Abstract
Background
The impact of the 2017 American College of Cardiology (ACC)/American Heart Association (AHA) guidelines for diagnosis and management of hypertension on the prevalence of hypertension in India is unknown.
Methods
We analyzed data from the Cardiac Prevent 2015 survey to estimate the change in the prevalence of hypertension. The JNC8 guidelines defined hypertension as a systolic blood pressure of ≥140 mmHg or diastolic blood pressure of ≥90 mmHg. The 2017 ACC/AHA guidelines define hypertension as a systolic blood pressure of ≥130 mmHg or diastolic blood pressure of ≥80 mmHg. We standardized the prevalence as per the 2011 census population of India. We also calculated the prevalence as per the World Health Organization (WHO) World Standard Population (2000–2025).
Results
Among 180,335 participants (33.2% women), the mean age was 40.6 ± 14.9 years (41.1 ± 15.0 and 39.7 ± 14.7 years in men and women, respectively). Among them, 8,898 (4.9%), 99,791 (55.3%), 35,694 (11.9%), 23,084 (12.8%), 9,989 (5.5%) and 2,878 (1.6%) participants belonged to age group 18–19, 20–44, 45–54, 55–64, 65–74 and ≥ 75 years respectively. The prevalence of hypertension according to the JNC8 and 2017 ACC/AHA guidelines was 29.7% and 63.8%, respectively- an increase of 115%. With the 2011 census population of India, this suggests that currently, 486 million Indian adults have hypertension according to the 2017 ACC/AHA guidelines, an addition of 260 million as compared to the JNC8 guidelines.
Conclusion
According to the 2017 ACC/AHA guidelines, 3 in every 5 Indian adults have hypertension.
Keywords: 2017 ACC/AHA blood Pressure guideline, Prevalence, Hypertension, India, Health policy
1. Introduction
In 2017, the American College of Cardiology (ACC)/American Heart Association (AHA) suggested new guidelines to define and manage hypertension [1]. The new guidelines define hypertension as either a systolic blood pressure (SBP) of ≥130 mmHg or a diastolic blood pressure (DBP) of ≥80 mmHg [1]. Previously, the report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC8) guidelines were used to define hypertension [2]. JNC8 defined hypertension as either an SBP of ≥140 mmHg or a DBP of ≥90 mmHg. The new guidelines also set a lower blood pressure target of ≤130/80 mmHg as opposed to ≤140/90 mmHg by JNC8 [2].
With the lowered cut-off, there is an expected increase in the prevalence of hypertension, as suggested by analysis of survey data from the US, China, and Nepal [[3], [4], [5]]. With the burden of cardiovascular diseases on the rise, it is important to study the impact of these guidelines on the prevalence of hypertension in India. [[6], [7], [8]]. This study aimed to assess the impact of the 2017 ACC/AHA hypertension guidelines on the prevalence of hypertension in India.
2. Materials and methods
The study was conducted following the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (Supplemental Table 1).
2.1. Study design and participants
We used data from the Cardiac Prevent 2015 survey. In this survey, data on BP, comorbidities, and risk factors were recorded among adults aged ≥18 years on a single day from 9 am to 5 pm as previously described [9]. Briefly, the survey was conducted in 24 states and union territories of India (constitute 62.7% of the national population). As part of the study protocol, the participant should not have taken tea or coffee in the last 10 min and should be seated for ≥3 min before the measurement of BP. Self-reported history of hypertension, intake of anti-hypertensive medications, diabetes mellitus, dyslipidemia, smoking, and smokeless tobacco was recorded.
2.2. Blood pressure measurement
BP was measured using automated oscillometer machines. Participants with the first BP measurement ≥140/90 mmHg underwent a re-measurement after 3 min. The blood pressure was rounded off to the nearest whole number. A printed report with BP measurements was given to the participant. Individual site coordinators were responsible for data collection which was fed real-time into an online portal. An independent auditor, not involved in data collection, reviewed and verified the data from each site.
