ABSTRACT
Background
Posttraumatic stress disorder is associated with a high economic burden. Costs of treatment are known to be high, and cost-effectiveness has been analysed for several treatment options.
Objective
As no review on economic aspects of posttraumatic stress disorder exists, the aim of this study was to systematically review costs-of-illness studies and economic evaluations of therapeutic treatment for posttraumatic stress disorder, and to assess their quality.
Method
A systematic literature search was performed in March 2017 and was last updated in February 2020 in the databases PubMed, PsychInfo and NHS Economic Evaluation Database. Cost-of-illness studies and economic evaluations of treatment for posttraumatic stress disorder were selected. Extracted cost data were categorized as direct costs and indirect costs and inflated to 2015 US-$ purchasing power parities (PPP). Quality was assessed using an adapted cost-of-illness studies quality checklist, the Consensus on Health Economic Criteria list, and the questionnaire to assess relevance and credibility of modelling studies by the International Society for Pharmacoeconomics and Outcome Research.
Results
In total, 13 cost-of-illness studies and 18 economic evaluations were included in the review. Annual direct excess costs ranged from 512 US-$ PPP to 19,435 US-$ PPP and annual indirect excess costs were 5,021 US-$ PPP per person. Trauma-focused cognitive-behavioural therapy (+selective serotonin re-uptake inhibitor) was found to be cost-effective compared with treatment as usual and no treatment. Overall, included studies were of low and moderate quality. Studies used inappropriate economic study designs and lacked information on the economic perspective used.
Conclusions
Posttraumatic stress disorder is a major public health problem that causes high healthcare costs. While trauma-focused cognitive-behavioural therapy was found to be cost-effective, further investigations regarding pharmacotherapy and other treatments are necessary.
KEYWORDS: Systematic review, posttraumatic stress disorder, economic evaluation, cost-of-illness, economic expenditure
HIGHLIGHTS: • Costs of PTSD were associated with trauma experience, symptom severity and treatment status.• TF-CBT (+SSRI) was cost-effective for children, adolescents and adults with PTSD.• Integrative care was cost-effective for adults with PTSD; however, evidence for children and adolescents is lacking.
Antecedentes: El trastorno por estrés postraumático está asociado con una alta carga económica. Se sabe que los costos de tratamiento son elevados, y su costo-efectividad ha sido analizado para varias opciones de tratamiento.
Objetivo: Debido a que no existe ninguna revisión sobre los aspectos económicos del trastorno de estrés postraumático, el objetivo de este estudio fue hacer una revisión sistemática de estudios de costo de enfermedad y evaluaciones económicas del tratamiento terapéutico para trastorno por estrés postraumático, y evaluar su calidad.
Métodos: Se realizó una revisión sistemática de la literatura en Marzo de 2017 y fue actualizada por última vez en Febrero 2020 en las bases de datos PubMed, PsychInfo y la Base de datos de Evaluación Económica de NHS. Se seleccionaron estudios de costo de enfermedad y evaluaciones económicas de tratamiento para trastorno por estrés postraumático. Los datos extraídos sobre los costos fueron categorizados como costos directos e indirectos y elevados al dolar estadounidense del 2015 y su Paridad de Poder Adquisitivo (PPP por sus siglas en inglés). La calidad fue evaluada usando una lista de chequeo adaptada sobre la calidad de estudios de costo de enfermedad, la lista del Consenso en Criterios de Economía de Salud, y el cuestionario para evaluar relevancia y credibilidad de estudios de modelado de la Sociedad Internacional de Farmacoeconomía e investigación de Resultados.
Resultados: En total, 13 estudios de costo de enfermedad y 18 evaluaciones económicas fueron incluidas en la revisión. Los costos anuales directos en exceso oscilaron entre 512 US-$ PPP a 19,435 US-$ PPP y los costos anuales indirectos en exceso fueron de 5,021 US-$ PPP por persona. La terapia cognitivo-conductual focalizada en el trauma (+ un inhibidor selectivo de la recaptura de la serotonina) fue costo-efectiva en comparación con el tratamiento usual y con no tratar. Los estudios usaron diseños inapropiados para un estudio económico y carecían de información sobre la perspectiva económica usada.
Conclusiones: el trastorno por estrés postraumático es un problema de salud pública importante que causa grandes costos en atención de salud. Si bien se encontró que la terapia cognitivo-conductual focalizada en el trauma fue costo-efectiva,se requieren investigaciones futuras en relación a la farmacoterapia y otros tratamientos.
PALABRAS CLAVE: Revisión Sistemática, Trastorno por estrés postraumático, evaluación económica, costo de enfermedad, inversión económica
背景:创伤后应激障碍与高经济负担相关。已知治疗费用很高, 并且已经针对几种治疗方案的成本效益进行了分析。
目标:由于尚无关于创伤后应激障碍经济方面的综述, 本研究旨在对创伤后应激障碍的疾病成本研究及其治疗的经济评估系统地进行综述, 并评估研究质量。
方法:于2017年3月在PubMed, PsychInfo和NHS经济评估数据库进行了系统的文献检索, 最后于2020年2月进行了更新。选取了针对创伤后应激障碍的疾病成本研究及其治疗的经济评估。提取的成本数据分为直接成本和间接成本, 并将其通货膨胀为2015年美元购买力平价 (PPP) 。使用一项疾病成本研究质量清单——《卫生经济标准共识清单》的改编版本, 以及国际药物经济学及结果研究协会评估模型研究相关性和可信性的问卷, 对研究质量进行了评估。
结果:总共纳入了13项疾病成本研究和18项经济评估。年度直接超额成本从512美元PPP至19,435美元PPP不等, 年度间接超额成本为每人5,021美元PPP。与常规治疗和不治疗相比, 聚焦创伤的认知行为疗法 (+选择性5-羟色胺再摄取抑制剂) 被认为具有成本效益。总体而言, 纳入的研究具有较低和中等质量。研究使用了不适当的经济研究设计, 并且缺乏所用经济学观点的信息。
结论:创伤后应激障碍是导致公共卫生费用高昂的主要公共卫生问题。尽管发现聚焦创伤的认知行为疗法具有成本效益, 但有必要对药物疗法和其他疗法进行进一步研究。
关键词: 系统综述; 创伤后应激障碍; 经济评估; 疾病成本; 经济支出
1. Introduction
Posttraumatic Stress Disorder (PTSD) is a highly prevalent mental disorder with a lifetime prevalence of 1% to 8% (Alonso et al., 2004; Bunting, Murphy, O’Neill, & Ferry, 2012; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995), with women affected more often than men (Kessler et al., 1995). According to the DSM-5, PTSD is diagnosed in individuals who were exposed to a trauma, or who witnessed a traumatic event, which is re-experienced by, inter alia, flashbacks or nightmares. In addition, individuals diagnosed with PTSD have a high physical arousal and negative thoughts, leading to avoidance of trauma-related stimuli (American Psychiatric Association, 2013). They often suffer from comorbidities, especially depression and anxiety disorders (Frayne et al., 2004; Sareen et al., 2007). Thus, they have a high healthcare utilisation (van Zelst, de Beurs, Beekman, van Dyck, & Deeg, 2006) and show severe impairments in health-related quality of life (Rapaport, Clary, Fayyad, & Endicott, 2005; van Zelst et al., 2006). Persons with PTSD have also been found to be less satisfied with their life (Rapaport et al., 2005; van Zelst et al., 2006), feel lonelier (van Zelst et al., 2006) and attempt suicide more often (Sareen et al., 2007).
Trauma-focused psychotherapies, such as trauma-focused cognitive-behavioural therapy (TF-CBT), eye movement desensitization and reprocessing (EMDR) and prolonged exposure, are recommended for treatment of PTSD (American Psychological Association, 2017; Bisson, Roberts, Andrew, Cooper, & Lewis, 2013; National Institute for Health and Care Excellence, 2018; VA/DoD Clinical Practice Guideline Working Group, 2017). In addition, non-trauma-focused psychotherapies, such as non-trauma-focused cognitive-behavioural therapy (non-TF-CBT) and anger management, are recommended (American Psychological Association, 2017; Bisson et al., 2013; National Institute for Health and Care Excellence, 2018; VA/DoD Clinical Practice Guideline Working Group, 2017). TF-CBT is recommended as primary treatment for both adults and children (National Institute for Health and Care Excellence, 2018; Watkins, Sprang, & Rothbaum, 2018). TF-CBT, as a variant of cognitive-behavioural therapy, is trauma-specific. It has the aim of modifying excessively negative appraisals of the trauma and its sequelae, reducing the re-experiencing of the trauma through the elaboration of the trauma memories and discrimination of triggers, and removal of dysfunctional behaviours and cognitive strategies (Ehlers et al., 2010). General behavioural and cognitive strategies of CBT are exposure, cognitive restructuring, changes in behaviour and development of coping skills (American Psychological Association, 2017). As secondary treatment, EMDR is recommended for children not responding to TF-CBT or adults preferring EMDR (National Institute for Health and Care Excellence, 2018; Watkins et al., 2018). In short, the procedure of EMDR involves rhythmic saccadic eye movements while having the patient imagine the worst part of a traumatic memory in order to desensitize memories, restructure conditions and alter the traumatic pictures (Rothbaum, Astin, & Marsteller, 2005; Shapiro, 1989). If persons are unable or unwilling to participate in a trauma-focused psychotherapy, non-trauma-focused psychotherapy can be offered (National Institute for Health and Care Excellence, 2018; Watkins et al., 2018). In general, non-trauma-focused therapies aim to reduce symptoms, without targeting trauma-related thoughts or emotions (Watkins et al., 2018). Non-trauma-focused psychotherapies for individuals with PTSD focus on anxiety reduction strategies, such as stress inoculation training, which seeks to teach skills like relaxation, thought stopping and guided dialogue (American Psychological Association, 2017). Finally, in addition to psychotherapy, the use of a selective serotonin reuptake inhibitor (SSRI) is recommended for the treatment of comorbid depression in adults (National Institute for Health and Care Excellence, 2018). Furthermore, integrated care, i.e. the linkage and coordination of services to overcome fragmentation of care for patients with complex needs (e.g. collaborative care, stepped care, patient-involvement) (Stokes, Checkland, & Kristensen, 2016), has the potential to reduce the health and economic burden (National Institute for Health and Care Excellence, 2018).
As PTSD negatively influences social life and psychotherapy is advised, the overall economic burden is expected to be high (National Institute for Health and Care Excellence, 2018; Statistisches Bundesamt, 2019). Knowing the economic burden of a disorder is important for decision-makers to be able to justify budgets of promotion of research and intervention programs (Ament & Evers, 1993; Rice, 1994). Cost-of-illness studies (COIs) determine direct and indirect costs of a particular disorder by taking a specific perspective, such as a societal perspective or a healthcare payer’s perspective (Byford, Torgerson, & Raftery, 2000). Direct costs are defined as those payments directly associated with a disorder (e.g. costs of inpatient or outpatient treatment, drugs). Indirect costs sum up the loss of employment resources (e.g. absenteeism, presenteeism) and unpaid caregivers’ labour (e.g. informal care) (Ament & Evers, 1993; Ernst, 2006). The societal perspective is widely used, as it considers all direct and indirect costs (Johnston, Buxton, Jones, & Fitzpatrick, 1999). In contrast, the healthcare payer’s perspective neglects costs not covered by the health insurance (e.g. indirect costs). COIs frequently report excess costs, which represent healthcare cost differences of individuals with a particular disorder compared with those without.
As COIs do not set treatment costs in relation to the effectiveness of interventions, economic evaluations (EEs) are conducted (Thielen et al., 2016; van Mastrigt et al., 2016). A full EE, such as a cost-effectiveness analysis (CEA) or cost-utility analysis (CUA) primarily compares costs and effects/utilities of two or more alternative interventions. Effects are normally measured by clinical units, such as symptom severity, whereas utilities are measured by quality-adjusted life years (QALYs) or disability-adjusted life years (DALYs) (van Mastrigt et al., 2016). In contrast, a partial EE compares two or more alternative interventions by their costs without necessarily considering effects or utilities in relation to costs (Rabarison, Bish, Massoudi, & Giles, 2015). EEs either are conducted alongside a clinical trial or are based on a model. EEs based on a model use various data sources such as empirical studies, literature on aggregated health data and statistical estimations of parameters for the assessment of the relation of costs and effects of alternative interventions (Wijnen et al., 2016).
