Abstract
Objective
Federal funds have been spent to reduce the disproportionate effects of HIV/AIDS on racial/ethnic minority groups in the United States. We investigated the association between federal domestic HIV funding and age-adjusted HIV death rates by race/ethnicity in the United States during 1999-2017.
Methods
We analyzed HIV funding data from the Kaiser Family Foundation by federal fiscal year (FFY) and US age-adjusted death rates (AADRs) by race/ethnicity (Hispanic, non-Hispanic white, non-Hispanic black, and Asian/Pacific Islander and American Indian/Alaska Native [API+AI/AN]) from Centers for Disease Control and Prevention WONDER detailed mortality files. We fit joinpoint regression models to estimate the annual percentage change (APC), average APC, and changes in AADRs per billion US dollars in HIV funding, with 95% confidence intervals (CIs). For 19 data points, the number of joinpoints ranged from 0 to 4 on the basis of rules set by the program or by the user. A Monte Carlo permutation test indicated significant (P < .05) changes at joinpoints, and 2-sided t tests indicated significant APCs in AADRs.
Results
Domestic HIV funding increased from $10.7 billion in FFY 1999 to $26.3 billion in FFY 2017, but AADRs decreased at different rates for each racial/ethnic group. The average rate of change in AADR per US billion dollars was −9.4% (95% CI, −10.9% to −7.8%) for Hispanic residents, −7.8% (95% CI, −9.0% to −6.6%) for non-Hispanic black residents, −6.7% (95% CI, −9.3% to −4.0%) for non-Hispanic white residents, and −5.2% (95% CI, −7.8% to −2.5%) for non-Hispanic API+AI/AN residents.
Conclusions
Increased domestic HIV funding was associated with faster decreases in age-adjusted HIV death rates for Hispanic and non-Hispanic black residents than for residents in other racial/ethnic groups. Increasing US HIV funding could be associated with decreasing future racial/ethnic disparities in the rate of HIV-related deaths.
Keywords: HIV, health care economics and organizations, mortality
Several studies have found racial/ethnic differences in HIV mortality in the United States.1,2 One study found that the black–white HIV mortality ratio and absolute difference increased during 1996-2006 after the introduction of highly active antiretroviral therapy. That same study speculated that the black–white mortality gap might have widened for many reasons, including differential dissemination of highly active antiretroviral therapy among racial/ethnic populations and government policies that inadvertently limited access to care in low-income communities. However, the study did not explain how governmental policies might have led to those effects.3
Chesson et al4 used state-level data to show an association between higher levels of HIV and sexually transmitted disease prevention funding each year and reductions in reported gonorrhea incidence rates in subsequent years during 1981-1998. Williams and Chesson5 reported that 2014 changes in the federal funds allocation formula for controlling sexually transmitted diseases in geographic areas with high racial/ethnic disparities resulted in more funds for some areas and the same level of funds for other areas. Williams et al6 also estimated that a 1% increase in annual federal funding for controlling sexually transmitted infections was associated with a 0.17% decrease in chlamydia rates during 2000-2016 and a 0.33% decrease in gonorrhea rates during 1981-2016; changes in disease rates lagged 0-2 years behind changes in funding levels. Grembowski et al7 found that increased expenditures per capita by local health departments or percentage of local public revenue allocated to them were associated with reduced black–white disparities in all-cause mortality for persons aged 15-44 and for males of all ages during 1990-1997.
Holtgrave and Kates8 estimated that the annual incidence of HIV in the United States increased 1 year in advance of the annual HIV prevention budget of the Centers for Disease Control and Prevention (CDC), with a positive correlation (r = 0.97) until the mid-1980s; thereafter, annual HIV incidence decreased as CDC’s HIV prevention budget increased, with a negative correlation (r = −0.91) and the same 1-year lag during 1986-2006. Hayek et al9 calculated that a 30-cent increase in per-capita allocation of CDC funding for HIV testing to a state was associated with a 2.4 percentage-point increase in the number of persons tested for HIV per state during 2010-2011. Federal policy makers and the public expect that higher levels of federal domestic HIV funding will lead to better HIV-related health outcomes.10 However, in 2018, when our study began, we did not know whether associations between funding levels and HIV mortality trends varied by race/ethnicity.
Each year since 1982, Congress has determined the amount of federal domestic funding for HIV programs that serve US residents affected by the HIV epidemic.11 Federal domestic funding for HIV programs is both mandatory (62%) and discretionary (38%). Mandatory spending limits are determined by the number of eligible recipients, the cost of services for health insurance coverage (eg, Medicaid, Medicare, and Social Security Disability Insurance), and cash assistance (eg, supplemental security income) to beneficiaries as prescribed by law.12 Discretionary spending pays for health care services, supplemental security income for persons with disabilities, and housing assistance13 for US residents living with HIV (eg, the Ryan White HIV/AIDS program); HIV surveillance, testing, and prevention programs; and HIV research.