2.3. Hypertension definition
The 2017 ACC/AHA guidelines defines four categories for classification: normal (SBP <120 and DBP <80 mmHg), Elevated (SBP 120–129 and DBP <80 mmHg), Stage 1 hypertension (SBP 130–139 or DBP 80-89 mmHg) and Stage 2 hypertension (SBP ≥140 or DBP ≥90 mmHg) [1]. The JNC8 guidelines define hypertension as either an SBP ≥140 mmHg or a DBP of ≥90 mmHg [2].
2.4. Statistical analysis
We calculated crude prevalence, prevalence adjusted for the 2011 census population of India [10], and the prevalence adjusted for the WHO standard population for the year 2000–2025 [11]. Distribution of hypertension across the 4 classifications was calculated across 6 mutually exclusive groups (18–19 years, 20–44 years. 45–54 years, 55–64 years, 65–74 years, and ≥75 years) to compare the impact with a previously published report from the US [4]. The prevalence was converted into absolute numbers taking census 2011 population of India as the reference. We evaluated the association of self-reported risk factors with hypertension in a multivariable logistic model with age, diabetes mellitus, dyslipidemia, current smoking, and smokeless tobacco using odds ratio with 95% confidence intervals. Continuous variables were represented as medians with interquartile ranges and categorical variables were represented as counts with proportions. The Wilcoxon rank-sum test and Chi-squared tests were used to identify the differences in baseline characteristics in continuous and categorical variables, respectively. All statistical analyses were conducted in Stata version 14.2 (StataCorp, College Station, TX, U.S.A.). We used de-identified data and the Institutional Review Board clearance was not required.
3. Results
We recorded BP of 180,335 participants (120,425 [66.8%] men and 59,910 [33.2%] women) with a mean age of 40.6 ± 14.9 years (41.1 ± 15 and 39.7 ± 14.7 years in men and women, respectively). Among them 8,898 (4.9%), 99,791 (55.3%), 35,694 (11.9%), 23,084 (12.8%), 9,989 (5.5%) and 2,878 (1.6%) participants belonged to age group 18–19, 20–44, 45–54, 55–64, 65–74 and ≥ 75 years respectively. Mean SBP and DBP were 125 ± 18 mmHg and 79 ± 11 mmHg respectively, which was higher among men than women across all age groups. There were 12.9% (95% confidence interval 12.7, 13.0) participants already on anti-hypertensive medications.
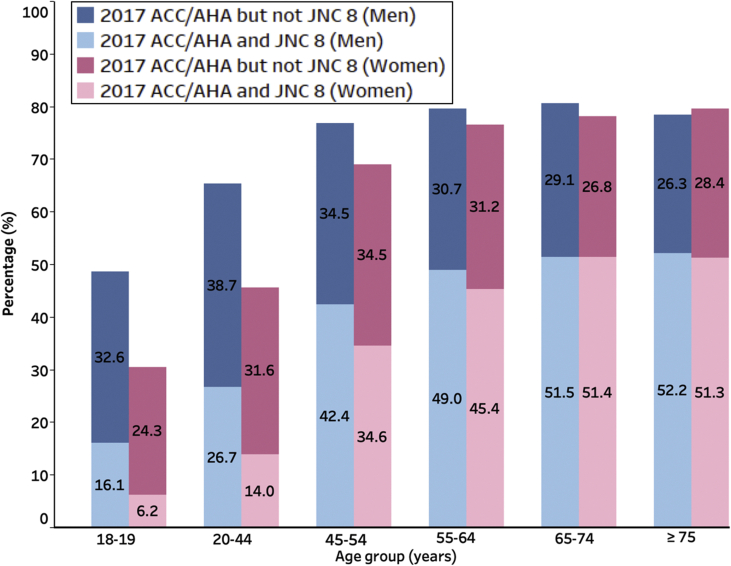
As per the JNC8 guidelines, there were 55,370 participants with hypertension, with an adjusted prevalence of 29.7%. According to the 2017 ACC/AHA guideline, there were 117,287 participants with hypertension, with an adjusted prevalence of 63.8%, a relative increase of 115% as compared to the JNC8 guideline. The adjusted prevalence among men and women was 68.7% and 55.1%, respectively. The impact of the new guidelines is given in Table 1 and Fig. 1. The highest impact of the 2017 ACC/AHA guidelines was observed in the age group of 18–19 years, with prevalence increasing around 3 times among men (16%–49%) and 5 times among women (6%–31%) (Table 1 and Fig. 1).
