Supplemental Digital Content is available in the text.
Keywords: acute kidney injury, antioxidant, coronavirus disease 2019, hypoxia, sepsis, sodium ascorbate
Objectives:
Oxidative stress appears to initiate organ failure in sepsis, justifying treatment with antioxidants such as vitamin C at megadoses. We have therefore investigated the safety and efficacy of megadose sodium ascorbate in sepsis.
Design:
Interventional study.
Setting:
Research Institute.
Subjects:
Adult Merino ewes.
Interventions:
Sheep were instrumented with pulmonary and renal artery flow-probes, and laser-Doppler and oxygen-sensing probes in the kidney. Conscious sheep received an infusion of live Escherichia coli for 31 hours. At 23.5 hours of sepsis, sheep received fluid resuscitation (30 mL/kg, Hartmann solution) and were randomized to IV sodium ascorbate (0.5 g/kg over 0.5 hr + 0.5 g/kg/hr for 6.5 hr; n = 5) or vehicle (n = 5). Norepinephrine was titrated to restore mean arterial pressure to baseline values (~80 mm Hg).
Measurements and Main Results:
Sepsis-induced fever (41.4 ± 0.2°C; mean ± se), tachycardia (141 ± 2 beats/min), and a marked deterioration in clinical condition in all cases. Mean arterial pressure (86 ± 1 to 67 ± 2 mm Hg), arterial Po2 (102.1 ± 3.3 to 80.5 ± 3.4 mm Hg), and renal medullary tissue Po2 (41 ± 5 to 24 ± 2 mm Hg) decreased, and plasma creatinine doubled (71 ± 2 to 144 ± 15 µmol/L) (all p < 0.01). Direct observation indicated that in all animals, sodium ascorbate dramatically improved the clinical state, from malaise and lethargy to a responsive, alert state within 3 hours. Body temperature (39.3 ± 0.3°C), heart rate (99.7 ± 3 beats/min), and plasma creatinine (32.6 ± 5.8 µmol/L) all decreased. Arterial (96.5 ± 2.5 mm Hg) and renal medullary Po2 (48 ± 5 mm Hg) increased. The norepinephrine dose was decreased, to zero in four of five sheep, whereas mean arterial pressure increased (to 83 ± 2 mm Hg). We confirmed these physiologic findings in a coronavirus disease 2019 patient with shock by compassionate use of 60 g of sodium ascorbate over 7 hours.
Conclusions:
IV megadose sodium ascorbate reversed the pathophysiological and behavioral responses to Gram-negative sepsis without adverse side effects. Clinical studies are required to determine if such a dose has similar benefits in septic patients.
Sepsis is the main cause of death in ICUs, with a global occurrence rate of 49 million cases and 11 million deaths in 2017 (1). Standard-of-care practice consists of antibiotics, fluid resuscitation, and vasopressor support. There are no treatments that reverse the deterioration in clinical state and organ dysfunction associated with sepsis.
Oxidative stress may be responsible for inflammation and mitochondrial dysfunction, common pathophysiologic features that contribute to sepsis-induced renal dysfunction (2–4). Indeed, we recently demonstrated that renal medullary tissue hypoxia develops early after the initiation of ovine sepsis and precedes the development of acute kidney injury (AKI) (5, 6). It is likely that a similar scenario contributes to the dysfunction of other organs in sepsis.
Vitamin C has antioxidant and anti-inflammatory effects (7). Patients with sepsis have subnormal plasma levels of vitamin C that correlate inversely with the occurrence rate of multiple-organ failure (8). In septic patients, high doses of vitamin C (50 and 200 mg/kg/24 hr) reduced the Sequential Organ Failure Assessment (SOFA) scores and the levels of proinflammatory biomarkers (9). In addition, in a single-center retrospective study, combined treatment with vitamin C (1.5 g every 6 hr) with hydrocortisone and thiamine reduced the SOFA score and mortality (10). Another trial of IV vitamin C (1.5 g, every 6 hr for 96 hr) showed a numerical reduction in 28-day mortality (11). However, in a recent randomized multicenter clinical trial in septic patients, IV infusion of vitamin C (1.5 g every 6 hr), together with thiamine and hydrocortisone, did not significantly improve SOFA scores or mortality (12). Thus, the benefit of vitamin C therapy in sepsis remains controversial.
Dose, timing, and duration of vitamin C administration are critical factors that likely determine the response in sepsis, but these factors lack detailed investigation. We reasoned that, in the setting of established severe sepsis, a much higher dose (megadose) than tested so far would be needed. Since extremely high doses of vitamin C have been given in cancer and burn patients without major side effects (13), we hypothesized that such a dose would be safe and might be effective in established sepsis. We therefore determined the safety and efficacy of IV megadose sodium ascorbate, the sodium salt of vitamin C, on cardiovascular, renal, pulmonary, and hepatic functions in an ovine model of sepsis in the presence of clinical triggers for intervention. Furthermore, compassionate use of IV sodium ascorbate is reported in a critically ill coronavirus disease 2019 (COVID-19) patient.
MATERIALS AND METHODS
Animal Preparation
Experimental protocols were approved by the Animal Ethics Committee of the Florey Institute of Neuroscience and Mental Health under guidelines of the National Health and Medical Research Council of Australia. The experiments adhered to the Animal Research: Reporting of In Vivo Experiments guidelines (14). Two aseptic surgical procedures, separated by 3–4 weeks, were performed in 12 Merino ewes (35–45 kg; 1.5–2.0 years old) under general anesthesia. Sheep were instrumented to record arterial pressure, heart rate, cardiac output, renal blood flow (RBF) and renal cortical and medullary perfusion, oxygen tension (Po2), and body temperature continuously (see Supplementary Digital Content (http://links.lww.com/CCM/G27) for details).