Although federal funding for HIV increased substantially from several hundred thousand dollars in federal fiscal year (FFY) 1982 to more than $32 billion in FFY 2017, HIV remains a serious public health problem in the United States; more than 700 000 US residents have died from HIV/AIDS since 1981.14 During 2017, CDC estimated that 1.1 million US residents were living with HIV, and 38 739 US residents had received a diagnosis of HIV infection.15 The annual Congressional appropriation for US domestic HIV/AIDS prevention programs, an essential policy intervention, aims to prevent HIV deaths for all US residents. Avoiding racial/ethnic disparities in HIV mortality and morbidity are key Healthy People objectives.16 To address the disproportionate effects of HIV/AIDS on US residents among racial/ethnic minority groups, the US Congress established the Secretary’s Minority AIDS Initiative Fund in 1989 (renamed the Minority HIV/AIDS Fund in 2019).17 Each year, other agencies within the US Department of Health and Human Services spend additional amounts of their appropriated funds to prevent and control HIV/AIDS among racial/ethnic minority populations.10
Our literature review did not reveal any studies that examined associations between annual domestic HIV funding and racial/ethnic differences in trends in HIV mortality among US residents. To reduce the disproportionate effects of HIV/AIDS on racial/ethnic minority groups, we investigated whether changes in annual domestic HIV funding were associated with changes in HIV mortality by race/ethnicity during calendar years 1999-2017.
Methods
Study Design
We used joinpoint regression models to compare rates of decrease in age-adjusted death rates (AADRs) with HIV as the underlying cause among 4 racial/ethnic groups of US residents during 1999-2017. During the study period, in a natural quasi-experiment, each racial/ethnic group was exposed to the same overall levels of increasing domestic HIV funding and targeted funding initiatives focused on HIV testing and improving HIV treatment for racial/ethnic minority groups; each group served as its own historical control. We examined whether increasing levels of domestic HIV funding were associated with differential trends in AADRs by race/ethnicity. Because this study did not involve human research, institutional review board review was not needed.
Study Populations and Data Sources
We compared the experiences of persons who self-identified as non-Hispanic white, non-Hispanic black, non-Hispanic Asian/Pacific Islander (API) or non-Hispanic American Indian/Alaska Native (AI/AN), and Hispanic residents of the 50 US states and the District of Columbia. We combined estimates for API and AI/AN (API+AI/AN) residents to ensure statistically stable estimates from the joinpoint regression model. We used the National Center for Health Statistics’ bridged-race population estimates for each racial/ethnic group during 1999-2017 from the CDC WONDER Detailed Mortality File.18 Bridged-race population estimates reconcile 4 race categories from the 1977 US standards with 31 race categories from the 1997 standards for measuring race.
Primary Exposure Variable: Annual US Federal Domestic HIV Funding
We used estimates of US federal domestic HIV funding by category for health care, research, cash or housing social security benefits, and prevention by FFY. Funding data were reported by the Henry J. Kaiser Family Foundation from analyses of data for FFY 1999-2017 US budgets and Congressional budget justifications; Congressional appropriations bills and conference reports; all federal agencies’ operational plans; the White House; the White House Office of Management and Budget; and personal communications.11 We used the Consumer Price Index inflation calculator for All Urban Consumers US city average series for all items, not seasonally adjusted, to convert current US dollars to 2018 constant (ie, adjusted for inflation to facilitate comparison between periods) US dollars in billions.19
Primary Outcome Variable: HIV Mortality
We used annual AADRs (adjusted to the year 2000 US standard population) with HIV as the underlying cause (International Classification of Diseases, 10th Revision codes B20-B24) by race/ethnicity among residents of the 50 US states and District of Columbia during 1999-2017, with racial/ethnic population estimates described in the previous section. We extracted AADRs from the CDC WONDER Detailed Mortality File.18
Statistical Analysis
We used the Joinpoint Regression Statistical Software Program version 4.7.0.020 for the trend analysis to fit 4 joinpoint regression models. Each joinpoint regression model calculated the annual rate of change in HIV mortality for each unit change in annual HIV spending. The models also indicated the years of HIV funding levels (joinpoints) when the trend in HIV mortality decline accelerated significantly (from slower to faster) or decelerated significantly (from faster to slower).
Model 1 fit death year as the independent variable, AADR as the dependent variable, and race/ethnicity as the bivariable. This method resulted in separate group regression analyses for the 4 racial/ethnic groups as follows: non-Hispanic white, non-Hispanic black, non-Hispanic API+AI/AN, and Hispanic—all races. Model 2 was similar to model 1 except that annual HIV funding in current US billion dollars was the independent variable. Model 3 was similar to model 2 except that annual HIV funding in 2018 constant US billion dollars was the independent variable. Model 4 estimated the rate of change in AADR for the US population as annual HIV funding for each category (health care, research, cash/housing, and prevention) changed.
