Abstract
Patient: Male, 70-year-old
Final Diagnosis: Hemobilia • hemorrhagic cholecystitis
Symptoms: Abdominal distension • abdominal pain
Medication: —
Clinical Procedure: —
Specialty: Gastroenterology and Hepatology
Objective:
Rare disease
Background:
Hemorrhagic cholecystitis is a rare disease which can be fatal in some cases. Hemorrhagic cholecystitis can sometimes be confused with common biliary diagnoses, as its symptoms imitate other hepatobiliary diseases. We report a case of hemorrhagic cholecystitis with hemobilia caused by the administration of anticoagulant agents.
Case Report:
A 70-year-old man was admitted with abdominal distention and pain. Ultrasound (US) and computed tomography (CT) showed a distended and wall-thickened gallbladder with hyperdense materials. Based on these findings and the laboratory data, the patient was diagnosed with acute cholecystitis with cholangitis. Because the patient’s hemodynamics were stable, endoscopic retrograde cholangiopancreatography (ERCP) was performed first to improve the bile flow. The results of ERCP showed blood from the common bile duct by cannulation, which was suspected to reflect hemorrhagic cholecystitis. As the abdominal symptom and CT findings worsened on the day after ERCP, emergency laparoscopic cholecystectomy was performed. An examination of the specimen revealed ulcer formation on the mucosal side of the gallbladder. The patient was discharged 6 days after the operation without any surgical complications.
Conclusions:
ERCP and early laparoscopic cholecystectomy were performed for a patient with hemorrhagic cholecystitis and hemobilia. Early diagnosis and treatment can lead to good outcomes in patients with hemorrhagic cholecystitis. Since the number of patients who are taking antithrombotic agents is increasing, hemorrhagic cholecystitis should be considered when any unusual imaging findings associated with cholecystitis are observed.
MeSH Keywords: Cholecystectomy, Laparoscopic; Cholecystitis; Hemobilia
Background
Hemorrhagic cholecystitis is a specific condition of acute cholecystitis and is potentially fatal [1]. Hemorrhage in the gallbladder may be caused by various reasons, including trauma, iatrogenic causes, cancer, and bleeding disorders. In many cases, symptoms of hemorrhagic cholecystitis, which include right upper-quadrant pain, fever, and increasing leukocytes, resemble those of calculous cholecystitis. Hemorrhagic cholecystitis may be hard to detect because it frequently shows symptoms that similar to other common diagnoses. Imaging can reveal the characteristic findings to help diagnose this rare disease. An early diagnosis can lead to good treatment outcomes. We herein describe a case of hemorrhagic cholecystitis with hemobilia due to bleeding from the gallbladder, performed with early laparoscopic cholecystectomy.