Experimental Protocol
In conscious sheep, 4 days after the second surgery, 24 hours of baseline measurements commenced. Subsequently, Gram-negative sepsis was induced by IV infusion of live Escherichia coli, administered as a loading infusion of 2.8 × 109 colony-forming units over 30 minutes followed by continuous infusion of 1.26 × 109 colony-forming units/hr for 30.5 hours. One sheep in each group died (17% mortality) before the intervention period; data from these animals were excluded from the analysis. At 23.5 hours of sepsis, fluid bolus therapy with Hartmann solution (Baxter Australia, 30 mL/kg over 30 min) was administered. A blocked randomization design was used to allocate sheep to treatment with sodium ascorbate or vehicle. At 24 hours of sepsis, a loading dose of sodium ascorbate (0.5 g/kg over 30 min; Biological Therapies, Braeside, VIC, Australia) was given, followed by infusion of sodium ascorbate at 0.5 g/kg/hr for 6.5 hours (n = 5). In the vehicle group, fluid-matched Hartmann solution was administered from 24 to 31 hours of sepsis (n = 5). At 25 hours of sepsis, norepinephrine (Hospira, Melbourne, VIC, Australia) was infused at a dose to maintain mean arterial pressure (MAP) at baseline values (~80 mm Hg). At 31 hours of sepsis, infusions of E. coli and sodium ascorbate were stopped and ceftriaxone (1 g in 5 mL) was given intravenously, with a repeated dose 24 hours later. All animals received a maintenance infusion of Hartmann solution (1 mL/kg/hr) during the 48 hours of recovery.
To examine the effect of administering an equivalent amount of sodium to that in the sodium ascorbate infusion, using a similar protocol, two septic sheep were infused with a loading dose of NaHCO3 (8.4 g/kg over 30 minutes) followed by an infusion (8.4 g/kg/hr for 6.5 hr).
Analog signals of cardiovascular and renal variables and temperature were continuously monitored and blood and urine samples were collected at set intervals (6, 15) (see Supplementary Digital Content (http://links.lww.com/CCM/G27) for details of Methods and Statistical Analysis). At 48 hours of recovery from sepsis, animals were euthanized with IV pentobarbital (100 mg/kg) and the left kidney was collected for histology (see Supplementary Digital Content, http://links.lww.com/CCM/G27, for Histological Methods).
Treatment of One COVID-19 Patient With Sodium Ascorbate
While the sheep studies were being performed, as compassionate use and considering reports of high-dose vitamin C use (16, 17), attending clinicians administered megadose vitamin C to an extremely ill patient with COVID-19 acute respiratory distress syndrome, AKI, and hypotension. This decision was made by an independent clinical team of ICU and infectious diseases clinicians aware of the sheep experiments. They administered sodium ascorbate (Biological Therapies) as a loading dose (30 g over 30 min) followed by a maintenance dose (30 g over 6.5 hours) once on ICU day 3. The treatment of this patient adhered to the CARE guidelines (for CAse REports) (18) and the patient gave informed consent to use the data.
RESULTS
Septic sheep demonstrated malaise and lethargy, were drowsy and unresponsive to external stimuli, mostly lay down, and did not eat or drink. They all developed a persistent high fever (41.4 ± 0.2°C) and tachycardia (141 ± 2 beats/min) (Fig. 1, D and F). Fluid bolus therapy had no effect on this clinical state. After infusion of sodium ascorbate for 3 hours, the clinical state of all sheep dramatically improved. They stood up, were alert and responsive to external stimuli, and began to drink water and eat. They looked well and similar to a normal, healthy animal. This improvement in clinical condition remained during the sodium ascorbate infusion and the 2 recovery days. Furthermore, body temperature decreased to normal levels (~39°C in sheep) during sodium ascorbate therapy (Fig. 1F).
Figure 1.
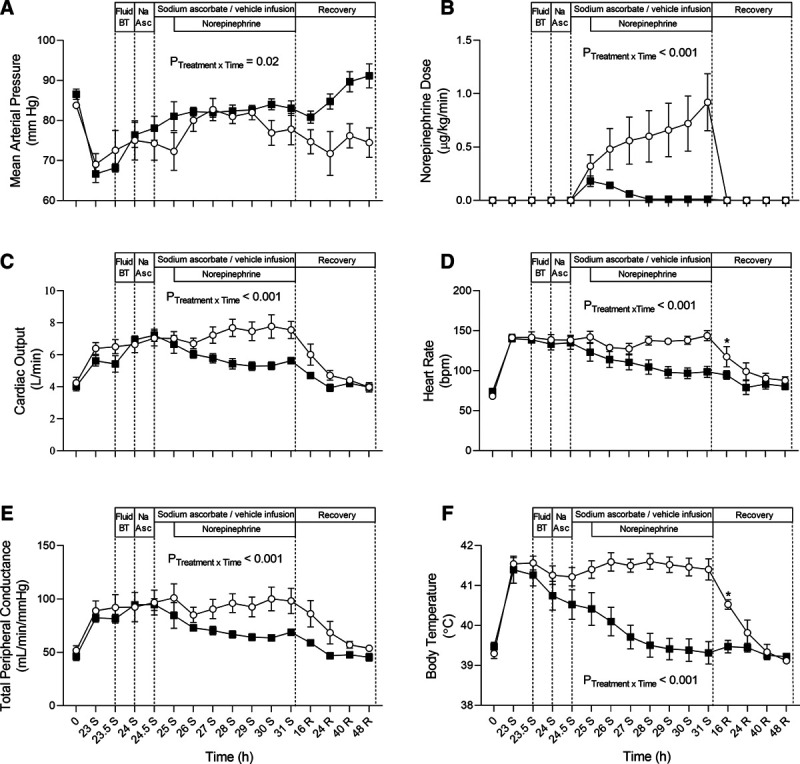
Changes in systemic hemodynamics in response to sodium ascorbate (Na Asc) (closed squares, n = 5) or vehicle (open circles, n = 5) treatment during ovine sepsis and during recovery from Gram-negative infection. Mean arterial pressure (A), norepinephrine dose (B), cardiac output (C), heart rate (D), total peripheral conductance, and core temperature (F) during infusion of Escherichia coli from 0 to 31 hr of sepsis and then recovery over 48 hr following antibiotic therapy. All animals were initially resuscitated with fluid bolus therapy (fluid BT, 30-mL/kg balanced crystalloid over 30 min) from 23.5 to 24 hr of sepsis. Animals were randomized to receive Na Asc (0.5 g/kg) or vehicle, crystalloid BT, from 24 to 24.5 hr of sepsis followed by an infusion of sodium ascorbate (0.5 g/kg/hr) or vehicle crystalloid from 24.5 to 31 hr of sepsis. Norepinephrine doses were titrated to maintain mean arterial pressure at baseline levels (75–80 mm Hg) from 25 to 31 hr of sepsis. All animals received IV antibiotics at 31 hr of sepsis (1-g ceftriaxone), with a repeated dose at 24 hr, and their recovery from infection was monitored over 48 hr. Time 0 is the mean of the 24th hr of baseline and times 23–31 hr of sepsis and 48 hr of recovery are means of 0.5-hr periods. Data are presented as treatment group-specific mean ± sd. p values represent treatment-time interactions from a two-way repeated measures analysis of variance from 23 to 31 hr of Gram-negative sepsis. Following antibiotic therapy and cessation of Escherichia coli infusion, significant differences between the baseline (time 0) time point and the 16-, 24-, 40-, and 48-hr time points are indicated by *p < 0.05 in the vehicle treatment group. p values represent the results of a Dunnett test using absolute values.