Earlier reviews on economic aspects of PTSD were able to identify relevant literature (Canadian Agency for Drugs and Technologies in Health, 2012; Canadian Agency for Drugs and Technologies in Health, 2010; Hetrick, Purcell, Garner, & Parslow, 2010; Solomon & Davidson, 1997). However, the included literature was limited to specific treatments for PTSD, such as day-programming or combined pharmacotherapy and psychotherapy. Thus, a comprehensive review on economic aspects of PTSD does not yet exist. Furthermore, existing reviews were published before 2013. As a considerable number of articles have been published in recent years, an update of the existing reviews, without any restrictions with respect to sample characteristics such as age or gender, or the traumatic experience or intervention, is required.
Costs of PTSD could be influenced by the specifics of healthcare systems of different countries, as well as by interpersonal characteristics, such as traumatic experiences, gender and age at PTSD-onset. Veterans with PTSD, for instance, are often treated within the military health system (Eekhout, Geuze, & Vermetten, 2016; Morland et al., 2013); thus, costs of PTSD in veteran samples may differ to those in civilian samples. Furthermore, some traumatic experiences, such as traumatic war experiences are more common in men (Eekhout et al., 2016; Morland et al., 2013), whereas others, such as sexual and physical abuse are more common in children, adolescents, and women (Gospodarevskaya & Segal, 2012; Priebe et al., 2017; Suris, Lind, Kashner, Borman, & Petty, 2004; Walker et al., 2003).
Apart from the aim to identify cost structures in PTSD and potential cost-driving factors, another aim of this study was to determine whether integrated care, TF-CBT, non-TF-CBT and EMDR are cost-effective compared with treatment as usual (TAU), and compared with each other.
Therefore, the current review referred to the following research questions:
What are the costs associated with PTSD?
Which factors influence the costs of PTSD?
(3.1) Which treatment options based on psychotherapies and models of integrated care are cost-effective for children and adolescents with PTSD?
(3.2) Which treatment options based on psychotherapies and models of integrated care are cost-effective for adults with PTSD?
In order to achieve these aims, literature on economic aspects of PTSD was systematically reviewed and their methodological quality was assessed.
2. Materials and methods
2.1. Literature search and selection criteria
A systematic literature search was performed in the databases PubMed, PsychInfo and the NHS Economic Evaluation Database in March 2017 and was updated in February 2019 and February 2020. The following sensitive search syntax was used: posttraumatic stress disorder (MeSH) AND (cost* OR economic* OR expenditure* OR cost-effectiveness*). No restrictions related to publication year were imposed. Articles were independently selected by title and abstract. Two authors (JD, RvdW) independently screened literature for their relevance. Only articles that primarily addressed PTSD and reported costs or cost-effectiveness were selected. Only studies available in English or German were considered and only original research was included. Editorials, letters or case reports were excluded. Subsequently, screening results of both authors were checked against each other. If the fulfilment of inclusion criteria by an abstract was unclear to at least one author, the abstract would be discussed by both authors. Finally, the full-texts of articles selected by at least one author were screened based on inclusion and exclusion criteria. Again, screening results of both authors were checked against each other and any disagreement on relevance was resolved through discussion. Additionally, references of the full-texts were scanned for further eligible articles.
2.2. Data extraction
Data on study characteristics (e.g. study design, sample and study setting), effects and costs were extracted from COIs and EEs. Extracted cost data were categorized as direct costs (i.e. inpatient treatment, outpatient physician treatment, drugs, non-physician treatment, rehabilitation and non-medical costs) and indirect costs (i.e. presenteeism, absenteeism and informal care). All cost data were adapted to annual costs per person, inflated to the year 2015 using country-specific consumer price indexes and converted to US-$ using purchasing power parities (US-$ PPP) (Organisation for Economic Co-operation and Development. Health Statistics 2017, 2017). If no reference year for the adaption of cost data was given, the year of publication was assumed as the base year for inflation.
Data on the incremental cost-effectiveness ratio (ICER), i.e. the ratio of the difference in the mean costs ( and the difference of the mean effects () of two treatments, were extracted from full EEs (Kilian, 2008):
2.3. Quality assessment
Quality of trial-based EEs was assessed using the Consensus on Health Economic Criteria (CHEC) list by Evers et al. (Evers, Goossens, de Vet, van Tulder, & Ament, 2005). For the quality of model-based EEs, the questionnaire on the relevance and credibility of modelling studies for informing healthcare decision-making by the International Society for Pharmacoeconomics and Outcome Research (ISPOR) was used (Jaime Caro et al., 2014). Both, the CHEC list and the ISPOR questionnaire have been recommended by Wijnen et al. (2016) for the critical appraisal of the quality of trial-based and model-based EEs in systematic reviews. Neither of them is applicable for COIs and no formal international guideline for quality assessment of COIs is available at present (Wang, Si, Cocker, Palmer, & Sanderson, 2018). Therefore, quality of COIs was assessed using an adapted COI quality checklist by Schirr-Bonnans et al. (2017) based on Molinier et al. (2008) and Drummond, Sculpher, Torrance, O’Brien, & Stoddart (2005) that has been already used by multiple systematic reviews (e.g. Mutyambizi, Pavlova, Chola, Hongoro, & Groot, 2018; Shafie, Tan, & Ng, 2018; Wang et al., 2018). The CHEC list comprises 19 yes-or-no questions each addressing a single category (e.g. economic study design, time horizon and cost valuation) (Evers et al., 2005). The ISPOR questionnaire comprises 15 yes-or-no questions addressing the eight sections: relevance, validation, design, data, analysis, reporting, interpretation and conflict of interest (Jaime Caro et al., 2014). The COI quality checklist comprises nine yes-partial-no-questions each addressing a single category (e.g. definition of the illness, study perspective and cost valuation) (Schirr-Bonnans et al., 2017).
In accordance with earlier systematic reviews, the overall quality was summarized as the percentage of fulfilled items. Overall quality was represented on an ordinal scale with the categories ‘excellent quality’, ‘good quality’, ‘moderate quality’ and ‘low quality’, defined as 100%, >75% to <100%, >50% to ≤75% and ≤50% of the checklist items fulfilled, respectively (Hamberg-van Reenen, Proper, & van den Berg, 2012; Wong, Liao, Guo, Xin, & Lam, 2017).
3. Results
3.1. Search results
In total, 1,558 studies were identified through database searching. Subsequently, 154 duplicates were removed and thus 1,404 records were screened. Approximately, 95% of the screened records were excluded, as either PTSD or cost and cost-effectiveness, were not addressed. In the context of the screening of titles and abstracts, 35 studies were discussed, as the fulfilment of inclusion criteria was unclear for at least one author. Of the discussed studies, 10 were selected for full-text assessment. Subsequently, 57 studies were selected by at least one author for full-text assessment. Based on full-text assessment, nine studies were discussed, as the fulfilment of inclusion criteria was unclear for at least one author. Of the discussed studies, one was selected for qualitative synthesis. Subsequently, 24 studies were selected by at least one author for qualitative synthesis. Additionally, seven studies were identified through manual search and the screening of reference lists of the selected studies. Finally, 31 studies, 13 COIs, 13 EEs (four CEAs and nine CUAs) and five partial EEs were included in the review. A flow chart of the selection process is presented in Figure 1.
Figure 1.
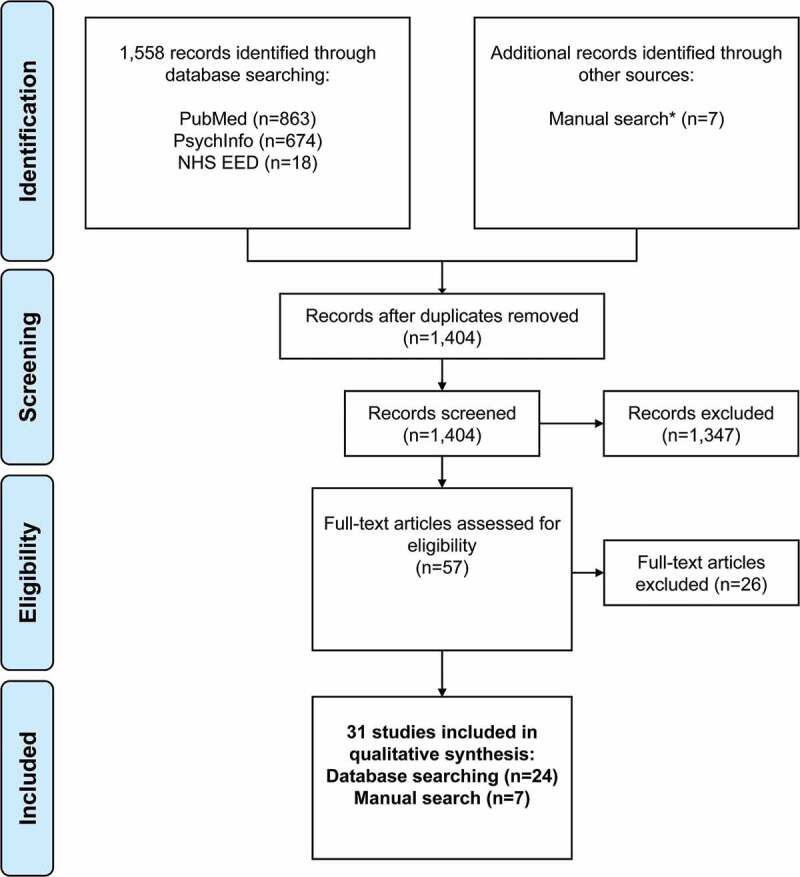
Study selection process.
3.2. Cost-of-illness studies
3.2.1. Study characteristics
The earliest COIs were published in 2003 (Chan, Medicine, Air, & McFarlane, 2003; Walker et al., 2003), and the most recent COI was published in 2017 (Priebe et al., 2017) (Table 1). Six studies were conducted in North America (Chan, Cheadle, Reiber, Unutzer, & Chaney, 2009; Ivanova et al., 2011; Lamoureux-Lamarche, Vasiliadis, Preville, & Berbiche, 2016; Suris et al., 2004; Walker et al., 2003), six were conducted in Europe (Eekhout et al., 2016; Ferry et al., 2015; Priebe et al., 2009, 2010, 2017; Sabes-Figuera et al., 2012) and two in Australia (Chan et al., 2003; O’Donnell, Creamer, Elliott, & Atkin, 2005). The sample size of the studies ranged from N = 74 (Priebe et al., 2017) to N = 18,834 (Ivanova et al., 2011) in trial-based COIs. Three studies determined costs of PTSD from a healthcare payers’ perspective (Ivanova et al., 2011; Lamoureux-Lamarche et al., 2016; Walker et al., 2003), whereas 10 studies did not report the perspective used for cost-measurement (Chan et al., 2009, 2003; Eekhout et al., 2016; Ferry et al., 2015; O’Donnell et al., 2005; Priebe et al., 2009, 2010, 2017; Sabes-Figuera et al., 2012; Suris et al., 2004).
Table 1.
