Abstract
Background
The improved life expectancy observed in patients living with human immunodeficiency virus (HIV) infection has made age‐related cardiovascular complications, including arrhythmias, a growing health concern.
Hypothesis
We describe the temporal trends in frequency of various arrhythmias and assess impact of arrhythmias on hospitalized HIV patients using the Nationwide Inpatient Sample (NIS).
Methods
Data on HIV‐related hospitalizations from 2005 to 2014 were obtained from the NIS database using International Classification of Diseases, 9th Revision (ICD‐9) codes. Data was further subclassified into hospitalizations with associated arrhythmias and those without. Baseline demographics and comorbidities were determined. Outcomes including in‐hospital mortality, cost of care, and length of stay were extracted. SAS 9.4 (SAS Institute Inc., Cary, NC) was utilized for analysis. A multivariable analysis was performed to identify predictors of arrhythmias among hospitalized HIV patients.
Results
Among 2 370 751 HIV‐related hospitalizations identified, the overall frequency of any arrhythmia was 3.01%. Atrial fibrillation (AF) was the most frequent arrhythmia (2110 per 100 000). The overall frequency of arrhythmias increased over time by 108%, primarily due to a 132% increase in AF. Arrhythmias are more frequent among older males, lowest income quartile, and nonelective admissions. Patients with arrhythmias had a higher in‐hospital mortality rate (9.6%). In‐hospital mortality among patients with arrhythmias decreased over time by 43.8%. The cost of care and length of stay associated with arrhythmia‐related hospitalizations were mostly unchanged.
Conclusions
Arrhythmias are associated with significant morbidity and mortality in hospitalized HIV patients. AF is the most frequent arrhythmia in hospitalized HIV patients.
Keywords: arrhythmia, atrial fibrillation, frequency, human immunodeficiency virus (HIV)
1. INTRODUCTION
According to the Center for Disease Control and Prevention (CDC), there were 39 782 incident cases of human immunodeficiency virus (HIV) infection in 2016 in the United States. 1 Access to effective antiretroviral therapy (ART) has substantially reduced HIV mortality, acquired immune deficiency syndrome (AIDS), and AIDS‐related hospitalizations. This has led to an overall improved life expectancy in the HIV patient population. 2 However, in the aging HIV‐infected population, cardiovascular complications such as hypertension, coronary artery disease (CAD) and heart failure have become a growing health concern. 3 , 4 , 5 , 6 Other contributors such as the HIV infection itself, immune dysfunction, chronic inflammation, ART exposure and toxicity are also implicated in heart disease and can lead to complications such as myocardial infarction and cardiomyopathy. 7 , 8 In addition, arrhythmias are also important contributors to cardiovascular morbidity and mortality in patients with HIV. 9 , 10 The temporal trends of the frequency and outcome of arrhythmias in patients with HIV have not been adequately described.
2. METHODS
The primary objective of this study was to describe the temporal trends in the frequency of arrhythmias among hospitalized HIV patients. Secondary objectives included identifying comorbidities associated with arrhythmias in this cohort as well as determine the outcomes associated with arrhythmias including in‐hospital mortality, length of stay, and cost of care.
2.1. Data source
The data were obtained from the Nationwide Inpatient Sample (NIS) data set from 2005 to 2014. 11 The NIS is a nationally representative survey of hospitalizations conducted by the Healthcare Cost and Utilization Project in collaboration with the participating states. It is the largest inpatient data set in the United States and includes a sample of US community hospitals that approximates 20% of all US community hospitals. 12 No institutional review board approval was sought because of the publicly available de‐identified data set used in this research.
2.2. Study population
Our target population consisted of HIV‐related hospitalizations from January 1, 2005 to December 21, 2014. We included hospital admissions with a diagnosis of HIV infection in primary and secondary diagnostic field during our study period. We subclassified this group into hospitalizations with associated cardiac arrhythmia and those without arrhythmia for trend analysis using ICD codes for cardiac arrhythmias such as ventricular tachycardia (VT), ventricular fibrillation (VF), supraventricular tachycardia (SVT), AF, and atrial flutter (AFL). Interventions such as ICD implantation, use of vasopressors, cardiac catheterization, endotracheal intubation, and CPR were identified.
2.3. Definition of variables
We used NIS variables to identify patient level and hospital level variables. We divided age into 4 subgroups: 18 to 49 years of age, 50 to 64 years of age, 65 to 79 years of age, and 80 years of age and older. We defined the severity of comorbid conditions by using the Deyo modification of the Charlson Comorbidity Index. Co‐morbidities associated with hospitalization for HIV infection were identified using AHRQ comorbidity measures, that is, by using ICD‐9‐CM diagnoses and the Diagnosis Related Group (DRG) in effect on the discharge date. 13
2.4. In hospital mortality, cost, and length of stay
In‐hospital mortality was defined as death from any cause during the same hospital stay. LOS was already provided by the Healthcare Cost and Utilization Project (HCUP) for each entry. The HCUP NIS contains data on total charges for each hospital in the databases, which represents the amount that hospitals billed for services. To calculate estimated cost of hospitalizations, the NIS data were merged with Cost to Charge Ratios (CCR) available from HCUP. 14 , 15 Using the merged data elements from the CCR files and the total charges reported in the NIS database, we converted the hospital total charge data to cost estimates by simply multiplying total charges with the appropriate CCR. These costs are essentially standardized, can be measured across hospitals, and are used for the remainder of this report.
2.5. Statistical analysis
The statistical software package SAS 9.4 (SAS Institute Inc., Cary, NC) was utilized for the analyses. Since NIS represents a 20% stratified random sample of US hospitals, analyses were performed using hospital‐level discharge weights to obtain national estimates of arrhythmia associated with HIV hospitalizations. For categorical variables, the modified chi‐squared test of trend for proportions (Cochrane Armitage test) was used. For continuous variable, simple linear regression was used. Multivariable models for predictors of arrhythmia were performed with independent variables which were either clinically significant or statistically significant in univariate model. Multivariate model included patient‐level variables such as age and gender; year of admission, admission type (elective vs nonelective), co‐morbidities such as diabetes mellitus, chronic lung disease, peripheral vascular disease etc.; hospital course requiring ICD implantation, use of vasopressors, cardiac catheterization, endotracheal intubation and CPR. A P‐value <.05 was deemed statistically significant.
