Abstract
Background
Recent review of hypertension guidelines requires fresh updates of prevalence and control rates. Though retrospective analysis provided burden estimates, control rates were grossly misleading. We set out to update the prevalence and control rates of hypertension in the USA using contemporary NHANES data.
Methods
Persons with mean systolic blood pressure (mSBP) ≥130 mmHg or mean diastolic blood pressure (mDBP) ≥80 mmHg or self-reported current use of antihypertensive medications were classified as hypertensives. Hypertensives on medications with mSBP <130 mmHg and mDBP <80 mmHg were classified as having well-controlled hypertension. Subgroup comparisons of hypertension prevalence were computed using Chi-square test. Predictors of hypertension and well-controlled BP were assessed using multivariable logistic regressions. Two tailed p-values <0.05 were considered statistically significant.
Results
The prevalence of hypertension in the USA in 2017–2018 was 49.64% (95% CI 46.67–52.61) corresponding to 115(95% CI 104–128) million persons. NH Blacks: 58.53% (95% CI 55.39–61.60); Men: 54.46% (95% CI 51.01–57.87); older persons and obese individuals: 61.03% (95% CI 57.31–64.63) as well as persons with diabetes and CKD, comparatively. The overall rate of well-controlled hypertension was 39.64% (95% CI 36.20–42.81). Persons with at least a college degree: OR 2.20(95% CI 1.02–5.04, p=0.049) and persons with incomes ≥3 times the poverty threshold; OR 1.88(95% CI 1.1.8–2.99, p=0.011) had higher rates of well-controlled hypertension when compared to lowest categories.
Conclusion
One in every two persons ≥20 years in the USA has hypertension with only 39.64% on medications having well-controlled hypertension. Significant discrepancies exist in the burden and control rates in different subpopulation categories. Targeted interventions could help improve the prevalence and hypertension control rates in the USA.
Keywords: Hypertension, Prevalence, Blood pressure control
1. Introduction
Hypertension remains the most significant and modifiable risk factor for cardiovascular diseases worldwide [1]. For several decades since the recognition of hypertension as a major disease condition, the threshold for diagnosis and treatment was considerably higher [2]. New evidence however showed reasonable benefits with intensive blood pressure (BP) control targeting lower BP goals compared to then standard management with higher BP treatment goal [3]. This ushered in the new era in hypertension management characterized by a lower diagnostic threshold and BP treatment target for hypertension [4].
Following this major revision in guidelines, there has been renewed efforts aimed at defining the true burden of hypertension and rates of well-controlled BP. However, this has been greatly limited by the absence of contemporary data. Retrospective analysis of existing data however provided early insights on the prevalence and rates of well-controlled hypertension [5]. Using the 2015–2016 NHANES survey data (then latest available data preceding the update in guidelines), the prevalence of hypertension in the USA according to updated guidelines was 45.4%, corresponding to an estimated 108 million individuals [5]. Though the prevalence of hypertension is very high, Non-Hispanic (NH) Blacks, increasing age, and persons with comorbidities such as diabetes and chronic kidney disease (CKD) continue to have higher prevalence, comparatively.
Though the retrospective analysis provided early insights into the burden of hypertension, evaluating rates of BP control against new treatment targets, which were then not used as treatment goals, could be grossly misleading as a quality measure. With new available nationally representative data following the change in guidelines, it is necessary to provide reliable and context relevant estimates of the prevalence and control rates of hypertension in the USA. It is in this light that we set out to provide updates on the prevalence of hypertension and rates of well-controlled blood pressure as well as their determinants in the USA using the NHANES data of 2017-208 survey cycle.
2. Methods
2.1. Survey design
The NHANES, conducted by the Center for Disease Control/National Center for Health Statistics, collects nationally representative data on the health and nutritional status of non-institutionalized US population. It utilizes a multistage probability sampling design and targets approximately 5000 persons in 15 counties per year. Detailed information on the survey design is available from the survey documentation [6]. We included records of participants aged 20years or older with valid entries of systolic and diastolic blood pressure.
