Abstract
Background: Pediatric urolithiasis may coexist with congenital urinary tract abnormalities, complicating conventional methods of stone treatment. Here, we present an effective case of robot-assisted laparoscopy and simultaneous ureteropyeloscopy for the definitive management of pediatric urolithiasis complicated by a congenital ureteral stricture.
Case Presentation: A 3-year-old girl presented to clinic with an outside noncontrast CT scan showing two 6–7 mm nonobstructing calculi in a mildly distended upper pole moiety of a duplex left kidney. Ureteral duplication status was unclear. The patient had suffered multiple febrile urinary tract infections throughout her life. Retrograde ureteropyelogram showed a stenotic waist in the upper pole ureter just proximal to the duplex ureteral convergence, and flexible ureteroscopy confirmed a congenital ureteral stricture. Simultaneous robot-assisted laparoscopic and ureteroscopic ureterolithotomy and ureteroplasty were offered and performed using a 3-armed robotic approach. The precise location of the stricture was identified robotically with simultaneous left ureteroscopy. A medial 1.5 cm longitudinal ureterotomy was made through the ureteral stricture to facilitate upper moiety ureterorenoscopy. The calculi were visualized in the upper moiety and retrieved in whole using a stone basket. The calculi were passed via the ureterotomy to the robotic instruments intraperitoneally. The longitudinal ureterotomy was closed transversely. A ureteral stent was placed, and indocyanine green was administered intravenously to confirm good perfusion of the ureteroplasty segment via fluorescence imaging.
The stent was removed at 4 weeks. Retrograde ureterography and flexible ureteroscopy revealed complete patency of the anastomosis. At 11 months, the upper pole moiety remained decompressed on ultrasonography. The patient has remained off antibiotic prophylaxis without further infection.
Conclusion: Robot-assisted approaches can be primary or adjunct tools in the definitive treatment of pediatric urolithiasis with concomitant urinary tract abnormalities.
Keywords: ureterolithotomy, lithotomy, ureteroplasty, robotic surgery, robot-assisted laparoscopic surgery
Introduction and Background
The incidence of stone disease has continued to rise in children, now comprising an estimated 1 case every 685 pediatric hospitalizations in the United States.1 While there are several differences in the presentation of urolithiasis in adults versus children, an understudied factor is the effect of congenital renal and ureteral abnormalities on the management of renal stones in young pediatric patients. We present a case of pediatric urolithiasis in a duplex renal moiety obstructed from a congenital ureteral stricture. Robot-assisted laparoscopy and simultaneous ureteropyeloscopy facilitated definitive management of both conditions.
Presentation of Case
A 3-year-old girl with global developmental delay presented to the pediatric urology clinic with history of two febrile urinary tract infections (UTIs) before the age of 12 months. After birth at 36 weeks, the patient required open diaphragmatic hernia repair and spent 50 days in the neonatal intensive care unit. By mother's report, a renal and bladder ultrasound (RBUS) at that time showed left renal urolithiasis. Between the age of 12 months and 3 years, the patient had been intermittently taking prophylactic nitrofurantoin. In the months preceding the initial clinic appointment, she had stopped antibiotic prophylaxis and suffered two culture-proven febrile UTIs. Limited outside records indicated Escherichia coli infections.
At the initial clinic visit, vital signs and physical examination were unremarkable. RBUS showed a normal right kidney and left duplex kidney with a normal lower moiety and a distended left upper moiety collecting system with Society of Fetal Urology grade 2 hydronephrosis with two 6–7 mm calculi. A voiding cystourethrogram was normal. Single-photon emission computed tomography (SPECT) 99mTc dimercaptosuccinic acid renography confirmed the size of two 6–7 mm calculi. The left kidney contributed 45% differential renal function with the upper moiety accounting for 22% (∼10% of total renal function). It was not clear whether the left collecting system was completely or incompletely duplicated. It was presumed that the calculi formed following furosemide administration early in life.