Table 1.
Relative increase in prevalence, age group, and gender-wise.
| Age (years) | Prevalence (JNC 8) (%) | Prevalence (2017 ACC/AHA) (%) | Difference (2017 ACC/AHA but not JNC8) | Relative increase (%) |
|---|---|---|---|---|
| Men | ||||
| 18-19 (n = 5,448) | 16.1 (15.1, 17.08) | 48.7 (47.4, 50) | 32.6 | 202.5 |
| 20-44 (n = 66,039) | 26.7 (26.4, 27) | 65.4 (65, 65.8) | 38.7 | 144.9 |
| 45-54 (n = 23,789) | 42.4 (41.8, 43) | 76.9 (76.4, 77.4) | 34.5 | 81.4 |
| 55-64 (n = 15,874) | 49 (48.2, 49.8) | 79.7 (79.1, 80.3) | 30.7 | 62.7 |
| 65-74 (n = 7,181) | 51.5 (50.3, 52.7) | 80.6 (79.7, 81.5) | 29.1 | 56.5 |
| ≥75 (n = 2,094) | 52.2 (50.1, 54.3) | 78.5 (76.7, 80.3) | 26.3 | 50.4 |
| Overall | 39.4 (39.1, 39.7) | 69.9 (69.9, 70.2) | 30.2 | 76.6 |
| Women | ||||
| 18-19 (n = 3450) | 6.2 (5.4, 7) | 30.5 (29, 32) | 24.3 | 391.9 |
| 20-44 (n = 33,753) | 14 (13.6, 14.4) | 45.6 (45.1, 46.1) | 31.6 | 225.7 |
| 45-54 (n = 11,905) | 34.6 (33.8, 35.5) | 69.1 (68.3, 69.9) | 34.5 | 99.7 |
| 55-64 (n = 7,210) | 45.4 (44.3, 46.6) | 76.6 (75.6, 77.6) | 31.2 | 68.7 |
| 65-74 (n = 2,808) | 51.4 (49.6, 53.3) | 78.2 (76.7, 79.7) | 26.8 | 52.1 |
| ≥75 (n = 784) | 51.3 (47.8, 54.8) | 79.7 (76.9, 82.5) | 28.4 | 55.4 |
| Overall | 29.3 (28.9, 29.7) | 48 (47.6, 48.4) | 18.7 | 63.8 |
ACC/AHA = American College of Cardiology/American Heart Association; JNC8 = 8th Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
Fig. 1.
Prevalence of hypertension according to the 2017 ACC/AHA and the JNC8 guidelines. ACC/AHA, American College of Cardiology/American Heart Association; JNC8, Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.
After standardization according to the national population, there were 226 million and 486 million adults with hypertension in India according to the JNC8 and the 2017 ACC/AHA guidelines, respectively- an increase of about 260 million. Total prevalence was 66.7% (AHA/ACC 2017) and 30.7% (JNC 8), standardized for WHO Standard Population (2000–2025).
Prevalence of hypertension among each age group was higher in men as compared to women, except in those >65 years, where almost equal prevalence was found. With the new cut-offs, only 28.6% of participants were found to have normal BP (22.6% and 40.8% of men and women, respectively) (Table 2).
Table 2.