The septic clinical state was associated with a hypotensive, hyperdynamic circulatory state and stage 1 AKI (Table S1, http://links.lww.com/CCM/G27) (19). The deterioration in renal function occurred despite increased RBF and increased renal oxygen delivery. Renal hyperemia was associated with increased renal cortical tissue perfusion and Po2, but large reductions in renal medullary tissue perfusion and Po2. Sheep also developed moderate arterial hypoxemia (Pao2 ~80 mm Hg) and hyperlactatemia (~2.0 mmol/L) (Table S1, http://links.lww.com/CCM/G27).
Cardiovascular Function
Fluid bolus therapy caused a small improvement in MAP and further increased cardiac output (Fig. 1, A and C). During the subsequent infusion of sodium ascorbate, from 24 to 31 hours of sepsis, the dose of norepinephrine required to maintain MAP progressively decreased, such that by 4 hours of sodium ascorbate infusion, norepinephrine was not required in four of five sheep (Fig. 1B). Despite the reduced norepinephrine dose, to zero in four of the five sheep, the level of peripheral vasoconstriction increased, accompanied by significant, progressive decreases in cardiac output and heart rate toward baseline values (Fig. 1C–E). In contrast, in the vehicle group, the dose of norepinephrine had to be continuously increased, and by 30 hours of sepsis, responsiveness to norepinephrine had declined to a such degree that it was not possible to maintain the target MAP (Fig. 1A).
Renal Function, Perfusion, and Oxygenation
Sepsis caused increases in RBF and renal vascular conductance (RVC) that were maintained from 24 to 31 hours of sepsis in the vehicle-treated group, whereas both RBF and RVC decreased toward healthy levels in the sodium ascorbate-treated group (Fig. 2, A and B). Fluid bolus therapy transiently improved both medullary perfusion and Po2, but the levels decreased during infusion of vehicle and norepinephrine (Fig. 2, C and E). In contrast, with sodium ascorbate, the increase in medullary perfusion improved toward preseptic levels and medullary Po2 increased further throughout the infusion (Fig. 2, C and E). These beneficial changes were maintained for the following 2 days. The elevations in renal cortical perfusion observed in the vehicle group after fluid and norepinephrine therapy were absent in sheep treated with sodium ascorbate (Fig. 2D). Neither fluid bolus therapy, sodium ascorbate, nor norepinephrine had significant effects on renal cortical tissue Po2 (Fig. 2F).
Figure 2.
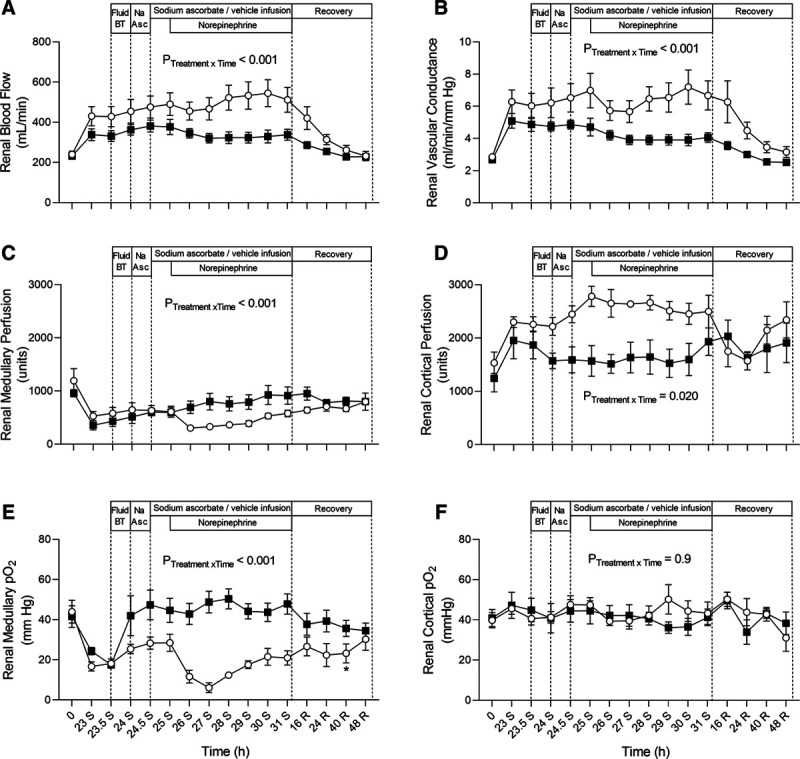
Changes in renal hemodynamics, intrarenal tissue perfusion, and oxygenation in response to sodium ascorbate (Na Asc) (closed squares, n = 5) or vehicle (open circles, n = 5) treatment during ovine sepsis and during recovery from Gram-negative infection. Renal blood flow (A), renal vascular conductance (B), medullary perfusion (C), cortical perfusion (D), medullary oxygen tension (Po2) (E), and cortical Po2 (F) during infusion of Escherichia coli from 0 to 31 hr of sepsis and then recovery over 48 hr following antibiotic therapy. Fluid and drug infusions and statistical analyses are as detailed in Figure 1. BT = bolus therapy.
