Abstract
Background: Although the prostatic urethral stents are no longer used in the United States for treatment of prostatomegaly, urologists will encounter patients with complications of previously placed permanent prostatic stents. We report two cases of persistent bothersome lower urinary tract symptoms (LUTS) after prostatic stent placement treated with simultaneous holmium laser enucleation of prostate (HoLEP) with endoscopic removal of the prostatic urethral stent using high-power holmium laser. We also reviewed the literature regarding the removal of prostatic stents with holmium laser combined with surgical management of benign prostatic hyperplasia.
Case Presentation: A 71-year-old man who presented with LUTS, recurrent gross hematuria, and urinary infection, which developed after placement of a prostatic stent 10 years prior for urinary retention secondary to prostatomegaly (80 g). He underwent combined HoLEP with endoscopic removal of the prostatic stent using 100 W holmium laser at a power setting of 2 J and 30 Hz. The surgical steps comprised fragmentation of the stent in situ by making incisions at 5, 7, and 12 o'clock positions followed by enucleation of the prostate. The stent was then separated from enucleated tissue in the urinary bladder. The remaining prostate adenoma was then morcellated and removed. The patient remained asymptomatic at 10-year follow-up. Another patient was 62-year-old man who developed recurrence of bothersome LUTS, 1 year after placement a prostatic stent for urinary retention. On investigation his prostate was 105 g and stent showed partial migration in the bladder with overlying calcification. HoLEP and stent removal was performed in a manner similar to the first patient. This patient also remained asymptomatic at a 1-year follow-up.
Conclusion: Combined HoLEP with removal of a prostatic urethral stent using a high-power holmium laser is safe and effective with long-term durable outcome.
Keywords: HoLEP, urethral stent, UroLume, enucleation, holmium laser
Introduction and Background
The permanent epithelizing endoprosthesis UroLume® stent was FDA approved in 1988 for minimally invasive treatment of benign prostatic enlargement (benign prostatic hyperplasia [BPH]). The procedure lacked long-term efficacy and was frequently associated with unfavorable outcome secondary to persistent irritative voiding symptoms, hyperplastic tissue reaction, stent migration, encrustation, and recurrent obstruction. As per European Association of Urology (EAU) guidelines on male non-neurogenic lower urinary tract symptoms (LUTS) 2018, there is weak evidence in the current literature supporting use of prostatic urethral stents.1 They can only be offered to unfit men as an alternative to catheterization. Although the UroLume is no longer on the market in United States, urologists may continue to encounter patients that suffer from the complications of a previously placed permanent prostatic stent.
Holmium laser, because of its ablative, cutting, and hemostatic properties along with minimal depth of penetration has been described for the safe endoscopic removal of migrated UroLume prostatic urethral stent.2 Holmium laser enucleation of prostate (HoLEP) is also recommended as size-independent treatment modality for surgical treatment of enlarged prostate.1 It is the preferred option in high-risk anticoagulated patients. We report two cases of persistent bladder outlet obstruction after prior prostatic stent placement treated with combined HoLEP and endoscopic removal of a permanent prostatic stent using high-power holmium laser at S. L. Raheja (Fortis associate) Hospital in Mumbai, India. We also provide a detailed technique description and review the literature on combined removal of permanent prostatic stent using holmium laser with simultaneous surgical management of BPH.
Presentation of Cases
Case 1
A 71-year-old man patient presented with a 2-year history of bothersome LUTS with International Prostate Symptom Score (IPSS) of 28/35. He also suffered from recurrent gross hematuria and recurrent urinary tract infection. His past medical history included diabetes, hypertension, ischemic heart disease, and was being managed on dual antiplatelet medication. A UroLume prostatic urethral stent was placed 10 years back to treat urinary retention secondary to enlarged prostate after coronary angioplasty. Despite maximal medical therapy of tamsulosin 0.4 mg and finasteride 5 mg daily, his symptoms did not improve. His maximum flow rate was (Qmax) 6.8 mL/seconds and residual volume was 125 mL. Prostate size was 80 mL on abdominal ultrasonography and X-ray pelvis confirmed the presence of metallic stent. Cystoscopy revealed a prostatic stent lying submucosally with trilobar enlargement of prostate (Fig. 1A). He underwent combined prostatic stent fragmentation and removal using a high-power holmium laser with HoLEP. A detailed surgical technique is described as follows. The duration of surgery was 90 minutes and resected tissue weighed 52 g. The duration of postoperative catheterization was 21 hours and hospital stay was 38 hours. There were no intra- and postoperative complications. At 6-month follow-up, he noted good symptomatic improvement with IPSS of 3/35, Qmax of 21.7 mL/seconds and postvoid residual urine of 31 mL. At 10-year follow-up he remained asymptomatic without evidence of recurrent obstruction.