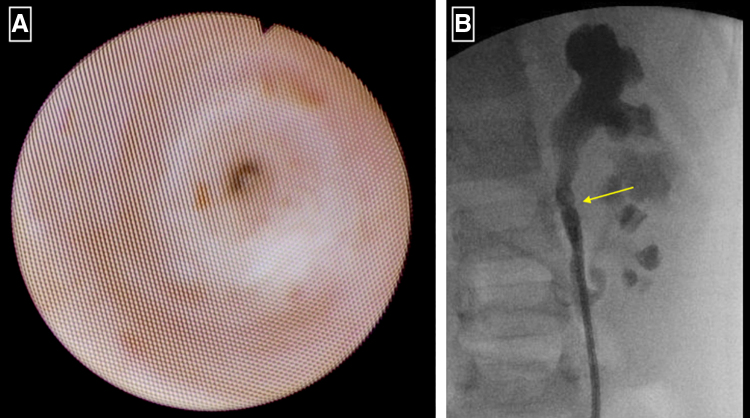
In the operating room with the patient in dorsal lithotomy, retrograde ureteropyelogram showed an incompletely duplicated left ureter with a stenotic waist to the left upper moiety ureteral segment proximal to the convergence with the lower moiety ureter. The upper and lower moiety ureters converged just inferior to the lower margin of the kidney. Dilation of the ureterovesical junction with an 8 F dilator permitted passage of a 7.5 F KARL STORZ FLEX-X2S (Tuttlingen, Germany) flexible ureteroscope. Flexible ureteroscopy confirmed a congenital ureteral stricture of the upper moiety ureter (Fig. 1). Robot-assisted laparoscopic (RAL) ureterolithotomy (RALUL) was planned.
FIG. 1.
(A) The presence of a congenital ureteral stricture of the upper moiety ureter was confirmed via ureteroscopy. (B) Intraoperative retrograde ureteropyelogram demonstrated a stenotic waist in the upper pole ureter just proximal to the ureteral convergence, as indicated by yellow arrow.
A 0.035 hydrophilic guidewire and 4 F angle-tip angiographic catheter were placed proximal to the stenosis to maintain ureteral access. The patient was moved to a modified right lateral decubitus position with the left side supported by a triangular wedge. Arms were secured at the sides. An 8 mm robotic trocar was placed at the umbilicus for the robotic camera. Left and right robotic 8 mm robotic trocars were placed 7 cm superior and inferior to the camera port for the working arms. An additional 12 mm assistant port was placed in the right lower quadrant to facilitate gastrostomy adhesion takedown and eventual stone extraction. The stomach was released from the anterior abdominal wall with a laparoscopic stapler. Robotically, enterolysis was performed and the descending colon was released along the white line and reflected medially. The proximal common ureter was identified and dissected proximally. The ureteroscope was passed over a guidewire and positioned distal to the stricture. The precise location of the stricture was identified robotically. A medial 1.5 cm longitudinal ureterotomy was made through the ureteral stricture with robotic Potts scissors to facilitate upper moiety ureterorenoscopy and eventual Heineke–Mikulicz strictureplasty.
Under combined ureteroscopic and robotic vision, the bedside assistant directed the ureteroscope proximal to the stricture via the ureterotomy and into the upper moiety collecting system. The first calculus was visualized and grasped using a 1.7 F stone basket. The ureteroscope was then directed distally and into the abdomen via the ureterotomy (Fig. 2). The surgeon at the robotic control received handoff of the calculus and it was placed in a laparoscopic specimen bag. The process was repeated for the second calculus. A third pass of the ureteroscope through the upper moiety caliceal system confirmed the absence of residual stone fragments. The ureteroscope was visually withdrawn from the ureter to confirm the absence of residual fragments or ureteral injury. The 4 F angiogenic catheter was positioned proximal to the ureterotomy to preserve access and facilitate ureteral stent placement.
FIG. 2.
