Key Points
Question
In the US from 2010 to 2017, what were national-level and state-level rates in neonatal abstinence syndrome (NAS) and maternal opioid-related diagnoses (MOD)?
Findings
In this repeated cross-sectional analysis including 11.8 million hospitalizations from 47 states and the District of Columbia, the national estimated rate of NAS was 7.3 per 1000 birth hospitalizations and the rate of MOD was 8.2 per 1000 delivery hospitalizations in 2017. From 2010 to 2017, estimated rates significantly increased nationally and for the majority of states, with substantial state-level variation.
Meaning
In the US, NAS and MOD rates increased from 2010 to 2017, with notable state-level variation.
Abstract
Importance
Substantial increases in both neonatal abstinence syndrome (NAS) and maternal opioid use disorder have been observed through 2014.
Objective
To examine national and state variation in NAS and maternal opioid-related diagnoses (MOD) rates in 2017 and to describe national and state changes since 2010 in the US, which included expanded MOD codes (opioid use disorder plus long-term and unspecified use) implemented in International Classification of Disease, 10th Revision, Clinical Modification.
Design, Setting, and Participants
Repeated cross-sectional analysis of the 2010 to 2017 Healthcare Cost and Utilization Project’s National Inpatient Sample and State Inpatient Databases, an all-payer compendium of hospital discharge records from community nonrehabilitation hospitals in 47 states and the District of Columbia.
Exposures
State and year.
Main Outcomes and Measures
NAS rate per 1000 birth hospitalizations and MOD rate per 1000 delivery hospitalizations.
Results
In 2017, there were 751 037 birth hospitalizations and 748 239 delivery hospitalizations in the national sample; 5375 newborns had NAS and 6065 women had MOD documented in the discharge record. Mean gestational age was 38.4 weeks and mean maternal age was 28.8 years. From 2010 to 2017, the estimated NAS rate significantly increased by 3.3 per 1000 birth hospitalizations (95% CI, 2.5-4.1), from 4.0 (95% CI, 3.3-4.7) to 7.3 (95% CI, 6.8-7.7). The estimated MOD rate significantly increased by 4.6 per 1000 delivery hospitalizations (95% CI, 3.9-5.4), from 3.5 (95% CI, 3.0-4.1) to 8.2 (95% CI, 7.7-8.7). Larger increases for MOD vs NAS rates occurred with new International Classification of Disease, 10th Revision, Clinical Modification codes in 2016. From a census of 47 state databases in 2017, NAS rates ranged from 1.3 per 1000 birth hospitalizations in Nebraska to 53.5 per 1000 birth hospitalizations in West Virginia, with Maine (31.4), Vermont (29.4), Delaware (24.2), and Kentucky (23.9) also exceeding 20 per 1000 birth hospitalizations, while MOD rates ranged from 1.7 per 1000 delivery hospitalizations in Nebraska to 47.3 per 1000 delivery hospitalizations in Vermont, with West Virginia (40.1), Maine (37.8), Delaware (24.3), and Kentucky (23.4) also exceeding 20 per 1000 delivery hospitalizations. From 2010 to 2017, NAS and MOD rates increased significantly for all states except Nebraska and Vermont, which only had MOD increases.
Conclusions and Relevance
In the US from 2010 to 2017, estimated rates of NAS and MOD significantly increased nationally and for the majority of states, with notable state-level variation.
This study uses US national hospital database data to update estimates of prevalence of neonatal abstinence syndrome and maternal opioid-related diagnoses between 2010 and 2017, and to describe state-level variation and associated lengths of stay and costs.
Introduction
The US opioid crisis has had a significant effect on many populations, including pregnant women and infants. From 2000 to 2014, substantial increases have occurred for national rates of maternal opioid use disorder (OUD) documented at delivery (1.1-6.5 per 1000 delivery hospitalizations)1 and neonatal abstinence syndrome (NAS; 1.2-8.0 per 1000 hospital births),2,3 a postnatal withdrawal syndrome commonly attributed to prenatal opioid exposure.4,5 For the mother-infant dyad, opioid misuse and exposure is associated with adverse outcomes. For example, maternal OUD is associated with severe maternal complications, including mortality,6,7 and infants diagnosed with NAS have longer and more complicated hospital stays than nonaffected infants.2,3,4,5
Rates of NAS and maternal OUD have been shown to vary greatly across states in the US.1,8 However, these analyses included a limited number of states and occurred before the transition from International Classification of Disease, 9th Revision, Clinical Modification (ICD-9-CM) to International Classification of Disease, 10th Revision, Clinical Modification (ICD-10-CM) in October 2015, which may have influenced identification of these conditions in hospital discharge records through expanded opioid-related codes.9 To address these gaps, a collaboration was undertaken between the Health Resources and Services Administration, the Agency for Healthcare Research and Quality (AHRQ), and the Centers for Disease Control and Prevention to evaluate the effect of the transition to ICD-10-CM on NAS and maternal opioid-related diagnoses (MODs), including OUD, and provide updated national and state rates. The objectives of this study were to update nationally estimated rates of NAS and MOD with the most recently available data in 2017 and examine changes since 2010, including associated length of stay and costs, and describe state-level variation in NAS and MOD rates in 2017 and changes since 2010 in all 47 states and the District of Columbia participating in AHRQ’s Healthcare Cost and Utilization Project (HCUP).10
Methods
As a secondary analysis of anonymized data, the AHRQ human protections administrator determined this project did not constitute research involving human participants; thus, informed consent and institutional review board approval were not required by the AHRQ.
Data Sources
National data were obtained from the HCUP National Inpatient Sample (NIS),11 an all-payer database of hospital discharges from community, nonrehabilitation hospitals for 2010 through 2017 (the latest available data year at the time of analysis). For any given year, the NIS is sampled from all available State Inpatient Databases (SID),12 which include a census of discharges from community, nonrehabilitation hospitals from participating states. In 2012, the NIS design changed from including all discharges within a 20% stratified random sample of hospitals to a 20% self-weighted, stratified, systematic random sample of discharges from all hospitals. State data were obtained from the SID from a total of 47 states and the District of Columbia that contributed at least 1 year of data within 2010 to 2017, representing approximately 97% of all US hospitalizations. Alabama, Idaho, and New Hampshire were the only states that did not contribute any data during the study period, and Alaska, Delaware, District of Columbia, Mississippi, and North Dakota contributed data during some of the study period. Discharge records contained ICD-coded diagnoses and procedures, as well as hospitalization characteristics, including patient demographics, admission source, discharge disposition, length of stay, and hospital charges. Neither the NIS nor the SID contain linkages between maternal deliveries and infant hospitalization; therefore, these were analyzed separately.
Primary Outcomes
Primary prespecified outcomes included NAS and MOD rates. Cases of NAS among birth hospitalizations were identified by ICD-9-CM diagnosis code 779.5 (drug withdrawal syndrome in newborn) and ICD-10-CM diagnosis code P96.1 (neonatal withdrawal symptoms from maternal use of drugs of addiction). Possible iatrogenic exclusions in ICD-9-CM (eTable 1 in the Supplement) are no longer necessary in ICD-10-CM with the introduction of P96.2 (withdrawal symptoms from therapeutic use of drugs in newborn). Birth hospitalizations were identified from ICD-CM diagnosis codes indicating single or multiple liveborn neonates (eTable 1 in the Supplement). The restriction of NAS diagnoses to birth hospitalizations differs from previous national analyses of NAS identified at any hospitalization,2,3,13 offering a conservative approach that avoids duplication of cases that may be identified in both the birth hospitalization and subsequent hospitalizations, but misses those only identified in a transfer admission or readmission. Birth hospitalizations that indicated a transfer from another hospital were also excluded to reduce duplication (<1%).