3. RESULTS
We identified 2 370 751 HIV‐related hospitalizations from January 1, 2005 through December 31, 2014. The frequency of all variables is per 100 000 hospitalizations, unless specifically mentioned.
3.1. Frequency of arrhythmias
Among 2 370 751 HIV‐related hospitalizations, 71 285 hospitalizations had either a primary or secondary arrhythmia‐related diagnosis. This amounts to a 3.01% frequency of arrhythmia‐related diagnoses in HIV related hospitalization (Table 1). The frequency of specific arrhythmias (per 100 000 hospitalizations) in the study was as follows: 2110 AF, 560 VT, 420 AFL, 170 SVT, and 130 VF.
TABLE 1.
Comparison of baseline characteristics and course of hospitalization between HIV patients with arrhythmias and without arrhythmias from 2005 through 2014
| Patients with arrhythmia | Patients without arrhythmia | Overall | P value | |
|---|---|---|---|---|
| Primary admission | 71 285 (3.01%) | 2 299 466 | 2 370 751 | |
| Patient level variables | ||||
| Age | <.0001 | |||
| 18‐49 | 30.42 | 62.2 | 61.24 | |
| 50‐64 | 49.25 | 33.38 | 33.85 | |
| 65‐79 | 18.47 | 4.21 | 4.64 | |
| ≥80 | 1.87 | 0.22 | 0.27 | |
| Gender | <.0001 | |||
| Male | 76.42 | 65.73 | 66.05 | |
| Female | 23.58 | 34.27 | 33.95 | |
| Deyo/Charlson Score | <.0001 | |||
| <2 | 18.36 | 27.58 | 27.3 | |
| >=2 | 81.64 | 72.42 | 72.7 | |
| Hospital course | ||||
| Use of vasopressor | 1.3 | 0.24 | 0.28 | <.0001 |
| Cardiac catheterization | 7.17 | 1.54 | 1.71 | <.0001 |
| Endotracheal intubation | 12.74 | 3.7 | 3.97 | <.0001 |
| CPR | 3.4 | 0.41 | 0.5 | <.0001 |
| Cardiogenic shock | 1.9 | 0.12 | 0.17 | <.0001 |
| Cardiac arrest | 4.09 | 0.42 | 0.53 | <.0001 |
| Median household income category for patient's zip code | <.0001 | |||
| 1. 0‐25th percentile | 44.85 | 49.39 | 49.25 | |
| 2. 26‐50th percentile | 22.9 | 23.05 | 23.05 | |
| 3. 51‐75th percentile | 19.16 | 17.03 | 17.09 | |
| 4. 76‐100th percentile | 13.09 | 10.54 | 10.61 | |
| Primary payer | <.0001 | |||
| Medicare/Medicaid | 74.72 | 70.13 | 70.27 | |
| Private including HMO | 17.36 | 15.7 | 15.75 | |
| Self‐pay/no charge/other | 7.8 | 13.95 | 13.76 | |
| Missing | 0.12 | 0.22 | 0.22 | |
| Admission type | <.0001 | |||
| Nonelective | 90.77 | 88.28 | 88.36 | |
| Elective | 9.23 | 11.72 | 11.64 | |
| Admission day | <.0001 | |||
| Weekdays | 78.14 | 78.85 | 78.83 | |
| Weekend | 21.86 | 21.15 | 21.17 | |
| Hospital characteristics | ||||
| Hospital bed size | <.0001 | |||
| Small | 8.64 | 9.38 | 9.36 | |
| Medium | 24.47 | 24.3 | 24.31 | |
| Large | 66.89 | 66.32 | 66.34 | |
| Hospital teaching status | <.0001 | |||
| Nonteaching | 30.75 | 29.33 | 29.38 | |
| Teaching | 69.25 | 70.67 | 70.62 | |
| Discharge | <.0001 | |||
| Home | 68.33 | 78.78 | 78.46 | |
| Facility | 19.04 | 12.76 | 12.95 | |
| In hospital mortality | 9.6 | 2.84 | 3.04 | <.0001 |
| Length of stay during index admission in days (median, IQR) | 5(3‐10) | 4 (2‐7) | 4 (2‐7) | <.0001 |
| Cost of care (median, IQR) | 12 210 (6248‐26 167) | 7577 (4401‐14 083) | 7665 (4435‐14 336) | <.0001 |
Abbreviations: CPR, cardiopulmonary resuscitation; HMO, Health Maintenance Organization; IQR, interquartile range.
From 2005 through 2014, the frequency of arrhythmia among HIV‐related hospitalizations increased by 108% (from 4412 in 2005 to 9435 in 2014). This increase in arrhythmia was primarily the result of the increased frequency of AF (132.5% increase, from 2898 patients in 2005 to 6955 in 2014), followed by VT (72.1% increase, from 985 in 2005 to 1735 in 2014) and AFL (192.7% increase, from 427 in 2005 to 1265 in 2014). The frequency of SVT has increased marginally over the years (14.8% increase) relative to other arrhythmias, as shown in Figure 1 (P < .001 for all trends).
FIGURE 1.
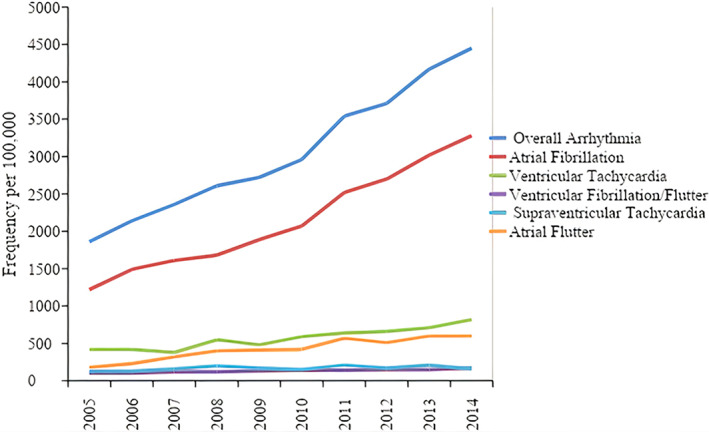
Frequency of arrhythmia‐related hospitalizations by arrhythmia type for the entire study period
3.2. Demographics
Baseline characteristics of HIV‐related hospitalizations with arrhythmias are summarized in Table 2. Arrhythmias were most commonly present in patients aged 50 to 64 (49.3%). This is in contrast to the predominantly younger age group found in all hospitalizations. 61.2% of hospitalized HIV patients were in the 18 to 49 age range, and the 50 to 64 age group comprised 33.9% of all hospitalizations. While there was an increase in frequency of arrhythmias in all age groups, the increase in frequency was greatest in patients aged 18 to 49 (81% relative increase). Figure 2 illustrates the temporal trends in frequency of any arrhythmia per 100 000 HIV hospitalizations within various age groups.