Blood pressure categories according to 2017 ACC/AHA criteria among those not taking anti-hypertensive medications (n = 157,121).
| Normal (%) <120/<80 mmHg |
Elevated Blood Pressure (%) 120-129/<80 mmHg |
Stage 1 (%) 130-139/80–89 mmHg |
Stage 2 (%) ≥140/≥90 mmHg |
|
|---|---|---|---|---|
| Total | 28.6 (28.4, 28.8) | 9.4 (9.3, 9.5) | 35.4 (35.2, 35.6) | 26.6 (36.4, 26.8) |
| Men (n = 104,983) | 22.6 (22.4, 22.9) | 9.9 (9.7, 10.1) | 37.0 (36.7, 37.3) | 30.5 (30.2, 30.8) |
| Women (n = 52,138) | 40.8 (40.4, 41.2) | 8.3 (8.1, 8.5) | 32.0 (31.6, 32.4) | 18.8 (18.5, 19.1) |
| Age group (years) | ||||
| 18-19 (n = 8,851) | 45.0 (43.4, 46.0) | 13.5 (12.8, 14.2) | 29.4 (28.5, 30.4) | 12.1 (11.4, 12.8) |
| 20-44 (n = 95,204) | 32.6 (32.3, 32.9) | 9.9 (9.7, 10.1) | 36.6 (36.3, 36.9) | 21.0 (20.7, 21.3) |
| 45-54 (n = 28,916) | 20.8 (20.3, 21.3) | 7.7 (7.4, 8.0) | 36.0 (35.5, 36.6) | 35.5 (35.0, 36.1) |
| 55-64 (n = 16,127) | 16.7 (16.1, 17.3) | 8.0 (7.6, 8.4) | 32.7 (32.0, 33.4) | 42.6 (41.8, 43.4) |
| 65-74 (n = 6,239) | 15.2 (14.3, 16.1) | 8.4 (7.7, 9.1) | 30.9 (29.8, 32.1) | 45.5 (44.3, 46.7) |
| ≥75 (n = 17,84) | 17.2 (15.5, 19.0) | 8.6 (7.3, 9.9) | 29.3 (27.2, 31.4) | 44.8 (42.5, 47.1) |
There was a higher overall prevalence of self-reported diabetes mellitus, current smoking, and smokeless tobacco in men vs. women (all p < 0.001) (Table 3). Self-reported dyslipidemia was more common in women (8.2% vs. 7.0% for women and men, respectively, p < 0.001) (Table 3). There was a differential association of self-reported risk factors with the risk of hypertension across gender such that age, diabetes mellitus, and smoking were associated with a higher odd of hypertension among women vs. men (Table 3). The self-reported risk factors and association with hypertension across age categories in men and women are given in Supplement Table 2.
Table 3.
Prevalence and association of self-reported risk factors with hypertension as per 2017 ACC/AHA guidelines in men and women.
| Men (n = 120,425) | Odds Ratio (95% CI) | Women (n = 59,910) | Odds Ratio (95% CI) | |
|---|---|---|---|---|
| Age (years) | 39 (27, 50) | 1.03 (1.03, 1.03) | 40 (29, 52) | 1.05 (1.05, 1.05) |
| Diabetes Mellitus | 12,432 (10.3%) | 1.77 (1.67, 1.88) | 5,763 (9.6%) | 2.07 (1.91, 2.25) |
| Dyslipidemia | 8,370 (7.0%) | 2.17 (2.02, 2.34) | 4,923 (8.2%) | 1.78 (1.64, 1.94) |
| Current Smoking | 15,193 (12.6%) | 1.09 (1.04, 1.13) | 427 (0.7%) | 1.72 (1.36, 2.18) |
| Smokeless Tobacco | 12,396 (10.3%) | 0.97 (0.93, 1.01) | 1213 (2.0%) | 0.87 (0.77, 0.99) |
Data are presented as median (interquartile range) for age and n (%) for self-reported risk factors. Association of self-reported risk factors and hypertension (2017 ACC/AHA definition) in the multivariable model adjusted for age, diabetes mellitus, dyslipidemia, current smoking, and smokeless tobacco. CI, confidence interval.
4. Discussion
In this cross-sectional study to estimate the prevalence of hypertension among Indian adults, we found that the prevalence according to the JNC8 and 2017 ACC/AHA guidelines was 29.7% and 63.8%, respectively– a relative increase of 115%. Most patients above 65 years had stage 2 hypertension and the relative increase in hypertension prevalence decreased with advancing age.