Cases of MOD among delivery hospitalizations were identified from diagnoses of opioid dependence and opioid abuse (eTable 1 in the Supplement), aligning with Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria.14 MOD cases identified using ICD-10-CM also included new coding additions of long-term use of opioid medications and unspecified opioid use, both of which may contribute to NAS. Although the ICD-9-CM MOD definition aligns with OUD, previous maternal OUD analyses included diagnoses of remission1,7,13 and are not directly comparable. We excluded remission because it does not indicate active opioid use.15 Delivery hospitalizations were identified by ICD diagnosis codes, Medicare Severity Diagnosis Related Group delivery codes, and ICD procedure codes for select delivery-related procedures (eTable 1 in the Supplement).16
Secondary Outcomes
To evaluate resource utilization patterns among births and deliveries associated with NAS and MOD, secondary prespecified outcomes included hospital length of stay and hospital costs. Hospital costs per discharge were calculated using the following method: hospital charges were obtained from the discharge abstract, charges were converted to costs using HCUP’s Cost-to-Charge Ratio Files,17 and costs were adjusted for inflation to 2017 US dollars using the gross domestic product price index,18 which is recommended for trends in expenditures and more broadly reflective of the US economy than the Consumer Price Index based on urban consumers.19
Demographic Characteristics
Demographic characteristics selected for analysis on the basis of previous associations included race/ethnicity, maternal age (for MOD only), primary expected payer, median household income quartile by zip code, and urban/rural residence.2,3,6,13 Race/ethnicity data, which were collected by self-report on admission to the hospital using fixed categories, were examined with the HCUP disparities analysis file.20 This separate file is produced for the National Healthcare Quality and Disparities Report and is constructed from SID files with reliable race/ethnicity reporting. Primary expected payer information reflects billing and expected reimbursement at the time of hospital discharge rather than final determination of insurance type or eligibility, and was grouped into the following categories: private, Medicaid, other public (including Medicare, workers’ compensation, Civilian Health and Medical Program of the Uniformed Services, Civilian Health and Medical Program of Veterans Affairs, Title V, and other governmental programs), and self-pay (including no charge). Urban/rural residence was defined as large metropolitan counties (>1 million residents in at least 1 urbanized area of a core-based statistical area), small metropolitan counties (50 000-999 999 residents in at least 1 urbanized area of a core-based statistical area), and nonmetropolitan/rural counties (micropolitan or non–core-based statistical area) based on a simplification of the US Department of Agriculture’s Urban Influence Codes.21 The 2003 codes were used for 2010 to 2013 data and the 2013 codes were used for 2014 to 2017 data.
Statistical Analyses
For national estimates from the NIS, we first described the demographic distribution of birth and delivery hospitalizations and NAS and MOD cases documented in 2017 (ICD-10-CM). National estimated NAS and MOD rates per 1000 birth and delivery hospitalizations were calculated overall and by demographic characteristics from 2010 through the third quarter of 2015 (ICD-9-CM) and 2016 and 2017 (ICD-10-CM). The fourth quarter of 2015 was excluded to acknowledge coding changes and allow clear comparisons between ICD-CM versions. Demographic differences in estimated rates were compared using t tests. Median length of stay and mean total hospital costs per NAS and MOD case and all other birth and delivery hospitalizations were calculated for 2010 to 2017 and compared using t tests. Differences in rates, median length of stay, and mean total hospital costs between 2010 and 2017 were compared with both absolute or simple differences (2017 – 2010) and relative percentage change calculations [(2017 – 2010)/2010 × 100] with 95% CIs,22 the latter of which facilitates comparisons across measures with different units and baseline values. Comparing the first and last estimates provides a measure of overall or total change without making assumptions on the rate or pace of change during this period. All NIS and disparity analysis file estimates were weighted to be nationally representative of hospitalizations in the universe of community nonrehabilitation hospitals in the American Hospital Association’s annual survey by sampling strata of census division, location and teaching status, bed size category, and ownership. Trend weights were applied to the 2010 and 2011 NIS to account for design changes and ensure consistent nationally representative estimates from 2010 through 2017. Standard errors and associated 95% CIs accounted for the complex sampling design.
For state-level analyses from the SID, NAS and OUD rates based on state of residence were calculated from 2010 through the third quarter of 2015 (using ICD-9-CM codes) and 2016 to 2017 (using ICD-10-CM codes). Consistent with national analyses, differences between 2010 and 2017 were compared using both absolute or simple differences and relative percentage changes with 95% CIs,22 the latter of which facilitates comparisons across states with varying baseline levels. Differences and percentage changes were only calculated for states that participated in HCUP and met reporting thresholds for confidentiality protections (≥10 cases) in both years. Maps were constructed using ArcGIS software to show 2017 variation and changes from 2010 to 2017 for both outcomes.
Individuals with missing data were excluded from respective analyses. Analyses were conducted using SAS version 9.4 (SAS Institute), with a statistical significance threshold of P < .05 for 2-sided tests. Because of the potential for type I error due to multiple comparisons, findings for secondary outcomes and analyses should be interpreted as exploratory.
Results
National Data
In 2017, there were 751 037 sampled birth hospitalizations, among which there were 5375 newborns with NAS, and 748 239 sampled delivery hospitalizations, among which there were 6065 women with MOD (Table 1). Mean gestational age for birth hospitalizations was 38.4 weeks and mean maternal age for delivery hospitalizations was 28.8 years. Less than 1% of birth and delivery hospitalizations were missing demographic information and less than 3% were missing secondary outcome information. Compared with all birth hospitalizations, neonates with NAS were significantly more likely (P < .001) to be non-Hispanic White (77.5% vs 52.2%), Medicaid-billed (84.0% vs 46.3%), reside in zip codes in the lowest quartile of median income (38.1% vs 28.1%), and live in nonmetropolitan counties (22.1% vs 13.4%). Similarly, compared with all delivery hospitalizations, individuals with MOD were significantly more likely (P < .001) to be non-Hispanic White (79.9% vs 52.5%), aged 25 to 29 years (37.0% vs 29.2%), Medicaid-billed (77.1% vs 43.3%), reside in zip codes in the lowest quartile of median income (36.4% vs 28.1%), and live in nonmetropolitan counties (20.6% vs 13.4%).
