Important Are Patient-Reported Outcomes, Quality of Life and Disability? Dig Dis 2010;28:463–71. 10.1159/000320403 [DOI] [PubMed] [Google Scholar]
- 21. Bramer WM, Rethlefsen ML, Kleijnen J, et al. Optimal database combinations for literature searches in systematic reviews: a prospective exploratory study. Syst Rev 2017;6:245 10.1186/s13643-017-0644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Booth A, Papaioannou D, Sutton A. The literature review: its role within research. in Systematic Approaches to a Successful Literature Review 1–16 2012.
- 23. Atkinson KM, Koenka AC, Sanchez CE, et al. Reporting standards for literature searches and report inclusion criteria: making research syntheses more transparent and easy to replicate. Res Synth Methods 2015;6:87–95. 10.1002/jrsm.1127 [DOI] [PubMed] [Google Scholar]
- 24. Hart C. Doing a literature search. SAGE London 2001;1:1–25. [Google Scholar]
- 25. García-Vega E, Fernandez-Rodriguez C. A stress management programme for Crohn’s disease. Behav Res Ther 2004;42:367–83. 10.1016/S0005-7967(03)00146-3 [DOI] [PubMed] [Google Scholar]
- 26. Tanaka M, Kazuma K. Ulcerative colitis: factors affecting difficulties of life and psychological well being of patients in remission. J Clin Nurs 2005;14:65–73. 10.1111/j.1365-2702.2004.00955.x [DOI] [PubMed] [Google Scholar]
- 27. Wolfe BJ, Sirois FM. Beyond standard quality of life measures: the subjective experiences of living with inflammatory bowel disease. Qual Life Res 2008;17:877–86. 10.1007/s11136-008-9362-1 [DOI] [PubMed] [Google Scholar]
- 28. Joanna Briggs Institute and The university of Adelaide Critical Appraisal Tools - JBI. Available: http://joannabriggs.org/research/critical-appraisal-tools.html [Accessed 23 Sep 2018].
- 29. Zhang Y, Wildemuth BM. Qualitative Analysis of Content. in Applications of Social Research Methods to Questions in Information and Library Scienc 2009.
- 30. Walsh D, et al. Qualitative metasynthesis: issues and techniques. Qual Health Res 2002;8:365–71. [Google Scholar]
- 31. Pope C, Mays N, Popay J. Synthesizing qualitative and quantitative health evidence : a guide to methods. Open University Press, McGraw Hill Education, 2007. [Google Scholar]
- 32. Viazis N, et al. Inflammatory bowel disease: Greek patients’ perspective on quality of life, information on the disease, work productivity and family support. Ann. Gastroenterol 2013. [PMC free article] [PubMed] [Google Scholar]
- 33. Devlen J, et al. The burden of inflammatory bowel disease: a patient-reported qualitative analysis and development of a conceptual model. Inflamm. Bowel Dis 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Skrautvol K, Nåden D. Tolerance limits, self-understanding, and stress resilience in integrative recovery of inflammatory bowel disease. Holist Nurs Pract 2017;31:30–41. 10.1097/HNP.0000000000000189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Cohen BL, Zoëga H, Shah SA, et al. Fatigue is highly associated with poor health-related quality of life, disability and depression in newly-diagnosed patients with inflammatory bowel disease, independent of disease activity. Aliment Pharmacol Ther 2014;39:811–22. 10.1111/apt.12659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Villoria A, García V, Dosal A, et al. Fatigue in out-patients with inflammatory bowel disease: prevalence and predictive factors. PLoS One 2017;12:e0181435 10.1371/journal.pone.0181435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. van Langenberg DR, Gibson PR. Factors associated with physical and cognitive fatigue in patients with Crohn's disease: a cross-sectional and longitudinal study. Inflamm Bowel Dis 2014;20:115–25. 10.1097/01.MIB.0000437614.91258.70 [DOI] [PubMed] [Google Scholar]
- 38. Opheim R, Fagermoen MS, Bernklev T, et al. Fatigue interference with daily living among patients with inflammatory bowel disease. Qual Life Res 2014;23:707–17. 10.1007/s11136-013-0508-4 [DOI] [PubMed] [Google Scholar]
- 39. Castillo-Cejas MD, Robles V, Borruel N, et al. Questionnaries for measuring fatigue and its impact on health perception in inflammatory bowel disease. Rev Esp Enferm Dig 2013;105:144–53. 10.4321/S1130-01082013000300005 [DOI] [PubMed] [Google Scholar]
