Abstract
In pregnant women with type 1 diabetes, a low but sufficient, intake of carbohydrates is important to aim for near normal glycemic control. However, knowledge about the carbohydrate intake in this group is limited. To assess the average quantity and quality of carbohydrate intake in pregnant women with type 1diabetes compared to healthy pregnant women and current dietary reference intakes. A narrative literature search was performed in PubMed, Embase, and Cochrane Library and by using a snow‐ball search technique to identify papers published on studies conducted in industrialized countries within the last 20 years. Intakes of carbohydrate were assessed qualitatively in relation to the Dietary Reference Intakes recommended by the American Diabetes Association and quantitatively as mean intake of dietary fiber. Five observational studies including 810 pregnant women with type 1 diabetes and 15 observational studies with a total of 118,246 healthy pregnant women were identified. The mean total carbohydrate intake was within the Acceptable Macronutrient Distribution Range (45%–64% of energy intake) in both groups. In pregnant women with type 1 diabetes, the average total intake was 218 ± 19 g/day, which was 20% (53 g/day) lower than in healthy pregnant women. Mean intake of dietary fiber in women with diabetes was lower than the recommended adequate intake for healthy women. With the limitations of pronounced heterogeneity across the included studies, pregnant women with type 1 diabetes reported a mean total carbohydrate intake, which was lower than in healthy pregnant women but still within the recommended range.
Keywords: carbohydrate quality, carbohydrate quantity, dietary reference intake, pregnancy

1. INTRODUCTION
Glycemic control, with postprandial glycemic excursions within a limited range among pregnant women with diabetes, is of uppermost importance for maternal health and for prevention of adverse pregnancy outcome such as congenital malformations, fetal overgrowth, and preterm delivery (Colstrup et al., 2013; Jensen et al., 2004; Tennant et al., 2015). In addition, avoiding excessive gestational weight gain is important for reducing risk of fetal overgrowth in both healthy (Gaudet et al., 2014) and diabetic pregnancy (Mathiesen, 2016). For pregnant women with type 1 diabetes, strict glycemic control can be obtained mainly through a low, but sufficient, intake of carbohydrates and insulin therapy. The American Diabetes Association (ADA) has set the glycemic target during pregnancy to glycated hemoglobin A1c (HbA1C) below 6% (42mmol/mol) if this can be achieved without significant hypoglycemia (American Diabetes Association, 2020). Both in pregnant women with type 1 diabetes and healthy pregnancies, carbohydrates are essential dietary fuel for growth of the fetus (Hanson et al., 2015). Intake of other macronutrients as protein and lipids as well as micronutrients is also important, but will not be covered in this paper.
The quantity and quality of carbohydrate intake are the main determinants of the postprandial glucose in type 1 diabetes pregnancy (Mathiesen & Vaz, 2008). The ADA recommendations for carbohydrates in women with diabetes follow the recommendations for people with diabetes in general (American Diabetes Association, 2020). In summary, ADA recommends that intakes of carbohydrate to be individually targeted following individual treatment goals and consists mainly of carbohydrates of low glycemic index. The ADA recommendations to pregnant women (American Diabetes Association, 2020) is also based on the dietary reference intake (DRI) given by the National Academy of Medicine (NAM, known as Institute of Medicine (IOM)) with at least 175 g carbohydrate daily. The DRI for all pregnant women of 175 g/day of carbohydrates is recommended regardless of presence of diabetes to cover the glucose utilized by the fetus and brain.
Total carbohydrate intake is recommended to be within the Acceptable Macronutrient Distribution Range (AMDR) of 45% to 65% of total energy intake (2005). However, carbohydrate intake in the upper end of this range makes the blood glucose control more challenging (James et al., 2016). ADA recommends an intake of a minimum of 28 g/day of dietary fiber because the amount of dietary fiber, especially viscous type of fiber, may attenuate the postprandial blood glucose response (Abutair et al., 2016).
Changes in macronutrient distribution and total energy have been seen in the population from the 1970s to the 2010s in national dietary surveys from United States (Austin et al., 2011) and Australia (Grech et al., 2018). In the period 1970s to 2013, national dietary surveys from United States (Austin et al., 2011) have demonstrated an increased consumption of energy and carbohydrates. A similar increase was seen in the Australian population until 1995; thereafter, the intake decreased (Grech et al., 2018). Studies assessing the carbohydrate intake in pregnant women with type 1 diabetes in comparison with healthy pregnant women and recommended intake are limited.
The aim of the present study is to assess the average quantity and quality of carbohydrate intake in pregnant women with type 1 diabetes in relation to healthy pregnant women and current dietary reference intakes.
2. METHOD
A narrative review was conducted through a literature search in the following databases: PubMed, Embase, and Cochrane Library and by using a snow‐ball search technique to identify relevant articles. The criteria in selecting the literature were that articles were published in English and within the period 1999–2020.
