Abstract
Background
Hypertension, diabetes, dyslipidemia and smoking are established coronary risk factors for coronary heart disease in the general population. However, in Japanese patients with acute myocardial infarction (AMI), the impact of the number of coronary risk factors on in-hospital morality remains unclear.
Methods
The Japan Acute Myocardial Infarction Registry (JAMIR) is a nationwide real-world database. We examined the association between the number of coronary risk factors and in-hospital mortality.
Results
Data were obtained from total of 20462 AMI patients (mean age, 68.8 ± 13.3 years old; 15281 men, 5181 women). The prevalence of hypertension increased with advancing age, while the prevalence of smoking decreased with advancing age. The prevalence of diabetes and dyslipidemia were highest in middle age. A majority (76.9%) of the patients with AMI had at least 1 of these coronary risk factors. Overall, the number of coronary risk factor was relatively less in older subjects and women under 50 years old. Crude in-hospital mortality rates were 10.7%, 10.5%, 7.2%, 5.0% and 4.5% with 0, 1, 2, 3 and 4 risk factors, respectively. After adjusting for age and sex, there was an inverse association between the number of coronary risk factors and the in-hospital mortality (adjusted odds ratio [1.68; 95% confidence interval, 1.20–2.35] among individuals with 0 vs. 4 risk factors).
Conclusion
In the present study of Japanese patients with AMI, who received modern medical treatment, in-hospital mortality was inversely related to the number of coronary risk factors. To investigate the underlying reasons for these findings, further studies are needed.
Keywords: Coronary risk factors, Acute myocardial infarction, In-hospital mortality
1. Introduction
Hypertension, diabetes, dyslipidemia and smoking are well-established coronary risk factors that should be controlled according to many guidelines for the primary and secondary prevention of cardiovascular disease [[1], [2], [3], [4]]. Historically, establishing these coronary risk factors took very long time [5]. For example, in the mid-20th century, many believed that a permissible systolic blood pressure was 100 plus the patient's age in millimeters of mercury [5]. The Framingham studies made tremendous progress in this field [5].
In Japan, the above-mentioned coronary risk factors were found to be similarly important for the incidence of coronary artery disease, as shown in the Hisayama studies [6,7]. These epidemiologic studies recommend risk stratification using the Framingham score or similar [7,8]. In these risk stratification methods, the more coronary risk factors that are present, the greater the likelihood of having coronary artery disease [7,8]. Therefore, the number of coronary risk factors influences the prediction and prevention of the incidence of coronary artery disease in the general population [7,8]. However, how the number of coronary risk factors affects in-hospital mortality of patients who have developed acute myocardial infarction (AMI) remains unclear.
In the present study, we assessed the impact of the number of coronary risk factors on the in-hospital mortality using the Japan Acute Myocardial Infarction Registry (JAMIR).
2. Methods
The JAMIR consists of 10 representative regional AMI registry groups or institutions in Japan [9,10]. A total of 20,596 consecutive patients with spontaneous AMI, defined as type 1 by the Joint European Society of Cardiology/American Heart Association/World Heart Federation, were included between 2011 and 2013 in a retrospective manner [11]. When the troponin level was not available, the WHO Monitoring of Trends and Determinants in CardioVascular Disease (MONICA) criteria were applied [12]. Procedure-related MI (type 1) and patients hospitalized within 24 h after the onset were excluded from the JAMIR.
Coronary risk factors included hypertension, diabetes (fasting plasma glucose level of ≥126 mg/dl, casual glucose level of ≥200 mg/dl, 2-h level of ≥200 mg/dl, hemoglobinA1c ≥ 6.5%, or use of medications for diabetes), dyslipidemia (low-density lipoprotein cholesterol level ≥140 mg/dl, high-density cholesterol level ≤40 mg/dl, triglyceride level ≥150, or use of lipid-lowering medications), and current smoking (smoking within the preceding year). The assessment of coronary risk factors refers to both before and/or during admission. Hypertension was defined if the resting blood pressure is persistently at or above 140/90 mmHg. Patients under antihypertensive treatment were also included. The treatment strategy, including medication and reperfusion therapy, was left up to the individual cardiologist at the local institution. The study was approved by the local institutional review board.