Approximately 486 million Indian adults have hypertension according to the new guidelines, an increase of 260 million over 226 million already diagnosed as per the JNC8 guidelines. Our results are similar to a study done using another survey data from India where a relative increase of 140% was reported [12]. In a similar study done to assess the impact in the US adult population, an increase from 31.9% to 45.6% was reported [4]. Another study (age group 45–75 years), done using nationally representative data of the US and Chinese population reported a prevalence of 63% in the US population (a relative increase of 74%) and 55% (a relative increase of 45%) in the Chinese population according to the new guidelines [3]. In Nepal, there was a 92% relative increase in prevalence [5]. This data suggests that a heterogeneous impact of the new guidelines on the regional prevalence of hypertension with a higher impact in Asia as compared to North America. A large change is due to the reclassification of participants with prehypertension (SBP 120–139 mmHg) according to old guidelines into stage 1 hypertension according to the new guidelines [13].
The new guidelines recommend treatment in stage 2 hypertension, as well in high-risk groups with SBP of 130–139 mmHg or a DBP 80–89 mmHg. The high-risk features include age ≥65 years, previous atherosclerotic cardiovascular disease (ASCVD) event, the 10-year risk of ASCVD risk score ≥10%, diabetes mellitus, or chronic kidney disease [1]. We did not have laboratory values to compute the ASCVD risk score or confirm diabetes mellitus. Therefore, we cannot estimate how many participants with hypertension as per the new definition would require treatment.
Data from the US suggests that around 80% of patients who qualify as having hypertension according to the new guideline would require treatment [4]. If we apply these numbers to the current Indian population, this would imply that around 390 million out of 486 million patients with hypertension would require treatment. Given the already poor awareness, treatment, and control of blood pressure among patients with high blood pressure, this would require a restructuring of public health policy to meet the unmet needs.
Currently, Indian guidelines do not endorse the 2017 ACC/AHA guidelines for the classification and treatment of hypertension. Few studies have reported the impact of new guidelines on the epidemiology transition in the management of BP [3,4]. India is expected to become the country with the largest population by 2024 [14]. India has a single national-level program on the prevention and control of cancer, diabetes, stroke, and cardiovascular diseases [15]. The Indian guidelines endorse capacity building and integration of non-communicable disease management at the primary health care level. Program data for the year 2016–17 suggests that only 22 million patients attended these clinics and out-reach services screened only 16 million participants [15]. This is a dismally small number compared to the 486 million that require screening and monitoring.
Poor availability of infrastructure and competing agendas like tuberculosis have marred India's potential to control the epidemic of cardiovascular diseases [16]. As the average blood pressure continues to rise in India, there is an expected large increase in cardiovascular diseases [17,18]. Due to the huge economic costs of treatment, non-pharmacological intervention in the form of reduced salt intake, regular exercise, and weight reduction needs to be emphasized for primary prevention [19].
We found that there is a significant association of hypertension with diabetes mellitus, dyslipidemia, and current smoking, both among men and women. Smokeless tobacco leads to a higher circulating level of nicotine, sympathetic neural stimulation, and increased systolic and diastolic blood pressure [20]. The association of chronic smokeless tobacco with hypertension is complex, multifactorial, and depends on the participant's age [21]. Smokeless tobacco has proven cardiovascular and non-cardiovascular adverse effects [22]. Lifestyle changes, such as cessation of all forms of tobacco intake, sodium restriction, decreased intake of total and saturated fats with weight reduction should be strongly advocated and emphasized as essential adjuncts to effective pharmacological management of hypertension [1].