Table 1. Demographic Distribution of Birth and Delivery Hospitalizations and Neonatal Abstinence Syndrome and Maternal Opioid-Related Diagnoses, 2017a,b.
| Characteristic | Percent distribution | |||
|---|---|---|---|---|
| Neonatal abstinence syndrome | All birth hospitalizationsc | Maternal opioid-related diagnoses | All delivery hospitalizationsc | |
| Unweighted No. (weighted %) | 5375 (0.7) | 751 037 | 6065 (0.8) | 748 239 |
| Race/ethnicityd | ||||
| Non-Hispanic White | 77.5 | 52.2 | 79.9 | 52.5 |
| Non-Hispanic Black | 8.1 | 15.3 | 8.1 | 15.5 |
| Hispanic | 8.5 | 19.4 | 7.8 | 20.8 |
| Non-Hispanic Asian/Pacific Islander | 0.8 | 6.1 | 0.8 | 6.3 |
| Non-Hispanic other/multiple races | 5.1 | 6.9 | 3.5 | 4.9 |
| Maternal age, ye | ||||
| ≤19 | 1.5 | 5.2 | ||
| 20-24 | 18.7 | 19.8 | ||
| 25-29 | 37.0 | 29.2 | ||
| 30-34 | 28.4 | 28.3 | ||
| ≥35 | 14.4 | 17.5 | ||
| Primary expected payer | ||||
| Medicaid | 84.0 | 46.3 | 77.1 | 43.3 |
| Private | 10.0 | 46.3 | 16.4 | 50.9 |
| Self-pay | 4.8 | 4.9 | 1.8 | 2.5 |
| Other public | 1.2 | 2.5 | 4.7 | 3.3 |
| Zip code income quartilef | ||||
| 1 (lowest) | 38.1 | 28.1 | 36.4 | 28.1 |
| 2 | 28.8 | 25.7 | 30.6 | 25.7 |
| 3 | 20.9 | 24.4 | 21.1 | 24.4 |
| 4 (highest) | 12.2 | 21.9 | 11.9 | 21.8 |
| Urban/rural residenceg | ||||
| Metro | ||||
| Large | 42.3 | 57.2 | 44.4 | 57.0 |
| Small | 35.6 | 29.4 | 35.1 | 29.5 |
| Nonmetro | 22.1 | 13.4 | 20.6 | 13.4 |
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, National Inpatient Sample, 2017.
All estimates are weighted to the universe of community nonrehabilitation hospitals in the American Hospital Association’s annual survey by sampling strata of census division, urban/rural location and teaching status, bed size category, and ownership.
Birth hospitalizations refer to liveborn infant discharge records; delivery hospitalizations refer to maternal discharge records, regardless of pregnancy outcome.
From the Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, State Inpatient Databases disparities analysis file; nationally weighted from all records in states with reliable race/ethnicity reporting, which is collected by self-report on admission to the hospital using fixed categories.
Infant and maternal discharge records are not linked.
Median household income in quartile 1 is less than $44 000; quartile 2, $44 000 to $55 999; quartile 3, $56 000 to $73 999; and quartile 4, at least $74 000.
Based on a simplification of the US Department of Agriculture’s Urban Influence Codes to the following categories: large metropolitan counties (≥1 million residents in at least 1 urbanized area of a core-based statistical area), small metropolitan counties (50 000-999 999 residents in at least 1 urbanized area of a core-based statistical area), and nonmetropolitan/rural counties (micropolitan or non–core-based statistical area).
Between 2010 and 2017, the estimated rate of NAS significantly increased from 4.0 (95% CI, 3.3-4.7) to 7.3 (95% CI, 6.8-7.7) per 1000 birth hospitalizations, representing an absolute increase of 3.3 per 1000 birth hospitalizations (95% CI, 2.5-4.1) and a relative increase of 82% (95% CI, 57%-107%) (Table 2; eFigure 1 in the Supplement). The estimated rate of MOD significantly increased from 3.5 (95% CI, 3.0-4.1) to 8.2 (95% CI, 7.7-8.7) per 1000 delivery hospitalizations, representing an absolute increase of 4.6 per 1000 delivery hospitalizations (95% CI, 3.9-5.4) and a relative increase of 131% (95% CI, 101%-161%) (Table 3; eFigure 1 in the Supplement). Larger increases for MOD rates than for NAS rates occurred with new ICD-10-CM codes in 2016 (eFigure 1 in the Supplement). Estimated rates significantly increased across all demographic groups, with the exception of those with other public expected payers for NAS rates and those expected to self-pay for MOD rates, for which the increases were not statistically significant. In 2017, estimated rates of NAS and MOD were highest among those who were non-Hispanic White (NAS: 10.4 [95% CI, 9.7-11.1]; MOD: 12.4 [95% CI, 11.6-13.2]), were Medicaid-billed (NAS: 13.2 [95% CI, 12.3-14.1]; MOD: 14.6 [95% CI, 13.5-15.6]), resided in zip codes in the lowest code income quartile (NAS: 9.8 [95% CI, 9.0-10.7]; MOD: 10.5 [95% CI, 9.6-11.4]), and were rural residents (NAS: 12.1 [95% CI, 10.7-13.5]; MOD: 12.5 [95% CI, 11.1-13.9]). Conversely, estimated rates of NAS and MOD were lowest among those who were non-Hispanic Asian/Pacific Islander (NAS: 0.9 [95% CI, 0.7-1.1]; MOD: 1.0 [95% CI, 0.8-1.2]), were privately billed (NAS: 1.6 [95% CI, 1.4-1.7]; MOD: 2.6 [95% CI, 2.4-2.9]), resided in the zip codes in the highest income quartile (NAS: 4.0 [95% CI, 3.5-4.5]; MOD: 4.4 [95% CI, 3.9-5.0]), and were urban residents from large metropolitan areas (NAS: 5.4 [95% CI, 4.9-5.9]; MOD: 6.4 [95% CI, 5.7-7.0]).
Table 2. Neonatal Abstinence Syndrome Rates per 1000 Birth Hospitalizations, 2010-2017a,b.
| Characteristic | Rate per 1000 birth hospitalizationsc | Absolute difference (95% CI) from 2010-2017e | Change (95% CI) from 2010-2017, %e | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 (Q1-Q3)d |
2016 | 2017 | |||||
| Total | 4.0 | 4.1 | 4.7 | 5.8 | 6.4 | 6.5 | 7.0 | 7.3 | 3.3 (2.5 to 4.1) | 82 (57 to 107) | ||
| Race/ethnicityf | ||||||||||||
| Non-Hispanic White | 4.6 | 5.8 | 6.4 | 7.9 | 8.9 | 10.0 | 10.3 | 10.4 | 5.8 (4.9 to 6.6) | 124 (101 to 148) | ||
| Non-Hispanic Black | 1.8 | 1.9 | 2.0 | 2.8 | 3.0 | 3.3 | 3.7 | 3.7 | 1.9 (1.5 to 2.4) | 110 (75 to 145) | ||
| Hispanic | 1.3 | 1.6 | 1.8 | 2.0 | 2.2 | 2.3 | 2.7 | 3.1 | 1.6 (1.2 to 2.4) | 142 (75 to 210) | ||
| Non-Hispanic Asian/Pacific Islander | 0.2 | 0.5 | 0.4 | 0.8 | 0.6 | 0.7 | 0.7 | 0.9 | 0.5 (0.5 to 0.9) | 323 (142 to 504) | ||
| Non-Hispanic Other/multiple races | 1.8 | 2.7 | 2.9 | 2.9 | 3.8 | 3.3 | 4.7 | 5.1 | 2.7 (2.3 to 4.4) | 192 (115 to 268) | ||
| Primary payer | ||||||||||||
| Medicaid | 7.0 | 7.1 | 8.3 | 10.1 | 11.5 | 11.8 | 12.8 | 13.2 | 7.1 (4.6 to 7.8) | 89 (61 to 117) | ||
| Private | 1.1 | 1.3 | 1.3 | 1.6 | 1.7 | 1.7 | 1.5 | 1.6 | 1.3 (0.2 to 0.8) | 47 (21 to 72) | ||
| Self-pay | 4.1 | 4.7 | 5.3 | 6.9 | 6.6 | 6.6 | 6.8 | 7.1 | 4.7 (1.3 to 4.7) | 74 (27 to 122) | ||
| Other public | 2.8 | 2.9 | 2.6 | 2.6 | 3.3 | 3.6 | 4.1 | 3.6 | 2.9 (–0.7 to 2.4) | 29 (–28 to 87) | ||
| Zip code income quartileg | ||||||||||||
| 1 (lowest) | 5.2 | 5.1 | 6.3 | 7.6 | 8.5 | 8.6 | 9.2 | 9.8 | 5.1 (3.3 to 6.0) | 90 (58 to 123) | ||
| 2 | 4.1 | 4.1 | 4.9 | 6.3 | 6.8 | 7.0 | 8.0 | 8.1 | 4.1 (3.0 to 5.1) | 100 (67 to 133) | ||
| 3 | 4.1 | 3.8 | 4.1 | 5.0 | 5.7 | 5.8 | 6.3 | 6.2 | 3.8 (1.1 to 3.2) | 52 (24 to 80) | ||
| 4 (highest) | 2.5 | 3.0 | 3.1 | 3.6 | 3.9 | 4.0 | 3.7 | 4.0 | 3.0 (0.8 to 2.3) | 62 (27 to 97) | ||
| Urban/rural residenceh | ||||||||||||
| Metro | ||||||||||||
| Large | 3.6 | 3.8 | 3.9 | 4.5 | 5.0 | 5.1 | 5.4 | 5.4 | 3.8 (0.8 to 2.9) | 51 (18 to 84) | ||
| Small | 4.3 | 4.4 | 5.3 | 6.7 | 7.4 | 8.0 | 8.5 | 8.8 | 4.4 (3.2 to 5.8) | 105 (66 to 144) | ||
| Nonmetro | 5.0 | 4.6 | 6.8 | 8.4 | 10.5 | 9.3 | 10.6 | 12.1 | 4.6 (5.1 to 9.0) | 140 (86 to 194) | ||
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, National Inpatient Sample.