Case Report
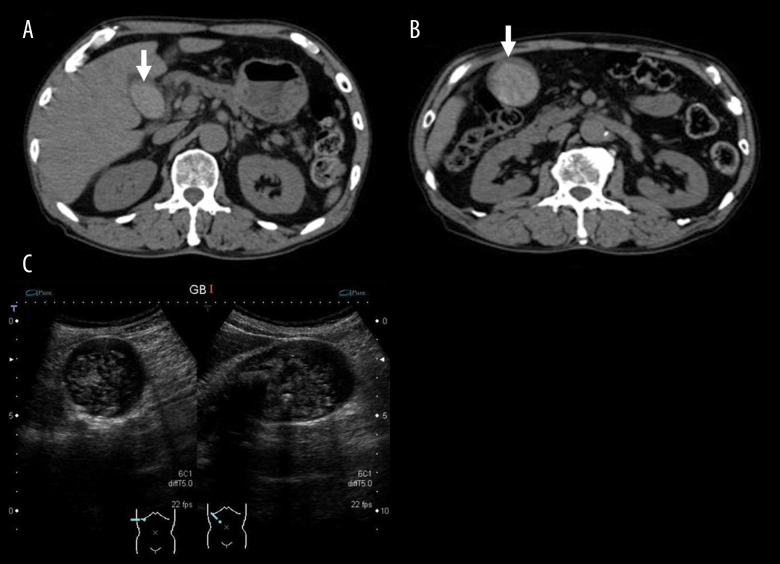
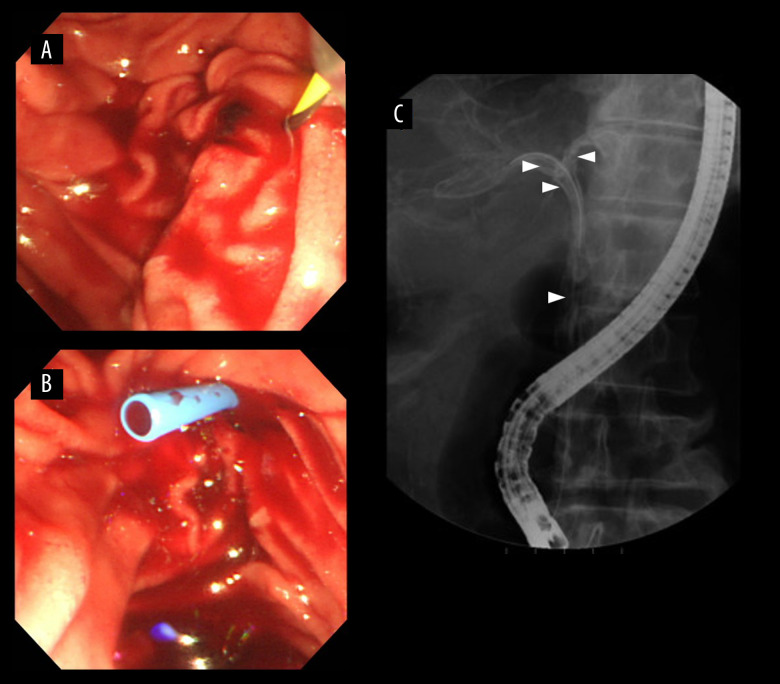
A 70-year-old man with a 7-h history of abdominal distension, pain, and nausea was admitted to our hospital. His past medical history included lumbar disc herniation, congestive heart failure, old myocardial infarction, and thrombosis in the left ventricle. He had been taking warfarin (3.0 mg) and aspirin (100 mg). Clopidogrel (75 mg) was started under the suspicion of angina pectoris, 3 weeks prior to his admission, and treatment at the Cardiology Department of our hospital had been planned. At presentation, he was afebrile, with blood pressure 131/84 mmHg and pulse 117 beats/min. An abdominal examination revealed a soft and flat abdomen; tenderness was present over the right upper quadrant, without any involuntary guarding or rebound tenderness. He had no change in bowel movements and no melena. The laboratory findings at the time of presentation were: white blood cell count, 13 000/uL; hemoglobin, 15.1 g/dL; platelet count, 19 5000/uL; total bilirubin, 2.3 mg/dL; aspartate aminotransferase, 1481 IU/L; alanine aminotransferase, 988 IU/L; alkaline phosphatase, 1058 IU/L; gamma-glutamyltranspeptidase, 315 IU/L; C-reactive protein, 0.96 mg/dL; and activated partial thromboplastin time, 34.8 s. Two days before he came to our hospital, his international normalized ratio (INR) was 2.41. Cholangitis was suspected based on these laboratory data, and acute cholecystitis was confirmed with computed tomography (CT) of the abdomen. It showed a distended, edematous gallbladder containing hyperdense material, suggestive of blood. There was no dilatation at the common or intrahepatic bile ducts. Ascites was not detected in the abdominal cavity (Figure 1A, 1B). Ultrasound (US) showed a slightly distended gallbladder with wall-thickening, gallstones, and mass-like debris without shadowing, which suggested the possibility of pus or hemorrhage (Figure 1C). Due to jaundice, suspected cholangitis, and stable hemodynamics, endoscopic retrograde cholangiopancreatography (ERCP) was performed. Fresh blood was observed on the duodenal papilla. After cannulation of the bile duct, the flow of old blood from the mammary papilla was recognized (Figure 2A, 2B). On cholangiography, numerous defects in the common bile duct were noticed and the common bile duct seemed to be filled with clots (Figure 2C). The hemobilia was initially improved, and an endoscopic retrograde biliary drainage (ERBD) tube was placed.
