Abstract
Background:
To plan for decreasing the prevalence of malnutrition among children, reliable data of current status are required. The aim of the present cross-sectional study was to estimate the prevalence and trend of malnutrition among Iranian children.
Methods:
PubMed, ISI Web of Science, Scopus, Google Scholar, and Iranian databases including SID and Magiran were searched for studies published prior to October 2017 with MeSH terms of Malnutrition, Nutrition Disorders, Wasting, Stunting, Underweight, Undernutrition, Nutrition, Anthropometry, Weight, and Children and Iran. Three random effect models were applied to estimate the pooled prevalence of underweight, stunting, and wasting. Meta-regression and cumulative meta-analysis were performed. All analyses were also conducted separately for two different age groups including 0–6 years old (preschool) and 7–11 years old (primary school). Seventy-five studies (information of 1,069,815 individuals) were included in the final meta-analysis.
Results:
The overall prevalence of underweight, stunting, and wasting was estimated to be 8.4% [95% confidence interval (CI): 7.6–9.1], 14.5% (95% CI: 13.1–15.9) and 5.6% (95% CI: 5–6.2) in children age 0–6 years, and 6.6% (95% CI: 4.8–8.4), 7.3% (95% CI: 5.6–9.1), and 8.3% (95% CI: 6–10.7) in children age 7–11 years, respectively.
Conclusions:
The cumulative meta-analysis showed a decrease in the general trend of malnutrition in both preschool and primary school children of Iran. Stunting and wasting were the most common form of malnutrition in Iranian preschool and primary school children, respectively. The decreasing trend of malnutrition was much more noticeable about stunting.
Keywords: Child, growth disorders, Iran, malnutrition, stunting, underweight, wasting
Introduction
Lack of the provision of children's nutritional needs inhibits optimal growth and development. As a result, malnutrition occurs which is a big challenge that nations face. Although the estimated global prevalence of malnutrition has shown a decline from the 1990s, it still affects a lot of people in low- and middle-income countries. According to the United Nations International Children's Emergency Fund (UNICEF)/World Health Organization (WHO)/World Bank Group Joint Child Malnutrition Estimates in 2017, the worldwide prevalence of childhood stunting and wasting was 22.2% and 7.5%, respectively.[1] It has been estimated that 45% of deaths of children under 5 years of age are related to malnutrition.[2] Malnutrition also has long-term consequences such as poor physical and mental function, increased vulnerability to infections, developing noncommunicable diseases in adulthood, and economic burden for healthcare system.[3] Some of these effects can be persistent and irreversible.[4] Despite classification of Iran as an upper-middle income country by the World Bank and an increase in the number of overweight and obese children, malnutrition is still a problem in this country. In the UNICEF global nutrition report in 2016, Iran has been ranked 14th and 53rd regarding stunting and wasting among nearly 130 countries, respectively.[5] A national survey of the under-5-year Iranian children in 2010 showed that 5.7% were underweight, 10.13% were stunted, and the prevalence of wasting was 3.29%.[6]
Different factors may play roles in developing pediatrics malnutrition. Socioeconomic status, infectious diseases, maternal educational level, poor hygiene, and low health literacy are the most important factors determining undernutrition in children.[7] Lack of access to health services, low education,[8,9,10] poverty, food insecurity, and lack of nutritional knowledge have been proposed as main risk factors of malnutrition in Iran.
To plan for decreasing the prevalence of malnutrition among children, reliable data sources are required. The huge amount of all national information in this field should be summarized with a systematic review study. In addition, evaluating national trend of malnutrition can help policymakers to assess the effectiveness of interventional programs designed to solve the problem. Therefore, we conducted a systematic review and meta-analysis to determine the prevalence and trend of malnutrition in 0–6 years compared with 7–11 years old Iranian children. To the best of our knowledge, our study is comprehensive because (1) it covers two age groups of children, (2) it is based on all three indices of malnutrition (underweight, stunting, and wasting), and (3) it investigates the trend of malnutrition. According to our knowledge, there is no comprehensive study evaluating the trend of malnutrition among Iranian children.
Methods
Study design and search strategy
PubMed, ISI Web of Science, Scopus, Google Scholar, and English and Persian Iranian databases including SID and Magiran were searched for studies published prior to October 2017 with MeSH terms “malnutrition OR wasting OR wasted OR stunting OR stunted OR underweight OR undernutrition OR undernourished OR nutrition OR anthropometry OR weight OR height OR stature OR failure to thrive OR nutrition status” AND “children OR child OR childhood” AND “Iran.”
Based on the definition of the WHO, malnutrition in children is diagnosed when weight for age, height for age (HAZ), or weight for height (WHZ) z-scores are below 2 standard deviation compared with the international reference median value.[11]
Inclusion and exclusion criteria
In addition to primary articles, articles' references were also manually searched for additional studies. After excluding duplicates, the titles and abstracts of each article were reviewed independently by two of the authors for inclusion. The inclusion criteria were as follows: studies that were conducted in Iran (published articles in either Persian or English languages), participants less than 12 years, and classification of malnutrition according to the National Center for Health Statistics (NCHS)/WHO criteria.
The exclusion criteria were reported malnutrition using percentiles or percent of median (not based on the WHO definition of malnutrition), studies on nonhealthy children, and studies which their full-texts were not found after contacting their journal office. In cases of disagreement between two authors, the third author was consulted.
Quality assessment and data extraction
The quality of studies was assessed through “Quality Assessment Checklist for Prevalence Studies” (adapted from Hoy et al.).[12] The total score of this checklist was categorized into three subgroups including low risk (0–3), moderate risk (4–6), and high risk (7–9) of bias. Studies with a low risk of bias were included in meta-analysis accordingly.
Data analysis
The variance of underweight, stunting, and wasting, as the three most commonly used anthropometric indices for the assessment of malnutrition in children, was computed using the binomial distribution formula in each study. Publication bias was evaluated through visual examination of funnel plots and through Egger's test. The heterogeneity index among different studies calculated using tau square (t2) test.
