Highlights
-
•
COVID-19 can present varied dermatological manifestations.
-
•
Cutaneous small-vessel vasculitis is one of these forms of cutaneous manifestation of COVID-19.
-
•
Vesicobullous hemorrhagic lesions can be the clinical presentation.
-
•
Most cases of cutaneous vasculitis present in mild cases of COVID-19.
-
•
Microvascular thrombosis seems to be part of the pathophysiological process of the cutaneous lesion in COVID-19.
Abbreviations: CoVID-19, coronavirus disease; CSVV, cutaneous small-vessel vasculitis; LCV, leukocytoclastic cutaneous vasculitis; rRT-PCR, real-time reverse transcription polymerase chain reaction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2
Keywords: Coronavirus infections, Cutaneous leukocytoclastic vasculitis, Coronavirus 2019, COVID-19, SARS-CoV-2
Abstract
We described a case of exuberant cutaneous small-vessel vasculitis in a 27-year-old male with mild CoVID-19 in Brazil. The patient presented painful purpuric papules and vesicobullous lesions with hemorrhagic content located in the larger amount in the lower limbs and, to a lesser extent in the region of the back and upper limbs, saving palms and soles of the feet. Influenza-like syndrome with anosmia and ageusia was reported seven days before the skin lesions. A real-time reverse transcription polymerase chain reaction was positive on a nasopharyngeal swab for SARS-CoV-2. Histopathological study showed leukocytoclastic cutaneous vasculitis affecting small vessels and microthrombi occluding some vessels. The patient presented an improvement in skin lesions by the fifth day of prednisone therapy. This case highlights the importance of the SARS-CoV-2 test in investigating the etiology of cutaneous vasculitis during this pandemic.
Introduction
Pandemic coronavirus disease (CoVID-19) has a 0.25 %–3.0 % case-fatality risk estimate, mainly due to pneumonia [1]. Despite the severity of respiratory symptoms, other manifestations have also drawn the attention of the scientific community. Several reports have been described of different cutaneous lesions in CoVID-19 cases. The frequency of skin lesions in these patients varies between 1.8 % and 20.4 % [2]. The major dermatologic morphologies described in CoVID-19 cases were morbilliform, pernio-like, urticaria, macular erythema, vesicle, papulosquamous and retiform purpura [3]. We describe here a case of cutaneous small-vessel vasculitis (CSVV) in a patient affected by CoVID-19.
Case report
A 27-year-old previous healthy male presented to internal medicine department with a 7-day history of skin lesions and low-grade fever, in addition to pain, hyperemia and major testicular edema. The cutaneous lesions had upward progression, located in the larger amount in the lower limbs and, to a lesser extent in the region of the back and upper limbs, sparing the palms and soles of the feet. He denied having any new medications, insect bites, and family history of autoimmune disorders. Flu-like syndrome with anosmia and ageusia was reported seven days before the skin lesions, during peak cases of CoVID-19 in the state of Pernambuco, Brazil. Treatment had been started in the emergency department with acyclovir and ceftriaxone, with no improvement in injuries.
Dermatological examination showed painful purpuric papules and vesicobullous lesions, strained from 0.3 to 5 cm in diameter with hemorrhagic content, some with central necrosis and erythematous halo (Fig. 1, Fig. 2). On admission, blood count, kidney function, liver enzymes and coagulation profile were normal. C-reactive protein level (37 mg/L), D-dimer (7540 ng/mL), and serum ferritin were increased. A clinical diagnosis of cutaneous vasculitis was made and a punch biopsy of one palpable purple papule was performed. Prednisone 1 mg/kg/day and prophylactic enoxaparin were initiated.
Fig. 1.
Tense vesiculobullous and purpuric lesions over bilateral lower extremities.
Fig. 2.
Presence of palpable purpura evident, in addition to the central necrotic areas on the vesicles.
Vasculitis work-up included negative antinuclear antibodies, antiphospholipid antibodies, rheumatoid factor, antineutrophilic cytoplasmic autoantibody, and cryoglobulins with normal serum complement levels. Herpes simplex, HIV, hepatitis B and C, and VDRL test were also negative. A real-time reverse transcription polymerase chain reaction (rRT-PCR) for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was positive in a nasopharyngeal swab.
