Abstract
Background: Chronic pain in the region of varicocele embolization is not well described and can be a challenging symptom to manage, with limited options for treatment after failing conservative measures. It is important to counsel patients of this potential complication when determining the best option for varicocele repair. To our knowledge, there are no reported cases of gonadal vein excision for chronic abdominal pain after coil embolization.
Case Presentation: A 63-year-old Caucasian male presented to our urology clinic after coil embolization. His testicular pain resolved but he reported new left-sided abdominal pain after coil embolization for a large left varicocele. After failing conservative measures including nonsteroidal anti-inflammatory drugs, antibiotics, and prednisone, he was referred for further work-up and to discuss treatment options. On presentation, the patient reported pain on the left side of his abdomen consistent with the location of gonadal vein. After extensive counseling that surgical removal may not alleviate his pain, robotic gonadal vein excision was offered, and the patient elected to proceed. Intraoperatively, the coils were easily seen through the wall of the vessel. This segment of the gonadal vein containing the coil was excised in its entirety. The patient was discharged on postoperative day 1 with only nonsteroidal pain medications. Six weeks postoperatively, the patient reported no complications, and almost complete resolution of his preoperative pain.
Conclusions: To our knowledge, this is the first case report demonstrating the surgical removal of the gonadal vein for treatment of chronic abdominal pain after varicocele embolization. After failing conservative measures, this may present another viable treatment option to address this difficult complication in a select group of patients.
Keywords: varicocele, chronic pain, coil embolization, minimally invasive surgery, robotics
Introduction and Background
Varicocele is a common anatomic variant observed in ∼15% of men.1 Although often varicoceles are asymptomatic, they are known to impair spermatogenesis and may also cause pain. In either instance, treatment options for varicocele include surgical ligation or endovascular coil embolization.
Coil embolization for varicocele was first described by Lima et al. in 1978 and has demonstrated efficacy in treating infertility or pain because of varicocele.1,2 In a retrospective review, 87% of 154 patients had complete resolution of pain after >3 years of follow-up after varicocele embolization, making this a safe and effective choice in management.3 Although varicocele recurrence is a known side effect of coil embolization with rates ranging from 0% to 24% in the literature, other adverse outcomes, such as pain after coil embolization, are not as well described and can be a challenging symptom to manage.1
In this report, we describe a case of new onset chronic abdominal pain in the region of varicocele embolization, with resolution of the pain after surgical resection of the embolized left gonadal vein.
Presentation of Case
A 63-year-old Caucasian male presented after coil embolization to our urology clinic with left-sided periumbilical pain. Before embolization, he had a history of long standing left scrotal pain that progressively worsened over the course of the day and was diagnosed with a grade 3 left varicocele. He was referred to interventional radiology and coil embolization was performed. The venogram revealed a moderate-to-large left gonadal vein with valve incompetence and a large amount of reflux into numerous left-sided scrotal varices. Per report, a single 0.035″ 8 cm tornado coil was placed with seven separate 0.035″ 10 × 14 mm Cook Nester coils placed within and an additional 7 8 × 20 mm Cook Nester coil within the vein, resulting in embolization of the left gonadal vein from near the inguinal canal up to the left renal vein (Fig. 1).
FIG. 1.

Preoperative CT-scout film showing the left gonadal vein embolic coils.
His testicular pain resolved but he reported new left-sided abdominal pain shortly after embolization that persisted despite several conservative measures, including nonsteroidal anti-inflammatory drugs, antibiotics, and prednisone. After these interventions failed, he was referred to our urology clinic for further work-up and to discuss treatment options. On presentation, the patient reported 6 to 9/10 pain on the left side of his abdomen consistent with the location of the gonadal vein, left of the umbilicus extending vertically along his abdomen. After extensive counseling that surgical removal may not alleviate his pain, robotic gonadal vein excision was offered, and the patient elected to proceed.
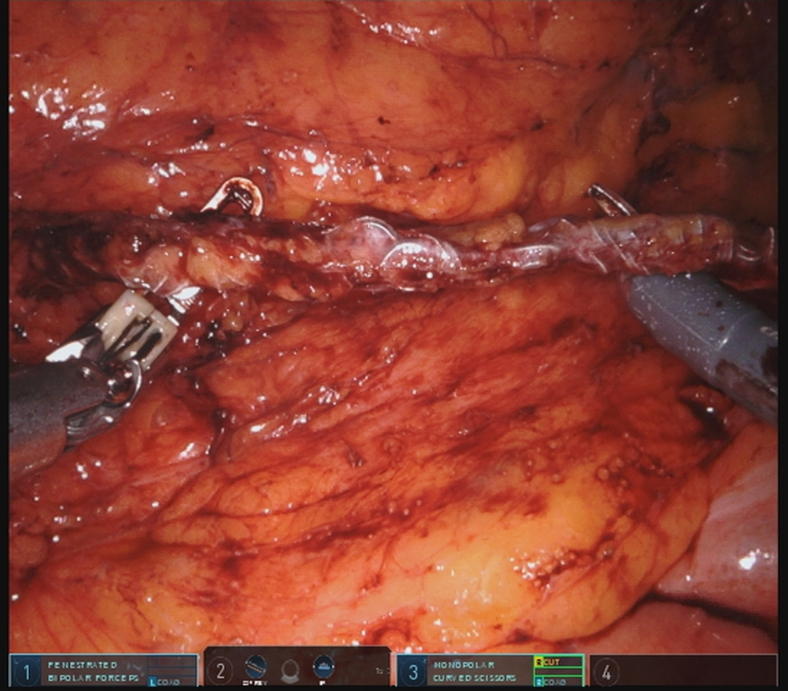
The patient was positioned in right lateral decubitus and a transperitoneal laparoscopic-assisted robotic approach was utilized. After reflecting the colon, the gonadal vein was easily identified by the visible endovascular coils seen transluminally. Although mild edema of the surrounding tissue in the retroperitoneum was noted, extensive inflammation was not present, leading to an uncomplicated dissection. The length of the vein was dissected from near its drainage into the left renal vein, all the way just proximal to the internal ring (Fig. 2), then clipped and resected. The total robot dock time for the case was 54 minutes with negligible blood loss. The patient was discharged on postoperative day 1 with only nonopioid pain medications. Pathology analysis returned with a report of foreign body giant cell reaction. The gross specimen is shown in Figure 3.
