Abstract
Background
Complete injury of the recurrent laryngeal nerve (RLN) is a serious complication of thyroid surgery. Increasingly researches focus on the voice recovery of patients with RLN injury. This paper studied the effect of immediate end-to-end neuroanastomosis after complete injury of the unilateral RLN during thyroid surgery on postoperative vocal function.
Methods
Thirteen patients who underwent end-to-end neuroanastomosis for the treatment of complete injury of the unilateral RLN caused by thyroid surgery in Hunan Provincial People’s Hospital between October 2009 and January 2020 were selected. The basic information, cause of RLN injury, postoperative voice recovery, recovery time, and subjective assessment of voice by auditory perception results (Grade, Roughness, Breathiness, Asthenia, and Strain, the GRBAS score) of the patients were recorded.
Results
Among the 13 cases with RLN injury, the cause of RLN injury in 10 cases was transection by sharp instruments, and the voice was recovered one day after the operation. The cause of RLN injury in one case was suture of the RLN branch, and the voice was recovered one day after the operation. The cause of RLN injury in two cases was thermal injury, and the times for voice recovery after end-to-end neuroanastomosis were 3 and 4 months. The patients with a GRBAS score of 0 or 1 recovered their voice one day after the operation. The GRBAS score reached 1 in the two thermal injury cases, with voice recovery at 3 and 4 months after surgery. By 6 months, the voice recovery rate of the patients was 100%.
Conclusions
After complete injury of the unilateral RLN, immediate end-to-end anastomosis of the RLN can maximally preserve the postoperative vocal function of patients.
Keywords: Recurrent laryngeal nerve injury (RLN injury), thyroid surgery, neuroanastomosis
Introduction
Thyroid surgery is a common operation in the Department of Breast and Thyroid Surgery and has been widely carried out in clinical practice. Recurrent laryngeal nerve (RLN) injury is a common complication of thyroid surgery, and unilateral injury may cause hoarseness or accidental aspiration, while bilateral injury may lead to dyspnea. RLN injury not only has a considerable impact on the lives of patients but also has a certain psychological impact on patients. In recent years, due to the improvement of surgical techniques and the gradual accumulation of surgical experience, the injury rate has decreased significantly. However, sporadic reports of RLN injuries remain (1). The temporary RLN injury rate has been reported to be 3–14%, and the permanent injury rate is 1–3% (2,3). At present, increasingly researches focus on the voice recovery of patients with RLN injury, from the initial RLN anastomosis to gene therapy and stem cell therapy, and have achieved corresponding curative effect (4,5). In this paper, we investigated the efficacy of immediate end-to-end neuroanastomosis after complete injury of the unilateral RLN in thyroid surgery, and the outcomes were satisfied, which is reported as follows.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/gs-20-633).
Methods
Study subjects
Thirteen patients who underwent neuroanastomosis for the treatment of RLN injury caused by thyroid surgery at the Hunan Provincial People’s Hospital between October 2009 and January 2020 were selected, including two males and 11 females aged 13–58 years, with a mean age of 39 years. Two patients had multinodular goiter (MNG), 10 had papillary thyroid carcinoma (PTC), and one had medullary thyroid carcinoma (MTC) (Table 1).
Table 1. Basic information of the patients.
| No. | Time | Age (years) | Sex | Diagnosis |
|---|---|---|---|---|
| 1 | 2009.10 | 45 | F | MNG |
| 2 | 2010.5 | 32 | F | PTC |
| 3 | 2010.7 | 56 | M | PTC |
| 4 | 2013.4 | 13 | F | PTC |
| 5 | 2014.9 | 23 | F | PTC |
| 6 | 2015.12 | 47 | M | MTC |
| 7 | 2016.6 | 58 | F | PTC |
| 8 | 2017.8 | 34 | F | PTC |
| 9 | 2018.4 | 40 | F | MNG |
| 10 | 2018.11 | 33 | F | PTC |
| 11 | 2019.6 | 51 | F | PTC |
| 12 | 2019.11 | 38 | F | PTC |
| 13 | 2019.11 | 35 | F | PTC |
MNG, multinodular goiter; PTC, papillary thyroid carcinoma; MTC, medullary thyroid carcinoma.
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by committee board of Hunan Provincial People’s Hospital Medical Faculty (NO.: 2019117) and informed consent was taken from all the patients.