To the best of our knowledge, this is the single largest cross-sectional study to estimate the impact of the 2017 ACC/AHA guidelines on the prevalence of hypertension among Indian adults. But there are important limitations to our study. The results are based on a cross-sectional survey and the limitations inherent to survey-based epidemiological studies apply. Most of the participants in the survey had a single BP measurement. Further, our protocol allowed BP measurement after only 10 minutes of coffee or tea consumption but the effect of these stimulants may last up to 3 hours [23]. This may cause an overestimation of hypertension prevalence, but the effect is likely to be small given the large sample size. There was no pre-specified sampling technique and the sample was not nationally representative. However, we standardized the results of our survey. Our prevalence estimate according to the JNC8 is similar to that reported in a meta-analysis of 142 studies on hypertension prevalence in India (29.8% in the meta-analysis vs. 29.7% in our study) [24]. This suggests the accuracy of our methodology. We did not have data to analyze urban-rural differences. Further, self-reported diabetes mellitus and dyslipidemia were used in the multivariable model with no laboratory confirmation.
The benefits of aggressive blood pressure reduction remain unknown for the Indian population. The European Society of Cardiology/European Society of Hypertension guidelines and the International Society of Hypertension guidelines continue to use the ≥140/90 mmHg cutoff to define and treat hypertension [25,26]. Longitudinal studies, such as the Framingham Cohort Study, are required to understand the benefits-risks of aggressive BP control for the Indian population.
5. Conclusion
With the 2017 ACC/AHA guidelines, the prevalence of hypertension in India increases from 29.7% to 63.8%- a relative increase of 115%. Longitudinal cohort studies are required to investigate the unique risk factors in the Indian population and their association with risk of major adverse cardiovascular events.
Credit author statement
Conceptualization: KG, SR.
Methodology: KG, SR.
Software: KG, KM.
Validation: KG, KM.
Formal analysis: KG, KM, TSK, SR.
Investigation: KG, SR, RS, DJ, NB, RG, SB, RKN, ST, GSW, SG, SM, NBS, GS, DR, SD, KG, SNR, SSM, BPS, BBB, MKD, PKD PD, AS.
Resources: SR, KM, GZ, SR, PPM, KV, SS, RS, DJ, NB, RG, SB, RKN, ST, GSW, SG, SM, NBS, GS, DR, SD, KG, SNR, SSM, BPS, BBB, MKD, PKD PD, AS.
Data Curation: KG, KM, PG.
Writing - Original Draft: KG, TSK, PG, SR.
Writing - Review & Editing: KG, RG, PD, SR.
Visualization: KG, SR, KM.
Supervision: SR.
Project administration: SR.
Funding acquisition: SR.
Declaration of competing interest
None of the authors have any conflict of interest to declare with this manuscript.
Acknowledgments
The investigators would like to thank Omron Healthcare India Pvt. Ltd. for providing blood pressure apparatus, Torrent Pharmaceuticals Ltd., USV Pvt. Ltd. and Zydus Pharmaceuticals Ltd. for partial financial support. RP Singh of Zydus Pharmaceuticals Ltd. provided logistic support.
Footnotes
All authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijchy.2020.100055.
Contributor Information
Sivasubramanian Ramakrishnan, Email: drramaaiims@gmail.com.
CSI-Great India BP Campaign Investigators:
