Summary
Background
The association of air pollution with multiple adverse health outcomes is becoming well established, but its negative economic impact is less well appreciated. It is important to elucidate this impact for the states of India.
Methods
We estimated exposure to ambient particulate matter pollution, household air pollution, and ambient ozone pollution, and their attributable deaths and disability-adjusted life-years in every state of India as part of the Global Burden of Disease Study (GBD) 2019. We estimated the economic impact of air pollution as the cost of lost output due to premature deaths and morbidity attributable to air pollution for every state of India, using the cost-of-illness method.
Findings
1·67 million (95% uncertainty interval 1·42–1·92) deaths were attributable to air pollution in India in 2019, accounting for 17·8% (15·8–19·5) of the total deaths in the country. The majority of these deaths were from ambient particulate matter pollution (0·98 million [0·77–1·19]) and household air pollution (0·61 million [0·39–0·86]). The death rate due to household air pollution decreased by 64·2% (52·2–74·2) from 1990 to 2019, while that due to ambient particulate matter pollution increased by 115·3% (28·3–344·4) and that due to ambient ozone pollution increased by 139·2% (96·5–195·8). Lost output from premature deaths and morbidity attributable to air pollution accounted for economic losses of US$28·8 billion (21·4–37·4) and $8·0 billion (5·9–10·3), respectively, in India in 2019. This total loss of $36·8 billion (27·4–47·7) was 1·36% of India's gross domestic product (GDP). The economic loss as a proportion of the state GDP varied 3·2 times between the states, ranging from 0·67% (0·47–0·91) to 2·15% (1·60–2·77), and was highest in the low per-capita GDP states of Uttar Pradesh, Bihar, Rajasthan, Madhya Pradesh, and Chhattisgarh. Delhi had the highest per-capita economic loss due to air pollution, followed by Haryana in 2019, with 5·4 times variation across all states.
Interpretation
The high burden of death and disease due to air pollution and its associated substantial adverse economic impact from loss of output could impede India's aspiration to be a $5 trillion economy by 2024. Successful reduction of air pollution in India through state-specific strategies would lead to substantial benefits for both the health of the population and the economy.
Funding
UN Environment Programme; Bill & Melinda Gates Foundation; and Indian Council of Medical Research, Department of Health Research, Ministry of Health and Family Welfare, Government of India.
Introduction
Air pollution is a major cause of premature death and disease, and is the largest environmental health threat globally.1, 2, 3, 4, 5 Besides endangering health and shortening lifespan, air pollution adversely affects economic productivity.6, 7 The Sustainable Development Goals (SDGs) call for reduction of the burden of deaths and diseases from air pollution.8
Air pollution risks are typically quantified for ambient particulate matter pollution, household air pollution, and, to a smaller extent, tropospheric ozone. The main sources of ambient particulate matter pollution in India are residential and commercial biomass burning, windblown mineral dust, coal burning for energy generation, industrial emissions, agricultural stubble burning, waste burning, construction activities, brick kilns, transport vehicles, and diesel generators.9, 10, 11, 12, 13, 14, 15, 16 Household air pollution is caused mainly by the use of solid fuels for cooking, such as wood, dung, agricultural residues, coal, and charcoal.17, 18, 19 Ground-level ambient ozone is produced when pollutants emitted from transport vehicles, power plants, factories, and other sources react in the presence of sunlight with hydrocarbons emitted from diverse sources.20
Evidence of the adverse effects of air pollution on health has been growing in India.21 Studies from India have shown that short-term and long-term exposure are associated with disease burden and mortality.22, 23, 24, 25 The India State-Level Disease Burden Initiative has reported detailed findings on exposure to air pollution and its impacts on deaths, disease burden, and life expectancy in the states of India as part of the Global Burden of Disease Study (GBD) 2017.21 Improved methods and new data used in GBD 2019 have led to revised estimates of the impact of air pollution on deaths and disease burden.26 In this Article, we present these updated estimates for India and its states.
Research in context.
Evidence before the study
Existing evidence suggests that air pollution not only affects health but also has consequences for the economy. We searched PubMed for published literature on the health and economic impacts of air pollution in India, Google for reports in the public domain, and references in these papers and reports, using the search terms “air pollutants”, “air pollution”, “ambient ozone pollution”, “ambient particulate matter pollution”, “burden”, “cost-of-illness”, “DALY”, “death”, “economic impact”, “household air pollution”, “India”, “indoor pollution”, “morbidity”, “mortality”, and “PM2·5 exposure”, on June 12, 2020. There are many publications on the health impacts of air pollution and some studies have assessed the economic burden of air pollution in India, but there are no studies that have assessed the economic impacts of the different components of air pollution in each state of India.
Added value of this study
This study provides the updated estimates of deaths and morbidity attributable to air pollution in every state of India in 2019 based on the improved GBD 2019 methods, which reveal that this burden is higher than was previously estimated. It estimates the economic loss due to lost output from premature death and morbidity attributable to different components of air pollution at the state level based on the updated estimates of deaths and morbidity attributable to air pollution. The findings in this paper highlight that the disease burden attributable to air pollution and its economic impact are high in India, with substantial variations across the states. The wide variations in economic loss attributable to ambient particulate matter pollution, household air pollution, and ambient ozone pollution across the states of India, both in absolute terms and as a percentage of gross domestic product, can be useful for the planning and implementation of targeted interventions at the state level.
Implications of all the available evidence
The high burden of air pollution in India and its substantial adverse impact on output could impede India's overall economic development and social wellbeing unless they are addressed as a priority. The variations in these impacts between states indicate that investments in state-specific air pollution control strategies are needed to reduce the significant adverse health and economic impact of air pollution across India.
Diseases attributable to air pollution adversely affect economic growth through reduced productivity and decreased labour supply, and via health-care expenditures and lost welfare.3, 27, 28 In the public health literature, the cost-of-illness method is the main approach used to estimate the economic burden of disease outcomes, including diseases attributable to air pollution.29, 30, 31, 32, 33, 34 The cost-of-illness method includes estimation of direct costs of health care as well as indirect costs, measured as the loss of output due to premature mortality and morbidity.35 The output-based approach to estimating indirect cost equates the economic cost of premature mortality to the present value of lost income, and values morbidity by lost output.33, 34 We use this output-based approach to estimate the economic cost of premature deaths and morbidity attributable to air pollution in each state of India using the GBD 2019 air pollution estimates.
Methods
Overview
The India State-Level Disease Burden Initiative estimates disease burden for the states of India as part of GBD. The work of this initiative is approved by the Health Ministry Screening Committee at the Indian Council of Medical Research and the ethics committee of the Public Health Foundation of India. The analysis of the economic impact of air pollution-related diseases and deaths was done on the basis of an invitation extended to the UN Environment Programme by the Indian Ministry of Environment, Forest and Climate Change.
Estimation of exposure, deaths, and DALYs attributable to air pollution
A detailed description of the GBD methods for estimating deaths and disability-adjusted life-years (DALYs) attributable to air pollution is reported elsewhere,21, 26 and provided in the appendix (pp 3–14). DALY is a composite metric that combines the years of life lost due to premature death (YLLs) and the years lived with disability (YLDs).
Ambient particulate matter pollution was estimated as exposure to fine particulate matter with an aerodynamic diameter of 2·5 μm or less (PM2·5) in a cubic meter of air (μg/m3).21, 26 We used PM2·5 as the indicator of ambient particulate matter pollution because it has the strongest association with disease burden and mortality.36 Exposure to PM2·5 was estimated with use of aerosol optical depth data from multiple satellite sources combined with a chemical transport model and calibration with data from ground-level monitoring station locations in India. Household air pollution was estimated from data on the proportion of individuals using various types of solid fuels for cooking from a number of nationwide surveys. Exposure to solid fuels was converted to PM2·5 exposure on the basis of data from a global measurement database including several studies conducted in India.
Ozone exposure was defined as the highest seasonal average 8 h daily maximum concentration, in parts per billion (ppb), with season defined as the 6-month period with the highest mean ozone concentrations. To estimate exposure to ozone in ambient air, ozone ground measurement data from various locations in India were combined with chemical transport models.
Estimates of PM2·5 exposure from ambient particulate matter and household air pollution and ambient ozone pollution exposure were used to estimate the attributable burden from various diseases using the standardised GBD comparative risk assessment framework, which uses worldwide literature on the association of each risk factor with particular diseases, as described previously.26 We estimated deaths and DALYs attributable to air pollution as a whole and attributable independently to ambient particulate matter, household air pollution, and ambient ozone pollution.
GBD 2019 included a number of methodological updates and new input data for estimation of deaths and DALYs attributable to air pollution, as described elsewhere.26 These updates included the addition of burden attributable to ambient particulate air pollution and household air pollution that is mediated by low birthweight and short gestation, along with the previously included attributable burden from chronic obstructive pulmonary disease (COPD), lower respiratory infections, lung cancer, ischaemic heart disease, stroke, type 2 diabetes, and cataract. Another update was the addition of recent studies on air pollution and a new approach to the development of risk curves that enabled exclusion of active smoking studies, which removed an important source of uncertainty related to the differences in exposure between active smoking and air pollution PM2·5 sources. A further update was the generation of risk curves for every 5-year age group from 25 years onward for ischaemic heart disease and stroke, which allowed more robust estimates. A detailed description of methodological changes in GBD 2019 and the improvement in estimates from GBD 2017 is available in appendix (pp 3–14) and has been published previously.26
We estimated deaths, DALYs, YLLs, and YLDs attributable to air pollution, ambient particulate matter pollution, household air pollution, and ambient ozone pollution for 31 geographical units in India: the 28 states; the union territory of Delhi, the two union territories of Jammu & Kashmir and Ladakh combined, and the other small union territories combined (Andaman and Nicobar Islands, Chandigarh, Dadra and Nagar Haveli, Daman and Diu, Lakshadweep, and Puducherry). We examined the trends in death rates attributable to each of the three components of air pollution from 1990 to 2019. We assessed the Pearson correlation coefficient between the crude DALY rates attributable to each of the three components of air pollution and the per capita gross domestic product (GDP) of the states in 2018–19.37 We estimated DALYs and deaths attributable to air pollution in India in 2019 from various diseases.