Surgical methods
A 1–2-cm arcuate incision was made at the suprasternal notch, and the length of the incision was determined according to the needs of the surgery. The upper and lower flaps were freed, the deep cervical fascia and cervical linea alba were longitudinally incised, the thyroid gland was separated and exposed, the masses were palpated, and the number of the masses was determined to determine the scope of resection. The RLN was exposed, and the inferior thyroid artery approach was used to dissect the RLN: the lower pole of the thyroid gland was identified, the RLN was determined by identifying Simon’s triangle (The triangular area between the common carotid artery, the inferior thyroid artery and the lateral wall of the trachea), the inferior artery was ligated, and then the dissection extended up to the larynx along one side of the RLN. The key to identifying the RLN lies in patience and meticulousness, caution against impatience, and avoidance of alacrity.
Voice assessment
In the examination room with environmental noise <45 dBA, all patients were asked to read the poem Quiet Night Thoughts aloud with natural tone and volume. After the reading was finished, two physicians engaged in voice work for more than 3 years jointly rated overall hoarseness G using the subjective assessment of voice by auditory perception (Grade, Roughness, Breathiness, Asthenia, and Strain, the GRBAS score) (6) (grade 0 is normal, grade 1 is mildly abnormal, grade 2 is moderately abnormal, and grade 3 is severely abnormal), and the average value was used for final grading. A grade of 0 or 1 after surgery was considered voice recovery.
Results
A total of 5,389 patients underwent thyroid surgery in our hospital from October 2009 to January 2020, 13 of whom experienced complete injury of the unilateral RLN, with no cases of bilateral RLN injury. The details of the cases with unilateral RLN injury are listed in Table 2.
Table 2. Intraoperative basic data and postoperative recovery of the patients.
| No. | Anastomotic side | Voice recovery | Recovery time | GRBAS score | Cause of injury |
|---|---|---|---|---|---|
| 1 | Right | YES | 1 day after surgery | 0 | Sharp resection |
| 2 | Left | YES | 1 day after surgery | 1 | Sharp resection |
| 3 | Right | YES | 1 day after surgery | 0 | Suture |
| 4 | Right | YES | 1 day after surgery | 1 | Sharp resection |
| 5 | Right | YES | 1 day after surgery | 0 | Sharp resection |
| 6 | Left | YES | 1 day after surgery | 0 | Sharp resection |
| 7 | Right | YES | 1 day after surgery | 0 | Sharp resection |
| 8 | Left | YES | 1 day after surgery | 1 | Sharp resection |
| 9 | Right | YES | 1 day after surgery | 0 | Sharp resection |
| 10 | Right | YES | 1 day after surgery | 0 | Sharp resection |
| 11 | Right | YES | 4 months after surgery | 1 | Thermal injury |
| 12 | Right | YES | 1 day after surgery | 1 | Sharp resection |
| 13 | Left | YES | 3 months after surgery | 1 | Thermal injury |
GRBAS, subjective assessment of voice by auditory perception, including Grade, Roughness, Breathiness, Asthenia, and Strain.
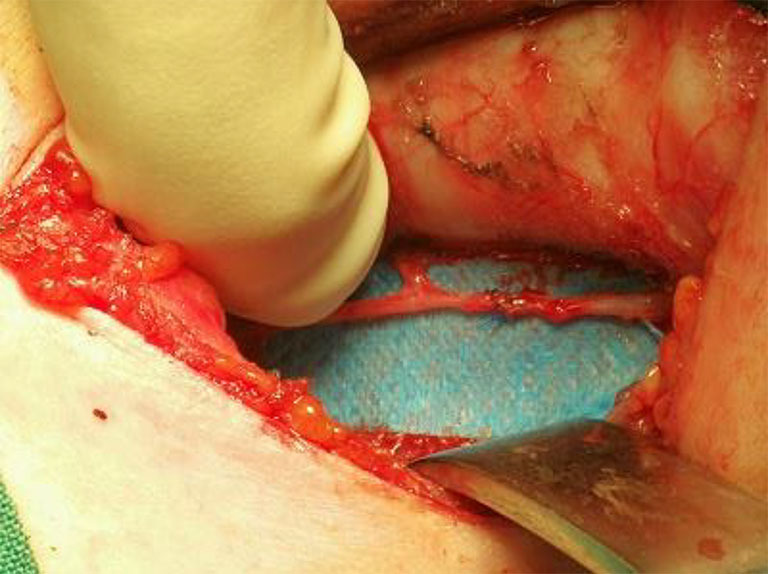
Causes of injury and treatment process
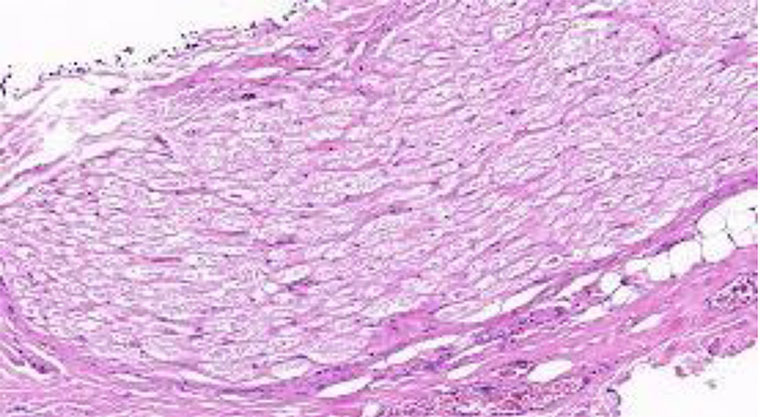