The patient improved during hospitalization with significant pain relief, with no more fever and no new lesions on the third day of corticosteroid therapy. He also had a reduction in testicular edema and an improvement in skin lesions by the fifth day of therapy. Histopathological study showed leukocytoclastic cutaneous vasculitis (LCV) affecting small vessels, microthrombi occluding some vessels and absence of IgA, IgG, IgM and C3 on direct immunofluorescence examination (Fig. 3, Fig. 4). In the context of pandemic CoVID-19, a confirmatory test for such infection and a negative vasculitis investigation, a diagnosis of CSVV secondary to SARS-CoV-2 infection was established. The patient was discharged using prednisone in good clinical condition.
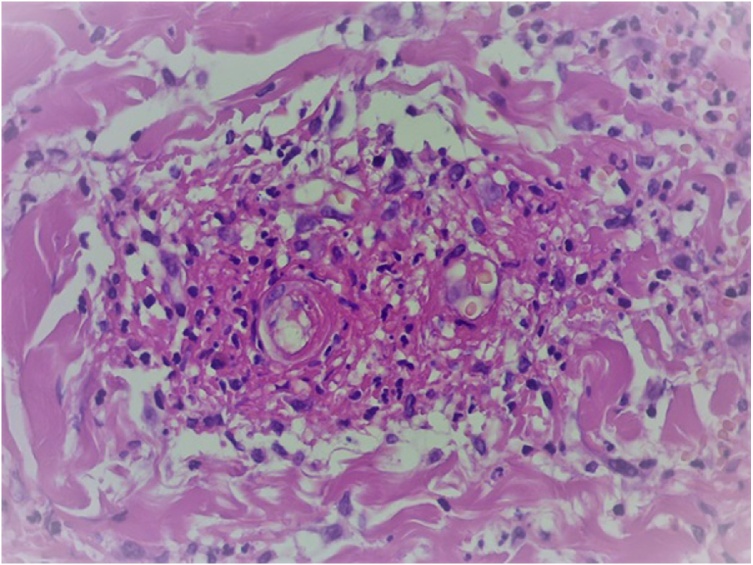
Fig. 3.
Deposition of fibrinoid material within the lumen and small vessel wall associated with neutrophilic inflammatory infiltrate with leukocytoclasia (HE 400x).
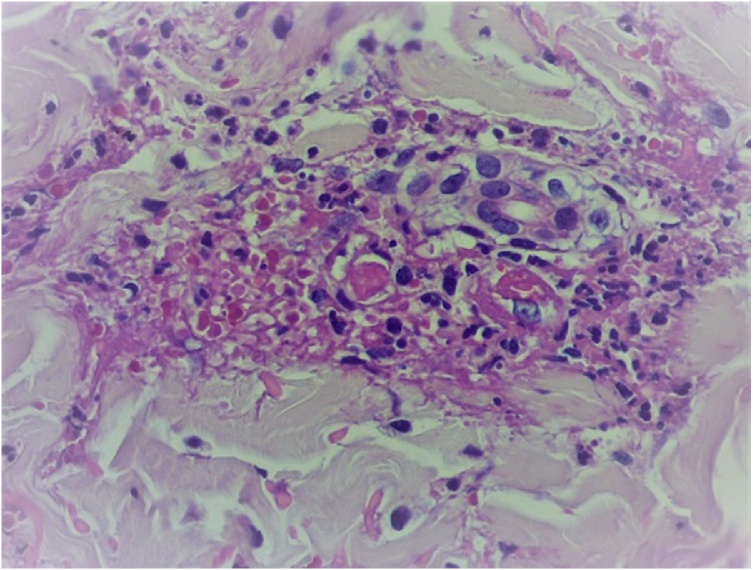
Fig. 4.
Presence of vascular occlusion by fibrina microthrombi (HE 400x).
Discussion
Few cases are described in the literature of CSVV associated with CoVID-19 [[4], [5], [6], [7]], including one case of IgA vasculitis [8]. In researching this diagnosis, we performed histopathology with immunofluorescence, but it was negative. Our patient had more extensive and exuberant bullous hemorrhagic eruptions than similar cases published in Italy and Dubai. The Italian patient, however, had a more severe systemic and pulmonary condition and died, while the other patient was asymptomatic respiratory at the beginning of the skin lesions [5,6].