Continuous variables were expressed as the mean ± standard deviation or median value (25th-75th percentile) as appropriate. The normality of data was tested with the Shapiro-Wilk test. Categorical variables were expressed as percentages. Comparisons of continuous variables with normal distribution were tested by an analysis of variance. Comparisons of continuous variables with a non-normal distribution were tested by Wilcoxon's test. Categorical variables were analyzed by the chi-square test as appropriate. Multivariable logistic regression was performed to assess the association of the number of coronary risk factors. Age and sex were entered into this model. The JMP software program, ver. 14 (SAS institute, Cary, NC, USA), was used for the statistical analyses. P-values of <0.05 were considered statistically significant.
3. Results
3.1. Baseline characteristics
A total of 20,462 patients (15,281 men and 5181 women) were included after excluding 134 patients <20 years old. Table 1 shows the baseline characteristics of the study patients, which were stratified by the number of coronary risk factors. The average age was oldest (71 ± 14 years old) in patients with 1 coronary risk factor and youngest (62 ± 12 years old) in those with 4 coronary risk factors. Similarly, the male proportion was smallest in the patients with one coronary risk factor but largest in those with four coronary risk factors.
Table 1.
Baseline characteristics by the number of coronary risk factors.
| Number of coronary risk factors | Overall | 0 | 1 | 2 | 3 | 4 | P-value |
|---|---|---|---|---|---|---|---|
| Number (n) | 20462 | 4734 | 5139 | 6037 | 3656 | 896 | |
| Age (years) | 69 ± 13 | 69 ± 13 | 71 ± 14 | 69 ± 13 | 66 ± 12 | 62 ± 12 | <0.0001 |
| Male (%) | 74.7% | 73.5% | 70.8% | 73.6% | 79.6% | 90.5% | <0.0001 |
| Coronary risk factors | |||||||
| Hypertension (%) | 63.6% | 0.0% | 50.5% | 77.0% | 92.0% | 100.0% | <0.0001 |
| Diabetes (%) | 32.8% | 0.0% | 12.8% | 32.1% | 66.7% | 100.0% | <0.0001 |
| Dyslipidemia (%) | 46.2% | 0.0% | 17.1% | 56.5% | 86.0% | 100.0% | <0.0001 |
| Smoking (%) | 34.5% | 0.0% | 21.1% | 35.8% | 56.5% | 100.0% | <0.0001 |
| Killip | <0.0001 | ||||||
| 1 (%) | 71.8% | 73.1% | 68.0% | 73.1% | 73.4% | 70.8% | |
| 2 (%) | 11.8% | 9.7% | 13.6% | 12.3% | 11.6% | 11.9% | |
| 3 (%) | 6.3% | 4.9% | 7.1% | 6.3% | 6.9% | 7.8% | |
| 4 (%) | 10.1% | 12.2% | 11.4% | 8.3% | 8.2% | 9.5% | |
| STEMI (%) | 79.7% | 84.3% | 79.8% | 78.1% | 76.6% | 76.9% | <0.0001 |
| E-CAG (%) | 89.6% | 87.6% | 88.3% | 90.8% | 90.6% | 91.9% | <0.0001 |
| Ant-MI (%) | 47.6% | 49.3% | 49.1% | 46.4% | 45.9% | 45.5% | 0.0018 |
| LMT-culprit (%) | 3.0% | 5.1% | 3.5% | 2.5% | 2.2% | 2.9% | <0.0001 |
| Multi vessel disease (%) | 58.9% | 42.1% | 45.2% | 47.9% | 53.7% | 58.9% | <0.0001 |
| Primary PCI (%) | 87.9% | 86.5% | 85.7% | 88.8% | 89.8% | 93.1% | <0.0001 |
| Door-to-balloon time (min) | 80 (52–142) | 82 (60–124) | 81 (50–167) | 83 (50–160) | 80 (49–161) | 93 (55–185) | 0.02 |
| Onset-to-balloon time (min) | 230 (141–420) | 245 (161–464) | 236 (145–494) | 245 (145–555) | 260 (148–577) | 260 (161–595) | 0.48 |
| Final TIMI flow | <0.0001 | ||||||
| 0 (%) | 2.1% | 3.0% | 2.1% | 1.4% | 1.9% | 1.3% | |
| 1 (%) | 1.1% | 1.4% | 1.3% | 0.9% | 1.1% | 1.1% | |
| 2 (%) | 5.2% | 6.7% | 5.3% | 4.4% | 4.7% | 5.2% | |
| 3 (%) | 91.6% | 89.0% | 91.3% | 93.4% | 92.4% | 94.0% | |
STEMI, ST-elevation myocardial infarction; E-CAG, emergent coronary angiography; Ant-MI, anterior myocardial infarction; LMT, left main trunk; PCI, percutaneous coronary intervention.