2.2. Data collection
Survey participants were interviewed in their homes to ascertain demographic characteristics (age, gender, level of education, ethnicity, marital status, place of birth, health insurance and smoking status) using a Computer-Assisted Personal Interviewing system (i.e., interviewer-administered). Questions on disease conditions were generally followed by four categorical response options (“Yes” “No” “Refuse” “Don't know”). Persons who responded “Yes” were classified as “Yes” and all other responses were classified as “No”. Persons who reported current cigarette use were classified as active smokers and all others including past smokers were classified as nonsmokers. The body mass index (BMI) was calculated from measured weight and height at subsequent follow up visits in the mobile examination center by trained health technicians using standard protocols. BMI(kg/m2) was grouped into three categories: <25.00, 25.00–29.99, ≥30.00, representing normal, overweight and obesity, respectively. The family poverty index ratio (PIR) was computed by dividing the total family income by the poverty threshold income, as defined by the USA census bureau, with adjustment for family size at the time of the interview [7]. Family PIR of <1 and ≥ 1 were defined as living “below poverty line” and “at or above poverty line”, respectively. Family PIR was grouped into 3 categories (PIR<1.00, PIR 1.00–2.99 and PIR≥3.00). Laboratory measures were completed on collected specimens using standard laboratory methods [8]. Persons with hemoglobin A1C values of ≥6.5%, those who reported taking antidiabetic medications or insulin or persons with random blood sugar >200 mg/dl were classified as having diabetes. Glomerular filtration rate (GFR) was computed using the CKD-EPI formula [9]. Persons with GFR values < 60 mL/min per 1.73 m2 or with albumin-creatinine ratio >30 mg/g were classified as having chronic kidney disease (CKD) [10].
Three consecutive blood pressure (BP) readings with at least 30 seconds intervals in between measurements were obtained by certified technicians following at least 5 minutes of complete rest. If a BP measurement was interrupted or incomplete, a fourth attempt was made. Mean systolic and diastolic blood pressures were computed using all valid entries. Persons who reported current use of antihypertensive medications, or with mean diastolic systolic blood pressures ≥130 mmHg or with a mean diastolic ≥80 mmHg, respectively, were classified as having high blood pressure in accordance with the updated AHA guidelines [4]. Persons who reported current use of antihypertensive medications with either mean systolic blood pressure ≥130 mmHg or mean diastolic blood pressure ≥80 mmHg were considered as having uncontrolled high blood pressure in accordance with the updated AHA guidelines [4]. All study questionnaires, exact question wording, response options and data are available free to the public [11].
2.3. Statistical analysis
Master data file was compiled by merging relevant data files containing variables of interest. To ensure that our findings are representative of the entire non-institutionalized USA population, analysis was conducted in keeping with stipulated analytical guidelines using appropriate survey weights [12]. Included in our analysis were persons 20 years or older with valid blood pressure entries. With only 4% (weighted percentage) of participants with missing blood pressure values, further statistical measures to address missing data were deemed unnecessary. Prevalence measures are reported in percentage. Associations of various variables with hypertension and blood pressure controlled were assessed using Chi squared test. Determinants of hypertension and well-controlled blood pressure were further assessed using a multivariable logistic regression model comprising of variables with association p < 0.10. All analyses were done using STATA 16 and two-tailed p-values less than 0.05 were considered statistically significant.
3. Results
3.1. General characteristics
Of the 9,254 individuals who participated in the NHANES 2017–2018 cycle, 5,569 persons were 20 years or older. Of these, about 96% had valid BP recordings. Some reasons for absent BP values were time constraint and refusal among others. About 52% of the study population were women. Most of our study participants were Non-Hispanic (NH) Whites and about 62% had at least some college level of education. Approximately 12% lived below the poverty line and about 73% were at least overweight. The prevalence of smoking, CKD and diabetes were 17.36%, 15.85% and 12.79%, respectively. Table 1 shows the general characteristics of our study participants.
Table 1.