In septic sheep, infusion of sodium ascorbate dramatically increased urine flow, to greater than 10 mL/kg/hr, within 30 minutes. Urine flow remained at these high levels throughout the infusion (Fig. 3A). The following 2 days, urine flow remained at normal baseline levels. Treatment with sodium ascorbate corrected the increased plasma creatinine to below baseline levels (Fig. 3B) and significantly increased creatinine clearance and fractional excretion of sodium (Fig. 3, C and D), but did not alter fraction excretion of potassium (Fig. 3F). Consistent with the predicted high levels of vitamin C in plasma, the plasma osmolar clearance increased (Fig. 3E). In contrast, in the vehicle group, AKI persisted: plasma creatinine remained elevated, and creatinine clearance and urine flow remained at low levels (Fig. 3).
Figure 3.
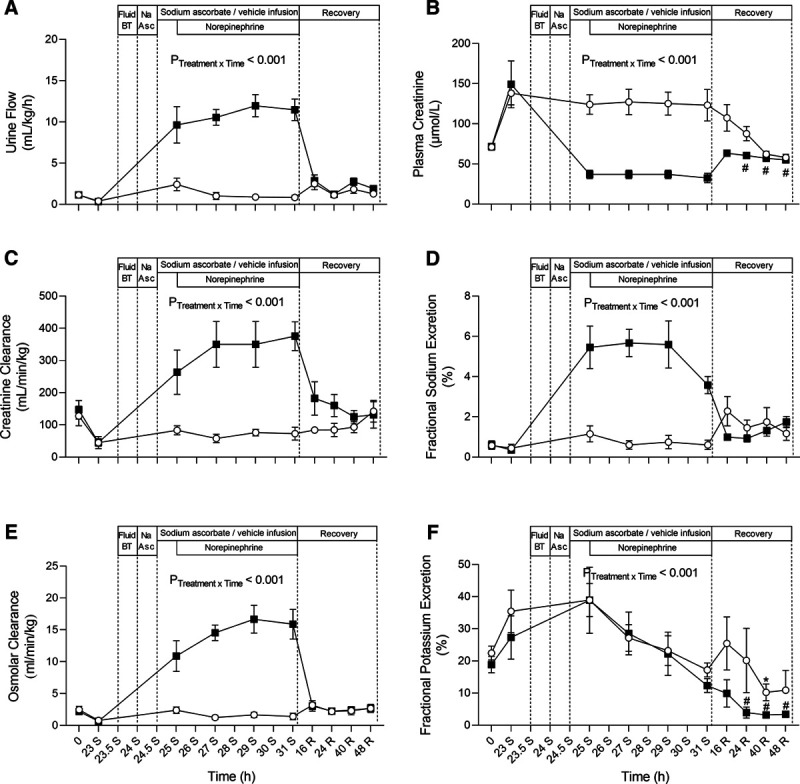
Changes in renal functional and plasma osmolar gap in response to sodium ascorbate (Na Asc) (closed squares, n = 5) or vehicle (open circles, n = 5) treatment during ovine sepsis and during recovery from Gram-negative infection. Urine output (A), plasma creatinine (B), creatinine clearance (C), fractional sodium excretion (D), plasma osmolar gap (E), and fractional potassium excretion (F) during infusion of Escherichia coli from 0 to 31 hr of sepsis and then recovery over 48 hr following antibiotic therapy. Significant differences between the baseline (time 0) time point and the 16-, 24-, 40-, and 48-hr time points are indicated by *p < 0.05 in the vehicle-treatment group and #p < 0.05 in the Na Asc–treatment group. Fluid and drug infusions and statistical analyses are as detailed in Figure 1. BT = bolus therapy.
Blood Gases and Biochemistry
By 23 hours of sepsis, arterial lactate had tripled in both groups (0.6 ± 0.1 to 2.0 ± 0.2 mmol/L) (Table S1 [http://links.lww.com/CCM/G27]). In the vehicle-treated group, arterial lactate remained increased throughout the intervention period. In contrast, with sodium ascorbate, there was a significant, progressive reduction in lactate (Fig. 4A).
Figure 4.
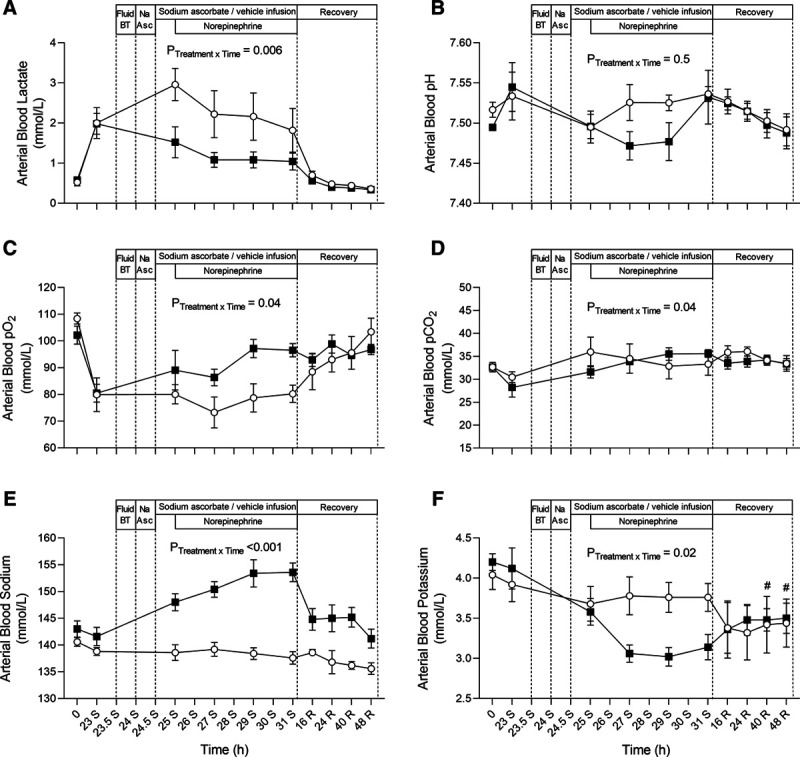
Changes in arterial blood biochemistry in response to sodium ascorbate (Na Asc) (closed squares, n = 5) or vehicle (open circles, n = 5) treatment during ovine sepsis and during recovery from Gram-negative infection. Arterial blood lactate (A), arterial blood pH (B), oxygen tension (Po2) (C), arterial blood sodium (D), partial pressure of carbon dioxide (Pco2) (E), and arterial blood potassium (F) during infusion of Escherichia coli from 0 to 31 hr of sepsis and then recovery over 48 hr following antibiotic therapy. Significant differences between the baseline (time 0) time point and the 16-, 24-, 40-, and 48-hr time points are indicated by #p < 0.05 in the Na Asc–treatment group. Fluid and drug infusions and statistical analyses are as detailed in Figure 1. BT = bolus therapy.