2.1. Search strategy
For the pregnant women with type 1 diabetes, the search terms in Title and abstracts were ‘‘type 1 diabetes’’ AND “pregnancy” AND “carbohydrate” AND “carbohydrate intake”. As the same search terms for healthy women gave no results, the final search in title and abstract was adjusted to “pregnancy” AND “carbohydrate” AND “macronutrient“ AND “dietary intake”.
The literature search was done in the period April 2019 to June 2019.
2.2. Selection criteria
The inclusion criteria were as follows: observational cross‐sectional studies; published after January 1998; report of daily carbohydrate intake; singleton pregnancy in women and conducted in western countries with type 1 diabetes or in healthy women. In addition, only papers that describe their use of validated dietary assessment tools, including Food Frequency Questionnaire (FFQ), dietary records or from 24‐hr recall were included. Studies were excluded if the participating women had other health conditions than diabetes that might influence dietary intake. If multiple publications were available and collected from the same data set, the publication that reported that largest number of nutrient variables was selected for inclusion.
2.3. Estimation of dietary intake
In studies where information on total carbohydrate, sugar, and dietary fiber intake was provided only in grams, energy intake, or in energy percent, calculations were performed to provide data on intake expressed in energy percent. Simple descriptive statistics with mean carbohydrate intake and standard deviation (SD) of the included studies were calculated for diabetic and healthy women, respectively. Due to a very large range in the individual number of participants in each study the different population size was not taken into account. Carbohydrate intake during pregnancy in the background population was reported for early, mid and late pregnancy, separately. The population characteristics and the method of reporting of the carbohydrate intake varied considerably from study to study and further statistics were therefore not applied.
3. RESULTS
3.1. Carbohydrate intake in pregnant women with type 1 diabetes
A total of 35 articles were identified, where 9 studies were duplicates (Figure 1a). The screening for relevance by title and abstract or full text reading excluded 21 articles, leaving five articles for the narrative review. The five studies were conducted in different countries (Denmark, UK, Canada, and Poland) and they varied in size from 26 to 555 participants (Table 1). The most frequently used dietary assessment method employed was a dietary record (Ásbjörnsdóttir et al., 2017; Kozlowska et al., 2018; Neoh et al., 2018) followed by a Food Frequency Questionnaire (FFQ) (Hill et al., 2012) and a 24‐hr dietary recall (McManus et al., 2013).
FIGURE 1.
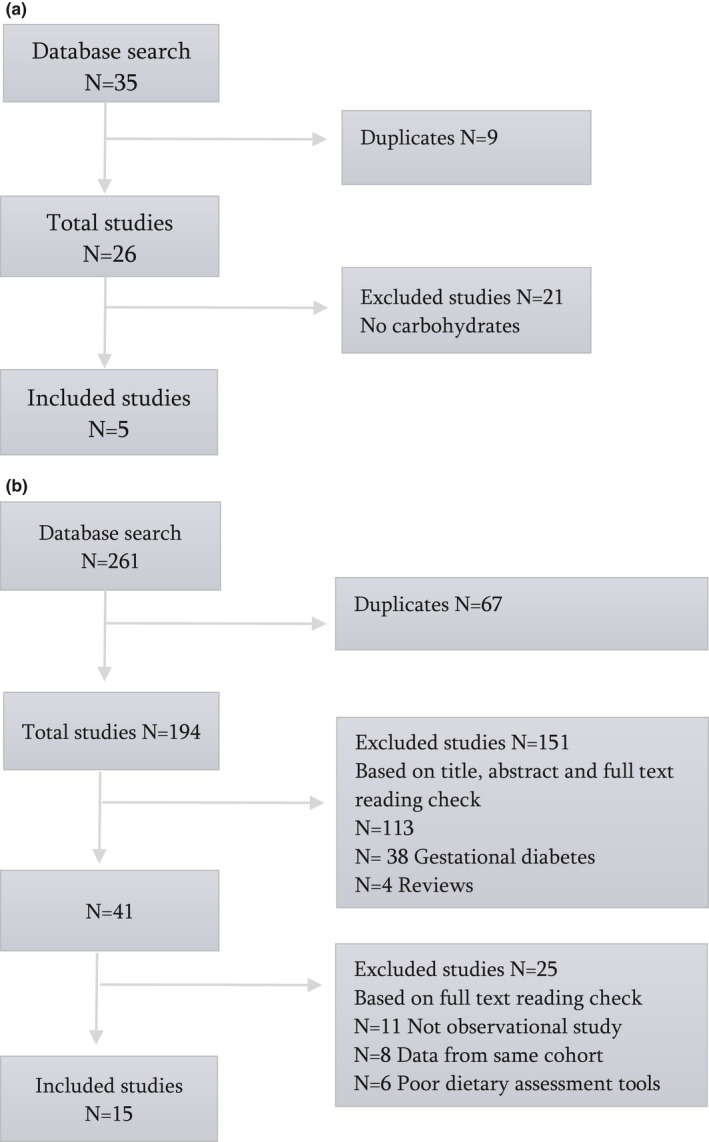
(a) Flow chart of the included studies regarding carbohydrate intake among pregnant women with type 1 diabetes. (b) Flow chart of the included studies regarding carbohydrate intake among healthy 13 pregnant women
Table 1.