Table showing general characteristic of study population and prevalence of hypertension.
| Variable | Category | All (%) | Prevalence of hypertension % (95% CI) |
p-valuea | Multivariate analysisb |
|
|---|---|---|---|---|---|---|
| OR (95% CI) | p-valueb | |||||
| All | 49.64 (46.67–52.61) | |||||
| Age (years) | 20–44 | 44.01 | 27.22 (24.63–29.98) | <0.0001 | 1 | – |
| 45–54 | 16.06 | 54.05 (46.12–61.78) | 2.95 (2.11–4.12) | <0.001 | ||
| 55–64 | 19.56 | 65.81 (62.12–69.31) | 4.97 (4.00–6.19) | <0.001 | ||
| 65–74 | 12.05 | 72.33 (66.43–77.54) | 5.43 (4.36–6.76) | <0.001 | ||
| ≥75 | 8.31 | 86.17 (81.95–89.53) | 14.58 (10.41–20.41) | <0.001 | ||
| Gender | Male | 48.4 | 54.46 (51.01–57.87) | 0.0001 | 1 | |
| Female | 51.6 | 45.13 (41.52–48.79) | 0.60 (0.48–0.78) | <0.001 | ||
| Race | NH White | 62.64 | 50.01 (45.61–54.41) | <0.0001 | 1 | – |
| Hispanic | 15.44 | 41.85 (38.49–45.30) | 0.87 (0.65–1.16) | 0.307 | ||
| NH Black | 11.43 | 58.53 (55.39–61.60) | 1.80 (1.42–2.29) | <0.001 | ||
| Others | 10.49 | 49.25 (43.58–54.95) | 1.32 (0.93–1.87) | 0.108 | ||
| Education | Less than high school | 11.07 | 54.03 (48.56–59.41) | 0.0017 | 1 | – |
| High school or GED | 27.35 | 52.04 (47.83–56.22) | 1.00 (0.79–1.27) | 0.998 | ||
| Some college | 30.68 | 53.87 (49.53–58.15) | 1.16 (0.89–1.51) | 0.250 | ||
| College and above | 30.91 | 41.61 (35.61–47.94) | 0.68 (0.46–1.01) | 0.054 | ||
| Poverty (PIR) | <1 | 12.44 | 44.13 (38.27–50.16) | 0.2061 | ||
| 1 to 3 | 36.14 | 51.37 (47.20–55.53) | ||||
| ≥3 | 51.42 | 49.36 (44.71–54.03) | ||||
| Place of birth | USA | 81.04 | 50.29 (46.88–53.71) | 0.1404 | ||
| Non-USA | 18.96 | 46.87 (46.68–52.61) | ||||
| Smoking | Active smoker | 17.36 | 50.11 (46.62–53.60) | 0.3314 | ||
| No active smoker | 82.64 | 47.42 (42.92–51.96) | ||||
| BMI | Normal | 26.10 | 33.14 (28.15–38.53) | <0.0001 | 1 | – |
| Overweight | 30.35 | 47.50 (43.81–51.22) | 1.42 (0.98–2.05) | 0.063 | ||
| Obese | 43.55 | 61.03 (57.31–64.63) | 2.59 (1.91–3.52) | <0.001 | ||
| CKD | Yes | 15.85 | 77.52 (71.94–82.27) | <0.0001 | 2.15 (1.48–3.12) | 0.001 |
| No | 84.15 | 44.60 (41.52–47.73) | 1 | – | ||
| Diabetes | Yes | 12.79 | 83.62 (80.39–86.42) | <0.0001 | 2.60 (1.87–3.62) | <0.001 |
| No | 87.21 | 44.66 (41.59–47.77) | 1 | – | ||
| Insurance | Yes | 86.26 | 37.91 (30.33–46.12) | 0.0016 | 1.18 (0.85–1.65) | 0.306 |
| No | 13.74 | 51.51 (48.49–54.53) | 1 | – | ||
Represents output from univariate analysis.
Represents output from multivariable logistic regression. Only variables with p-values less than 0.1 were retained for multivariate logistic regressions.