TABLE 2.
Baseline characteristics and course of hospitalization among hospitalized HIV patients from 2005 through 2014
| 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Overall | Relative change (%) | P value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary admission | 4412 | 5629 | 5709 | 6197 | 6776 | 7873 | 8414 | 7955 | 8885 | 9435 | 71 285 | 108 | <.0001 |
| Patient level variables | |||||||||||||
| Age | |||||||||||||
| 18‐49 | 1060 | 1190 | 1350 | 1430 | 1390 | 1630 | 1780 | 1870 | 1750 | 1940 | 1490 | 81 | <.0001 |
| 50‐64 | 3460 | 3640 | 3680 | 3900 | 3870 | 3860 | 4680 | 4810 | 5550 | 5590 | 4370 | 64 | <.0001 |
| 65‐79 | 8750 | 9980 | 10 980 | 10 470 | 11 360 | 12 020 | 12 820 | 11 970 | 13 660 | 14 010 | 11 970 | 53 | <.0001 |
| ≥80 | 26 710 | 13 930 | 14 970 | 17 900 | 17 630 | 21 020 | 23 470 | 21 710 | 18 090 | 27 640 | 20 810 | 19 | <.0001 |
| Gender | |||||||||||||
| Male | 2120 | 2530 | 2730 | 3050 | 3260 | 3410 | 4080 | 4190 | 4880 | 5080 | 3480 | 138 | <.0001 |
| Female | 1310 | 1400 | 1690 | 1750 | 1650 | 2130 | 2490 | 2770 | 2780 | 3250 | 2090 | 147 | <.0001 |
| Deyo/Charlson score | |||||||||||||
| <2 | 1380 | 1620 | 1550 | 2060 | 1920 | 2050 | 2250 | 2070 | 2640 | 2740 | 2020 | 90 | <.0001 |
| ≥2 | 2040 | 2330 | 2650 | 2800 | 3010 | 3290 | 4040 | 4370 | 4820 | 5170 | 3380 | 156 | <.0001 |
| Comorbidities | |||||||||||||
| Hyperlipidemia | 3540 | 4350 | 4430 | 4990 | 5280 | 6750 | 6350 | 7430 | 8080 | 7930 | 6350 | 133 | <.0001 |
| History of hypertension | 2960 | 3510 | 3850 | 4100 | 4360 | 4520 | 5480 | 5650 | 6180 | 6580 | 4830 | 119 | <.0001 |
| Diabetes mellitus | 2530 | 3770 | 3920 | 4110 | 4440 | 4570 | 5670 | 6110 | 6550 | 7110 | 5000 | 165 | <.0001 |
| Chronic pulmonary disease | 2400 | 3030 | 3220 | 3430 | 3280 | 3600 | 4460 | 5080 | 5760 | 5880 | 4070 | 144 | <.0001 |
| Peripheral vascular disease | 5230 | 5010 | 7930 | 8040 | 6250 | 7980 | 9110 | 10 050 | 11 100 | 11 850 | 8820 | 123 | <.0001 |
| Neurological disorder or paralysis | 1970 | 2410 | 2160 | 2670 | 2790 | 2890 | 3620 | 3470 | 4230 | 5140 | 3160 | 141 | <.0001 |
| Hematological or oncological malignancy | 2520 | 2300 | 3320 | 3440 | 3260 | 4260 | 3980 | 4040 | 4090 | 4850 | 3660 | 86 | <.0001 |
| Anemia | 1690 | 1990 | 2330 | 2780 | 2940 | 3210 | 4170 | 4320 | 4870 | 5400 | 3430 | 219 | <.0001 |
| Obesity | 3080 | 3640 | 4700 | 4890 | 3980 | 5140 | 4380 | 5890 | 6630 | 6940 | 5310 | 108 | <.0001 |
| Coronary artery disease | 7390 | 8120 | 8300 | 9210 | 9350 | 9630 | 11 090 | 11 660 | 12 080 | 13 110 | 10 330 | 75 | <.0001 |
| History of previous myocardial infarction | 7050 | 5930 | 8140 | 10 290 | 7660 | 8350 | 11 630 | 10 860 | 10 860 | 12 570 | 9730 | 79 | <.0001 |
| History of previous CABG | 9200 | 6720 | 6970 | 9440 | 11 930 | 11 750 | 14 650 | 14 220 | 14 850 | 15 180 | 12 210 | 96 | <.0001 |
| Congestive heart failure | 9850 | 10 530 | 13 190 | 11 980 | 11 750 | 13 640 | 14 980 | 15 550 | 17 870 | 16 890 | 14 020 | 76 | <.0001 |
| Renal failure | 4570 | 4690 | 5090 | 5500 | 5360 | 5960 | 7420 | 8030 | 8400 | 8870 | 6530 | 102 | <.0001 |
| Hospital course | |||||||||||||
| Use of vasopressor | 10 640 | 9320 | 12 270 | 9640 | 16 270 | 15 110 | 13 180 | 14 770 | 17 710 | 16 590 | 14 180 | 69 | <.0001 |
| Cardiac catheterization | 9310 | 10 480 | 11 400 | 12 110 | 13 430 | 12 940 | 10 780 | 14 250 | 14 150 | 16 050 | 12 590 | 56 | <.0001 |
| Endotracheal intubation | 6840 | 6910 | 8780 | 8350 | 9680 | 9230 | 11 000 | 10 940 | 12 670 | 12 750 | 9650 | 89 | <.0001 |
| CPR | 14 460 | 14 360 | 19 390 | 18 440 | 16 730 | 21 120 | 20 490 | 26 470 | 25 220 | 29 380 | 20 480 | 97 | <.0001 |