The mean dietary intake of energy, total carbohydrate, sugar, and dietary fiber among pregnant women with type 1 diabetes
| Study | Term of pregnancy | No of women | Dietary assessment method | Energy intake (kJ) | Total carbohydrate g/day E% | Sugar g/day | Fiber g/day | |
|---|---|---|---|---|---|---|---|---|
| Ásbjörnsdóttir et al. (2017) | Early | 107 | Dietary record | ‐ | 205 c | NA | ‐ | ‐ |
| Hill et al. (2012) | Mid | 555 | FFQ b | 6,745 | 221 | 55 | ‐ | 21 |
| McManus et al. (2013) | Mid | 29 | 24‐hr dietary recall | 8,058 | 251 | 51 | ‐ | 20 |
| Kozlowska et al. (2018) | Mid | 26 | Dietary record | 7,088 | 215 | 46 | 27 d | 22 |
| Neoh et al. (2018) | Late | 93 | Dietary record | 7,000 | 198 | 50 | 91e | 15 |
| Sum/Total mean | ‐ | 810 | ‐ | 7,401 ± 498 | 218 ± 19 | 51 ± 3 | NA | 20 ± 3 f |
Part of a randomized placebo‐controlled trial. Reference: McCance DR, Holmes VA, Maresh MJA et al. Vitamins C and E for prevention of pre‐eclampsia in women with type 1 diabetes (DAPIT): a randomized placebo‐controlled trial. Lancet. 2010;24:259–266.
Food Frequency Questionnaire.
Major source of carbohydrates (e.g., bread, potatoes, rice, pasta, dairy products, fruits, and candy) and estimated amount from minor source of carbohydrate (e.g., vegetables, nuts, almonds, meatballs, and sauces) was set to 25 gram carbohydrate.
Added sugar; eNonrecommended source of carbohydrates (e.g., sugar, biscuits, cakes, nonalcoholic beverages).
The average of sugar intake is not calculated due to the small sample size and the heterogeneity in the definition of intake.
In total 810 pregnant women with type 1 diabetes were included, with a mean total dietary carbohydrate intake of 218 ± 19 g/day and 51 ± 3 energy percent (Table 1). Due to different definition of sugar intake and small number of samples, the average intake could not be calculated. However, two studies (Kozlowska et al., 2018; Neoh et al., 2018) describe the amount of sugar and the mean intake was 27 g/day and 91 g/day, respectively. Four studies (Hill et al., 2012; Kozlowska et al., 2018; McManus et al., 2013; Neoh et al., 2018) describe intake of dietary fibers with a mean intake of 20 ± 3 and thereby lower than the recommended intake of 28 g/day by ADA (American Diabetes Association, 2020). The mean energy intake was 7,401 ± 498 kJ per day (Table 1).
3.2. Carbohydrate intake during healthy pregnancy
A total of 261 articles were identified, where 67 studies were duplicates (Figure 1b). The screening for relevance by title and abstract or full text reading excluded 151 articles as not relevant, leaving 43 articles for the narrative review. Altogether, 25 studies were excluded because eleven studies were review articles or intervention studies, data from eight studies came from same cohorts, and six studies used nonvalidated dietary assessments tools, leaving 15 articles to be included.
The 15 studies were conducted in different countries (Australian, Denmark, England, Germany, Iceland, Ireland, Norway, Singapore, and USA) and varied in size from 32 to 68,201 participants (Table 2). The most frequently used dietary assessment method employed to obtain the dietary data was a Food Frequency Questionnaire (FFQ). Dietary records and 24‐hr dietary recalls were also used in three of the studies, and one study used both methods.
Table 2.