Characteristics of cost-of-illness studies, cost-effectiveness analyses and cost-utility analyses.
| Study | Study year | Country | Study design | Study sample | Age in mean years (SD) | PTSD measure/utility measure | Sample size |
|---|---|---|---|---|---|---|---|
| COIs – Excess costs | |||||||
| Chan et al. (2003) | 2003 | Australia | OS | Victims of traffic accidents | 39 (13) and 39 (13)a | PCL-C | 391 |
| O’Donnell et al. (2005) | 2005 | Australia | OS | Victims of traffic accidents | 37 (14) | CAPS | 255 |
| Chan et al. (2009) | 2009 | USA | OS | Veterans with depression | - | PC-PTSD | 606 |
| Eekhout et al. (2016) | 2016 | The Netherlands | OS | Soldiers deployed to Afghanistan | 28 (9) | SRIP | 1,007 |
| Lamoureux-Lamarche et al. (2016) | 2016 | Canada | OS | Older adults aged >65 | 72 (6) and 74 (6)a | PTSS | 1,456 |
| COIs – Cost comparisons based on (sub-)groups | |||||||
| Walker et al. (2003) | 2003 | USA | OS | Females aged 18 to 65 | 42 (12) | PCL-C | 1,225 |
| Suris et al. (2004) | 2004 | USA | OS | Female sexually assaulted veterans | 47 (12) | CAPS | 270 |
| Priebe et al. (2009) | 2009 | Persons from FYR living in Croatia, Serbia, Germany, UK | ES | War-affected adults aged 18 to 70 | 43 (12) | CAPS | 264 |
| Priebe et al. (2010) | 2010 | FYR | OS | War-affected adults aged 18 to 65 | 44 (11) | CAPS | 463 |
| Ivanova et al. (2011) | 2011 | USA | OS | Adults aged 18–64 who had at least 2 claims for PTSD based on ICD-9 | 38 (12) and 43 (12)b | - | 18,834 |
| Sabes-Figuera et al. (2012) | 2012 | BiH, Croatia, Kosovo, FYR Macedonia, Serbia, and persons from FYR living in Germany, Italy, UK | OS | War-affected adults aged 18 to 65 | 42 | LSC-R; MINI | 4,167 |
| Ferry et al. (2015) | 2015 | Northern Ireland | OS | Adults who met the criteria for 12-month or lifetime DSM-IV PTSD | - | - | 4,340 |
| Priebe et al. (2017) | 2017 | Germany | RCT | Sexually assaulted females with PTSD and comorbid mental disorder | 36 (10) | PTDS, CAPS | 74 |
| CEAs/CUAs – Psychotherapy | |||||||
| Gospodarevskaya & Segal (2012) | 2012 | AU | M-CUA | Sexually abused children with PTSD | - | QALY | - |
| Morland et al. (2013) | 2013 | USA | QES-CEA | Male veterans with PTSD and moderate to severe anger problems | 56 (8) | CAPS | 74 |
| Le, Doctor, Zoellner, & Feeny (2014) | 2014 | USA | RPT-CUA | Adults aged 18 to 65 with PTSD based on DSM-IV | 38 (11) | QALY (EQ-5D-3 L) | 200 |
| Mihalopoulos et al. (2015) | 2015 | AU | M-CUA | Adults, children and adolescents with PTSD based on DSM-IV | - | QALY (AQoL-4D)/DALY | - |
| Macdonald et al. (2016) | 2016 | UK | M-CEA | Sexually abused children | - | - | - |
| Slade et al. (2017) | 2017 | USA | RCT-CEA | Adults with severe PTSD and severe mental disorder | 44 (1) and 43 (1)c | CAPS | 183 |
| Shearer et al. (2018) | 2018 | UK | RCT-CUA + M-CUA | Children and adolescents aged 8 to 17 with PTSD based on ICD-10 | - | QALY (CHU-9D) | 29 |
| Aas, Iversen, Holt, Ormhaug, & Jensen (2019) | 2019 | Norway | RCT-CUA | Adolescents aged 10 to 18 with PTSD symptoms based on CPSS | 15 (2) | QALY (16D) | 156 |
| CEAs/CUAs – Integrated care | |||||||
| Domino, Morrissey, Nadlicki-Patterson, & Chung (2005) | 2005 | USA | QES-CEA | Physically and/or sexually abused females with mental health and substance use disorder | - | - | 2,006 |
| Cohen et al. (2017) | 2017 | USA | M-CEA | Adults with PTSD after natural disaster | - | DALY/PCL | 2,642,713 |
| Painter, Fortney, Austen, & Pyne (2017) | 2017 | USA | RCT-CUA | Veterans with PTSD based on CAPS | 52 (14) | QALY (QWB) | 265 |
| Chang, Andersen, Berisha, Estrup, & Wang (2018) | 2018 | Kosovo | RCT-CUA | War-affected persons with comorbid disorders | - | QALY (WHODAS 2.0) | 34 |
| CEAs/CUAs – Other | |||||||
| Issakidis, Sanderson, Corry, Andrews, & Lapsley (2004) | 2004 | AU | M-CEA | Adults who had a claim for PTSD based on ICD-10 | - | YLD | 129,211 |
| Partial EE | |||||||
| Fontana & Rosenheck (1997) | 1997 | USA | QES | Male veterans with PTSD | 45 (3) | CAPS, M-PTSD | 785 |
| McCrone et al., (2005) | 2005 | UK | RCT | Sexually abused female children | - | O-PTSD | 71 |
| Gilbert (2009) | 2009 | USA | QES | Females with co-occurring disorders and histories of abuse victimization | 37 | PTDS | 2,001 |
| Wood et al. (2009) | 2009 | USA | QES | Males with combat-related PTSD based on DSM-IV | - | PCL-M | 12 |
| Greer, Grasso, Cohen, & Webb, (2014) | 2014 | USA | OS | Maltreated children with PTSD symptoms | 12 | UCLA PTSD | 180 |
AU: Australia, BiH: Bosnia and Herzegovina, AQoL-4D: assessment of quality of life instrument, CEA: cost-effectiveness analysis, CHU-9D: child health utility index 9D, COI: cost-of-illness study, CPSS: child posttraumatic symptom scale, CUA: cost-utility analysis, CAPS: clinician-administered PTSD scale, DALY: disability-adjusted life years, DSM: diagnostic and statistical manual of mental disorders, EE. economic evaluation, ES: exploratory study, FYR: Former Yugoslav Republic, HTQ: Harvard trauma questionnaire, ICD: international statistical classification of diseases and related health problems, LSC-R: life stressor checklist-revised, MINI: mini international neuropsychiatric interview, M: model-based study, M-PTSD: Mississippi scale for combat-related PTSD, O-PTSD: Orvaschel’s scales for PTSD, OS: observational study, PC-PTSD: primary care PTSD screen, PCL: PTSD checklist, PCL-C: PTSD checklist–civilian version, PCL-M: PTSD checklist–military version, PTDS: posttraumatic diagnostic scale, PTSD: posttraumatic stress disorder, PTSS: posttraumatic stress syndrome scale, QALY: quality-adjusted life years, QES: quasi-experimental study, QWB: quality of well-being scale, RCT: randomized controlled trial, RPT: randomized preference trial, SD: standard deviation, SRIP: Self Report Inventory for Posttraumatic stress disorder, UCLA PTSD: University of California at Los Angeles Posttraumatic Stress Disorder Reaction Index for DSM-IV, UK: UK, USA: USA, WHODAS 2.0: 12-item short-form version of the World Health Organisation disability assessment schedule 2.0, YLD: years lived with disability.
aPersons with PTSD and persons without PTSD, b Medicaid patients and privately insured patients, c Patients in cognitive-behavioural therapy group and patient group with a brief intervention that focused on breathing retraining and psychoeducation.
3.2.2. Aims and outcomes
The majority of COIs determined excess costs (Chan et al., 2009, 2003; Eekhout et al., 2016; Lamoureux-Lamarche et al., 2016; O’Donnell et al., 2005) or country-specific differences in costs (Priebe et al., 2009, 2010; Sabes-Figuera et al., 2012) (Table 2). The specific populations addressed were war-affected adults (Priebe et al., 2009, 2010; Sabes-Figuera et al., 2012), women with PTSD (Walker et al., 2003), sexually assaulted women (Priebe et al., 2017; Suris et al., 2004), victims of traffic accidents (Chan et al., 2003; O’Donnell et al., 2005) and soldiers (Chan et al., 2009; Eekhout et al., 2016). Two studies focused on the general adult population with PTSD (Ferry et al., 2015; Ivanova et al., 2011). Ten studies reported costs of psychiatric contacts (Chan et al., 2009, 2003; Ferry et al., 2015; Ivanova et al., 2011; O’Donnell et al., 2005; Priebe et al., 2010, 2017; Sabes-Figuera et al., 2012; Suris et al., 2004; Walker et al., 2003), or inpatient and outpatient treatment (Chan et al., 2009, 2003; Ferry et al., 2015; Ivanova et al., 2011; Lamoureux-Lamarche et al., 2016; O’Donnell et al., 2005; Priebe et al., 2009, 2010, 2017; Walker et al., 2003). Nine studies reported costs of drugs (Chan et al., 2009, 2003; Ferry et al., 2015; Ivanova et al., 2011; Lamoureux-Lamarche et al., 2016; Priebe et al., 2009, 2017; Sabes-Figuera et al., 2012; Walker et al., 2003). Only a few studies included costs of non-physician outpatient contacts (Chan et al., 2003; Ferry et al., 2015; O’Donnell et al., 2005; Priebe et al., 2009, 2010), non-medical contacts (Chan et al., 2003; Priebe et al., 2010), rehabilitation (Priebe et al., 2010), and indirect costs (Chan et al., 2003; Ferry et al., 2015; Priebe et al., 2009).
Table 2.
Cost-of-illness per person per year in 2015 US-$ PPP.
|
Direct costs |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Study group | Total | Psychiatric contact* | Inpatient treatment** | Outpatient physician** | Drugs | Non-physician outpatient contact | Rehabilitation | Non-medical contact | Other costs | Indirect costs |
| Excess costs | |||||||||||
| Chan et al. (2003) | PTSD compared to no PTSD | 4,295 | 1,266 | 251 | 1,833 | 69 | 707 | - | 3,334 | - | 5,021a |
| O’Donnell et al. (2005) | PTSD compared to no PTSD/high physical functioning | 19,435 | 1,460 | 7,342 | 4,250 | - | 6,384 | - | - | - | - |
| PTSD compared to no PTSD/low physical functioning | 3,203 | 1,142 | −1,084 | 608 | - | 2,537 | - | - | - | - | |
| Chan et al. (2009) | PTSD compared to no PTSD | 2,579 | 1,648 | −3,933 | 1,670b | 565 | - | - | - | 507 c | - |
| Eekhout et al. (2016) | High SRIP scores compared to lower SRIP scores*** | 521 | - | - | - | - | - | - | - | - | - |
| Lamoureux-Lamarche et al. (2016) | PTSS positive compared to PTSS negative | 1,414 | - | −44 | 413 | 849 | - | - | - | - | - |
| Other cost comparisons | |||||||||||
| Walker et al. (2003) | Low PCL score | 2,316 | 49 | 414 | 1,903 | 225 | - | - | - | - | - |
| Moderate PCL score | 2,504 | 211 | 266 | 2,238 | 338 | - | - | - | - | - | |
| High PCL score | 4,306 | 228 | 643 | 3,663 | 466 | - | - | - | - | - | |
| Suris et al. (2004) | Non-military sexual assault | 23,207 | 6,141 | - | - | - | - | - | - | - | - |
| Military sexual assault | 19,392 | 4,235 | - | - | - | - | - | - | - | - | |
| Non-sexual assault | 13,200 | 2,115 | - | - | - | - | - | - | - | - | |
| Priebe et al. (2009) | Croatia | 9,274 | - | 105 | 526 | 130 | 6 | - | - | - | 8,520d |
| Serbia | 7,110 | - | 1,342 | 359 | 198 | 6 | - | - | - | 5,212d | |
| Germany | 14,802 | - | 2,795 | 2,850 | 563 | 43 | - | - | 19e | 8,532d | |
| UK | 7,648 | - | 365 | 686 | 346 | 383 | - | - | 56e | 5,806d | |
| Priebe et al. (2010) | Belgrade | 590 | 504 | - | 139 | - | - | 6 | 68 | - | - |
| Sarajevo | 198 | 128 | 523 | 2 | - | 3 | 12 | 2 | - | - | |
| Rijeka | 575 | 289 | 111 | 170 | - | 2 | - | 2 | - | - | |
| Zagreb | 485 | 345 | 51 | 37 | - | 2 | 62 | 11 | - | - | |
| Ivanova et al. (2011) | Medicaid | 20,762 | 2,985 | 8,263 | 11,954 | 6,166 | - | - | - | 423 f | - |
| Medicaid/MDD | 19,918 | 1,558 | 7,369 | 11,944 | 5,917 | - | - | - | 324 f | - | |
| Private insurance | 12,134 | 1,246 | 3,971 | 6,445 | 2,682 | - | - | - | 545 f | - | |
| Private insurance/MDD | 11,098 | 853 | 3,408 | 5,587 | 2,815 | - | - | - | 416 f | - | |
| Sabes-Figuera et al. (2012) | UK | 2,337 | 199 | - | - | 383 | - | - | - | 776 g/979e | - |
| Germany | 9,591 | 2,923 | - | - | 239 | - | - | - | 1,123 g/5,305e | - | |
| Italy | 2,486 | 81 | - | - | 59 | - | - | - | 632 g/1,714e | - | |
| Serbia | 835 | 32 | - | - | 9 | - | - | - | 176 g/614e | - | |
| Croatia | 1,096 | 320 | - | - | 50 | - | - | - | 257 g/474e | - | |
| BiH | 875 | 230 | - | - | 54 | - | - | - | 158 g/429e | ||
| FYR Macedonia | 429 | 18 | - | - | 18 | - | - | - | 99 g/289e | ||
| Kosovo | 289 | 41 | - | - | 9.02 | - | - | - | 63 g/171e | ||
| Ferry et al. (2015) | Ireland | 26,991 | 4,328 | 6,715 | 5,037 | 4,631 | 5,666 | - | - | - | 3,032 h |
| Priebe et al. (2017) | Before treatment | 24,594i | 24,594 | 20,643i | 2,242i | 2,643i | - | - | - | - | - |
| After treatment | 9,828i | 9,828 | 4,694i | 2,408i | 2,725i | - | - | - | - | - | |
BiH: Bosnia and Herzegovina, FYR: Former Yugoslav Republic, MDD: major depressive disorder, PCL: PTSD checklist, PPP: purchasing power parities, PTSD: posttraumatic stress disorder, PTSS: posttraumatic stress syndrome, SRIP: Self Report Inventory for PTSD, UK: UK.