As the heterogeneity among studies was significant, three random effect models using Meta command in Stata was applied to estimate the pooled prevalence of underweight, stunting, and wasting. The effect of different variables as the source of the heterogeneity was investigated using meta-regression approach (quality score, mean age, age group, deprivation index, date of publication group, and sample size group were the variables that were included in the meta-regression approach). Cumulative meta-analysis was performed to evaluate the time-trend of each anthropometric index of children malnutrition after data sorting by publication date. The quality score of studies, mean age of participants, age group, sample size of studies, publication date, and deprivation index of cities were entered in meta-regression as independent variables. The sample size was categorized into extra small (n< 200), small (n = 201–500), medium (n = 501–1000), large (n = 1001–10,000), and extra-large (n ≥ 10,000). Publication date of studies was categorized into four groups: before 2000, 2000–2005, 2006–2011, and 2012–2017. Deprivation index of cities was determined according to Sheikh-Beiglou's study[13] in which cities have a score of 1–30 based on four methods used to measure the development level. All analyses were also conducted separately for two different age groups of target population including 0–6 years old (preschool) and 7–11 years old (primary school) and were compared. We used Stata version 11 (College Station, TX, USA) for conducting the analysis.
Results
Summary of included studies
Out of 513 identified studies through our search strategy, 75 studies (age group 0–6, 60; and age group 7–12, 15 studies) had our inclusion criteria and were included in the meta-analysis [Figure 1 and Table 1]. In total, the information of 1,052,143 children age 0–6 years and 17,672 children age 7–11 years were considered in meta-analysis.
Figure 1.
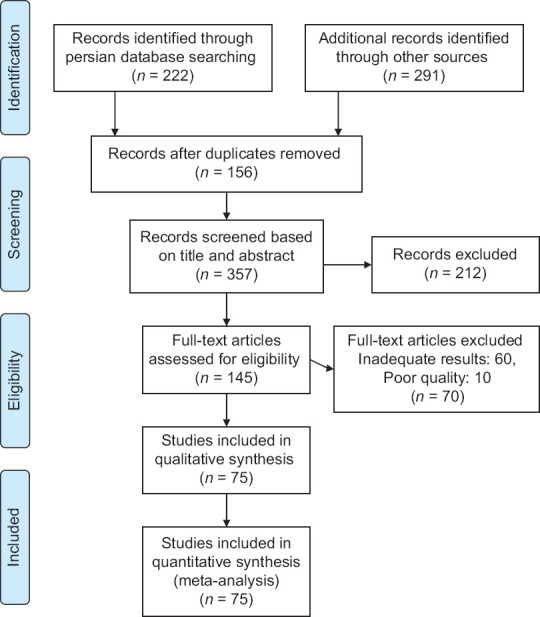
Study selection process based on PRISMA 2009 flow diagram
Table 1.
Description of studies that met our eligibility criteria
| Authors | Year of publication | Province/city | Sample Size | Prevalence (%) | Age | Quality score | ||
|---|---|---|---|---|---|---|---|---|
| WAZ | HAZ | WHZ | ||||||
| 0-6 years old | ||||||||
| Farrokh-Eslamlou et al.[23] | 2013 | West Azarbaijan Province | 3341 | 4.3 | 8.7 | 7.5 | Under 5 years | 1 |
| Holakoui-Naieni et al.[24] | 2002 | Eslamshahr_Rey_Qom | 1624 | 5.4 | 24.4 | 4.5 | Under 5 years | 2 |
| Yarparvar et al.[25] | 2006 | Bam | 500 | 15.2 | 8.9 | 5.6 | 6-59 months | 1 |
| Farajzadeh et al.[26] | 2012 | Birjand | 1132 | 9.9 | 3.6 | 25 | 5-7 years | 1 |
| Fesharakinia et al.[27] | 2013 | Birjand | 480 | 6.3 | 9.8 | 0.8 | Under 5 years | 1 |
| Poorabdollahi et al.[28] | 2004 | Tabriz | 400 | 6.6 | 9.4 | 2.0 | Under 6 years | 2 |
| Nasiri-Rineh et al.[29] | 2003 | Tonekabon | 425 | 37.0 | 80.0 | Under 5 years | 1 | |
| Naderi-Beni et al.[30] | 2013 | Chadegan | 403 | 6.5 | 12.7 | 2.7 | Under 5 years | 1 |
| Ramazani et al.[31] | 2009 | South Khorasan Province | 700 | 10.6 | 5.3 | 11.6 | 0-24 months | 1 |
| Sharifzadeh et al.[32] | 2008 | South Khorasan Province | 1807 | 12.9 | 16.6 | 7.5 | Under 6 years | 1 |
| Moradi-Lake et al.[33] | 2009 | Robat-Karim | 1406 | 7.7 | Under 6 years | 1 | ||
| Salem et al.[34] | 2002 | Rafsanjan | 1070 | 11.5 | 10.3 | 5.8 | 1-5 years | 1 |
| Ansari et al.[35] | 2009 | Zahedan | 1245 | 3.4 | 7.6 | 4.2 | 2-5 years | 2 |
| Sheykhi et al.[36] | 2012 | Zahedan | 514 | 17.3 | 25.3 | 6.8 | 6-59 months | 2 |
| Nakhshab et al.[37] | 2002 | Sari | 700 | 3.9 | Under 2 years | 1 | ||
| Rimaz[38] | 2004 | Savojbolagh | 1243 | 4.1 | 9.4 | 3.9 | Under 5 years | 1 |
| Emamian et al.[39] | 2011 | Shahrood | 1395 | 5.7 | 10.3 | 4.7 | Under 6 years | 1 |
| Zabihi et al.[39] | 2013 | Babol | 782 | 2.8 | 2.7 | 6.9 | Under 2 years | 2 |
| Nojomi et al.[40] | 2003 | Karaj | 600 | 13.9 | 20.3 | 4.9 | Under 5 years | 1 |
| Ahmadipour et al.[41] | 2016 | Kerman | 360 | 9.2 | 6.4 | 15.2 | 2-5 years | 2 |
| Razavieh et al.[42] | 2001 | Kermanshah | 400 | 17.5 | 8.8 | 14.3 | 0-36 months | 3 |
| Veghari et al.[43] | 1999 | Gorgan | 491 | 4.7 | 40.3 | Under 5 years | 2 | |
| Kabir et al.[44] | 2006 | Golestan Province | 1473 | 4.1 | 10.8 | 3.2 | Under 2 years | 2 |
| Soheili-Azad et al.[45] | 2004 | Nahavand | 300 | 3.0 | 13.3 | 2.7 | 0-36 months | 2 |
| Gholami et al.[46] | 2013 | Neishabour | 1621 | 8.1 | 3-6 years | 2 | ||
| Dehghan et al.[47] | 2004 | Dayer | 450 | 14.4 | 15.4 | 9.1 | Under 5 years | 2 |