The prevalence and number of each coronary risk factors per age by decade and sex are shown in Table 2. The prevalence of hypertension increased as the patients aged, while the prevalence of smoking decreased. The prevalence of diabetes was greatest among subjects in their 60s for both men and women. The prevalence of dyslipidemia was greatest among subjects in their 40s for men and in their 50s for women. Regarding the number of coronary risk factors, women under 50 years old showed distinctly different features from the rest because a substantial number of these patients had no coronary risk factors. Subjects in their 40s had the most coronary risk factors in men (1.8 ± 1.2), while those in their 50s had most coronary risk factors in women (1.6 ± 1.2).
Table 2.
The prevalence and number of each coronary risk factors per age by decade and sex.
| Age (years) |
Under 40 |
40–49 |
50–59 |
60–69 |
70–79 |
80–89 |
Over 90 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female |
| Number (n) | 316 | 25 | 1402 | 129 | 2756 | 307 | 4303 | 866 | 3961 | 1560 | 2265 | 1809 | 278 | 485 |
| Hypertension (%) | 41.4 | 22.2 | 53.8 | 50.5 | 56.6 | 46.9 | 60.1 | 63.1 | 67.5 | 70.1 | 67.6 | 73.3 | 69.1 | 73.2 |
| Dyslipidemia (%) | 56.4 | 38.9 | 58.9 | 34.3 | 56.4 | 55.8 | 49 | 51.8 | 42 | 49.4 | 33.5 | 40.5 | 21.4 | 26.7 |
| Diabetes (%) | 18.9 | 11.1 | 30.4 | 24.1 | 31.7 | 28.9 | 35.5 | 38.4 | 35.4 | 36.6 | 30.9 | 28.6 | 20.2 | 25.6 |
| Smoking (%) | 66.3 | 22.2 | 61.7 | 33.9 | 56.9 | 34.9 | 46.3 | 21.8 | 30.6 | 10.1 | 23.6 | 5.4 | 18.1 | 2.4 |
| Number of coronary risk factors | ||||||||||||||
| 0 (%) | 20.3 | 68.0 | 19.1 | 40.3 | 21.3 | 23.8 | 22.8 | 22.9 | 23.6 | 23.5 | 24.8 | 23.3 | 30.6 | 25.6 |
| 1 (%) | 29.1 | 12.0 | 20.5 | 20.2 | 19.7 | 25.4 | 21.4 | 24.1 | 25.2 | 25.7 | 30.7 | 32.4 | 37.1 | 41.2 |
| 2 (%) | 25.9 | 4.0 | 30.2 | 20.2 | 28.8 | 25.4 | 29.1 | 31.5 | 30.0 | 32.0 | 28.6 | 32.7 | 20.9 | 25.6 |
| 3 (%) | 18.4 | 16.0 | 22.0 | 17.8 | 22.9 | 19.2 | 20.6 | 18.5 | 17.5 | 17.3 | 13.4 | 10.7 | 10.4 | 7.6 |
| 4 (%) | 6.3 | 0.0 | 8.3 | 1.6 | 7.3 | 6.2 | 6.1 | 3.0 | 3.8 | 1.5 | 2.6 | 0.8 | 1.1 | 0.0 |
| Average number of coronary risk factors (mean ± SD) | 1.6 ± 1.2 | 0.7 ± 1.1 | 1.8 ± 1.2 | 1.2 ± 1.2 | 1.8 ± 1.2 | 1.6 ± 1.2 | 1.7 ± 1.2 | 1.5 ± 1.1 | 1.5 ± 1.1 | 1.5 ± 1.1 | 1.4 ± 1.1 | 1.3 ± 1.0 | 1.1 ± 1.0 | 1.2 ± 0.9 |
SD, standard deviation.