FIG. 2.
Intraoperative laparoscopic view of the isolated left gonadal vein.
FIG. 3.
Gross specimen—left gonadal vein.
Six weeks postoperatively, the patient reported no complications, and almost complete resolution of his preoperative pain.
Discussion and Literature Review
In this case report, we describe the resolution of postembolization pain after surgical resection of the coil embolized vein. To our knowledge, coil-related pain and its resolution with surgical excision have not previously been described.
Complications after embolization are rare and thus scarcely reported in the literature. These include vein perforation and proximal coil migration, leading to the left renal vein, even to the vena cava or pulmonary circulatory system.4 In addition, hydrocele and epididymitis are reported at 0% to 12% and 3%, respectively.1 Persistence of chronic scrotal pain ranges from 0% to 13%, depending on study and follow-up duration.1
Interestingly, the patient reported resolution of his left-sided testis pain postembolization, with migration of his pain to the periumbilical region. The rationale for the surgery stemmed from the possibility that his new onset periumbilical pain was caused by his endovascularly placed coils. Although acute periprocedure pain is described and expected in many cases, this concept of chronic “pain from endovascular coils” has never been described previously in the literature, specifically for varicocele veins or from endovascular coils in any interventional setting. As a result, studies describing the prevalence or pathogenesis of coil-related pain are lacking. Although the intraoperative findings of perivessel edema would support inflammation as a possible etiology, the lack of efficacy of anti-inflammatory medications preoperatively contradicts this idea. Additional reports of similar cases and subsequent analysis are required to develop a stronger hypothesis regarding the pathogenesis of postembolization pain.
Previous reports, including a case report in 1994 by Brooks and colleagues, describe persistence of testis pain after gonadal vein embolization.5 In this specific case, it was a grade 1 left varicocele that was believed to be the cause of a patient's chronic orchialgia. After persistence of pain after embolization, the patient was offered laparoscopic resection of the left gonadal vein including embolic coils and spermatic cord. The result was complete resolution of his left testis pain. However, in this case, his pain persisted in the scrotal/inguinal area and surgical treatment included a spermatic cord dissection that included ligation of the nerves of the spermatic cord. Although this case includes the common theme of resection of an embolized gonadal vein, which should be acknowledged, the resolution of his chronic scrotal pain was likely related to his spermatic cord resection.
It is possible this represented recurrence of his varicocele-related pain with referred pain to the periumbilical region. However, it has not previously been described that patients experience pain from the varicocele in the periumbilical region, and additionally no spermatic cord denervation was performed in our treatment.
Although it cannot be proven that the coils themselves were the cause of the patient's pain, we can assert with robot-assisted laparoscopic resection, the procedure can be performed efficiently with minimal morbidity. Although he had some mild incisional pain rated 1 to 2/10 at 6 weeks postoperatively, he requires further follow-up to determine the complete resolution of his chronic pain.
Conclusion
To our knowledge, this is the first case report demonstrating the surgical removal of the gonadal vein for treatment of chronic abdominal pain after varicocele embolization. After failing conservative measures, this may present a viable treatment option to address this sequalae should it arise in subsequent patients after coil embolization for a varicocele. Additional cases of postembolization abdominal pain with surgical vein are required to establish the causative relationship of the coils with the patient symptomatology and the efficacy of resection.
Abbreviation Used
- CT
computed tomography
Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Cite this article as: Doolittle J, Maniar V, Dietrich P, Sandlow J, Johnson S, Kansal J (2020) Resolution of abdominal pain after coil embolization of varicocele with robotic resection of gonadal vein, Journal of Endourology Case Reports 6:4, 533–535, DOI: 10.1089/cren.2020.0171.
References
- 1. Halpern J, Mittal S, Pereira K, Bhatia S, Ramasamy R. Percutaneous embolization of varicocele: Technique, indications, relative contraindications, and complications. Asian J Androl 2016;18:234–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lima SS, Castro MP, Costa OF. A new method for the treatment of varicocele. Andrologia 1978;10:103–106 [DOI] [PubMed] [Google Scholar]
- 3. Puche-Sanz I, Flores-Martín JF, Vázquez-Alonso F, Pardo-Moreno PL, Cózar-Olmo JM. Primary treatment of painful varicocoele through percutaneous retrograde embolization with fibred coils. Andrology 2014;2:716–720 [DOI] [PubMed] [Google Scholar]
- 4. Lenz M, Hof N, Kersting-Sommerhoff B, Bautz W. Anatomic variants of the spermatic vein: Importance for percutaneous sclerotherapy of idiopathic varicocele. Radiology 1996;198:425–431 [DOI] [PubMed] [Google Scholar]
- 5. Brooks JD, Moore RG, Kavoussi LR. Laparoscopic management of testicular pain after embolotherapy of varicocele. J Endourol 1994;8:361–363 [DOI] [PubMed] [Google Scholar]