| Hooshyarrad et al.[48] | 2008 | National | 2562 | 7.6 | 13.1 | 4.5 | Under 5 years | 0 |
| Sheikholeslam et al.[49] | 2008 | National | 34200 | 5.2 | 4.7 | 3.7 | Under 5 years | 0 |
| Veghari et al.[50] | 2007 | Gorgan | 2802 | 6.4 | 48.3 | Under 6 years | 2 | |
| Veghari et al.[51] | 1997 | Gorgan | 2639 | 6.7 | 45.5 | 4.3 | Under 5 years | 2 |
| Veghari et al.[51] | 2004 | Gorgan | 2858 | 5.0 | 19.3 | 3.4 | Under 5 years | 2 |
| Nouri-Saeidlou et al.[52] | 2014 | West Azerbaijan | 902 | 2.3 | 7.3 | 1.4 | 6-59 months | 1 |
| Nouri-Saeidlou et al.[52] | 2014 | Kermanshah | 829 | 3.6 | 3.3 | 2.6 | 6-59 months | 1 |
| Nouri-Saeidlou et al.[52] | 2014 | Isfahan | 794 | 5.9 | 11.2 | 5.0 | 6-59 months | 1 |
| Malekafzali et al.[53] | 2000 | Sibak_Borujen | 99 | 11.0 | 9.0 | Under 5 years | 3 | |
| Namakin et al.[54] | 2014 | Birjand | 822 | 5.2 | 11.8 | 1.8 | Under 2 years | 1 |
| Veghari et al.[55] | 2015 | Gorgan | 2530 | 6.4 | 15.4 | 2.6 | Under 5 years | 2 |
| Shafieian et al.[56] | 2013 | Mashhad | 671 | 4.3 | 3.1 | 4.3 | 24-59 months | 1 |
| Motlagh et al.[57] | 2010 | National | 862433 | 19.1 | 6.5 | 6-7 y | 0 | |
| Delvarianzadeh et al.[58] | 2017 | Shahroud | 706 | 7.1 | 5.9 | 4.5 | Under 2 years | 1 |
| Zahraei et al.[59] | 2016 | Sistan-va-Baluchestan | 263 | 11.4 | 12 months | 1 | ||
| Maddah et al.[60] | 2007 | Rasht | 1319 | 7.1 | 8.6 | 8.0 | 3-6 years | 1 |
| Veghari et al.[61] | 2009 | Gorgan | 1569 | 5.2 | 21.7 | 25-60 months | 2 | |
| Almasian Kia et al.[6] | 2017 | National | 8443 | 5.7 | 10.1 | 3.3 | Under 2 years | 0 |
| Jahanihashemi et al.[62] | 2017 | Qazvin | 1351 | 4.8 | 5.8 | 10.3 | 0-72 months | 1 |
| Akhlaghi et al.[63] | 2013 | Yasuj | 285 | 2.8 | 1.4 | 5.0 | ≤18 months | 2 |
| NouriSaeidlou et al.[64] | 2014 | Salmas (west Azerbijan) | 902 | 9.0 | 28.7 | 5.8 | 0-59 months | 1 |
| Sheikholeslam et al.[65] | 2004 | Ilam | 1178 | 10.6 | 19.6 | 1.1 | 6-35 months | 1 |
| Sheikholeslam et al.[65] | 2004 | Borazjan (Bushehr) | 1117 | 17.7 | 27.8 | 6.8 | 6-35 months | 1 |
| Sheikholeslam et al.[65] | 2004 | Bardsir (Kerman) | 1031 | 25.9 | 34.0 | 3.9 | 6-35 months | 1 |
| Ahmadi et al.[66] | 2014 | Shiraz | 150 | 1.4 | 4.8 | 2.7 | 36-48 months | 1 |
| Zavoshy et al.[67] | 2012 | Qazvin | 2385 | 4.1 | 3-6 years | 1 | ||
| Kavosi et al.[68] | 2014 | Fars Province | 15408 | 9.7 | 9.5 | 8.2 | 0-6 years | 1 |
| Payandeh et al.[69] | 2013 | Khorasan | 70339 | 7.5 | 12.5 | 4.4 | 0-5 years | 1 |
| Karajibani et al.[70] | 2014 | Sistan and Baluchestan | 1570 | 19.4 | 32.1 | 9.4 | 0-6 years | 1 |
| Sharifzadeh et al.[71] | 2010 | South Khorasan Province | 1807 | 12.8 | 16.6 | 7.4 | Under 6 years | 1 |
| Mahyar et al.[72] | 2010 | Qazvin | 804 | 1.3 | 2.8 | 0-24 months | 1 | |
| Khatibi et al.[73] | 2016 | Kerman | 443 | 25.2 | 3.1 | 2-6 years | 1 | |
| Haratipour et al.[74] | 2016 | Shahroud | 1850 | 6.7 | 5.8 | 7.7 | 4-6 years | 1 |
| Edalat et al.[75] | 2014 | Shiraz | 202 | 12.3 | 4.9 | 12.3 | 3-6 years | 1 |
| 7-11 years old | ||||||||
| Hooshmand et al.[76] | 2012 | Ahwaz | 2232 | 1.4 | 5.6 | 1.7 | 6-9 years | 1 |
| Aghamolaei et al.[77] | 2003 | Bandar Abbas | 1300 | 12.2 | 11.7 | 15.7 | 7-12 years | 1 |
| Mahboob et al.[78] | 2004 | Tabriz | 480 | 4.4 | 4.6 | 6-12 years | 2 | |
| Pourhashemi et al.[79] | 2007 | Tehran | 788 | 1.5 | 1.8 | 5.2 | 7 years | 1 |
| Delvarianzadeh et al.[80] | 2005 | Shahrood | 630 | 6.5 | 8.1 | 5.9 | 6-12 years | 2 |
| Delvarianzadeh et al.[81] | 2006 | Shahrood | 890 | 14.7 | 15.3 | 11.6 | 6-12 years | 2 |
| Darvishi et al.[82] | 2009 | Kordestan Province | 1100 | 6.9 | 5.6 | 10.8 | 7-11 years | 1 |
| Alavi-Naeini et al.[83] | 2002 | Kerman | 905 | 8.8 | 11.8 | 10 years | 1 | |
| Noroozi et al.[84] | 2011 | Golpayegan | 1062 | 5.4 | 3.0 | 7-11 years | 2 | |
| Dehghan et al.[85] | 2010 | Larestan | 876 | 7.3 | 6.5 | 9.8 | 7-11 years | 1 |
| Alipour et al.[86] | 2016 | Tabriz | 330 | 1.2 | 3.6 | 7-11 years | 1 | |
| Nematian et al.[87] | 2008 | Tehran | 209 | 2.8 | 21.0 | 7-11 years | 1 | |
| Hamedi-Shahraki et al.[88] | 2016 | Sistan and Baluchestan | 610 | 12.8 | 16.9 | 7-11 years | 1 | |
| Veghari et al.[9] | 2013 | Gorgan | 5698 | 3.2 | 4.9 | 5.1 | 6-10 years | 2 |
| Soheili Azad et al.[45] | 2004 | Tehran | 562 | 6.5 | 6.5 | 9.6 | 6-10 years | 1 |
WAZ=Weight for age, HAZ=Height for age, WHZ=Weight for height
Meta-analysis
The overall prevalence of underweight was 8.1% [95% confidence interval (CI): 7.3–8.8], stunting was 13.1% (95% CI: 11.9–14.2), and wasting was 6.1% (95% CI: 5.5–6.6) in both age groups.