* A psychiatric contact is defined as any psychiatric and psychological treatment in an inpatient and outpatient setting, ** without psychiatric contacts if reported separately, *** split at the 95th percentile, a absenteeism costs, b contains non-physician outpatient contact costs, c general medical care costs, d informal care costs, e costs declared as ‘others’, f emergency room costs, g community healthcare costs, h presentism and absenteeism costs, i total costs not differentiated from psychiatric costs.
3.2.3. Summary of results
Mean annual direct excess costs of PTSD ranged from 521 US-$ PPP (Eekhout et al., 2016) to 19,435 US-$ PPP (O’Donnell et al., 2005) per person, which were mainly caused by inpatient treatment (−3,933 US-$ PPP (Chan et al., 2009) to 7,342 US-$ PPP (O’Donnell et al., 2005) per person) and outpatient treatment (413 US-$ PPP (Lamoureux-Lamarche et al., 2016) to 4,250 US-$ PPP (O’Donnell et al., 2005) per person; Table 2). Mean annual indirect excess costs of 5,021 US-$ PPP per person were described by one study (Chan et al., 2003).
In most South Eastern European countries, the mean annual direct excess costs of PTSD per person were low (198 US-$ PPP to 7,110 US-$ PPP) (Priebe et al., 2009, 2010; Sabes-Figuera et al., 2012), whereas excess costs of PTSD in the UK, Germany and Northern Ireland were rather high (2,337 US-$ PPP to 26,991 US-$ PPP) (Ferry et al., 2015; Priebe et al., 2009; Sabes-Figuera et al., 2012). Mean annual indirect costs due to informal care were similar for the UK and Serbia (5,212 US-$ PPP and 5,806 US-$ PPP per person, respectively) as well as for Germany and Croatia (8,532 US-$ PPP and 8,520 US-$ PPP per person, respectively) (Priebe et al., 2009).
Mean annual direct costs of PTSD were negatively influenced by the severity of PTSD symptoms. Costs were almost twice as high for females with severe symptoms, compared with females with mild symptoms (4,206 US-$ PPP vs. 2,316 US-$ PPP per person) (Walker et al., 2003). Furthermore, differences in direct excess costs of PTSD were lower by 512 US-$-PPP per person for soldiers with severe symptoms compared with soldiers with milder symptoms (Eekhout et al., 2016). Mean annual direct costs of PTSD were positively influenced by comorbidities. They were lower for adults with PTSD and major depression than for those without major depression (11,098 to 19,918 US-$ PPP vs. 12,134 to 20,762 US-$ PPP per person) (Ivanova et al., 2011). The influence of treatment on mean annual direct costs of PTSD was ambiguous. Costs were reduced by more than half after treatment of sexually assaulted females with PTSD (24,594 US-$ PPP vs. 9,828 US-$ PPP per person) (Priebe et al., 2017). In contrast, costs of victims of traffic accidents with PTSD without psychiatric treatment were twice as high as of those with psychiatric treatment (24,128 US-$ PPP vs. 12,801 US-$ PPP per person) (Chan et al., 2003).
3.3. Economic evaluations
3.3.1. Study characteristics
The earliest EE was published in 1997 (Fontana & Rosenheck, 1997) and the most recent EE was published in 2019 (Aas et al., 2019) (Table 1). Ten studies were conducted in the USA (Cohen et al., 2017; Domino et al., 2005; Fontana & Rosenheck, 1997; Gilbert, 2009; Greer et al., 2014; Le et al., 2014; Morland et al., 2013; Painter et al., 2017; Slade et al., 2017; Wood et al., 2009), three in Australia (Gospodarevskaya & Segal, 2012; Issakidis et al., 2004; Mihalopoulos et al., 2015) and five in Europe (Aas et al., 2019; Chang et al., 2018; Macdonald et al., 2016; McCrone et al., 2005; Shearer et al., 2018). The sample size of the studies ranged from N = 29 (Shearer et al., 2018) to N = 2,006 (Domino et al., 2005) in trial-based EEs. Nine studies measured costs from a healthcare payer’s perspective (Cohen et al., 2017; Domino et al., 2005; Gilbert, 2009; Gospodarevskaya & Segal, 2012; Issakidis et al., 2004; Mihalopoulos & Chatterton, 2015; Painter et al., 2017; Shearer et al., 2018; Slade et al., 2017). Two studies measured costs from a societal perspective (Chang et al., 2018; Le et al., 2014) and one study from a mental health service provider perspective (McCrone et al., 2005). Six studies did not report the perspective used for cost-measurement (Aas et al., 2019; Fontana & Rosenheck, 1997; Greer et al., 2014; Macdonald et al., 2016; Morland et al., 2013; Wood et al., 2009).
3.3.2. Aims and outcomes
Nine EEs reported the cost-effectiveness of psychotherapies, in particular, TF-CBT (Aas et al., 2019; Gospodarevskaya & Segal, 2012; Macdonald et al., 2016; Mihalopoulos et al., 2015; Shearer et al., 2018; Slade et al., 2017), non-directive counselling (Gospodarevskaya & Segal, 2012), prolonged exposure therapy (Le et al., 2014) and anger management (Morland et al., 2013) (Table 3). No study reported the cost-effectiveness of non-TF-CBT and EMDR. Four studies determined the cost-effectiveness of integrated care, in particular, stepped care (Cohen et al., 2017), telemedicine-based collaborative care (Painter et al., 2017), comprehensive, integrated, trauma-informed and patient-involved services (CIT and CSR-involved services) (Domino et al., 2005), and a multidisciplinary rehabilitation program (Chang et al., 2018). Furthermore, one EE determined the cost-effectiveness of optimal treatment (Issakidis et al., 2004). Partial EEs compared specialized TF-CBT with TAU (Greer et al., 2014), treatment in long-stay PTSD units, with treatment in short-stay PTSD units and treatment in general psychiatric units (Fontana & Rosenheck, 1997), individual psychotherapy with group psychotherapy (McCrone et al., 2005), integrated counselling with usual care (Gilbert, 2009), and virtual reality graded exposure therapy with TAU (Wood et al., 2009). Most EEs included costs of psychiatric contacts (Aas et al., 2019; Cohen et al., 2017; Domino et al., 2005; Fontana & Rosenheck, 1997; Gilbert, 2009; Gospodarevskaya & Segal, 2012; Greer et al., 2014; Issakidis et al., 2004; Le et al., 2014; Macdonald et al., 2016; McCrone et al., 2005; Mihalopoulos et al., 2015; Morland et al., 2013; Painter et al., 2017; Shearer et al., 2018; Slade et al., 2017; Wood et al., 2009), inpatient treatment (Domino et al., 2005; Fontana & Rosenheck, 1997; Gilbert, 2009; Greer et al., 2014; Issakidis et al., 2004; Le et al., 2014; Shearer et al., 2018; Slade et al., 2017), outpatient treatment (Domino et al., 2005; Fontana & Rosenheck, 1997; Gilbert, 2009; Gospodarevskaya & Segal, 2012; Greer et al., 2014; Issakidis et al., 2004; Le et al., 2014; Mihalopoulos et al., 2015; Painter et al., 2017; Shearer et al., 2018; Slade et al., 2017), and drugs (Domino et al., 2005; Gilbert, 2009; Gospodarevskaya & Segal, 2012; Issakidis et al., 2004; Le et al., 2014; Mihalopoulos et al., 2015; Painter et al., 2017; Shearer et al., 2018; Slade et al., 2017).
Table 3.
Cost-effectiveness analyses and cost-utility analyses – included cost categories, incremental effects, and incremental effects and costs and cost-effectiveness in 2015 US-$ PPP per annum.
| Study | Treatment | Time horizon (years) |
Discount rate of costs/effects (%) | Included cost categories |
Incremental costs (US-$ PPP) | Incremental effects | ICER (US-$ PPP per health effect) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Psychiatric contacta | Inpatient treatment | Outpatient treatment | Drugs | Non-physician outpatient contact | Rehabilitation | Non-medical contact | Indirect costs | |||||||
| CEAs/CUAs – Psychotherapy | ||||||||||||||
| Gospodarevskaya & Segal (2012) | Non-directive counselling vs. no treatment | 1 | - | + | - | + | + | - | - | + | - | 1,480 | 0.06 QALYs gained | 24,667 |
| 31 | 5.0/- | 1,515 | 1.02 QALYs gained | 1,485 | ||||||||||
| TF-CBT vs. no treatment | 1 | - | 1,464 | 0.09 QALYs gained | 16,263 | |||||||||
| 31 | 5.0/- | 1,507 | 1.28 QALYs gained | 1,177 | ||||||||||
| TF-CBT + SSRI vs. no treatment | 1 | - | 1,617 | 0.10 QALYs gained | 16,170 | |||||||||
| 31 | 5.0/- | 1,632 | 1.34 QALYs gained | 1,218 | ||||||||||
| TF-CBT vs. non-directive counselling | 1 | - | −16 | 0.03 QALYs gained | Dominant | |||||||||
| 31 | 5.0/- | −20 | 0.20 QALYs gained | Dominant | ||||||||||
| TF-CBT + SSRI vs. non-directive counselling | 1 | - | −137 | 0.04 QALYs gained | Dominant | |||||||||
| 31 | 5.0/- | −105 | 0.26 QALYs gained | Dominant | ||||||||||
| TF-CBT + SSRI vs. TF-CBT | 1 | - | 125 | 0.01 QALYs gained | 12,502 | |||||||||
| 31 | 5.0/- | 124 | 0.06 QALYs gained | 2,071 | ||||||||||
| Morland et al. (2013) | CVT anger management vs. in-person anger management | Varying | - | + | - | - | - | - | - | - | - | −745 | 5%/15%/18% reduction on NAS-T/T-ANG/AEI score | Dominantb |
| Le et al. (2014) | Prolonged exposure therapy vs. sertraline | 1 | - | + | + | + | + | - | - | + | + | −274 | 0.06 QALYs gained | Dominant |
| Choice of treatment vs. no choice of treatment | −1,907 | 0.01 QALYs gained | Dominant | |||||||||||
| Mihalopoulos et al. (2015) | TF-CBT vs. TAU (adults) | 5 | 3.0/3.0 | + | - | + | + | + | - | - | - | 57,914 | 4.40 QALYs gained | 13,162 |
| TF-CBT vs. TAU (children and adolescents) | 622 | 0.09 QALYs gained | 6,912 | |||||||||||
| SSRI vs. TAU (adults who are prescribed medication) | 858 | 3.70 QALYs gained | 232 | |||||||||||
| Macdonald et al. (2016) | TF-CBT vs. TAU | 1 | - | + | - | - | - | - | - | - | - | 2015 | 0.30 point reduction of SMD psychological distress/mental health | 6,502 |
| Slade et al. (2017) | TF-CBT vs. breathing retraining and psychoeducation | 1 | - | + | + | + | + | + | - | + | - | 4,330 | 11% additional PTSD remission | 39,366 |
| Shearer et al. (2018) | TF-CBT vs. TAU | 3 | 3.5/3.5 | + | + | + | + | + | - | + | - | 139 | 0.04 QALYs gained | 3,159 |
| Aas et al. (2019) | TF-CBT vs. TAU | 2 | - | + | - | - | + | - | + | + | - | −150 | 0.04 QALYs gained | Dominant |
| CEAs/CUAs – Integrated care | ||||||||||||||
| Domino et al. (2005) | CIT and CSR-involved services vs. TAU | 0,5 | - | + | + | + | + | - | - | + | - | −19 | 38% reduction on PSS score | Dominant |
| Cohen et al. (2017) | Stepped care + non-TF-CBT vs. TAU | 10 | 3.0/3.0 | + | - | - | - | - | - | - | - | 16 | 0.00 DALYs averted | 3,319 |
| 20.04 additional PTSD-free days | 1 | |||||||||||||
| Painter et al. (2017) | Telemedicine-based collaborative care vs. enhanced TAU | 1 | - | + | - | + | + | - | - | - | - | 2,605 | 0.01 QALYs gained | 193,781 |
| Chang et al. Chang et al. (2018) | Multidisciplinary rehabilitation programmec vs. waiting list + multidisciplinary rehabilitation programme | 1.5 | 3.5/3.5 | - | - | - | - | - | + | - | + | 1,301d | 0.10 QALYs gainede | 13,421 |
| CEAs/CUAs – Other treatment | ||||||||||||||
| Issakidis et al. (2004) | Optimal treatmentf vs. TAU | 1 | - | + | + | + | + | - | - | + | - | −80 | 0.02 YLD averted | Dominant |
| Partial EEs | ||||||||||||||
| Fontana & Rosenheck (1997) | Treatment in long-stay PTSD units vs. treatment in short-stay PTSD units | 1 | - | + | + | + | - | - | - | - | - | 29,949 | 3.6/−3.2 point reduction on CAPS score/M-PTSD score | - |
| Treatment in long-stay PTSD units vs. treatment in general psychiatric units | 23,100 | 7.5/−1.8 point reduction on CAPS score/M-PTSD score | - | |||||||||||
| Treatment in general psychiatric units vs. treatment in short-stay PTSD units | 6,849 | −3.9/−1.4 point reduction on CAPS score/M-PTSD score | - | |||||||||||
| McCrone et al. (2005) | Individual psychotherapy vs. group psychotherapy | Varying | - | + | - | - | - | - | - | - | - | 2,207 | Similar effective | - |
| Gilbert, (2009) | Integrated counselling vs. TAU | 1 | - | + | + | + | + | + | + | + | + | −9,405 g | Greater improvement in PTSD symptoms | - |
| Wood et al. (2009) | Virtual reality graded exposure therapy vs. TAU | 10 weeks | - | + | - | - | - | - | - | - | - | −125,730 | More effective | - |
| Greer et al. (2014) | TF-CBT vs. TAU | 1 | - | + | + | + | - | + | - | - | - | −104,737 | Greater reduction in post-traumatic stress | - |
AEI: Anger Expression Index subscale of State-Trait Anger Expression Inventory-2, CBT: cognitive-behavioural therapy, CIT: comprehensive, integrated, trauma informed, CSR: consumer/survivor/recovering person, CVT: clinical video teleconferencing, DALY: disability-adjusted life year, EE: economic evaluation, NAS-T: Novaco Anger Scale Total, PPP: purchasing power parities, PSS: post-traumatic stress symptom scale, CAPS: clinician-administered PTSD scale, HTQ: Harvard trauma questionnaire, ICER: incremental cost-effectiveness ratio, QALY: quality-adjusted life year, SMD: standard mean difference, SSRI: selective serotonin reuptake inhibitor, T-ANG: Trait Anger subscale of State-Trait Anger Expression Inventory-2, TAU: treatment as usual; TF-CBT: trauma focused-cognitive-behavioural therapy, YLD: years lived with disability.