Arterial Po2 was significantly reduced at 23 hours of sepsis (102 ± 2 to 80 ± 3 mm Hg) and remained at this moderately hypoxic level during infusion with vehicle. In contrast, sodium ascorbate progressively improved arterial Po2 (to 96.5 ± 3.4 mm Hg) (Fig. 4C), but had no effects on pH or partial pressure of carbon dioxide (Fig. 4, B and D).
Arterial blood levels of sodium and potassium were unchanged by sepsis or infusion of vehicle. Infusion of sodium ascorbate, however, caused hypernatremia (153.6 ± 1.7 mmol/L) and hypokalemia (3.14 ± 0.16 mmol/L) (Fig. 4, E and F). Potassium chloride (16 mmol/hr) was infused if arterial potassium decreased below 2.5 mmol/L.
The increases in plasma bilirubin and plasma aspartate aminotransferase during sepsis were significantly reduced by sodium ascorbate (Fig. S8, http://links.lww.com/CCM/G27).
Renal Histology
There was no acute tubular necrosis or interstitial fibrosis within the renal cortex, corticomedullary junction, or medulla in either treatment group (Fig. S9 and Table S2 [http://links.lww.com/CCM/G27] for details of interstitial mononuclear infiltrate, granular, cellular and hyaline casts, birefringent crystal deposits, and polymorphonuclear cells, which were not different between the groups).
Infusion of NaHCO3
Infusion of hypertonic NaHCO3, at a dose to equal the sodium load with sodium ascorbate, did not reproduce the effects of sodium ascorbate: MAP decreased and increasing doses of norepinephrine were required, heart rate and RBF were not reduced, there was no improvement in arterial Po2 or renal medullary perfusion or Po2, and no reduction in plasma creatinine or increase in creatinine clearance was observed, although urine flow increased. There was a large increase in blood pH, with hypernatremia and hypokalemia. During the infusion of NaHCO3, there was intermittent shivering and large increases in body temperature. Due to the exacerbated level of sickness in these sheep, for ethical reasons, this experiment was not completed in further animals (Figs. S10–S16, http://links.lww.com/CCM/G27).
Case Report of One COVID-19 Patient
The patient was weaned off norepinephrine immediately after the loading dose of sodium ascorbate. During the maintenance infusion, MAP increased from 65 to 90 mm Hg without restarting vasopressors or fluid bolus therapy (Fig. 5, A and C). Plasma creatinine decreased (118–84 µmol/L), whereas urine flow increased (10–400 mL/hr) during the treatment (Fig. 5, D and F). Heart rate dropped (130–105 beats/min) (Fig. 5E) and lactate decreased (2.6–1.9 mmol/L). Arterial Po2 increased, although Fio2 dropped (0.45–0.30) with the same setting of positive end-expiratory pressure (14 cm H2O) and without prone-positioning (Fig. 5B). The patient was extubated on intensive care day 15 (12 days after the treatment) and discharged from hospital without any complications at 22 days after the treatment.
Figure 5.
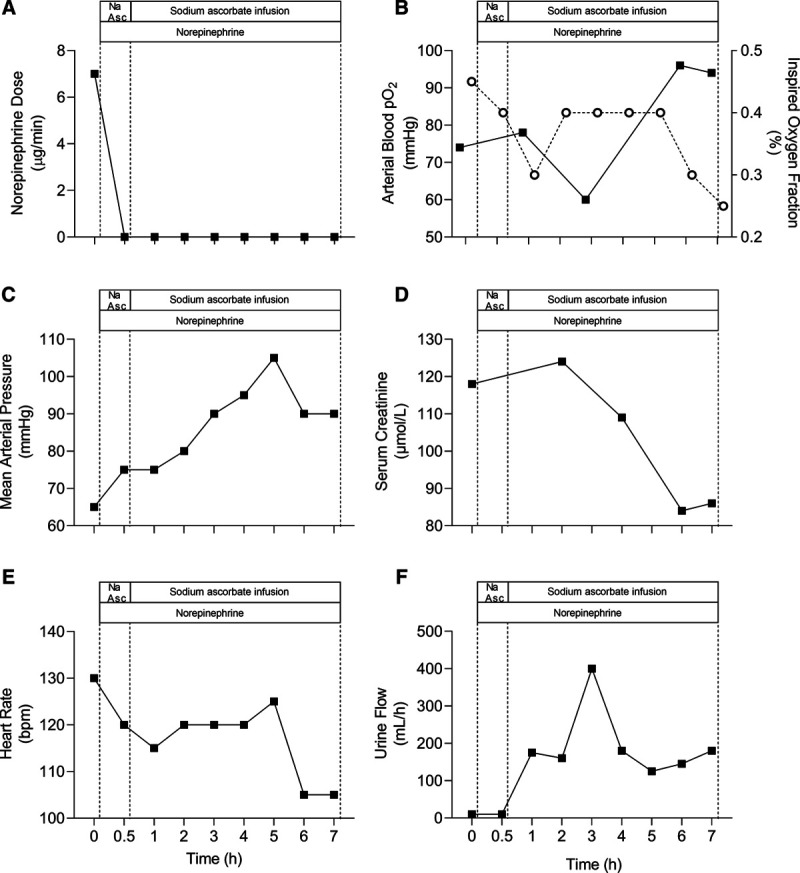
Changes in systemic hemodynamics and renal function in response to megadose sodium ascorbate (Na Asc) treatment in one septic patient with a severe case of coronavirus disease 2019 (n = 1). Norepinephrine dose (A), oxygen tension (Po2) (filled squares) and inspired oxygen fraction (open circles) (B), mean arterial pressure (C), serum creatinine (D), heart rate (E), and urine output (F) are presented at pretreatment (time 0), after a 30-min infusion of Na Asc bolus therapy (BT, 30 g), and then at hourly intervals during an infusion of Na Asc for 6.5 hr (4.6 g/hr).