- 40. Artom M, Czuber-Dochan W, Sturt J, et al. The contribution of clinical and psychosocial factors to fatigue in 182 patients with inflammatory bowel disease: a cross-sectional study. Aliment Pharmacol Ther 2017. [DOI] [PubMed] [Google Scholar]
- 41. Habibi F, et al. Quality of life in inflammatory bowel disease patients: a cross-sectional study. J. Res. Med. Sci 2017;22:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cohen BL, Zoëga H, Shah SA, et al. Fatigue is highly associated with poor health-related quality of life, disability and depression in newly-diagnosed patients with inflammatory bowel disease, independent of disease activity. Aliment Pharmacol Ther 2014;39:811–22. 10.1111/apt.12659 10.1111/apt.12659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bol Y, Duits AA, Vertommen-Mertens CER, et al. The contribution of disease severity, depression and negative affectivity to fatigue in multiple sclerosis: a comparison with ulcerative colitis. J Psychosom Res 2010;69:43–9. 10.1016/j.jpsychores.2009.11.011 [DOI] [PubMed] [Google Scholar]
- 44. Whitehead L. The measurement of fatigue in chronic illness: a systematic review of unidimensional and multidimensional fatigue measures. J Pain Symptom Manage 2009;37:107–28. 10.1016/j.jpainsymman.2007.08.019 [DOI] [PubMed] [Google Scholar]
- 45. Fukuda K, et al. The chronic fatigue syndrome: a comprehensive approach to its definition and study. Ann Intern Med 1994;121:953–9. 10.7326/0003-4819-121-12-199412150-00009 [DOI] [PubMed] [Google Scholar]
- 46. Armes J, Krishnasamy M, Higginson I. Fatigue in cancer. Oxford University Press, 2004. [Google Scholar]
- 47. Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: one or many? Lancet 1999. [DOI] [PubMed] [Google Scholar]
- 48. Power JD, Badley EM, French MR, et al. Fatigue in osteoarthritis: a qualitative study. BMC Musculoskelet Disord 2008;9 10.1186/1471-2474-9-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. White JH, et al. Exploring the experience of post-stroke fatigue in community dwelling stroke survivors: a prospective qualitative study. Disabil. Rehabil 2012. [DOI] [PubMed] [Google Scholar]
- 50. Gignac MAM, Cott C, Badley EM. Adaptation to chronic illness and disability and its relationship to perceptions of independence and dependence. J Gerontol Series B 2000;55:P362–72. 10.1093/geronb/55.6.P362 [DOI] [PubMed] [Google Scholar]
- 51. Flensner G, Ek A-C, Söderhamn O. Lived experience of MS-related fatigue—a phenomenological interview study. Int J Nurs Stud 2003;40:707–17. 10.1016/S0020-7489(03)00010-5 [DOI] [PubMed] [Google Scholar]
- 52. Woodward S, Dibley L, Coombes S, et al. Identifying disease-specific distress in patients with inflammatory bowel disease. Br J Nurs 2016;25:649–60. 10.12968/bjon.2016.25.12.649 [DOI] [PubMed] [Google Scholar]
- 53. Magalhães J, Castro FDde, Carvalho PB, et al. Quality of life in patients with inflammatory bowel disease: importance of clinical, demographic and psychosocial factors. Arq Gastroenterol 2014;51:192–7. 10.1590/S0004-28032014000300005 [DOI] [PubMed] [Google Scholar]
- 54. Faust AH, Halpern LF, Danoff-Burg S, et al. Psychosocial factors contributing to inflammatory bowel disease activity and health-related quality of life. Gastroenterol. Hepatol. 2012;8:173–81. [PMC free article] [PubMed] [Google Scholar]
- 55. Minderhoud IM, Oldenburg B, Dam PS, et al. High prevalence of fatigue in quiescent inflammatory bowel disease is not related to adrenocortical insufficiency. Am J Gastroenterol 2003;98:1088–93. 10.1111/j.1572-0241.2003.07414.x 10.1111/j.1572-0241.2003.07414.x [DOI] [PubMed] [Google Scholar]
- 56. Romberg-Camps MJL, Bol Y, Dagnelie PC, et al. Fatigue and health-related quality of life in inflammatory bowel disease: results from a population-based study in the Netherlands: the IBD-South Limburg cohort. Inflamm Bowel Dis 2010;16:2137–47. 10.1002/ibd.21285 [DOI] [PubMed] [Google Scholar]