aPsychiatric contact is defined as any psychiatric and psychological treatment in an inpatient and outpatient setting, b the cost-effectiveness analysis was based on a non-inferiority randomized controlled trial, c the multidisciplinary rehabilitation programme consisted of physiotherapy, biofeedback-supported psychotherapy and social support, d the incremental costs were reported as mean costs of the intervention group and control group, e the incremental effect was reported as mean QALY of the intervention group and control group, f optimal treatment was not further specified by the authors, g females with moderate to severe PTSD.
3.3.3. Summary of results
3.3.3.1. Economic evaluations of psychotherapies for children and adolescents
In studies with a time horizon of three or less than 3 years, TF-CBT for children and adolescents with PTSD was dominant compared with TAU/no treatment (Aas et al., 2019). The ICER of TF-CBT was 16,263 US-$ PPP (Gospodarevskaya & Segal, 2012) per QALY gained (Table 3). Furthermore, in a study with a time horizon of 1 year, the ICER of TF-CBT compared with TAU was 6,502 US-$ PPP per point reduction on a symptom scale (Macdonald et al., 2016). In studies with a time horizon of more than 3 years, the ICER ranged from 1,177 US-$ PPP (Gospodarevskaya & Segal, 2012) to 3,159 US-$ PPP (Shearer et al., 2018) per QALY gained. Furthermore, one partial EE reported incremental costs of −104,737 US-$ PPP and a greater reduction in post-traumatic stress of TF-CBT compared with TAU (Greer et al., 2014).
Furthermore, the ICER of TF-CBT+SSRI compared with no treatment was 16,170 US-$ PPP (1,218 US-$ PPP) per QALY gained in a study with a time horizon of 1 year (31 years) (Gospodarevskaya & Segal, 2012). In the same study, the ICER of non-directive counselling compared with no treatment was 24,667 US-$ PPP (1,485 US-$ PPP) per QALY gained (Gospodarevskaya & Segal, 2012). One partial EE reported incremental costs of 2,207 US-$ PPP and similar effectiveness of individual psychotherapy compared with group psychotherapy (McCrone et al., 2005).
3.3.3.2. Economic evaluations of psychotherapies for adults
The ICER of TF-CBT compared with TAU for adults with PTSD was 13,162 US-$ PPP per QALY gained (Mihalopoulos et al., 2015). The ICER of TF-CBT compared with breathing retraining and psychoeducation was 39,366 US-$ PPP per additional PTSD remission (Slade et al., 2017). Furthermore, the use of clinical video teleconferencing (CVT) anger management was dominant compared with in-person anger management treatment for male veterans with PTSD and moderate to severe anger problems (Morland et al., 2013). One partial EE reported incremental costs of −125,730 US-$ PPP and a greater effectiveness of virtual reality graded exposure therapy compared with TAU (Wood et al., 2009).
3.3.3.3. Economic evaluations of integrated care and other treatments for adults
CIT and CSR-involved services for physically and/or sexually abused females with mental health and substance use disorders were dominant compared with TAU (Domino et al., 2005). The ICER of telemedicine-based collaborative care compared with enhanced TAU for veterans with PTSD was 193,781 US-$ PPP per QALY gained (Painter et al., 2017). Furthermore, optimal treatment was dominant compared with TAU (Issakidis et al., 2004). One partial EE reported incremental costs of −9,405 US-$ PPP and greater improvement in symptoms of integrated counselling compared with TAU for veterans with PTSD (Gilbert, 2009).
3.4. Quality assessment
Based on the COI quality checklist, except for one good-quality COI (Lamoureux-Lamarche et al., 2016), the COIs were of low or moderate quality, with 22% to 50% and 63% to 75% fulfilment of criteria, respectively (Table 4) (Chan et al., 2009, 2003; Eekhout et al., 2016; Ferry et al., 2015; Ivanova et al., 2011; Lamoureux-Lamarche et al., 2016; O’Donnell et al., 2005; Priebe et al., 2009, 2010, 2017; Sabes-Figuera et al., 2012; Suris et al., 2004; Walker et al., 2003). Most of the included trial-based and model-based EEs were of moderate to good quality based on the CHEC list and the ISPOR questionnaire, and fulfilled 53% to 95% and 67% to 87% of the particular criteria, respectively (Tables 5 and 6) (Aas et al., 2019; Cohen et al., 2017; Domino et al., 2005; Fontana & Rosenheck, 1997; Gilbert, 2009; Gospodarevskaya & Segal, 2012; Le et al., 2014; McCrone et al., 2005; Mihalopoulos et al., 2015; Painter et al., 2017; Shearer et al., 2018; Slade et al., 2017). All EEs with a time horizon longer than 12 months applied a discount rate to measured costs and effects (Chang et al., 2018; Cohen et al., 2017; Gospodarevskaya & Segal, 2012; Mihalopoulos et al., 2015; Shearer et al., 2018) except for one EE (Aas et al., 2019). Overall, the quality of full EEs was better than the quality of partial EEs according to the CHEC list (71% vs. 49%).
Table 4.
Quality assessment of cost-of-illness-studies according to the adapted COI quality checklist by Schirr-Bonnans et al. (2017).
| Item of quality assessment |
Excess costs |
Cost comparisons based on (sub-)groups |
Studies that fulfilled criterion (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chan et al. (2003) | O’Donnell et al. (2005) | Chan et al. (2009) | Eekhout et al. (2016) | Lamoureux-Lamarche et al. (2016) | Walker et al. (2003) | Suris et al. (2004) | Priebe et al. (2009) | Priebe et al. (2010) | Ivanova et al. (2011) | Sabes-Figuera et al. (2012) | Ferry et al. (2015) | Priebe et al. (2017) | ||
| Was a clear definition of the illness given? | (✓) | ✓ | (✓) | − | ✓ | ✓ | ✓ | ✓ | ✓ | (✓) | − | (✓) | ✓ | 54 |
| Was the epidemiological approach described? | (✓) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | (✓) | ✓ | (✓) | (✓) | (✓) | ✓ | 62 |
| Was the perspective described? | − | − | − | − | ✓ | ✓ | − | − | − | ✓ | − | − | − | 23 |
| Were the different types of costs described? | ✓ | ✓ | ✓ | − | ✓ | ✓ | − | ✓ | (✓) | ✓ | (✓) | ✓ | ✓ | 69 |
| Were activity data sources described? | ✓ | − | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 92 |
| Was cost valuation appropriately described? | − | − | (✓) | (✓) | ✓ | (✓) | (✓) | ✓ | − | (✓) | ✓ | ✓ | ✓ | 38 |
| Was cost discounting provided? | − | − | N/A | − | N/A | N/A | − | N/A | N/A | N/A | N/A | N/A | N/A | 0 |
| Were the major assumptions tested in a sensitivity analysis? | − | − | − | (✓) | − | − | − | (✓) | − | − | (✓) | − | − | 0 |
| Was the presentation of study results consistent with the objective and the methodology of the study? Were costs sufficiently disaggregated? | ✓ | ✓ | ✓ | (✓) | ✓ | ✓ | ✓ | ✓ | (✓) | ✓ | ✓ | ✓ | ✓ | 85 |
| Items fulfilled (%) | 33 | 44 | 50 | 22 | 88 | 75 | 44 | 63 | 38 | 50 | 38 | 50 | 75 | 51 |
[✓] Item was fulfilled without any limitation, [(✓)] item was partially fulfilled, [−] item was not fulfilled, [N/A] not applicable.
COI: cost-of-illness study
Table 5.
Quality assessment of trial-based economic evaluations according to the CHEC-list (Evers et al., 2005).
| Item of quality assessment | Psychotherapy |
Integrated Care |
Partial EEs |
Studies that fulfilled criterion (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Morland et al. (2013) | Le et al. (2014) | Slade et al. (2017) | Shearer et al. (2018) | Aas et al. (2019) | Domino et al. (2005) | Painter et al. (2017) | Chang et al. (2018) | Fontana & Rosenheck (1997) | McCrone et al. (2005) | Gilbert (2009) | Wood et al. (2009) | Greer et al. (2014) | ||
| Clearly described study population | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Clearly described competing alternatives | − | ✓ | ✓ | ✓ | ✓ | − | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 85 |
| Well-defined research question | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Appropriate economic study design | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | − | − | − | − | − | 62 |
| Appropriate time horizon | − | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | − | ✓ | 85 |
| Appropriate perspective | − | ✓ | − | − | ✓ | − | − | ✓ | − | − | ✓ | − | − | 31 |
| Important and relevant costs identified | − | ✓ | ✓ | ✓ | − | ✓ | ✓ | − | − | − | ✓ | − | − | 46 |
| Costs measured appropriately | − | ✓ | ✓ | ✓ | ✓ | ✓ | − | − | ✓ | ✓ | ✓ | − | ✓ | 69 |
| Costs valued appropriately | ✓ | ✓ | ✓ | − | ✓ | ✓ | − | − | ✓ | ✓ | ✓ | − | − | 62 |
| Important and relevant outcomes identified | ✓ | ✓ | ✓ | − | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | − | 85 |
| Outcomes measured appropriately | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | − | ✓ | ✓ | ✓ | ✓ | − | 85 |
| Outcomes valued appropriately | − | ✓ | ✓ | − | ✓ | − | ✓ | − | − | − | − | − | − | 31 |
| Incremental analysis performed | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | − | − | − | − | − | − | 54 |
| Costs and outcomes discounted appropriately | − | ✓ | ✓ | ✓ | − | ✓ | ✓ | ✓ | ✓ | − | ✓ | − | ✓ | 69 |
| Appropriate sensitivity analysis | − | ✓ | ✓ | ✓ | ✓ | ✓ | − | − | − | − | − | − | − | 31 |
| Conclusion follow the data reported | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | − | ✓ | ✓ | ✓ | − | − | 77 |
| Study discusses the generalizability | − | ✓ | ✓ | ✓ | − | ✓ | ✓ | ✓ | − | − | − | ✓ | − | 54 |
| Article indicates no potential conflict of interest | ✓ | ✓ | ✓ | ✓ | − | ✓ | ✓ | − | − | ✓ | − | ✓ | ✓ | 69 |
| Ethical and distributional issues discussed appropriately | − | − | − | − | − | − | − | − | − | − | − | − | − | 0 |
| Items fulfilled (%) | 47 | 95 | 89 | 74 | 74 | 79 | 74 | 47 | 53 | 53 | 63 | 37 | 37 | 62 |
[✓] Item was fulfilled without any limitation, [−] item was not fulfilled.