3.2. Burden of hypertension
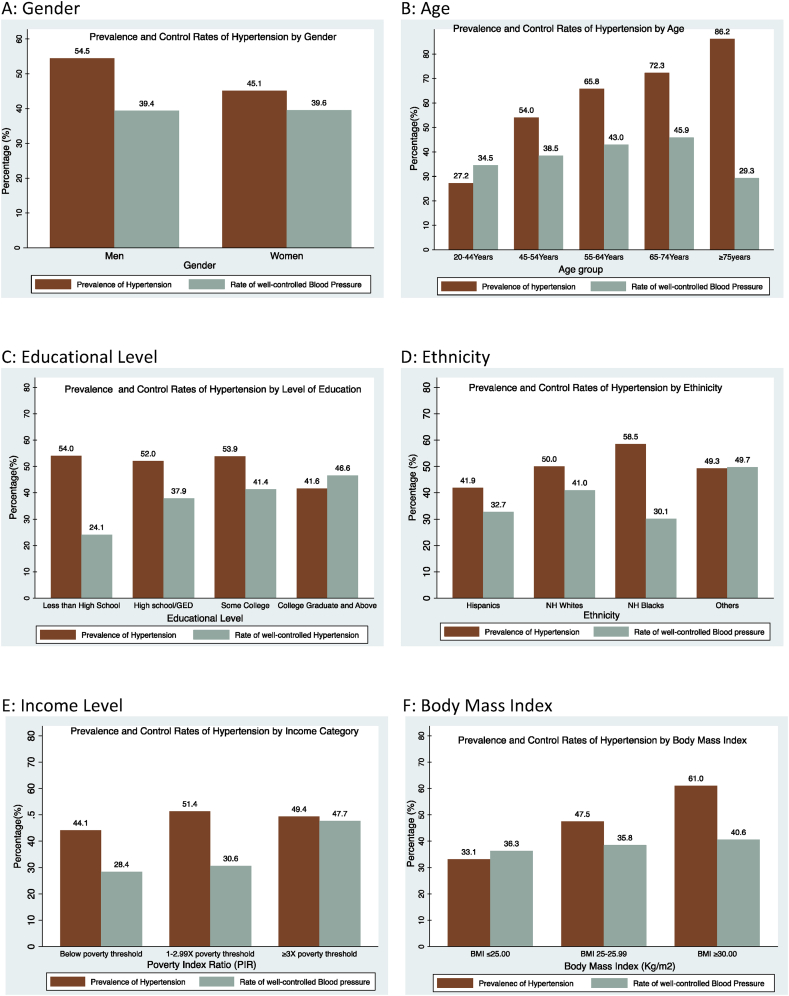
The national prevalence of hypertension in the USA population was 49.64% (95% CI 46.67–52.61) corresponding to 115 (95% CI 104–128) Million persons. In univariate models, the prevalence of hypertension was significantly higher in NH Blacks 58.53% (95% CI 55.39–61.60), obesed individuals 61.03% (95% CI 57.31–64.63), and older persons. Also, persons with CKD: 77.52% (95% CI 71.94–82.27), diabetes: 83.62% (95% CI 80.39–86.42) and without health insurance: 51.51% (95% CI 48.49–54.53) had significantly higher prevalence, comparatively. Men 54.46% (95% CI 51.01–57.87) were more likely to have hypertension than women 45.13% (95% CI 41.52–48.79). Persons with at least a college degree had lower prevalence of hypertension compared to other educational categories. There was no difference in the prevalence of hypertension across categories of country of birth and income status as shown on Table 1. In multivariable analysis, increasing age, male gender, obese individuals, diabetics and CKD were independent determinants of hypertension status as shown on Table 1. Also, Fig. 1 shows prevalence and control rates of hypertension across various categories of age, gender, ethnicity, educational level, income and body mass index (BMI).
Fig. 1.
Bar charts showing prevalence and control rates of hypertension in select groups.
3.3. Blood pressure control
Among known hypertensives on medications, 39.64% (95% CI 36.20–42.81) had well-controlled blood pressure. Proportions of persons with well-controlled BP was lower in NH Blacks 30.15% (95% CI 26.45–34.13) and Hispanics 32.70% (95% CI 24.47–42.16) compared to other races. In univariate models, the proportion of persons with well-controlled BP steadily increased with increasing level of education. Persons with incomes of at least three times the poverty threshold had highest rates of well-controlled BP 47.69% (95% CI 41.69–53.76) compared to others in lower income categories. Also, 40% of those with insurance had well-controlled BP compared to 22.2% of those without insurance, albeit not statistically significant. There were no differences in the percentage of persons with well-controlled blood pressure across all other categories as shown on Table 2. Using multivariable logistics regression, higher educational level and incomes ≥3times the PIR were independent predictors of well-controlled blood pressure.