The mean dietary intake of energy, total carbohydrate, sugar, and dietary fiber among healthy pregnant women
| Study | Term of pregnancy | No of women | Dietary assessment method | Energy intake (kJ) | Total carbohydrate g/day E% | Sugar g/day | Fiber g/day | |
|---|---|---|---|---|---|---|---|---|
| Olafsdottir et al. (2005) | Early | 436 | FFQ a | 8,651 | 262 | 51 | 64h | ‐ |
| Rad et al. (2011) | Early | 32 | Dietary record | 9,301 | 281 | 52 | ‐ | ‐ |
| Murrin et al. (2013) | Early | 1,004 | FFQ a | 10,661b | 306 | 50 | 140i | ‐ |
| Derbyshire et al. (2016) | Early | 51 | Dietary record | 8,715c | 263 | 53 | ‐ | 39m |
| Rifas‐Shiman et al. (2006) | Early | 1,543 | FFQ a | 8,565 | 224 | 55 | ‐ | 20 |
| Diemert et al. (2016) | Early | 200 | Dietary record | 8,314 | 239 | 51 | 103j | 24 |
| Okubo et al. (2014) | Early | 906 | FFQ a | 8,820 | 286 | 57 | ‐ | 26 |
| Blumfield, et al. (2012) | Early | 141 | FFQ a | 7294d | 182 | 41 | 86k | 39 |
| Veyhe et al. (2012) | Mid | 381 | FFQ a | 8,100 | 219 | 46 | 28i | 25 |
| Haugen et al. 2008) | Mid | 40,108 | FFQ a | 9,753e | 313 | 54 | ‐ | ‐ |
| Siega‐Riz et al. (2002) | Mid | 2,247 | FFQ a | 1,184f | 372 | 55 | 24 | |
| Shapiro et al. (2016) | Mid | 1,079 | Dietary record | 8,640 | 251 | 50 | 15h | 18 |
| Chong et al. (2015) | Mid | 835 | Dietary record | 7,962 | 234 | 52 | ‐ | ‐ |
| Knudsen et al. (2013) | Mid | 68,201 | FFQ a | 9,900g | 319 | 56 | ‐ | 27 |
| Scholl (2004) | Late | 1,082 | Dietary record | 10,058 | 309 | 56 | 49l | 15 |
| Sum/total mean | ‐ | 118,246 | ‐ | 9,105 ± 605 | 271 ± 47 | 52 ± 4 | NA | ± 7n |
Food Frequency Questionnaire. b,c,d,e,f,gCalculated cutoff limits to unrealistic reporting of energy intake were used. hDefined as; add sugar. iDefined as; sugar. jDefined as; monosaccharide and saccharose. kDefined as; fructose, glucose, sucrose, maltose, lactose, and galactose. lDefined as; sucrose. mDefined as: southgate fiber and Englyst fiber. nThe average of sugar intake is not calculated due to the heterogeneity in the definition of intake.
In total 118,246 healthy pregnant women were included, with a total mean energy intake of 9,105 ± 605 kJ/day, and the amount of carbohydrate intake was 271 ± 47 g/day corresponding to 52 ± 4 energy percent (Table 2). Mean total carbohydrate intakes were above the RDA values in all studies (Derbyshire et al., 2016; Rifas‐Shiman et al., 2006; Diemert et al., 2016; Okubo et al., 2014; Blumfield, et al., 2012; Veyhe et al., 2012; Siega‐Riz et al., 2002; Shapiro et al., 2016; Knudsen et al., 2013; Scholl, 2004).
Data of dietary fiber (Blumfield, et al., 2012; Derbyshire et al., 2016; Diemert et al., 2016; Haugen et al., 2008; Knudsen et al., 2013; Okubo et al., 2014; Rifas‐Shiman et al., 2006; Scholl, 2004; Shapiro et al., 2016; Siega‐Riz et al., 2002; Veyhe et al., 2012) were available in 10 studies with a total mean intake of 26 ± 8 g/day. Separate data for sugar intake were given in seven studies (Blumfield, et al., 2012; Diemert et al., 2016; Murrin et al., 2013; Olafsdottir et al., 2005; Scholl, 2004; Shapiro et al., 2016; Veyhe et al., 2012), but the definition of sugar intake differed considerably and the average intake could not be calculated. In nine of fifteen studies, food frequency questionnaire was used to estimate dietary intake.
The mean carbohydrate intake in pregnant women with type 1 diabetes was on average 53 g/day lower than in healthy women but still well above the minimum requirement of 175 g/day (Table 1). The mean dietary fiber was 20 ± 3 g/day in pregnant women with diabetes and 26 ± 8 g/day in healthy women and both lower than recommended by ADA.
In five of the studies (Blumfield, et al., 2012; Diemert et al., 2016; Okubo et al., 2014; Rad et al., 2011; Siega‐Riz et al., 2002), data on daily intake of energy and carbohydrate intake were collected at least twice during healthy pregnancy (Table 3). The mean total carbohydrate intake and carbohydrate intake presented as energy percent were almost stable during a healthy pregnancy with small changes from minus 3% to plus 8% during pregnancy in the individual five studies.
Table 3.
Carbohydrate intake in early, mid, and late pregnancy of healthy women
| Study | Energy intake (kJ) | Carbohydrate g/day | ||||
|---|---|---|---|---|---|---|
| Early | Mid | Late | Early | Mid | Late | |
| Diemert et al. (2016) | 8,314 | 8,653 | 9,000 | 239 | 245 | 254 |
| Rad et al. (2011) | 9,237 | 9,496 | 9,525 | 281 | 281 | 281 |
| Siega‐Riz et al. (2002) | 8,565 | 8,941 | ‐ | 270 | 277 | |
| Okubo et al. (2014) | 8,820 | ‐ | 9,586 | 286 | ‐ | 309 |
| Blumfield, et al. (2012) | 7,294 | ‐ | 7,200 | 182 | ‐ | 179 |
4. DISCUSSION
This review provides a new insight of dietary carbohydrate intake in pregnant women with type 1 diabetes. The mean total carbohydrate intake of was around 20% lower in pregnant women with type 1 diabetes compared with the intake of healthy pregnant women. The total carbohydrate intake was 218 ± 19 g/day and thus above the RDA value of 175 g/day (American Diabetes Association, 2020; Mathiesen & Vaz, 2008), and when expressed as energy percent, the total carbohydrate intake was within the AMDR (45–64 energy percent). Intake of dietary fiber was below the recommended adequate intake of 28 g/day (American Diabetes Association, 2020; Mathiesen & Vaz, 2008).