The corresponding figure in two subgroups of age is shown in Table 2, Figures 2a-f and 3. The results of meta-regression showed the date of publication (coefficient = −0.02; 95% CI: −0.04; −0.004) and deprivation index (coefficient = 0.002; 95% CI: 0.11–0.35) for underweight; the date of publication (coefficient = −0.06; 95% CI: −0.09, −0.03) for stunting; and the mean age of children in each age group (coefficient = 0.02; 95% CI: 0.009–0.03) and age group (coefficient = −0.09; 95% CI: −0.16, −0.02) for wasting were the main sources of the heterogeneity [Table 3].
Table 2.
Prevalence of underweight, stunting, and wasting in 0-6 and 7-11 years old Iranian children
| 0-6 years | 7-11 years | |
|---|---|---|
| Underweight % (95% CI) | 8.4 (7.6-9.1) | 6.6 (4.8-8.4) |
| Stunting % (95% CI) | 14.5 (13.1-15.9) | 7.3 (5.6-9.1) |
| Wasting %(95% CI) | 5.6 ( 5-6.2) | 8.3 (6-10.7) |
CI=confidence interval
Figure 2a.
Forest plot of the prevalence of underweight in 0–6 years old Iranian children
Figure 2f.
Forest plot of the prevalence of wasting in 7–11 years old Iranian children
Figure 3.

The prevalence of malnutrition in 0–6 years old Iranian children compared with 7–11 years old children. WAZ = Weight for age, HAZ = Height for age, WHZ = Weight for height
Table 3.
Results of meta-regression model for underweight, stunting, and wasting in Iranian children (for studies published prior to October 2017)
| Predictors | WAZ | HAZ | WHZ | |||
|---|---|---|---|---|---|---|
| Coefficient (95% CI) | P | Coefficient (95% CI) | P | Coefficient (95% CI) | P | |
| Quality score | −0.01 (−0.04-0.1) | 0.25 | 0.01 (−0.04-0.06) | 0.66 | 0.007 (−0.01-0.03) | 0.49 |
| Mean age | 0.01 (−0.004-0.02) | 0.15 | −0.004 (−0.03-0.02) | 0.74 | 0.02 (0.009-0.03) | 0.00* |
| Age group (reference group: 0-6 years) | −0.08 (−0.17-0.01) | 0.08 | −0.06 (−0.24-0.11) | 0.46 | −0.09 (−0.16- -0.02) | 0.01* |
| Sample size group | −0.01 (−0.026-0.006) | 0.22 | 0.005 (−0.03-0.04) | 0.74 | −0.0009 (−0.01-0.01) | 0.88 |
| Date of publication group | −0.02 (−0.04- -0.004) | 0.02* | −0.06 (−0.09- -0.03) | <0.001* | −0.001 (−0.01-0.01) | 0.83 |
| Deprivation index | 0.002 (0.11-0.35) | 0.02* | 0.0008 (−0.002-0.004) | 0.57 | 0.0006 (−0.0005-0.002) | 0.27 |
WAZ=Weight for age, HAZ=Height for age, WHZ=Weight for height; CI=Confidence interval. *Significant coefficient
Figure 2b.
Forest plot of the prevalence of underweight in 7–11 years old Iranian children
Figure 2c.
Forest plot of the prevalence of stunting in 0–6 years old Iranian children
Figure 2d.
Forest plot of the prevalence of stunting in 7–11 years old Iranian children
Figure 2e.

Forest plot of the prevalence of wasting in 0–6 years old Iranian children
Cumulative meta-analysis
The results of meta-regression and cumulative meta-analysis showed the significant decreasing trends of underweight and stunting in both age groups; however, the trend of wasting was decreasing but not significant. This trend was more obvious in age group 0–6 years old. Moreover, the trend of reduction was more noticeable for stunting in both age groups [Table 3 and Figure 4a-f].
Figure 4a.

Cumulative meta-analyses of the prevalence of underweight in 0–6 years old Iranian children
Figure 4f.
Cumulative meta-analyses of the prevalence of wasting in 7–11 years old Iranian children
Figure 4b.
Cumulative meta-analyses of the prevalence of underweight in 7–11 years old Iranian children
Figure 4c.

Cumulative meta-analyses of the prevalence of stunting in 0–6 years old Iranian children
Figure 4d.

Cumulative meta-analyses of the prevalence of stunting in 7–11 years old Iranian children
Figure 4e.