Estimation of economic loss attributable to air pollution
We estimated the economic cost of premature mortality by the present discounted value of output lost when a person died in 2019 of pollution-related diseases. The cost of morbidity was estimated as the output lost when a person had pollution-related YLDs in 2019. Both required estimates of output per worker.
The output per worker in a given state in 2019 was calculated as the labour share of GDP multiplied by GDP in 2018–19,37 divided by the number of people who were employed. The labour share of GDP in each state was estimated using data from the Penn World Tables 21.38 Workers of all ages in a state were assumed to produce the same output per worker. Because not all people of a given age were working, output per worker was adjusted by the fraction of people in each age group who were working. This information was obtained from the National Sample Survey on employment and unemployment for 2011–12.39 To predict output in future years, output per worker was assumed to grow at the historical real rate of growth of output per worker, estimated using data from the KLEMS database.40 For people not working, expected output per worker in each year was assumed to be equal to 30% of market output to allow for non-market production.41
To quantify the output losses in future years if a person of a given age dies in the current year requires estimating the present discounted value of their future output. An individual's output at each age is the product of output per worker (as described above) and the probability that a person is working at each age, measured as the ratio of the working population to the total population at that age. This estimate of lost output must be adjusted to reflect the probability a person survives to each future age. Survival probabilities were estimated using state-specific life tables from GBD 2019. Expected future output at each age was discounted to the present at a rate of interest of 6%, taken to be the yield on 10-year Indian Government bonds in late 2020. A sensitivity analysis was done to examine the impact of using different discount rates between 4% and 8% on the estimate of economic loss.
The total output lost through premature mortality attributable to air pollution was estimated as the present discounted value of lost market and non-market output for a person who dies in 2019 at each age multiplied by the number of deaths due to air pollution in 2019 for that age, with the result summed over all ages. The present value of lost output per person over the remainder of the person's working life is a conservative estimate of the loss in output that is a consequence of premature death.
To estimate the total output losses attributable to air pollution-related morbidity, the expected market and non-market output loss per person in 2019, by age group, was multiplied by the YLDs attributable to air pollution in 2019 for each age group and the result summed over all ages.21 Details of these methods are presented in the appendix (pp 15–17). We report the output losses in monetary terms and as a percentage of GDP for deaths and YLDs attributable to air pollution, and separately for ambient particulate matter pollution, household air pollution, and ambient ozone pollution, for every state of India in 2019 and for India overall by aggregating the state estimates.
Role of the funding source
Some of the contributors to this study work with the Indian Council of Medical Research and the UN Environment Programme. The other funder, the Bill & Melinda Gates Foundation, had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication. All authors had access to the estimates presented in the paper.
Results
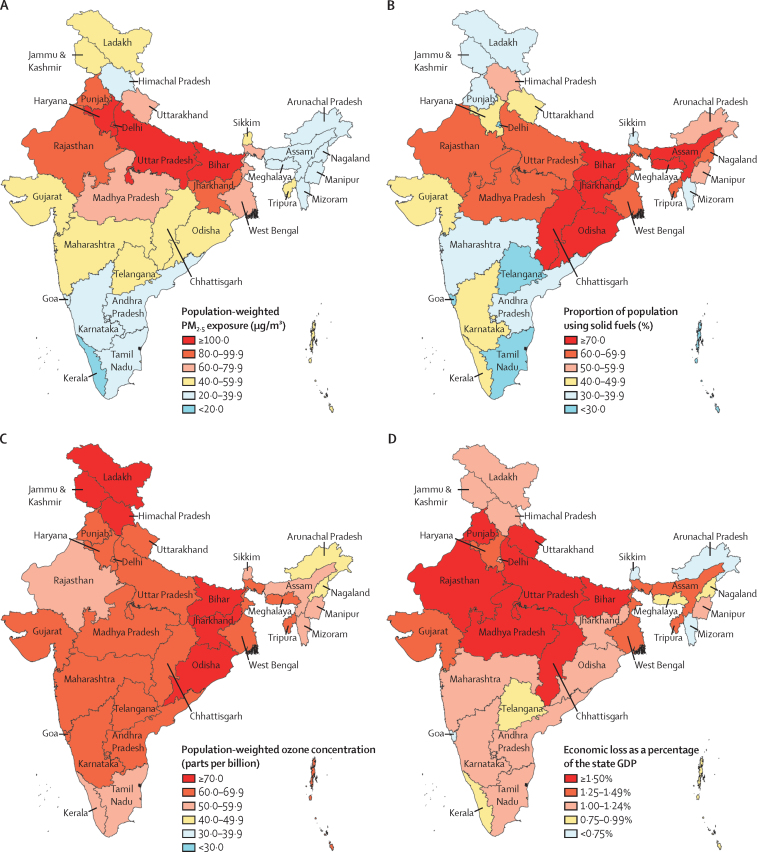
The annual average population-weighted mean PM2·5 concentration (as a measure of ambient particulate matter exposure) was 91·7 μg/m3 (95% uncertainty interval [UI] 69·6–113·9) in India in 2019. Across the states of India, exposure to ambient particulate matter ranged from 15·8 μg/m3 (13·0–18·7), in Kerala, to 217·6 μg/m3 (117·9–297·3), in Delhi—a 13·8 times difference. Higher concentrations were found in the northern states, including the four states with the highest exposures (123·5–217·6 μg/m3; figure 1A; appendix p 18). The proportion of the population using solid fuels for cooking in India in 2019 was 56·3% (55·1–57·4). This proportion was highest in the eastern and northern states, with proportion above 70% in six states (figure 1B; appendix p 18). Use of solid fuels contributed an average 82·8 μg/m3 PM2·5 (41·9–153·8) in households, in addition to the ambient 91·7 μg/m3 PM2·5 present in India in 2019 (appendix p 18). The average ambient ozone concentration in India in 2019 was 66·2 ppb (66·0–66·3), ranging from 47·4 ppb (46·3–48·5), in Arunachal Pradesh, to 76·6 ppb (75·8–77·4), in Jammu & Kashmir and Ladakh (figure 1C; appendix p 18).
Figure 1.
Exposure to air pollution and economic loss due to premature deaths and morbidity attributable to air pollution in the states of India, 2019
(A) Population-weighted mean ambient PM2·5 concentration. (B) Proportion of population using solid fuels. (C) Population-weighted ozone concentration in parts per billion. (D) Economic loss due to premature deaths and morbidity attributable to air pollution as a percentage of the state GDP. GDP=gross domestic product. PM2·5=fine particulate matter with an aerodynamic diameter of 2·5 μm or less.
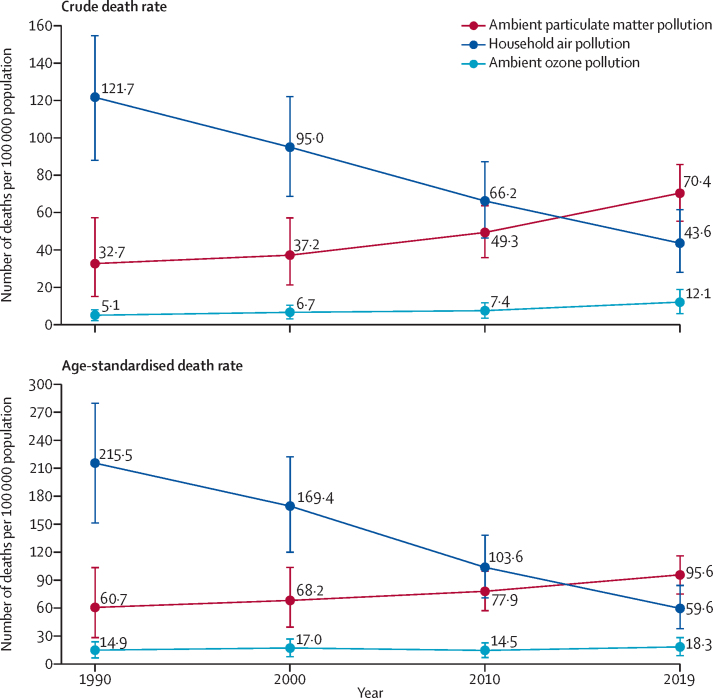
In 2019, 1·67 million (95% UI 1·42–1·92) deaths in India were attributable to air pollution, accounting for 17·8% (15·8–19·5) of the total deaths in India (table 1).42 0·98 million (0·77–1·19) deaths were attributable to ambient particulate matter pollution, 0·61 million (0·39–0·86) to household air pollution, and 0·17 million (0·08–0·26) to ambient ozone pollution (table 1). The crude death rate per 100 000 population due to household air pollution decreased in India by 64·2% (52·2–74·2) from 1990 to 2019, while that due to ambient particulate matter pollution increased by 115·3% (28·3–344·4) and that due to ambient ozone pollution increased by 139·2% (96·5–195·8; figure 2; appendix p 19). The age-standardised death rate due to household air pollution decreased by 72·3% (63·6–79·8) from 1990 to 2019 and that due to ambient ozone pollution increased by 23·2% (0·5–52·0), while the 95% UI of the estimated 57·4% increase in death rate due to ambient particulate matter pollution overlapped with zero (–4·4 to 225·3; figure 2).
Table 1.