Each model started with the minimum number of joinpoints (ie, 0 joinpoints, which is a straight line) and tested whether more joinpoints were significant when added to the model (up to a maximum of 4 joinpoints). We used the annual percentage change (APC) in HIV mortality rate per year or per US billion dollars in HIV funding to determine trends. The average annual percentage change (AAPC) during a range of years or HIV funding levels indicated the average value of APCs across all segments between observation series endpoints. We computed 95% confidence intervals for APCs by using the t distribution and for AAPCs by using the normal distribution. The APC web analysis tool used a Monte Carlo permutation test of significance of an apparent change in trend at each joinpoint, with P < .05 considered significant. We used 2-sided t tests to determine significant APCs of AADRs, with P < .05 considered significant.
Results
Age-Adjusted HIV-Related Death Rates
Federal domestic HIV funding increased from $10.7 billion ($16.2 billion in 2018 US dollars) in FFY 1999 to $26.3 billion ($26.9 billion in 2018 US dollars) in FFY 2017 (Table 1). HIV AADRs among all US residents decreased from 5.32 per 100 000 population in 1999 to 1.60 per 100 000 population in 2017.
Table 1.
Domestic HIV funding, HIV deaths, and age-adjusted death rates, by race/ethnicity, United States, 1999-2017a
| Federal Fiscal or Death Year | Domestic HIV Fundinga | All US Residents | Non-Hispanic White | Non-Hispanic Black | Non-Hispanic API+AI/AN | Hispanic | |
|---|---|---|---|---|---|---|---|
| Current Funding, in Billions, $ | 2018 Constant Funding, in Billions, $b | Age- Adjusted Death Ratec | No. of HIV Deathsd (Age-Adjusted Death Ratec) | No. of HIV Deathsd (Age-Adjusted Death Ratec) | No. of HIV Deathsd (Age-Adjusted Death Ratec) | No. of HIV Deathsd (Age-Adjusted Death Ratec) | |
| 1999 | 10.7 | 16.2 | 5.3 | 4744 (2.3) | 7751 (24.0) | 143 (1.1) | 1958 (7.0) |
| 2000 | 11.9 | 17.4 | 5.2 | 4562 (2.2) | 7708 (23.6) | 119 (0.9) | 1908 (6.7) |
| 2001 | 13.0 | 18.4 | 5.0 | 4286 (2.1) | 7710 (23.2) | 145 (1.0) | 1853 (6.2) |
| 2002 | 14.2 | 19.8 | 4.9 | 4224 (2.1) | 7714 (23.0) | 156 (1.0) | 1855 (6.0) |
| 2003 | 15.4 | 21.0 | 4.7 | 4126 (2.0) | 7351 (21.6) | 152 (1.0) | 1890 (6.0) |
| 2004 | 16.4 | 21.8 | 4.5 | 3862 (1.9) | 7163 (20.7) | 170 (1.1) | 1758 (5.3) |
| 2005 | 17.3 | 22.2 | 4.2 | 3755 (1.8) | 6908 (19.7) | 150 (0.9) | 1645 (4.8) |
| 2006 | 17.1 | 21.3 | 4.0 | 3519 (1.7) | 6767 (18.9) | 141 (0.9) | 1617 (4.5) |
| 2007 | 16.8 | 20.4 | 3.7 | 3182 (1.5) | 6398 (17.6) | 146 (0.8) | 1516 (4.1) |
| 2008 | 18.2 | 21.2 | 3.3 | 3003 (1.4) | 5686 (15.4) | 157 (0.9) | 1365 (3.6) |
| 2009 | 19.6 | 22.9 | 3.0 | 2640 (1.2) | 5307 (14.2) | 124 (0.7) | 1263 (3.2) |
| 2010 | 20.7 | 23.8 | 2.6 | 2454 (1.1) | 4598 (12.0) | 123 (0.6) | 1134 (2.8) |
| 2011 | 21.8 | 24.3 | 2.4 | 2228 (1.0) | 4138 (10.7) | 111 (0.6) | 1133 (2.7) |
| 2012 | 22.2 | 24.3 | 2.2 | 2240 (1.0) | 3848 (9.8) | 103 (0.5) | 947 (2.2) |
| 2013 | 22.5 | 24.3 | 2.1 | 2161 (1.0) | 3673 (9.2) | 115 (0.6) | 927 (2.1) |
| 2014 | 24.0 | 25.5 | 2.0 | 2105 (0.9) | 3527 (8.6) | 101 (0.4) | 916 (2.0) |
| 2015 | 25.5 | 27.0 | 1.9 | 1984 (0.9) | 3379 (8.2) | 126 (0.6) | 889 (1.8) |
| 2016 | 25.9 | 27.1 | 1.8 | 2020 (0.9) | 3149 (7.5) | 116 (0.5) | 811 (1.7) |
| 2017 | 26.3 | 26.9 | 1.6 | 1750 (0.8) | 2965 (6.9) | 99 (0.4) | 816 (1.7) |
Abbreviation: API+AI/AN, Asian/Pacific Islander and American Indian/Alaska Native.