Of the 13 cases with complete injury of the RLN, in two cases, the RLN was cut accidentally due to the altered RLN course resulting from compression of the surrounding structures caused by the growth of a goiter (Figure 1), and the patients’ voices recovered. In eight cases, thyroid cancer invaded the RLN, and separating it from the RLN was difficult; thus, the invaded RLN had to be removed, end-to-end anastomosis of the RLN was performed (Figure 2), and the patients’ voices recovered. In one case, during treatment of small vessel bleeding at the location where the RLN enters larynx, the RLN was mistakenly sutured into the knot. Subsequently, nerve exploration and ligation site resection were performed, end-to-end neuroanastomosis was carried out, and the patient’s voice returned to normal. In two cases, the transverse thermal spread produced by the use of bipolar forceps resulted in complete damage of the RLN on one side. The injured nerve was resected as much as possible until reaching the normal nerve, end-to-end neuroanastomosis was performed, and the voices of the two patients returned to normal after surgery.
Figure 1.

A completely resected RLN. RLN, recurrent laryngeal nerve.
Figure 2.
Anastomotic RLN. RLN, recurrent laryngeal nerve.
Results of voice recovery
Among the 13 cases, the voice returned to normal in 11 cases just one day after surgery, and the GRBAS score was either 0 or 1. Voice recovery was slow in the two cases with thermal injury, requiring 3 and 4 months after surgery, but the GRBAS scores also reached 1. By 6 months, the voice recovery rate of the patients reached 100%.
Discussion
RLN injury is a postoperative complication warranting special attention from surgeons during thyroid surgery. Once it occurs, RLN injury can cause great physical and psychological trauma to patients. Further investigation of better RLN protection is necessary.
The RLN injury classifications are summarized in Table 3, and the causes of RLN injury are described in detail below.
Table 3. Classification, definition, and severity of RLN injury (7).
| Classification | Definition | Severity |
|---|---|---|
| Traction | The RLN running on Berry’s ligament or adhered to the thyroid goiter was pulled and damaged during surgery | Mild |
| Mechanical injury | During dissection, the RLN was injured by blunt instruments, contusion, pressure, clamping, aspiration, or compression of the trachea by surgical instruments | Mild-moderate |
| Ligation, suture | During or after nerve dissection, the RLN was ligated or sutured into knots or vascular clips of small vessel branches | Mild-moderate |
| Thermal injury | When small blood vessels were ligated or connective tissues were dissected at the tracheal groove, the RLN was damaged by direct contact with energy-based devices or transverse thermal spread | Moderate-severe |
| Complete resection | The RLN was inadvertently severed due to being visually misidentified as a blood vessel or a strip of connective tissue or due to tumor encapsulation and adhesions | Severe |
RLN, recurrent laryngeal nerve.
Causes of RLN injury (8)
Traction, clamping, and suture damage: The RLN is very delicate, its transverse diameter is only approximately (1.93±0.35) mm, and it is wrapped by only three layers of connective tissues, which are the endoneurium, perineurium, and epineurium (9). Moreover, when the thyroid gland is pulled inward during surgery, the RLN at Berry’s ligament bears a large traction force, which tends to cause intraoperative RLN injury (10), representing the most common cause of temporary RLN injury. RLN injury caused by traction has not occurred in our recent cases, although we cannot overlook the consequences that it causes. RLN injury caused by suture and ligation occurred in one case in this study.