Deaths and DALYs attributable to air pollution in India in 2019
| Number of deaths, millions* | Percentage of total deaths† | Number of DALYs, millions* | Percentage of total DALYs† | |
|---|---|---|---|---|
| Air pollution | 1·67 (1·42–1·92) | 17·8% (15·8–19·5) | 53·5 (46·6–60·9) | 11·5% (10·2–12·8) |
| Ambient particulate matter pollution | 0·98 (0·77–1·19) | 10·4% (8·4–12·3) | 31·1 (24·6–37·5) | 6·7% (5·3–8·0) |
| Household air pollution | 0·61 (0·39–0·86) | 6·5% (4·3–9·0) | 20·9 (14·1–28·7) | 4·5% (3·0–6·1) |
| Ambient ozone pollution | 0·17 (0·08–0·26) | 1·8% (0·9–2·7) | 3·06 (1·51–4·83) | 0·7% (0·3–1·0) |
Data are point estimate (95% UI). DALYs=disability-adjusted life-years.
The sums of deaths and DALYs attributable to each component of air pollution are more than the estimates for overall air pollution because the population attributable fractions from component risk factors can add up to more than the population attributable fraction for the parent risk factor, even if the components are independent.
In 2019, 9·39 million total deaths and 467·8 million total DALYs were estimated for India.42
Figure 2.
Death rate attributable to ambient particulate matter pollution, household air pollution, and ambient ozone pollution per 100 000 population in India, 1990–2019
11·5% of the total DALYs in India in 2019 were attributable to air pollution,42 the majority of which were due to ambient particulate matter pollution (6·7% [5·3–8·0]) and household air pollution (4·5% [3·0–6·1]; table 1). The crude DALY rate attributable to ambient particulate matter pollution varied 5·5 times across the states in 2019, with several northern states having the highest rates (appendix p 20). The crude DALY rate attributable to household air pollution varied 132·3 times, with the highest rates in the northern and northeastern states (appendix p 20). The crude DALY rate attributable to ambient ozone pollution varied 11·2 times across the states in 2019, with a mixed pattern with regard to geographical location (appendix p 20). The crude DALY rate attributable to household air pollution had a significant inverse correlation with the per-capita GDP of the states (r=–0·71, r2=0·50; p<0·0001), but there was no significant correlation between the per-capita GDP of the states and the crude DALY rate attributable to ambient particulate matter pollution (r=0·25, r2=0·06, p=0·17) or ambient ozone pollution (r=–0·11, r2=0·01, p=0·56).
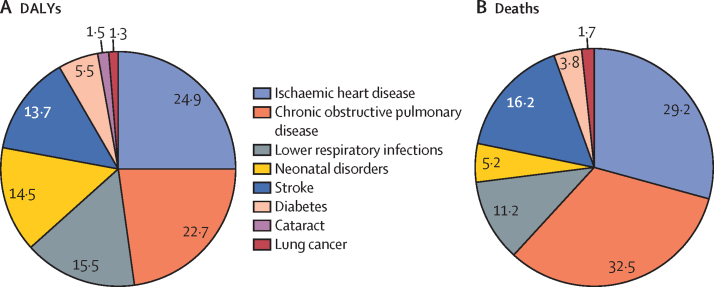
Of the total DALYs attributable to air pollution in India in 2019, 39·5% were from lung diseases, which included COPD (22·7%), lower respiratory infections (15·5%), and lung cancer (1·3%; figure 3A). The remaining DALYs were from ischaemic heart disease (24·9%), stroke (13·7%), diabetes (5·5%), neonatal disorders (14·5%), and cataract (1·5%). Of the total deaths attributable to air pollution in India in 2019, the largest proportions were due to COPD (32·5%) and ischaemic heart disease (29·2%), followed by stroke (16·2%) and lower respiratory infections (11·2%; figure 3B).
Figure 3.
Causes of DALYs (A) and deaths (B) attributable to air pollution in India, 2019
Individual causes are shown as a percentage of total DALYs or deaths. DALYs=disability-adjusted life-years.
The economic loss due to lost output from premature deaths attributable to air pollution in India in 2019 was US$28·8 billion (95% UI 21·4–37·4), and from morbidity attributable to air pollution was $8·0 billion (5·9–10·3; table 2; appendix p 21). Of the total economic loss of $36·8 billion (27·4–47·7) attributable to air pollution in India in 2019, 36·6% was from lung diseases, which included COPD (21·1%), lower respiratory infections (14·2%), and lung cancer (1·2%), and the rest was from ischaemic heart disease (24·9%), stroke (14·1%), diabetes (8·4%), neonatal disorders (13·3%), and cataract (2·7%).
Table 2.
Total and per-capita economic loss due to premature deaths and morbidity attributable to air pollution in the states of India, 2019
| Premature deaths, US$ millions | Morbidity, US$ millions | Total, US$ millions | Per capita, US$ | |
|---|---|---|---|---|
| India | 28 799 (21 429–37 421) | 8005 (5940–10 289) | 36 804 (27 369–47 710) | 26·5 (19·7–34·3) |
| Bihar | 1257 (931–1646) | 296 (223–376) | 1553 (1153–2022) | 12·7 (9·4–16·6) |
| Uttar Pradesh | 4255 (3153–5508) | 876 (663–1108) | 5130 (3816–6616) | 21·1 (15·7–27·2) |
| Manipur | 30 (21–41) | 11 (8–14) | 40 (29–55) | 11·5 (8·2–15·6) |
| Jharkhand | 408 (297–542) | 136 (101–173) | 543 (398–715) | 14·3 (10·5–18·9) |
| Madhya Pradesh | 1614 (1212–2090) | 356 (268–452) | 1970 (1480–2542) | 22·2 (16·7–28·7) |
| Assam | 528 (389–698) | 129 (95–167) | 657 (483–865) | 18·2 (13·4–24·0) |
| Meghalaya | 30 (20–43) | 9 (7–12) | 39 (27–55) | 11·5 (7·9–16·0) |
| Jammu & Kashmir and Ladakh | 201 (150–261) | 51 (38–66) | 252 (188–327) | 18·0 (13·4–23·3) |
| Chhattisgarh | 549 (409–712) | 141 (103–182) | 690 (512–894) | 21·8 (16·1–28·2) |
| West Bengal | 1607 (1233–2018) | 519 (389–659) | 2125 (1623–2677) | 21·3 (16·3–26·9) |
| Nagaland | 26 (17–37) | 8 (6–10) | 34 (23–47) | 17·2 (11·8–24·0) |
| Odisha | 609 (430–831) | 197 (144–257) | 807 (574–1088) | 17·3 (12·3–23·3) |
| Rajasthan | 1902 (1376–2504) | 392 (298–492) | 2294 (1674–2996) | 28·5 (20·8–37·3) |
| Tripura | 70 (50–94) | 21 (16–27) | 91 (66–121) | 22·6 (16·4–30·1) |
| Arunachal Pradesh | 19 (13–28) | 7 (5–9) | 26 (18–37) | 15·1 (10·2–21·2) |
| Mizoram | 17 (11–24) | 6 (4–7) | 22 (15–31) | 17·6 (12·0–24·5) |
| Andhra Pradesh | 1007 (717–1373) | 342 (252–445) | 1349 (969–1818) | 24·9 (17·9–33·5) |
| Punjab | 920 (695–1176) | 229 (167–298) | 1149 (862–1474) | 37·0 (27·7–47·4) |
| Tamil Nadu | 1886 (1397–2457) | 643 (460–853) | 2529 (1857–3310) | 31·7 (23·3–41·5) |
| Maharashtra | 3003 (2279–3835) | 972 (725–1245) | 3975 (3004–5080) | 31·9 (24·1–40·7) |
| Telangana | 841 (591–1153) | 275 (202–356) | 1116 (793–1508) | 28·7 (20·4–38·7) |
| Kerala | 741 (555–962) | 349 (253–458) | 1091 (808–1421) | 31·2 (23·1–40·6) |
| Himachal Pradesh | 192 (142–251) | 62 (46–80) | 254 (188–331) | 33·3 (24·7–43·5) |
| Karnataka | 2113 (1593–2718) | 568 (413–741) | 2681 (2006–3459) | 39·4 (29·5–50·9) |
| Uttarakhand | 413 (309–537) | 114 (84–146) | 527 (393–683) | 44·5 (33·2–57·7) |
| Gujarat | 2288 (1728–2938) | 571 (429–729) | 2860 (2158–3667) | 41·3 (31·2–53·0) |
| Haryana | 1224 (929–1575) | 342 (259–434) | 1566 (1188–2009) | 53·8 (40·8–69·0) |
| Other small union territories | 86 (60–118) | 35 (25–46) | 120 (85–164) | 31·7 (22·5–43·2) |
| Sikkim | 17 (12–24) | 8 (6–11) | 25 (18–35) | 38·6 (27·3–52·5) |
| Delhi | 893 (672–1153) | 314 (235–402) | 1207 (906–1555) | 62·0 (46·6–79·9) |
| Goa | 54 (37–75) | 26 (19–35) | 80 (56–110) | 52·2 (36·3–71·9) |
The states are listed in increasing order of per-capita gross domestic product in 2018–19.
