Abstract
Background: Intraoperative indocyanine green near-infrared fluorescence guidance is an emerging optical imaging technology to facilitate better understanding of surgical landmarks. Herein, this technique was applied during the surgery for urachal carcinoma.
Case Presentation: A 50-year-old man with urachal carcinoma underwent laparoscopic partial cystectomy and pelvic lymph node dissection (PLND). Before the laparoscopic surgery, indocyanine green was injected cystoscopically around the tumor at the submucosa level. The tumor location and lymph drainage were clearly viewed. The lymphatic flow was along the superior vesical artery and the umbilical ligament. The obturator and external lymph nodes were not fluoresced. Template PLND was performed. Partial cystectomy was completed with cystoscopic monitoring of the margin and with endoscopic stapler to avoid tumor spillage.
Conclusion: Intraoperative indocyanine green fluorescence views lymph drainage and tumor location and is useful to improve the quality of PLND and partial cystectomy.
Keywords: indocyanine green, lymph node excision, optical imaging, partial cystectomy, surgery, urachal cancer
Introduction
Intraoperative indocyanine green (ICG) near-infrared fluorescence (NIRF) guidance is an emerging optical imaging technology that facilitates better understanding of surgical landmarks. In the field of urology, ICG is used to delineate tumor margins, view lymph node drainage, and identify an important vasculature.1 Several reports have shown the efficacy of real-time guidance for ICG in the pelvic lymph node dissection (PLND) for radical cystectomy or prostatectomy.2,3 Meanwhile, studies that used ICG to surgery for urachal carcinoma are limited. Herein, we described a case with improved quality of partial cystectomy and PLND for urachal carcinoma with ICG NIRF support.
Presentation of Case
A 50-year-old man with no significant history presented with asymptomatic gross hematuria. Cystoscopy revealed a single nodular tumor at the dome of the bladder. He underwent computed tomography scan and magnetic resonance imaging, revealing a 4.4 cm mass at the dome extending from the urachal remnant (Fig. 1). He initially underwent transurethral resection of the tumor. Mucinous adenocarcinoma with muscle invasion was found in the histopathologic analysis. With the urachal carcinoma Sheldon stage IIIA diagnosis, he underwent partial cystectomy with excision of the remaining urachal ligament and PLND.
FIG. 1.
T2-weighted sagittal magnetic resonance imaging of the patient.
After initiating the general anesthesia, the patient was at a lithotomy position, and 5 mL of 0.25 mg/mL ICG (Diagnogreen; Daiichi Pharmaceutical, Tokyo, Japan) was cystoscopically injected around the tumor at the submucosa level. The bladder was filled with 100 mL normal saline for 30 min after the injection. The patient was placed at a 15° Trendelenburg position. Laparoscopic surgery was started through a five-port transperitoneal approach. A laparoscopic NIR imaging system (Olympus Medical Systems, Tokyo, Japan) was used to identify the lymphatic pathway and tumor location. Lymph drainage ran along the umbilical ligament and proceeded cranially (Fig. 2). The tumor was easily identified by NIR imaging (Fig. 2). The lateral vesical space was opened, and the root of the umbilical ligament was identified. A surgical field should be carefully prepared with minimum disruption of lymphatic structures to avoid ICG leakage from damaged lymphatic vessels. Then, the ureterogastric fascia and internal iliac artery were dissected. NIRF imaging showed another flow that came from the superior vesical artery (Fig. 2). The template PLND of the obturator, external, internal, common iliac, and presacral lymph node was performed. According to the ICG finding, the superior vesical artery was skeletonized (Fig. 3). The umbilical ligament was excised at the distal area of the superior vesical artery. The urachus was excised at its attachment to the umbilicus. The transverse fascia of the bladder was also resected to secure the margin. Flexible cystoscopy was inserted, and the resection line was determined with a safety margin. The peritoneum and the detrusor muscle around the resection line were carefully dissected. With cystoscopic monitoring, the endoscopic stapler was used to divide and seal the bladder and excised tissues. After completing the partial cystectomy, the staple line at the bladder was resected at the frozen section. The bladder was closed in two layers.