Cumulative meta-analyses of the prevalence of wasting in 0–6 years old Iranian children
Discussion
This systematic review and meta-analysis was conducted on the published literature to estimate the prevalence of malnutrition among Iranian children. Totally, 75 published studies gained eligibility for inclusion in this review, most of which were published during the past decade. The national prevalence of underweight, stunting, and wasting in children age 0–6 years was as follows: 8.4%, 14.5%, and 5.6%. The corresponding figures for children age 7–11 years was 6.6%, 7.3%, and 8.3%. According to the reported statistics of malnutrition in neighboring countries of Iran including Turkey in 2008:[14] (underweight 2.8%, stunting 10.3%, and wasting 0.9%) and Pakistan in 2012:[15] (underweight 39.4%, stunting 63.9%, and wasting 17.9%), Iran represents an intermediate state. This variation could be related to the differences in risk factors of pediatrics malnutrition including short birth spacing, socioeconomic status, mother's low level of education, and insufficient nutritional knowledge.[16]
Interestingly, stunting was more prevalent among 0–6 years old children. This observed prevalence was higher than the World Bank data (7.1% in 2004)[17] and lower than the global prevalence of stunting among children under 5 years of age (25% in 2013).[18] In addition, compared with the latest WHO website statistics,[1] our finding is more promising. Our findings confirm that stunting is the most common form of malnutrition in children below 6 years of age.[18] Stunting is associated with higher morbidity and mortality rates, retardate physical and mental growth, and an increased risk of adulthood diseases.[18] As stunting is reflective of chronic malnutrition, performing more accurate screening programs might result in achieving global nutrition targets for 2025.[19]
In children age 7–11 years, wasting was more noticeable than underweight and stunting. In contrast to HAZ, WHZ is a measure of more acute malnutrition. This finding was comparable with a study in Nigeria by Adedeji et al. In this study, the prevalence of thinness was 11.1%, underweight had a prevalence of 10.7%, and 10.1% of children were stunted.[20] Inadequate intake of carbohydrate, having a large family size, and household food insecurity have been introduced as determinants of malnutrition in school children.[21]
The results of cumulative meta-analysis can be interpreted in two ways: first, regarding the last line of cumulative meta-analysis result, the cumulative prevalence of underweight, stunting, and wasting was 6.5% (95% CI: 6.4–6.6), 6.9% (95% CI: 6.8–6.9), and 4.3% (95% CI: 4.2–4.4) in children age 0–6 years, and 3.4% (95% CI: 3.1–3.6), 5.3% (95% CI: 5–5.7), and 4.7% (95% CI: 4.4–5) in children age 7—11 years, respectively. Second, the general trend of malnutrition is decreasing in both preschool and primary school Iranian children; this is much more noticeable about stunting. Our results are comparable with the world trend in malnutrition. A decrease in the global prevalence of malnutrition has been reported from nearly 40% in 1990 to 25% in 2013.[18] This illustrates Iran's significant success in achieving global nutrition targets for 2025. This reduction was highly significant for Asian countries. According to the “ first 1000 days theory,”[22] failure to grow in the period between conception and child's second birthday has a critical role in being stunted. So, our further reduction in stunting compared with wasting and underweight could be attributed to improved prenatal health cares.
Limitation of Study
This study can be considered as an important step in highlighting the extent of the problem by producing reliable data sources and help policymakers improve children nutrition policies. However, several limitations should be considered when interpreting our findings. Mentioned heterogeneity could confound the observed results. In addition, some studies included in the review did not report all malnutrition indicators, or few studies had presented their results divided by sex; therefore, we were unable to perform subgroup analysis by sex. Moreover, any potential misclassification bias is possible to have been occurred in the results of included studies.
Conclusions
To the best of our knowledge, this systematic review is the first study that compared the pooled prevalence and trend of malnutrition between Iranian preschool and primary school children. Stunting and wasting were the most common form of malnutrition in Iranian preschool and primary school children, respectively. The general trend of malnutrition is decreasing in both preschool and primary school Iranian children; this is much more noticeable about stunting. In summary, the prevalence of malnutrition in Iran was in the lower limit of the global statistics. Higher number of stunted children under 5 years of age is an alarm for politicians to design preventive national programs for controlling chronic malnutrition.
Financial support and sponsorship
This research was supported by Arak University of Medical Sciences.
Conflict of interest
There is no conflict of interest.
References
- 1.World Health Organization (WHO) UNICEF/WHO/World Bank Group Joint Child Malnutrition Estimates. [Last accessed on 2019 Jan 01]. Available from: https://wwwwhoint/nutgrowthdb/2018-jme-brochurepdfua=1 .
- 2.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 3.Martins VJ, Toledo Florêncio TM, Grillo LP, do Carmo P, Franco M, Martins PA, et al. Long-lasting effects of undernutrition. Int J Environ Res Public Health. 2011;8:1817–46. doi: 10.3390/ijerph8061817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahan LK, Raymond JL, Escott-Stump S. Krause's Food & the Nutrition Care Process – E-Book: Elsevier Health Sciences. 2013 [Google Scholar]
- 5.United Nations International Children's Emergency Fund (UNICEF) UNCsF Global Nutrition Report. [[Last accessed on 2018 Apr 01]]. Available from: https://datauniceforg/wp-content/uploads/2016/06/130565-1pdf .
- 6.Almasian Kia A, Rezapour A, Khosravi A, Afzali Abarghouei V. Inequality in malnutrition in under-5 children in Iran: Evidence from the multiple indicator demographic and health survey, 2010. J Prev Med Public Health. 2017;50:201–9. doi: 10.3961/jpmph.17.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohseni M, Aryankhesal A, Kalantari N. Factors associated with malnutrition among under five-year-old children in Iran: A systematic review. Ann Trop Med Public Health. 2017;10:1147–58. [Google Scholar]
- 8.Karimi B, Ghorbani R, Niaki MA. Malnutrition and some related factors in primary school children, Semnan, Iran. J Egypt Public Health Assoc. 2016;91:174–8. doi: 10.1097/01.EPX.0000508181.56447.51. [DOI] [PubMed] [Google Scholar]
- 9.Veghari G. The relationship of ethnicity, socio-economic factors and malnutrition in primary school children in North of Iran: A cross-sectional study. J Res Health Sci. 2012;13:58–62. [PubMed] [Google Scholar]
- 10.Rabiee F, Geissler C. Causes of malnutrition in young-children – Gilan, Iran. J Trop Pediatr. 1990;36:65–170. doi: 10.1093/tropej/36.4.165. [DOI] [PubMed] [Google Scholar]
- 11.ECoPS W Physical status: The use of and interpretation of anthropometry. Report of a WHO Expert Committee. Geneva: World Health Organization; 1995. [PubMed] [Google Scholar]
- 12.Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: Modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–9. doi: 10.1016/j.jclinepi.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 13.Rana SB. Identifying deprived areas of Iran using combined ranking. Res Urban Planning. 2011;2:53–70. [Google Scholar]
- 14.Hacettepe University Institute of Population Studies MoHGDoMACHaFPTRPMUoSPOaT Turkey Demographic and Health Survey 2008 (TDHS-2008) [[Last accessed on 2018 Apr 01]]. Available from: http://wwwhipshacettepeedutr/eng/tdhs08zTDHS-2008_Main_Reportpdf .