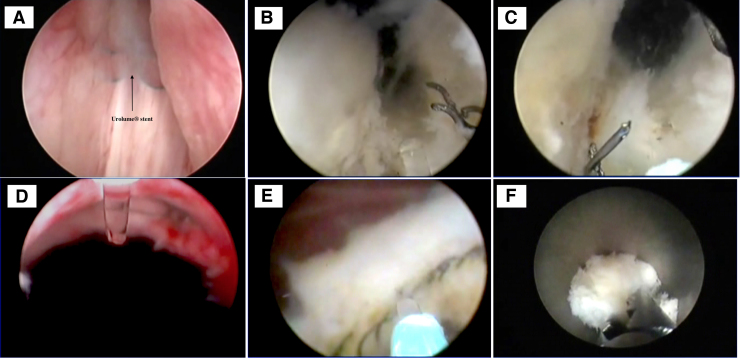
FIG. 1.
Step-by-step surgical technique. (A) Cystourethroscopy revealed the prostatic urethral stent present submucosally (black arrow) with trilobar enlargement of prostate. (B) Incision at 5 o'clock. (C) Incision at 7 o'clock. (D) Incision at 12 o'clock. (E) Separating the stent from enucleated prostatic tissue. (F) Stent pieces along with surrounding prostatic tissues are removed by grasping forceps.
Case 2
A 62-year-old diabetic man was referred for recurrence of bothersome LUTS 1 year after UroLume placement for urinary retention. On bladder ultrasonography his prostate was noted to be 105 mL in size. Cystoscopy revealed that the prostatic stent had migrated proximally into the urinary bladder with evidence of calcification and trilobar enlargement of prostate. HoLEP and stent removal was performed as described hereunder. The duration of the entire surgery, including fragmentation of calcification, was 75 minutes and weight of resected tissue was 89 g. The duration of postoperative catheterization and hospital stay was 29 and 41 hours, respectively. There were no intra- or postoperative complications. At 1-year follow-up, he was voiding well with IPSS of 3/35 and no evidence of obstruction.
Surgical Technique and Postoperative Care
A 100 W holmium laser with 550 μ laser fiber was used for the earlier procedures (Lumenis, Santa Clara, California). Our laser power setting was 2 J and 30 W. First, the stent was fragmented in situ: An incision was made at 5 o'clock position from bladder neck to verumontanum and the metallic stent was fragmented along its length using the holmium laser (Fig. 1B). The groove was deepened up to the prostatic capsule. A similar incision was made at 7 o'clock position (Fig. 1C) and the median lobe was enucleated along with incorporated fragmented stent. Enucleation was then started on the left lateral lobe by deepening the groove between verumontanum and apical lobe. An incision was made on the anterior commissure at 12 o'clock position (Fig. 1D). The metallic stent at this position was similarly fragmented during this incision. After the left lobe of the prostate was enucleated and pushed into bladder, similar steps are employed to enucleate right lobe. The stent was then separated from the enucleated lobe of prostate using holmium laser in the urinary bladder (Fig. 1E). At the power setting of 2 J and 30 Hz there was no difficulty in fragmentation of the UroLume stent. There were no concerning or observably unique interactions between the laser pulse and the metallic surface of the stent except for intermittent sparking.
We then removed the fragmented pieces of stent using grasping forceps. This step is done before morcellation of prostate adenoma to prevent damage to the morcellator blades by the fragmented stents (Fig. 1F). Morcellation of the remaining prostate adenoma was performed using Lumenis Versacut morcellator™.
Postoperatively, both patients had a urethral 20F Foley catheter that was not kept on traction. However, both patients had overnight bladder irrigation. They both had voiding trials the next day and were discharged home on second postoperative day. They were asked to come for follow-up at 3, 6, and 12 months, and yearly thereafter.
