Abstract
We describe a case of a middle-aged woman who presented with progressive jaundice and was suspected to have rebound choledocholithiasis, which was initially managed with balloon extraction through endoscopic retrograde cholangiopancreatography at her first presentation. Healthcare in Pakistan, like many other developing countries, is divided into public and private sectors. The public sector is not always completely free of cost. Patients seeking specialised care in the public sector may find lengthy waiting times for an urgent procedure due to a struggling system and a lack of specialists and technical expertise. Families of many patients find themselves facing ‘catastrophic healthcare expenditure’, an economic global health quandary much ignored.
Keywords: biliary intervention, global health, health economics, healthcare improvement and patient safety, general surgery
Background
Catastrophic health expenditure is any event that leads to incurring debt or pushing a person into poverty due to health expenses.1 In countries like Pakistan2 and in other developing countries, this can prove to be a major determinant of healthcare-related issues, delays in care and suboptimal healthcare delivery. One of the reasons that we found could potentially lead to such a financial crunch was shortage of specialists and specialised equipment, even in large urban cities. Although national data supporting this are scarce and difficult to access, there is an estimated shortage of 0.2 million doctors in Pakistan to care for the required population, and this figure does not take into account the shortage of specialists. World Bank data show that specialist surgical workforce is 6 per 100 000 in South Asia compared with 71 per 100 000 in high-income countries. Similarly, for physicians, World Bank data show 0.8 per 1000 in South Asia, whereas high-income countries have 3.0 physicians per 1000. This shortage certainly holds true for most developing countries and is in dire need of a solution. Patients needing urgent procedures may find themselves shuffled between tertiary care public hospitals, yet face a backlog and an unacceptable waiting time even in the face of urgency. This leads to an inevitable struggle in resource-limited settings, where the prioritization of patient’s healthcare issues and waiting time is undertaken by healthcare workers and translates into a mammoth task. It becomes glaringly clear that the only value one can place is in finding solutions to address the need of the time with regard to healthcare delivery.
Case presentation
A 55-year-old woman, a resident of Lahore, presented to surgical emergency at the end of December 2019 with mild jaundice and right hypochondrium pain. An ultrasound done at the time showed a gallstone in the common bile duct (CBD) with a diameter of 10 mm and one gallstone in the gall bladder, suggesting obstructive jaundice. Her bilirubin at the time of admission was 4.0 mg/dL. She was managed medically with hydration, pain management, antibiotics and proton pump inhibitors until definite management via endoscopic retrograde cholangiopancreatography (ERCP) could be undertaken. There are limited pubic sector tertiary care hospitals in the city where an ERCP can be done at a marginally lower cost. Our hospital does not have the facilities for ERCP in its nascent gastroenterology department. Consults were sent at the time to different public sector hospitals with ERCP facilities, with the case explained, and patients were given varying waiting times for the procedure, ranging between 2 weeks and 3 months. The patient in this case report was stable and doing better. However, after a week, her family found that the waiting time for the earliest appointment had been increased to a month instead of 2 weeks. They proceeded to get her ERCP done from a gastroenterologist working at a private hospital.
It must be noted, and stressfully for the sake of comparison, that an ERCP done privately costs more than a junior doctor’s monthly salary, and such a cost places an extremely high burden on a family working on daily wage, as was the case with our patient’s husband, who belongs to a lower income strata of the society. They earned an income of between 10 000 and 20 000 Pakistani rupees a month, while an ERCP costs between 50 000 and 80 000 Pakistani rupees. With the help of their relatives, savings and by selling some assets, they were able to procure the amount needed and proceeded with ERCP on 2 January 2020. At this time the size of her CBD was 18 mm, her bilirubin was 5.4 mg/dL and her total leucocyte count was 4.4×109/L. ERCP found a large filling defect and a balloon sweep was done and the stone was removed. There was a thick sludge present with some pus, along with distal CBD stenosis for which stenting was done and was removed 2 weeks later, at which time her ultrasound showed a CBD calibre of 8.7 mm, with a contracted gall bladder with minimal sludge and no stones. No malignant lesion was identified at this time. She was discharged from the surgical floor 5 days later with a diagnosis of choledocholithiasis, but in good health and with normal laboratory parameters. An ultrasound follow-up performed by a radiology resident showed no stones in the gall bladder and a CBD of normal calibre.