aData sources: Henry J. Kaiser Family Foundation’s analysis of data from US budgets; Congressional budget justifications, appropriations bills, and conference reports; all federal agencies’ operational plans; the White House; the White House Office of Management and Budget; and personal communications, 2019.11
bData source: adjusted for inflation by using the Consumer Price Index calculator.19 Constant funding is that which is adjusted for inflation to facilitate comparison between periods.
cAge-adjusted death rates to the year 2000 US standard million with HIV as the underlying cause of death (International Classification of Diseases, 10th Revision codes B20-B24) among residents of the 50 US states and the District of Columbia.
dData source: Centers for Disease Control and Prevention WONDER Detailed Mortality File.18
In model 1, HIV AADRs changed at varying rates for each racial/ethnic group (Table 2). Average changes in AADRs were −7.8% (95% CI, −8.7% to −6.8%) for Hispanic residents, −6.6% (95% CI, −7.2% to −6.1%) for non-Hispanic black residents, −5.9% (95% CI, −6.6% to −5.1%) for non-Hispanic white residents, and −5.2% (95% CI, −6.2% to −4.1%) for non-Hispanic API+AI/AN residents. The AADRs changed direction (decreasing faster or slower) significantly in 2004 and 2013 (2 joinpoints) for Hispanic residents: they declined by −4.8% (95% CI, −6.5% to −3.0%) during 1999-2004, by −10.1% (95% CI, −11.1% to −9.2%) during 2004-2013, and by −6.1% (95% CI, −9.7% to −2.3%) during 2013-2017. AADRs changed direction significantly in 2002, 2007, and 2011 (3 joinpoints) for non-Hispanic black residents: they declined by −4.9% (95% CI, −6.0% to −3.8%) during 2002-2007, by −12.0% (95% CI, −14.0% to −10.0%) during 2007-2011, and by −6.8% (95% CI, −7.7% to −6.0%) during 2011-2017. AADRs changed direction significantly in 2005 and 2010 (2 joinpoints) for non-Hispanic white residents: they declined by −3.9% (95% CI, −4.9% to −3.0%) during 1999-2005, by −9.8% (95% CI, −11.8% to −7.7%) during 2005-2010, and by −4.6% (95% CI, −5.8% to −3.4%) during 2010-2017. With no joinpoints for non-Hispanic API+AI/AN residents, their annual AADRs changed significantly by −5.2% (95% CI, −6.2% to −4.1%) during the study period.
Table 2.
Domestic HIV funding and age-adjusted HIV death rates, by race/ethnicity, United States, 1999-2017a
| Model | Independent Variable | Dependent Variable | Race/Ethnicity | No. of Joinpoints | Observation Segment | Percentage Change (95% CI) per Year or per Billion US Dollars | Average Percentage Change (95% CI) per Year or per Billion US Dollars |
|---|---|---|---|---|---|---|---|
| 1 | Death year | Age-adjusted death rate | Hispanic | 2 | 1999-2004 | −4.8 (−6.5 to −3.0)b | −7.8 (−8.7 to −6.8)b |
| 2004-2013 | −10.1 (−11.1 to −9.2)b | ||||||
| 2013-2017 | −6.1 (−9.7 to −2.3)b | ||||||
| Non-Hispanic black | 3 | 1999-2002 | −1.6 (−3.3 to 0.2) | −6.6 (−7.2 to −6.1)b | |||
| 2002-2007 | −4.9 (−6.0 to −3.8)b | ||||||
| 2007-2011 | −12.0 (−14.0 to −10.0)b | ||||||
| 2011-2017 | −6.8 (−7.7 to −6.0)b | ||||||
| Non-Hispanic white | 2 | 1999-2005 | −3.9 (−4.9 to −3.0)b | −5.9 (−6.6 to −5.1)b | |||
| 2005-2010 | −9.8 (−11.8 to −7.7)b | ||||||
| 2010-2017 | −4.6 (−5.8 to −3.4)b | ||||||
| Non-Hispanic API+AI/AN | 0 | 1999-2017 | −5.2 (−6.2 to −4.1)b | −5.2 (−6.2 to −4.1)b | |||