All estimates are weighted to the universe of community nonrehabilitation hospitals in the American Hospital Association’s annual survey by sampling strata of census division, urban/rural location and teaching status, bed size category, and ownership.
Birth hospitalizations refer to liveborn infant discharge records and are not linked to maternal discharge records; thus, maternal age is not available.
Excludes the fourth quarter to distinguish the transition to the International Classification of Disease, 10th Revision, Clinical Modification (ICD-10-CM) in October 2015.
Reflects the overall or total difference between the 2 end points: absolute difference (2017 – 2010) and percentage change [(2017 – 2010)/2010 × 100]
From the Healthcare Cost and Utilization Project, State Inpatient Databases disparities analysis file; nationally weighted from all records in states with reliable race/ethnicity reporting, which is collected by self-report on admission to the hospital using fixed categories.
Median household income of residents in the patient’s zip code was updated annually; 2017 range for quartile 1 was less than $44 000; quartile 2, $44 000 to $55 999; quartile 3, $56 000-$73 999; and quartile 4, at least $74 000.
Based on a simplification of the US Department of Agriculture’s Urban Influence Codes to the following categories: large metropolitan counties (≥1 million residents in at least 1 urbanized area of a core-based statistical area), small metropolitan counties (50 000-999 999 residents in at least 1 urbanized area of a core-based statistical area), and nonmetropolitan/rural counties (micropolitan or non–core-based statistical area).
Table 3. Maternal Opioid-Related Diagnoses Rates per 1000 Delivery Hospitalizations, 2010-2017a,b.
| Characteristic | Rate per 1000 delivery hospitalizationsc | Absolute difference (95% CI) from 2010-2017e | Change (95% CI) from 2010-2017, %e | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2011 | 2012 | 2013 | 2014 | 2015 (Q1-Q3)d |
2016 | 2017 | |||
| Total | 3.5 | 3.5 | 4.4 | 5.2 | 5.9 | 6.1 | 8.0 | 8.2 | 4.6 (3.9 to 5.4) | 131 (101 to 161) |
| Race/ethnicityf | ||||||||||
| Non-Hispanic White | 4.1 | 5.0 | 5.9 | 7.0 | 8.4 | 9.2 | 12.1 | 12.4 | 8.3 (7.4 to 9.3) | 205 (173 to 237) |
| Non-Hispanic Black | 1.4 | 1.5 | 1.7 | 2.2 | 2.4 | 2.6 | 3.8 | 4.2 | 2.9 (2.3 to 3.4) | 208 (143 to 273) |
| Hispanic | 0.9 | 1.3 | 1.3 | 1.5 | 2.0 | 1.8 | 2.7 | 3.0 | 2.1 (1.5 to 2.7) | 229 (139 to 319) |
| Non-Hispanic Asian/Pacific Islander | 0.2 | 0.2 | 0.5 | 0.5 | 0.5 | 0.6 | 0.8 | 1.0 | 0.8 (0.6 to 1.0) | 451 (178 to 724) |
| Non-Hispanic other/multiple races | 1.9 | 2.1 | 2.5 | 2.9 | 3.4 | 3.5 | 5.8 | 5.8 | 4.0 (2.8 to 5.1) | 211 (129 to 293) |
| Maternal age, y | ||||||||||
| ≤19 | 0.9 | 1.1 | 1.3 | 2.0 | 2.1 | 1.8 | 2.3 | 2.3 | 1.4 (0.8 to 2.0) | 158 (78 to 238) |
| 20-24 | 4.1 | 4.1 | 5.2 | 6.1 | 7.0 | 6.9 | 7.9 | 7.7 | 3.6 (2.6 to 4.6) | 88 (58 to 117) |
| 25-29 | 4.4 | 4.7 | 5.6 | 6.6 | 7.7 | 8.0 | 10.4 | 10.4 | 6.0 (4.9 to 7.0) | 135 (101 to 169) |
| 30-34 | 3.5 | 3.3 | 4.3 | 5.1 | 5.6 | 5.7 | 7.9 | 8.2 | 4.8 (3.9 to 5.6) | 138 (103 to 172) |
| ≥35 | 2.7 | 2.1 | 2.6 | 2.9 | 3.4 | 3.9 | 6.1 | 6.7 | 4.0 (3.1 to 4.9) | 147 (97 to 197) |
| Primary payer | ||||||||||
| Medicaid | 6.1 | 6.3 | 7.9 | 9.2 | 10.8 | 11.5 | 14.5 | 14.6 | 8.5 (7.0 to 10.0) | 139 (104 to 174) |
| Private | 1.0 | 1.0 | 1.1 | 1.5 | 1.7 | 1.6 | 2.4 | 2.6 | 1.6 (1.3 to 1.9) | 161 (116 to 207) |
| Self-pay | 3.9 | 6.6 | 6.3 | 7.4 | 6.8 | 6.0 | 7.2 | 5.8 | 2.0 (0.0 to 4.0) | 51 (–4 to 106) |
| Other public | 5.1 | 4.5 | 5.3 | 6.3 | 6.4 | 7.1 | 9.8 | 11.7 | 6.6 (4.2 to 9.0) | 129 (72 to 187) |
| Zip code income quartileg | ||||||||||
| 1 (lowest) | 4.8 | 5.1 | 6.0 | 7.1 | 8.1 | 7.9 | 10.6 | 10.5 | 5.8 (4.5 to 7.0) | 121 (87 to 155) |
| 2 | 3.8 | 3.6 | 4.7 | 5.7 | 6.4 | 6.8 | 8.8 | 9.7 | 5.8 (4.8 to 6.9) | 153 (114 to 193) |
| 3 | 3.4 | 3.0 | 3.9 | 4.4 | 5.2 | 5.5 | 7.2 | 7.0 | 3.6 (2.7 to 4.6) | 106 (70 to 142) |
| 4 (highest) | 1.9 | 2.1 | 2.5 | 3.1 | 3.3 | 3.6 | 4.5 | 4.4 | 2.6 (1.8 to 3.3) | 136 (84 to 188) |
| Urban/rural residenceh | ||||||||||
| Metro | ||||||||||
| Large | 3.3 | 3.2 | 3.6 | 4.1 | 4.6 | 4.7 | 6.4 | 6.4 | 3.0 (2.0 to 4.1) | 92 (53 to 131) |
| Small | 3.5 | 3.9 | 4.7 | 5.7 | 6.5 | 7.2 | 9.3 | 9.7 | 6.2 (5.0 to 7.3) | 176 (127 to 225) |
| Nonmetro | 4.4 | 4.4 | 6.6 | 8.2 | 10.3 | 9.4 | 11.9 | 12.5 | 8.1 (6.4 to 9.8) | 183 (126 to 241) |
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, National Inpatient Sample.