- 15.Arif GM, Nazir S, Satti MN, Farooq S. Child malnutrition in Pakistan: Trends and determinants. Pak Inst Dev Econ. 2012 [Google Scholar]
- 16.Moridi G, Fathi M. A review of the malnutrition status of under-five year children in Iran. Adv Nurs Midwifery. 2009;64:47–53. [Google Scholar]
- 17.World Bank Group Prevalence of stunting height for age (% of children under 5) [[Last accessed 2018 Mar 01]]. Available from: https://dataworldbankorg/indicator/SHSTASTNTZSlocations=IR .
- 18.Onis M, Branca F. Childhood stunting: A global perspective. Matern Child Nutr. 2016;12:12–26. doi: 10.1111/mcn.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Organization WH. Sixty-Fifth World Health Assembly Resolutions, Decisions, Annexes.2012 WHA65/2012/REC/1 May 21-26 [Google Scholar]
- 20.Adedeji I, John C, Okolo S, Ebonyi A, Abdu H. Bashir M.Malnutrition and the Intelligence Quotient of Primary School Pupils in Jos, Nigeria. Br J Med Med Res. 2017;21:1–13. [Google Scholar]
- 21.Wolde M, Berhan Y, Chala A. Determinants of underweight, stunting and wasting among schoolchildren. BMC Public Health. 2015;15:8. doi: 10.1186/s12889-014-1337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.English R, Peer N, Honikman S, Tugendhaft A, Hofman KJ. 'First 1000 days' health interventions in low-and middle-income countries: Alignment of South African policies with high-quality evidence. Glob Health Action. 2017;10:1340396. doi: 10.1080/16549716.2017.1340396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Farrokh-Eslamlou HR, Oshnouei S, Ahmadi N, Babaei F. Geographical distribution of nutrition deficiency among children under five years old in the west Azerbaijan province, Iran. Urmia Med J. 2013;24:201–9. [Google Scholar]
- 24.Holakoui-Naieni K, Sadeghipour Rodsary H, Pishva H, Panahandeh Z, Assasi P. Monitoring growth in children aged up to 5 years in Islamshahr, Rey and Qom. J School Public Health Institute Public Health Res. 2002;1:17–27. [Google Scholar]
- 25.Yarparvar A.H, Omidvar N, Golestan B, Kalantari N. Study of nutritional status and some related factors in preschool children 6 to 59 months in areas damaged by earthquake in Bam city. Iran J Nutri Sci Food Industry. 2006;1:33–43. [Google Scholar]
- 26.Farajzadeh Z, Saadatjoo SA, Hosseini S, Hassani H, Taghizadeh M, Alahyari F. Prevalence of malnutrition in preschool children in Birjand City in 2010.New care. Mod Care J Sci. 2012;9 [Google Scholar]
- 27.Fesharakinia A, Sharifzadeh G. Prevalence of malnutrition in under 5-year old children in Birjand city in 2011. J Birjand Univ Med Sci. 2013;20:77–84. [Google Scholar]
- 28.Poorabdollahi P, Ebrahimi M, Kooshavar H. Food pattern and the growth status of preschool children in kindergartens of Tabriz. Med J Tabriz Univ Med Sci. 2004;38:22–6. [Google Scholar]
- 29.Nasiri-Rineh H, Salarkia N. Height and weight of under 5 year children in Tonekabon (2000) J Babol Univ Med Sci. 2004;6:55–9. [Google Scholar]
- 30.Naderi Beni M, Lak R, Jazaeri S, Eftekhar Ardebili H. Prevalence of Malnutrition under five years in chadegan (area district city) Iran 2011. Iran J Epidemiol. 2013;9:22–8. [Google Scholar]
- 31.Ramazani A, Raghebi S, Amirkhizi F. Nutritional status and its related factors in 0-24 month children in South Khorasan Province in 2006. Iran J Epidemiol. 2009;5:8–13. [Google Scholar]
- 32.Sharifzadeh GhR, Safari Raghebi S, Zeraatkar VA, Moudi M. Prevalence of malnutrition in under 6-year old children in South Khorasan in 2006. J Birjand Univ Med Sci. 2008;15:73–80. [Google Scholar]
- 33.Moradi-Lake M, Montazer M, Moradi M, Mahmoodi SMH, AlamzadehBahreini SAP, Askari S. Trend of stunting in children aged 0-6 years old in rural population of Robatkarim between 1997-1998 – Effect of age, birth cohort and period of time. Iranian J Epidemiol. 2009;5:27–34. [Google Scholar]
- 34.Salem Z. Anthropometric characteristics of rafsanjan primary schoolchildren based on body mass index and waist circumference in 2008. J Kerman Univ Med Sci. 2009;8:40–8. [Google Scholar]
- 35.Ansari H, Zareban I, Norouzi M, Fallah S, Lotfi B. Malnutrition among children aged 2-5 years old in Zahedan between 2007-2008. J Shahrekord Univ Med Sci. 2009;11:46–54. [Google Scholar]
- 36.Sheykhi M, Eftekhari-Nia M, Hadipour M, Esmaillzadeh A. Prevalence of stunting, underweight and wasting according to national center for health statistics criteria in under six years rural children of Zahedan, Iran, in 2010. Health Res J. 2012;9:153–8. [Google Scholar]
- 37.Nakhshab M, Nasiri H. Prevalence of malnutrition and its risk factors in children under 2 years of age in Sari, 1999. J Mazandaran Univ Med Sci. 2002;12:47–56. [Google Scholar]
- 38.Rimaz SH, Moghtaderi A, Shidfar F, Poor Malek F. Prevalence and determinants of protein-energy malnutrition among children under the age of 5 in Savojbolagh (2002-2003) J Iran Univ Med Sci. 2004;12:97–105. [Google Scholar]
- 39.Emamian MH, Gorgani N, Fateh M. Malnutrition status in children of Shahroud, Iran. Knowledge Health. 2011;6:7–14. [Google Scholar]
- 40.Nojomi N, Kafashi A, Najmabadi SH. The study of frequency of malnutrition risk factors in under 5 years children in Karaj, 2001-2002. J Iran Univ Med Sci. 2003;10:123–32. [Google Scholar]
- 41.Ahmadipour H, Mirzaesmaeili S. The frequency of malnutrition and its related factors in 2-5-year old children of Kerman Suburb srea in 2014. Health Develop J. 2016;5:188–95. [Google Scholar]