Patients without coronary risk factors had a greater prevalence of Killip 4, ST-elevation MI (STEMI), left main trunk (LMT) culprit, anterior MI and final thrombolysis in MI (TIMI) 0 flow than those with risk factors. Patients with four coronary risk factors had the greatest prevalence of emergent coronary angiography (E-CAG), multi-vessel disease and primary percutaneous coronary intervention (PCI) and the longest door-to-balloon time.
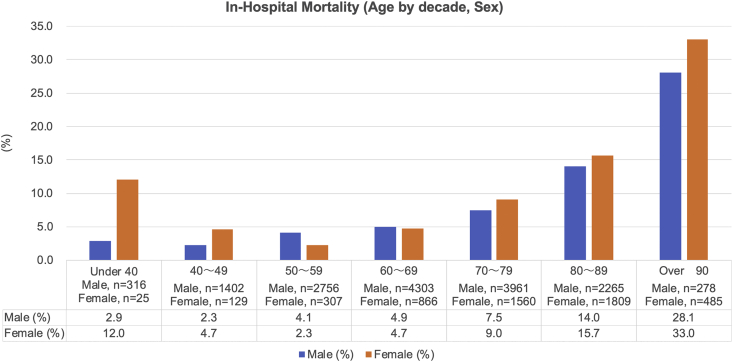
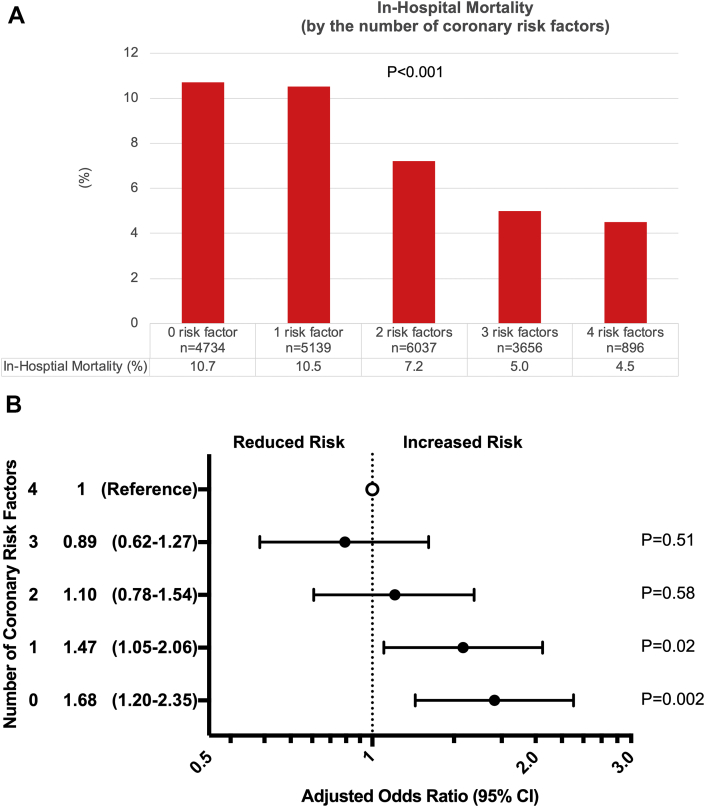
Fig. 1 shows the in-hospital mortality of AMI for men and women per decade. The in-hospital mortality was the lowest among subjects in their 40s for men and those in their 50s for women. Surprisingly, the in-hospital mortality of women under 40 years old was as high as 12%, which resulted in a J-curve phenomenon for the in-hospital mortality of AMI in women. Fig. 2A shows the in-hospital mortality by the number of coronary risk factors, with the in-hospital mortality being the greatest in patients without any risk factors followed by 1, 2, 3 and 4 risk factors (10.7%, 10.5%, 7.2%, 5.0% and 4.4%, respectively). In order to adjust for the age and sex, a multivariable model was used to assess the in-hospital mortality (Fig. 2B, reference = patients with 4 coronary risk factors). Patients with 0 or 1 coronary risk factors showed a significant risk for in-hospital mortality compared with patients with 4 coronary risk factors.