Three weeks later, she presented to us again deeply jaundiced, with fever of 38.3C and right hypochondrium pain, associated with nausea and general malaise. An ultrasound performed the following day showed CBD dilatation of 16 mm with proximal stone, dilated intrahepatic biliary channels and a liver span of 14.8 cm. The gall bladder was contracted. Her bilirubin was 3.5 mg/dL, alanine transaminase (ALT) was 84 U/L, and amylase and electrolytes were within normal limits. International normalised ratio (INR) was 1.2, the normal range of which is 0.8–1.0. She had a significantly raised white cell count (WCC) of 16.7×109/L. The clinical picture was suggestive of cholangitis.
Suspecting rebound choledocholithiasis, even though the interval was inexplicably short, and ascending cholangitis, she was once again started on medical management with broad spectrum antibiotics, hydration and symptomatic management. Consults were sent to various public hospitals for an urgent ERCP; however, the earliest time that was available was 1 month later. The family explained how they were now financially bankrupt after her previous stay in the hospital and that they would first try to wait and see how she responds to non-interventional management.
One week into her second admission she had an INR of 1.5, an activated partial thromboplastic time that was prolonged by 8 s, suggesting the development of coagulopathy, a WCC of 22.2x109/L with 93% neutrophil differential, a platelet count of 22x109/L (150–450x109/L), and a haemoglobin of 83 g/L from a baseline haemoglobin of 131 g/L. Her total bilirubin was 11.8 mg/dL, with a direct component of 5.4 mg/dL and indirect 6.4 mg/dL. Her serum creatinine was 1.8 mg/dL and showed onset of acute tubular necrosis. Her calcium was 7.2 mg/dL and albumin was 2.4 g/dL. Electrolytes were within the normal range. Her Glasgow Coma Scale (GCS) score had begun to drop and it was 10/15 at this point. She was drowsy and incoherent. She had developed non-pitting, dependent oedema on her arms and legs. Her urine output had decreased to 0.5 mL/kg/hour from 2 mL/kg/hour. The clinical picture coupled with the laboratory parameters suggested the onset of multiorgan dysfunction syndrome. She maintained her vitals, but needed 5 L of oxygen via face mask to maintain saturations, and she had coarse basal crepts. We decided to give her mannitol on suspicion of acute tubular necrosis and a detailed urine report and culture were sent. Blood cultures previously sent reported no growth and fresh cultures were sent. The intensive care unit team was consulted and said her arterial blood gas showed metabolic acidosis and that she did not require mechanical ventilation at the moment and to continue treatment in the high dependency unit. The family was counselled regarding her deteriorating condition and decided to speak to the gastroenterologist who had initially done her ERCP. Two days later her GCS score was 13/15, and responding to the mannitol she was now producing good urine output, although she was still oxygen-dependent and intermittently drowsy. Realising this might be a small golden window before the sepsis and multiorgan dysfunction progressed to irreversible septic shock unless biliary drainage was achieved, the private practice gastroenterologist was personally called by the surgical team. A discounted ERCP was agreed on and this was then funded by the doctors in the spirit of charity and marginally covered by the family. An ambulance was arranged, with high-risk consent and counselling, and the patient was taken for ERCP on oxygen a day later. One must acknowledge that this delay and financing crisis for healthcare could have been averted given the public healthcare system was adequately equipped and able to cope with healthcare demands. Further, one would envision that charitable funds should be readily available through a system where such a need arises, rather than ad-hoc collection by doctors in the ward.