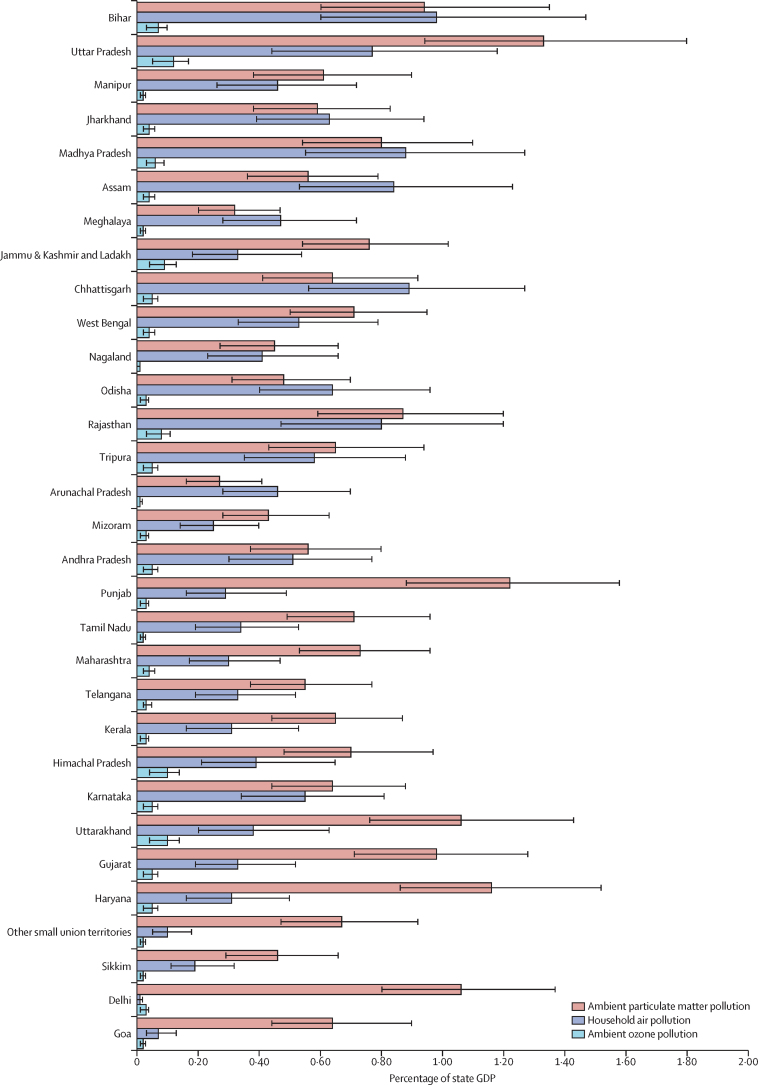
The economic loss due to lost output from premature deaths and morbidity attributable to air pollution was 1·36% (95% UI 1·01–1·76) of India's GDP in 2019 (appendix p 22). A sensitivity analysis showed that, with a discount rate of 4% instead of 6%, the economic loss would be 1·86% of the GDP, and with a discount rate of 8% it would be 1·10% of the GDP (appendix p 15). The economic loss attributable to air pollution as a percentage of state GDP varied from 0·67% (0·47–0·91) to 2·15% (1·60–2·77)—a 3·2 times difference—across the states, and was highest in the states of Uttar Pradesh (2·15%), Bihar (1·95%), Madhya Pradesh (1·70%), Rajasthan (1·70%), and Chhattisgarh (1·55%), which have a relatively low per-capita GDP, and in Punjab (1·52%) and Uttarakhand (1·50%) which have relatively high per-capita GDP (figure 1D; appendix p 22). The per-capita economic loss due to air pollution in India was $26·5 (19·7–34·3), and varied 5·4 times across the states; this economic loss per capita was highest in Delhi ($62·0 [46·6–79·9]) and Haryana ($53·8 [40·8–69·0]) and was generally higher in the states with high per-capita GDP (table 2).
The economic loss due to lost output from premature deaths and morbidity attributable to ambient particulate matter pollution as a percentage of GDP in India was 0·84% (0·59–1·13) in 2019 (appendix p 22). This proportion varied 4·9 times across the states (from 0·27% [0·16–0·41] to 1·34% [0·94–1·80]) and was highest in Uttar Pradesh (1·34%) which has a relatively low per-capita GDP, followed by Punjab (1·22%), Haryana (1·16%), Uttarakhand (1·06%), and Delhi (1·06%), which have a relatively high per-capita GDP (figure 4; appendix p 22).
Figure 4.
Economic loss due to premature deaths and morbidity attributable to ambient particulate matter pollution, household air pollution, and ambient ozone pollution as a percentage of state GDP in India, 2019
States are listed in increasing order of per-capita GDP in 2018–19. Error bars represent 95% uncertainty intervals. GDP=gross domestic product.
The economic loss due to lost output from premature deaths and morbidity attributable to household air pollution as a percentage of state GDP in India was 0·49% (0·29–0·75) in 2019, with 110·3 times variation (from 0·01% [0·00–0·02] to 0·98% [0·60–1·47]) across the states (figure 4; appendix p 22). This proportion was highest in Bihar (0·98%), Chhattisgarh (0·89%), Madhya Pradesh (0·88%), Assam (0·84%), Rajasthan (0·79%), and Uttar Pradesh (0·77%), which have a relatively low per-capita GDP.
In 2019, the economic loss due to lost output from premature deaths attributable to ambient ozone pollution as a percentage of GDP in India was 0·05% (0·02–0·09) and varied 11·2 times across the states, ranging from 0·01% (0·00–0·02) in Nagaland to 0·12% (0·05–0·20) in Uttar Pradesh (figure 4; appendix p 22).
The economic loss due to lost output from premature deaths and morbidity attributable to ambient particulate matter pollution ranged from $9·5 million in the small northeastern state of Arunachal Pradesh to $3188·4 million in the northern state of Uttar Pradesh, and that attributable to household air pollution ranged from $7·6 million in the small western state of Goa to $1829·6 million in Uttar Pradesh (appendix p 21). The economic loss due to lost output from premature deaths attributable to ambient ozone pollution ranged from $0·4 million in the small northeastern state of Nagaland to $286·2 million in Uttar Pradesh (appendix p 21).
Discussion
Important revisions in the GBD 2019 methods have led to more robust estimates of deaths and DALYs attributable to air pollution compared with the previous GBD estimates. The main contributors to the higher estimates in GBD 2019 are the inclusion of disease burden attributable to air pollution mediated by low birthweight and short gestation, and updated relative risk curves, particularly for stroke, with the availability of recent evidence, including from India.26, 43, 44, 45 These method updates resulted in an increased estimate of the burden attributable to air pollution in India, which accounted for an estimated 1·67 million deaths in India in 2019. For comparison with the estimate of 1·24 million (1·09–1·39) air pollution attributable deaths in India in 2017 in GBD 2017,21 the 2017 estimate for India in GBD 2019 is 1·60 million (1·41–1·80) deaths.
The burden of household air pollution decreased substantially in India between 1990 and 2019; however, the burden attributable to ambient particulate matter pollution and ambient ozone pollution increased during this period. In 2019, the less developed states in north and northeastern India had a higher burden from household air pollution than the more developed states, whereas states in northern India had a high burden of ambient particulate matter pollution irrespective of whether they were less or more developed.
The economic loss due to lost output from premature deaths and morbidity attributable to air pollution is high in India, equivalent to 1·36% of India's GDP in 2019. A further source of economic loss is the health-care cost of treating diseases attributable to air pollution. Based on National Health Accounts data,46 we estimated the total health-care cost in India in 2019 to be $103·7 billion. With air pollution responsible for 11·5% of the disease burden (measured as DALYs) in India in 2019, a crude estimate of the health-care cost for air pollution-related diseases would be $11·9 billion (or 0·44% of India's GDP).
In 2019, there was a three-fold variation between the states with regard to the economic loss due to lost output from premature deaths and morbidity attributable to air pollution as a percentage of state GDP, and a five-fold variation in absolute per-capita economic loss, with a relatively higher burden in the northern states compared with the other states of India. The economic loss due to premature mortality and morbidity is a disinvestment in human capital stock.33 Human capital is a broad concept, defined as the stock of knowledge and skills possessed by a population and the health status of that population, which is an important component of the inclusive wealth of a nation.47, 48, 49
The increasing death rate attributable to ambient particulate matter pollution reflects increasing pollutant emissions from rising energy consumption, accelerated urbanisation, rapid industrialisation, and growing numbers of petroleum-powered vehicles.50 Evidence suggests that climate change can amplify the adverse impacts of air pollution through atmospheric stagnation, temperature-driven increases in PM2·5 concentration, and ground-level ozone formation, which are likely to be particularly severe in India.51, 52 The economic burden due to lost productivity will increase in magnitude in the years ahead if air pollution continues to worsen. If air pollution is not aggressively controlled and managed, its great costs could not only undermine plans to increase India's economy to $5·0 trillion by 2024, but would also impede the growth in inclusive wealth of the nation through reduced human capital stock.
The total health expenditure in India is 3·8% of GDP,46 while the economic loss due to lost output from premature deaths and morbidity attributable to air pollution estimated in this study was 1·36% of GDP, indicating that the total economic impact of air pollution is high. The loss of output in monetary terms attributable to air pollution at the state level is associated with the number and the age-distribution of deaths and morbidity in each state and state GDP per worker. The economic loss due to air pollution as a percentage of state GDP was highest in northern states of India because people in these states are exposed to very high concentrations of ambient PM2·5 and a high proportion of their population uses solid fuels. The states of Uttar Pradesh and Bihar, with the highest economic loss as a percentage of their GDP, had the lowest per-capita GDP among the states of India, indicating that these poor states are most vulnerable to the adverse economic impacts of air pollution.
Several studies have evaluated the economic impacts of premature mortality and morbidity attributable to air pollution, in India and globally, using various approaches. A study using the output-based approach and GBD 2013 mortality data estimated the total forgone labour output due to air pollution in India in 2013 to be 0·84% of GDP.33 This estimate is lower than our estimate of 1·36% of GDP because the former provided estimates for output lost due to premature mortality only and was based on earlier estimates of PM2·5 mortality. This study also estimated the loss of economic welfare due to premature mortality attributable to air pollution, using the willingness-to-pay approach, to be 7·7% of GDP in India in 2013.33 The estimated loss of economic welfare is much higher than the estimates of productivity loss alone because what people are willing to pay to reduce their risk of death from a risk factor or disease is generally always higher than the present value of lost output.3 Moreover, the willingness-to-pay approach values all premature mortality attributable to air pollution, whereas the output-based approach considers premature mortality only in working-age groups.3 The willingness-to-pay approach is also sensitive to the assumptions associated with the estimation of the value per statistical life, which has wide variations in the studies reported from India.53
In other countries, the human capital-augmented production function framework for estimating the macroeconomic cost of air pollution in China resulted in an annual economic loss accounting for 0·5% of GDP.54 Other studies used a damage function approach and estimated the morbidity and mortality effects of particulate matter pollution on the population as 3·4% of GDP in 1999 in Singapore32 and 1% of GDP in Jakarta during the same period.55 These variations in the magnitude of economic burden attributable to air pollution across different studies in India and other countries are likely to be due to geographical differences in the patterns of premature deaths and morbidity, as well as differences in labour force dynamics, types of data used, and methodological approaches.