Transection due to indistinct anatomy or tumor invasion of the RLN: (i) RLN branch variation: Bifurcation of an abnormal branch of the RLN often occurs at its intersection with the inferior thyroid artery. A close relationship exists between the inferior thyroid artery and the RLN. One autopsy study in which 160 RLNs were dissected showed that on the left side, 86.25% of the RLNs were located behind the inferior thyroid artery, 7.5% of the nerves were located in front of the artery, and 2.5% of the nerves ran between the arterial branches; on the right side, 75% of the nerves were located in front of the artery, 10% were behind the artery, and 5% ran between the arterial branches. The locations of the remaining RLNs were uncertain (11). (ii) Tumor adhesion or reoperation: Thyroid tumors or adhesions from previous surgery may encapsulate the nerve, resulting in difficult dissection or even inadvertent transection, leaving the nerve at high risk (12). Reoperation for both benign and malignant thyroid diseases has been reported to increase the risk of RLN injury (13). (iii) A non-RLN (NRLN): RLN injury caused by this anomaly occurred in 11 cases in this study, which required attention. We believe that this anomaly is also related to the fact that some patients did not seek timely treatment.
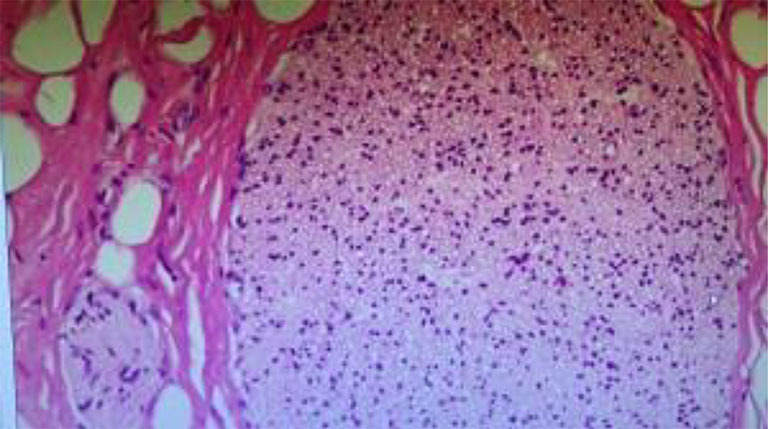
Thermal injury associated with improper use of energy devices: (i) energy devices can be too close to the RLN while in use. The use of an electric knife within 3 mm of RLN has been shown to lead to RLN injury (14). Owaki et al. noted that postoperative RLN palsy occurred when an ultrasonic scalpel was used in thyroid surgery, which may be related to thermal damage to surrounding tissues (15). (ii) Excessive use of an energy device results in extremely high temperatures in the RLN. Lateral heat conduction may occur when an energy device is used, and if the device is used for too long near the RLN, the RLN tends to have an increased temperature and can even be injured (Figures 3 and 4). When an ultrasonic knife is used in porcine muscle, the temperature inside the muscle 1 mm away from the tip of the knife has been reported to exceed 62 °C for 20 seconds, which almost reaches the temperature of protein denaturation (16). (iii) Improper use of energy devices: when managing small blood vessels at the location where the RLN enters the larynx, the use of an energy device in a narrow space may cause thermal injury, for example, the use of monopolar electrocautery near the RLN for electrocoagulation and hemostasis. When the device is operated in the area around the nerve, thermal injury can destroy cell membranes to disintegrate nerve fibers while also destroying the blood supply to the nerve, resulting in chronic ischemic changes in the nerve. RLN injury due to thermal injury occurred in two cases in this study and required attention. At the same time, we also noted that the patients with thermal injury in this study had slower voice recovery than the patients with RLN injuries due to other causes. In these two cases, postoperative pathological examination showed that one end of the injured nerve was not completely removed, which may have contributed to the slow postoperative voice recovery in the patients with thermal injury of the RLN in this study. In future operations, can we use intraoperative pathological examination of frozen sections to determine whether the injured nerve has been completely removed, thereby improving the speed of voice recovery in patients with RLN thermal injury?
Figure 3.
A degenerated and necrotic RLN stump (HE staining, magnification: 15×): cell degeneration, edema, and decreased nuclear staining of the nerve stump are evident. HE, hematoxylin-eosin. RLN, recurrent laryngeal nerve.
Figure 4.
A normal RLN stump (HE staining, magnification: 15×). HE, hematoxylin-eosin. RLN, recurrent laryngeal nerve.
Treatments of RLN injury
Intraoperative treatment: if clamping, traction, and ligation injuries are found, they should be released immediately, nerve-nurturing drugs and symptomatic treatment can be given after surgery, and in general, patients can recover within 2–3 months (17). If the RLN is mistakenly cut, resulting in transection injury, end-to-end neuroanastomosis should be performed immediately. Performing the operation under a microscope if conditions allow is better to ensure minimal tension in the anastomosis and to promote postoperative neurological recovery as soon as possible. In general, patients can recover within 3–6 months (18,19).