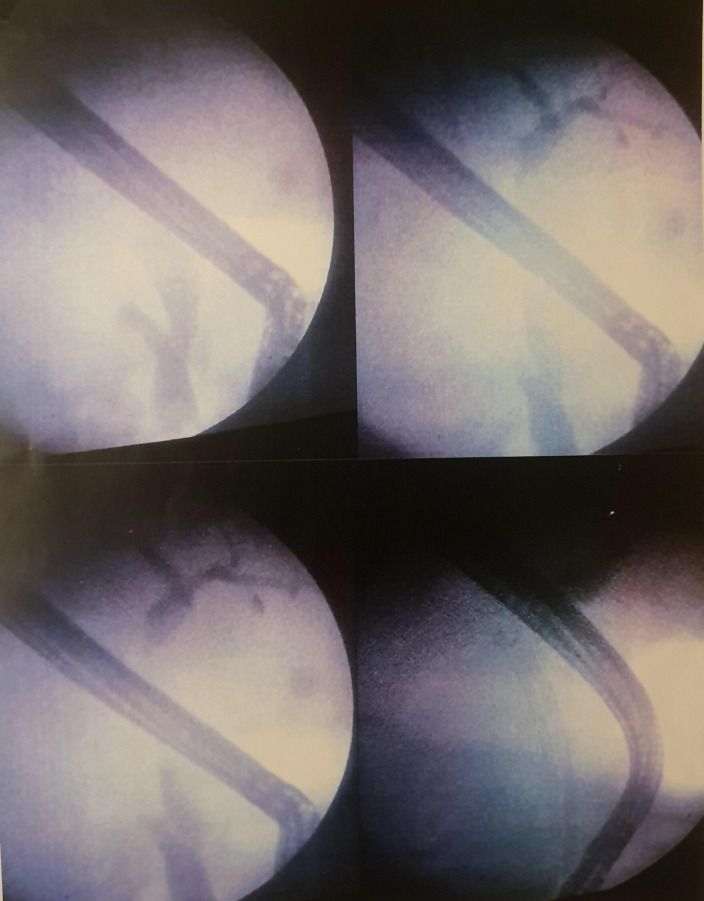
ERCP this time proved to be a surprise. There was an ulcer seen in the duodenum, which was likely a stress ulcer from critical care despite proton pump inhibitors and possibly the cause of her slowly decreasing haemoglobin. There was some fungating tissue identified proximal to the ampulla. The CBD was dilated but there was no stone. The common hepatic duct showed stricturing, and the distal CBD stricture was present and had increased in length; two biliary stents were placed, each of 10F. Hepatobiliary malignancy was strongly suspected (figure 1).
Figure 1.
Images at the time of the second endoscopic retrograde cholangiopancreatography.
During the ERCP her blood pressure had been borderline hypotensive at 95/60 and 100/65, with tachycardia of around 100–110 beats per minute. The gastroenterologist worked at a small private practice with limited capabilities of handling emergency situations; thus, the sedation given for the ERCP was also conservative and limited in nature given her drowsy state and overall sick condition and the risk of the patient becoming apnoeic and needing intubation and a ventilator as a result. The gastroenterologist, after placing the stent with difficulty and with a procedure that took around 35 min, with the patient becoming agitated towards the end as the sedation weaned off, suggested that a redo ERCP after a CT scan of the abdomen could be undertaken for biopsy as the patient’s condition was not fit to undergo a lengthier procedure. The main objective of placing the stents and allowing biliary drainage was achieved. He took the decision to abort the procedure at that moment and not take a biopsy of the fungating mass which had been visualised earlier in the procedure. Had an ERCP been available timely in a public hospital, a biopsy might have been viable when the patient was in better medical condition to tolerate the procedure and sedatives.
Although her ultrasound at first discharge showed a CBD of normal calibre, ultrasound has its limitations in terms of visualisation, and due to stent placement the proximal CBD may have shown to be of normal calibre. It is important to understand and note that many ultrasounds in public healthcare hospitals are performed by radiology residents initially and are only taken for re-evaluation by a consultant if there are positive findings or if there are findings that the resident might not understand. In short, this is due to a very large workload with limited residents and limited consultants available in most public hospitals in Pakistan. Further, we understand that ultrasound is user-dependent, which is one of its largest limitations. Thus, missed findings on an ultrasound are ubiquitously common.
Although the ultrasound and the ERCP reports may seem inconsistent, as in our case initially, we realise that hepatobiliary malignancy is notoriously aggressive and a 3-week interval would be sufficient for such an extensive progression of the disease. Due to the association of CBD strictures with gallstones, the initial CBD stricture was not imagined to be malignant or due to external compression from malignancy; thus, at that time, further investigations with imaging were not undertaken and would have been once the patient had come back for an interval cholecystectomy, although unfortunately she presented earlier than planned with disease progression.
The patient improved during her stay in the ward after stenting and drainage were accomplished. Her GCS score improved and her jaundice decreased. She was transfused with packed cells and haemoglobin built up. Due to septic acute tubular necrosis a CT scan with contrast was not undertaken. Instead a Ca-19-9 level was sent, which was highly raised at 400.8 U/mL.