| Cardiogenic shock | 28 090 | 22 160 | 25 100 | 28 000 | 34 320 | 34 470 | 36 550 | 35 400 | 30 100 | 37 600 | 32 900 | 42 | <.0001 |
| Cardiac arrest | 14 020 | 15 370 | 18 960 | 18 620 | 20 220 | 20 510 | 21 620 | 25 520 | 26 140 | 28 650 | 21 060 | 97 | <.0001 |
| Median household income category for patient's zip code | |||||||||||||
| 1. 0‐25th percentile | 1840 | 2080 | 2170 | 2490 | 2490 | 2740 | 3430 | 3470 | 3850 | 4050 | 2800 | 124 | <.0001 |
| 2. 26‐50th percentile | 1740 | 2290 | 2360 | 2390 | 2940 | 3140 | 3600 | 3900 | 4300 | 4750 | 3050 | 165 | <.0001 |
| 3. 51‐75th percentile | 1890 | 2160 | 2540 | 3310 | 3470 | 3300 | 4530 | 4480 | 4830 | 5170 | 3440 | 177 | <.0001 |
| 4. 76‐100th percentile | 2350 | 2540 | 3130 | 3280 | 3570 | 4190 | 4760 | 4830 | 5640 | 5310 | 3790 | 144 | <.0001 |
| Primary payer | |||||||||||||
| Medicare/Medicaid | 1900 | 2280 | 2550 | 2670 | 2780 | 3190 | 3750 | 3960 | 4470 | 4760 | 3200 | 149 | <.0001 |
| Private including HMO | 2390 | 2190 | 2750 | 3160 | 3430 | 3370 | 3910 | 3950 | 4240 | 4140 | 3310 | 87 | <.0001 |
| Self‐pay/no charge/other | 1020 | 1460 | 1290 | 1590 | 1760 | 1570 | 1830 | 2060 | 2360 | 2810 | 1710 | 143 | <.0001 |
| Admission type | |||||||||||||
| Nonelective | 1910 | 2250 | 2460 | 2640 | 2730 | 3080 | 3610 | 3790 | 4270 | 4600 | 3090 | 138 | <.0001 |
| Elective | 1550 | 1310 | 1630 | 2360 | 2610 | 2250 | 3030 | 3120 | 3360 | 3290 | 2380 | 138 | <.0001 |
| Hospital characteristics | |||||||||||||
| Hospital bed size | |||||||||||||
| Small | 2110 | 1910 | 1900 | 2360 | 2230 | 2960 | 3170 | 3050 | 3540 | 4050 | 2770 | 98 | <.0001 |
| Medium | 1330 | 2000 | 2470 | 2870 | 2800 | 3000 | 3160 | 3760 | 4260 | 4730 | 3030 | 221 | <.0001 |
| Large | 2040 | 2230 | 2370 | 2560 | 2710 | 2980 | 3730 | 3800 | 4250 | 4430 | 3030 | 125 | <.0001 |
| Discharge | |||||||||||||
| Home | 1670 | 1890 | 2040 | 2280 | 2370 | 2550 | 3080 | 3230 | 3650 | 3790 | 2620 | 130 | <.0001 |
| Facility | 2350 | 2990 | 2930 | 3600 | 4100 | 4200 | 5260 | 5570 | 6610 | 7130 | 4420 | 201 | <.0001 |
| Length of stay during index admission in days (median, IQR) | 6 (3‐11) | 6 (3‐11) | 5 (3‐10) | 5 (3‐10) | 5 (3‐9) | 5 (3‐10) | 5 (3‐9) | 5 (2‐9) | 5 (2‐9) | 5 (3‐10) | 5 (3‐10) | .0483 | |
| Cost of care (median, IQR) | 12 285 (6446‐27 184) | 12 974 (6502‐27 557) | 12 181 (6117‐26 158) | 11 486 (6107‐25 911) | 12 362 (6029‐25 850) | 12 029 (6210‐25 024) | 12 570 (6396‐25 312) | 12 043 (6274‐25 683) | 11 602 (6111‐25 629) | 12 410 (6410‐27 253) | 12 210 (6248‐26 167) | .4019 |
Abbreviations: CABG, coronary artery bypass graft; CPR, cardiopulmonary resuscitation; HMO, Health Maintenance Organization; ICD, implantable cardioverter defibrillator; IQR, interquartile range.
FIGURE 2.
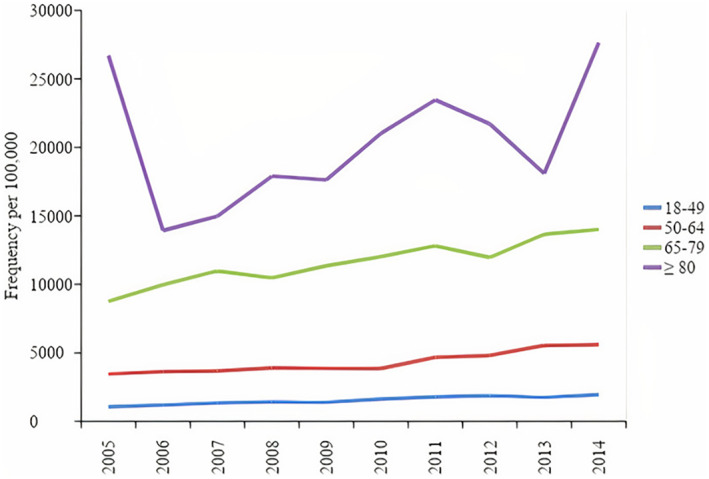
Temporal trends in frequency of any arrhythmia per 100 000 HIV hospitalizations within various age groups
The majority of arrhythmias were present in males (76.42%) compared to females (23.58%). Over the years, there was a comparable increase in the frequency of arrhythmias among both genders (138% in males and 147% in females). Arrhythmias were most frequent in patients within lowest quartile for household income (0‐25th percentile, 44.85%). Arrhythmias were less frequent with every increase in quartile for household income. Similar to all HIV hospitalizations, patients with arrhythmias were most commonly admitted nonelectively (90.77%). Patients with arrhythmia had a greater burden of comorbidities, as evidenced by a Deyo/Charlson score of ≥2, which was present in 81.64% of patients with any arrhythmia, compared to 72.42% found in patients with no arrhythmias (P < .0001).