It is reassuring that pregnant women with type 1 diabetes reported a mean total carbohydrate intake which was lower than in healthy pregnant women but still within the recommended range. This relatively low mean carbohydrate intake probably improves the probability of a lower postprandial increase in plasma glucose fluctuations around meals.
Only one (Blumfield, et al., 2012) out of 15 studies in healthy women reported energy percent of carbohydrates below the range of AMDR. However, in this study, the mean energy intake was reported to be considerably lower (7,294 kJ) compared with the other studies, suggesting that the Food Frequency Questionnaire (FFQ) used in this study may not have been able to full depict an accurate dietary intake.
Considering the long‐term focus on the role of sugar intake in relation to health, it is of note that separate data for sugar intake were only available from two studies of pregnant women with type 1 diabetes. In which even report high heterogeneity in the intake at 27 and 91 g/day, respectively, that may relate to differences in the definitions of added sugar or cultural differences of the cohorts.
Overall, the separate intake for sugar intake was available from less than half of the studies of healthy pregnancy. Patients with type 1 diabetes are recommended to minimize their intake of added sucrose (American Diabetes Association, 2020), and this recommendation is especially underlined for pregnant women with type 1 diabetes, where added sugar particularly should be reduced to a minimum (American Diabetes Association, 2020). In a review of healthy pregnancies, women reported approximately 100 g of sugars intake per day where 50 g came from added sugar (Blumfield et al., 2012).
The dietary fiber was lower than recommended by ADA in both pregnant women with diabetes and in healthy pregnancy and lowest among the women with diabetes. Studies reporting the glycemic index of the carbohydrate intake in pregnant women with type 1 diabetes were not identified.
In total, the quality of carbohydrates intake was not documented to be superior among pregnant women with type 1 diabetes when compared to healthy women. Whether the intake of simple sugars for episodes of hypoglycemia may account for this remains speculative. Both the amount and quality of carbohydrates are important for the diabetic women to know in order to tailor the insulin dose to the carbohydrate intake.
Mean carbohydrate intake was reported several times in pregnancy in five of the studies in healthy pregnancies (Blumfield, et al., 2012; Diemert et al., 2016; Okubo et al., 2014; Rad et al., 2011; Siega‐Riz et al., 2002). The mean total carbohydrate intake and carbohydrate intake expressed, as energy percent, was almost stable during healthy pregnancy. This is in accordance with a systematic review (Blumfield, et al., 2012) reporting that the percentage of energy provided by carbohydrate was stable during pregnancy in industrialized countries. Extra energy is often reported required during pregnancy for growth and maintenance of the fetus, placenta, and maternal tissues (2005). However, energy requirements during pregnancy are complex and influenced by many factors, including physical activity. Thus, energy homeostasis in late pregnancy may be achieved by a reduction in physical activity without extra energy intake (Meltzer et al., 2008; Renault et al., 2012). Cumulative reductions in basal metabolic rate during pregnancy are also reported (Forsum & Lof, 2007).
4.1. Strengths and weaknesses
This review is based on a strict search strategy and a comprehensive search in both PubMed, Embase, and Cochrane Library. To our knowledge, this is the first review summarizing the total carbohydrate intake in pregnant women with type 1 diabetes. However, the number of studies identified in this group was low. At the same time, the number of studies in healthy pregnant women was relatively high, improving the external validity for this group. To improve the assessment of carbohydrate intake, data were expressed both as a total daily carbohydrate intake g/day and as the energy percent of total energy intake. However, the study has also several limitations. First, the low number of studies identified for the pregnant women with type 1 diabetes and the pronounced heterogeneity across all studies regarding study design, study duration, eligibility criteria, and cohort sizes. The different dietary methods are of a special concern, as this increases the potential for response bias and measurement error. However, it is acknowledged that some of the differences between the studies may be due to the different dietary assessments tools (Prentice et al., 2011). In general, estimates of dietary intake obtained from Food Frequency Questionnaires (FFQs) tend to be somewhat higher compared to estimates obtained from dietary records (Thomson, 2003), probably due to a lower number of food items, estimated rather than weighed portion sizes and other factors. This is important to keep in mind when comparing different estimates of dietary intake obtained from different dietary assessments tools.
However, as we took a critical appraisal of the dietary assessment methods and only included studies with validated food frequency questionnaire, dietary records, and 24‐hr recall methods, the major sources of potential bias have been excluded.
5. CONCLUSION AND PERSPECTIVES
The mean total carbohydrate intake in pregnant women with type 1 diabetes was lower than in healthy pregnant women but still within the recommended range. Mean dietary fiber intake was lower than recommended for pregnant women regardless of presence of diabetes, and focus on sufficient fiber intake is needed. However, it is a limitation that there was a pronounced heterogeneity across all studies regarding study design, eligibility criteria, and cohort sizes. Additional studies of total carbohydrate intake including data on fiber and sugar intake with their relation to glycemic control and pregnancy outcome are needed in pregnant women with type 1 diabetes before more stringent recommendations for dietary carbohydrate intake during pregnancy can be developed. Focus on the minimum carbohydrate intake that is safe to recommend in pregnant women with diabetes is urgently needed.