At discharge, a month after her readmission, her WCC had settled to 12.4×109 /L. Haemoglobin was 108 g/L and there was no melaena present which had occurred a week earlier following the ERCP. Her INR and partial thromboplastin time (PTT)were normal and her vitamin K was stopped. Bilirubin had come down to 3.8, with a creatinine of 0.7. Her ALT had improved to 22. Post-ERCP amylase was followed, which had risen to 119 U/L (normal up to 80); however, it had decreased to 70 U/L at discharge. She was now able to take a few steps on her own and speak sentences, which she was not able to previously. She had been given partial parenteral nutrition during her stay for a week and was at discharge able to tolerate semisolid and liquid in small quantities. A nutritionist was involved to help with adequate caloric intake at home. Oncology was consulted before discharge and requested tissue biopsy and CT imaging; however, the patient and her husband refused any aggressive management or further work-up.
They had been counselled regarding the high suspicion of hepatobiliary malignancy given the absence of gallstones, progressive disease in the biliary tree from the previous ERCP and the short time before rebound symptoms occurred following previous discharge. Respecting their decision she was discharged on palliative medicine.
Many of the issues and shortcomings that are highlighted in this patient’s care fall under the umbrella of global health issues faced by many patients in developing countries. Issues include delays in care due to uncoordinated care in one tertiary care hospital, requiring private practice visits, and spending time getting appointments from other public hospitals due to lack of available specialists and technology. Cumbersome healthcare costs that bring about a crippling financial blow to those in the lower income strata are a well-known issue in global health. Funding in terms of sourcing and structure of healthcare, especially in developing countries, in order to achieve universal healthcare coverage and achieve standardised and safe healthcare is highlighted in our patient’s case.
Timeline of hospital stay
The patient was admitted with choledocholithiasis and obstructive jaundice.
First ERCP undergone 10 days after admission, stone retrieved, biliary stricture identified and biliary stents placed.
Two weeks later stents removed and the condition of the patient was satisfactory.
Discharged 5 days later.
Readmitted 3 weeks after discharge, with suspicion of cholangitis and rebound choledocholithiasis.
11 days later redo ERCP done, suspicion of biliary malignancy raised and biliary stents placed.
Tumour marker for hepatobiliary malignancy returned raised, and the patient’s condition improved after redo ERCP.
12 days after redo ERCP, the patient was discharged in stable condition on palliative care as per the patient and her family’s wishes.
Global health problem list
Catastrophic financial events related to healthcare.
Shortage of specialists in developing countries even in large urban areas.
Burden on limited specialists available.
Costs of public and private healthcare.
Global health problem analysis
Catastrophic financial events overburden patients who are below poverty line and their family. In the South East Asian region, out-of-pocket expenditures account for nearly 60% of all healthcare expenditures.3 In India, a survey found that nearly 8% of the population had been pushed below poverty line due to catastrophic healthcare expenditures in 2015. Further it is estimated that 3.3% of the population faces this dilemma yearly.4 5 This is an unreasonably high amount of expenditure that is being borne by the patients in times of illness. The trend for catastrophic expenditures increases in countries where insurance or free-of-cost public healthcare is unable to cover the costs for the individuals, and developing countries in the region frequently face this issue. In Pakistan the gross domestic product (GDP) expenditure on healthcare was 0.97% in 2017–2018, and as the World Bank data show in South Asia the current expenditure on health as a whole was 3.55% of GDP. This expenditure could merit a modest increase, which could in turn help decrease financial risk being incurred by poorer populations. In Pakistan out-of-pocket expenditures may be as high as 70%.6 The Asian Development Bank found that 24.3% lived below the poverty line, 4.5% were unemployed and 2.3% were employed below $1.90 per day.7 With these, along with the increasing costs of healthcare, a larger proportion of individuals find themselves below poverty line due to catastrophic events, while those already below it find themselves further crippled. Overburdened by loans and selling of liquid assets, individuals desperately try to achieve dignity and a chance at healthcare for their loved ones. The solutions for this are multifold: public health insurance2 and access to care without incurring the costs of long distance travel. Staying in a city with no support is one of the important barriers to healthcare access, as per the Eastern-Meditteranean Regional Office of the World Health Organisation (EMRO) health systems profile and is applicable to many other developing nations.
Healthcare funding in Pakistan takes different forms. A study identified nine major sources, which included the federal government, the provincial government, the district government, social security funds, autonomous bodies, private health insurance, out-of-pocket expenditures, local non-governmental organisations (NGOs) and official donor agencies. Of these, in 2007–2008, 66% were from out-of-pocket expenditures, and largely the scenario could be extrapolated to be similar today. All three government-level funding combined was only 23% and local NGOs and official donor agencies combined provided nearly 8% of healthcare funding.6 Crowdfunding is a relatively new concept where funds are generated by small donations online for a cause. Crowdfunding for healthcare in Pakistan occurs through informal platforms such as Facebook and WhatsApp and through formal organisations such as Transparent Hands.8 Similar to Transparent Hands there are other crowdfunding sources available for healthcare in Pakistan; however, the outreach is limited to specific individuals and cases. This could definitely be capitalised on with public hospitals partnering up with a crowdfunding organisation that could then transparently and publicly allocate funds on a need basis to these public hospitals, whether at a national, provincial or district level. Further, it would encourage donors if one handling body can provide more transparency than donating to different groups or on a case-by-case basis via social media outreach.