- 42.Razavieh SV, Poorabdollahi P, Nikkhah S, Dastgiri S, Karimnejad-Asl M. Prevalence of malnutrition in children aged 0-36 months in Kermanshah health centers. J Tabriz Univ Med Sci. 2001;35:27–32. [Google Scholar]
- 43.Veghari Gh, Ahmadpour M, Vakili MA. Assessment of height and weight of under 6 year children in Gorgan villages in 1998. J Mazandaran Univ Med Sci. 1999;12:66–73. [Google Scholar]
- 44.Kabir MJ, Keshtkar A, Lashkar-Blooki F. Prevalence of malnutrition in children under two years of age and its underlying factors in Golestan province. J Gorgan Univ Med Sci. 2006;8:32–9. [Google Scholar]
- 45.Azad AA, Nourjah N, Shahbazi F. Relationship of intestinal parasitic infections to malnutrition among schoolchildren near Tehran, Iran. Southeast Asian J Trop Med Public Health. 2004;35:116–9. [Google Scholar]
- 46.Gholami AS, Rastegari A, Taghavi A. Prevalence of underweight in 3-6 year-old children in Neishabour. J Neishabour Univ Med Sci. 2013;1:10–3. [Google Scholar]
- 47.Dehghan A, Akbarzadeh F. Prevalence of malnutrition in children under 5 years old in Dayyer, 2001. Secrets Welfare. 2004;30:16–20. [Google Scholar]
- 48.Hooshyarrad A, Dorosti-Motlagh AR, Kalantari N, Abdollahi M, Abtahi M. Prevalence of stunting, underweight, wasting and overweight in Iranian children under the age of five (2000-2002) Iran J Nutr Sci Food Technol. 2008;3:49–56. [Google Scholar]
- 49.Sheikholeslam RN, Abdollahi Z, Zarrati M, Vaseghi S, Sadeghi-Ghotbabadi F, Kolahdooz F, et al. Current status and ten-year trend malnutrition in children under 5 Year in Iran. Iran J Epidemiol. 2008;4:21–8. [Google Scholar]
- 50.Veghari GR. Assessment of physical growth among the under 6 years children in rural area in Gorgan, Iran. Pakistan J Nutr. 2007;6:252–5. [Google Scholar]
- 51.Veghari Gh, Ahmadpour M. Comparison of nutritional status of children under 5 years old in villages of Gorgan in 1998 and 2003. Researcher. 2006;11:101–5. [Google Scholar]
- 52.Nouri Saeidlou S, Babaei F, Ayremlou P. Children malnutrition in northwestern, central and southern regions of Iran: Does geographic location matter? Glob J Health Sci. 2014;6:36–41. doi: 10.5539/gjhs.v6n4p36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Malekafzali H, Abdollahi Z, Mafi A, Naghavi M. Community-based nutritional intervention for reducing malnutrition among children under 5 years of age in the Islamic Republic of Iran. East Mediterr Health J. 2000;6:238–45. [PubMed] [Google Scholar]
- 54.Namakin K, Sharifzadeh GR, Zardast M, Khoshmohabbat Z, Saboori M. Comparison of the WHO child growth standards with the NCHS for estimation of malnutrition in Birjand-Iran. Int J Prev Med. 2014;5:653–7. [PMC free article] [PubMed] [Google Scholar]
- 55.Veghari G, Marjani A, Kazemi S, Bemani M, Shabdin M, Hashimifard A. The comparison of under-5-year nutritional status among Fars-native, Turkman and Sistani ethnic groups in the north of Iran. Int J Prev Med. 2015;6:69. doi: 10.4103/2008-7802.162061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shafieian T, Latiff LA, Lee MH, Mazidi M, Mobarhan MG, Tabatabaei G, et al. Determinants of nutritional status in children living in Mashhad, Iran. Int J Pediatr. 2013;1:9–18. [Google Scholar]
- 57.Motlagh ME, Kelishadi R, Amirkhani MA, Ziaoddini H, Dashti M, Aminaee T, et al. Double burden of nutritional disorders in young Iranian children: Findings of a nationwide screening survey. Public Health Nutr. 2011;14:605–10. doi: 10.1017/S1368980010002399. [DOI] [PubMed] [Google Scholar]
- 58.Delvarianzadeh M, Khosravi F, Gharibi H, Taghavi N. Factors affecting malnutrition and failure to thrive in children under 2 years of age in Shahroud, Iran, in 2015. Health Scope. 2017;6:e14176. [Google Scholar]
- 59.Zahraei SM, Izadi S, Mokhtari-Azad T. Factors affecting the seroconversion rate of 12-month-old babies after the first injection of measles vaccine in the southeast of Iran. Hum Vaccin Immunother. 2016;12:3118–24. doi: 10.1080/21645515.2016.1214346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maddah M, Mohtasham-Amiri Z, Rashidi A, Karandish M. Height and weight of urban preschool children in relation to their mothers' educational levels and employment status in Rasht City, northern Iran. Matern Child Nutr. 2007;3:52–7. doi: 10.1111/j.1740-8709.2007.00065.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Veghari G, Asadi J, Eshghinia S. Impact of ethnicity upon body composition assessment in Iranian northern children. J Clin Diagn Res. 2009;3:1779–83. [Google Scholar]
- 62.Jahanihashemi H, Noroozi M, Zavoshy R, Afkhamrezaei A, Jalilolghadr S, Esmailzadehha N. Malnutrition and birth related determinants among children in Qazvin, Iran. Eur J Public Health. 2017;27:559–62. doi: 10.1093/eurpub/ckx043. [DOI] [PubMed] [Google Scholar]
- 63.Akhlaghi M, Sadri Z, Tabatabaee HR. Malnutrition frequency and its family-related factors among infants in Yasuj City in Iran, 2011. J Health Sci Surv Syst. 2013;1:19–26. [Google Scholar]
- 64.Nouri Saeidlou S, Babaei F, Ayremlou P. Malnutrition, overweight, and obesity among urban and rural children in north of west Azerbijan, Iran? J Obes. 2014;2014:541213. doi: 10.1155/2014/541213. doi: 10.1155/2014/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sheikholeslam R, Kimiagar M, Siasi F, Abdollahi Z, Jazayeri A, Keyghobadi K, et al. Multidisciplinary intervention for reducing malnutrition among children in the Islamic Republic of Iran. East Mediterr Health J. 2004;10:844–52. [PubMed] [Google Scholar]