Table 2.
Table showing the proportion of patients with well controlled blood pressure.
| Variable | Category | Well controlled blood pressure % (95% CI) |
p-valuea | Multivariate analysisb |
|
|---|---|---|---|---|---|
| OR (95% CI) | p-valueb | ||||
| All | 39.46 (36.20–42.81) | ||||
| Age (years) | 20–44 | 34.51 (26.15–43.95) | 0.110 | ||
| 45–54 | 38.46 (24.91–54.06) | ||||
| 55–64 | 42.96 (35.81–50.43) | ||||
| 65–74 | 45.91 (37.26–54.82) | ||||
| ≥75 | 29.27 (23.94–35.25) | ||||
| Gender | Male | 39.35 (34.34–44.59) | 0.952 | ||
| Female | 39.55 (35.10–44.18) | ||||
| Race | NH White | 32.70 (24.47–42.16) | 0.003 | 1 | – |
| Hispanic | 41.00 (35.98–46.20) | 0.96 (0.55–1.65) | 0.866 | ||
| NH Black | 30.15 (26.45–34.13) | 0.78 (0.50–1.23) | 0.269 | ||
| Others | 49.72 (43.24–56.21) | 1.42 (0.98–2.08) | 0.061 | ||
| Education | Less than high school | 24.08 (17.93–31.53) | 0.028 | 1 | – |
| High school or GED | 37.88 (32.52–43.56) | 1.96 (1.20–3.19) | 0.010 | ||
| Some college | 41.36 (34.35–48.73) | 1.95 (1.17–3.24) | 0.014 | ||
| College and above | 46.40 (36.42–57.07) | 2.20 (1.02–5.04) | 0.049 | ||
| Poverty (PIR) | <1 | 28.38 (22.14–35.58) | 0.002 | 1 | – |
| 1 to 3 | 30.63 (26.37–35.25) | 1.01 (0.71–1.44) | 0.955 | ||
| ≥3 | 47.69 (41.69–53.76) | 1.88 (1.1.8–2.99) | 0.011 | ||
| Place of birth | USA | 39.86 (35.90–43.96) | 0.589 | ||
| Non-USA | 37.21 (29.37–45.78) | ||||
| Smoking | Active smoker | 43.58 (29.06–59.29) | 0.517 | ||
| No active smoker | 38.90 (36.19–41.67) | ||||
| BMI | Normal | 36.31 (28.65–44.74) | 0.583 | ||
| Overweight | 38.52 (32.21–45.24) | ||||
| Obese | 40.59 (37.47–43.79) | ||||
| CKD | Yes | 37.72 (31.59–44.26) | 0.615 | ||
| No | 40.49 (34.13–47.20) | ||||
| Diabetes | Yes | 40.39 (33.96–47.17) | 0.780 | ||
| No | 39.01 (33.68–44.60) | ||||
| Insurance | Yes | 40.49 (36.92–44.16) | 0.063 | 1.84 (0.58–5.93) | 0.279 |
| No | 22.20 (10.65–40.59) | 1 | – | ||
Represents output from univariate analysis.
Represents output from multivariable logistic regression. Only variables with p-values less than 0.1 were retained for multivariate logistic regressions.
4. Discussion
Using nationally representative data, we report the prevalence of hypertension in the USA during the years 2017–2018 as 49.64%. Increasing age, male gender, obese individuals, diabetics and CKD were independent determinants of having hypertension. Only 39.64% of hypertensive patients on medications had well-controlled BP. Higher educational level and income ≥3times the poverty threshold were independent predictors of well controlled blood pressure. To the best of our knowledge, our study provides the latest nationally representative estimates on the burden and control rates of hypertension in the USA.