| 2 | HIV funding in billion US dollars | Age-adjusted death rate | Hispanic | 1 | $11-$15 billion | −5.0 (−10.0 to 0.2) | −9.4 (−10.9 to −7.8)b |
| $15-$26 billion | −11.2 (−12.4 to −9.9)b | ||||||
| Non-Hispanic black | 1 | $11-$15 billion | −1.9 (−5.8 to 2.1) | −7.8 (−9.0 to −6.6)b | |||
| $15-$26 billion | −10.3 (−11.2 to −9.3)b | ||||||
| Non-Hispanic white | 2 | $11-$16 billion | −3.9 (−6.3 to −1.4)b | −6.7 (−9.3 to −4.0)b | |||
| $16-$20 billion | −13.6 (−24.7 to −1.0)b | ||||||
| $20-$26 billion | −5.6 (−8.1 to −3.0)b | ||||||
| Non-Hispanic API+AI/AN | 1 | $11-$15 billion | 0.4 (−8.1 to 9.7) | −5.2 (−7.8 to −2.5)b | |||
| $15-$26 billion | −7.5 (−9.3 to −5.7)b | ||||||
| 3 | HIV funding in 2018 billion US dollars | Age-adjusted death rate | Hispanic | 0 | $16-$27 billion | −13.3 (−15.9 to −10.6)b | −13.3 (−15.9 to −10.6)b |
| Non-Hispanic black | 1 | $16-$22 billion | −5.2 (−9.4 to −0.8)b | −11.5 (−14.4 to −8.4)b | |||
| $22-$27 billion | −17.6 (−22.3 to −12.7)b | ||||||
| Non-Hispanic white | 1 | $16-$21 billion | −5.6 (−11.6 to 0.8) | −10.2 (−13.3 to −7.1)b | |||
| $21-$27 billion | −13.7 (−17.4 to −9.8)b | ||||||
| Non-Hispanic API+AI/AN | 2 | $16-$22 billion | −1.0 (−5.3 to 3.5) | −6.0 (−26.3 to 19.9) | |||
| $22-$26 billion | −19.1 (−28.3 to −8.8)b | ||||||
| $26-$27 billion | 10.9 (−82.3 to 594.6) |
Abbreviation: API+AI/AN, Asian/Pacific Islander and American Indian/Alaska Native.
aAge-adjusted death rates to the year 2000 US standard million with HIV as the underlying cause of death (International Classification of Diseases, 10th Revision codes B20-B24) among residents of the 50 US states and the District of Columbia.
b2-sided t tests were used to determine significant average percentage changes of age-adjusted death rates; P < .05 was considered significant.
Age-Adjusted HIV Death Rates per US Billion-Dollar Increase in HIV Funding
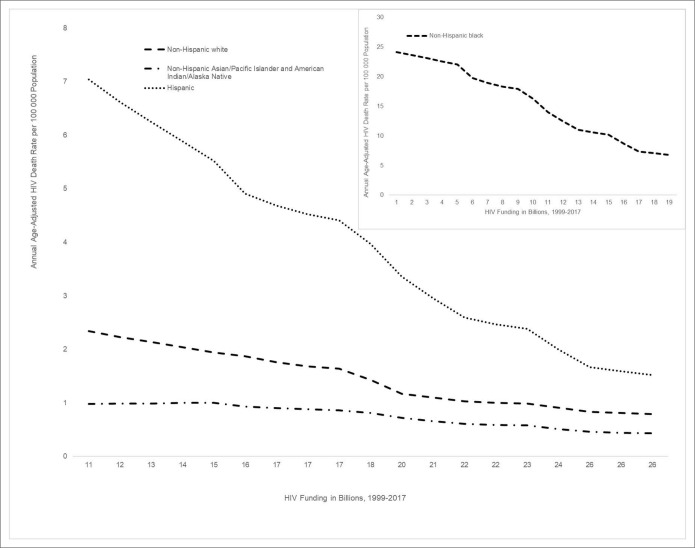
In model 2, the percentage decrease in HIV AADR per US billion-dollar (in current US dollars) increase in HIV funding varied for each racial/ethnic group (Table 2). The AAPC in AADRs changed significantly per US billion-dollar increase in HIV funding by an average of −9.4% (95% CI, −10.9% to −7.8%) for Hispanic residents; by −7.8% (95% CI, −9.0% to −6.6%) for non-Hispanic black residents; by −6.7% (95% CI, −9.3% to −4.0%) for non-Hispanic white residents; and by −5.2% (95% CI, −7.8% to −2.5%) for API+AI/AN residents. For Hispanic residents, the model had 1 joinpoint at $15 billion, and the AAPC in AADRs per US billion dollars changed significantly by −11.2% (95% CI, −12.4% to −9.9%). For non-Hispanic black residents, the model had 1 joinpoint at $15 billion, and the AAPC in AADRs per US billion dollars changed significantly by −10.3% (95% CI, −11.2% to −9.3%). For non-Hispanic white residents, the model had 2 joinpoints at which the AAPC in AADRs per US billion dollars changed significantly: at $16 billion (−3.9%; 95% CI, −6.3% to −1.4%) and at $20 billion (−5.6%; 95% CI, −8.1% to −3.0%). For non-Hispanic API+AI/AN residents, the model had 1 joinpoint at $15 billion, and the AAPC in AADRs per US billion dollars changed significantly by −7.5% (95% CI, −9.3% to −5.7%) (Table 2; Figure 1; Supplemental Figures S1 A-D available online).