- 66.Ahmadi A, Moazen M, Mosallaei Z, Mohammadbeigi A, Amin-Iari F. Nutrient intake and growth indices for children at Kindergartens in Shiraz, Iran. J Pak Med Assoc. 2014;64:316–21. [PubMed] [Google Scholar]
- 67.Zavoshy R, Noroozi M, Jahanihashemi H, Kiamiri D. Nutritional intervention on malnutrition in 3-6 years old rural children in Qazvin Province, Iran. Pak J Biol Sci. 2012;15:347–52. doi: 10.3923/pjbs.2012.347.352. [DOI] [PubMed] [Google Scholar]
- 68.Kavosi E, Hassanzadeh Rostami Z, Kavosi Z, Nasihatkon A, Moghadami M, Heidari M. Prevalence and determinants of under-nutrition among children under six: A cross-sectional survey in Fars province, Iran. Int J Health Policy Manag. 2014;3:71–6. doi: 10.15171/ijhpm.2014.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Payandeh A, Saki A, Safarian M, Tabesh H, Siadat Z. Prevalence of malnutrition among preschool children in northeast of Iran, a result of a population based study. Glob J Health Sci. 2013;5:208–12. doi: 10.5539/gjhs.v5n2p208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Karajibani M, Shaykhei M, Montazerifar F, Eftekharenia M. Prevalence of malnutrition in children under 6 years in sistan and baluchestan province, Iran. Zahedan J Res Med Sci. 2014;16:20–4. [Google Scholar]
- 71.Sharifzadeh G, Mehrjoofard H, Raghebi S. Prevalence of malnutrition in under 6-year olds in South Khorasan, Iran. Iran J Pediatr. 2010;20:435–441. [PMC free article] [PubMed] [Google Scholar]
- 72.Mahyar A, Ayazi P, Fallahi M, Javadi T, Farkhondehmehr B, Amir J, et al. Prevalence of underweight, stunting and wasting among children in Qazvin, Iran. Iran J Pediatr Soc. 2010;2:37–43. [Google Scholar]
- 73.Khatibi M, Sanjari M, Farrokhi H, Amirzadeh R, Kashani B. Prevalence of underweightness and obesity as risk factors of future cardiovascular disease and type 2 diabetes among children in Iran. World Heart J. 2016;8:251–9. [Google Scholar]
- 74.Haratipour H, Sohrabi M B, Zolfaghari P, Nezakati E, Yahyaei E, Rezvani S. The relationship between malnutrition and intestinal parasitic infections among preschool children in East area of Iran. Int J Pediatr Mashhad. 2016;4:2011–8. [Google Scholar]
- 75.Edalat A, Abbaszadeh M, Eesvandi M, Heidari A. The relationship of severe early childhood caries and body mass index in a group of 3- to 6-year-old children in shiraz. J Dent (Shiraz) 2014;15:68–73. [PMC free article] [PubMed] [Google Scholar]
- 76.Hooshmand S. Nutritional status and stunting in primary school children from selected urban areas of Iran and India. 2012. [[Last accessed on 2020 Sep 16]]. Available from: http://irinflibnetacin:8080/jspui/handle/10603/109850 .
- 77.Aghamolaei T, Sobhani A. Evaluation of nutritional status of elementary school children in Bandar Abbas. J School Public Heal Institute Health Res. 2003;7:49–56. [Google Scholar]
- 78.Mahboob S, Shahraki M, Mahdavi R, Ghaemmaghami J. Nutritional assessment of 6-12 years old children in Tabriz. J Lorestan Univ Med Sci. 2004;21:25–33. [Google Scholar]
- 79.Pourhashemi SJ, Golestan B, Keshavarz SA. Micronutrients intake and their relationship with anthropometric indices and dental health among children. Tehran Univ Med J. 2007;65:72–7. [Google Scholar]
- 80.Delvarianzadeh M, Hosseinzadeh S. Nutritional status of elementary school children in Shahroud (2004) J Semnan Univ Med Sci. 2005:7. [Google Scholar]
- 81.Delvarianzadeh M, Sadeghian S. Prevalence of energy-protein malnutrition in elementary school students and relative factors. Payesh. 2006;5:263–9. [Google Scholar]
- 82.Darvishi SH, Hazhir MS, Reshadmanesh N, Shahsavari S. Malnutrition and its related factors in elementary school children of Kurdistan province. J Kurdistan Univ Med Sci. 2009;14:78–87. [Google Scholar]
- 83.Aiavi-Naieny AM, Djazayery A, Keyghobadi K, Hashemi M, Neekian Y. Comparative survey of nutritional status in 1-year-old female students in Kerman. J School Public Health Institute Health Res. 2002;1:57–67. [Google Scholar]
- 84.Noroozi H, Kazemi A, Tavakoli M, Alavi Sh, Bangaleh Z. Assessment of wasting and underweight among primary school students in urban and rural areas of Golpaygan. J Paramed Sci Tehran Univ Med Sci (Health Promotion) 2011;5:41–6. [Google Scholar]
- 85.Dehghan A, Ershad-Langroodi M, Kamali-Sarvestani M, Shahosseini S. Prevalence of malnutrition in primary school students in Larestan (2010) J North Khorasan Univ Med Sci. 2010;2:25–8. [Google Scholar]
- 86.Alipour B, Abbasalizad Farhangi M, Asghari S, Amirkhizi F, Dahri M, Abedimanesh N, et al. Child-specific food insecurity and its sociodemographic and nutritional determinants among Iranian schoolchildren. Ecol Food Nutr. 2016;55:231–40. doi: 10.1080/03670244.2015.1129324. [DOI] [PubMed] [Google Scholar]
- 87.Nematian J, Gholamrezanezhad A, Nematian E. Giardiasis and other intestinal parasitic infections in relation to anthropometric indicators of malnutrition: A large, population-based survey of schoolchildren in Tehran. Ann Trop Med Parasitol. 2008;102:209–14. doi: 10.1179/136485908X267876. [DOI] [PubMed] [Google Scholar]
- 88.Shahraki SH, Amirkhizi F, Amirkhizi B, Hamedi S. Household food insecurity is associated with nutritional status among iranian children. Ecol Food Nutr. 2016;55:473–90. doi: 10.1080/03670244.2016.1212710. [DOI] [PubMed] [Google Scholar]