J. Shivkumar Rao, B.P. Singh, B.B. Bharti, A.K. Sinha, Kartik Gupta, Sivasubramanian Ramakrishnan, Sudha Bhushan, Sunil K. Verma, Balram Bhargava, Ambuj Roy, Sandeep Bansal, Sanjay Sood, H.S. Isser, Neeraj Pandit, Ranjit K. Nath, Sanjay Tyagi, Vijay Trehan, Mohit D. Gupta, M.P. Girish, Ramandeep Ahuja, S.C. Manchanda, Arun Mohanty, Peeyush Jain, Sameer Shrivastava, I.P.S. Kalra, B.S. Sarang, H.S. Ratti, G. Bala Sahib, Rakesh Gupta, S K Agarwal Amit, K.C. Goswami, V.K. Bahl, H.K. Chopra, Ashok Seth, Geevar Zachariah, P.P. Mohanan, K. Venugopal, George Koshy, Tiny Nair, N. Shyam, Anil Roby, Raju George, Sudhaya Kumar, Abdul Kader, Mathew Abraham, Sunitha Viswanathan, A. Jabir, Jaideep Menon, Govindan Unni, Cibu Mathew, P.B. Jayagopal, Sajeev, P.K. Ashokan, Asharaf, Subroto Mandal, A.K. Pancholia, Neil Bardolei, A.K. Gupta, Neil Bardolei, Rupam Das, Dinesh Aggarwal, Amit Malviya, S.N. Routray, S.S. Mishra, Syed Manzor Ali, Parag Barward, Navreet Singh, Yashbir S. Tomar, Davinder Chaddha, Sameer Dani, Chirayu Vyas, Kinjal Bhatt, Shrenik Doshi, G.S. Wander, Satish Gupta, Chandra Bhan Meena, Santosh Sateesh, Nagendra Boopathy Senguttuvan, Geetha Subramanyam, Subramanyam, Ajit Mullasari Muruganandam, Rishi Sethi, Varun Narain, R.K. Saran, Dharmendra Jain, Praveen Jain, Sudeep Kumar, P.K. Goel, Debabatra Roy, Sibananda Datta, Kajal Ganguly, M.K. Das, Soumitra Kumar, Sarat Chandra, Amal Banerjee, Santanu Guha, and P.K. Deb
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Whelton P.K., Carey R.M., Aronow W.S., Casey D.E., Jr., Collins K.J., Dennison Himmelfarb C. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 2018;71(19):e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 2.James P.A., Oparil S., Carter B.L., Cushman W.C., Dennison-Himmelfarb C., Handler J. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) J. Am. Med. Assoc. 2014;311(5):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 3.Khera R., Lu Y., Lu J., Saxena A., Nasir K., Jiang L. Impact of 2017 ACC/AHA guidelines on prevalence of hypertension and eligibility for antihypertensive treatment in United States and China: nationally representative cross sectional study. BMJ. 2018;362:k2357. doi: 10.1136/bmj.k2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muntner P., Carey R.M., Gidding S., Jones D.W., Taler S.J., Wright J.T., Jr. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137(2):109–118. doi: 10.1161/CIRCULATIONAHA.117.032582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kibria G.M.A., Swasey K., Kc A., Mirbolouk M., Sakib M.N., Sharmeen A. Estimated change in prevalence of hypertension in Nepal following application of the 2017 ACC/AHA guideline. JAMA Netw. Open. 2018;1(3) doi: 10.1001/jamanetworkopen.2018.0606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prabhakaran D., Jeemon P., Roy A. Cardiovascular diseases in India: current epidemiology and future directions. Circulation. 2016;133(16):1605–1620. doi: 10.1161/CIRCULATIONAHA.114.008729. [DOI] [PubMed] [Google Scholar]
- 7.Gupta R., Gaur K., Ram C.V.S. Emerging trends in hypertension epidemiology in India. J. Hum. Hypertens. 2019;33:575–587. doi: 10.1038/s41371-018-0117-3. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed S.T., Rehman H., Akeroyd J.M., Alam M., Shah T., Kalra A. Premature coronary Heart disease in South Asians: burden and determinants. Curr. Atherosclerosis Rep. 2018;20(1):6. doi: 10.1007/s11883-018-0706-1. [DOI] [PubMed] [Google Scholar]
- 9.Ramakrishnan S., Zachariah G., Gupta K., Shivkumar Rao J., Mohanan P.P., Venugopal K. Prevalence of hypertension among Indian adults: results from the great India blood pressure survey. Indian Heart J. 2019;71(4):309–313. doi: 10.1016/j.ihj.2019.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaduganathan M., Pareek M., Qamar A., Pandey A., Olsen M.H., Bhatt D.L. Baseline blood pressure, the 2017 ACC/AHA high blood pressure guidelines, and long-term cardiovascular risk in SPRINT. Am. J. Med. 2018;131(8):956–960. doi: 10.1016/j.amjmed.2017.12.049. [DOI] [PubMed] [Google Scholar]
- 11.Ahmad O.B., Boschi Pinto C., Lopez A D., Jl Murray C., Lozano R., Inoue M. 2001. Age Standardization of Rates: A New WHO Standard. [Google Scholar]