Studies on sources of emission in major cities of India have identified a number of important contributing sources, although there is variation over space and time, and uncertainty in their contributions because of the use of different methods and underlying uncertainty in source signatures and emission inventories.11, 12, 13, 14, 16, 56 These studies have highlighted the contributions of industrial sources, energy production, and especially residential emissions from the use of polluting fuels for cooking and heating. In urban areas, contributions from transportation sources are also important.12, 14, 16
The Government of India has developed a series of programmes to monitor and control ambient air pollution (appendix pp 23–26). The National Air Quality Monitoring Programme was initiated in 1984 to determine the status and trends of ambient air quality, which now extends to 339 cities in 29 Indian states or union territories and operates 779 air quality monitoring stations.57, 58, 59, 60 In 2019, the National Clean Air Programme was launched, which coordinates air pollution control efforts across sectors, educates the Indian public about the importance of clean air for health, and aims for 20–30% reductions in PM2·5 and PM10 concentrations by 2024 in 102 cities.60, 61 The Smart City Mission was launched in 2015 to develop 100 citizen-friendly and sustainable cities across the country.62 Based on the severity of ambient air pollution, these programmes along with others are tailored to the local situation in each city.
Evidence suggests that household air pollution in India contributes substantially to ambient particulate matter pollution.63 Therefore, the programmes aimed at controlling household air pollution have a double benefit by also reducing ambient particulate matter. Several attempts have been made to reduce the household air pollution in India through various government programmes,64, 65, 66 including Unnat Chulha Abhiyan, launched in 2014 to provide modified biomass cook stoves to low-income households, and the Pradhan Mantri Ujjwala Yojana programme, launched in 2016 to provide liquefied petroleum gas to 80 million low-income households. The Pradhan Mantri Ujjwala Yojana programme has been highly successful and has exceeded its target in 2019.67, 68, 69, 70, 71 However, additional efforts are required to achieve consistent usage of liquefied petroleum gas for cooking. The full realisation of the social, economic, and health benefits of household air pollution reduction can be achieved by overcoming the continuing challenges of limited translation of initial liquefied petroleum gas adoption to sustained adoption and limited abandonment of traditional fuels.72 This could be achieved by implementation research that explores the social, economic, and cultural factors influencing clean fuel adoption.73
The improvements in air quality across India during the COVID-19 lockdown period,74 and its upsurge again with the easing of restrictions,75 provide interesting pointers to the extent of air pollution reduction that is possible with reduced human activity. Evidence also suggests that exposure to air pollution is associated with increased risk of morbidity and mortality from COVID-19.76, 77 Therefore, reduction in air pollution could help in reducing the adverse effect of COVID-19 as well.
Air pollution has the potential to impede accumulation of future human capital by reducing children's survival, undermining their health, and reducing their ability to benefit from education.78 The cost savings resulting from the prevention of productivity losses attributable to air pollution would contribute to the formation of new human capital. The potential magnitude of the benefits, both for human health and the economy, of investing in air pollution control strategies can be seen in the experience of the USA, where every dollar invested in the control of ambient air pollution since 1970 is estimated to have yielded an economic benefit of $30, based on the willingness-to-pay approach.3 There has been a substantial reduction in air pollution in the USA over the past few decades along with significant economic growth,79 indicating that the successful implementation of air pollution control strategies could help in improving the health of the population, even when the economy is growing. The reduction of airborne lead pollution through removal of lead from gasoline in the USA has also been linked with boosted economic output through reductions in children's blood lead concentrations, thereby increasing their intelligence, creativity, and economic productivity.80 These findings indicate that investing in control of air pollution in India could be highly cost-effective and pay for itself many times over.
There are several limitations of this study. First, our estimates of premature deaths and morbidity attributable to pollution are conservative because they are based on air pollution–disease pairs for which the evidence of causality is considered adequate in the GBD analysis.21, 26 Air pollution could potentially lead to other adverse outcomes as well, such as dementia81 and loss of intelligence quotient,82 but conclusive evidence for such associations is not yet available. Additionally, the disease burden attributable to air pollution in GBD is limited to that related to long-term exposure to ambient PM2·5, household air pollution, and ozone, and does not yet consider additional pollutants such as nitrogen dioxide or the impacts of short-term variations in exposure.83 Furthermore, GBD estimates of household air pollution include only solid fuels used for cooking and not for heating. Second, we have not quantified the direct health-care costs and other potentially negative economic impacts of air pollution, such as effects on tourism or ecosystem services. Third, our output estimates depend on a number of assumptions, which, if changed, would alter the estimates. For simplicity, we assumed that the rate of growth in real output per worker is the same for all the states and that labour's share of GDP remains constant at its current value. The state-specific life tables were assumed to remain constant over the lifetimes of people currently alive, which is likely to understate the economic losses in less developed states, where survival probabilities are likely to increase in the future. Our results are also dependent on the rate at which future output is discounted. Even with these limitations, our study provides useful estimates of economic loss attributable to air pollution in every state of India using the most recent air pollution burden data.
The findings in this report should motivate the central and state governments to allocate sufficient long-term funding to prevent the adverse health impacts of air pollution. Control of air pollution in India will not only improve health as envisioned in the SDGs, but will also accelerate the potential to achieve other SDG targets, including alleviating poverty, promoting social justice, enhancing the liveability of India's cities, and reducing the pace of climatic changes. Air pollution control in India is not an expenditure, but rather an essential investment in the country's future economic growth. Strengthening the ongoing efforts to manage and prevent air pollution would help in avoiding the substantial economic losses attributable to air pollution in the states of India.
Data sharing
The air pollution exposure and disease burden data used in these analyses are available at http://ghdx.healthdata.org/gbd-2019, https://vizhub.healthdata.org/gbd-compare/india, and from the authors on request. The economic data used in these analyses are available from the authors on request.
Acknowledgments
Acknowledgments
The research reported in this publication was funded by the UN Environment Programme; Bill & Melinda Gates Foundation; and Indian Council of Medical Research, Department of Health Research, Ministry of Health and Family Welfare, Government of India. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the UN Environment Programme, Bill & Melinda Gates Foundation, the Government of India, or WHO. We gratefully acknowledge the Ministry of Health and Family Welfare of the Government of India for its support and encouragement of the India State-Level Disease Burden Initiative, the governments of the states of India for their support of this work, and the many institutions and investigators across India who provided data and other inputs for this study, the valuable guidance of the advisory board of this initiative, and the large number of staff at the Indian Council of Medical Research, Public Health Foundation of India, and the Institute for Health Metrics and Evaluation for their contribution to various aspects of the work of this Initiative.
Contributors
LD, AP, MB, MLC, PuK, and PJL conceptualised this paper and drafted it with contributions from KB, PMa, SD, BT, GAK, and RPK. The other authors provided data, participated in the analysis, or reviewed the findings, or a combination of these, and contributed to the interpretation. All authors agreed with the final version of the paper and had access to the study data as needed. LD, AP, MB, MLC, and GAK verified the data underlying this study.
India State-Level Disease Burden Initiative Air Pollution Collaborators
Anamika Pandey, Michael Brauer, Maureen L Cropper, Kalpana Balakrishnan, Prashant Mathur, Sagnik Dey, Burak Turkgulu, G Anil Kumar, Mukesh Khare, Gufran Beig, Tarun Gupta, Rinu P Krishnankutty, Kate Causey, Aaron J Cohen, Stuti Bhargava, *Ashutosh N Aggarwal, *Anurag Agrawal, *Shally Awasthi, *Fiona Bennitt, *Sadhana Bhagwat, *P Bhanumati, *Katrin Burkart, *Joy K Chakma, *Thomas C Chiles, *Sourangsu Chowdhury, *D J Christopher, *Subhojit Dey, *Samantha Fisher, *Barbara Fraumeni, *Richard Fuller, *Aloke G Ghoshal, *Mahaveer J Golechha, *Prakash C Gupta, *Rachita Gupta, *Rajeev Gupta, *Shreekant Gupta, *Sarath Guttikunda,*David Hanrahan, *Sivadasanpillai Harikrishnan, *Panniyammakal Jeemon, *Tushar K Joshi, *Rajni Kant, *Surya Kant, *Tanvir Kaur, *Parvaiz A Koul, *Praveen Kumar, *Rakesh Kumar, *Samantha L Larson, *Rakesh Lodha, *Kishore K Madhipatla, *P A Mahesh, *Ridhima Malhotra, *Shunsuke Managi, *Keith Martin,*Matthews Mathai, *Joseph L Mathew, *Ravi Mehrotra, *B V Murali Mohan, *Viswanathan Mohan, *Satinath Mukhopadhyay, *Parul Mutreja, *Nitish Naik, *Sanjeev Nair, *Jeyaraj D Pandian, *Pallavi Pant, *Arokiasamy Perianayagam, *Dorairaj Prabhakaran, *Poornima Prabhakaran, *Goura K Rath, *Shamika Ravi, *Ambuj Roy, *Yogesh D Sabde, *Sundeep Salvi, *Sankar Sambandam, *Bhavay Sharma, *Meenakshi Sharma, *Shweta Sharma, *R S Sharma, *Aakash Shrivastava, *Sujeet Singh, *Virendra Singh, *Rodney Smith, *Jeffrey D Stanaway, *Gabriella Taghian, *Nikhil Tandon, *J S Thakur, *Nihal J Thomas, *G S Toteja, *Chris M Varghese, *Chandra Venkataraman, *Krishnan N Venugopal, *Katherine D Walker, *Alexandrea Y Watson, *Sarah Wozniak, *Denis Xavier, *Gautam N Yadama, *Geetika Yadav, *D K Shukla, Hendrik J Bekedam, K Srinath Reddy, Randeep Guleria, Theo Vos, Stephen S Lim, Rakhi Dandona, Sunil Kumar, Pushpam Kumar, Philip J Landrigan, Lalit Dandona. *Names listed alphabetically.