Fig. 1.
In-hospital morality was shown according to age by decade and sex.
Fig. 2.
A. The crude in-hospital mortality by the number of coronary risk factors. B. The adjusted in-hospital mortality risk by the number of coronary risk factors.
4. Discussion
In this Japanese nation-wide study, the relationship between the number of coronary risk factors and in-hospital morality of AMI in community practice was examined. A high prevalence of risk factor exposure with AMI was confirmed in Japanese patients. The number of coronary risk factors was the greatest in middle-aged subjects (those in their 40s for men and 50s for women), while the in-hospital mortality of AMI was the lowest in the subjects. The in-hospital mortality of AMI was thus inversely related to the number of coronary risk factors in Japanese patients who received modern medical treatment.
The number of coronary risk factors have previously been reported to be associated with incidence of coronary artery disease in the general population [[5], [6], [7], [8]]. We are not challenging this common sense, however, in this study, we only assessed the impact of the number of coronary risk factors on in-hospital mortality in an AMI population not in the general population. Thus, multiple coronary risk factors seem to influence in-hospital mortality differently between the AMI population and the general population. A similar study has been carried out by Canto et al. in 542,008 patients with their first MI and no history of cardiovascular disease [13]. In that study, the in-hospital mortality was investigated according to the number of coronary risk factors, including hypertension, diabetes, dyslipidemia, smoking and a family history [13]. The crude in-hospital mortality was 14.9%, 10.9%, 7.9%, 5.3%, 4.2% and 3.6% for patients with 0, 1, 2, 3, 4 and 5 coronary risk factors, respectively, which was consistent with the findings of our study, although the subjects differed in race [13]. Another point which needs to be mentioned is the fact that the proportion of patients with cardiogenic shock (Killip 4) was found to be greater as the number of coronary risk factors decreased, and this finding was also consistent with the findings of a previous study [13]. In the study by Canto et al., the proportion of patents with cardiogenic shock was 6.1%, 5.0%, 4.4%, 3.7%, 3.5% and 3.3% for patients with 0, 1, 2, 3, 4 and 5 coronary risk factors, respectively [13]. Our study population included AMI patients with previous MI, which might have affected the higher prevalence of cardiogenic shock in comparison to the study by Canto et al.
The impact of coronary risk factors may be modified by modern medical treatment approaches, such as statin treatment or intensive diabetic control. Studies predicting the prevalence of cardiovascular disease were mainly performed before evidence had been obtained concerning the efficacy of statin treatment or intensive diabetic control [5,6,8,14,15]. The penetration rate of statin treatment for high-cholesterol and intensive diabetic control has been increasing, as it is highly recommended by guidelines [[1], [2], [3], [4],16]. Indeed, in Japan, despite a continuous and marked rise in total cholesterol levels, a continuous decline in mortality due to coronary heart disease has been observed [17].
The obesity paradox reported by Hastie et al. is another phenomenon that resembles the findings of our present study [18]. In the study by Hastie et al., overweight (body mass index [BMI] ≥27.5 but <30) was associated with a lower mortality than a normal weight (BMI ≥20 but <25) or underweight (BMI <20) among patients undergoing PCI. Of note, that study showed that a higher BMI was associated with an increased number of coronary risk factors, such as hypertension and diabetes. Similar findings were also reported in previous studies [19,20]. The inverse association between the number of coronary risk factors and in-mortality in our study may therefore partially represent the underlying obesity paradox.
