Abstract
Background: Extrinsic compression of the ureter can result from multiple different malignancies, typically in the presence of known or disseminated disease. Rarely, hydroureteronephrosis and flank pain can occur as the presenting sign and symptom of lymphoma. In this study, we present two cases of primary ureteral obstruction in patients without a prior diagnosis of lymphoma and without bulky retroperitoneal lymphadenopathy.
Case Presentation: Case #1 was a healthy 58-year-old man who presented with acute left flank pain. He was found to have left hydroureteronephrosis secondary to a proximal periureteral mass. Diagnostic ureteroscopy demonstrated this to be an extrinsic compression on the ureter and preoperative imaging was negative aside from one enlarged periaortic node. Laparoscopic ureterolysis and biopsy were remarkable for periureteral dystrophic tissue concerning for lymphoma. Case #2 was a 47-year-old woman with a solitary kidney secondary to prior left nephrectomy who presented with hydronephrosis of her solitary kidney and acute kidney injury. Retrograde pyelogram showed high-grade obstruction at the junction of the mid- and distal ureter. Periureteral thickening was noted, but no definitive masses were seen on cross-sectional imaging. Robotic ureterolysis showed dense fibrosis around the ureter. Pathology report from Cases #1 and #2 were both remarkable for marginal zone lymphoma and both patients received bendamustine and rixuximab with resolution of ureteral obstruction and their lymphoma.
Conclusion: Ureteral compression as the primary presentation of periureteral lymphoma is a rare but important etiology of extrinsic malignant ureteral obstruction. These cases emphasize that malignant obstruction can occur even in the absence of disseminated disease.
Keywords: ureteral obstruction, hydronephrosis, lymphoma
Introduction and Background
New onset hydronephrosis can arise from a multitude of clinical etiologies and commonly results in patient discomfort with flank pain. Differentiating between intrinsic and extrinsic compression of the ureter is an important part in the work-up of these patients. Malignant extrinsic compression of the ureter commonly occurs secondary to malignancies arising from the genitourinary or gastrointestinal tracts as well as secondary to retroperitoneal lymphadenopathy as seen in lymphoma.1 Although not well described in the literature, our clinical experience has demonstrated this typically to be seen in patients with advanced stages and local invasion from a known or disseminated malignancy. However, in this study we present two cases of extrinsic ureteral compression and obstruction secondary to periureteral marginal zone lymphoma as the presenting symptom of their disease.
Presentation of the Case
Case 1
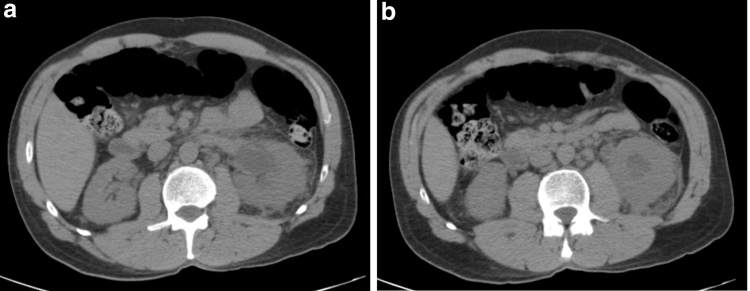
After initially presenting with acute onset left-sided abdominal pain, a 58-year-old man with unremarkable past medical history and taking no prescription medications was found to have left hydronephrosis. A CT scan demonstrated a left proximal ureter and ureteropelvic junction mass, although it was difficult to determine if hydronephrosis was secondary to intrinsic or extrinsic compression (Fig. 1A, B). The only other significant finding was a questionable lymph node in the left periaortic area.
FIG. 1.
Case 1 CT scan at time of presentation with (a) hydronephrosis and (b) a proximal periureteral mass causing obstruction.
The patient underwent ureteroscopic evaluation that demonstrated no intraluminal tumor. There was concentric narrowing in the proximal left ureter that appeared to be associated with chronic scarring or ischemia. A ureteral stent was placed at that time and subsequently a nuclear medicine Lasix renal scan demonstrated equal split renal function.
Patient opted for left robot-assisted laparoscopic ureterolysis and biopsy. Laparoscopic evaluation demonstrated encasement of the proximal ureter and ureteropelvic junction in dystrophic fat concerning for possible lymphatic tissue or retroperitoneal fibrosis. This tissue was excised as well as the periaortic lymph node and were both sent for frozen analysis, which returned as “increased lymphoid aggregate.” The ureter had been freed from the ureteropelvic junction down to its crossing of the iliac vessels. The patient received routine postoperative care and was discharged home on postoperative day number 1.