Postoperative treatments: if patients develop hoarseness within a few days after surgery, which is considered to be caused by suture, ligation, or adhesion compression, then nerve exploration and decompression should be performed as soon as possible, and most patients can recover after the suture or adhesion is removed (20). Late postoperative treatments include vocal cord injection, thyroplasty, and arytenoidectomy, which shift the vocal cords medially to improve vocal function. Moreover, laser arytenoidectomy with vocal cord fixation enlarges the glottis and improves dyspnea (21). Now, there are more and more methods to repair RLN injury, such as simple anastomosis of nerve stump, nerve scaffold, tissue engineering and gene therapy (4,5,22).
RLN injury prevention
RLN exposure: RLN exposure can improve the safety of thyroid surgery (23,24). Hermann et al. studied a total of 26,323 RLNs in 15,513 patients undergoing thyroid surgery, and the rates of permanent RLN injury were 0.4% and 1.1% (P≤0.001) in the exposure group (41/10,458) and the nonexposure group (174/15,865), respectively (25). However, surgeons should focus on avoiding the pursuit of full exposure and excessive skeletonization of the RLN, which tend to damage the nutrient vessels of the RLN (26). If the operation is performed under a magnifier or a microscope, the likelihood of nerve injury can be minimized.
Refinement of thyroid surgery: We believe that thyroid surgery is an “art in surgery”. For the surgeon, a meticulous operation determines the efficacy of surgery and the postoperative quality of life of the patient. The surgeon should be patient, meticulous, and gentle during the operation, maintain a clean surgical field, avoid nerve injury caused by clamping and excessive traction of the nerve, and be aware of the possibility of an NRLN.
Proper use of energy tools: Traction, clamping, and other behaviors often injure the epineurium and perineurium, while heat conduction often injures the endoneurium and causes permanent functional damage (27). Lin et al. studied the critical temperature of porcine RLNs using the Continuous Intraoperative Neuromonitoring (C-IONM) system and found that 60 °C was the critical temperature (28). These results indicate that if an energy device is used improperly, its heat can easily cause damage to the RLN, and the thermal damage to the RLN is invisible to the surgeon and may not be recognized during surgery (29). Therefore, proper use of energy tools is extremely important for the surgeon. The energy devices commonly used in surgery include an electric knife, bipolar electrocoagulation, and an ultrasonic scalpel. Studies have shown that the thermal spread produced by the use of an ultrasonic scalpel is lower than that produced by the use of a monopolar electric knife, and its damage to axons is also significantly less severe than that caused by an electric knife (30); therefore, proper use of ultrasonic scalpels is helpful for dissection of the RLN (31). However, Maeda et al. (32) reported that the use of an ultrasonic knife could induce temporary RLN palsy when the knife was within 3 mm of the RLN; thus, a distance greater than 5 mm from the RLN was recommended when using an ultrasonic knife. In addition, when using an ultrasonic knife, the working blade of the ultrasonic knife must be oriented towards the thyroid gland, and the protection blade should be oriented towards the back. The running time of the ultrasonic knife should be short to avoid damage to the RLN caused by transverse thermal spread from the ultrasonic knife. Wet gauze can also be used in the RLN area when an ultrasonic knife is used, which can prevent not only thermal damage from the energy device but also hot steam droplets from the ultrasonic knife from falling on the surface of the RLN when addressing the back of thyroid gland. However, important anatomical structures should not be contacted by the blade immediately after use, which may cause thermal injury.
Application of an RLN monitoring system: Intraoperative Neuromonitoring (IONM) is used in 20–40% of thyroid surgeries (33). IONM is a technique that can assist in identifying the RLN and judging its function. Determining the approximate course of the RLN, identifying an NRLN, and monitoring the function of the RLN are helpful. Because energy devices carry the risk of thermal injury to the RLN, IONM can guide the use of these devices and reduce their risk of damaging the RLN. However, many different views on IONM exist, and some scholars suggest that the use of IONM can reduce the incidence of RLN injury (34). Higgins et al. conducted a meta-analysis on the data of 64,699 patients and found no significant difference in the incidence of RLN injury when comparing operations with IONM to those performed under direct visualization alone (35). However, IONM is beneficial for neuroprotection in patients who require surgical treatment for thyroid malignancy, thyroid reoperation, a retrosternal goiter, existing unilateral vocal cord paralysis, and contralateral lobes (36). At present, extensive data are needed to further confirm the clinical value of IONM. In the last few years, the new technique which is Continuous Intraoperative Neuromonitoring (C-IONM) has emerged. Compared with IONM, this technique can improve the amplitude of neural signals in real-time surgery and determine the risk of RLN injury at vagal latency (37). We believe that C-IONM has broad application prospects.