All estimates are weighted to the universe of community nonrehabilitation hospitals contained in the American Hospital Association’s annual survey by sampling strata of census division, urban/rural location and teaching status, bed size category, and ownership.
Delivery hospitalizations refer to maternal discharge records, regardless of pregnancy outcome.
Excludes the fourth quarter to distinguish the transition to International Classification of Disease, 10th Revision, Clinical Modification (ICD-10-CM) in October 2015, which expanded maternal opioid-related diagnoses to include new codes for long-term use of opioid medications and unspecified opioid use in addition to opioid dependence and abuse.
Reflects the overall or total difference between the 2 end points: absolute difference (2017 – 2010) and percentage change [(2017 – 2010)/2010 × 100].
From the Healthcare Cost and Utilization Project, State Inpatient Databases disparities analysis file; nationally weighted from all records in states with reliable race/ethnicity reporting, which is collected by self-report upon admission to the hospital using fixed categories.
Median household income of residents in the patient’s zip code was updated annually; 2017 range for quartile 1 was less than $44 000; quartile 2, $44 000 to $55 999; quartile 3, $56 000-$73 999; and quartile 4, at least $74 000.
Based on a simplification of the US Department of Agriculture’s Urban Influence Codes to the following categories: large metropolitan counties (≥1 million residents in at least 1 urbanized area of a core-based statistical area), small metropolitan counties (50 000-999 999 residents in at least 1 urbanized area of a core-based statistical area), and nonmetropolitan/rural counties (micropolitan or non–core-based statistical area).
Length of Stay and Costs of NAS and MOD
Compared with other birth hospitalizations in 2017, neonates with NAS had a significantly longer estimated median length of stay (9.2 days longer [95% CI, 8.3-10.0]) (10.8 days [95% CI, 9.9-11.6] vs 1.6 [95% CI, 1.6-1.6]; P < .001) and greater estimated mean cost (approximately $14 600 more [95% CI, $13 100-$16 000]) ($18 800 [95% CI, $17 400-$20 300] vs $4200 [95% CI, $4000-$4500]; P < .001; Table 4). Compared with other delivery hospitalizations, women with MOD also had a significantly longer estimated median length of stay (0.3 days longer [95% CI, 0.2-0.3]) (2.1 [95% CI, 2.0-2.1] vs 1.8 [95% CI, 1.8-1.9]; P < .001) and greater estimated mean costs (approximately $900 more [95% CI, $700- $1100) ($6100 [95% CI, $6000-$6300] vs $5200 [95% CI, $5100-$5300]; P < .001). Estimated median length of stay and estimated mean costs did not change significantly for either NAS or MOD between 2010 and 2017, despite significant increases in mean costs for other birth and delivery hospitalizations.
Table 4. Length of Stay and Costs Associated With Neonatal Abstinence Syndrome and Maternal Opioid-Related Diagnoses, 2010-2017a,b.
| Outcome | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 (Q1-Q3)c |
2016 | 2017 | Absolute difference (95% CI) from 2010-2017d | Change (95% CI) from 2010-2017, %d |
|---|---|---|---|---|---|---|---|---|---|---|
| Neonatal abstinence syndrome | ||||||||||
| Unweighted, No. | 3102 | 3205 | 3594 | 4322 | 4887 | 3734 | 5265 | 5375 | ||
| Median length of stay, (IQR), d | 12.0 (4.8-22.9) | 10.7 (4.4-22.5) | 10.5 (10.5-21.1) | 11.1 (4.2-21.8) | 10.8 (4.2-20.6) | 10.9 (4.3-20.7) | 11.3 (4.3-20.8) | 10.8 (4.4-20.1) | –1.2 (–3.1 to 0.7) | –10 (–26 to 6) |
| Costs, mean (SD) $e | 18 100 (24 900) | 18 800 (33 200) | 17 700 (29 100) | 18 700 (26 100) | 16 900 (24 500) | 18 000 (27 600) | 18 900 (33 900) | 18 800 (42 000) | 700 (–2000 to 3400) | 4 (–11 to 19) |
| Other birth hospitalizationsf | ||||||||||
| Unweighted No. | 779 291 | 791 546 | 753 893 | 746 715 | 756 367 | 568 035 | 750 141 | 732 452 | ||
| Length of stay, median (IQR), d | 1.6 (1.1-2.4) | 1.6 (1.1-2.3) | 1.6 (1.2-2.3) | 1.6 (1.1-2.3) | 1.6 (1.1-2.3) | 1.6 (1.1-2.2) | 1.6 (1.1-2.2) | 1.6 (1.1-2.2) | 0.0 (–0.1 to 0.0) | –2 (–6 to 1) |
| Costs, mean (SD), $e | 3600 (16 500) | 3700 (19 000) | 3800 (20 000) | 3900 (20 500) | 3900 (19 300) | 4000 (20 700) | 4300 (23 300) | 4200 (24 200) | 600 (200 to 1000) | 16 (6 to 27) |
| Maternal opioid-related diagnoses | ||||||||||
| Unweighted No. | 2734 | 2755 | 3309 | 3896 | 4509 | 3487 | 6055 | 6065 | ||
| Length of stay, median (IQR), d | 2.1 (1.4-3.0) | 2.0 (1.4-2.9) | 2.0 (1.4-2.8) | 2.0 (1.4-2.9) | 2.0 (1.4-2.9) | 2.1 (1.4-2.9) | 2.1 (1.4-2.9) | 2.1 (1.4-2.9) | 0.0 (–0.1 to 0.0) | –1 (–6 to 4) |
| Costs, mean (SD), $d | 6100 (8100) | 6300 (6400) | 5700 (5800) | 6100 (6300) | 5800 (5300) | 6100 (11 000) | 6200 (6300) | 6100 (5600) | 0 (–600 to 600) | 0 (–10 to 10) |
| Other delivery hospitalizationsf | ||||||||||
| Unweighted No. | 774 449 | 793 614 | 749 831 | 744 343 | 755 751 | 568 449 | 750 714 | 734 763 | ||
| Length of stay, median (IQR), d | 1.8 (1.3-2.6) | 1.8 (1.3-2.6) | 1.8 (1.3-2.6) | 1.8 (1.3-2.6) | 1.8 (1.3-2.6) | 1.8 (1.3-2.6) | 1.8 (1.3-2.6) | 1.8 (1.3-2.6) | 0.0 (–0.1 to 0.1) | 0 (–3 to 3) |
| Costs, mean (SD), $e | 4700 (4000) | 4800 (4000) | 4900 (4200) | 5000 (7400) | 5000 (4200) | 5100 (8000) | 5200 (4400) | 5200 (4600) | 500 (300 to 700) | 10 (6 to 14) |
Abbreviation: IQR, interquartile range.
Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, National Inpatient Sample.
All estimates, except for sample sizes, are weighted to the universe of community nonrehabilitation hospitals in the American Hospital Association’s annual survey by sampling strata of census division, urban/rural location and teaching status, bed size category, and ownership.
Excludes the fourth quarter to distinguish the transition to International Classification of Disease, 10th Revision, Clinical Modification (ICD-10-CM) in October 2015, which expanded maternal opioid-related diagnoses to include new codes for long-term use of opioid medications and unspecified opioid use in addition to opioid dependence and abuse.
Reflects the overall or total difference between the 2 end points: absolute difference (2017 – 2010) and percentage change [(2017 – 2010)/2010 × 100].
Adjusted to 2017 US dollars using the gross domestic product price index and rounded to the nearest hundred.
Birth hospitalizations refer to liveborn infant discharge records; delivery hospitalizations refer to maternal discharge records, regardless of pregnancy outcome.
State Data
In 2017, there were 3 550 105 birth hospitalizations and 3 561 752 in the census of discharge records from the SID of 47 states and the District of Columbia. NAS rates ranged from 1.3 per 1000 birth hospitalizations in Nebraska to 53.5 per 1000 birth hospitalizations in West Virginia, while MOD rates ranged from 1.7 per 1000 delivery hospitalizations in Nebraska to 47.3 per 1000 delivery hospitalizations in Vermont (Figure; eTables 2 and 3 in the Supplement). In addition to West Virginia, 4 other states had NAS rates that exceeded 20 per 1000 birth hospitalizations (Maine [31.4], Vermont [29.4], Delaware [24.2], and Kentucky [23.9]). In addition to Vermont, 4 other states had MOD rates that exceeded 20 per 1000 delivery hospitalizations (West Virginia [40.1], Maine [37.8], Delaware [24.3], and Kentucky [23.4]).
Figure. Neonatal Abstinence Syndrome and Maternal Opioid-Related Diagnoses Rates .
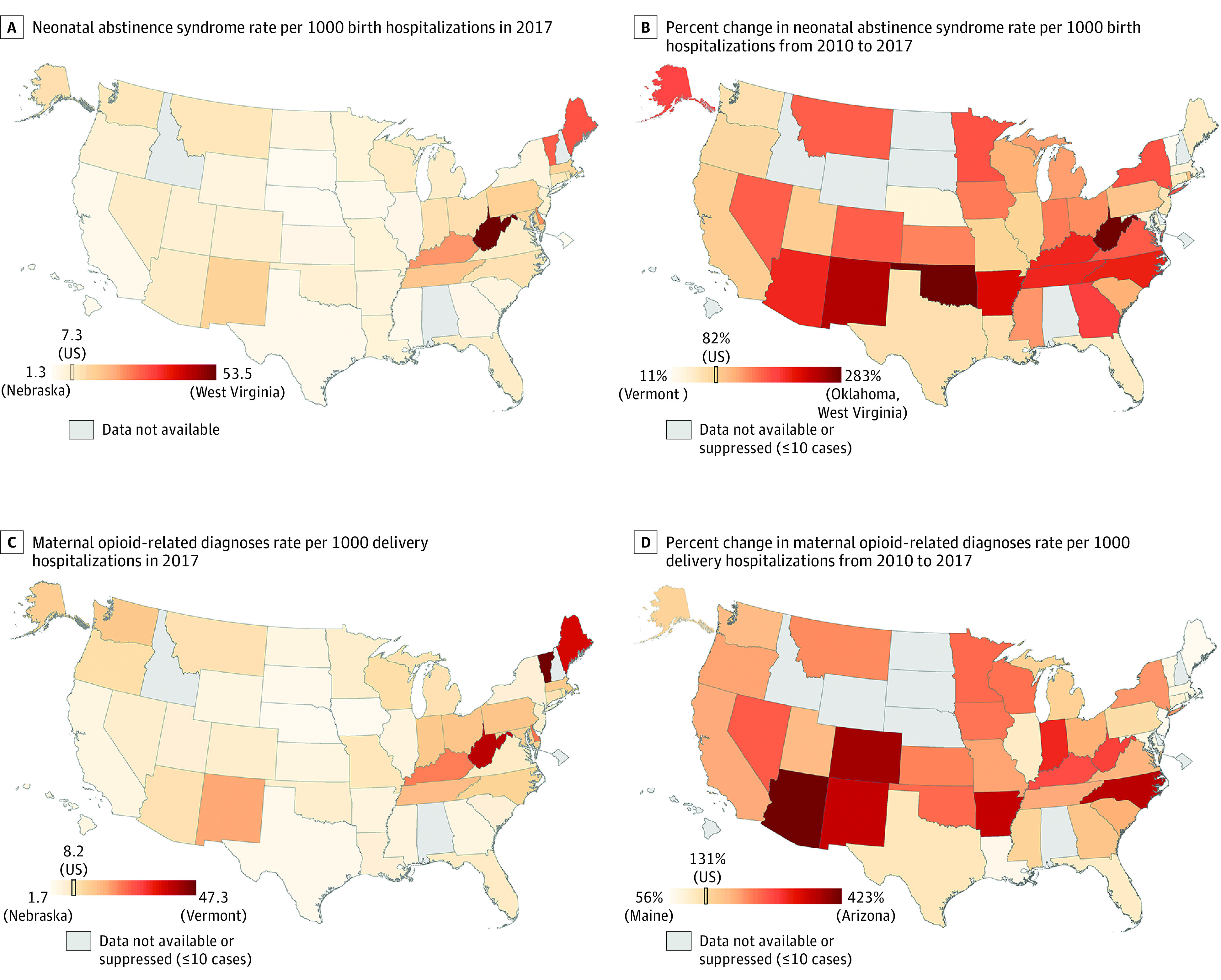
Birth hospitalizations refer to liveborn infant discharge records; delivery hospitalizations refer to maternal discharge records, regardless of pregnancy outcome. Percent change reflects the overall or total percentage change between the 2 end points [(2017 – 2010)/2010 × 100]; The International Classification of Disease, 10th Revision, Clinical Modification, implemented in October 2015, expanded maternal opioid-related diagnoses to include new codes for long-term use of opioid medications and unspecified opioid use in addition to opioid dependence and abuse. Source: Agency for Healthcare Research and Quality, Healthcare Cost and Utilization Project, State Inpatient Databases, 47 States and the District of Columbia (excludes Alabama, Idaho and New Hampshire; Delaware, District of Columbia, and North Dakota did not participate in 2010).
Between 2010 and 2017, NAS rates increased significantly for all 42 states except Nebraska and Vermont and MOD rates increased significantly for all 41 states with data in both years (Figure; eTables 2 and 3 in the Supplement). Relative increases in NAS rates across states ranged from 11% [95% CI, –14% to 36%] in Vermont (from 26.4 to 29.4 per 1000 birth hospitalizations ) to 283% (95% CI, 206%-360%) in Oklahoma (from 1.7 to 6.6 per 1000 birth hospitalizations) and 283% (95% CI, 238%-327%) in West Virginia (from 14.0 to 53.5 per 1000 birth hospitalizations). Relative increases in MOD rates ranged from 56% (95% CI, 36%-76%) in Maine (from 24.2 to 37.8 per 1000 delivery hospitalizations) to 423% (95% CI, 345%-501%) in Arizona (from 1.9 to 9.9 per 1000 delivery hospitalizations).