Among all comorbidities assessed, patients with any arrhythmia had a significantly greater frequency of hypertension (55.56% vs 33.94%), congestive heart failure (31.73% vs 6.03%), renal failure (29.06% vs 12.9%), chronic pulmonary disease (26.23% vs 19.16%), CAD (24.31% vs 6.54%), diabetes mellitus (23.43% vs 13.8%), hyperlipidemia (22.22% vs 10.16%), previous myocardial infarction (8.24% vs 2.37%), previous CABG (4.23% vs 0.94%) and obesity (6.98% vs 3.86%) compared to hospitalized patients with no arrhythmias (P < .0001 for all comorbidities) (Figure 3).
FIGURE 3.
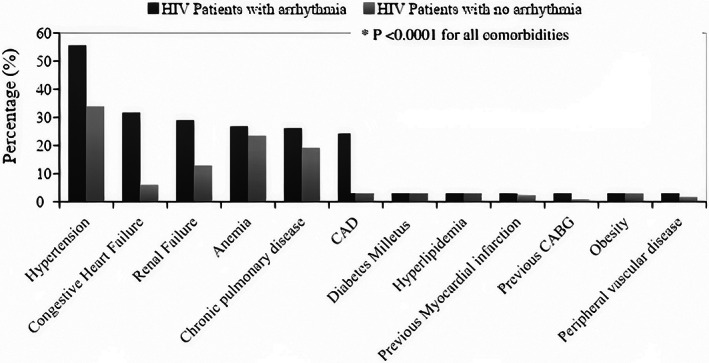
Percentage of comorbidities among HIV patients with arrhythmia and with no arrhythmia. CABG, coronary artery bypass graft; CAD, coronary artery disease
3.3. Hospital course in patients with any arrhythmia
Hospitalization course among patients with arrhythmias is summarized in Table 2. HIV‐related hospitalizations with arrhythmias had a statistically significant longer average length of stay, compared to without arrhythmias (5 days vs 4 days; P < .0001). The median cost of care was significantly higher in patients with arrhythmias compared to all hospitalizations ($12 210 vs $7665, IQR $6248‐$26 167 in patients with arrhythmias and $4435‐$14 336 in all hospitalizations; P < .0001). The median length of stay and cost of care in HIV‐related hospitalizations with arrhythmias has mostly remained unchanged over the years (P value of .0483 and .4019 respectively).
Markers of increased disease severity were more common among HIV‐related hospitalizations with arrhythmia compared to patients with no arrhythmia. These include vasopressor use (1.3% vs 0.24%), cardiac catheterization (7.17% vs 1.54%), cardiac arrests (4.09% vs 0.42%), CPR (3.4% vs 0.41%) and endotracheal intubation (12.75% vs 3.7%).
All‐cause in‐hospital mortality was associated with the presence of any cardiac arrhythmia. Patients with arrhythmias had an in‐hospital mortality rate of 9.6%, as opposed to a rate 2.84% found in patients with no arrhythmia. However, the in‐hospital mortality rate in patients with any arrhythmia has decreased over the years from 12.35% in 2005 to 7.9% in 2014 (decrease of 43.8%; P < .001 for trend). Among the arrhythmias, the highest reduction in in‐hospital mortality was observed in patients with VT (decrease of 57.5%; P < .0001 for trend).
As anticipated, the highest in‐hospital mortality was associated with patients who had VF (46.11%), followed by VT (14.48%), SVT (8.73%), and atrial flutter (7.51%). Despite being the most frequent arrhythmia in HIV patients, AF was associated with the lowest in‐hospital mortality (6.8%). Results for in‐hospital mortality throughout the years, stratified by arrhythmia type are summarized in Table 3.
TABLE 3.
In‐hospital mortality in hospitalized HIV patients from 2005 through 2014, stratified by arrhythmia type
| (%) | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Overall | Relative change (%) | P value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall arrhythmia | 12.35 | 11.21 | 12.97 | 10.7 | 10.21 | 10.31 | 9.19 | 7.48 | 7.32 | 7.9 | 9.6 | −43.8 | <.0001 |
| Ventricular tachycardia | 13.32 | 16.11 | 18.56 | 22.2 | 18.32 | 17.09 | 12.67 | 8.83 | 9.93 | 11.24 | 14.48 | −57.5 | <.0001 |
| Ventricular fibrillation/flutter | 56.58 | 50.89 | 57.93 | 49.57 | 47.67 | 46.64 | 42.28 | 39.39 | 42.19 | 34.72 | 46.11 | −36.0 | <.0001 |
| Supraventricular tachycardia | 9.77 | 4.22 | 7.68 | 10.38 | 10.42 | 9.33 | 11.64 | 9.72 | 5.49 | 7.58 | 8.73 | 1.2 | <.0001 |
| Atrial fibrillation | 9.71 | 9.19 | 9.95 | 5.67 | 6.7 | 7.01 | 6.85 | 5.52 | 5.13 | 5.61 | 6.8 | −47.0 | <.0001 |
| Atrial flutter | 12.79 | 4.51 | 9.56 | 8.43 | 7.18 | 6.02 | 7.84 | 4.07 | 7.48 | 9.49 | 7.51 | −16.8 | <.0001 |
Note: Values are presented as percentages (%).
3.4. Association of arrhythmias in HIV patients with demographics and comorbidities
On multivariate analysis, later year of admission had a higher odds ratio (OR) for arrhythmia among HIV patients compared to earlier years (year 2014 vs 2005 OR was 1.391; P < .0001). Older age was also associated with arrhythmias (OR 1.055; P < .0001). Female sex was associated with lower odds of arrhythmias (OR 0.689, P < .0001).
Among comorbidities assessed, congestive heart failure had the strongest correlation with arrhythmias (OR 3.345; P < .0001), followed by obesity (OR 1.504; P < .0001), coronary artery disease (OR 1.46; P < .0001), renal failure (OR 1.397; P < .0001), hypertension (OR 1.205; P < .0001), and chronic pulmonary disease (OR 1.183; P < .0001).
In addition, cardiogenic shock, cardiac arrest and endotracheal intubation had high odds for arrhythmias (OR 3.18, 2.966, and 2.261, respectively; P < .0001).
Higher income was associated with arrhythmia‐related hospitalization in HIV patients (OR 1.279 in patients with top quartile for income; P < .0001). Other variables assessed were not strongly associated with arrhythmias. The multivariate predictors for arrhythmias are detailed in Table 4.
TABLE 4.