Figure 1.
Trends in annual age-adjusted HIV death rates per 100 000 population associated with annual domestic HIV funding in billion US dollars, United States, 1999-2017. The figure is a graph of annual US domestic HIV funding in current billion US dollars during 1999-2017 on the x-axis and annual average age-adjusted death rate (AADR) per 100 000 population for each of 4 racial/ethnic groups indicated in the figure legend. Because the AADRs for non-Hispanic black persons are orders of magnitude larger than the AADRs for the other racial/ethnic groups, that chart is inset.
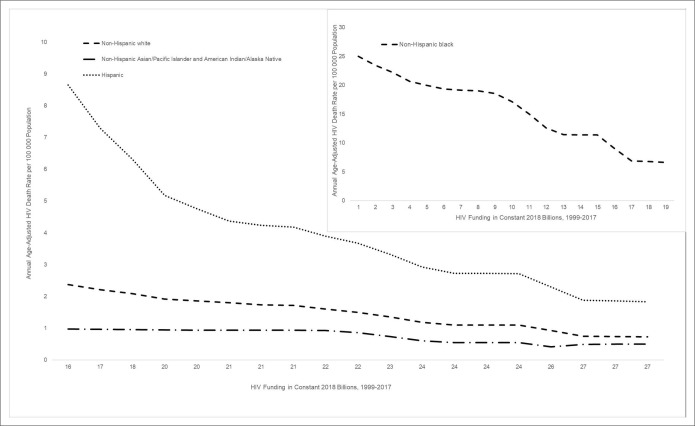
In model 3, using inflation-adjusted HIV spending levels in 2018 constant US billion dollars, differences in trends among racial/ethnic groups of US residents were similar to those described previously by using current HIV spending levels (Table 2; Figure 2).
Figure 2.
Trends in annual age-adjusted HIV death rates per 100 000 population associated with annual domestic HIV funding in 2018 constant (ie, adjusted for inflation to facilitate comparison between periods) billion US dollars, United States, 1999-2017. US domestic HIV funding in 2018 billion US dollars is adjusted for inflation by using the Consumer Price Index during 1999-2017.19 Because the age-adjusted death rates (AADRs) for non-Hispanic black persons are orders of magnitude larger than the AADRs for the other racial/ethnic groups, that chart is inset.
In model 4, the APC and AAPC in AADR per US billion-dollar increase (in current US billion dollars) in HIV funding varied for each category of funding (Supplemental Figures S2 A-D available online). With no joinpoints in HIV spending for health care, the APC in AADR changed by −9.1% (95% CI, −10.1% to −8.0%) per US billion-dollar increase. With no joinpoints in HIV spending for research, the APC in AADR changed significantly by −58.7% (95% CI, −72.3% to −38.4%) per US billion-dollar increase. With 1 joinpoint in HIV spending for cash or housing social security benefits, the APC in AADR changed significantly by −29.7% (95% CI, −54.9% to −9.4%) per US billion-dollar increase (from $1.5 to $1.9 billion) and by −53.4% (95% CI, −56.9% to −49.6%) per US billion-dollar increase (from $1.9 to $3.0 billion). With no joinpoint for HIV prevention, the APC in AADR changed significantly by −95.2% (95% CI, −99.9% to −3.0%) per US billion-dollar increase.
Discussion
We found that increasing federal domestic HIV funding was associated with differential trends in HIV AADRs by race/ethnicity during 1999-2017. Without empirical causation proof from a randomized controlled trial (impractical in this context), we can consider the plausibility of the findings, given how federal domestic HIV funding accelerated progress in science and programs that led to earlier diagnoses and increased survival rates for all US residents over time.4,8 Those advances in science and program implementation included more effective antiretroviral treatment, single-pill regimens, and recommendations for earlier treatment for persons with higher CD4+ cell counts compared with the past.14
Moreover, increasing federal HIV funding might have accelerated efforts in improving care within racial/ethnic minority groups, thereby decreasing disparities.17 A more rapid decrease in AADRs among certain racial/ethnic groups might be consistent with varying rates of distribution of those scientific and program advances by racial/ethnic populations,21,22 despite varying rates of undiagnosed infection, linkage to care, retention in care, and viral suppression.21 Meanwhile, programs might have reached racial/ethnic groups among US residents with varying effectiveness in preventing premature death. Early diagnosis and treatment effectiveness might have varied because of differences in the stage of the epidemic among those populations during 1999-2017.22
Thus, funding might have been more effective among Hispanic and non-Hispanic black residents than among non-Hispanic white residents because AADRs were higher among Hispanic and non-Hispanic black residents during that period and AADRs had greater propensity to decrease toward the overall population mean. HIV funds might have been used more or less effectively within various racial/ethnic groups, adding to the effects of differences in funding levels on the association between HIV funding level and HIV mortality trends by race/ethnicity. Funding for care (>70% of the total) and cash/housing benefit medically underserved populations, including high percentages of racial/ethnic minority groups. Moreover, federal agencies have encouraged state and local health departments and community-based organizations to use assistance funds to benefit racial/ethnic populations most affected by HIV. Although the APC or AAPC in AADRs for the US population decreased at different rates per US billion-dollar increase in HIV funding for health care, research, cash/housing, and prevention, model 4 findings do not include estimates of the APC or AAPC within racial/ethnic groups because federal funding for health care, research, cash/housing, and prevention were not allocated by racial/ethnic group.