Discussion
In the US from 2010 to 2017, estimated rates of NAS and MOD significantly increased nationally and for nearly all states and demographic groups. Larger increases in MOD rates than in NAS rates occurred with the transition to ICD-10-CM, which included additional codes for long-term and unspecified opioid use. Definitional differences notwithstanding, this indicates continued increases in both NAS and MOD since 2000.1,2,3 In 2017, the vast majority of individuals with NAS and MOD were non-Hispanic White, Medicaid-billed, and metropolitan residents. However, rural areas6,13 have been disproportionately affected with larger increases and 2017 rates that were approximately twice those for residents of large metropolitan areas.
NAS and MOD rates varied by individual demographics and more so by state of residence. Previous studies reporting state NAS and OUD rates8 excluded at least 18 states, including Delaware, Pennsylvania, and Tennessee, which were among the states with some of the highest NAS and/or MOD rates in 2017. Between 2010 and 2017, 24 states saw increases of 100% or more for both indicators. However, more recent plateaus in heavily affected New England states (Maine, Massachusetts, and Vermont) may suggest some progress in addressing MOD and NAS. NAS case counts for select states with data from 2008 to 2018 also show a plateau into 2017 and decrease in 2018.23 Although this study investigated changes in state rates of MOD and NAS, it did not investigate underlying causes for these changes. Many states have implemented various strategies to address opioid misuse and dependence in the general population24,25 and specifically among pregnant women and infants,26 the effect of which could be investigated in future research.
For diagnoses in hospital discharge records, NAS offers a reliable sentinel indicator with high sensitivity and specificity.27,28,29 No studies could be located that have validated OUD or opioid-related diagnoses from hospital discharge records, either in pregnancy or more generally, but some evidence suggests substantial under-ascertainment. According to the National Survey of Drug Use and Health, 1.4% of pregnant women report past-month opioid misuse (heroin use or prescription pain reliever misuse),30 yet MOD was identified in only 0.8% of delivery hospitalizations in this study. Although development of NAS is dependent on multiple factors,4,5 the nationally estimated MOD rate was similar to the estimated rate of NAS in 2017 and varied across states, with some having considerably higher MOD rates than NAS rates (eg, 47.3 vs 29.4 in Vermont) and vice versa (eg, 40.1 vs 53.5 in West Virginia). State variation in the difference between MOD and NAS rates may reflect state differences in coding and working clinical and surveillance definitions31; screening and treatment efforts specific to pregnant women; various policies, including criminal penalties for substance use in pregnancy26,32,33; and the prevalence of nonopioid substance use that may contribute to NAS, such as barbiturates and benzodiazepines.4,5
Median hospital length of stay and mean costs were greater for those with NAS and MOD relative to overall birth and delivery hospitalizations. Those with NAS had hospital stays that were approximately 9 days longer and $14 600 more in 2017 costs. Although median length of stay did not appear to improve significantly from 2010, care standardization efforts may be too recent to observe effects.4 Although mean hospital costs per case also did not change significantly from 2010 to 2017, the rising caseload has increased overall costs to the health care system, particularly for individuals with Medicaid.2,3,6
Limitations
This study had several limitations. First, hospital discharge data may have limited sensitivity, particularly for MOD, which may not be as reliably identified compared with NAS. NAS may be underestimated by restricting to the birth hospitalization and excluding cases that may have only been identified in a transfer facility or readmission. Linked hospital discharge and birth certificate data from Michigan indicate that the number of NAS cases identified only after birth is approximately equal to the number of cases identified in both birth and subsequent hospitalizations (Chris Fussman, MS, Michigan Department of Health and Human Services, personal communication, September 19, 2019). Thus, the true NAS rate is likely to be in between these birth hospitalization estimates and those from previous analyses including all NAS diagnoses,2,3,13 which have reported rates approximately 25% higher than this study (8.0 vs 6.4 per 1000 in 2014).3 This conservative approach avoids duplication and is consistent with new guidance from the Council of State and Territorial Epidemiologists.34 Second, although the HCUP is the most complete and only all-payer uniform data source available for examining cases of MOD and NAS, it lacks data from 3 states (Alabama, Idaho, and New Hampshire) and does not include federal facilities, such as military, Veterans Affairs, and Indian Health Service hospitals. Third, the cost estimates are conservative because they do not include fees for physician services or transfers. In particular, costs for individuals with MOD only contain hospital charges for delivery and not any substance use disorder treatment costs in either pregnancy or postpartum periods. Fourth, the ICD-10-CM transition complicates the analysis of MOD trends over time with new codes that increased ascertainment of opioid exposure and exaggerated estimated increases. Fifth, greater recognition of opioid use and misuse may have affected diagnostic coding and rate comparisons over time and state. Although this analysis was unable to determine the extent to which state variation was the result of differences in diagnostic coding rather than clinical pathology, observed geographic patterns are similar to other opioid-related complications with different sources, including overdose death.35 Sixth, state-level estimates mask considerable county-level variation,36,37 including counties with high rates in states with lower overall rates, such as Colorado, Montana, and Utah.37 Exploration of county-level variation is important to target preventative efforts. Seventh, although these are the most recent federally available data, they are several years old and may not reflect current NAS and MOD rates.
Conclusions
In the US from 2010 to 2017, estimated rates of NAS and MOD significantly increased nationally and for the majority of states, with notable state-level variation.
eTable 1. Neonatal Abstinence Syndrome, Maternal Opioid-Related Diagnoses, and Birth and Delivery Hospitalization Codes
eFigure 1. Neonatal Abstinence Syndrome and Maternal Opioid-Related Diagnoses Rates per 1,000, 2010-2017
eTable 2. Neonatal Abstinence Syndrome per 1,000 Birth Hospitalizations by State of Residence, 2010-2017
eTable 3. Maternal Opioid-Related Diagnoses per 1,000 Delivery Hospitalizations by State of Residence, 2010-2017
References
- 1.Haight SC, Ko JY, Tong VT, Bohm MK, Callaghan WM. Opioid use disorder documented at delivery hospitalization: United States, 1999-2014. MMWR Morb Mortal Wkly Rep. 2018;67(31):845-849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patrick SW, Schumacher RE, Benneyworth BD, et al. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009. JAMA. 2012;307(18):1934-1940. [DOI] [PubMed] [Google Scholar]
- 3.Winkelman TNA, Villapiano N, Kozhimannil KB, Davis MM, Patrick SW. Incidence and costs of neonatal abstinence syndrome among infants with Medicaid: 2004-2014. Pediatrics. 2018;141(4):e20173520. doi: 10.1542/peds.2017-3520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McQueen K, Murphy-Oikonen J. Neonatal abstinence syndrome. N Engl J Med. 2016;375(25):2468-2479. doi: 10.1056/NEJMra1600879 [DOI] [PubMed] [Google Scholar]