Pathologically, AMI is not a single homogenous disease, as it is caused by multiple types of culprit plaque, including plaque rupture, plaque erosion and calcified nodules [21]. The impact of coronary risk factors differs depending on the culprit plaque [[22], [23], [24]]. Plaque rupture is highly associated with a high level of cholesterol, while plaque erosion is less closely associated with coronary risk factors [22,23]. In the present study, women under 50 years old showed distinct features of a low number of coronary risk factors but a relatively high in-hospital mortality, although the total number of women under 50 years old was only 154, accounting for 0.7% of the total population. These women are more likely to develop plaque erosion than other population according to previous studies [[21], [22], [23]]. Spontaneous coronary artery dissection may be partially involved, as which often occur in younger women and its in-hospital mortality is reported to be higher [25]. The elderly are another population that showed a high in-hospital mortality of AMI despite relatively few coronary risk factors. The culprit plaque is more likely to be calcified nodules in people over 80 years old than in other populations, and this type seems to be associated with a poorer outcome than other culprit plaques [21,23,24,26].
The in-hospital mortality of patients over 80 years old is markedly high despite relatively few coronary risk factors, which may have affected the results of our study. Multiple factors influence the outcomes of elderly patients. Physical fitness, which is important and protective against cardiovascular disease, is generally impaired in this population [27]. Previous studies have shown that older AMI patients are often complicated with heart failure, which may be associated with increased ventricular systolic and diastolic stiffness in elderly patients [9,28,29]. Therefore, despite the relatively few coronary risk factors in older people, the cumulative effects of coronary risk factors are likely to matter. Another point is that superaged patients (over 80 years old) tend to have less chance to undergo revascularization therapy [9,30]. In our population, only 79.9% of patients ≥80 years old received primary PCI, while 90.3% of those <80 years old received primary PCI [9]. This might have influenced the high in-hospital mortality of patients over 80 years old who have relatively few coronary risk factors, although the actual situation is not quite that simple [9,29]. The selection of an invasive strategy for super-aged AMI patients is expected to increase as the average life expectancy time increases and technology improves [29]. Overall, in elderly patients, multiple factors beyond traditional coronary risk factors exist, which makes predicting the outcomes of this population quite complex.
4.1. Limitations
Several limitations associated with the present study warrant mention. Information on the family history and a previous history of either coronary artery disease or the prevalence of chronic kidney disease was not collected, which might have had some effect on the results. It is also possible that an accurate diagnosis of coronary risk factors in more severe AMI patients may have been missed or overlooked due to a patient's severe condition. Similarly, masked hypertension, diabetes, dyslipidemia and smoking may have been under-reported. The lack of a quantifiable analysis of the coronary risk factors may also have limited the extent of the study. Our study findings only apply to AMI patients with an onset-to-door time of 24 h or less.
5. Conclusion
In the present study of Japanese patients with AMI who received modern medical treatment, middle-aged subjects (40s for men and 50s for women) had the most coronary risk factors but the lowest in-hospital mortality. The in-hospital mortality of AMI was inversely related to the number of coronary risk factors. Further studies are needed to investigate the underlying reasons for these findings.
Financial support
This work was supported in part by a Grant-in-Aid for Scientific Research (17K09542) from the Ministry of Education, Culture, Sports, Science and Technology, Japan.
Credit author statement
Hiroyoshi Mori: Conceptualization, Investigation, Writing Original Draft; Hiroshi Suzuki: Writing Review & Editing, Supervision; Kensaku Nishihira: Writing Review & Editing, Supervision, Project administration; Satoshi Honda: Writing Review & Editing, Supervision; Sunao Kojima: Data curation, Writing Review; Misa Takegami: Data curation, Writing Review; Jun Takahashi: Data curation, Writing Review; Tomonori Itoh: Data curation, Writing Review; Tetsu Watanabe: Data curation, Writing Review; Takashi Takenaka: Data curation, Writing Review; Masaaki Ito: Data curation, Writing Review; Morimasa Takayama: Data curation, Writing Review; Kazuomi Kario: Data curation, Writing Review; Tetsuya Sumiyoshi: Data curation, Writing Review; Kazuo Kimura: Data curation, Writing Review; Satoshi Yasuda: Writing Review & Editing, Supervision, Project administration, Funding acquisition.