CHEC: Consensus on Health Economic Criteria, EE: economic evaluation.
Table 6.
Quality assessment of model-based economic evaluations according to the ISPOR questionnaire (Jaime Caro et al., 2014).
| Item of quality assessment | Psychotherapy |
Integrated Care |
Other |
Studies that fulfilled criterion (%) | |||
|---|---|---|---|---|---|---|---|
| Gospodarevskaya & Segal (2012) | Mihalopoulos et al. (2015) | Macdonald et al. (2016) | Shearer et al. (2018) | Cohen et al. (2017) | Issakidis et al. (2004) | ||
| Population relevant | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Critical interventions missing | ✓ | ✓ | ✓ | ✓ | ✓ | − | 83 |
| Relevant outcomes missing | ✓ | ✓ | − | ✓ | ✓ | ✓ | 83 |
| Context applicable | ✓ | ✓ | − | ✓ | − | − | 50 |
| External validation of the model sufficient | ✓ | ✓ | − | − | ✓ | − | 50 |
| Internal validation of the model sufficient | − | − | − | − | − | − | 0 |
| Face validity sufficient | ✓ | ✓ | − | − | ✓ | − | 50 |
| Design of the model adequate | ✓ | − | − | − | ✓ | − | 33 |
| Data used in populating the model suitable | − | ✓ | ✓ | − | − | ✓ | 50 |
| Analysis performed using the model adequate | ✓ | ✓ | − | ✓ | ✓ | ✓ | 83 |
| Effects of uncertainty adequately assessed | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Reporting of the model adequate | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Interpretation of results fair and balanced | − | ✓ | − | ✓ | − | − | 33 |
| Potential conflict of interest | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | 100 |
| Conflicts of interest addressed | ✓ | ✓ | − | ✓ | ✓ | − | 67 |
| Items fulfilled (%) | 80 | 87 | 40 | 67 | 73 | 47 | 64 |
[✓] Item was fulfilled, [−] item was not fulfilled, [?] can’t answer item fulfilment.
ISPOR: International Society for Pharmacoeconomics and Outcomes Research.
4. Discussion
The aim of this study was to systematically review the economic aspects of PTSD without restrictions on the sample population, traumatic experience or interventions. COIs revealed a high economic burden associated with high direct costs of PTSD. In particular, costs of outpatient treatment, non-physician outpatient contacts and psychiatric contacts for persons with PTSD were high. Costs of drugs and rehabilitation were comparatively lower. An increase in costs of psychiatric contacts was caused by increased healthcare utilisation (Chan et al., 2009, 2003; Lamoureux-Lamarche et al., 2016; O’Donnell et al., 2005). Even though several studies showed a significant increase of outpatient treatment costs induced by PTSD (Chan et al., 2009, 2003; Lamoureux-Lamarche et al., 2016), the difference in outpatient treatment costs between persons with and without PTSD was not statistically significant (Chan et al., 2009, 2003).
Results for excess inpatient treatment costs of PTSD varied. Three studies (Chan et al., 2009; Lamoureux-Lamarche et al., 2016; O’Donnell et al., 2005) reported negative excess inpatient treatment costs, whereas two studies (Chan et al., 2003; O’Donnell et al., 2005) reported positive excess costs. However, differences in costs of inpatient treatment were not statistically significant in two of those studies (Chan et al., 2009, 2003). Overall, heterogeneous results of costs of inpatient treatment may be caused by the low quality of COIs included in this review. For example, causes of high healthcare costs of PTSD, as well as discrepancies between reported costs and healthcare utilisation, were not discussed by any COI.
In line with the costs of other mental disorders, the mean annual direct costs of PTSD were lower in most South Eastern European countries compared with other European countries, like the UK or Germany (Gustavsson et al., 2011). These higher costs might have been caused by differences in wages or healthcare spending between those countries. For the South Eastern European countries of Slovenia, Hungary and the Slovak Republic, wages and healthcare spending were reported to be below 30.000 US-$ PPP and 2.000 US-$ PPP per person, respectively (Organisation for Economic Co-operation and Development. Average Wages 2019, 2019; Organisation for Economic Co-operation and Development. Health spending 2019, 2019). For other European countries, wages were above 40.000 US-$ PPP and annual healthcare spending was above 4.000 US-$ PPP per person (Organisation for Economic Co-operation and Development. Average Wages 2019, 2019; Organisation for Economic Co-operation and Development. Health spending 2019, 2019). In this respect, it can be presumed that in these European countries, mental healthcare has a higher priority within society than in South Eastern European countries.
Direct costs of PTSD for some healthcare systems of European countries, like Germany or Italy (Priebe et al., 2009; Sabes-Figuera et al., 2012), were mainly caused by inpatient treatment. Whereas direct costs of PTSD for the healthcare systems of the USA, the UK or Australia (Chan et al., 2003; Ivanova et al., 2011; O’Donnell et al., 2005; Priebe et al., 2009; Walker et al., 2003) were mainly caused by outpatient treatment. Thus, differences in direct costs of PTSD across countries might also be caused by differing healthcare system structures.
Furthermore, costs of PTSD differed by trauma experience (Priebe et al., 2009, 2010, 2017; Suris et al., 2004) and symptom severity (Eekhout et al., 2016; Walker et al., 2003). Healthcare costs were high, particularly for sexually assaulted women (Priebe et al., 2017; Suris et al., 2004), whose costs were 40% to 60% higher than costs of war-affected adults (Priebe et al., 2009, 2010) and 80% higher than costs of females with early childhood maltreatment (Suris et al., 2004; Walker et al., 2003). However, as no COI included children or adolescents with PTSD, the costs of PTSD in children are still unknown.
Likewise, the costs of PTSD differed by symptom severity (Eekhout et al., 2016; Walker et al., 2003). Thus, treatment of PTSD that was able to improve PTSD symptoms can above reduce direct costs, despite the high costs of psychiatric contacts.
In one study, costs of inpatient treatment were reduced after treatment that was able to improve PTSD symptoms led to a reduction of hospital days (Priebe et al., 2017). Therefore, early diagnosis and treatment of PTSD would be desirable. However, most persons with PTSD feel guilty or are ashamed by the experienced traumatic event; thus, late diagnosis and treatment of PTSD are common (Lee & Daniels, 2008). It is recommended by treatment guidelines for PTSD that TF-CBT is the first-line treatment and EMDR is a second-line treatment for children and adolescents (National Institute for Health and Care Excellence, 2018; Phoenix Australia – Centre for Posttraumatic Mental Health, 2013; Watkins et al., 2018). Literature on cost-effectiveness revealed that TF-CBT and TF-CBT+SSRI were cost-effective compared with TAU or non-directive counselling (Gospodarevskaya & Segal, 2012; Greer et al., 2014; Macdonald et al., 2016; Mihalopoulos et al., 2015; Shearer et al., 2018). Furthermore, TF-CBT+SSRI was cost-effective compared with TF-CBT alone (Gospodarevskaya & Segal, 2012). For children and adolescents, SSRIs were not effective for the treatment of PTSD (Cohen, Mannarino, Perel, & Staron, 2007; Robb, Cueva, Sporn, Yang, & Vanderburg, 2010; Robert et al., 2008; Stoddard et al., 2011) and SSRIs were not recommended by treatment guidelines (National Institute for Health and Care Excellence, 2018; Phoenix Australia – Centre for Posttraumatic Mental Health, 2013; Watkins et al., 2018). However, the current literature review reported that TF-CBT+SSRI was more effective in terms of QALYs gained, compared with TF-CBT alone (Gospodarevskaya & Segal, 2012). Therefore, SSRI might improve health-related quality of life but not PTSD symptoms. To date, the cost-effectiveness of the second-line treatment EMDR, as well as models of integrated care for treatment of children and adolescents with PTSD, has not yet been evaluated.
In general, it is possible that cost-effectiveness of treatment options for children and adolescents depended on the studies’ time horizon. Studies with longer time horizons reported lower ICERs. One example is a model-based EE with a time horizon of 31 years, where the incremental costs remained static compared with the ICER after 1 year, whilst the incremental effects remained constant over time (Gospodarevskaya & Segal, 2012). However, it is not straightforward to conclude from model-based EEs that there is an association between a studies’ time horizon and the cost-effectiveness of treatment options, as long-term incremental effects and costs rather depend on assumptions than on observations.
For adults with PTSD, TF-CBT and EMDR are also guideline-recommended as first and second-line treatment, respectively (National Institute for Health and Care Excellence, 2018; Phoenix Australia – Centre for Posttraumatic Mental Health, 2013; Watkins et al., 2018). Furthermore, SSRIs are recommended for the treatment of comorbid major depression (National Institute for Health and Care Excellence, 2018). Literature on cost-effectiveness revealed that TF-CBT was cost-effective compared with TAU or no treatment, and prolonged exposure therapy was cost-effective compared with pharmacotherapy with sertraline (Le et al., 2014). Furthermore, SSRIs were cost-effective for adults who were prescribed medication (Mihalopoulos et al., 2015). To date, the cost-effectiveness of the second-line treatment EMDR for the treatment of adults with PTSD has not been evaluated. With respect to models of integrated care, it has become apparent that CIT and CSR-involved services stepped care + non-TF-CBT and multidisciplinary rehabilitation programs were cost-effective for the treatment of adults with PTSD, compared with TAU or waiting list (Chang et al., 2018; Cohen et al., 2017; Domino et al., 2005). Telemedicine-based collaborative care, however, was not cost-effective, when compared with TAU (Painter et al., 2017). Models for integrated care were not explicitly recommended by treatment guidelines for PTSD (National Institute for Health and Care Excellence, 2018; Phoenix Australia – Centre for Posttraumatic Mental Health, 2013; Watkins et al., 2018). However, for adults with PTSD and complex needs, such as comorbid psychological disorders or unsafe and unstable personal circumstances (National Institute for Health and Care Excellence, 2018), integrated care might be an adequate and effective alternative to TAU. With integrated care, persons with PTSD may benefit due to the increased ability to address special needs by combining medical, psychological, social and cultural care (Lake & Turner, 2017).
According to the CHEC list, the ISPOR questionnaire and the COI quality checklist, the overall quality of the EEs and COIs included in this review were moderate and low. A large proportion of the EEs did not present the valuation of outcomes appropriately and did not discuss ethical and distributional issues. Model-based EEs often did not adequately describe the design of the model used. Furthermore, in the majority of EEs, results were not interpreted in a fair and balanced manner. No EE conducted an internal validation of the models. Even though the CHEC list and the ISPOR questionnaire are commonly used to address the quality of economic literature, they have some well-known limitations. First, items of the CHEC list and the ISPOR questionnaire address multiple criteria and items are scored as being fulfilled if at least a certain proportion of the criterion was addressed. Therefore, even if a study fulfils most of the items, some important quality aspects of items may not be addressed sufficiently. Second, as both instruments address quality, interpretation of item fulfilment strongly relies on the experience of the assessor. Therefore, the quality of the studies included in the current review was assessed by two authors independently and discrepancies were discussed subsequently. Finally, both the CHEC list and the ISPOR questionnaire do not discriminate between more simple and more complex items.
Policy and decision-makers should further target TF-CBT as first-line treatment for persons with PTSD. It was recommended by treatment guidelines and it was cost-effective compared with TAU and no treatment for children and adults with PTSD. However, further research that addresses the cost-effectiveness of other recommended treatments for persons with PTSD such as EMDR, as well as research that addresses indirect costs of PTSD, is still needed.
Additionally, further research concerning the influence of sociodemographic characteristics, such as age, gender, or the time since trauma experience, on costs of PTSD is needed. Such research could lead to policy implications and recommendations tailored to subgroups of persons with PTSD.
Nevertheless, as the current systematic review revealed that there were differences in costs of PTSD between countries, future economic evaluations and cost analyses should be country-specific, and policy and decision-makers should not merely adopt evidence from research conducted in foreign countries.
5. Strengths and limitations
As PTSD is a major public health problem and no current review of either COIs or EEs of treatments for PTSD was available, the current review is of high relevance for both decision-makers and healthcare practitioners. In order to ensure a high reporting quality, this review has been structured according to current guidelines for health economic reviews (Thielen et al., 2016; van Mastrigt et al., 2016; Wijnen et al., 2016). Furthermore, quality of included COIs and EEs of treatments for PTSD was assessed using established quality checklists (Evers et al., 2005; Jaime Caro et al., 2014; Schirr-Bonnans et al., 2017).