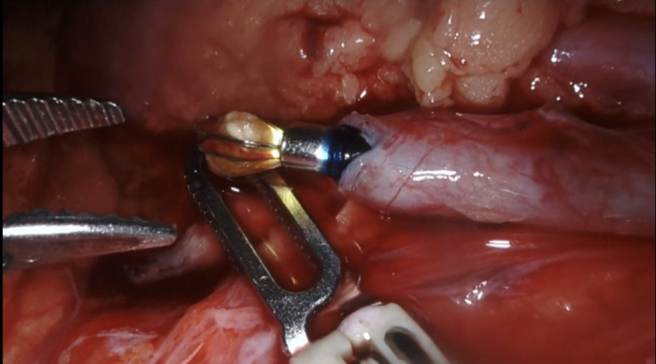
The first calculus was visualized via combined ureteroscopic and robotic vision and grasped using a 1.7 F stone basket.
The longitudinal ureterotomy was closed transversely with interrupted simple 6-0 polydioxanone on a TF needle. A ureteral stent was placed in retrograde manner over a guidewire to the upper moiety renal pelvis through the repair to ensure postoperative drainage. Given the degree of manipulation to the ureteral segment, indocyanine green 1.25 mg (0.5 mL of 25 mg/10 cc solution) was administered intravenously and good perfusion was confirmed via Firefly® (Intuitive, Sunnyvale, CA) fluorescence imaging (Fig. 3).
FIG. 3.
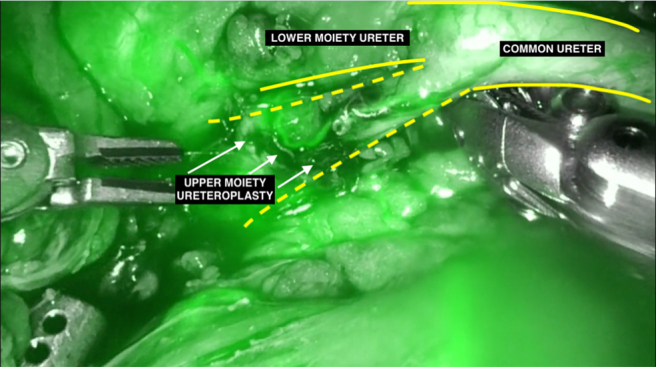
Indocyanine green 1.25 mg (0.5 mL of 25 mg/10 cc solution) was administered intravenously to confirm adequate perfusion of the ureteral segment via Firefly® (Intuitive, Sunnyvale, CA) fluorescence imaging.
The laparoscopic specimen bag was removed via the 12 mm assistant port. All trocars were removed, and fascia closed under laparoscopic visualization using 2-0 polyglactin. Dermis was closed with buried simple interrupted stitches of 4-0 polyglactin. Skin was closed with running subcuticular 5-0 poliglecaprone. Intraoperative fluoroscopy confirmed proper position of the stent and absence of residual calcifications.
The ureteral stent was removed in the operating room 4 weeks later. Retrograde ureteropyelogram confirmed patency of the repair. Ureteropyeloscopy was performed to visualize the repair and to check for residual calculi. The segment easily accepted an 8.5 F Olympus URF-V (Center Valley, PA) digital flexible ureteroscope and was visualized to be widely patent. There were no residual calculi. At the 11-month follow-up, RBUS showed a normal duplex kidney without collecting system dilatation or calcifications. The patient remains asymptomatic off antibiotic prophylaxis. Calculus compositional analysis was 50% calcium oxalate monohydrate, 12% calcium oxalate dihydrate, 35% calcium phosphate, and 3% protein.
Discussion
Urolithiasis in children is increasing, with observational studies demonstrating up to a 10% increase in incidence annually over a 10-year period in the United States.2 Surgical techniques for the management of urolithiasis have been widely documented; however, the literature for RAL surgery for the treatment of stones in the presence of congenital genitourinary abnormalities in the pediatric population is lacking. Here we present a complex case of urolithiasis presenting within a duplex kidney with a congenital ureteral stricture that was effectively managed using RAL and ureteroscopic ureterolithotomy and ureteroplasty. In our patient, the presence of urolithiasis was likely due to her early exposure to furosemide and the presence of a congenital ureteral stricture that contributed to urine stasis, preventing spontaneous resolution typically seen in pediatric furosemide-associated urolithiasis.