- 57. Häuser W, Stallmach A, Kocalevent R-D, et al. Biopsychosocial predictors of fatigue in quiescent and mild ulcerative colitis: an explorative study. GMS Psycho-Social-Medicine 2005;2:1–10. [PMC free article] [PubMed] [Google Scholar]
- 58. Sainsbury A, Heatley RV. Review article: psychosocial factors in the quality of life of patients with inflammatory bowel disease. Aliment Pharmacol Ther 2005;21:499–508. 10.1111/j.1365-2036.2005.02380.x [DOI] [PubMed] [Google Scholar]
- 59. Duff W, Haskey N, Potter G, et al. Non-Pharmacological therapies for inflammatory bowel disease: recommendations for self-care and physician guidance. WJG 2018;24:3055–70. 10.3748/wjg.v24.i28.3055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sharpe M, Wilks D. Fatigue. BMJ 2002;325:480–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Todorovic V. Providing holistic support for patients with inflammatory bowel disease. Br. J. Community Nurs 2012. [DOI] [PubMed] [Google Scholar]
- 62. Sammut J, Scerri J, Xuereb RB. The lived experience of adults with ulcerative colitis. J Clin Nurs 2015;24:2659–67. 10.1111/jocn.12892 [DOI] [PubMed] [Google Scholar]
- 63. Taft TH, Keefer L, Leonhard C, et al. Impact of perceived stigma on inflammatory bowel disease patient outcomes. Inflamm Bowel Dis 2009;15:1224–32. 10.1002/ibd.20864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Crocker J, Major B. Social stigma and self-esteem: the self-protective properties of stigma. Psychol Rev 1989;96:608–30. 10.1037/0033-295X.96.4.608 [DOI] [Google Scholar]
- 65. Hilbert RA, et al. Social stigma: the psychology of marked relationships. Contemp Sociol 1985. 10.2307/2071381 [DOI] [Google Scholar]
- 66. Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav 2000;41:50 10.2307/2676360 [DOI] [PubMed] [Google Scholar]
- 67. Lebel S, Devins GM. Stigma in cancer patients whose behavior may have contributed to their disease. Future Oncology 2008;4:717–33. 10.2217/14796694.4.5.717 [DOI] [PubMed] [Google Scholar]
- 68. Taft TH, Keefer L, Artz C, et al. Perceptions of illness stigma in patients with inflammatory bowel disease and irritable bowel syndrome. Qual Life Res 2011;20:1391–9. 10.1007/s11136-011-9883-x [DOI] [PubMed] [Google Scholar]
- 69. Zhou Y, Ren W, Irvine EJ, et al. Assessing health-related quality of life in patients with inflammatory bowel disease in Zhejiang, China. J Clin Nurs 2010;19:79–88. 10.1111/j.1365-2702.2009.03020.x [DOI] [PubMed] [Google Scholar]
- 70. Umberson D, Karas Montez J. Social relationships and health: a Flashpoint for health policy. J Health Soc Behav 2010;51:S54–66. 10.1177/0022146510383501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Mohr DC, Hart SL, Goldberg A. Effects of treatment for depression on fatigue in multiple sclerosis. Psychosom Med 2003;65:542–7. 10.1097/01.PSY.0000074757.11682.96 [DOI] [PubMed] [Google Scholar]
- 72. Lesage A-C, Hagège H, Tucat G, et al. Results of a national survey on quality of life in inflammatory bowel diseases. Clin Res Hepatol Gastroenterol 2011;35:117–24. 10.1016/j.gcb.2009.08.015 [DOI] [PubMed] [Google Scholar]
- 73. McNelly AS, Monti M, Grimble GK, et al. The effect of increasing physical activity and/or omega-3 supplementation on fatigue in inflammatory bowel disease. Gastrointestinal Nursing 2016;14:39–50. 10.12968/gasn.2016.14.8.39 [DOI] [Google Scholar]
- 74. Stewart AL, Hays RD, Wells KB, et al. Long-Term functioning and well-being outcomes associated with physical activity and exercise in patients with chronic conditions in the medical outcomes study. J Clin Epidemiol 1994;47:719–30. 10.1016/0895-4356(94)90169-4 [DOI] [PubMed] [Google Scholar]
- 75. Cramp F, Byron-Daniel J, Cochrane Pain, Palliative and Supportive Care Group . Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev 2012;339 10.1002/14651858.CD006145.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. McCullagh R, Fitzgerald AP, Murphy RP, et al. Long-Term benefits of exercising on quality of life and fatigue in multiple sclerosis patients with mild disability: a pilot study. Clin Rehabil 2008;22:206–14. 10.1177/0269215507082283 [DOI] [PubMed] [Google Scholar]