Rwanda is one such country that tried to introduce a community-based health insurance scheme, in which socioeconomic groups were stratified into four and premiums were set based on their income, with the lowest earning group paying no premium. However, this model, although in theory could decrease out-of-pocket payments and increase health coverage, is dependent on enrolment of community members and annual enrolment. Given that enrolment rates drop or are not sufficient and incentives are not sufficient for the higher premium paying groups to enrol, the model would inevitably fail as the pool of insurance decreases. A study done showed that low adherence may be due to discontent on prolonged waiting times until being seen by a healthcare provider and time between healthcare service delivery.9 This ultimately ties up with the fact that there is severe shortage of healthcare providers, both general practitioners and specialists, in most developing countries. Out-of-pocket payments and seeing a private healthcare practitioner reduce delays in care and waiting times, thus ensuring service satisfaction to an affording strata of society. However, this in itself is a problem one would face if introducing a community-based healthcare insurance scheme in developing countries like Pakistan, such that those who are able to pay the premium would be unlikely to visit a public healthcare hospital, thus disincentivising participation in such a scheme. Greater government funding and directing healthcare funding from NGOs and other organisations into restructuring public hospitals to provide care and services for all strata of society, through research into what higher income groups would want to see in a public healthcare system before they used it, might help in the success of such a community-based insurance health scheme or any public health insurance scheme that envisions to protect societies’ most disenfranchised from entering debt through healthcare costs.
Public healthcare in Pakistan is currently undergoing a change that is meeting resistance in the form of the Medical Teaching Institutions Act, which aims to revamp tertiary care teaching hospitals with a board of governors that would handle administrative operations. This includes but is not limited to funding and creation of posts and handling the needs that each specific hospital has. This is in a way an attempt to introduce a ‘business’ model to public healthcare in Pakistan. The ‘business’ of hospital administration has come under scrutiny multiple times in the past, including with the National Health Service, although refuted on many accounts. Hospitals in the USA have faced this backlash recently during the COVID-19 pandemic.10 11 Despite these criticisms, in developing countries, introducing a board of governors in public hospitals, delegating resource mobilisation, and handling and fund raising at a hospital level might be in part solutions to protecting poorer patients from catastrophic healthcare-related debts.
The EMRO profile found that nearly two-thirds of consultations initially occur with a private practitioner, likely due to the backlog in public healthcare facilities and the lack of trust in healthcare delivery in the public healthcare system borne out of the burden and backlog they face. This figure also ties up greatly with the fact that there is specialist shortage in developing countries,12 for if there were more specialists available there would be more doctors to see patients in the public healthcare system, thus decreasing the backlog. With better delivery of care and less burden on fewer specialists, patients will find themselves gaining trust in the public healthcare system, thus fewer having to resort to paying out of pocket for private healthcare.
Developing countries face a shortage of doctors—57 countries have an absolute shortage of 2.3 million physicians.12 There is also a brain drain, where doctors hoping for better education, healthcare and security for themselves and their families tend to leave for developed countries, which was a tangible solution for many to overcome physician shortage. This insomuch created a large physician to population discrepancy between developed and developing countries.13 14 Furthermore, many trained specialists settled in developed countries, leaving a dearth of trained specialists in their native countries.15
In India, which has a similar social ethos to Pakistan and has faced similar healthcare challenges in the past few decades, it was found that the primary healthcare coverage was close to optimal; however, 70% of specialist posts for rural communities lay vacant. The study further stressed on the need for more specialists and specialist care to optimally provide for those in rural areas or smaller cities, thus avoiding the backlog faced by larger tertiary care hospitals in large cities.16 Similarly, in Bangladesh one can find that the concentration of doctors is in four of its larger cities, where only a minority of the population lives. The rural areas find less doctors willing to work there due to decreased resources available to them and no growth potential professionally, among others. Creating incentives for specialist doctors to work in areas which are less appealing in developing countries is key to increasing healthcare delivery, alongside increasing specialist healthcare workforce. Both human resources and technical resources would have to be made available to them in these areas.17 Iran has faced a large emigration of doctors in the last few years and has recognised that it has a shortage of specialist doctors in various fields. It is actively trying to increase their numbers. Further, the Iranian government, realising that the urban density of specialists is higher, created mobility so that more specialist doctors could be available in rural areas. Iran is an example of a country that has recognised the issue of specialist healthcare shortage and is in the process of resolving it.18
Both in India and Bangladesh corruption was identified as a factor of why doctors are resistant to working outside big cities.16 17 These include corrupt practices in promotions, in resource allocation and in funding. Pakistan is no stranger to this phenomenon, and deep-rooted corruption has been a hindrance to healthcare coverage in the country.19 However, understanding corruption and its solution is beyond the scope of this article. It is essential to note that it plays a role in developing countries in both spheres of what this article is aiming to bring light to, which is that there is shortage of specialist healthcare delivery in developing countries and this is largely tied to increased out-of-pocket expenditure and incurring debt in a large section of their population.