DISCUSSION
IV megadose sodium ascorbate reversed the pathophysiological and behavioral changes of established ovine sepsis. The clinical improvement was dramatic: from sepsis-induced sickness behavior to normal alert behavior in 3 hours. There were marked improvements in cardiovascular, renal, pulmonary, and hepatic functions and decreases in arterial lactate and body temperature. The only observed side effects were hypernatremia and hypokalemia, both of which could be managed in intensive care settings.
Vitamin C has numerous actions that would be expected to decrease the deleterious consequences of sepsis. It has antioxidant properties that counteract oxidative stress and reduce mitochondrial dysfunction and cellular damage. Vitamin C accumulates in neutrophils, lymphocytes, monocytes, and platelets leading to improved immune function and reduced coagulation, and it prevents the loss of endothelial and epithelial functions and increases the synthesis of endogenous vasopressors (reviewed in [20] and [21]). However, patients with sepsis have low plasma levels of vitamin C (22, 23), due to reduced uptake and increased metabolic consumption. These effects are compounded by the inability of humans to synthesis vitamin C.
Clinical Response
Sepsis-induced typical sickness behavior: all sheep exhibited malaise, lethargy, and somnolence, and they were unresponsive to external stimuli, lay down, and did not eat or drink. In all cases, within 3 hours of infusion of sodium ascorbate, sheep became alert, responsive, and mobile. They stood up, started drinking and eating, and looked well. This remarkable improvement was maintained throughout the sodium ascorbate infusion and the 2-day recovery period. Over 18 years of experimentation with our model of ovine sepsis, we have not seen such an improvement in clinical state with any other treatment, including different vasopressors, diuretics, sympatholytics, and fluids (6, 15, 24–30). We are unaware of any treatment that has similar effects in any model of experimental sepsis or in septic patients.
Cardiovascular Changes
Sodium ascorbate increased MAP and reduced norepinephrine requirements, with complete withdrawal in four of five sheep. Despite such withdrawal, there was increased systemic vasoconstriction, suggesting enhanced vascular sensitivity to endogenous vasopressors. The improvement in MAP was accompanied by a reduction in the high levels of cardiac output and heart rate to normal.
These findings are in accord with the reported effects of vitamin C in septic patients (10, 31) and in septic mice in which sodium ascorbate restored the vascular responsiveness to norepinephrine (32). As high levels of catecholamines may have detrimental effects in sepsis (15, 33), such reduced requirements may be beneficial.
Renal Effects
Treatment with sodium ascorbate returned RVC and RBF to normal and corrected the substantial decreases in renal medullary perfusion and Po2 that are hallmarks of microvascular dysfunction in ovine septic AKI (5, 15). There are multiple mechanisms by which vitamin C might cause these beneficial effects. Ascorbate can prevent microvascular dysfunction in septic rats (34) and reduce inflammation by inhibiting tumor necrosis factor alpha-induced activation of necrosis factor-κB (35). There is also evidence that ascorbate is taken up by endothelial cells and increases endothelial nitric oxide synthase (36), which is reduced in the renal medulla in ovine septic AKI (37). Thus, ascorbate may improve medullary nitric oxide bioavailability and improve renal medullary perfusion and oxygenation. The reduction in renal tubular sodium reabsorption induced by sodium ascorbate may also reduce oxygen utilization and contribute to the improvement in medullary Po2.
A further important finding was the ability of sodium ascorbate to reverse established AKI at 23 hours of sepsis, with function being maintained above premorbid levels until the end of the 2-day recovery period. The increase in urine flow is probably an osmotic diuresis in response to the high circulating levels of sodium and ascorbate overloading the renal tubular uptake mechanism. Microvascular dysfunction, reduced medullary perfusion, and medullary hypoxia appear to be significant early contributors to the development of septic AKI (2, 38). Thus, the ability of ascorbate to improve microvascular function, together with its antioxidant action, likely contributed to the shunting of perfusion from the renal cortical to the medullary circulation and improvement in medullary Po2. In ovine septic AKI, norepinephrine causes further worsening of the underlying medullary hypoperfusion and hypoxia (15, 29, 30). Thus, the reduction in the dose of norepinephrine during infusion of sodium ascorbate likely contributed to the improvement in medullary perfusion and Po2.
Effects on Pulmonary and Hepatic Function
Sodium ascorbate attenuated the level of arterial hypoxemia, suggesting that it may reduce lung injury. This is in accord with findings that ascorbic acid attenuated the proinflammatory and procoagulant state that induced vascular lung injury in mice challenged with lipopolysaccharide (39, 40). Treatment with sodium ascorbate also reduced the sepsis-induced increases in plasma bilirubin and aspartate aminotransferase, indicative of reduced liver injury (Fig. S8 [http://links.lww.com/CCM/G27]).