Figure 1.
Imaging findings of abdomen at admission. (A, B) Non-contrast CT showed hyperdense materials in the wall-thickening gallbladder (arrow) and no ascites. (C) The abdominal ultrasound demonstrated distended gallbladder with stones, echogenic materials, and a thickened wall.
Figure 2.
Results of ERCP. (A) Duodenoscopy showed blood around the duodenal papilla. (B) Cannulation led to the flow of old blood and clots from the common bile duct. (C) On cholangiography, many defects were observed in the common bile duct (arrowheads).
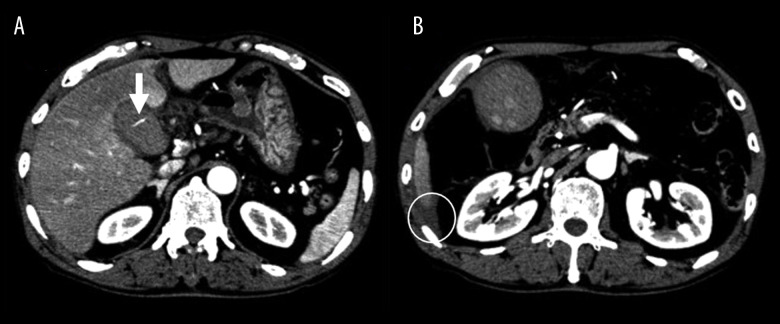
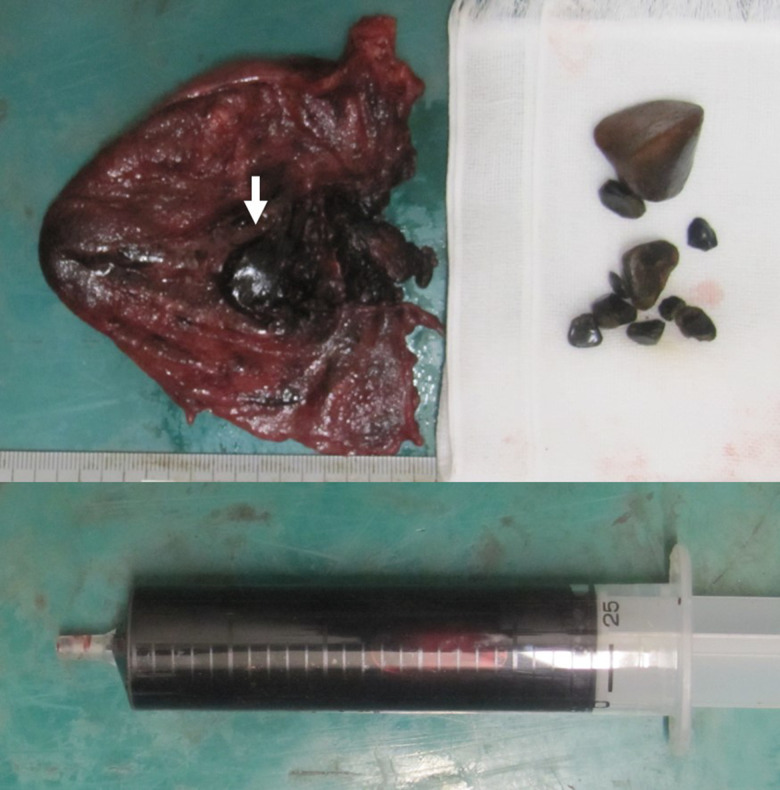
On the next day of admission, contrast CT was performed, as an abdominal physical examination showed the appearance of peritoneal irritation at the right upper quadrant. The contrast-enhanced phase revealed extravasation of contrast medium into the gallbladder lumen (Figure 3A). CT demonstrated the appearance of fluid accumulation in the Morrison fossa (Figure 3B). Since the abdominal symptoms and CT findings were exacerbated, emergency laparoscopic cholecystectomy was performed, showing a distended edematous gallbladder with a small amount of hemorrhagic ascites. Subtotal cholecystectomy was conducted under laparoscopy, and a “C-tube” was placed into the common bile duct through the cystic duct. The sample showed that the gallbladder was filled with dark blood, clots, and gallstones (Figure 4). A pathological examination of the specimen confirmed hemorrhaging, acute inflammation, and the formation of an ulcer on the mucosal side of the gallbladder. There was a muscular artery on the bottom of the ulcer, which might have been broken due to inflammation. No malignancy was detected. The postoperative course was uneventful. Anticoagulation therapy was successfully restarted on postoperative day 2. The C-tube was removed on postoperative day 3. He was discharged without any complications 6 days after the procedure.
Figure 3.
Contrast CT scan: An arterial-phase contrast CT scan revealed extravasation (arrow) into the gallbladder lumen (A) and fluid accumulation on the Morison fossa (circle) (B).
Figure 4.