However, the quantity of physicians and specialists is only part of the problem; the other lies in the quality of care. Quality of care provided by a handful of physicians is a multifaceted problem in developing countries, where resources to provide quality care, medical education and training, and adherence to guidelines are all interlinked and contribute to the problem of substandard quality of care. The solution lies in addressing all of these issues, working on each issue side by side.20 Once again, an increase in specialists providing education and training to medical students and residents, especially those who may have received specialist education from developed countries, may provide a viable interim bridging solutions; thus, specialist shortage is tied to the problem at hand even in terms of delivery of quality care.
Ameliorating the quality of care and the quality of physicians is a broad field, although there are many examples from developing countries that show that, with the right collaborations and efforts, improving quality service delivery is very much possible. The Carabayllo model used to combat tuberculosis in Peru showed that, with correct collaborations and funding, teams could be created that in essence had transparency to their work. Maintaining ledgers, providing a systems-based approach to a problem, and on-site regulation and provision of medical supplies were some of the ways that enabled them to achieve better quality of care with existing human resources. However, central to these models is gaining confidence among all stakeholders, from the government down to the healthcare workers, and having them work as a team targeting specific problems.21 These models have proven successful for infectious diseases and some chronic diseases. However, the problem we find that is being underaddressed is that of specialist care, and the quality of care can be addressed here in a similar way. Given governments understand where and which specialists are lacking, systems can be designed to help rotate specialists through these areas with incentives and a system designed to promote transparency. Quality of care and delivery of care may improve in such a way.
The lack of technical medical equipment22 23 and the costs of operating and maintaining such equipment in developing countries are surely reasons why some of these specialists do not return. Of course, lack of technical resources, although an impediment, could be partly compensated for by increasing efficiency in systems and processes in healthcare service delivery in low-income countries, as was seen in Jamaica.20 Furthermore, one must appreciate that where medical equipment and technology are lacking, this is not limited to the availability of ERCP or radiological minimally invasive procedures, among many other advances that developing countries have a dearth of—both due to lack of skilled manpower and lack of equipment. Electronic health records, something simple that is well established in the developed world, is still lacking in the developing countries, especially so in public or subsidised healthcare bodies.24–27 This lack of simple electronic medical records, and broadly speaking medical technology and equipment, utilities that most physicians come to rely on while training and practising in developed countries, disincentivises practitioners from returning to practice in their native countries and underlies a large reason as to why many physicians seek to practise and train in developed countries, thus leading to healthcare worker migrancy and in precis contributes to dearth in specialists. Incentive building via access to medical equipment in developing countries may make specialists return and render services—this becomes a global health dilemma with an onus that lies on all countries.
In Pakistan a vice chancellor of one of the large university hospitals expressed that community centres were the need of the hour in Pakistan. In lieu of community centres, mid-sized tertiary care hospitals, with small district clusters around them, where various specialists are available, might cater better to the needs of the patients. Although primary healthcare, and above all specialised primary healthcare,28 and its importance cannot be emphasised enough for developing countries to ameliorate health indicators and outcomes,29 primary or basic healthcare cannot compensate for the lack of specialist healthcare services. Even in large tertiary care hospitals not all specialties are available and weak referral systems are in place, with weak emergency medical services systems to begin with.30 However, these are all but a few cogs of a very large problematic wheel.
