Case presentation
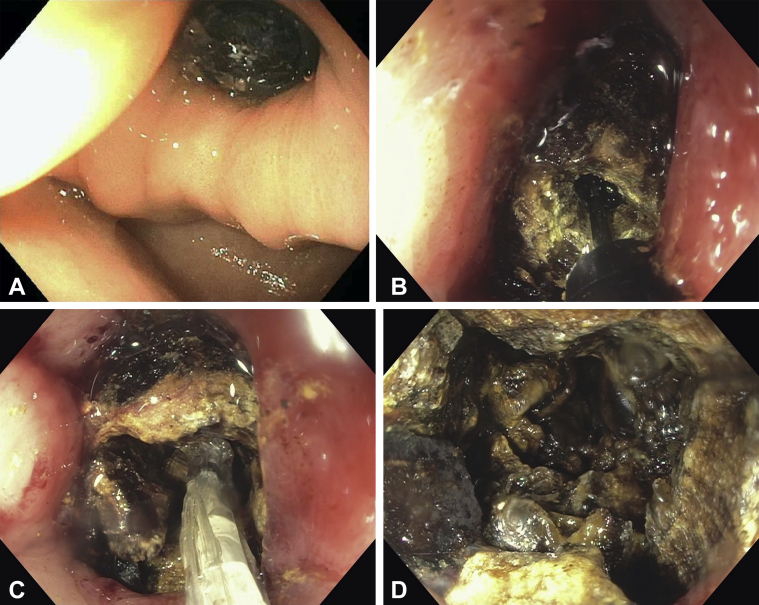
A 59-year-old white woman with unresectable metastatic adenocarcinoma of the gallbladder and a malignant hilar stricture managed with palliative uncovered metal stents in a Y-shaped configuration and repeated radiofrequency ablation (RFA) for tumor ingrowth was incidentally found to have duodenal obstruction caused by a large stone precluding a scheduled session of RFA. Because she had no complaints or symptoms related to the presence of the stone, a decision was made to abort the procedure and proceed with further assessment. A contrast-enhanced CT confirmed cholecystoduodenal fistula (Fig. 1), although no definite gallstone was identified implying its radiolucency. The diagnosis was compatible with Bouveret syndrome, and the patient agreed to endoscopic management using electrohydraulic lithotripsy (EHL) (Video 1, available online at www.VideoGIE.org).
Figure 1.
CT scan showing a fistulous communication between the gallbladder and the duodenum (arrows).
Procedure
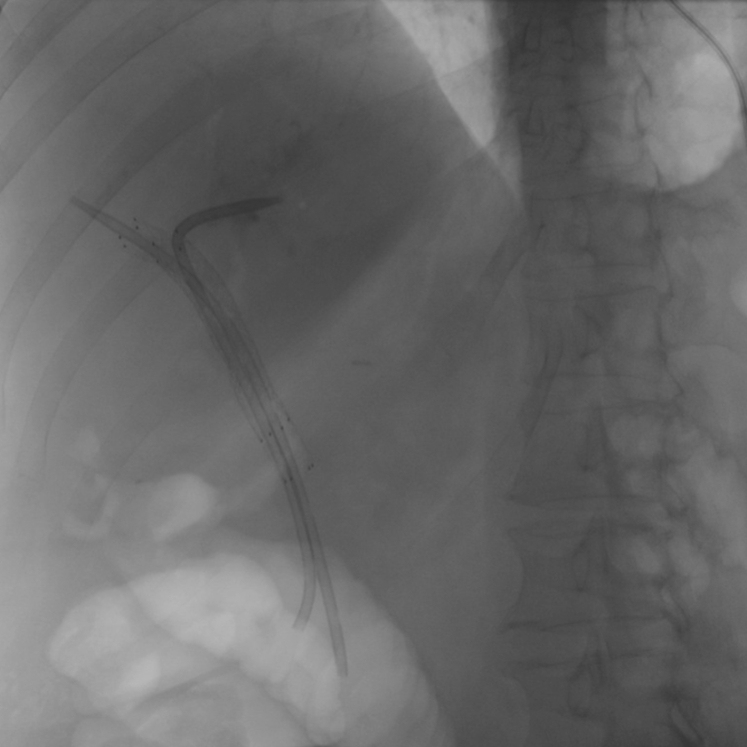
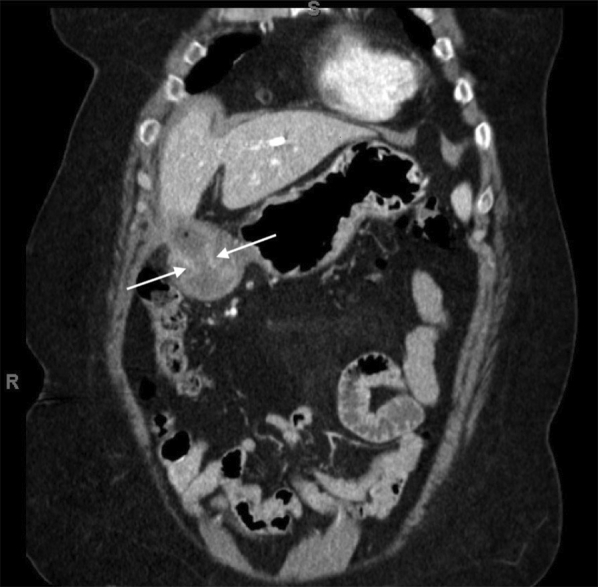
Esophagogastroduodenoscopy revealed excessive fluid in the gastric body and an impacted 50-mm gallstone in the pyloric channel (Fig. 2A). EHL (power 100 and shots 50) was performed with great difficulty with complete stone fragmentation after 4 hours of lithotripsy. The principal strategy was to drill a large crater within the stone and then dilate it for further fragmentation using a balloon dilator (Fig. 2B, C, and D). All fragments were then extracted (Fig. 3), allowing endoscopic advancement into the duodenum. Subsequently, previously placed coaxial plastic biliary stents were removed by using a snare, and selective biliary cannulation showed malignant stenosis involving the bifurcation of the hepatic ducts with adjacent portion of the common hepatic duct (CHD) (Fig. 4). Two straight 0.025-inch guidewires were passed into the left and right main hepatic ducts to secure position, and endobiliary RFA (soft coagulation; 2 bursts of 30 seconds each) was performed within the bifurcation and CHD, coagulating tumor ingrowth. The biliary tree was then swept using a 12-mm balloon catheter to remove the coagulated tumor debris, and two 10F × 7-cm plastic stents were placed through the indwelling metal stents into the hepatic ducts to prevent postcicatrization injury (Fig. 5). The patient was discharged uneventfully on the same day with a plan for a second ERCP for re-evaluation in 3 months. Surgical treatment of the fistula was not chosen in this frail patient because of the potential morbidity of such a procedure, and the choice was made to preserve the fistula.
Figure 2.
Endoscopic views showing (A) a gallstone obstructing the pyloric channel; (B) electrohydraulic lithotripsy being applied to the gallstone; (C) use of a balloon dilator for stone fragmentation; and (D) a large crater within the gallstone with partial fragmentation.
Figure 3.
A photo of retrieved gallstone fragments.
Figure 4.
Malignant biliary stricture containing the bifurcation of the hepatic ducts and adjacent common hepatic duct (arrows); known metastatic gallbladder cancer as the etiologic factor.