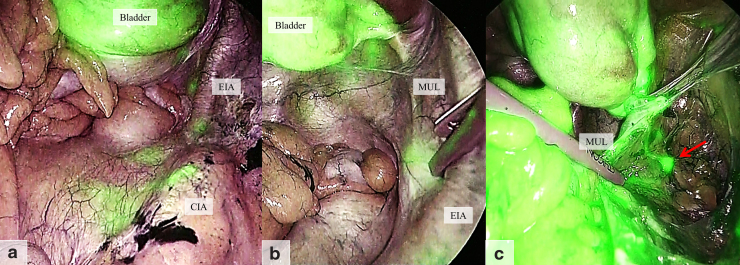
FIG. 2.
Intraoperative indocyanine green imaging. Lymphatic flow from the bladder to the presacral area was clearly viewed (a). The flow ran along medial umbilical ligament and accumulates at the root (b). The imaging detected another flow and lymph node through the superior vesical artery (red arrow) (c). CIA, common iliac artery; EIA, external iliac artery; MUL, medial umbilical ligament.
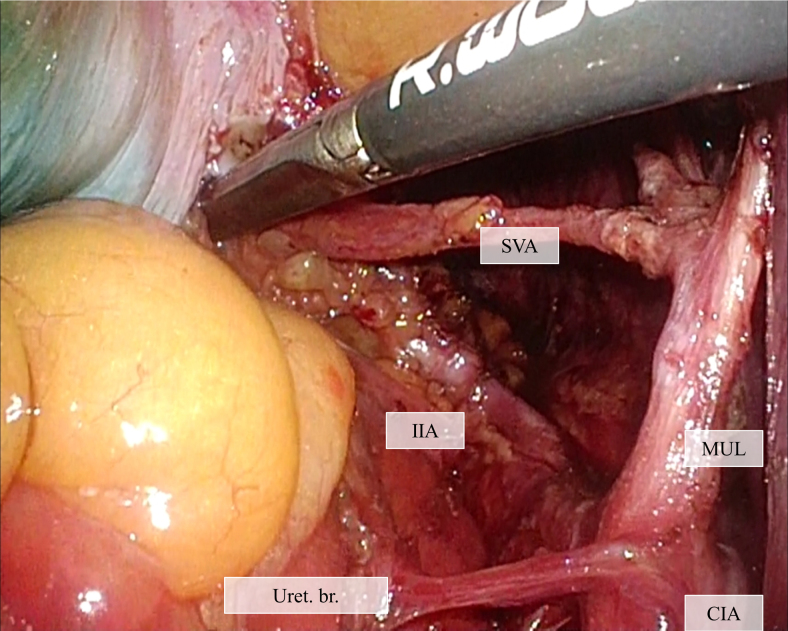
FIG. 3.
Surgical view after the lymph node dissection. The umbilical ligament and superior vesical artery were thoroughly skeletonized. SVA, superior vesical artery; Uret. Br., ureter branch.
The postoperative course of the patient was uneventful. The bladder catheter was removed on day 7. The final pathology report confirmed urachal carcinoma with peritoneum invasion.