There are many multifaceted issues that developing countries face in terms of healthcare delivery, access and quality of care. We found that catastrophic events leading to financial crisis, specialist shortages and shortage of medical equipment were all interlinked and tied together and were important perspectives we gained from our patient’s story. We reported this case to focus on the fact that increasing specialist doctors and medical equipment available might decrease the burden on the ones present in the few scattered tertiary care hospitals. Further, patients may benefit from expedient healthcare delivery, avoiding costly and delayed healthcare. Increasing awareness through reporting of such cases might start a global initiative to increase access to medical equipment for the present specialists and to train more specialists in every area in developing countries.
Patient’s perspective.
Patient’s perspective through her husband and his perspective:
“So, when my wife first became sick, I took treatment from private hospitals, I’m a poor man and I didn’t have many resources, I took loans from people to finance her treatment. I kept getting her treated, but it didn’t help much. After that I brought her here to the hospital. You saw her and recommended an ERCP as the next step. I went to other government hospitals for an ERCP appointment, but they gave a long waiting time, and this issue was best resolved quickly. So, I took some loans from people, some financial help we got from our doctors, and I had the ERCP done. Financially, I have no resources left I am extremely worried. I haven’t worked, since December, till today; I have been caregiving and been with my patient. At home, I only have one son, and five daughters. Only my son earns, and our house is also on rent. We are getting by with great difficulty. While she was admitted here she was quite troubled, she had given up hope, and wasn’t sure what the future held for her. Now, thank God, she is somewhat better.”
Learning points.
There is grave limited resources in the health sector of developing countries and affordability of treatment may be a recurring issue even in public healthcare, and these need to be addressed.
Identifying patients and their hardships and stories is vital to engender a process that will lead to solutions.
Advocating for patients by healthcare workers is vital in resource-limited settings to ensure they get the correct diagnostic work-up and treatment.
Key aspects, whether on hearsay or based on practice, should be identified especially with regard to the difficulties faced in local settings, such as shortages in specialist care as well as shortages in equipment needed by specialists.
Raise your voice and unearth the facts and figures pertinent to these deficiencies to pave the way forward towards a solution.
Global health approaches must inculcate a perspective where the patient, their families and their circumstances are accounted for to plan effective healthcare without compromise.
Acknowledgments
We would like to acknowledge Servier Pakistan for providing access to BMJ Case Reports.
Footnotes
Twitter: @vishalraza
Contributors: KJK was involved with conception, report writing and editing, planning and overseeing the discussion pertaining to the case, and final analysis of the work. VFR was involved with acquisition of data, writing and editing the case report, conception and idea evolution, and discussions pertaining to the work and its development.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Next of kin consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Li Y, Wu Q, Xu L, et al. Factors affecting catastrophic health expenditure and impoverishment from medical expenses in China: policy implications of universal health insurance. Bull World Health Organ 2012;90:664–71. 10.2471/BLT.12.102178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Raza VF, Iftikhar M, Gulab A, et al. Impressions and attitudes of adult residents of Karachi towards a possible public health insurance scheme. J Pak Med Assoc 2017;67:1460–5. [PubMed] [Google Scholar]
- 3.Majumder MAA. Economics of healthcare financing in WHO South East Asia region. SE Asia J Pub Health 2013;2:3–4. 10.3329/seajph.v2i2.15936 [DOI] [Google Scholar]
- 4.Kumar K, Singh A, Kumar S, et al. Socio-economic differentials in impoverishment effects of out-of-pocket health expenditure in China and India: evidence from WHO SAGE. PLoS One 2015;10:e0135051. 10.1371/journal.pone.0135051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swetha NB, Shobha S, Sriram S. Prevalence of catastrophic health expenditure and its associated factors, due to out-of-pocket health care expenses among households with and without chronic illness in Bangalore, India: a longitudinal study. J Prev Med Hyg 2020;61:E92–7. 10.15167/2421-4248/jpmh2020.61.1.1191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khalid M, Sattar A. Households study on out-of-pocket health expenditures in Pakistan. Forman J Econ Stud 2016;12:75–88. 10.32368/FJES.20161205 [DOI] [Google Scholar]