Final pathology report was consistent with marginal zone lymphoma in both the periureteral tissue and periaortic lymph node. He was subsequently seen and evaluated by oncology at which point a positron emission tomography (PET) scan showed mediastinal and right hilar lymphadenopathy (Fig. 2). He was found to have Stage IIIA disease, which subsequently went into remission after participation in a clinical trial in which he received bendamustine and rixuximab for six cycles followed by 2 years of maintenance rixuximab. He has now been in remission for 8 years without evidence of disease recurrence. He underwent repeat nuclear medicine renal Lasix scan, which showed 50/50% split renal function with a t½ of 7 minutes on the left and 5 minutes on the right.
FIG. 2.
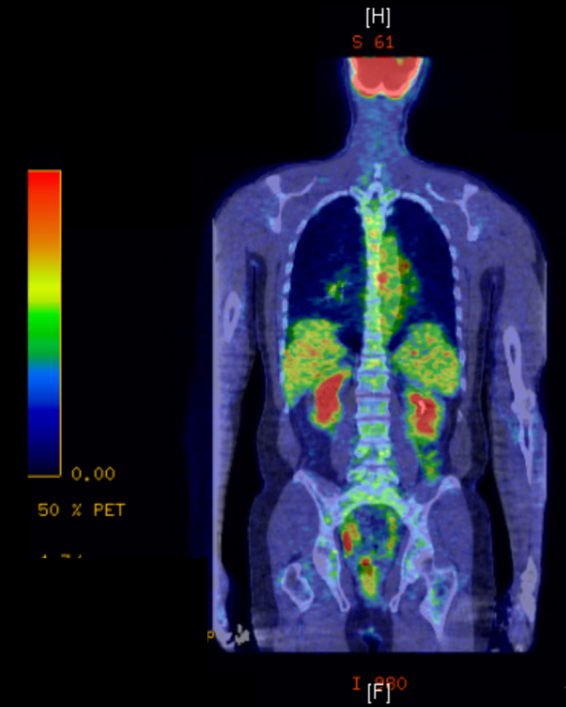
Case 1 PET scan showing periaortic mediastinal disease.
Case 2
A 47-year-old woman with history of left renal cell carcinoma status postlaparoscopic left nephrectomy, hypertension, hypothyroidism presented for evaluation of right ureteral obstruction of her solitary kidney. This was first identified when the patient sought care in the emergency department for renal colic symptoms with right flank pain associated with nausea and vomiting. A CT scan demonstrated right hydroureteronephrosis with distal ureteral thickening, and laboratories were remarkable for an acute kidney injury. She subsequently underwent right diagnostic ureteroscopy with biopsy and stent placement. The ureteral biopsies obtained were unremarkable, but retrograde pyelogram showed obstruction starting at the junction of the mid-distal ureter (Fig. 3). For the next few months, she continued to have intermittent bouts of flank pain associated with emesis that appeared to be associated with menstrual cycles. Given the cyclical nature of her symptoms, there was concern for endometriosis vs idiopathic ureteral stricture. An MRI was obtained for further work-up and did not show any definitive masses but did show periureteral thickening with indwelling stent in place (Fig. 4). She later underwent right nephrostomy tube placement for acute renal failure with subsequent improvement in her kidney function and symptoms.
FIG. 3.

Case 2 retrograde pyelogram showing right ureteral obstruction.
FIG. 4.
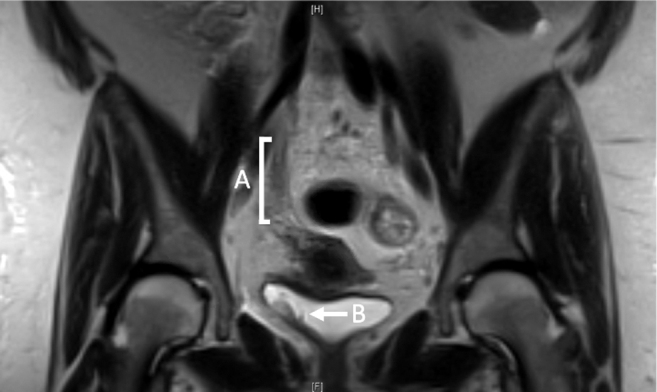
Case 2 preoperative MRI findings. (A) Periureteral thickening at mid-distal ureter. (B) Indwelling ureteral stent.