However, several shortcomings exist in this study. (I) No postoperative objective voice examination was performed in a timely manner; in this study, only a subjective voice examination was performed, and an objective voice examination was not performed to avoid unnecessary doctor-patient disputes because the doctor-patient relationship in China is still relatively intense. (II) No relevant animal experiments were performed. In this study, we investigated RLN function after anastomosis and found that timely intraoperative end-to-end neuroanastomosis was feasible for ensuring the patient’s vocal function, but it has not been further explored from the perspective of electrophysiological recovery. (III) In this study, several patients had to undergo resection of the diseased RLN followed by end-to-end neuroanastomosis due to tumor invasion of the RLN (Figure 5), and we could not macroscopically determine whether the nerve resection margin still had cancer tissue invasion. If anastomosis of the resection margins containing residual cancer tissue is compared with anastomosis of clean resection margins, could the postoperative recovery of a patient’s vocal function be different?
Figure 5.
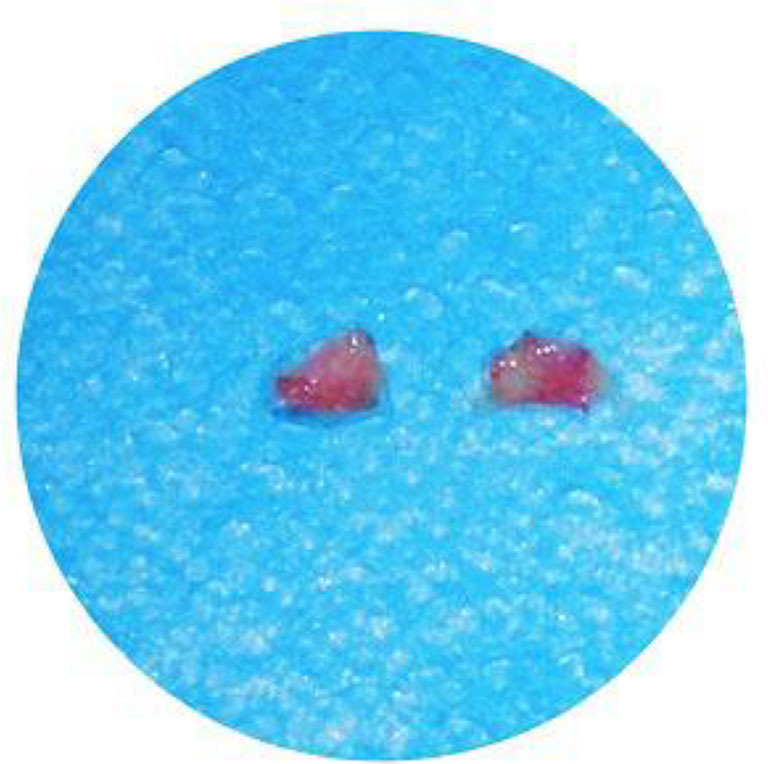
Excised RLN lesions. RLN, recurrent laryngeal nerve.
Based on the gradual promotion of advanced surgical instruments and IONM in clinical practice, surgeons can avoid RLN injury as much as possible. Even if the unilateral RLN is completely injured, immediate end-to-end anastomosis of the RLN can maximize preservation of the postoperative vocal function of patients.
Acknowledgments
We thank all the patients who participated in this study.
Funding: Hunan Provincial Health and Family Planning Commission sponsored this article through the project of the 2017 annual scientific research plan. (Project number: A2017003).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by committee board of Hunan Provincial People’s Hospital Medical Faculty (NO.: 2019117) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
Footnotes
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/gs-20-633
Data Sharing Statement: Available at http://dx.doi.org/10.21037/gs-20-633
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/gs-20-633). All author report grants from Projects of Hunan Provincial Health and Family Planning Commission, outside the submitted work. The authors have no other conflicts of interest to declare.