Discussion
To the best of our knowledge, this is the first case report that applies ICG NIRF imaging on partial cystectomy and PLND for urachal carcinoma. The effectiveness of ICG lymphography has been well studied in the field of plastic surgery, and ICG would be sufficient as a single tracer during sentinel lymph node biopsy for breast cancer with >90% detection rate.1 In the field of urology, the several studies have assessed the effectiveness of ICG imaging in radical prostatectomy. A systematic review found a median sensitivity of 95.2% to detect sentinel lymph node, but the only one prospective randomized trial showed ICG-supported PLND produced a sensitivity of 44%.1 The several studies also reported initial experience of ICG for radical cystectomy.2 The tumor localization was effective in nine out of ten patients. The reported sensitivity and specificity to detect nodal malignancy was 75% and 52%, respectively. The differences in surgical approach and application site of the tracer were considered reason for wide range of the accuracy. To the date, ICG lymphangiography has not been sensitive enough to replace PLND, but has been shown to facilitate better understanding of anatomical landmark and pelvic lymph drainage.2,3
Urachal carcinoma extends to the bladder and sometimes metastasizes to the pelvic lymph node. Thus, PLND with partial cystectomy is recommended for urachal carcinoma,4 although its therapeutic role remains unknown. Compared with radical cystectomy for urothelial carcinoma, PLND for urachal carcinoma is unique in the following two points. First, the lymphatic drainage route of urachal carcinoma was unknown. Because of the different histologic features and the limited tumor location, urachal carcinoma may have a different lymphatic flow. Second, bladder vascular flow must be preserved. Impaired bladder blood flow may adversely affect the postoperative recovery of bladder function. The lymphatic flow was observed along the superior vesical artery and umbilical ligament. These lymphatic flows merged at the root of the umbilical ligament and run cranially. ICG was not fluoresced in the obturator and external lymph nodes. This finding indicates the importance of thorough lymph node dissection in the superior vesical artery and the root of the umbilical ligament. These vessels should be carefully skeletonized to preserve bladder flow. To date, no lymph node mapping study of urachal carcinoma was conducted. Further studies are needed to determine the appropriate extent of PLND for the management of urachal carcinoma.
ICG imaging can also be used to identify tumor location. As partial cystectomy for urachal cancer poses a risk of local recurrence, obtaining a negative resection margin is paramount.4 Tumor localization using ICG allows extensive resection around the tumor. Flexible cystoscopy was also used to monitor the intravesical tumor margin. An endoscopic stapler prevented exposure and spillage of tumor cells. The staple line was examined as a frozen section intraoperatively to confirm no remaining tumor. These utmost efforts can minimize the risk of local recurrence.
There are some pitfalls with the use of ICG. First, once PLND was initiated, observation was no longer feasible because of lymph fluid leakage. Surgeons should carefully plan the surgical field before observation to avoid disruption of lymphatic structures. Second, part of the ICG penetrated the bladder wall, making the bladder dissection difficult. Technical improvement is needed to appropriately inject ICG in the submucosal layer.
Conclusion
Intraoperative ICG NIRF imaging views lymph drainage and tumor location and is useful in improving the quality of PLND and partial cystectomy. Further studies are needed to identify the appropriate extent of PLND for the management of urachal carcinoma and the therapeutic benefits of ICG.
Acknowledgment
The authors thank Enago for the English language review.
Abbreviations Used
- ICG
intraoperative indocyanine green
- NIRF
near-infrared fluorescence
Disclosure Statement
The protocol for this research project has been approved by a suitably constituted Ethics Committee of the institution and conforms to the provisions of the Declaration of Helsinki. Informed consent was obtained from the patient. All authors declare no competing financial interests.
Funding Information
No funding was received for this article.
Cite this article as: Ito K, Takahashi T, Kanno T, Okada T, Higashi Y, Yamada H (2020) Indocyanine green fluorescence-guided partial cystectomy and pelvic lymphadenectomy for urachal carcinoma, Journal of Endourology Case Reports 6:4, 275–277, DOI: 10.1089/cren.2020.0025.
References
- 1. Kaplan-Marans E, Fulla J, Tomer N, et al. Indocyanine green (ICG) in urologic surgery. Urology 2019;132:10–17 [DOI] [PubMed] [Google Scholar]
- 2. Patel MN, Hemal AK. Molecular targeted fluorescence-guided intraoperative imaging of bladder cancer nodal drainage using indocyanine green during radical and partial cystectomy. Curr Urol Rep 2016;17:74. [DOI] [PubMed] [Google Scholar]
- 3. Miki J, Yanagisawa T, Tsuzuki S, et al. Anatomical localization and clinical impact of sentinel lymph nodes based on patterns of pelvic lymphatic drainage in clinically localized prostate cancer. Prostate 2018;78:419–425 [DOI] [PubMed] [Google Scholar]
- 4. Szarvas T, Modos O, Niedworok C, et al. Clinical, prognostic, and therapeutic aspects of urachal carcinoma-A comprehensive review with meta-analysis of 1,010 cases. Urol Oncol 2016;34:388–398 [DOI] [PubMed] [Google Scholar]