Photo of the gallbladder specimen showing dark blood, clots, and gallstones in the gallbladder. The ulcer (arrow) is formed on the mucosal side.
Discussion
Hemorrhagic cholecystitis with hemobilia is a rare disease associated with high rates of morbidity and mortality if perforation or necrosis occurs [1]. Sandblom published the first report of bleeding from the hepatobiliary system as hemobilia in 1948 [2]. Shah and Clegg first reported hemobilia caused by cholecystitis as hemorrhagic cholecystitis in 1979 [3]. Iatrogenic and non-iatrogenic factors can cause bleeding from the gall-bladder. The non-iatrogenic causes of hemobilia include trauma, malignancy, administration anticoagulants, and bleeding associated with renal failure or cirrhosis [1].
Cholelithiasis might be associated with microbleeding from the gallbladder, which results in injuries to the mucosa and vessel walls. Furthermore, it is thought that high pressure in the gallbladder due to acute cholecystitis can lead to bleeding because of damage to the mucosa and vessel walls [4–6]. Gremmels et al. [7] described pathological findings of acute cholecystitis, showing that intramural inflammation led to erosion of the mucosa, infarction, and ischemia. The mucosal breakdown may cause bleeding into the gallbladder, and the intraluminal effusions and debris may mix with blood [7]. In our case, the specimen showed the formation of an ulcer on the mucosal side of the gallbladder, which might have caused the bleeding. No specific bleeding disorder was observed; however, he was taking 3 antithrombotic agents. Although he had been taking 2 antithrombotic drugs for a long time, acute hemorrhagic cholecystitis occurred 3 weeks after an additional anti-thrombotic drug was started. PT-INR were prolonged at admission. Gallbladder stone and antithrombotic drugs might play an important role in development of this disease. Without anticoagulant therapy, mucosal ulcers caused by gallbladder stones may heal quickly, but they will not heal while an anticoagulant drug is being taken. That causes continuous bleeding, which results in acute hemorrhagic cholecystitis. Cholecystolithiasis and the oral administration of antithrombotic agents seemed to both be associated with the bleeding in the present case.