Declaration of competing interest
There are no financial or other relationships that could lead to a conflict of interest.
Contributor Information
Hiroyoshi Mori, Email: hymori@med.showa-u.ac.jp.
Satoshi Yasuda, Email: yasuda.satoshi.hp@ncvc.go.jp.
References
- 1.Arnett D.K., Blumenthal R.S., Albert M.A. ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American college of Cardiology/American heart association task force on clinical practice guidelines. Circulation. 2019;140(11):e596–646. doi: 10.1161/CIR.0000000000000678. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williams B., Mancia G., Spiering W. ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. 2018. [DOI] [PubMed] [Google Scholar]
- 3.Cosentino F., Grant P.J., Aboyans V. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J. 2019 doi: 10.1093/eurheartj/ehz486. 2019. [DOI] [PubMed] [Google Scholar]
- 4.Mach F., Baigent C., Catapano A.L. ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur. Heart J. 2019 doi: 10.1093/eurheartj/ehz455. 2019. [DOI] [PubMed] [Google Scholar]
- 5.Mahmood S.S., Levy D., Vasan R.S., Wang T.J. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Lancet (London, England) 2014;383(9921):999–1008. doi: 10.1016/S0140-6736(13)61752-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okumiya N., Tanaka K., Ueda K., Omae T. Coronary atherosclerosis and antecedent risk factors: pathologic and epidemiologic study in Hisayama, Japan. Am. J. Cardiol. 1985;56(1):62–66. doi: 10.1016/0002-9149(85)90567-3. [DOI] [PubMed] [Google Scholar]
- 7.Honda T., Yoshida D., Hata J. Development and validation of modified risk prediction models for cardiovascular disease and its subtypes: the Hisayama Study. Atherosclerosis. 2018;279:38–44. doi: 10.1016/j.atherosclerosis.2018.10.014. [DOI] [PubMed] [Google Scholar]
- 8.Wilson P.W.F., D'Agostino R.B., Levy D., Belanger A.M., Silbershatz H., Kannel W.B. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97(18):1837–1847. doi: 10.1161/01.CIR.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 9.Kojima S., Nishihira K., Takegami M. Nationwide real-world database of 20,462 patients enrolled in the Japanese Acute Myocardial Infarction Registry (JAMIR): impact of emergency coronary intervention in a super-aging population. IJC Hear Vasc. 2018;20:1–6. doi: 10.1016/j.ijcha.2018.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishihira K., Kojima S., Takegami M. Clinical characteristics and in-hospital mortality according to left main and non-left main culprit lesions. Circ Rep. 2019;1:601–609. doi: 10.1253/circrep.CR-19-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thygesen K., Alpert J.S., Jaffe A.S. Third universal definition of myocardial infarction. Eur. Heart J. 2012;33(20):2551–2567. doi: 10.1093/eurheartj/ehs184. [DOI] [PubMed] [Google Scholar]
- 12.Tunstall-Pedoe H., Kuulasmaa K., Amouyel P., Arveiler D., Rajakangas A.M., Pajak A. Myocardial infarction and coronary deaths in the World health organization. Circulation. 1994;90(1):583–612. doi: 10.1161/01.CIR.90.1.583. [DOI] [PubMed] [Google Scholar]
- 13.Canto J.G., Kiefe C.I., Rogers W.J. Number of coronary heart disease risk factors and mortality in patients with first myocardial infarction. JAMA, J. Am. Med. Assoc. 2011;306(19):2120–2127. doi: 10.1001/jama.2011.1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strandberg T.E., Pyörälä P.K., Cook T.J. Mortality and incidence of cancer during 10-year follow-up of the scandinavian simvastatin survival study (4S) Lancet. 2004;364(9436):771–777. doi: 10.1016/S0140-6736(04)16936-5. [DOI] [PubMed] [Google Scholar]
- 15.Holman R.R., Paul S.K., Bethel M.A., Matthews D.R., Neil H.A.W. 10-Year follow-up of intensive glucose control in type 2 diabetes. N. Engl. J. Med. 2008;359(15):1577–1589. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]