- 7.Poverty data: Pakistan [Internet], 2020. Available: https://www.adb.org/countries/pakistan/poverty
- 8.Husain O. Lahore-based startup helps fund critical healthcare for country’s poor. The Express Tribune 2016. [Google Scholar]
- 9.Mukangendo M, Nzayirambaho M, Hitimana R, et al. Factors contributing to low adherence to community-based health insurance in rural Nyanza district, southern Rwanda. J Environ Public Health 2018;2018:2624591. 10.1155/2018/2624591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Squires M. Is the NHS a business? Br J Gen Pract 2014;64:257–8. 10.3399/bjgp14X679886 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKee GA. US hospitals function like businesses. That’s why they are struggling amid COVID pandemic. USA Today, 2010. [Google Scholar]
- 12.Naicker S, Plange-Rhule J, Tutt RC, et al. Shortage of healthcare workers in developing countries--Africa. Ethn Dis 2009;1:S1–60. [PubMed] [Google Scholar]
- 13.Al-Shamsi M. Addressing the physicians' shortage in developing countries by accelerating and reforming the medical education: is it possible? J Adv Med Educ Prof 2017;5:210–9. [PMC free article] [PubMed] [Google Scholar]
- 14.Patel V. Recruiting doctors from poor countries: the great brain robbery? BMJ 2003;327:926–8. 10.1136/bmj.327.7420.926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eastwood JB, Conroy RE, Naicker S, et al. Loss of health professionals from sub-Saharan Africa: the pivotal role of the UK. Lancet 2005;365:1893–900. 10.1016/S0140-6736(05)66623-8 [DOI] [PubMed] [Google Scholar]
- 16.Deo MG. "Doctor population ratio for India - the reality". Indian J Med Res 2013;137:632–5. [PMC free article] [PubMed] [Google Scholar]
- 17.Darkwa EK, Newman MS, Kawkab M, et al. A qualitative study of factors influencing retention of doctors and nurses at rural healthcare facilities in Bangladesh. BMC Health Serv Res 2015;15:344. 10.1186/s12913-015-1012-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Financial Tribune Doctor-People ratio improving, shortage of specialists persists, 2017. [Google Scholar]
- 19.Yousafzai AW. Corruption in medical practice: where do we stand? J Ayub Med Coll Abbottabad 2015;27:515–6. [PubMed] [Google Scholar]
- 20.Peabody JW, Taguiwalo MM, Robalino DA, et al. Improving the quality of care in developing countries : Jamison DT, Breman JG, Measham AR, et al., Disease control priorities in developing countries. Washington, DC, 2006. [PubMed] [Google Scholar]
- 21.Berwick DM. Lessons from developing nations on improving health care. BMJ 2004;328:1124–9. 10.1136/bmj.328.7448.1124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Compton B, Barash DM, Farrington J, et al. Access to medical devices in low-income countries: addressing sustainability challenges in medical device donations. NAM Perspectives 2018;8 10.31478/201807a [DOI] [Google Scholar]
- 23.Moyimane MB, Matlala SF, Kekana MP. Experiences of nurses on the critical shortage of medical equipment at a rural district hospital in South Africa: a qualitative study. Pan Afr Med J 2017;28:100. 10.11604/pamj.2017.28.100.11641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Afrizal SH, Hidayanto AN, Handayani PW, et al. Narrative review for exploring barriers to readiness of electronic health record implementation in primary health care. Healthc Inform Res 2019;25:141–52. 10.4258/hir.2019.25.3.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Odekunle FF, Odekunle RO, Shankar S. Why sub-Saharan Africa lags in electronic health record adoption and possible strategies to increase its adoption in this region. Int J Health Sci 2017;11:59–64. [PMC free article] [PubMed] [Google Scholar]
- 26.Fraser HSF, Biondich P, Moodley D, et al. Implementing electronic medical record systems in developing countries. Inform Prim Care 2005;13:83–95. 10.14236/jhi.v13i2.585 [DOI] [PubMed] [Google Scholar]
- 27.Mustafa I. Intensive care in developing countries in the Western Pacific. Curr Opin Crit Care 2004;10:304–9. 10.1097/01.ccx.0000132653.52131.fc [DOI] [PubMed] [Google Scholar]
- 28.Okpokoro E. Primary health care: a necessity in developing countries? J Public Health Afr 2013;4:e17. 10.4081/jphia.2013.e17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rao M, Pilot E. The missing link--the role of primary care in global health. Glob Health Action 2014;7:23693. 10.3402/gha.v7.23693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zia N, Shahzad H, Baqir S, et al. Ambulance use in Pakistan: an analysis of surveillance data from emergency departments in Pakistan. BMC Emerg Med 2015;15(Suppl 2):S9. 10.1186/1471-227X-15-S2-S9 [DOI] [PMC free article] [PubMed] [Google Scholar]