Affiliations
Public Health Foundation of India, Gurugram, India (A Pandey PhD, G A Kumar PhD, R P Krishnankutty MPH, K K Madhipatla MS, R Malhotra MPH, P Mutreja MA, Prof D Prabhakaran DM, P Prabhakaran PhD, C M Varghese MPH, Prof K S Reddy DM, Prof R Dandona PhD, Prof L Dandona MD); Institute for Health Metrics and Evaluation, University of Washington, Seattle, WA, USA (Prof M Brauer ScD, K Causey MPH, F Bennitt BA, K Burkart PhD, S L Larson BS, J D Stanaway PhD, A Y Watson BA, S Wozniak BA, Prof T Vos PhD, Prof S S Lim PhD, Prof R Dandona, Prof L Dandona); School of Population and Public Health, The University of British Columbia, Vancouver, Canada (Prof M Brauer); Department of Economics, University of Maryland, College Park, MD, USA (Prof M L Cropper PhD, B Turkgulu MS); Department of Environmental Health Engineering, Sri Ramachandra University, Chennai, India (Prof K Balakrishnan PhD, Prof S Sambandam PhD); National Centre for Disease Informatics and Research, Indian Council of Medical Research, Bengaluru, India (P Mathur PhD); Centre for Atmospheric Sciences (Sagnik Dey PhD, S Chowdhury PhD) and Department of Civil Engineering (Prof M Khare PhD), Indian Institute of Technology Delhi, New Delhi, India; Indian Institute of Tropical Meteorology, Ministry of Earth Sciences, Government of India, Pune, India (Prof G Beig PhD); Department of Civil Engineering, Indian Institute of Technology Kanpur, Kanpur, India (Prof T Gupta ScD); Health Effects Institute, Boston, MA, USA (A J Cohen DSc, P Pant PhD, K D Walker ScD); Indian Council of Medical Research, New Delhi, India (S Bhargava PhD, J K Chakma MD, R Kant PhD, T Kaur PhD, Prof R Mehrotra DPhil, M Sharma PhD, S Sharma MPH, R S Sharma PhD, G S Toteja PhD, G Yadav DNB, D K Shukla PhD, Prof L Dandona); Department of Pulmonary Medicine (Prof A N Aggarwal DM), Advanced Pediatric Centre (Prof J L Mathew PhD), and School of Public Health (Prof J S Thakur MD), Post Graduate Institute of Medical Education and Research, Chandigarh, India; CSIR-Institute of Genomics and Integrative Biology, New Delhi, India (Prof A Agrawal PhD); Department of Paediatrics (Prof S Awasthi MD) and Department of Respiratory Medicine (Prof S Kant MD), King George's Medical University, Lucknow, India; WHO India Country Office, New Delhi, India (S Bhagwat MD, Rachita Gupta PhD, H J Bekedam MD); Social Statistics Division, Ministry of Statistics and Programme Implementation, Government of India, New Delhi, India (P Bhanumati MA); Boston College, Chestnut Hill, MA, USA (Prof T C Chiles PhD, S Fisher MPH, Praveen Kumar PhD, G Taghian BA, Prof G N Yadama PhD, Prof P J Landrigan MD); Department of Pulmonary Medicine (Prof D J Christopher FRCP) and Department of Endocrinology, Diabetes and Metabolism (Prof N J Thomas FRCP), Christian Medical College, Vellore, India; Disha Foundation, Gurugram, India (Subhojit Dey PhD); Muskie School of Public Service, University of Southern Maine, ME, USA (Prof B Fraumeni PhD); Pure Earth, New York, NY, USA (R Fuller BEng, D Hanrahan MSc); National Allergy Asthma Bronchitis Institute, Kolkata, India (Prof A G Ghoshal MD); Indian Institute of Public Health—Gandhinagar, Public Health Foundation of India, Gandhinagar, India (M J Golechha PhD); Healis—Sekhsaria Institute for Public Health, Mumbai, India (P C Gupta DSc); Eternal Heart Care Centre and Research Institute, Jaipur, India (Prof Rajeev Gupta PhD); Delhi School of Economics, New Delhi, India (Prof S Gupta PhD); Urban Emissions, New Delhi, India (S Guttikunda PhD); Department of Cardiology (Prof S Harikrishnan DM) and Achutha Menon Centre for Health Science Studies (P Jeemon PhD), Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum, India; Ministry of Health and Family Welfare, Government of India, New Delhi, India (T K Joshi MS); Department of Internal and Pulmonary Medicine, Sher-i-Kashmir Institute of Medical Sciences, Srinagar, India (Prof P Koul FRCP); CSIR National Environmental Engineering Research Institute, Nagpur, India (Rakesh Kumar PhD); Department of Paediatrics (Prof R Lodha MD), Department of Cardiology (Prof N Naik DM, Prof A Roy MD), Radiation Oncology (Prof G K Rath MD), and Department of Endocrinology and Metabolism (Prof N Tandon PhD), All India Institute of Medical Sciences, New Delhi, India; Department of Respiratory Medicine, Jagadguru Sri Shivarathreeshwara Medical College, Jagadguru Sri Shivarathreeshwara University, Mysuru, India (Prof P A Mahesh DNB); Department of Urban and Environmental Engineering, Kyushu University, Fukuoka, Japan (Prof S Managi PhD); Consortium of Universities for Global Health, Washington DC, USA (K Martin MD); Centre for Maternal and Newborn Health, Liverpool School of Tropical Medicine, Liverpool, UK (Prof M Mathai PhD); Narayan Hrudayalaya, Bengaluru, India (B V M Mohan MD); Department of Diabetology, Madras Diabetes Research Foundation and Dr. Mohan's Diabetes Specialities Centre, Chennai, India (V Mohan DSc); Department of Endocrinology and Metabolism, Institute of Postgraduate Medical Education and Research, Kolkata, India (Prof S Mukhopadhyay DM); Department of Pulmonary Medicine, Medical College, Trivandrum, India (S Nair MD); Department of Neurology, Christian Medical College, Ludhiana, India (Prof J D Pandian DM); International Institute for Population Sciences, Mumbai, India (Prof A Perianayagam PhD); Brookings India, New Delhi, India (S Ravi PhD); National Institute for Research in Environmental Health, Indian Council of Medical Research, Bhopal, India (Y D Sabde MD); Pulmocare Research and Education Foundation, Pune, India (S Salvi MD); World Resources Institute, New Delhi, India (B Sharma MSc); National Centre for Disease Control, Ministry of Health and Family Welfare, Government of India, New Delhi, India (A Shrivastava PhD, S Singh MD); Asthma Bhawan, Jaipur, India (V Singh MD); Department of Applied Economics, University of Minnesota, Saint Paul, MN, USA (Prof R Smith PhD); Indian Institute of Technology Bombay, Mumbai, India (Prof C Venkataraman PhD); Department of Cardiology, Pushpagiri Institute of Medical Sciences, Thiruvalla, India (Prof K Venugopal DM); Department of Pharmacology, St John's Medical College and Division of Clinical Research and Training, St John's Research Institute, Bengaluru, India (Prof D Xavier MD); All India Institute of Medical Sciences, New Delhi, India (Prof R Guleria DM); Directorate General Health Services, Ministry of Health and Family Welfare, Government of India, New Delhi, India (Prof Sunil Kumar MD); and Ecosystem Services Economics Unit, United Nations Environment Programme, Nairobi, Kenya (Pushpam Kumar PhD).
Declaration of interests
PMa, SB, JKC, RKa, TK, RMe, YDS, MSh, SSh, RSS, GST, GY, DKS, and LD work with the Indian Council of Medical Research, and PuK works with the UN Environment Programme, which partially funded this research. DX reports grants from AstraZeneca India, Boehringer Ingelheim, Bristol-Myers Squibb, Coco Cola India, and Pfizer, and speaker's fee from Eli Lilly and Sanofi. All other authors declare no competing interests.