Multivariate predictors of arrhythmias in hospitalized HIV patients
| Variables | OR | LL | UL | P‐value |
|---|---|---|---|---|
| Year 2014 vs 2005 | 1.391 | 1.271 | 1.521 | <.0001 |
| Age | 1.055 | 1.053 | 1.057 | <.0001 |
| Female | 0.689 | 0.658 | 0.721 | <.0001 |
| Comorbidities | ||||
| Hyperlipidemia | 1.116 | 1.06 | 1.175 | <.0001 |
| History of hypertension | 1.205 | 1.155 | 1.257 | <.0001 |
| Diabetes mellitus | 0.936 | 0.889 | 0.985 | .0116 |
| Chronic pulmonary disease | 1.183 | 1.132 | 1.238 | <.0001 |
| Peripheral vascular disease | 1.133 | 1.035 | 1.239 | .0069 |
| Neurological disorder or paralysis | 0.988 | 0.928 | 1.053 | .718 |
| Hematological or oncological malignancy | 1.088 | 1.006 | 1.177 | .0339 |
| Anemia | 0.964 | 0.922 | 1.007 | .0963 |
| Obesity | 1.504 | 1.391 | 1.627 | <.0001 |
| Coronary artery disease | 1.46 | 1.375 | 1.549 | <.0001 |
| History of previous myocardial infarction | 1.178 | 1.087 | 1.276 | <.0001 |
| History of previous CABG | 1.099 | 0.985 | 1.225 | .0909 |
| Congestive heart failure | 3.345 | 3.192 | 3.505 | <.0001 |
| Renal failure | 1.397 | 1.331 | 1.465 | <.0001 |
| Hospital course | ||||
| Use of vasopressor | 1.817 | 1.503 | 2.196 | <.0001 |
| Cardiac catheterization | 1.748 | 1.602 | 1.907 | <.0001 |
| Endotracheal intubation | 2.261 | 2.11 | 2.424 | <.0001 |
| CPR | 1.916 | 1.642 | 2.234 | <.0001 |
| Cardiogenic shock | 3.18 | 2.63 | 3.847 | <.0001 |
| Cardiac arrest | 2.966 | 2.573 | 3.42 | <.0001 |
| Median household income category for patient's zip code | ||||
| 0‐25th percentile | Referent | Referent | Referent | |
| 26‐50th percentile | 1.111 | 1.058 | 1.166 | .0499 |
| 51‐75th percentile | 1.233 | 1.171 | 1.299 | .0002 |
| 76‐100th percentile | 1.279 | 1.203 | 1.359 | <.0001 |
| Primary payer | ||||
| Medicare/medicaid | Referent | Referent | Referent | |
| Private including HMO | 1.201 | 1.141 | 1.264 | <.0001 |
| Self pay/no charge/other | 0.843 | 0.786 | 0.905 | <.0001 |
| Elective vs nonelective | 0.808 | 0.757 | 0.862 | <.0001 |
| weekdays vs weekend | 1.016 | 0.971 | 1.064 | .4938 |
| Hospital bed size | ||||
| Small | Referent | Referent | Referent | |
| Medium | 1.115 | 1.038 | 1.198 | .0261 |
| Large | 1.111 | 1.04 | 1.186 | .021 |
| Teaching vs nonteaching | 0.971 | 0.932 | 1.011 | .1489 |
Abbreviations: CABG, coronary artery bypass graft; CPR, cardiopulmonary resuscitation; HMO, Health Maintenance Organization.
4. DISCUSSION
In this analysis of HIV‐related hospitalizations from 2005 through 2014, we report an increase in the frequency of arrhythmias over time in this patient cohort. The presence of arrhythmia is associated with adverse outcomes, including a higher rate of in‐hospital mortality. In the current study, we report a 108% overall increase in the frequency of arrhythmia among HIV patients during the study period. To the best of our knowledge, this is the first study describing the temporal trends of arrhythmias in hospitalized HIV patients over time.
We found the following variables to be independently associated with the presence of arrhythmia in HIV‐related hospitalizations: male sex, older age, higher income, later year of admission and the presence of comorbidities such as congestive heart failure, obesity, coronary artery disease (CAD), renal failure, hypertension, chronic pulmonary disease, history of previous myocardial infarction, and peripheral vascular disease. It is notable that the frequency of these comorbidities has also increased over time, which could explain the rise in overall frequency of arrhythmias during the study period. Although the association between all‐cause in‐hospital mortality and arrhythmia was significant, the mortality rate among patients with any arrhythmia declined over the time. The contributory factors to this decrease are unclear, but could relate to improved diagnosis and management of cardiovascular disease. This trend was consistent with the decrement in all‐cause mortality found in HIV patients in general, as reported by multiple studies worldwide. 16 , 17 , 18
AF was the most frequent arrhythmia among hospitalized HIV patients. Our reported frequency of AF was 2.11%. This is concordant with a previous analysis of the Veterans Affairs HIV Clinical Case Registry, which reported a frequency of 2.6% of atrial fibrillation in a large cohort of over 30 000 HIV patients from 1996 to 2011. 9
While our study does not address the mechanisms underlying the significant frequency of arrhythmias in the setting of HIV, other studies provide insight. HIV infection is a known risk factor for atherosclerosis and stroke, 19 , 20 and similar mechanisms can explain the incidence of arrhythmias in that population. Both advanced age and inflammation have been associated with an increased risk for developing arrhythmias such as AF, 21 , 22 making older patients with chronic HIV particularly susceptible to developing it. Indeed, persistent immunodeficiency, accelerated immunosenescence and inflammation in HIV patients were found to accelerate the onset of age‐associated diseases, including cardiovascular diseases and arrhythmias such as AF. 23 Elution of inflammatory cytokines and reactive oxygen species by infected cardiac endothelium; expression of HIV‐associated proteins that lead to destruction of mitochondria and myocardial damage are mechanisms previously implicated in the pathogenesis of AF in HIV infected patients. 24 The severity of the HIV infection also correlates with risk of developing AF. A previous analysis identified low CD4+ cell count and high HIV RNA viral load as independent variables for the development of AF in HIV patients. 9 The exact mechanism underlying this correlation is difficult to establish given that many patients in the HIV population share similar risk factors for AF, such as CAD and heart failure, as demonstrated by our study. Additionally, components of highly active antiretroviral therapy (HAART) such as protease inhibitors are associated with development of metabolic syndrome, which is a risk factor for AF. 25
In our study, the frequency of malignant arrhythmias such as VF and VT has increased over the years. While the reason behind this rise is unclear, previous studies showed that patients with HIV can have a prolonged QTc, predisposing them to malignant arrhythmias including Torsades de Pointes, sustained VT and VF. This prolongation can be a direct result of the HIV infection itself, and can be observed in the absence of overt cardiovascular disease. 6 , 26 The severity of the HIV infection, evidenced by a low CD4+ cell count and high viral load, has been shown to be a risk factor for the development sudden cardiac death (SCD). 10 Furthermore, medications frequently administered to HIV patients, including pentamidine, TMP‐SMX (Trimethoprime‐Sulfamethoxazole), non‐nucleoside reverse transcriptase inhibitor efavirenz (Sustiva), and protease inhibitors such as atazanavir (Reyataz), 27 have also been associated with QTc prolongation. 6 , 28 , 29 It is possible that the widespread use of such medications contributed to the rise of malignant arrhythmias in the HIV population over the years. The increased frequency CAD and CHF in the HIV population, as shown by our study, have likely contributed to the rise of such arrhythmias. These findings call for increased scrutiny to the QTc interval in HIV patients, and warrant considering HIV disease status in the risk assessment of malignant arrhythmias.