- 12.Venkateshmurthy N.S., Geldsetzer P., Jaacks L.M., Prabhakaran D. Implications of the new American College of Cardiology guidelines for hypertension prevalence in India. JAMA Intern. Med. 2018;178(10):1416–1418. doi: 10.1001/jamainternmed.2018.3511. Implications of the new American College of Cardiology guidelines for hypertension prevalence in India Letters. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wander Gurpreet S., Ram C.V.S. Global impact of 2017 American Heart association/American College of Cardiology hypertension guidelines. Circulation. 2018;137(6):549–550. doi: 10.1161/CIRCULATIONAHA.117.032877. [DOI] [PubMed] [Google Scholar]
- 14.Lekoubou A., Bishu K.G., Ovbiagele B. Nationwide impact of the 2017 American College of Cardiology/American Heart association blood pressure guidelines on stroke survivors. J. Am. Heart Assoc. 2018;7(12) doi: 10.1161/JAHA.118.008548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vischer A.S., Mayr M., Socrates T., Winterhalder C., Leonardi L., Eckstein J. Impact of single-occasion American vs. Canadian office blood pressure measurement recommendations on blood pressure classification. Am. J. Hypertens. 2019;32(2):143–145. doi: 10.1093/ajh/hpy159. [DOI] [PubMed] [Google Scholar]
- 16.Prabhakaran D., Jaacks L.M. Reflections from India on scaling up risk factor control for cardiovascular diseases to reach 1 billion adults. Circulation. 2019;139(1):4–6. doi: 10.1161/CIRCULATIONAHA.118.035975. [DOI] [PubMed] [Google Scholar]
- 17.Danaei G., Finucane M.M., Lu Y., Singh G.M., Cowan M.J., Paciorek C.J. National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet. 2011;378(9785):31–40. doi: 10.1016/S0140-6736(11)60679-X. [DOI] [PubMed] [Google Scholar]
- 18.Roy A., Praveen P.A., Amarchand R., Ramakrishnan L., Gupta R., Kondal D. Changes in hypertension prevalence, awareness, treatment and control rates over 20 years in National Capital Region of India: results from a repeat cross-sectional study. BMJ Open. 2017;7(7) doi: 10.1136/bmjopen-2016-015639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gupta R., Guptha S. Strategies for initial management of hypertension. Indian J. Med. Res. 2010;132(5):531–542. [PMC free article] [PubMed] [Google Scholar]
- 20.Westman E.C. Does smokeless tobacco cause hypertension? South. Med. J. 1995;88(7):716–720. doi: 10.1097/00007611-199507000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Gupta R., Gurm H., Bartholomew J.R. Smokeless tobacco and cardiovascular risk. Arch. Intern. Med. 2004;164(17):1845–1849. doi: 10.1001/archinte.164.17.1845. [DOI] [PubMed] [Google Scholar]
- 22.Bolinder G.M., Ahlborg B.O., Lindell J.H. Use of smokeless tobacco: blood pressure elevation and other health hazards found in a large-scale population survey. J. Intern. Med. 1992;232(4):327–334. doi: 10.1111/j.1365-2796.1992.tb00593.x. [DOI] [PubMed] [Google Scholar]
- 23.Mesas A.E., Leon-Muñoz L.M., Rodriguez-Artalejo F., Lopez-Garcia E. The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis. Am. J. Clin. Nutr. 2011;94(4):1113–1126. doi: 10.3945/ajcn.111.016667. [DOI] [PubMed] [Google Scholar]
- 24.Anchala R., Kannuri N.K., Pant H., Khan H., Franco O.H., Di Angelantonio E. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J. Hypertens. 2014;32(6):1170–1177. doi: 10.1097/HJH.0000000000000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Williams B., Mancia G., Spiering W., Agabiti Rosei E., Azizi M., Burnier M. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH) Eur. Heart J. 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 26.Unger T., Borghi C., Charchar F., Khan Nadia A., Poulter Neil R., Prabhakaran D. 2020 international society of hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–1357. doi: 10.1161/HYPERTENSIONAHA.120.15026. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.