4.1. Prevalence of hypertension
Our prevalence and absolute burden is comparable to the 48.4% and the 45.4% reported by other authors [13,14] using the updated definition of hypertension [4]. However, this represents a significant jump from previous reports [15] which is largely attributed to the change in definition threshold as the persons who would have otherwise not be considered hypertensive are now classified as having hypertension [4]. The largely stable prevalence may suggest that preventive measures geared at reducing the burden of hypertension are insufficient. However, it would be premature, and maybe naive to think or conclude that preventive measures have had no meaningful impact as no one can tell for sure how explosive the prevalence might have been if these were absent.
Consistent with prior reports [5,15], increasing age, men, obesity, NH Blacks, persons with CKD and persons with diabetes were independent predictors of hypertension. Though these represent higher risk groups that could be preferentially screened for hypertension, the high prevalence of hypertension in the general population warrants that all person ≥20years old at every contact with the health system should be screened for early diagnosis and treatment. Though a common practice to relegate screening and management of hypertension to primary care providers, tasking every healthcare provider to participate in this process would certainly prove helpful. Given the strong association between obesity and hypertension and the rapidly increasing prevalence of obesity in the society [16], stalling or reversing the trend in the burden of hypertension might prove difficult unless obesity among other risk factors are succinctly tackled concomitantly. This certainly reinforces the urgent need for multimodal interventions in the fight against hypertension.
4.2. Blood pressure control
Consistent with prior reports [5], attaining blood pressure treatment goal remains a major challenge among patients with hypertension with only 39.64% of hypertensives on medications having a well-controlled BP. This rather stable proportion of patients with well-controlled BP is worrisome for several reasons. Dorans et al. [5] retrospectively analyzed data using the goal of <130/80 mmHg on patients who were treated at a time when the BP treatment goal was <140/90 mmHg. This therefore implies that providers and patients were evaluated on more stringent goals than were advised at the time and yet performed to similar levels even at 2years following the change in guidelines. With a change in the goal of treatment, we would have expected more aggressive management by both providers and patients resulting in higher proportions of well-controlled BP. The stable rates of BP control may suggest that the change in treatment goal might have largely remained theoretical and has not necessarily influenced long established treatment habits. Intense efforts would be warranted in this regard if patients must reap the benefits of well-controlled blood pressure, a major reason for the change in treatment target.
In univariate models, consistent with prior reports, NH Blacks and Hispanics continue to have greater proportion of poorly controlled blood pressure [5,15,17]. The combination of highest prevalence (prevalence of hypertension in NH Blacks is at least 10% points higher than that of any other race [15]) and lowest rates of well controlled BP largely explains the huge disproportionate burden of hypertension related complications in this population [1,18]. In multivariate models, poor blood pressure control was mainly explained by low income and poor educational status despite being on medications. This highlights the fact that medications acquisition alone may still prove insufficient in the control of blood pressure. Adhering to nondrug measures requires additional finances and It would not be surprising that poor and less educated individuals are more unlikely adhere to dietary and lifestyle modifications as well as prescribed medications compared to others.
4.3. Strengths and limitations
Blood pressure reading(s) used for defining hypertension were all measured on a single encounter as opposed to recommendations of at least two BP readings obtained on at least two different office visits which might have led to misclassification. Also, our definition of BP control is very conservative and might have overestimated control rates as only persons on medications were considered and thus should be interpreted along these lines. Furthermore, there still exists differing opinion on the optimal blood pressure control target with other associations such as American College of Physicians (ACP) and American Association of Family Physicians (AAFP) with significant followings dispensing primary care and thus managing a significant proportion of hypertensive patients still using a higher threshold of 140/90 mmHg. Finally, two years following the change in guidelines might not be sufficient time as old habits are often difficult to be changed and might require more than 2years before we start seeing meaningful change. However, using nationally representative data, we have been able to provide most up to date useful updates on the prevalence of hypertension and well-controlled blood pressure in the USA. We further highlight disproportionately affected groups as well as those posing serious challenges towards obtaining adequate BP control, which all serve as helpful hints to health practitioners.