6. TRANSPARENCY DECLARATION
The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported. The lead author affirms that no important aspects of the study have been omitted and that any discrepancies from the study as planned have been explained.
CONFLICT OF INTEREST
None of the authors had any conflict of interest.
ACKNOWLEDGMENTS
The authors thank Professor Lars Ove Dragsted at the Department of Nutrition, Exercise and Sports, University of Copenhagen for his excellent, support, and scientific advice in preparing the review. The study is not financially supported by fundraising and none of the authors had any conflict of interest.
Roskjær AB, Ásbjörnsdóttir B, Tetens I, Larnkjær A, Mølgaard C, Mathiesen ER. Dietary intake of carbohydrates in pregnant women with type 1 diabetes—A narrative review. Food Sci Nutr.2021;9:17–24. 10.1002/fsn3.1982
REFERENCES
- Abutair, A. S. , Naser, I. A. , & Hamed, A. T. (2016). Soluble fibers from psyllium improve glycemic response and body weight among diabetes type 2 patients (randomized control trial). Nutrition Journal, 15, 86 10.1186/s12937-016-0207-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association (2020). Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes 2020. Diabetes Care, 43(Suppl. 1), S183–S192. [DOI] [PubMed] [Google Scholar]
- Ásbjörnsdóttir, B. , Akueson, C. E. , Ronneby, H. , Rytter, A. , Andersen, J. R. , Damm, P. , & Mathiesen, E. R. (2017). The influence of carbohydrate consumption on glycemic control in pregnant women with type 1 diabetes. Diabetes Research and Clinical Practice, 127, 97–104. 10.1016/j.diabres.2016.12.012 [DOI] [PubMed] [Google Scholar]
- Austin, G. L. , Ogden, L. G. , & Hill, J. O. (2011). Trends in carbohydrate, fat, and protein intakes and association with energy intake in normal‐weight, overweight, and obese individuals: 1971–2006. The American Journal of Clinical Nutrition, 93, 836–843. 10.3945/ajcn.110.000141 [DOI] [PubMed] [Google Scholar]
- Blumfield, M. L. , Hure, A. J. , Macdonald‐Wicks, L. , Smith, R. , & Collins, C. E. (2012). Systematic review and meta‐analysis of energy and macronutrient intakes during pregnancy in developed countries. Nutrition Reviews, 70, 322–336. 10.1111/j.1753-4887.2012.00481.x [DOI] [PubMed] [Google Scholar]
- Blumfield, M. L. , Hure, A. J. , MacDonald‐Wicks, L. K. , Smith, R. , Simpson, S. J. , Giles, W. B. , Raubenheimer, D. , & Collins, C. E. (2012). Dietary balance during pregnancy is associated with fetal adiposity and fat distributon. The American Journal of Clinical Nutrition, 96, 1032–1041. [DOI] [PubMed] [Google Scholar]
- Chong, M.‐F. , Chia, A.‐R. , Colega, M. , Tint, M.‐T. , Aris, I. M. , Chong, Y.‐S. , Gluckman, P. , Godfrey, K. M. , Kwek, K. , Saw, S.‐M. , Yap, F. , van Dam, R. M. , & Lee, Y. S. (2015). GUSTO Study Group. Maternal Protein Intake during Pregnancy Is Not Associated with Offspring Birth Weight in a Multiethnic Asian Population. Journal of Nutrition, 145, 1303–1310. 10.3945/jn.114.205948 [DOI] [PubMed] [Google Scholar]
- Colstrup, M. , Mathiesen, E. R. , Damm, P. (2013). Pregnancy in women with type 1 diabetes: Have the goals of St. Vincent declaration been met concerning foetal and neonatal complications? The Journal of Maternal‐Fetal & Neonatal Medicine, 26, 1682–1686. [DOI] [PubMed] [Google Scholar]
- Derbyshire, E. , Davies, J. , Costarelli, V. , & Dettmar, P. (2016). Prepregnancy body mass index and dietary intake in the first trimester of pregnancy. Journal of Human Nutrition & Dietetics, 19, 267–273. 10.1111/j.1365-277X.2006.00705.x [DOI] [PubMed] [Google Scholar]
- Diemert, A. , Lezius, S. , Pagenkemper, M. , Hansen, G. , Drozdowska, A. , Hecher, K. , Arck, P. , & Zyriax, B. C. (2016). Maternal nutrition, inadequate gestational weight gain and birth weight: Results from a prospective birth cohort. BMC Pregnancy Childbirth, 16, 224 10.1186/s12884-016-1012-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsum, E. , & Lof, M. (2007). Energy metabolism during human pregnancy. Annual Review of Nutrition, 27, 277–292. 10.1146/annurev.nutr.27.061406.093543 [DOI] [PubMed] [Google Scholar]