Contributor Information
India State-Level Disease Burden Initiative Air Pollution Collaborators:
Anamika Pandey, Michael Brauer, Maureen L Cropper, Kalpana Balakrishnan, Prashant Mathur, Sagnik Dey, Burak Turkgulu, G Anil Kumar, Mukesh Khare, Gufran Beig, Tarun Gupta, Rinu P Krishnankutty, Kate Causey, Aaron J Cohen, Stuti Bhargava, Ashutosh N Aggarwal, Anurag Agrawal, Shally Awasthi, Fiona Bennitt, Sadhana Bhagwat, P Bhanumati, Katrin Burkart, Joy K Chakma, Thomas C Chiles, Sourangsu Chowdhury, D J Christopher, Subhojit Dey, Samantha Fisher, Barbara Fraumeni, Richard Fuller, Aloke G Ghoshal, Mahaveer J Golechha, Prakash C Gupta, Rachita Gupta, Rajeev Gupta, Shreekant Gupta, Sarath Guttikunda, David Hanrahan, Sivadasanpillai Harikrishnan, Panniyammakal Jeemon, Tushar K Joshi, Rajni Kant, Surya Kant, Tanvir Kaur, Parvaiz A Koul, Praveen Kumar, Rakesh Kumar, Samantha L Larson, Rakesh Lodha, Kishore K Madhipatla, P A Mahesh, Ridhima Malhotra, Shunsuke Managi, Keith Martin, Matthews Mathai, Joseph L Mathew, Ravi Mehrotra, B V Murali Mohan, Viswananthan Mohan, Satinath Mukhopadhyay, Parul Mutreja, Nitish Naik, Sanjeev Nair, Jeyaraj D Pandian, Pallavi Pant, Arokiasamy Perianayagam, Dorairaj Prabhakaran, Poornima Prabhakaran, Goura K Rath, Shamika Ravi, Ambuj Roy, Yogesh D Sabde, Sundeep Salvi, Sankar Sambandam, Bhavay Sharma, Meenakshi Sharma, Shweta Sharma, R S Sharma, Aakash Shrivastava, Sujeet Singh, Virendra Singh, Rodney Smith, Jeffrey D Stanaway, Gabrielle Taghian, Nikhil Tandon, J S Thakur, Nihal J Thomas, G S Toteja, Chris M Varghese, Chandra Venkataraman, Krishnan N Venugopal, Katherine D Walker, Alexandrea Y Watson, Sarah Wozniak, Denis Xavier, Gautam N Yadama, Geetika Yadav, D K Shukla, Hendrik J Bekedam, K Srinath Reddy, Randeep Guleria, Theo Vos, Stephen S Lim, Rakhi Dandona, Sunil Kumar, Pushpam Kumar, Philip J Landrigan, and Lalit Dandona
Supplementary Material
References
- 1.Lelieveld J, Evans JS, Fnais M, Giannadaki D, Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature. 2015;525:367–371. doi: 10.1038/nature15371. [DOI] [PubMed] [Google Scholar]
- 2.Cohen AJ, Brauer M, Burnett R. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389:1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landrigan PJ, Fuller R, Acosta NJR. The Lancet Commission on pollution and health. Lancet. 2018;391:462–512. doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- 4.Manisalidis I, Stavropoulou E, Stavropoulos A, Bezirtzoglou E. Environmental and health impacts of air pollution: a review. Front Public Health. 2020;8:14. doi: 10.3389/fpubh.2020.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO Air pollution. https://www.who.int/health-topics/air-pollution#tab=tab_1
- 6.Zivin JG, Neidell M. The impact of pollution on worker productivity. Am Econ Rev. 2012;102:3652–3673. doi: 10.1257/aer.102.7.3652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roth S. Air pollution, educational achievements, and human capital formation. IZA World of Labor. August, 2017. https://wol.iza.org/articles/air-pollution-educational-achievements-and-human-capital-formation/long
- 8.WHO Sustainable Development Goals for household energy. http://www.who.int/airpollution/household/sustainable-development-goals/en/
- 9.Central Pollution Control Board. Ministry of Environment. Forest and Climate Change. Government of India . CPCB; New Delhi: February, 2011. Air quality monitoring, emission inventory and source apportionment study for Indian cities—national summary report.http://cpcb.nic.in/displaypdf.php?id=RmluYWxOYXRpb25hbFN1bW1hcnkucGRm [Google Scholar]
- 10.Guttikunda SK, Goel R, Pant P. Nature of air pollution, emission sources, and management in the Indian cities. Atmos Environ. 2014;95:501–510. [Google Scholar]
- 11.Sharma M, Dikshit O. Department of Environment, Government of NCT of Delhi; January, 2016. Comprehensive study on air pollution and green house gases (GHGs) in Delhi.http://environment.delhigovt.nic.in/wps/wcm/connect/735190804acf830c8eec8f09c683c810/Final+Report09Jan2016.pdf?MOD=AJPERES&lmod=1109294014&CACHEID=735190804acf830c8eec8f09c683c810 [Google Scholar]
- 12.Upadhyay A, Dey S, Chowdhury S, Goyal P. Expected health benefits from mitigation of emissions from major anthropogenic PM2.5 sources in India: statistics at state level. Environ Pollut. 2018;242:1817–1826. doi: 10.1016/j.envpol.2018.07.085. [DOI] [PubMed] [Google Scholar]
- 13.GBD MAPS Working Group . Health Effects Institute; Boston: January, 2018. Burden of disease attributable to major air pollution sources in India. Special report 21.https://www.healtheffects.org/publication/gbd-air-pollution-india [Google Scholar]
- 14.The Automotive Research Association of India. The Energy and Resources Institute Source apportionment of PM2.5 and PM10 of Delhi NCR for identification of major sources. August, 2018. http://www.teriin.org/sites/default/files/2018-08/Exec-summary.pdf
- 15.Centre for Environment and Energy Development. Indian Institute of Technology, Delhi Know what you breathe: air pollution statistics for north Indian cities. May, 2018. http://ceedindia.org/know-what-you-breathe-air-pollution-statistics-for-north-indian-cities/
- 16.Indian Institute of Tropical Meteorology. Ministry of Earth Sciences. Government of India . Indian Institute of Tropical Meteorology; Pune: 2018. SAFAR-high resolution emission inventory of Delhi mega city—2018 (SAFAR-Delhi-2018-A) [Google Scholar]
- 17.Balakrishnan K, Sankar S, Parikh J. Daily average exposures to respirable particulate matter from combustion of biomass fuels in rural households of southern India. Environ Health Perspect. 2002;110:1069–1075. doi: 10.1289/ehp.021101069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Balakrishnan K, Sambandam S, Ramaswamy P, Mehta S, Smith KR. Exposure assessment for respirable particulates associated with household fuel use in rural districts of Andhra Pradesh, India. J Expo Anal Environ Epidemiol. 2004;14(suppl 1):S14–S25. doi: 10.1038/sj.jea.7500354. [DOI] [PubMed] [Google Scholar]
- 19.Arku RE, Birch A, Shupler M, Yusuf S, Hystad P, Brauer M. Characterizing exposure to household air pollution within the Prospective Urban Rural Epidemiology (PURE) study. Environ Int. 2018;114:307–317. doi: 10.1016/j.envint.2018.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.United States Environmental Protection Agency Ground-level ozone basics. https://www.epa.gov/ground-level-ozone-pollution/ground-level-ozone-basics
- 21.India State-Level Disease Burden Initiative Air Pollution Collaborators The impact of air pollution on deaths, disease burden, and life expectancy across the states of India: the Global Burden of Disease Study 2017. Lancet Planet Health. 2019;3:e26–e39. doi: 10.1016/S2542-5196(18)30261-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siddique S, Ray MR, Lahiri T. Effects of air pollution on the respiratory health of children: a study in the capital city of India. Air Qual Atmos Health. 2011;4:95–102. doi: 10.1007/s11869-010-0079-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Balakrishnan K, Ganguli B, Ghosh S. Part 1. Short-term effects of air pollution on mortality: results from a time-series analysis in Chennai, India. Res Rep Health Eff Inst. 2011;157:7–44. [PubMed] [Google Scholar]
- 24.Maji S, Ahmed S, Siddiqui WA, Ghosh S. Short term effects of criteria air pollutants on daily mortality in Delhi, India. Atmos Environ. 2017;150:210–219. [Google Scholar]
- 25.Prabhakaran D, Mandal S, Krishna B. Exposure to particulate matter is associated with elevated blood pressure and incident hypertension in urban India. Hypertension. 2020;76:1289–1298. doi: 10.1161/HYPERTENSIONAHA.120.15373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.GBD 2019 Risk Factors Collaborators Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chang T, Zivin JG, Gross T, Neidell M. The effect of pollution on worker productivity: evidence from call-center workers in China. June, 2016. http://ftp.iza.org/dp10027.pdf
- 28.Hansen-Lewis J. Does air pollution lower productivity? Evidence from manufacturing in India. Oct 11, 2018. http://barrett.dyson.cornell.edu/NEUDC/paper_324.pdf
- 29.Menzin J, Marton JP, Menzin JA, Willke RJ, Woodward RM, Federico V. Lost productivity due to premature mortality in developed and emerging countries: an application to smoking cessation. BMC Med Res Methodol. 2012;12:87. doi: 10.1186/1471-2288-12-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hanly PA, Sharp L. The cost of lost productivity due to premature cancer-related mortality: an economic measure of the cancer burden. BMC Cancer. 2014;14:224. doi: 10.1186/1471-2407-14-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hanly P, Soerjomataram I, Sharp L. Measuring the societal burden of cancer: the cost of lost productivity due to premature cancer-related mortality in Europe. Int J Cancer. 2015;136:E136–E145. doi: 10.1002/ijc.29105. [DOI] [PubMed] [Google Scholar]
- 32.Quah E, Boon TL. The economic cost of particulate air pollution on health in Singapore. J Asian Econ. 2003;14:73–90. [Google Scholar]
- 33.World Bank. Institute for Health Metrics and Evaluation . World Bank; Washington, DC: 2016. The cost of air pollution: strengthening the economic case for action.https://openknowledge.worldbank.org/handle/10986/25013 [Google Scholar]
- 34.Narain U, Sall C. World Bank; Washington, DC: 2016. Methodology for valuing the health impacts of air pollution: discussion of challenges and proposed solutions.http://hdl.handle.net/10986/24440 [Google Scholar]
- 35.Jo C. Cost-of-illness studies: concepts, scopes, and methods. Clin Mol Hepatol. 2014;20:327–337. doi: 10.3350/cmh.2014.20.4.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu C, Chen R, Sera F. Ambient particulate air pollution and daily mortality in 652 Cities. N Engl J Med. 2019;381:705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ministry of Statistics and Programme Implementation. Government of India State domestic product and other aggregates, 2011–2012 series. 2019. http://mospi.nic.in/data
- 38.Feenstra RC, Inklaar R, Timmer MP. The next generation of the Penn World Table. Am Econ Rev. 2015;105:3150–3182. [Google Scholar]