5. STUDY LIMITATIONS
Our study has a number of limitations. First, there are constraints with using administrative databases such as the NIS. It is a de‐identified database; making it impossible to validate individual ICD‐9 codes. Electrocardiograms and telemetry strips were not available to validate the type of arrhythmia in our sample. Furthermore, the use of ICD‐9 codes does not indicate whether the arrhythmia coded is new onset or existed prior to the ascertained hospitalization. The NIS also does not provide long term follow‐up data. It regards each hospitalization as a separate entity, so it is possible that readmissions were regarded as distinct hospitalizations, leading to an overestimation in the number of hospitalizations. The cause of in‐hospital mortality could not be ascertained since hospitalization notes are unavailable through the NIS. It is uncertain whether changes in coding practice patterns contribute to the changes in reported arrhythmia frequency, using NIS methodology. Furthermore, we cannot completely exclude the possibility that additional unknown confounding variables, not included in our analysis, may explain some of the associations found. We could not, for instance, ascertain the extent at which concurrent medication use such as anti‐retroviral therapy (ART) impacted the incidence of arrhythmias, nor could we determine the relationship between disease severity (CD4 count or viral load) and arrhythmia risk.
Future studies should be aimed at investigating the various drug regimens for HIV and their associated risk of developing arrhythmias. Data on CD4+ cell count and HIV viral load was not collected in our sample as they were not available through the NIS. Lastly, our sample did not include uninfected controls to directly compare the burden of arrhythmias between HIV and non‐HIV patients. Unfortunately this comparison was not feasible to perform due to the very large number of uninfected controls available through the NIS registry. Such a study is warranted to determine if HIV infection is an independent risk factor for the development of arrhythmias. Unfortunately, it was not possible to perform this analysis using the NIS registry. These limitations are, however, counterbalanced by the presence of a large unrestricted study sample which lacks the selection bias found in studies reported by individual specialized centers and skilled operators.
6. CONCLUSION
Among hospitalized HIV patients, cardiac arrhythmias are associated with significant morbidity and mortality. AF is the most frequent arrhythmia among hospitalized HIV patients. The presence of arrhythmias is associated with adverse outcomes in HIV patients, including a higher in‐hospital mortality rate and cost of care. The in‐hospital mortality among patients with any arrhythmia is significant but has decreased over the years.
CONFLICT OF INTEREST
The authors declare no potential conflict of interests.
Abudan AA, Vaidya VR, Tripathi B, et al. Burden of arrhythmia in hospitalized HIV patients. Clin Cardiol. 2021;44:44:66–77. 10.1002/clc.23506
DATA AVAILABILITY STATEMENT
The following information was supplied regarding data availability: The NIS database raw files were purchased through online HCUP (health care cost and utilization project) distributor. All purchasers and users of HCUP data must complete the online Data Use Agreement (DUA) training so that they are familiar with the rules and restrictions for the use of HCUP data. If this raw data is made public, then the likelihood of maintaining standards to complete the DUA training might be violated. Moreover, anyone who uses the database files we purchased must complete an HCUP Data Use Agreement form (a form which the owner of the data has to generate and acknowledge). Therefore, given these limitations, we have provided raw data for review purposes and not for publishing (i.e., to be shared with the public). Additionally, as per AHRQ‐HCUP, before the reviewers/editors may access any HCUP data (the raw files), they are required to complete the 15‐minute Data Use Agreement (DUA) training and read and sign the HCUP DUA. Both of these may be completed online at this link: https://www.hcup-us.ahrq.gov/tech_assist/dua.jsp
REFERENCES
- 1. Centers for Disease Control and Prevention . HIV Surveillance Report; vol. 28 2016. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed cited 2019 December 25, 2019.
- 2. Zaidi J, Grapsa E, Tanser F, Newell ML, Bärnighausen T. Dramatic increase in HIV prevalence after scale‐up of antiretroviral treatment. Aids. 2013;27(14):2301‐2305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Effros RB, Fletcher CV, Gebo K, et al. Aging and infectious diseases: workshop on HIV infection and aging: what is known and future research directions. Clin Infect Dis. 2008;47(4):542‐553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Savès M, Chêne G, Ducimetie`re P, Leport C, Le Moal G, Amouyel P, et al. Risk factors for coronary heart disease in patients treated for human immunodeficiency virus infection compared with the general population. Clin Infect Dis. 2003;37(2):292‐298. [DOI] [PubMed] [Google Scholar]
- 5. De Castro S et al. Frequency of development of acute global left ventricular dysfunction in human immunodeficiency virus infection. J Am Coll Cardiol. 1994;24(4):1018‐1024. [DOI] [PubMed] [Google Scholar]
- 6. Gopal M, Bhaskaran A, Khalife W, Barbagelata A. Heart disease in patients with HIV/AIDS‐an emerging clinical problem. Curr Cardiol Rev. 2009;5(2):149‐154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Friis‐Møller N et al. Class of antiretroviral drugs and the risk of myocardial infarction. N Engl J Med. 2007;356(17):1723‐1735. [DOI] [PubMed] [Google Scholar]
- 8. Zanetti HR, Mendes EL, Palandri Chagas AC, et al. Triad of the ischemic cardiovascular disease in people living with HIV? Association between risk factors, HIV infection, and use of antiretroviral therapy. Curr Atheroscler Rep. 2018;20(6):30. [DOI] [PubMed] [Google Scholar]
- 9. Hsu JC, Li Y, Marcus GM, et al. Atrial fibrillation and atrial flutter in human immunodeficiency virus‐infected persons: incidence, risk factors, and association with markers of HIV disease severity. J Am Coll Cardiol. 2013;61(22):2288‐2295. [DOI] [PubMed] [Google Scholar]
- 10. Tseng ZH, Secemsky EA, Dowdy D, et al. Sudden cardiac death in patients with human immunodeficiency virus infection. J Am Coll Cardiol. 2012;59(21):1891‐1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Databases H . Healthcare Cost and Utilization Project (HCUP). 2016. Available from: www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed February 18, 2018.