Discussion and Literature Review
The largest series of UroLume endoprosthesis removal came from the North American study group who noted that 19.6% of stents needed removal.3 They initially performed transurethral resection of the uroepithelial tissue covering the stent using pure resection current at low power settings. This was followed by either intact or piecemeal-wire by wire mechanical removal of stent. Procedure was, however, associated with moderate to severe bleeding, trauma to the urethra and external sphincter in about 25% of the patients. The complications were more in wire-by-wire technique as compared with intact removal.3
To minimize this complication, use of low-power (0.6 J, 6 Hz) holmium laser to remove an encrusted migrated UroLume stent was first described by Lallas et al.2 They initially vaporized the urothelium covering the stent and then cut through the stent. Since then, there are a few case reports on safe use of holmium laser for the removal of migrated or calcified prostatic stents. However, few of these have combined the procedure of prostatic stent removal employing holmium laser with simultaneous surgical treatment of BPH (Table 1). Kural et al.* in 2001 first described simultaneous transurethral resection of prostate and removal of prostatic stent using low-power holmium laser. They emphasized the importance of removing all the fragmented stent pieces from the urinary bladder and prostatic urethra before surgical removal of prostate.4 Dyer et al. was the first to describe use of high-power holmium laser (2.5 J and 40 Hz) to cut the UroLume stent using an end firing laser fiber along with simultaneous laser ablation of the prostate using a side firing laser fiber.4 The patient had 6 weeks follow-up as compared with 10 years follow-up in our patient. Mahajan et al.* had also reported simultaneous HoLEP and removal of a migrated prostatic stent into the urinary bladder using low-power laser (0.8 J, 6 Hz). But the technical nuances were not described in this case report.
Table 1.
Use of Holmium Laser in Prostatic Urethral Stent (UroLume®) Removal Along with Simultaneous Treatment of Enlarged Prostate
| Sr. No. | Author and year | Number of patients | Duration of stent in situ (months) | Position of prostatic urethral stent | Management of stent | Management of prostate | Energy settings | Follow-up duration (months) |
|---|---|---|---|---|---|---|---|---|
| 1 | Kural et al.* (2001) | 1 | 6 | Migrated partially to urinary bladder | Laser used to vaporize uroepithelial tissue covering the stent and cut the stent | TURP | 0.8 J, 6 Hz | 9 |
| 2 | Mahajan et al.* (2010) | 1 | 9 | Migrated to urinary bladder | Cut in small fragments | HoLEP | 1.2 J, 20 Hz | — |
| 3 | Dyer et al.4 (2013) | 1 | 96 | In situ | Cut in four large fragments | HoLAP | 2.5 J, 40 Hz | 1.5 |
| 4 | Our series (2020) | 2 | 24–120 | In situ and migrated to urinary bladder | Cut in three pieces along with prostate and later separated from enucleated adenoma in bladder | HoLEP | 2 J, 30 Hz | 12–120 |
Dyer et al. cited Kural et al. and Mahajan et al. in his article.
HoLAP, holmium laser ablation of prostate; HoLEP, holmium laser enucleation of prostate; Hz, hertz; TURP, transurethral resection of prostate.
We report two cases of bothersome LUTS after prostatic stent placement and also describe step-by-step approach for combined removal of prostatic stent and HoLEP using high-power laser setting. Our series is the longest available follow-up after endoscopic removal of prostatic stent and suggests that this technique is safe and durable.
Conclusion
High-power holmium laser can be safely used for removal of UroLume prostatic urethral stent combined with HOLEP to surgically treat patients with bladder outlet obstruction secondary to enlarged prostate and retained prostatic urethral stent.
Abbreviations Used
- BPH
benign prostatic hyperplasia
- HoLEP
holmium laser enucleation of prostate
- LUTS
lower urinary tract symptoms
- TURP
transurethral resection of prostate
Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Cite this article as: Banerjee I, Smith NA, Katz JE, Gokhale A, Shah R, Shah HN (2020) Simultaneous holmium laser enucleation of prostate with removal of the permanent prostatic urethral stent using the high-power holmium laser: technique in two cases and review of the literature, Journal of Endourology Case Reports 6:4, 438–441, DOI: 10.1089/cren.2020.0158.
References
- 1. Gravas S, Cornu JN, Drake MJ, et al. EAU guidelines on the assessment of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 2018;67:1099–1109 [DOI] [PubMed] [Google Scholar]
- 2. Lallas CD, Munver R, Preminger GM. Removal of a UroLume prostatic stent using the holmium laser. Urology 2001;57:166–167 [DOI] [PubMed] [Google Scholar]
- 3. Gajewski JB, Chancellor MB, Ackman CF, et al. Removal of Urolume endoprosthesis: Experience of North American study group for Detrusor-Sphincter Dyssynergia Application. J Urol 2000;163:773–776 [DOI] [PubMed] [Google Scholar]
- 4. Dyer A, Funk J, Twiss C. Endoscopic removal of urolume urethral stent using high power holmium laser. Videourology. 2013;27:DOI: 10.1089/vid.2013.0084 [DOI] [Google Scholar]