This review has some limitations. First, the systematic literature search used sensitive search terms, thus a high number of studies (n = 1,309) were excluded by the screening of titles and abstracts. Although a sensitive approach for the literature search benefits from a high number of possible suitable articles compared with a more specific approach, a high number of articles had to be screened and a high number of articles had to be excluded. Second, as the methods and settings of studies included in this review differed, comparability and generalizability of results are limited. Third, most of the studies included in this review only reported mean costs without, e.g. confidence intervals, and therefore, the uncertainty of these estimates could not be expressed in this review. Last, the CHEC list, the ISPOR questionnaire and the COI quality checklist to assess the quality of included studies do not account for the integrity of its addressed items.
6. Conclusions
A high economic burden of PTSD has been revealed, especially for sexually assaulted women or individuals with severe symptoms of PTSD. TF-CBT (+SSRI) was cost-effective compared with TAU for the treatment of children and adolescents with PTSD. However, SSRI has not been recommended for children by treatment guidelines for PTSD. Cost-effectiveness of EMDR and integrative care has not yet been evaluated for children and adolescents. For the treatment of adults with PTSD, TF-CBT (+SSRI) and integrative care were cost-effective compared with TAU. Just as for children and adolescents, the cost-effectiveness of EMDR has not yet been evaluated for adults. Because of the overall moderate quality of EEs included in this review, results on the cost-effectiveness varied widely, and for that reason, further EEs of treatments recommended for individuals with PTSD are necessary.
Acknowledgments
We would like to thank the anonymous reviewers who contributed with their useful suggestions to improve the quality of this study.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure statement
The authors declare that they have no conflict of interest.
References
- Aas, E., Iversen, T., Holt, T., Ormhaug, S. M., & Jensen, T. K. (2019). Cost-effectiveness analysis of trauma-focused cognitive behavioral therapy: A randomized control trial among Norwegian Youth. Journal of Clinical Child & Adolescent Psychology, 48, S298–S311. [DOI] [PubMed] [Google Scholar]
- Alonso, J., Angermeyer, M. C., Bernert, S., Bruffaerts, R., Brugha, T. S., ... Vollebergh, W. A. M. (2004). Prevalence of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica. Supplementum, 109(s420), 21–20. doi: 10.1111/j.1600-0047.2004.00327.x [DOI] [PubMed] [Google Scholar]
- Ament, A., & Evers, S. (1993). Cost of illness studies in health care: A comparison of two cases. Health Policy (Amsterdam, Netherlands), 26, 29–42. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- American Psychological Association . (2017). Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. Washington: Author. [Google Scholar]
- Bisson, J. I., Roberts, N. P., Andrew, M., Cooper, R., & Lewis, C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database of Systematic Reviews (Online), CD003388. doi: 10.1002/14651858.CD003388.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunting, B. P., Murphy, S. D., O’Neill, S. M., & Ferry, F. R. (2012). Lifetime prevalence of mental health disorders and delay in treatment following initial onset: Evidence from the Northern Ireland Study of Health and Stress. Psychological Medicine, 42, 1727–1739. [DOI] [PubMed] [Google Scholar]
- Byford, S., Torgerson, D. J., & Raftery, J. (2000). Economic note: Cost of illness studies. BMJ, 320, 1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian agency for Drugs and Technologies in Health . (2012). Day programming for post-traumatic stress disorder: A review of the clinical effectiveness, cost-effectiveness and guidelines. Ottawa: Author. [Google Scholar]
- Canadian Agency for Drugs and Technologies in Health . (2010). Cognitive behavioural therapy for post traumatic stress disorder: A review of the clinical and cost-effectiveness. CADTH Technology Overviews, 1, e0124. [PMC free article] [PubMed] [Google Scholar]
- Chan, A. O., Medicine, M., Air, T. M., & McFarlane, A. C. (2003). Posttraumatic stress disorder and its impact on the economic and health costs of motor vehicle accidents in South Australia. The Journal of Clinical Psychiatry, 64, 175–181. [DOI] [PubMed] [Google Scholar]
- Chan, D., Cheadle, A. D., Reiber, G., Unutzer, J., & Chaney, E. F. (2009). Health care utilization and its costs for depressed veterans with and without comorbid PTSD symptoms. Psychiatric Services, 60, 1612–1617. [DOI] [PubMed] [Google Scholar]
- Chang, W. L., Andersen, C. J., Berisha, B. S., Estrup, O., & Wang, S. J. (2018). Economic evaluation of a bio-psycho-social intervention for comorbid disorders in a traumatized population in post-war Kosovo. Journal of Rehabilitation Medicine, 50(5), 444–450. [DOI] [PubMed] [Google Scholar]
- Cohen, G. H., Tamrakar, S., Lowe, S., Sampson, L., Ettman, C., Linas, B., … Galea, S. (2017). Comparison of simulated treatment and cost-effectiveness of a stepped care case-finding intervention vs usual care for posttraumatic stress disorder after a natural disaster. JAMA Psychiatry (Chicago, Ill.), 74(12), 1251–1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. A., Mannarino, A. P., Perel, J. M., & Staron, V. (2007). A pilot randomized controlled trial of combined trauma-focused CBT and sertraline for childhood PTSD symptoms. Journal of the American Academy of Child & Adolescent Psychiatry, 46(7), 811–819. [DOI] [PubMed] [Google Scholar]
- Domino, M., Morrissey, J. P., Nadlicki-Patterson, T., & Chung, S. (2005). Service costs for women with co-occurring disorders and trauma. Journal of Substance Abuse Treatment, 28(2), 135–143. [DOI] [PubMed] [Google Scholar]
- Drummond, M., Sculpher, M. J., Torrance, G. W., O’Brien, B. J., & Stoddart, G. L. (2005). Methods for the economic evaluation of health care programmes. Oxford, New York: Oxford University Press. [Google Scholar]
- Eekhout, I., Geuze, E., & Vermetten, E. (2016). The long-term burden of military deployment on the health care system. Journal of Psychiatric Research, 79, 78–85. [DOI] [PubMed] [Google Scholar]
- Ehlers, A., Clark, D. M., Hackmann, A., Grey, N., Liness, S., Wild, J., … McManus, F. (2010). Intensive cognitive therapy for PTSD: A feasibility study. Behavioural and Cognitive Psychotherapy, 38, 383–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst, R. (2006). Indirect Costs and Cost-Effectiveness Analysis. Value in Health : The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 9, 253–261. [DOI] [PubMed] [Google Scholar]
- Evers, S., Goossens, M., de Vet, H., van Tulder, M., & Ament, A. (2005). Criteria list for assessment of methodological quality of economic evaluations: Consensus on Health Economic Criteria. International Journal of Technology Assessment in Health Care, 21, 240–245. [PubMed] [Google Scholar]
- Ferry, F. R., Brady, S. E., Bunting, B. P., Murphy, S. D., Bolton, D., & O’Neill, S. M. (2015). The economic burden of PTSD in Northern Ireland. Journal of Traumatic Stress, 28, 191–197. [DOI] [PubMed] [Google Scholar]
- Fontana, A., & Rosenheck, R. (1997). Effectiveness and cost of the inpatient treatment of posttraumatic stress disorder: Comparison of three models of treatment. The American Journal of Psychiatry, 154, 758–765. [DOI] [PubMed] [Google Scholar]
- Frayne, S. M., Seaver, M. R., Loveland, S., Christiansen, C. L., Spiro III, A., Parker, V. A., & Skinner, K. M. (2004). Burden of medical illness in women with depression and posttraumatic stress disorder. Archives of Internal Medicine, 164, 1306–1312. [DOI] [PubMed] [Google Scholar]
- Gilbert, A. R. (2009). Women with co-occurring disorders and histories of abuse: Moderators of treatment effect on service use and costs. Chapel Hill: University of North Carolina. [Google Scholar]
- Gospodarevskaya, E., & Segal, L. (2012). Cadth. Cost-utility analysis of different treatments for post-traumatic stress disorder in sexually abused children. Child and Adolescent Psychiatry and Mental Health, 6, 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greer, D., Grasso, D. J., Cohen, A., & Webb, C. (2014). Trauma-focused treatment in a state system of care: Is it worth the cost? Administration and Policy in Mental Health and Mental Health Services Research, 41(3), 317–323. [DOI] [PubMed] [Google Scholar]
- Gustavsson, A., Svensson, M., Jacobi, F., Allgulander, C., Alonso, J., Beghi, E., … Olesen, J. (2011). Cost of disorders of the brain in Europe 2010. European Neuropsychopharmacology, 21(10), 718–779. [DOI] [PubMed] [Google Scholar]
- Hamberg-van Reenen, H. H., Proper, K. I., & van den Berg, M. (2012). Worksite mental health interventions: A systematic review of economic evaluations. Occupational and Environmental Medicine, 69, 837–845. [DOI] [PubMed] [Google Scholar]
- Hetrick, S. E., Purcell, R., Garner, B., & Parslow, R. (2010). Combined pharmacotherapy and psychological therapies for post traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews (Online), CD007316. doi: 10.1002/14651858.CD007316.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Issakidis, C., Sanderson, K., Corry, J., Andrews, G., & Lapsley, H. (2004). Modelling the population cost-effectiveness of current and evidence-based optimal treatment for anxiety disorders. Psychological Medicine, 34(1), 19–35. [DOI] [PubMed] [Google Scholar]
- Ivanova, J. I., Birnbaum, H. G., Chen, L., Duhig, A. M., Dayoub, E. J., Kantor, E. S., & Phillips, G. A. (2011). Cost of post-traumatic stress disorder vs major depressive disorder among patients covered by medicaid or private insurance. The American Journal of Managed Care, 17, e314–e323. [PubMed] [Google Scholar]
- Jaime Caro, J., Eddy, D. M., Kan, H., Kaltz, C., Patel, B., Eldessouki, R., & Briggs, A. H. (2014). Questionnaire to assess relevance and credibility of modeling studies for informing health care decision making: An ISPOR-AMCP-NPC Good Practice Task Force report. Value in Health, 17, 174–182. [DOI] [PubMed] [Google Scholar]
- Johnston, K., Buxton, M. J., Jones, D. R., & Fitzpatrick, R. (1999). Assessing the costs of healthcare technologies in clinical trials. Health Technology Assessment, 3, 1–76. [PubMed] [Google Scholar]
- Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Kilian, R. (2008). Gesundheitsökonomische evaluation in der psychiatrischen Versorgungsforschung. Prävention Und Gesundheitsförderung, 3, 135–144. [Google Scholar]
- Lake, J., & Turner, M. S. (2017). Urgent need for improved mental health care and a more collaborative model of care. The Permanente Journal, 21, 17–024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamoureux-Lamarche, C., Vasiliadis, H.-M., Preville, M., & Berbiche, D. (2016). Healthcare use and costs associated with post-traumatic stress syndrome in a community sample of older adults: Results from the ESA-Services study. International Psychogeriatrics, 28, 903–911. [DOI] [PubMed] [Google Scholar]
- Le, Q. A., Doctor, J. N., Zoellner, L. A., & Feeny, N. C. (2014). Cost-effectiveness of prolonged exposure therapy versus pharmacotherapy and treatment choice in posttraumatic stress disorder (the Optimizing PTSD Treatment Trial): A doubly randomized preference trial. The Journal of Clinical Psychiatry, 75, 222–230. [DOI] [PubMed] [Google Scholar]
- Lee, K., & Daniels, M. J. (2008). Marginalized models for longitudinal ordinal data with application to quality of life studies. Statistics in Medicine, 27(21), 4359–4380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macdonald, G., Livingstone, N., Hanratty, J., McCartan, C., Cotmore, R., Cary, M., ... Churchill, R. (2016). The effectiveness, acceptability and cost-effectiveness of psychosocial interventions for maltreated children and adolescents: An evidence synthesis. Health Technology Assessment, 20(69), 1–508. doi: 10.3310/hta20690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrone, P., Weeramanthri, T., Knapp, M., Rushton, A., Trowell, J., Miles, G., & Kolvin, I. (2005). Cost-effectiveness of individual versus group psychotherapy for sexually abused girls. Child and Adolescent Mental Health, 10(1), 26–31. [DOI] [PubMed] [Google Scholar]