Side Effects
No overt adverse events were observed with megadose IV sodium ascorbate. As expected, the infusion caused hypernatremia; however, the peak sodium level was less than 154 mmol/L and was transient. Megadose vitamin C may cause oxalate nephropathy, but no oxalate crystals or any other adverse renal effects were observed on renal histology (Fig. S9 and Table S2 [http://links.lww.com/CCM/G27]).
Effects of NaHCO3
Infusion of NaHCO3 did not reproduce the beneficial effects of sodium ascorbate, implying that these depend on ascorbate, not the sodium load. In fact, NaHCO3 had several deleterious effects: increases in blood pH and body temperature, with a deterioration in the clinical state of animals with no improvement in cardiovascular, renal, pulmonary, or liver function.
There are some limitations to this study. Sheep, unlike humans, synthesize vitamin C, so during sepsis, they may have a smaller decrease in the plasma level than human septic patients. The lactate levels were lower than those seen in humans, because sheep do not generate high lactate levels during sepsis and typically die at lactate levels greater than 3 mmol/L. Although we collected samples for measurement of plasma ascorbate and cytokines, because of laboratory closures due to the COVID-19 crisis, we were unable to analyze these samples (see Supplementary Digital Content, http://links.lww.com/CCM/G27, for strengths and limitations of the study).
Treatment of a Patient With COVID-19 With Megadose Sodium Ascorbate
We present data on the treatment of a COVID-19 patient with megadose IV sodium ascorbate. Such data lack experimental validity but are presented to highlight that a large dose of sodium ascorbate (approximately 1 g/kg over 6 hours) has similar beneficial effects to those seen in ovine sepsis.
CONCLUSIONS
In established ovine sepsis, treatment with IV megadose sodium ascorbate was highly effective and safe. It caused a remarkable improvement in clinical state, reversed the pathophysiological decreases in cardiovascular, renal, pulmonary, and hepatic functions, and reduced the hyperlactatemia and body temperature. Importantly, we observed no adverse effects beyond hypernatremia and hypokalemia. It is now important to determine the optimal dose and treatment duration of sodium ascorbate and to investigate further the mechanisms of action. In addition, clinical studies are warranted to resolve the issue of whether megadose vitamin C has acute and long-term benefits in septic patients.
ACKNOWLEDGMENTS
We thank Ms. Jennifer Horvath and Ms. Violetta Kirac (Austin Health Pathology) for their technical expertise analyzing creatinine, electrolytes, and liver enzymes.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Supported, in part, by a grant from the National Health and Medical Research Council of Australia (GNT 1050672) and, in part, by funding from the Victorian Government Operational Infrastructure Support Grant. Supported by a Future Leader Fellowship by the National Heart Foundation of Australia (101853; to Dr. Lankadeva).
REFERENCES
- 1.Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: Analysis for the Global Burden of Disease Study. Lancet. 2020; 395:200–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lankadeva YR, Okazaki N, Evans RG, et al. Renal medullary hypoxia: A new therapeutic target for septic acute kidney injury? Semin Nephrol. 2019; 39:543–553 [DOI] [PubMed] [Google Scholar]
- 3.Lowes DA, Webster NR, Murphy MP, et al. Antioxidants that protect mitochondria reduce interleukin-6 and oxidative stress, improve mitochondrial function, and reduce biochemical markers of organ dysfunction in a rat model of acute sepsis. Br J Anaesth. 2013; 110:472–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yamaguchi J, Nagase M, Yamamoto Y, et al. Increased oxidative stress and renal injury in patients with sepsis. J Clin Biochem Nutr. 2018; 63:137–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Calzavacca P, Evans RG, Bailey M, et al. Cortical and medullary tissue perfusion and oxygenation in experimental septic acute kidney injury. Crit Care Med. 2015; 43:e431–e439 [DOI] [PubMed] [Google Scholar]
- 6.Lankadeva YR, Kosaka J, Evans RG, et al. Urinary oxygenation as a surrogate measure of medullary oxygenation during angiotensin II therapy in septic acute kidney injury. Crit Care Med. 2018; 46:e41–e48 [DOI] [PubMed] [Google Scholar]
- 7.Spoelstra-de Man AME, Elbers PWG, Oudemans-Van Straaten HM. Vitamin C: Should we supplement? Current Opin Crit Care. 2018; 24:248–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borrelli E, Roux-Lombard P, Grau GE, et al. Plasma concentrations of cytokines, their soluble receptors, and antioxidant vitamins can predict the development of multiple organ failure in patients at risk. Crit Care Med. 1996; 24:392–397 [DOI] [PubMed] [Google Scholar]
- 9.Fowler AA, 3rd, Syed AA, Knowlson S, et al. ; Medical Respiratory Intensive Care Unit Nursing. Phase I safety trial of intravenous ascorbic acid in patients with severe sepsis. J Transl Med. 2014; 12:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marik PE, Khangoora V, Rivera R, et al. Hydrocortisone, vitamin C, and thiamine for the treatment of severe sepsis and septic shock: A retrospective before-after study. Chest. 2017; 151:1229–1238 [DOI] [PubMed] [Google Scholar]
- 11.Fowler AA, 3rd, Truwit JD, Hite RD, et al. Effect of vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: The CITRIS-ALI randomized clinical trial. JAMA. 2019; 322:1261–1270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fujii T, Luethi N, Young PJ, et al. ; VITAMINS Trial Investigators. Effect of vitamin C, hydrocortisone, and thiamine vs hydrocortisone alone on time alive and free of vasopressor support among patients with septic shock: The VITAMINS randomized clinical trial. JAMA. 2020; 323:423–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yanase F, Fujii T, Naorungroj T, et al. Harm of IV high-dose vitamin C therapy in adult patients: A scoping review. Crit Care Med. 2020; 48:e620–e628 [DOI] [PubMed] [Google Scholar]