- 12. Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract. 2002;5(3):143‐151. [PubMed] [Google Scholar]
- 13. State and County QuickFacts – U.S. Census Bureau. https://www.census.gov/research/. Accessed February 18, 2018.
- 14. Singh V, Badheka AO, Patel SV, et al. Comparison of Inhospital outcomes of surgical aortic valve replacement in hospitals with and without availability of a transcatheter aortic valve implantation program (from a Nationally Representative Database). Am J Cardiol. 2015;116(8):1229‐1236. [DOI] [PubMed] [Google Scholar]
- 15. Patel NJ, Deshmukh A, Pant S, et al. Contemporary trends of hospitalization for atrial fibrillation in the United States, 2000 through 2010. Circulation. 2014;129(23):2371‐2379. [DOI] [PubMed] [Google Scholar]
- 16. Mocroft A, Brettle R, Kirk O, et al. Changes in the cause of death among HIV positive subjects across Europe: results from the EuroSIDA study. Aids. 2002;16(12):1663‐1671. [DOI] [PubMed] [Google Scholar]
- 17. Mocroft A, Gatell J, Reiss P, et al. Causes of death in HIV infection: the key determinant to define the clinical response to anti‐HIV therapy. Aids. 2004;18(17):2333‐2337. [DOI] [PubMed] [Google Scholar]
- 18. Lewden C, May T, Rosenthal E, et al. Changes in causes of death among adults infected by HIV between 2000 and 2005: the "Mortalité 2000 and 2005" surveys (ANRS EN19 and Mortavic). J Acquir Immune Defic Syndr. 2008;48(5):590‐598. [DOI] [PubMed] [Google Scholar]
- 19. Grunfeld C, Delaney JAC, Wanke C, et al. Preclinical atherosclerosis due to HIV infection: carotid intima‐medial thickness measurements from the FRAM study. Aids. 2009;23(14):1841‐1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chow FC, Regan S, Feske S, Meigs JB, Grinspoon SK, Triant VA. Comparison of ischemic stroke incidence in HIV‐infected and non‐HIV‐infected patients in a US health care system. J Acquir Immune Defic Syndr. 2012;60(4):351‐358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Aviles RJ, Martin DO, Apperson‐Hansen C, et al. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003;108(24):3006‐3010. [DOI] [PubMed] [Google Scholar]
- 22. Chung MK, Martin DO, Sprecher D, et al. C‐reactive protein elevation in patients with atrial arrhythmias: inflammatory mechanisms and persistence of atrial fibrillation. Circulation. 2001;104(24):2886‐2891. [DOI] [PubMed] [Google Scholar]
- 23. Deeks SG. HIV infection, inflammation, immunosenescence, and aging. Annu Rev Med. 2011;62:141‐155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hu YF, Chen YJ, Lin YJ, Chen SA. Inflammation and the pathogenesis of atrial fibrillation. Nat Rev Cardiol. 2015;12(4):230‐243. [DOI] [PubMed] [Google Scholar]
- 25. Samaras K, Wand H, Law M, Emery S, Cooper D, Carr A. Prevalence of metabolic syndrome in HIV‐infected patients receiving highly active antiretroviral therapy using international diabetes foundation and adult treatment panel III criteria: associations with insulin resistance, disturbed body fat compartmentalization, elevated C‐reactive protein, and [corrected] hypoadiponectinemia. Diabetes Care. 2007;30(1):113‐119. [DOI] [PubMed] [Google Scholar]
- 26. Sani MU, Okeahialam BN. QTc interval prolongation in patients with HIV and AIDS. J Natl Med Assoc. 2005;97(12):1657‐1661. [PMC free article] [PubMed] [Google Scholar]
- 27. Anson BD, Weaver JGR, Ackerman MJ, et al. Blockade of HERG channels by HIV protease inhibitors. Lancet (London, England). 2005;365(9460):682‐686. [DOI] [PubMed] [Google Scholar]
- 28. Kocheril AG et al. Long QTc and torsades de pointes in human immunodeficiency virus disease. Pacing Clin Electrophysiol. 1997;20(11):2810‐2816. [DOI] [PubMed] [Google Scholar]
- 29. Kroll CR, Gettes LS. T wave alternans and Torsades de pointes after the use of intravenous pentamidine. J Cardiovasc Electrophysiol. 2002;13(9):936‐938. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The following information was supplied regarding data availability: The NIS database raw files were purchased through online HCUP (health care cost and utilization project) distributor. All purchasers and users of HCUP data must complete the online Data Use Agreement (DUA) training so that they are familiar with the rules and restrictions for the use of HCUP data. If this raw data is made public, then the likelihood of maintaining standards to complete the DUA training might be violated. Moreover, anyone who uses the database files we purchased must complete an HCUP Data Use Agreement form (a form which the owner of the data has to generate and acknowledge). Therefore, given these limitations, we have provided raw data for review purposes and not for publishing (i.e., to be shared with the public). Additionally, as per AHRQ‐HCUP, before the reviewers/editors may access any HCUP data (the raw files), they are required to complete the 15‐minute Data Use Agreement (DUA) training and read and sign the HCUP DUA. Both of these may be completed online at this link: https://www.hcup-us.ahrq.gov/tech_assist/dua.jsp