References
- 1.He WL, Mai PC, Liu XJ. Nine cases report of laryngeal recurrent nerve injuty. J Mod Oncol 2003;11:184. [Google Scholar]
- 2.Jeannon JP, Orabi AA, Bluch GA, et al. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract 2009;63:624-9. 10.1111/j.1742-1241.2008.01875.x [DOI] [PubMed] [Google Scholar]
- 3.Zakaria HM, Al Awad NA, Al Kreedes AS, et al. Recurrent laryngeal nerve injury in thyroid surgery. Oman Med J 2011;26:34-8. 10.5001/omj.2011.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crumley RL. Laryngeal synkinesis revisited. Ann Otol Rhinol Laryngol 2000;109:365-71. 10.1177/000348940010900405 [DOI] [PubMed] [Google Scholar]
- 5.Caillaud M, Richard L, Vallat J M, et al. Peripheral nerve regeneration and intraneural revascularization. Neural Regen Res 2019;14:24-33. 10.4103/1673-5374.243699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karnell MP, Melton SD, Childes JM, et al. Reliability of clinician-based (GRBAS and CAPE-V) and patient-based (V-RQOL and IPVI) documentation of voice disorders. J Voice 2007;21:576-90. 10.1016/j.jvoice.2006.05.001 [DOI] [PubMed] [Google Scholar]
- 7.Dionigi G, Wu CW, Kim HY, et al. Severity of Recurrent Laryngeal Nerve Injuries in Thyroid Surgery. World J Surg 2016;40:1373-81. 10.1007/s00268-016-3415-3 [DOI] [PubMed] [Google Scholar]
- 8.Randolph GW, Dralle H, International Intraoperative Monitoring Study Group, et al Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 2011;121 Suppl 1:S1-S16. 10.1002/lary.21119 [DOI] [PubMed] [Google Scholar]
- 9.Altorjay A, Rüll M, Paál B, et al. "Mystic" transient recurrent nerve palsy after thyroid surgery. Head Neck 2013;35:934-41. 10.1002/hed.23048 [DOI] [PubMed] [Google Scholar]
- 10.Sancho JJ, Pascual-Damieta M, Pereira JA, et al. Risk factors for transient vocal cord palsy after thyroidectomy. Br J Surg 2008;95:961-7. 10.1002/bjs.6173 [DOI] [PubMed] [Google Scholar]
- 11.Tang WJ, Sun SQ, Wang XL, et al. An applied anatomical study on the recurrent laryngeal nerve and inferior thyroid artery. Surg Radiol Anat 2012;34:325-32. 10.1007/s00276-011-0905-8 [DOI] [PubMed] [Google Scholar]
- 12.Yarbrough DE, Thompson GB, Kasperbauer JL, et al. Intraoperative electromyographic monitoring of the recurrent laryngeal nerve in reoperative thyroid and parathyroid surgery. Surgery 2004;136:1107-15. 10.1016/j.surg.2004.06.040 [DOI] [PubMed] [Google Scholar]
- 13.Thomusch O, Machens A, Sekulla C, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: prospective multicenter study in Germany. World J Surg 2000;24:1335-41. 10.1007/s002680010221 [DOI] [PubMed] [Google Scholar]
- 14.Yang X, Cao J, Yan Y, et al. Comparison of the safety of electrotome, Harmonic scalpel, and LigaSure for management of thyroid surgery. Head Neck 2017;39:1078-85. 10.1002/hed.24701 [DOI] [PubMed] [Google Scholar]
- 15.Owaki T, Nakano S, Arimura K, et al. The ultrasonic coagulating and cutting system injures nerve function. Endoscopy 2002;34:575-9. 10.1055/s-2002-33221 [DOI] [PubMed] [Google Scholar]
- 16.Chávez KV, Barajas EM, Soroa F, et al. Safety assessment of the use of ultrasonic energy in the proximity of the recurrent laryngeal nerve in a porcine model. Am J Surg 2018;215:186-90. 10.1016/j.amjsurg.2017.04.013 [DOI] [PubMed] [Google Scholar]
- 17.Song Q, Li XM. Principles and strategies for the prevention and treatment of parathyroid and laryngeal nerve injuries during thyroid surgery Chin J Clin Oncol 2017;44:409-14. [Google Scholar]
- 18.Zhang D, Sun H, Tufano R, et al. Recurrent laryngeal nerve management in transoral endoscopic thyroidectomy. Oral Oncol 2020;108:104755. 10.1016/j.oraloncology.2020.104755 [DOI] [PubMed] [Google Scholar]
- 19.Dionigi G, Wu CW, Kim HY, et al. Severity of Recurrent Laryngeal Nerve Injuries in Thyroid Surgery. World J Surg 2016;40:1373-81. [DOI] [PubMed] [Google Scholar]