- 5.Kocherlakota P. Neonatal abstinence syndrome. Pediatrics. 2014;134(2):e547-e561. [DOI] [PubMed] [Google Scholar]
- 6.Admon LK, Bart G, Kozhimannil KB, et al. Amphetamine- and opioid-affected births: incidence, outcomes, and costs, United States, 2004-2015. Am J Public Health. 2019;109(1):148-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Maeda A, Bateman BT, Clancy CR, Creanga AA, Leffert LR. Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology. 2014;121(6):1158-1165. [DOI] [PubMed] [Google Scholar]
- 8.Ko JY, Patrick SW, Tong VT, Patel R, Lind JN, Barfield WD. Incidence of neonatal abstinence syndrome: 28 States, 1999-2013. MMWR Morb Mortal Wkly Rep. 2016;65(31):799-802. [DOI] [PubMed] [Google Scholar]
- 9.Heslin KC, Owens PL, Karaca Z, et al. Trends in opioid-related inpatient stays shifted after the us transitioned to ICD-10-CM diagnosis coding in 2015. Med Care. 2017;55(11):918-923. doi: 10.1097/MLR.0000000000000805 [DOI] [PubMed] [Google Scholar]
- 10.Healthcare Cost and Utilization Project Overview of HCUP. Agency for Healthcare Research and Quality. Updated October 1, 2019. Accessed June 30, 2020. https://www.hcup-us.ahrq.gov/overview.jsp
- 11.Healthcare Cost and Utilization Project (HCUP). Overview of the National (Nationwide) Inpatient Sample (NIS). Agency for Healthcare Research and Quality. Accessed October 16, 2020. https://www.hcup-us.ahrq.gov/nisoverview.jsp
- 12.Healthcare Cost and Utilization Project. Overview of the State Inpatient Databases (SID). Agency for Healthcare Research and Quality. Accessed October 16, 2020. https://www.hcup-us.ahrq.gov/sidoverview.jsp
- 13.Villapiano NL, Winkelman TN, Kozhimannil KB, et al. Rural and urban differences in neonatal abstinence syndrome and maternal opioid use, 2004 to 2013. JAMA Pediatr. 2017;171(2):194-196. [DOI] [PubMed] [Google Scholar]
- 14.Diagnostic and Statistical Manual of Mental Disorders.5th ed American Psychiatric Association; 2013. [Google Scholar]
- 15.Condition categories. Chronic Conditions Data Warehouse Accessed June 30, 2020. https://www2.ccwdata.org/web/guest/condition-categories
- 16.Kuklina EV, Whiteman MK, Hillis SD, et al. An enhanced method for identifying obstetric deliveries. Matern Child Health J. 2008;12(4):469-477. doi: 10.1007/s10995-007-0256-6 [DOI] [PubMed] [Google Scholar]
- 17.Healthcare Cost and Utilization Project. Cost-to-Charge Ratio Files. Agency for Healthcare Research and Quality Accessed June 30, 2020. https://hcup-us.ahrq.gov/db/state/costtocharge.jsp
- 18.Bureau of Economic Analysis Table 1.1.4: price indexes for gross domestic product. Accessed June 30, 2020. https://apps.bea.gov/iTable/iTable.cfm?reqid=19&step=2#reqid=19&step=2&isuri=1&1921=survey
- 19.Dunn A, Grosse SD, Zuvekas SH. Adjusting health expenditures for inflation: a review of measures for health services research in the United States. Health Serv Res. 2018;53(1):175-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barrett M, Mummert A, Kenney T, Heslin K. Methods Applying AHRQ Quality Indicators to Healthcare Cost and Utilization Project (HCUP) Data for the 2018 National Healthcare Quality and Disparities Report (QDR). US Agency for Healthcare Research and Quality; 2019. Accessed June 30, 2020. https://www.hcup-us.ahrq.gov/reports/methods/2019-01.pdf
- 21.Urban Influence Codes. US Dept of Agriculture Updated October 24, 2019. Accessed June 30, 2020. https://www.ers.usda.gov/data-products/urban-influence-codes/
- 22.Talih M, Huang DT. Measuring Progress Toward Target Attainment and the Elimination of Health Disparities in Healthy People 2020. National Center for Health Statistics; 2016. [Google Scholar]
- 23.Healthcare Cost and Utilization Project. Neonatal Abstinence Syndrome Births: Trends in the United States, 2008-2019 Agency for Healthcare Research and Quality; 2020. Accessed June 17, 2020. https://hcup-us.ahrq.gov/reports/ataglance/HCUPtrendsNASbirthsUS.pdf
- 24.5-Point strategy to combat the opioid crisis. US Dept of Health and Human Services Accessed March 11, 2020. https://www.hhs.gov/opioids/about-the-epidemic/hhs-response/index.html
- 25.Preventing opioid misuse and overdose in the states and territories. Association of State and Territorial Health Officials Accessed October 16, 2020. https://my.astho.org/opioids/home
- 26.Kroelinger CD, Rice ME, Cox S, et al. State strategies to address opioid use disorder among pregnant and postpartum women and infants prenatally exposed to substances, including infants with neonatal abstinence syndrome. MMWR Morb Mortal Wkly Rep. 2019;68(36):777-783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maalouf FI, Cooper WO, Stratton SM, et al. Positive predictive value of administrative data for neonatal abstinence syndrome. Pediatrics. 2019;143(1):e20174183. doi: 10.1542/peds.2017-4183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goyal S, Saunders KC, Moore CS, et al. Identification of substance-exposed newborns and neonatal abstinence syndrome using ICD-10-CM: 15 hospitals, Massachusetts, 2017. MMWR Morb Mortal Wkly Rep. 2020;69(29):951-955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Elmore AL, Tanner JP, Lowry J, et al. Diagnosis codes and case definitions for neonatal abstinence syndrome. Pediatrics. 2020;146(3):e20200567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Table 6.66B: illicit drug use, marijuana use, and opioid use in past month among females aged 15 to 44, by pregnancy status, demographic, socioeconomic, and pregnancy characteristics: percentages, 2016. and 2017. Substance Abuse and Mental Health Services Administration Accessed June 30, 2020. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHDetailedTabs2017/NSDUHDetailedTabs2017.htm#tab6-66B
- 31.Chiang KV, Okoroh EM, Kasehagen LJ, Garcia-Saavedra LF, Ko JY. Standardization of state definitions for neonatal abstinence syndrome surveillance and the opioid crisis. Am J Public Health. 2019;109(9):1193-1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gressler LE, Shah S, Shaya FT. Association of criminal statutes for opioid use disorder with prevalence and treatment among pregnant women with commercial insurance in the United States. JAMA Netw Open. 2019;2(3):e190338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Substance use during pregnancy. Guttmacher Institute Accessed June 30, 2020. https://www.guttmacher.org/state-policy/explore/substance-use-during-pregnancy
- 34.Neonatal Abstinence Syndrome Standardized Case Definition Council of State and Territorial Epidemiologists ; 2019. Accessed June 30, 2020. https://cdn.ymaws.com/www.cste.org/resource/resmgr/2019ps/final/19-MCH-01_final_7.31.19.pdf
- 35.The drug overdose epidemic: behind the numbers. Centers for Disease Control and Prevention Accessed October 14, 2020. https://www.cdc.gov/drugoverdose/data/index.html
- 36.Patrick SW, Faherty LJ, Dick AW, et al. Association among county-level economic factors, clinician supply, metropolitan or rural location, and neonatal abstinence syndrome. JAMA. 2019;321(4):385-393. doi: 10.1001/jama.2018.20851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Fingar KR, Stocks C, Henke RM, et al. The distribution and correlates of neonatal abstinence syndrome across counties in the United States, 2016. Accessed June 30, 2020.https://academyhealth.confex.com/academyhealth/2019arm/meetingapp.cgi/Paper/33577
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Neonatal Abstinence Syndrome, Maternal Opioid-Related Diagnoses, and Birth and Delivery Hospitalization Codes
eFigure 1. Neonatal Abstinence Syndrome and Maternal Opioid-Related Diagnoses Rates per 1,000, 2010-2017
eTable 2. Neonatal Abstinence Syndrome per 1,000 Birth Hospitalizations by State of Residence, 2010-2017
eTable 3. Maternal Opioid-Related Diagnoses per 1,000 Delivery Hospitalizations by State of Residence, 2010-2017