Most cases of CSVV emerged in mild cases of CoVID-19 [4,6,7]. Authors postulated that, even in these cases, endothelial damage may occur due to an immune response against viral antigen deposition or by an elevation of IL-6 during infection [4]. The “cytokine storm” (an increase in pro-inflammatory cytokines, in particular IL-6) could achieve the skin and activate dermal dendritic cells, lymphocytes and neutrophils, promoting the vasculitis process [2]. The present case, even with no severe systemic inflammatory manifestations of CoVID-19, had extensive vasculitis on the skin. Elevated inflammation markers such as CRP and ferritin corroborate the skin inflammatory process.
Other possibility in developing skin lesions in CoVID-19 patients is activation of coagulation system due to viral load [9]. Magro et al. identified complement activation and microvascular thrombosis in lung and skin biopsies in cases of persistent severe CoVID-19 [10]. Our patient had a remarkably high D-dimer and the presence of microthrombi in the skin biopsy despite the absence of other clinical and laboratory findings of thrombosis.
In summary, we present a case of exuberant bullous CSVV with microvascular thrombosis attributed to mild CoVID-19. We believe that cases of CSVV in undiagnosed patients during this pandemic should be investigated for SARS-CoV-2.
Funding
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
CRediT authorship contribution statement
Pedro Alves da Cruz Gouveia: Conceptualization, Methodology, Writing - original draft, Supervision. Ingrid Cardoso Cipriano: Investigation, Methodology, Data curation, Writing - original draft. Marina Acevedo Zarzar de Melo: Investigation, Methodology. Helena Texeira Araujo da Silva: Investigation, Methodology. Matheus Augusto de Oliveira Amorim: Investigation, Methodology. Clezio Cordeiro de Sá Leitão: Conceptualization, Investigation, Methodology. Maria Magalhães Vasconcelos Guedes: Investigation, Methodology. Daniela Mayumi Takano: Resources, Methodology. Norma Arteiro Filgueira: Conceptualization, Investigation, Methodology. Cláudia Elise Ferraz: Resources, Writing - review & editing.
Declaration of Competing Interest
Authors declare no conflict of interest.
References
- 1.Wilson N., Kvalsvig A., Barnard L.T. Case-fatality risk estimates for COVID-19 calculated by using a lag time for fatality. Emerg Infect Dis. 2020;26(6):1339–1341. doi: 10.3201/eid2606.200320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaya G., Kaya A., Saurat J.H. Clinical and histopathological features and potential pathological mechanisms of skin lesions in COVID-19: review of the literature. Dermatopathology (Basel) 2020;7(1):3–16. doi: 10.3390/dermatopathology7010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman E.E., McMahon D.E., Lipoff J.B. The spectrum of COVID-19-associated dermatologic manifestations: an international registry of 716 patients from 31 countries. J Am Acad Dermatol. 2020;83(4):1118–1129. doi: 10.1016/j.jaad.2020.06.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mayor-Ibarguren A., Feito-Rodriguez M., Quintana Castanedo L. Cutaneous small vessel vasculitis secondary to COVID-19 infection: a case report. J Eur Acad Dermatol Venereol. 2020;34(10):e541–2. doi: 10.1111/jdv.16670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Negrini S., Guadagno A., Greco M. An unusual case of bullous haemorrhagic vasculitis in a COVID-19 patient. J Eur Acad Dermatol Venereol. 2020;34(11):e675–6. doi: 10.1111/jdv.16760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tahir A., Sohail Z., Nasim B. Widespread cutaneous small vessel vasculitis secondary to COVID-19 infection. Int J Dermatol. 2020;59(10):1278–1279. doi: 10.1111/ijd.15106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dominguez-Santas M., Diaz-Guimaraens B., Abellas P.G. Cutaneous small-vessel vasculitis associated with novel 2019 coronavirus SARS-CoV-2 infection (COVID-19) J Eur Acad Dermatol Venereol. 2020;34(10):e536–7. doi: 10.1111/jdv.16663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allez M., Denis B., Bouaziz J.D. Covid-19 related IgA vasculitis. Arthritis Rheumatol. 2020;72(11):1952–1953. doi: 10.1002/art.41428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Criado P.R., Abdalla B.M.Z., de Assis I.C. Are the cutaneous manifestations during or due to SARS-CoV-2 infection/COVID-19 frequent or not? Revision of possible pathophysiologic mechanisms. Inflamm Res. 2020;69(8):745–756. doi: 10.1007/s00011-020-01370-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Magro C., Mulvey J.J., Berlin D. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1–13. doi: 10.1016/j.trsl.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]