- 16.Kimura K., Kimura T., Ishihara M. JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ. J. 2019;83(5):1085–1196. doi: 10.1253/circj.CJ-19-0133. [DOI] [PubMed] [Google Scholar]
- 17.Sekikawa A., Miyamoto Y., Miura K. Continuous decline in mortality from coronary heart disease in Japan despite a continuous and marked rise in total cholesterol: Japanese experience after the Seven Countries Study. Int. J. Epidemiol. 2015;44(5):1614–1624. doi: 10.1093/ije/dyv143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hastie C.E., Padmanabhan S., Slack R. Obesity paradox in a cohort of 4880 consecutive patients undergoing percutaneous coronary intervention. Eur. Heart J. 2010;31(2):222–226. doi: 10.1093/eurheartj/ehp317. [DOI] [PubMed] [Google Scholar]
- 19.Chan J.M., Rimm E.B., Colditz G.A., Stampfer M.J., Willett W.C. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care. 1994;17(9):961–969. doi: 10.2337/diacare.17.9.961. [DOI] [PubMed] [Google Scholar]
- 20.Field A.E., Coakley E.H., Must A. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch. Intern. Med. 2001;161(13):1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 21.Virmani R., Kolodgie F.D., Burke A.P., Farb A., Schwartz S.M. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler. Thromb. Vasc. Biol. 2000;20(5):1262–1275. doi: 10.1161/01.ATV.20.5.1262. [DOI] [PubMed] [Google Scholar]
- 22.Burke A.P., Farb A., Malcom G.T., Liang Y.H., Smialek J.E., Virmani R. Plaque rupture and sudden death related to exertion in men with coronary artery disease. J. Am. Med. Assoc. 1999;281(10):921–926. doi: 10.1001/jama.281.10.921. [DOI] [PubMed] [Google Scholar]
- 23.Yamamoto E., Yonetsu T., Kakuta T. Clinical and laboratory predictors for plaque erosion in patients with acute coronary syndromes. J Am Heart Assoc. 2019;8(21) doi: 10.1161/JAHA.119.012322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee T., Mintz G.S., Matsumura M. Prevalence, predictors, and clinical presentation of a calcified nodule as assessed by optical coherence tomography. JACC Cardiovasc Imag. 2017;10(8):883–891. doi: 10.1016/j.jcmg.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 25.Saw J., Starovoytov A., Humphries K. Canadian spontaneous coronary artery dissection cohort study: in-hospital and 30-day outcomes. Eur. Heart J. 2019;40(15):1188–1197. doi: 10.1093/eurheartj/ehz007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kobayashi N., Takano M., Tsurumi M. Features and outcomes of patients with calcified nodules at culprit lesions of acute coronary syndrome: an optical coherence tomography study. Cardiology. 2018;139(2):90–100. doi: 10.1159/000481931. [DOI] [PubMed] [Google Scholar]
- 27.Shigdel R., Dalen H., Sui X., Lavie C.J., Wisløff U., Ernstsen L. Cardiorespiratory fitness and the risk of first acute myocardial infarction: the HUNT study. J Am Heart Assoc. 2019;8(9) doi: 10.1161/JAHA.118.010293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Borlaug B.A., Redfield M.M., Melenovsky V. Longitudinal changes in left ventricular stiffness a community-based study. Circ Hear Fail. 2013;6(5):944–952. doi: 10.1161/CIRCHEARTFAILURE.113.000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sato K., Takahashi J., Hao K. Temporal trends in the prevalence and outcomes of geriatric patients with acute myocardial infarction in Japan–A report from the Miyagi AMI Registry Study–. J. Cardiol. 2019 doi: 10.1016/j.jjcc.2019.10.006. [DOI] [PubMed] [Google Scholar]
- 30.Tegn N., Abdelnoor M., Aaberge L. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (After Eighty study): an open-label randomised controlled trial. Lancet. 2016;387(10023):1057–1065. doi: 10.1016/S0140-6736(15)01166-6. [DOI] [PubMed] [Google Scholar]