- 20.Zheng HL, Zhou SM, Chen SC, et al. Laryngeal reinnervation for recurrent laryngeal nerve injuries caused by thyroid surgery. Chin J Gen Surg 2004;19:30-3. [Google Scholar]
- 21.Ding J, Dong P. Injury and repair of recurrent laryngeal nerve in thyroid surgery. Chin J Otorhinolaryngol Tradit West Med 2014;22:310-2. [Google Scholar]
- 22.Li Y, Garrett G, Zealear D. Current Treatment Options for Bilateral Vocal Fold Paralysis: A State-of-the-Art Review. Clin Exp Otorhinolaryngol 2017;10:203-12. 10.21053/ceo.2017.00199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zhang HT, Lu YF, Liao QH, et al. The evaluation of recurrent laryngeal nerves exposure during thyroid resection: a meta-analysis. Chin J Gen Surg 2005;20:204-6. [Google Scholar]
- 24.Zhang SQ, Yi WJ, Li ZQ, et al. The clinical implication of exposure of recurrent laryngeal nerve during operation for benign thyroid neoplasm. Chin J Gen Surg 2009;18:484-6. [Google Scholar]
- 25.Hermann M, Alk G, Roka R, et al. Laryngeal recurrent nerve injury in surgery for benign thyroid diseases: effect of nerve dissection and impact of individual surgeon in more than 27,000 nerves at risk. Ann Surg 2002;235:261-8. 10.1097/00000658-200202000-00015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu WW, Deng XZ, Fan YB, et al. Injury and precaution of recurrent laryngeal nerve during thyroid surgery. Shanghai Med J 2015;38:731-4. [Google Scholar]
- 27.Wu CW, Dionigi G, Sun H, et al. Intraoperative neuromonitoring for the early detection and prevention of RLN traction injury in thyroid surgery: a porcine model. Surgery 2014;155:329-39. 10.1016/j.surg.2013.08.015 [DOI] [PubMed] [Google Scholar]
- 28.Lin YC, Dionigi G, Randolph GW, et al. Electrophysiologic monitoring correlates of recurrent laryngeal nerve heat thermal injury in a porcine model. Laryngoscope 2015;125:E283-90. 10.1002/lary.25362 [DOI] [PubMed] [Google Scholar]
- 29.Dionigi G. Energy based devices and recurrent laryngeal nerve injury: the need for safer instruments. Langenbecks Arch Surg 2009;394:579-80; author reply 581-6. 10.1007/s00423-008-0454-8 [DOI] [PubMed] [Google Scholar]
- 30.Chen C, Kallakuri S, Cavanaugh JM, et al. Acute and subacute effects of the ultrasonic blade and electrosurgery on nerve physiology. Br J Neurosurg 2015;29:569-73. 10.3109/02688697.2015.1023772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sun H, Wu CW, Kim HY, et al. Neural monitoring represent central safety asset for new technologies in thyroid surgery in translational protocols. Am J Surg 2018;216:1235-6. 10.1016/j.amjsurg.2018.01.022 [DOI] [PubMed] [Google Scholar]
- 32.Maeda S, Shimizu K, Minami S, et al. Video-assisted neck surgery for thyroid and parathyroid diseases. Biomed Pharmacother 2002;56 Suppl 1:92s-95s. 10.1016/S0753-3322(02)00236-6 [DOI] [PubMed] [Google Scholar]
- 33.Horne SK, Gal TJ, Brennan JA. Prevalence and patterns of intraoperative nerve monitoring for thyroidectomy. Otolaryngol. Head Neck Surg 2007;136:952- 6. 10.1016/j.otohns.2007.02.011 [DOI] [PubMed] [Google Scholar]
- 34.Barczyński M, Konturek A, Cichoń S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 2009;96:240-6. 10.1002/bjs.6417 [DOI] [PubMed] [Google Scholar]
- 35.Higgins TS, Gupta R, Ketcham AS, et al. Recurrent laryngeal nerve monitoring versus identification alone on post-thyroidectomy true vocal fold palsy: a meta-analysis. Laryngoscope 2011;121:1009-17. 10.1002/lary.21578 [DOI] [PubMed] [Google Scholar]
- 36.Melin M, Schwarz K, Lammers BJ, et al. IONM-guided goiter surgery leading to two-stage thyroidectomy--indication and results. Langenbecks Arch Surg 2013;398:411-8. 10.1007/s00423-012-1032-7 [DOI] [PubMed] [Google Scholar]
- 37.Konturek A, Barczyński M. The evolution and progress of mechanism and prevention of recurrent laryngeal nerve injury. Ann Thyroid 2018;3:32 10.21037/aot.2018.11.02 [DOI] [Google Scholar]