- Mihalopoulos, C., & Chatterton, M. L. (2015). Economic evaluations of interventions designed to prevent mental disorders: A systematic review. Early Intervention in Psychiatry, 9(2), 85–92. [DOI] [PubMed] [Google Scholar]
- Mihalopoulos, C., Magnus, A., Lal, A., Dell, L., Forbes, D., & Phelps, A. (2015). Is implementation of the 2013 Australian treatment guidelines for posttraumatic stress disorder cost-effective compared to current practice? A cost-utility analysis using QALYs and DALYs. Australian & New Zealand Journal of Psychiatry, 49, 360–376. [DOI] [PubMed] [Google Scholar]
- Molinier, L., Bauvin, E., Combescure, C., Castelli, C., Rebillard, X., Soulie, M., … Grosclaude, P. (2008). Methodological considerations in cost of prostate cancer studies: A systematic review. Value in Health, 11, 878–885. [DOI] [PubMed] [Google Scholar]
- Morland, L. A., Raab, M., Mackintosh, M. A., Rosen, C. S., Dismuke, C. E., Greene, C. J., & Frueh, B. C. (2013). Telemedicine: A cost-reducing means of delivering psychotherapy to rural combat veterans with PTSD. Telemedicine and e-Health, 19, 754–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutyambizi, C., Pavlova, M., Chola, L., Hongoro, C., & Groot, W. (2018). Cost of diabetes mellitus in Africa: A systematic review of existing literature. Globalization and Health, 14, 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence . (2018). Post-traumatic stress disorder. NICE guideline. London: Author. [PubMed] [Google Scholar]
- O’Donnell, M. L., Creamer, M., Elliott, P., & Atkin, C. (2005). Health costs following motor vehicle accidents: The role of posttraumatic stress disorder. Journal of Traumatic Stress, 18, 557–561. [DOI] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development. Average Wages 2019 . (2019). Database: Organisation for Economic Co-operation and Development. Retrieved from https://data.oecd.org/earnwage/average-wages.htm
- Organisation for Economic Co-operation and Development. Health spending 2019 . (2019). Database: Organisation for economic co-operation and development. Retrieved from https://data.oecd.org/healthres/health-spending.htm
- Organisation for Economic Co-operation and Development. Health Statistics 2017 . (2017). Database: Organisation for economic co-operation and development. Retrieved from https://www.oecd.org/els/health-systems/health-data.htm
- Painter, J. T., Fortney, J. C., Austen, M. A., & Pyne, J. M. (2017). Cost-effectiveness of telemedicine-based collaborative care for posttraumatic stress disorder. Psychiatric Services, 68(11), 1157–1163. [DOI] [PubMed] [Google Scholar]
- Phoenix Australia - Centre for Posttraumatic Mental Health . (2013). Australian guidelines for the treatment of acute stress disorder and posttraumatic stress disorder. Melbourne, Victoria: Phoenix Australia. [Google Scholar]
- Priebe, K., Roth, M., Krüger, A., Glöckner-Fink, K., Dyer, A., Steil, R., & Bohus, M. (2017). Psychiatrische Behandlungskosten von Patientinnen mit Posttraumatischer Belastungsstörung nach sexuellem Missbrauch vor und nach stationärer DBT-PTSD. Psychiatrische Praxis, 44, 75–84. [DOI] [PubMed] [Google Scholar]
- Priebe, S., Gavrilovic, J. J., Matanov, A., Franciskovic, T., Knezevic, G., Ljubotina, D., & Schützwohl, M. (2010). Treatment outcomes and costs at specialized centers for the treatment of PTSD after the war in former Yugoslavia. Psychiatric Services, 61, 598–604. [DOI] [PubMed] [Google Scholar]
- Priebe, S., Matanov, A., Jankovic Gavrilovic, J., McCrone, P., Ljubotina, D., Knezevic, G., … Schützwohl, M. (2009). Consequences of untreated posttraumatic stress disorder following war in former Yugoslavia: Morbidity, subjective quality of life, and care costs. Croatian Medical Journal, 50, 465–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabarison, K. M., Bish, C. L., Massoudi, M. S., & Giles, W. H. (2015). Economic evaluation enhances public health decision making. Frontiers in Public Health, 3, 164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rapaport, M. H., Clary, C., Fayyad, R., & Endicott, J. (2005). Quality-of-life impairment in depressive and anxiety disorders. American Journal of Psychiatry, 162(6), 1171–1178. [DOI] [PubMed] [Google Scholar]
- Rice, D. P. (1994). Cost-of-illness studies: Fact or fiction? The Lancet, 344, 1519–1520. [DOI] [PubMed] [Google Scholar]
- Robb, A. S., Cueva, J. E., Sporn, J., Yang, R., & Vanderburg, D. G. (2010). Sertraline treatment of children and adolescents with posttraumatic stress disorder: A double-blind, placebo-controlled trial. Journal of Child and Adolescent Psychopharmacology, 20(6), 463–471. [DOI] [PubMed] [Google Scholar]
- Robert, R., Tcheung, W. J., Rosenberg, L., Rosenberg, M., Mitchell, C., Villarreal, C., & Meyer, W. J. (2008). Treating thermally injured children suffering symptoms of acute stress with imipramine and fluoxetine: A randomized, double-blind study. Burns, 34(7), 919–928. [DOI] [PubMed] [Google Scholar]
- Rothbaum, B. O., Astin, M. C., & Marsteller, F. (2005). Prolonged Exposure versus Eye Movement Desensitization and Reprocessing (EMDR) for PTSD rape victims. Journal of Traumatic Stress, 18, 607–616. [DOI] [PubMed] [Google Scholar]
- Sabes-Figuera, R., McCrone, P., Bogic, M., Ajdukovic, D., Franciskovic, T., Colombini, N., & Caylà, J. A. (2012). Long-term impact of war on healthcare costs: An eight-country study. PloS One, 7, e29603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sareen, J., Cox, B. J., Stein, M. B., Afifi, T. O., Fleet, C., & Asmundson, G. J. (2007). Physical and mental comorbidity, disability, and suicidal behavior associated with posttraumatic stress disorder in a large community sample. Psychosomatic Medicine, 69, 242–248. [DOI] [PubMed] [Google Scholar]
- Schirr-Bonnans, S., Costa, N., Derumeaux-Burel, H., Bos, J., Lepage, B., Garnault, V., … Molinier, L. (2017). Cost of diabetic eye, renal and foot complications: A methodological review. The European Journal of Health Economics, 18, 293–312. [DOI] [PubMed] [Google Scholar]
- Shafie, A. A., Tan, Y. P., & Ng, C. H. (2018). Systematic review of economic burden of heart failure. Heart Failure Reviews, 23, 131–145. [DOI] [PubMed] [Google Scholar]
- Shapiro, F. (1989). Eye movement desensitization: A new treatment for post-traumatic stress disorder. Journal of Behavior Therapy and Experimental Psychiatry, 20, 211–217. [DOI] [PubMed] [Google Scholar]
- Shearer, J., Papanikolaou, N., Meiser-Stedman, R., McKinnon, A., Dalgleish, T., Smith, P., … Byford, S. (2018). Cost-effectiveness of cognitive therapy as an early intervention for post-traumatic stress disorder in children and adolescents: A trial based evaluation and model. Journal of Child Psychology and Psychiatry, 59, 773–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade, E. P., Gottlieb, J. D., Lu, W., Yanos, P. T., Rosenberg, S., Silverstein, S. M., & Mueser, K. T. (2017). Cost-effectiveness of a PTSD intervention tailored for individuals with severe mental illness. Psychiatric Services, 68, 1225–1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon, S. D., & Davidson, J. R. (1997). Trauma: Prevalence, impairment, service use, and cost. The Journal of Clinical Psychiatry, 58, 5–11. [PubMed] [Google Scholar]
- Statistisches Bundesamt . (2019). Krankheitskosten nach Alter, Geschlecht, ICD10 (ab 2015). Database: Gesundheitsberichterstattung des Bundes. Retrieved from http://www.gbe-bund.de/gbe10/express.prc_expr?p_aid=90248447&p_uid=gast&p_sprachkz=D&p_var=0&nummer=63&p_indsp=&p_ityp=H&p_hlpnr=2&p_lfd_nr=1&p_sprache=D&p_news=&p_janein=J
- Stoddard, F. J., Jr., Luthra, R., Sorrentino, E. A., Saxe, G. N., Drake, J., Chang, Y., & Sheridan, R. L. (2011). A randomized controlled trial of sertraline to prevent posttraumatic stress disorder in burned children. Journal of Child and Adolescent Psychopharmacology, 21(5), 469–477. [DOI] [PubMed] [Google Scholar]
- Stokes, J., Checkland, K., & Kristensen, S. R. (2016). Integrated care: Theory to practice. Journal of Health Services Research & Policy, 21, 282–285. [DOI] [PubMed] [Google Scholar]
- Suris, A., Lind, L., Kashner, T. M., Borman, P. D., & Petty, F. (2004). Sexual assault in women veterans: An examination of PTSD risk, health care utilization, and cost of care. Psychosomatic Medicine, 66, 749–756. [DOI] [PubMed] [Google Scholar]
- Thielen, F. W., Van Mastrigt, G., Burgers, L. T., Bramer, W. M., Majoie, H., Evers, S., & Kleijnen, J. (2016). How to prepare a systematic review of economic evaluations for clinical practice guidelines: Database selection and search strategy development (part 2/3). Expert Review of Pharmacoeconomics & Outcomes Research, 16(6), 705–721. doi: 10.1080/14737167.2016.1246962 [DOI] [PubMed] [Google Scholar]
- VA/DoD Clinical Practice Guideline Working Group . (2017). VA/DoD Clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. Washington, DC: VA Office of Quality and Performance. [Google Scholar]
- van Mastrigt, G. A., Hiligsmann, M., Arts, J. J., Broos, P. H., Kleijnen, J., Evers, S. M., & Majoie, M. H. J. M. (2016). How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: A five-step approach (part 1/3). Expert Review of Pharmacoeconomics & Outcomes Research, 16, 689–704. [DOI] [PubMed] [Google Scholar]
- van Zelst, W. H., de Beurs, E., Beekman, A. T., van Dyck, R., & Deeg, D. D. (2006). Well-being, physical functioning, and use of health services in the elderly with PTSD and subthreshold PTSD. International Journal of Geriatric Psychiatry, 21(2), 180–188. [DOI] [PubMed] [Google Scholar]
- Walker, E. A., Katon, W., Russo, J., Ciechanowski, P., Newman, E., & Wagner, A. W. (2003). Health care costs associated with posttraumatic stress disorder symptoms in women. Archives of General Psychiatry, 60, 369–374. [DOI] [PubMed] [Google Scholar]
- Wang, L., Si, L., Cocker, F., Palmer, A. J., & Sanderson, K. (2018). A systematic review of cost-of-illness studies of multimorbidity. Applied Health Economics and Health Policy, 16, 15–29. [DOI] [PubMed] [Google Scholar]
- Watkins, L. E., Sprang, K. R., & Rothbaum, B. O. (2018). Treating PTSD: A review of evidence-based psychotherapy interventions. Frontiers in Behavioral Neuroscience, 12, 258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wijnen, B., Van Mastrigt, G., Redekop, W. K., Majoie, H., De Kinderen, R., & Evers, S. (2016). How to prepare a systematic review of economic evaluations for informing evidence-based healthcare decisions: Data extraction, risk of bias, and transferability (part 3/3). Expert Review of Pharmacoeconomics & Outcomes Research, 16, 723–732. [DOI] [PubMed] [Google Scholar]
- Wong, C. K. H., Liao, Q., Guo, V. Y. W., Xin, Y., & Lam, C. L. K. (2017). Cost-effectiveness analysis of vaccinations and decision makings on vaccination programmes in Hong Kong: A systematic review. Vaccine, 35, 3153–3161. [DOI] [PubMed] [Google Scholar]
- Wood, D. P., Murphy, J., McLay, R., Koffman, R., Spira, J., Obrecht, R. E., & Wiederhold, B. K. (2009). Cost effectiveness of virtual reality graded exposure therapy with physiological monitoring for the treatment of combat related post traumatic stress disorder. Studies in Health technology and Informatics, 144, 223–229. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Organisation for Economic Co-operation and Development. Average Wages 2019 . (2019). Database: Organisation for Economic Co-operation and Development. Retrieved from https://data.oecd.org/earnwage/average-wages.htm
- Organisation for Economic Co-operation and Development. Health spending 2019 . (2019). Database: Organisation for economic co-operation and development. Retrieved from https://data.oecd.org/healthres/health-spending.htm
- Organisation for Economic Co-operation and Development. Health Statistics 2017 . (2017). Database: Organisation for economic co-operation and development. Retrieved from https://www.oecd.org/els/health-systems/health-data.htm