The characteristic symptoms of hemobilia are abdominal pain, jaundice, and gastrointestinal bleeding through the common bile duct [8]. As these symptoms resemble those of common hepatobiliary diseases (right upper-quadrant pain, a Murphy sign, and leukocytosis), hemorrhagic cholecystitis can be easily missed by both physical and laboratory examinations [9]. History taking, a physical examination, laboratory findings, and imaging are important for the initiation of appropriate treatment of hemorrhagic cholecystitis. Although the physical and laboratory findings are similar to those for calculous acute cholecystitis, it is crucial to assess the patients’ history and investigate the administration of anticoagulants. Imaging findings can help in the diagnosis and demonstrate the characteristic findings of wall thickening of the distended gall-bladder and heterogeneous materials inside. US findings can show gallbladder distension with wall thickening, and heterogeneous echogenic materials. Blood is visualized as hyper-echoic, non-shadowing, non-mobile intraluminal materials in the gallbladder lumen [10]. CT can show the same findings as US. Furthermore, Pandya and O’Malley emphasized the value of the arterial phase of contrast-enhanced CT, which can indicate active extravasation of contrast into the gallbladder [11].
Many cases of hemorrhagic cholecystitis require endoscopic treatment, radiologic intervention, or surgery [12]. ERCP plays an important role in the treatment of hemobilia. As clots from a bleeding gallbladder may also cause common bile duct obstruction and jaundice, removing them in the common bile duct could lead to an improvement in bile flow [13]. Bleeding from the papilla of Vater is recognized in 30% of patients with hemorrhage cholecystitis when ERCP is performed [14]. Regardless of cause, the treatment for cholecystitis should follow the Tokyo Guideline 2018 (TG2018) [15]. TG2018 states that cholecystectomy is a definitive treatment for cholecystitis, while a percutaneous cholecystostomy can be performed for acute management bridging to surgery in patients with significant comorbidities [16]. However, strategies for treatment should be carefully selected. There was a case report of 1 case that underwent urgent cholecystostomy under anticoagulant therapy; unfortunately, the hyperdense contents increased within the gallbladder and CBD on follow-up CT [11]. Thus, cholecystostomy should be considered an option for preventing the need for surgery or as a bridge to surgery. TG2018 recommends early laparoscopic cholecystectomy for cholecystitis in patients without significant comorbidities, because laparoscopic surgery is becoming safer due to the development of techniques and devices. Laparoscopic cholecystectomy for patients receiving antithrombotic therapy has been controversial. However, there are a few reports of the safe performance of laparoscopic surgery for patients under antithrombotic therapy [17]. Thus, urgent surgical management, which is now recommended early in laparoscopic cholecystectomy, should be considered, according to surgeon experience, in order to prevent more serious complications [9,15]. In our case, as laboratory data showed suspected cholangitis and the patient’s hemodynamics were stable after he was admitted to our hospital, so ERCP was performed first in order to improve the flow of bile. The detection of blood in the biliary tract can reveal hemorrhagic cholecystitis. An emergency operation was performed because perforation was suspected based on the appearance of ascites and the worsening of abdominal symptoms on the following day.
Conclusions
ERCP and early laparoscopic cholecystectomy were performed for a patient with hemorrhagic cholecystitis and hemobilia who was receiving antithrombotic agents. Early diagnosis and treatment are the most important aspects in the management of hemorrhagic cholecystitis, and can lead to good outcomes. Since large numbers of patients are treated with various antithrombotic agents, hemorrhagic cholecystitis should be considered when unusual presentations of cholecystitis are encountered.
Footnotes
Conflicts of interest
None.