- Gaudet, L. , Ferraro, Z. M. , Wen, S. W. , & Walker, M. (2014). Maternal obesity and occurrence of fetal macrosomia: A systematic review and meta‐analysis. BioMed Research International. 640291. 10.1155/2014/640291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grech, A. , Rangan, A. , & Allman‐Farinelli, M. (2018). Macronutrient composition of the australian population’s diet; trends from three national nutrition surveys 1983, 1995 and 2012. Nutrients, 10, 1045 10.3390/nu10081045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanson, M. A. , Bardsley, A. , De‐Regil, L. M. , Moore, S. E. , Oken, E. , Poston, L. , Ma, R. C. , McAuliffe, F. M. , Maleta, K. , Purandare, C. N. , Yajnik, C. S. , Rushwan, H. , & Morris, J. L. The international Federation of Glynecology and Obstetrisc (FIGO) recommendations on adolescent, preconception, and maternal nutrition: “Think Nutrition First”. International Journal of Gynaecology and Obstetrics, 131, S213–S253. [DOI] [PubMed] [Google Scholar]
- Haugen, M. , Brantsæter, A. L. , Alexander, J. , & Meltzer, H. M. (2008). Dietary supplements contribute substantially to the total nutrient intake in pregnant Norwegian women. Annals of Nutrition & Metabolism, 52, 272–280. 10.1159/000146274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill, A. J. , Bronte, J. , Patterson, C. , Young, I. S. , Holmes, V. A. , & McCance, D. R. (2012). Nutrient intake of pregnant women with type 1 diabetes in the DAPIT Trial; relationships with anthropometry and glycaemic control. Proceedings of the Nutrition Society, 71, E167 10.1017/S0029665112002248 [DOI] [Google Scholar]
- Institute of Medicine of the National Academies (2005). Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids (macronutrients) National Academy Press; 2005. Available from https://www.nal.usda.gov/sites/default/files/fnic_uploads/energy/files/fnic_uploads/energy_full_report.pdf [Google Scholar]
- James, M. L. , Green, L. , Amiel, S. A. , Choudhary, P. (2016). Evaluation of the effect of carbohydrate intake on postprandial glucose in patients with type 1 diabetes treated with insulin pumps. Journal of Diabetes Science and Technology, 10, 1287–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen, D. M. , Damm, P. , Moelsted‐Pedersen, L. , Ovesen, O. , Westergaard, J. G. , Møller, M. , & Beck‐Nielsen, H. (2004). Outcomes in type 1 diabetic pregnancies: A nationwide, population‐based study. Diabetes Care, 27, 2819–2823. [DOI] [PubMed] [Google Scholar]
- Knudsen, V. K. , Heitmann, B. L. , Halldorsson, T. I. , Sørensen, T. I. A. , & Olsen, S. F. (2013). Maternal dietary glycaemic load during pregnancy and gestational weight gain, birth weight and postpartum weight retention: A study within the Danish National Birth Cohort. British Journal of Nutrition, 109, 1471–1478. 10.1017/S0007114512003443 [DOI] [PubMed] [Google Scholar]
- Kozlowska, A. , Jagielska, A. M. , Okreglicka, K. M. , Dabrowski, F. , Kanecki, K. , Nitsch‐Osuch, A. , Wielgos, M. , & Bomba‐Opon, D. (2018). Dietary macronutrients and fluid intakes in a sample of pregnant women with either gestational diabetes or type 1 diabetes mellitus, assessed in comparison with Polish nutritional guidelines. Ginekologia Polska, 89, 659–666. 10.5603/GP.a2018.0111 [DOI] [PubMed] [Google Scholar]
- Mathiesen, E. R. (2016). Pregnancy Outcomes in Women With Diabetes Lessons Learned From Clinical Research: The 2015 Norbert Freinkel Award Lecture. Diabetes Care, 39, 2111–2117. [DOI] [PubMed] [Google Scholar]
- Mathiesen, E. R. , & Vaz, J. A. (2008). Insulin treatment in diabetes pregnancy. Diabetes/Metabolism Research and Reviews, 24, 3–20. [DOI] [PubMed] [Google Scholar]
- McManus, R. M. , Bouwmeester, A. , Hinz, L. , Caraiscos, V. B. , Nairn, J. , & Giroux, I. (2013). Costs of recalled and recommended diets for pregnant women with type 1, type 2 and gestational diabetes. Canadian Journal of Diabetes, 37, 301–304. 10.1016/j.jcjd.2013.07.043 [DOI] [PubMed] [Google Scholar]
- Meltzer, H. M. , Brantsater, A. L. , Ydersbond, T. , Alexander, J. , & Haugen, M. , The MoBa Dietary Support Group (2008). The MoBa Dietary Support Group: Methodological challenges when monitoring the diet of pregnant women in a large study; experiences from the Norwegian Mother and Child Cohort Study. Maternal and Child Nutrition, 4, 14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murrin, C. , Shrivastava, A. , & Kelleher, C. C. (2013). Lifeways Cross‐generation Cohort Study Steering Group. Maternal macronutrient intake during pregnancy and 5 years postpartum and associations with child weight status aged five. European Journal of Clinical Nutrition, 67, 670–679. 10.1038/ejcn.2013.76 [DOI] [PubMed] [Google Scholar]