5. Conclusions
One in every two individuals aged 20 years and more in the USA has hypertension with only 39.64% of hypertensive on medications attaining well-controlled BP. There exists significant discrepancies in the prevalence and rates of well-controlled BP in different population subgroups. Interventions targeting these subgroups could help drive down the prevalence of hypertension as well as increased the rates of well-controlled blood pressure.
Authorship contribution
Muchi Ditah Chobufo (MD MPH), Vijay Gayam: Conception, data collection and analysis.
Jean Soluny (MD), Joyce Bei Foryoung (MD), Valirie Agbor (MD), Ebad Rahman and Sostanie Enoru: Drafting and review of manuscript.
Tonga Nfor (MD, MSPH), Dufresne Alix (MD): Critical review for intellectual content.
Funding
None.
Declaration of Competing Interest
None.
References
- 1.Virani S.S., Alonso A., Benjamin E.J. Heart disease and stroke statistics—2020 update: a report from the American heart association. Circulation. 2020;141(9) doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.James P.A., Oparil S., Carter B.L. 2014 evidence-based guideline for the management of high blood pressure in adults. JAMA. 2014;311(5):507. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 3.SPRINT Research Group W., Wright J.T., Williamson J.D. A randomized trial of intensive versus standard blood-pressure control. N. Engl. J. Med. 2015;373(22):2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whelton P.K., Carey R.M., Aronow W.S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. Hypertension. 2017;71(6) doi: 10.1161/HYP.0000000000000065. HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 5.Dorans K.S., Mills K.T., Liu Y., He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American Heart Association (ACC/AHA) guideline. J Am Heart Assoc. 2018;7(11) doi: 10.1161/JAHA.118.008888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Center for Health Statistics N. 2011. National Health and Nutrition Examination Survey: Analytic Guidelines.https://wwwn.cdc.gov/nchs/data/nhanes/2011-2012/analytic_guidelines_11_12.pdf [cited 2017 Apr 17]; Available from: [Google Scholar]
- 7.Bureau U.C. How the census bureau measures poverty. https://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html [cited 2019 Jan 15];Available from:
- 8.NHANES 2017-2018 laboratory methods. https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/labmethods.aspx?BeginYear=2017 [cited 2020 Jul 18];Available from:
- 9.Levey A.S., Stevens L.A., Schmid C.H. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Evaluation D. Correction: national kidney foundation practice guidelines for chronic kidney disease. Ann. Intern. Med. 2003;139(7):605. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 11.NHANES questionnaires, datasets, and related documentation. https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2017 [cited 2020 Mar 7];Available from:
- 12.NHANES survey methods and analytic guidelines. https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx#analytic-guidelines [cited 2020 Mar 7];Available from:
- 13.Mills K.T., Bundy J.D., Kelly T.N. Global disparities of hypertension prevalence and control. Circulation. 2016;134(6):441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ostchega Y., Fryar C.D., Nwankwo T., Nguyen D.T. National Center for Health Statistics; Hyattsville, MD: 2020. Hypertension Prevalence Among Adults Aged 18 and over: United States, 2017–2018. NCHS Data Brief, No 364. [PubMed] [Google Scholar]
- 15.Fryar C.D., Ostchega Y., Hales C.M., Zhang G.K.-M.D. Natl Center for Health Statistics; Hyattsville, MD: 2017. Hypertension Prevalence and Control Among Adults: United States, 2015–2016. NCHS Data Brief, No 289. [PubMed] [Google Scholar]
- 16.Hales C.M., Carroll M.D., Fryar C.D., O C.L. Natl Cent Heal Stat; Hyattsville, MD: 2020. Prevalence of Obesity and Severe Obesity Among Adults: United States, 2017–2018. NCHS Data Brief, No 360. [PubMed] [Google Scholar]
- 17.Leng B., Jin Y., Li G., Chen L., Jin N. Socioeconomic status and hypertension. J. Hypertens. 2015;33(2):221–229. doi: 10.1097/HJH.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 18.Ditah C.M., Rahman E., Agbor V.N. Disparities and drivers of early age at diagnosis of congestive heart failure in the USA. Int. J. Cardiol. 2019;293:143–147. doi: 10.1016/j.ijcard.2019.06.001. [DOI] [PubMed] [Google Scholar]