References:
- 1.Parekh J, Corvera CU. Hemorrhagic cholecystitis. Arch Surg. 2010;145(2):202–4. doi: 10.1001/archsurg.2009.265. [DOI] [PubMed] [Google Scholar]
- 2.Sandblom P. Hemorrhage into the biliary tract following trauma; traumatic hemobilia. Surgery. 1948;24(3):571–86. [PubMed] [Google Scholar]
- 3.Shah VR, Clegg JF. Haemorrhagic cholecystitis. Br J Surg. 1979;66(6):404–5. doi: 10.1002/bjs.1800660608. [DOI] [PubMed] [Google Scholar]
- 4.Bloechle C, Izbicki JR, Rashed MY, et al. Hemobilia: Presentation, diagnosis, and management. Am J Gastroenterol. 1994;89(9):1537–40. [PubMed] [Google Scholar]
- 5.Willemsen PJ, Vanderveken ML, De Caluwe DO, Tielliu IF. Hemobilia: A rare complication of cholecystitis and cholecystolithiasis. Case report. Acta Chir Belg. 1996;96(2):93–94. [PubMed] [Google Scholar]
- 6.Brady E, Welch JP. Acute hemorrhagic cholecystitis causing hemobilia and colonic necrosis. Dis Colon Rectum. 1985;28(3):185–87. doi: 10.1007/BF02554241. [DOI] [PubMed] [Google Scholar]
- 7.Gremmels JM, Kruskal JB, Parangi S, Kane RA. Hemorrhagic cholecystitis simulating gallbladder carcinoma. J Ultrasound Med. 2004;23(7):993–95. doi: 10.7863/jum.2004.23.7.993. [DOI] [PubMed] [Google Scholar]
- 8.Grove WJ. Biliary tract hemorrhage as a cause of hematemesis. Arch Surg. 1961;83:67–72. doi: 10.1001/archsurg.1961.01300130071008. [DOI] [PubMed] [Google Scholar]
- 9.Kwon JN. Hemorrhagic cholecystitis: Report of a case. Korean J Hepatobiliary Pancreat Surg. 2012;16(3):120–22. doi: 10.14701/kjhbps.2012.16.3.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chinn DH, Miller EI, Piper N. Hemorrhagic cholecystitis. Sonographic appearance and clinical presentation. J Ultrasound Med. 1987;6(6):313–17. doi: 10.7863/jum.1987.6.6.313. [DOI] [PubMed] [Google Scholar]
- 11.Pandya R, O’Malley C. Hemorrhagic cholecystitis as a complication of anticoagulant therapy: role of CT in its diagnosis. Abdom Imaging. 2008;33(6):652–53. doi: 10.1007/s00261-007-9358-2. [DOI] [PubMed] [Google Scholar]
- 12.Kim KH, Kim TN. Etiology, clinical features, and endoscopic management of hemobilia: A retrospective analysis of 37 cases. Korean J Gastroenterol. 2012;59(4):296–302. doi: 10.4166/kjg.2012.59.4.296. [DOI] [PubMed] [Google Scholar]
- 13.Shishida M, Ikeda M, Karakuchi N, et al. Hemorrhagic cholecystitis in a patient on maintenance dialysis. Case Rep Gastroenterol. 2017;11(2):488–93. doi: 10.1159/000479497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shin KY, Heo J, Kim JY, et al. A case of hemocholecyst associated with hemobilia following radiofrequency ablation therapy for hepatocellular carcinoma. Korean J Hepatol. 2011;17(2):148–51. doi: 10.3350/kjhep.2011.17.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miura F, Okamoto K, Takada T, et al. Tokyo Guidelines 2018: initial management of acute biliary infection and flowchart for acute cholangitis. J Hepatobiliary Pancreat Sci. 2018;25(1):31–40. doi: 10.1002/jhbp.509. [DOI] [PubMed] [Google Scholar]
- 16.Reens D, Podgorski B. Hemorrhagic cholecystitis: A case of expedited diagnosis by point-of-care ultrasound in the Emergency Department. J Emerg Med. 2019;57(1):74–76. doi: 10.1016/j.jemermed.2019.03.010. [DOI] [PubMed] [Google Scholar]
- 17.Imamura H, Minami S, Isagawa Y, et al. The impact of antithrombotic therapy in patients undergoing emergency laparoscopic cholecystectomy for acute cholecystitis – a single center experience. Asian J Endosc Surg. 2020;13(3):359–65. doi: 10.1111/ases.12751. [DOI] [PubMed] [Google Scholar]