The implications of our findings for policy and program interventions can be inferred by analogy with the national experience in eliminating racial/ethnic disparities in measles prevention and control in the 1990s. That experience revealed that a combination of universal interventions (ie, interventions that reach all children regardless of race/ethnicity) and interventions that target services to racial/ethnic minority children was successful in eliminating disparities in measles vaccine coverage and, thus, measles incidence in the United States during 1985-1997.23 Similarly, increases in domestic HIV funding that supported HIV prevention programs serving all US residents, combined with HIV funding initiatives (eg, the Minority HIV/AIDS Fund) that targeted prevention and treatment services to racial/ethnic minority US residents during FFY 1999-2017, amounted to a combination of universal and targeted interentions.17
Limitations
Our findings had several limitations. First, estimates of the exposure of each racial/ethnic group to levels of domestic HIV funding that supported prevention and treatment services were unavailable to support the conclusion that increases in the total federal domestic HIV funding levels caused the varying rates of decrease in AADRs within racial/ethnic groups. As such, we could not determine the direct effect of funding on HIV death rates within each racial/ethnic group. Second, our use of an ecologic study design (with groups rather than individuals as the unit of observation), with each group serving as its own control without unexposed concurrent control groups, made it impossible to prove a causal association in either direction. Therefore, we could not rule out reverse causality, wherein declining AADRs lead to larger populations of persons living with HIV infection being treated with antiretroviral agents at increasing costs that require higher levels of HIV funding for treatment, Medicaid, Medicare, supplemental security income, and the Ryan White HIV/AIDS program. Third, the downward trend in AADRs might be negatively correlated with the upward trend in HIV/AIDS funding even if no causal connection exists.
Fourth, although a time lag might have been present, the regression model did not account for any time lag between a change in funding and a change in AADRs, implying that funding in each year would have affected AADRs only during the same year. A more plausible assumption is that a decrease in AADRs in any year would have been affected by changes in funding during all previous years. Fifth, our models could not account for variations in competing causes of death by race/ethnicity nor the role of funding for sexually transmitted disease and substance use prevention on HIV mortality. As such, we have no basis for predicting the effects of adjustments for those factors on our results. Finally, rules for assigning HIV as a single underlying cause of death in death certification ignore the role of HIV as a contributing cause of death. As such, we have no basis for predicting the effects of adjustments for HIV as a contributing cause on our results.
Conclusions
Increased domestic HIV funding was associated with faster decreases in age-adjusted HIV death rates for Hispanic and non-Hispanic black residents than for other residents. Increasing US HIV funding could lead to a decrease in racial/ethnic disparities in rates of HIV-related deaths.
Supplementary Material
Acknowledgments
The authors thank Cheryll K. Smith for reviewing and editing the article; Harrell W. Chesson, PhD, Timothy Green, PhD, and Dawn Smith, MD, for their critical review of the article; and Jennifer Kates and Lindsey Dawson of the Henry J. Kaiser Family Foundation for providing HIV funding data by category.