Patient opted for a robot-assisted laparoscopic ureterolysis. On intraoperative examination, there was noted to be dense fibrosis around the ureter from the bladder to the renal pelvis. There were no obvious masses. This rind around the ureter was avascular proximally but vascular distally. This was excised and sent to pathology analysis. Final pathology report was positive for marginal zone lymphoma of the fibroadipose periureteral tissue. She subsequently underwent a bone marrow biopsy and PET scan with a final diagnosis of Stage IV Marginal Zone B cell lymphoma involving of left femoral area and right periureteral area. She received six cycles of bendamustine and rixuximab with significant improvement in her disease. After the fourth cycle, the nephrostomy tube was removed after antegrade nephrostogram demonstrated a wide-open ureter. The patient has since remained on surveillance for her lymphoma for >2 years without evidence of progression and has had no evidence of ureteral obstruction recurrence on renal scan or ultrasonography.
Discussion and Literature Review
Despite the multitude of etiologies for ureteral obstruction, malignant extrinsic compression of the ureter is common, occurring in ∼238,500 cases between 2010 and 2015 in the United States alone.1 It is unclear from this as well as other prior studies how often patients are found to have hydronephrosis at initial presentation vs at a later time secondary to disseminated disease; however, our clinical experience is more consistent with the later except for in these two cases presented in this study.
Lymphoma-associated obstruction itself can originate from different sources. There are various case reports and one larger series in the literature describing primary, extranodal lymphoma of the urinary tract, which can in some cases lead to ureteral obstruction. These tumors are rare, with 1 case/1,000,000 people per year, and are typically aggressive with poor overall survival.2 This emphasizes the importance of diagnostic ureteroscopy and direct observation of the ureter when the source of ureteral obstruction is unclear. Ureteroscopy was completed in both of these cases to rule out a primary malignancy of the ureter itself such as urothelial cell carcinoma, primary lymphoma of the urinary tract, or an alternative intrinsic process.
There has been one prior case report of mantle cell lymphoma arising from outside the urinary tract causing obstruction with findings concerning for a ureteropelvic junction obstruction.3 Our two cases varied in that the obstruction itself arose from periureteral disease and not from ureteral infiltration by the lymphoma, as was seen in this prior case report. No other cases in the literature to our knowledge describe extrinsic ureteral obstruction as the presenting symptom for periureteral lymphoma without evidence of extensive retroperitoneal disease.
Both patient cases reported in this study underwent ureteroscopic evaluation before additional surgical intervention. We believe that endoscopic evaluation is an important part of the work-up in patients presenting with ureteral obstruction. If endoscopic evaluation in such patients is unclear, then one may consider obtaining a PET scan to help elucidate the disease process. However, if there is a high level of suspicion for malignant obstruction, then operative intervention for tissue diagnosis should be considered. We had planned and consented both of these patients for ureterolysis and possible pyeloplasty or segmental resection depending on the intraoperative findings. If we had not been able to obtain pathologic diagnosis or the ureteral obstruction was not relieved with ureterolysis alone, then we would have likely proceeded with resection and reanastomosis.
Conclusion
Hydronephrosis secondary to periureteral lymphoma is a rare etiology for ureteral obstruction. These cases serve as examples of an important differential for hydronephrosis as these patients lacked diffuse retroperitoneal lymphadenopathy, disseminated disease, or a known cancer diagnosis, which is typical for patients with malignant extrinsic ureteral compression from lymphoma or other diseases. Future studies are needed to further evaluate the variety of etiologies, presentations, and the best management options for our patients with malignant ureteral obstruction.
Abbreviations Used
- CT
computed tomography
- MRI
magnetic resonance imaging
- PET
positron emission tomography
Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
Cite this article as: Whiles BB, Duchene DA (2020) Periureteral marginal zone lymphoma resulting in hydronephrosis and flank pain in the absence of disseminated disease: case report of two patients presenting with rare but important differential, Journal of Endourology Case Reports 6:4, 519–522, DOI: 10.1089/cren.2020.0184
References
- 1. Haas CR, Shah O, Hyams ES. Temporal trends and practice patterns for inpatient management of malignant extrinsic ureteral obstruction in the United States. J Endourol 2020;34:828–835 [DOI] [PubMed] [Google Scholar]
- 2. Lontos K, Tsagianni A, Msaouel P, et al. Primary urinary tract lymphoma: Rare but aggressive. Anticancer Res 2017;37:6989–6995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Naranji I, Zakri RH, Liston T. Mantle cell lymphoma presenting as a pelvi-ureteric junction obstruction: A case report. J Med Case Rep 2013;7:105. [DOI] [PMC free article] [PubMed] [Google Scholar]