Treatment of the left upper moiety urolithiasis was pursued with decision to preserve the left upper moiety. In counseling the patient's family, left percutaneous nephrolithotomy (PCNL) versus RAL pyelolithotomy (RALPL) was planned with final intraoperative decision-making on a procedure based on ureteral anatomy, collecting system dilatation, and caliceal architecture of the upper moiety. Given the limited dilatation of the upper moiety collecting system, it was felt that ureteroscopic-guided percutaneous access would be the safest approach for PCNL; however, the ureteral stricture limited access to the upper pole. It was felt that percutaneous access and nephrolithotomy would be technically difficult and unlikely to definitively treat the ureteral stricture. Furthermore, percutaneous access to the upper pole and tract dilation would most likely compromise the lower pole collecting system. We did not pursue laser ablation of the stricture due to concern for recurrence and parental preference for the most definitive therapy. Therefore, decision was made to pursue RAL treatment of the stricture and RAL-guided ureterolithotomy. The decision for ureteroplasty versus excision of the stricture and ureteroureterostomy was based on intraoperative assessment that excision of the stricture would place the ureteral repair on tension and risk kinking the common ureter convergence.
Although extracorporeal shock wave lithotripsy and ureteroscopy with laser lithotripsy are considered first line in the treatment of pediatric stones, RAL has proven to be a safe and efficacious approach especially in conditions also requiring concurrent reconstruction. In 2007, Lee et al. were the first to report the effective removal of large stones in four of five pediatric patients using RAL.3 Of the four effective stone-free patients, one patient had a concurrent ureteropelvic junction obstruction that was also repaired during the procedure. For the one ineffective patient, conversion to open pyelolithotomy was undertaken due to their inability to extract the stone from the intrarenal pelvis and ineffective attempts with electrohydraulic lithotripsy. It was felt that a combined, minimally invasive technique would offer increased visualization, ease of intracorporeal reconstruction, and improved ergonomics over other documented open or laparoscopic approaches to urolithiasis.4 We encourage surgeons in a similar future scenario to consider simultaneous ureteroscopy at the time of RAL ureteral stricture to ensure proper location of the ureterotomy and to minimize the length of the ureterotomy needed for the repair.
Conclusion
We present an effective case of RAL for definitive management of pediatric ureterolithiasis complicated by congenital abnormalities to add to the paucity of literature in the pediatric setting. As the incidence pediatric stone disease increases, we urge other urologists to consider RAL as a potential approach for large stones and urolithiasis requiring simultaneous urinary tract reconstruction.
Abbreviations Used
- CT
computed tomography
- PCNL
percutaneous nephrolithotomy
- RAL
robot-assisted laparoscopic
- RALPL
RAL pyelolithotomy
- RALUL
RAL ureterolithotomy
- RBUS
renal and bladder ultrasound
- SPECT
Single-photon emission computed tomography
- UTIs
urinary tract infections
Disclosure Statement
No competing financial interests exist.
Funding Information
There was no financial support for this project.
Cite this article as: Locke RA, Kwenda EP, Archer J, Bergamo J, Domino MP, DeMarco RT, Bayne CE (2020) Pediatric robot-assisted laparoscopic and ureteroscopic ureterolithotomy and ureteroplasty, Journal of Endourology Case Reports 6:4, 264–267, DOI: 10.1089/cren.2020.0043.
References
- 1. Bush NC, Xu L, Brown BJ, et al. Hospitalizations for pediatric stone disease in United States, 2002-2007. J Urol 2010;183:1151–1156 [DOI] [PubMed] [Google Scholar]
- 2. Routh JC, Graham DA, Nelson CP. Epidemiological trends in pediatric urolithiasis at United States freestanding pediatric hospitals. J Urol 2010;184:1100–1104 [DOI] [PubMed] [Google Scholar]
- 3. Lee RS, Passerotti CC, Cendron M, Estrada CR, Borer JG, Peters CA. Early results of robot assisted laparoscopic lithotomy in adolescents. J Urol 2007;177:2306–2309; discussion 2309. [DOI] [PubMed] [Google Scholar]
- 4. Ballesteros N, Snow ZA, Moscardi PRM, Ransford GA, Gomez P, Castellan M. Robotic management of urolithiasis in the pediatric population. Front Pediatr 2019;7:351. [DOI] [PMC free article] [PubMed] [Google Scholar]