Footnotes
Authors’ Note: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Benedict I. Truman https://orcid.org/0000-0001-6407-4664
References
- 1. Shiels MS., Chernyavskiy P., Anderson WF. et al. Trends in premature mortality in the USA by sex, race, and ethnicity from 1999 to 2014: an analysis of death certificate data. Lancet . 2017;389(10073):1043-1054. 10.1016/S0140-6736(17)30187-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Trepka MJ., Fennie KP., Sheehan DM., Niyonsenga T., Lieb S., Maddox LM. Racial-ethnic differences in all-cause and HIV mortality, Florida, 2000-2011. Ann Epidemiol . 2016;26(3):176-182. 10.1016/j.annepidem.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Levine RS., Briggs NC., Kilbourne BS. et al. Black–white mortality from HIV in the United States before and after introduction of highly active antiretroviral therapy in 1996. Am J Public Health . 2007;97(10):1884-1892. 10.2105/AJPH.2005.081489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chesson HW., Harrison P., Scotton CR., Varghese B. Does funding for HIV and sexually transmitted disease prevention matter? Evidence from panel data. Eval Rev . 2005;29(1):3-23. 10.1177/0193841X04270613 [DOI] [PubMed] [Google Scholar]
- 5. Williams AM., Chesson HW. Recent changes in prevention funding to areas with high racial and ethnic disparities in sexually transmitted disease rates. Sex Transm Dis . 2018;45(10):703-705. 10.1097/OLQ.0000000000000849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Williams AM., Kreisel K., Chesson HW. Impacts of federal prevention funding on reported gonorrhea and chlamydia rates. Am J Prev Med . 2019;56(3):352-358. 10.1016/j.amepre.2018.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grembowski D., Bekemeier B., Conrad D., Kreuter W. Are local health department expenditures related to racial disparities in mortality? Soc Sci Med . 2010;71(12):2057-2065. 10.1016/j.socscimed.2010.09.004 [DOI] [PubMed] [Google Scholar]
- 8. Holtgrave DR., Kates J. HIV incidence and CDC’s HIV prevention budget: an exploratory correlational analysis. Am J Prev Med . 2007;32(1):63-67. 10.1016/j.amepre.2006.08.033 [DOI] [PubMed] [Google Scholar]
- 9. Hayek S., Dietz PM., Van Handel M. et al. Centers for Disease Control and Prevention funding for HIV testing associated with higher state percentage of persons tested. J Public Health Manag Pract . 2015;21(6):531-537. 10.1097/PHH.0000000000000222 [DOI] [PubMed] [Google Scholar]
- 10. US Department of Health and Human Services, Health Resources & Services Administration A living history: Ryan White & global HIV/AIDS programs—Capitol Hill moves to pass landmark legislation. https://hab.hrsa.gov/livinghistory/legislation/index.htm. Accessed January 27, 2020.
- 11. Henry J. Kaiser Family Foundation U.S. federal funding for HIV/AIDS: trends over time. https://www.kff.org/global-health-policy/fact-sheet/u-s-federal-funding-for-hivaids-trends-over-time. Accessed January 27, 2020.
- 12. Center on Budget and Policy Priorities Policy basics—introduction to the federal budget process. https://www.cbpp.org/sites/default/files/atoms/files/3-7-03bud.pdf. Accessed January 27, 2020.
- 13. Terzian AS., Irvine MK., Hollod LM., Lim S., Rojas J., Shepard CW. Effect of HIV housing services on engagement in care and treatment, New York City, 2011. AIDS Behav . 2015;19(11):2087-2096. 10.1007/s10461-015-1003-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fauci AS., Redfield RR., Sigounas G., Weahkee MD., Giroir BP. Ending the HIV epidemic: a plan for the United States. JAMA . 2019;321(9):844-845. 10.1001/jama.2019.1343 [DOI] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention Diagnoses of HIV infection in the United States and dependent areas, 2018. HIV Surveill Rep . 2019;30:1-129. [Google Scholar]
- 16. Koh HK., Piotrowski JJ., Kumanyika S., Fielding JE. Healthy People: a 2020 vision for the social determinants approach. Health Educ Behav . 2011;38(6):551-557. 10.1177/1090198111428646 [DOI] [PubMed] [Google Scholar]
- 17. US Department of Health and Human Services Minority HIV/AIDS fund: overview. https://www.hiv.gov/federal-response/smaif/overview. Updated September 25, 2019. Accessed January 27, 2020.
- 18. Centers for Disease Control and Prevention, National Center for Health Statistics CDC WONDER: detailed mortality file. https://wonder.cdc.gov/ucd-icd10.html. Accessed January 27, 2020.
- 19. US Department of Labor, Bureau of Labor Statistics. Databases, tables & calculators by subject: CPI inflation calculator. https://www.bls.gov/data/inflation_calculator.htm. Accessed January 27, 2020.
- 20. National Institutes of Health, National Cancer Institute Joinpoint trend analysis software, version 4.7.0.0. https://surveillance.cancer.gov/joinpoint. Accessed January 27, 2020.
- 21. Bradley H., Hall HI., Wolitski RJ. et al. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV—United States, 2011. MMWR Morb Mortal Wkly Rep . 2014;63(47):1113-1117. [PMC free article] [PubMed] [Google Scholar]
- 22. Gant Z., Bradley H., Hu X. et al. Hispanics or Latinos living with diagnosed HIV: progress along the continuum of HIV care—United States, 2010. MMWR Morb Mortal Wkly Rep . 2014;63(40):886-890. [PMC free article] [PubMed] [Google Scholar]
- 23. Hutchins SS., Jiles R., Bernier R. Elimination of measles and of disparities in measles childhood vaccine coverage among racial and ethnic minority populations in the United States. J Infect Dis . 2004;189(suppl 1):S146-S152. 10.1086/379651 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.