- 14.Percie du Sert N, Hurst V, Ahluwalia A, et al. The ARRIVE guidelines 2.0: Updated guidelines for reporting animal research. Exp Physiol. 2020. Jul 14. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lankadeva YR, Kosaka J, Evans RG, et al. Intrarenal and urinary oxygenation during norepinephrine resuscitation in ovine septic acute kidney injury. Kidney Int. 2016; 90:100–108 [DOI] [PubMed] [Google Scholar]
- 16.Hiedra R, Lo KB, Elbashabsheh M, et al. The use of IV vitamin C for patients with COVID-19: A case series. Expert Rev Anti Infect Ther. 2020. Aug 1. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu F, Zhu Y, Zhang J, et al. Intravenous high-dose vitamin C for the treatment of severe COVID-19: Study protocol for a multicentre randomised controlled trial. BMJ Open. 2020; 10:e039519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: Explanation and elaboration document. J Clin Epidemiol. 2017; 89:218–235 [DOI] [PubMed] [Google Scholar]
- 19.Kellum JA, Lameire N; KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: A KDIGO summary (part 1). Crit Care. 2013; 17:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kashiouris MG, L’Heureux M, Cable CA, et al. The emerging role of vitamin C as a treatment for sepsis. Nutrients. 2020; 12:292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson JX. Mechanism of action of vitamin C in sepsis: Ascorbate modulates redox signaling in endothelium. Biofactors. 2009; 35:5–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schorah CJ, Downing C, Piripitsi A, et al. Total vitamin C, ascorbic acid, and dehydroascorbic acid concentrations in plasma of critically ill patients. Am J Clin Nutr. 1996; 63:760–765 [DOI] [PubMed] [Google Scholar]
- 23.Carr AC, Rosengrave PC, Bayer S, et al. Hypovitaminosis C and vitamin C deficiency in critically ill patients despite recommended enteral and parenteral intakes. Crit Care. 2017; 21:300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calzavacca P, Booth LC, Lankadeva YR, et al. Effects of clonidine on the cardiovascular, renal, and inflammatory responses to experimental bacteremia. Shock. 2019; 51:348–355 [DOI] [PubMed] [Google Scholar]
- 25.Calzavacca P, Lankadeva YR, Bailey SR, et al. Effects of selective β1-adrenoceptor blockade on cardiovascular and renal function and circulating cytokines in ovine hyperdynamic sepsis. Crit Care. 2014; 18:610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iguchi N, Lankadeva YR, Mori TA, et al. Furosemide reverses medullary tissue hypoxia in ovine septic acute kidney injury. Am J Physiol Regul Integr Comp Physiol. 2019; 317:R232–R239 [DOI] [PubMed] [Google Scholar]
- 27.Ishikawa K, Bellomo R, May CN. The impact of intrarenal nitric oxide synthase inhibition on renal blood flow and function in mild and severe hyperdynamic sepsis. Crit Care Med. 2011; 39:770–776 [DOI] [PubMed] [Google Scholar]
- 28.Lankadeva YR, Kosaka J, Iguchi N, et al. Effects of fluid bolus therapy on renal perfusion, oxygenation, and function in early experimental septic kidney injury. Crit Care Med. 2019; 47:e36–e43 [DOI] [PubMed] [Google Scholar]
- 29.Lankadeva YR, Ma S, Iguchi N, et al. Dexmedetomidine reduces norepinephrine requirements and preserves renal oxygenation and function in ovine septic acute kidney injury. Kidney Int. 2019; 96:1150–1161 [DOI] [PubMed] [Google Scholar]
- 30.Okazaki N, Iguchi N, Evans RG, et al. Beneficial effects of vasopressin compared with norepinephrine on renal perfusion, oxygenation, and function in experimental septic acute kidney injury. Crit Care Med. 2020; 48:e951–e958 [DOI] [PubMed] [Google Scholar]
- 31.Li J. Evidence is stronger than you think: A meta-analysis of vitamin C use in patients with sepsis. Crit Care. 2018; 22:258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu F, Wilson JX, Tyml K. Ascorbate inhibits iNOS expression and preserves vasoconstrictor responsiveness in skeletal muscle of septic mice. Am J Physiol Regul Integr Comp Physiol. 2003; 285:R50–R56 [DOI] [PubMed] [Google Scholar]
- 33.Singer M, Matthay MA. Clinical review: Thinking outside the box–an iconoclastic view of current practice. Crit Care. 2011; 15:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tyml K, Li F, Wilson JX. Delayed ascorbate bolus protects against maldistribution of microvascular blood flow in septic rat skeletal muscle. Crit Care Med. 2005; 33:1823–1828 [DOI] [PubMed] [Google Scholar]
- 35.Cárcamo JM, Pedraza A, Bórquez-Ojeda O, et al. Vitamin C suppresses TNF alpha-induced NF kappa B activation by inhibiting I kappa B alpha phosphorylation. Biochemistry. 2002; 41:12995–13002 [DOI] [PubMed] [Google Scholar]
- 36.Ladurner A, Schmitt CA, Schachner D, et al. Ascorbate stimulates endothelial nitric oxide synthase enzyme activity by rapid modulation of its phosphorylation status. Free Radic Biol Med. 2012; 52:2082–2090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Langenberg C, Gobe G, Hood S, et al. Renal histopathology during experimental septic acute kidney injury and recovery. Crit Care Med. 2014; 42:e58–e67 [DOI] [PubMed] [Google Scholar]
- 38.Ma S, Evans RG, Iguchi N, et al. Sepsis-induced acute kidney injury: A disease of the microcirculation. Microcirculation. 2019; 26:e12483. [DOI] [PubMed] [Google Scholar]
- 39.Fisher BJ, Kraskauskas D, Martin EJ, et al. Mechanisms of attenuation of abdominal sepsis induced acute lung injury by ascorbic acid. Am J Physiol Lung Cell Mol Physiol. 2012; 303:L20–L32 [DOI] [PubMed] [Google Scholar]
- 40.Fisher BJ, Seropian IM, Kraskauskas D, et al. Ascorbic acid attenuates lipopolysaccharide-induced acute lung injury. Crit Care Med. 2011; 39:1454–1460 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