Figure 5.
Two plastic biliary stents placed bilaterally through indwelling metal stents to prevent postcicatrization injury after tumor debulking with radiofrequency ablation.
Discussion
Bouveret syndrome is a rare form of gastric outlet obstruction (GOO) caused by an impacted gallstone in the pylorus or proximal duodenum after its passage through a biliodigestive fistula. It typically occurs in elderly patients with multiple comorbidities and requires a high degree of suspicion because symptoms are usually nonspecific including abdominal pain, nausea, and vomiting.1 Our case presents an incidental finding before symptoms of GOO could develop. Given its rarity, no standardized management strategies have been defined. Endoscopic retrieval of the obstructing gallstone with or without lithotripsy is an appealing option because it offers a less-invasive alternative in poor surgical candidates. Reported methods of lithotripsy include mechanical, laser, extracorporeal shockwave, and intracorporeal electrohydraulic lithotripsy.2,3 The choice depends mainly on the availability at the individual center and the endoscopist. An important drawback of these methods is the risk of dislodgement of stone fragments distally causing gallstone ileus.4 Despite its low success rate (10%), interventional endoscopy should always be attempted first, and surgery should be reserved when this fails.5
Informed consent was obtained for this case report. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Petr Vanek at vanek.pe@gmail.com.
Supplementary data
Successful use of intracorporeal electrohydraulic lithotripsy in the management of Bouveret syndrome followed by endobiliary radiofrequency ablation for tumor ingrowth in a complex procedure totaling >4.5 hours.
References
- 1.Cappell M.S., Davis M. Characterization of Bouveret's syndrome: a comprehensive review of 128 cases. Am J Gastroenterol. 2006;101:2139–2146. doi: 10.1111/j.1572-0241.2006.00645.x. [DOI] [PubMed] [Google Scholar]
- 2.Caldwell K.M., Lee S.J., Leggett P.L. Bouveret syndrome: current management strategies. Clin Exp Gastroenterol. 2018;11:69–75. doi: 10.2147/CEG.S132069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trikudanathan G., Singh D., Anderson K. Successful endoscopic management of Bouvaret syndrome using laser lithotripsy. Endoscopy. 2019;51:E305–E306. doi: 10.1055/a-0915-1603. [DOI] [PubMed] [Google Scholar]
- 4.Qasaimeh G.R., Bakkar S., Jadallah K. Bouveret's syndrome: an overlooked diagnosis. A case report and review of literature. Int Surg. 2014;99:819–823. doi: 10.9738/INTSURG-D-14-00087.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nickel F., Müller-Eschner M.M., Chu J. Bouveret's syndrome: presentation of two cases with review of the literature and development of a surgical treatment strategy. BMC Surg. 2013;13:33. doi: 10.1186/1471-2482-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Successful use of intracorporeal electrohydraulic lithotripsy in the management of Bouveret syndrome followed by endobiliary radiofrequency ablation for tumor ingrowth in a complex procedure totaling >4.5 hours.