- 39.National Sample Survey Office Ministry of Statistics & Programme Implementation, Government of India. Employment and unemployment situation in India: NSS 68th round (July 2011—June 2012) January, 2014. http://mospi.nic.in/sites/default/files/publication_reports/nss_report_554_31jan14.pdf
- 40.Das DK, Erumban AA, Aggarwal S, Das PC. Measuring productivity at the industry level: the India KLEMS data base—data manual 2017 (version 4) 2018. https://rbidocs.rbi.org.in/rdocs/PublicationReport/Pdfs/KLEMS27032018E6B6C80028604EBCAFDA3A82ACDE9B10.PDF
- 41.Pandey RN. Women's contribution to the economy through their unpaid household work. National Institute for Public Finance and Policy Working Paper. 2001. https://www.nipfp.org.in/media/pdf/working_papers/WP_2001_182.pdf
- 42.Indian Council of Medical Research. Public Health Foundation of India. Institute for Health Metrics and Evaluation . ICMR, PHFI, and IHME; New Delhi: 2019. GBD India Compare Data Visualization.http://vizhub.healthdata.org/gbd-compare/india [Google Scholar]
- 43.Hystad P, Duong M, Brauer M. Health effects of household solid fuel use: findings from 11 countries within the prospective urban and rural epidemiology study. Environ Health Perspect. 2019;127 doi: 10.1289/EHP3915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hystad P, Larkin A, Rangarajan S. Associations of outdoor fine particulate air pollution and cardiovascular disease in 157 436 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet Planet Health. 2020;4:e235–e245. doi: 10.1016/S2542-5196(20)30103-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yusuf S, Joseph P, Rangarajan S. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395:795–808. doi: 10.1016/S0140-6736(19)32008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.National Health Systems Resource Centre . Ministry of Health and Family Welfare, Government of India; New Delhi: 2019. National health accounts estimates for India (2016–17)http://nhsrcindia.org/sites/default/files/FINAL%20National%20Health%20Accounts%202016-17%20Nov%202019-for%20Web.pdf [Google Scholar]
- 47.Lim SS, Updike RL, Kaldjian AS. Measuring human capital: a systematic analysis of 195 countries and territories, 1990–2016. Lancet. 2018;392:1217–1234. doi: 10.1016/S0140-6736(18)31941-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Bank . World Bank; Washington, DC: 2020. The human capital index 2020 update: human capital in the time of COVID-19.http://hdl.handle.net/10986/34432 [Google Scholar]
- 49.Managi S, Kumar P, Kumar P. Routledge; London: 2018. Inclusive wealth report 2018: measuring progress towards sustainability.https://www.taylorfrancis.com/books/e/9781351002080 [Google Scholar]
- 50.International Energy Agency World Energy Outlook 2016 special report: energy and air pollution. 2016. https://webstore.iea.org/weo-2016-special-report-energy-and-air-pollution#:~:text=Clean%20air%20is%20vital%20for%20good%20health.&text=Alongside%20the%20mu
- 51.Horton DE, Skinner CB, Singh D, Diffenbaugh NS. Occurrence and persistence of future atmospheric stagnation events. Nat Clim Chang. 2014;4:698–703. doi: 10.1038/nclimate2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Madronich S, Shao M, Wilson SR, Solomon KR, Longstreth JD, Tang XY. Changes in air quality and tropospheric composition due to depletion of stratospheric ozone and interactions with changing climate: implications for human and environmental health. Photochem Photobiol Sci. 2015;14:149–169. doi: 10.1039/c4pp90037e. [DOI] [PubMed] [Google Scholar]
- 53.Cropper ML, Guttikunda S, Jawahar P. Applying benefit-cost analysis to air pollution control in the Indian power sector. J Benefit Cost Anal. 2019;10(suppl 1):185–205. doi: 10.1017/bca.2018.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen S, Bloom DE. The macroeconomic burden of noncommunicable diseases associated with air pollution in China. PLoS One. 2019;14 doi: 10.1371/journal.pone.0215663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Resosudarmo BP, Napitupulu L. Health and economic impact of air pollution in Jakarta. Econ Rec. 2004;80:S65–S75. [Google Scholar]
- 56.Guo H, Kota SH, Chen K. Source contributions and potential reductions to health effects of particulate matter in India. Atmos Chem Phys. 2018;18:15219–15229. [Google Scholar]
- 57.Rangarajan R. Centre for Development Finance; May 21, 2009. Air quality monitoring regime in India: an overview.http://www.indiaenvironmentportal.org.in/files/Air%20pollution%20note_final.pdf [Google Scholar]
- 58.Ministry of Environment, Forest, and Climate Change. Government of India Revised national ambient air quality standards (NAAQS) 2009 notified. Nov 18, 2009. http://moef.gov.in/wp-content/uploads/2019/10/Press-Note-on-RNAAQS_1.pdf
- 59.Central Pollution Control Board. Ministry of Environment. Forest and Climate Change. Government of India National Air Quality Monitoring Programme. 2017. http://cpcb.nic.in/about-namp/
- 60.Ministry of Environment. Forest and Climate Change. Government of India NCAP—National Clean Air Programme. 2019. http://moef.gov.in/wp-content/uploads/2019/05/NCAP_Report.pdf
- 61.Ministry of Environment, Forest, and Climate Change. Government of India Government launches National Clean Air Programme (NCAP) Jan 10, 2019. https://pib.gov.in/pressreleaseiframepage.aspx?prid=1559384
- 62.Ministry of Housing and Urban Affairs. Government of India Smart cities mission. 2017. http://smartcities.gov.in/content/innerpage/smart-city-features.php
- 63.Chowdhury S, Dey S, Guttikunda S, Pillarisetti A, Smith KR, Di Girolamo L. Indian annual ambient air quality standard is achievable by completely mitigating emissions from household sources. Proc Natl Acad Sci USA. 2019;116:10711–10716. doi: 10.1073/pnas.1900888116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Venkataraman C, Sagar AD, Habib G, Lam N, Smith KR. The Indian National Initiative for Advanced Biomass Cookstoves: the benefits of clean combustion. Energy Sustain Dev. 2010;14:63–72. [Google Scholar]
- 65.Ministry of New and Renewable Energy. Government of India Government making efforts to reduce dependence on traditional biomass cooking. March 22, 2019. https://pib.gov.in/Pressreleaseshare.aspx?PRID=1525934
- 66.Ministry of New and Renewable Energy. Ministry of New and Renewable Energy. Government of India National Biomass Cookstoves Programme. http://164.100.94.214/national-biomass-cookstoves-programme
- 67.Ministry of Petroleum & Natural Gas. Government of India LPG connection to every household. 2018. https://pib.gov.in/Pressreleaseshare.aspx?PRID=1525181
- 68.Ministry of Petroleum & Natural Gas. Government of India Pradhan Mantri Ujjwala Yojana. 2018. http://petroleum.nic.in/sites/default/files/PMUY_SchemeE.pdf
- 69.Cabinet Committee on Economic Affairs. Government of India Cabinet approves enhancement of target under Pradhan Mantri Ujjwala Yojana. Feb 7, 2018. https://pib.gov.in/PressReleseDetail.aspx?PRID=1519602
- 70.Ministry of Petroleum & Natural Gas. Government of India Release of 8 croreth PMUY connection by Hon'ble Prime Minister. Sept 6, 2019. www.pib.nic.in/Pressreleaseshare.aspx?PRID=1584346
- 71.Ministry of Petroleum & Natural Gas. Government of India Empowering women, changing lives: PM Ujjwala Yojana and much more. March 8, 2019. https://pib.gov.in/PressReleasePage.aspx?PRID=1568243
- 72.Yadama G. Oxford University Press; New York: 2013. Fires, fuel, and the fate of 3 billion: the state of the energy impoverished. [Google Scholar]
- 73.Gould CF, Urpelainen J. LPG as a clean cooking fuel: adoption, use, and impact in rural India. Energy Policy. 2018;122:395–408. doi: 10.1016/j.enpol.2018.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kumar P, Hama S, Omidvarborna H. Temporary reduction in fine particulate matter due to ‘anthropogenic emissions switch-off’ during COVID-19 lockdown in Indian cities. Sustain Cities Soc. 2020;62 doi: 10.1016/j.scs.2020.102382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ministry of Environment. Forest and Climate Change Central Pollution Control Board. https://cpcb.nic.in/index.php
- 76.Coker ES, Cavalli L, Fabrizi E. The effects of air pollution on COVID-19 related mortality in northern Italy. Environ Resour Econ. 2020;76:611–634. doi: 10.1007/s10640-020-00486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Austin W, Carattini S, Mahecha JG, Pesko M. COVID-19 mortality and contemporaneous air pollution. October, 2020. https://www.lse.ac.uk/granthaminstitute/wp-content/uploads/2020/10/working-paper-352-Austin-et-al-1.pdf [DOI] [PMC free article] [PubMed]
- 78.Wang P, Tuvblad C, Younan D. Socioeconomic disparities and sexual dimorphism in neurotoxic effects of ambient fine particles on youth IQ: A longitudinal analysis. PLoS One. 2017;12 doi: 10.1371/journal.pone.0188731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.United States Environmental Protection Agency Progress cleaning the air and improving people's health. 2015. https://www.epa.gov/clean-air-act-overview/progress-cleaning-air-and-improving-peoples-health
- 80.Grosse SD, Matte TD, Schwartz J, Jackson RJ. Economic gains resulting from the reduction in children's exposure to lead in the United States. Environ Health Perspect. 2002;110:563–569. doi: 10.1289/ehp.02110563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chen H, Kwong JC, Copes R. Exposure to ambient air pollution and the incidence of dementia: A population-based cohort study. Environ Int. 2017;108:271–277. doi: 10.1016/j.envint.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 82.Perera FP. Multiple threats to child health from fossil fuel combustion: impacts of air pollution and climate change. Environ Health Perspect. 2017;125:141–148. doi: 10.1289/EHP299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Achakulwisut P, Brauer M, Hystad P, Anenberg SC. Global, national, and urban burdens of paediatric asthma incidence attributable to ambient NO2 pollution: estimates from global datasets. Lancet Planet Health. 2019;3:e166–e178. doi: 10.1016/S2542-5196(19)30046-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The air pollution exposure and disease burden data used in these analyses are available at http://ghdx.healthdata.org/gbd-2019, https://vizhub.healthdata.org/gbd-compare/india, and from the authors on request. The economic data used in these analyses are available from the authors on request.