- Neoh, S. L. , Grisoni, J. A. , Feig, D. S. , & Murphy, H. R. , on behalf of the CONCEPTT Collaborative Group (2018). A pre‐specified secondary subgroup analysis among CONCEPTT participants. Diabetic Medicine, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okubo, H. , Crozier, S. R. , Harvey, N. C. , Godfrey, K. M. , Inskip, H. M. , Cooper, C. , & Robinson, S. M. (2014). Maternal dietary glycemic index and glycemic load in early pregnancy are associated with offspring adiposity in childhood: The Southampton Women’s Survey. The American Journal of Clinical Nutrition, 100, 676–683. 10.3945/ajcn.114.084905 [DOI] [PubMed] [Google Scholar]
- Olafsdottir, A. S. , Magnusardottir, A. R. , Thorgeirsdottir, H. , Hauksson, A. , Skuladottir, G. V. , & Steingrimsdottir, L. (2005). Relationship between dietary intake of cod liver oil in early pregnancy and birthweight. BJOG, 112, 424–429. 10.1111/j.1471-0528.2005.00477.x [DOI] [PubMed] [Google Scholar]
- Prentice, R. L. , Mossavar‐Rahmani, Y. , & Huang, Y. (2011). Evaluation and Comparison of Food Records, Recalls, and Frequencies for Energy and Protein Assessment by Using Recovery Biomarkers. American Journal of Epidemiology, 174, 591–603. 10.1093/aje/kwr140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rad, N. T. , Ritterath, C. , Siegmund, T. , Wascher, C. , Siebert, G. , Henrich, W. , & Buhling, K. J. (2011). Longitudinal analysis of changes in energy intake and macronutrient composition during pregnancy and 6 weeks post‐partum. Archives of Gynecology and Obstetrics, 283, 185–190. [DOI] [PubMed] [Google Scholar]
- Renault, K. , Nørgaard, K. , Secher, N. J. , Andreasen, K. R. , Baldur‐Felskov, B. , & Nilas, L. (2012). Physical activity during pregnancy in normal‐weight and obese women: Compliance using pedometer assessment. Journal of Obstetrics and Gynaecology, 32, 430–433. 10.3109/01443615.2012.668580 [DOI] [PubMed] [Google Scholar]
- Rifas‐Shiman, S. L. , Rich‐Edwards, J. W. , Willett, W. C. , Kleinman, K. P. , Oken, E. , & Gillman, M. W. (2006). Changes in dietary intake from the first to the second trimester of pregnancy. Paediatric and Perinatal Epidemiology, 20, 35–42. 10.1111/j.1365-3016.2006.00691.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scholl, T. O. (2004). The dietary glycemic index during pregnancy: Influence on infant birth weight, fetal growth, and biomarkers of carbohydrate metabolism. American Journal of Epidemiology, 1, 467–474. 10.1093/aje/kwh068 [DOI] [PubMed] [Google Scholar]
- Shapiro, A. L. B. , Kaar, J. L. , Crume, T. L. , Starling, A. P. , Siega‐Riz, A. M. , Ringham, B. M. , Glueck, D. H. , Norris, J. M. , Barbour, L. A. , Friedman, J. E. , & Dabelea, D. (2016). Maternal diet quality in pregnancy and neonatal adiposity: The Healthy Start Study. International Journal of Obesity (Lond), 40, 1056–1062. 10.1038/ijo.2016.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siega‐Riz, A. M. , Bodnar, L. M. , & Savitz, D. A. (2002). What are pregnant women eating? Nutrient and food group differences by race. American Journal of Obstetrics and Gynecology, 186, 480–486. 10.1067/mob.2002.121078 [DOI] [PubMed] [Google Scholar]
- Tennant, P. W. , Bilous, R. W. , Prathapan, S. , Bell, R. (2015) Risk and recurrence of serious adverse outcomes in the first and second pregnancies of women with preexisting diabetes. Diabetes Care, 38, 610–619. [DOI] [PubMed] [Google Scholar]
- Thomson, C. A. (2003). Measuring dietary change in a diet intervention trial: Comparing food frequency questionnaire and dietary recalls. American Journal of Epidemiology, 157, 754–762. 10.1093/aje/kwg025 [DOI] [PubMed] [Google Scholar]
- Veyhe, A. S. , Hansen, S. , Sandanger, T. M. , Nieboer, E. , & Odland, J. Ø. (2012). The Northern Norway mother‐and‐child contaminant cohort study: Implementation, population characteristics and summary of dietary findings. International Journal of Circumpolar Health, 71, 18644 10.3402/ijch.v71i0.18644 [DOI] [PMC free article] [PubMed] [Google Scholar]


