Abstract
Study objective
We use a national emergency medicine clinical quality registry to describe recent trends in emergency department (ED) visitation overall and for select emergency conditions.
Methods
Data were drawn from the Clinical Emergency Department Registry, including 164 ED sites across 35 states participating in the registry with complete data from January 2019 through November 15, 2020. Overall ED visit counts, as well as specific emergency medical conditions identified by International Classification of Diseases, Tenth Revision, Clinical Modification code (myocardial infarction, cerebrovascular accident, cardiac arrest/ventricular fibrillation, and venous thromboembolisms), were tabulated. We plotted biweekly visit counts overall and across specific geographic regions.
Results
The largest declines in visit counts occurred early in the pandemic, with a nadir in April 46% lower than the 2019 monthly average. By November, overall ED visit counts had increased, but were 23% lower than prepandemic levels. The proportion of all ED visits that were for the select emergency conditions increased early in the pandemic; however, total visit counts for acute myocardial infarction and cerebrovascular disease have remained lower in 2020 compared with 2019. Despite considerable geographic and temporal variation in the trajectory of the coronavirus disease 2019 outbreak, the overall pattern of ED visits observed was similar across regions and time.
Conclusion
The persistent decline in ED visits for these time-sensitive emergency conditions raises the concern that coronavirus disease 2019 may continue to impede patients from seeking essential care. Efforts thus far to encourage individuals with concerning signs and symptoms to seek emergency care may not have been sufficient.
Introduction
Background
In a Morbidity and Mortality Weekly Report, the Centers for Disease Control and Prevention described a 42% decline in emergency department (ED) visits during the early coronavirus disease 2019 (COVID-19) pandemic in March and April.1 Decreased ED presentations for acute myocardial infarction have been documented,2 and mortality surveillance data demonstrate excess deaths related to heart disease.3 Comparatively less is known about a broader range of ED visits for medical emergencies closely linked to COVID-19 such as venous thromboembolism and cardiac arrest, as well as whether these observed declines in ED presentation for time-sensitive medical emergencies have been sustained during the longer course of the pandemic.4
Editor’s Capsule Summary.
What is already known on this topic
The coronavirus disease 2019 pandemic altered health care based on patient and clinician concerns and subsequent mitigation efforts.
What question this study addressed
What happened to overall US emergency department (ED) visit volume during the pandemic?
What this study adds to our knowledge
An assessment of administrative data in a volunteer sample of 164 sites in 44 states showed that ED volume hit a nadir in April 2020 and remained lower than 2019 levels through November 2020, including for acute myocardial infarction and cerebrovascular conditions.
How this is relevant to clinical practice
Patient ED use changed, likely forcing operations changes and with uncertain effect on patient outcomes. We do not know how durable the changes will be.
Importance
Delay in care seeking for time-sensitive conditions may be one contributor to excess mortality nationwide during the COVID-19 pandemic.5 Limited to deaths not attributable directly to COVID-19 infection, there were an estimated 5 excess deaths per 100,000 population from March 1 through August 1, 2020.6 Most published reports of declines in ED visitation to date are limited to the early pandemic period (through April 30), with few data to guide policymakers, clinicians, and researchers seeking to distinguish between the effects of early outbreaks and shutdowns and that of an evolving pandemic through the summer and subsequent reopening of communities and the economy. As hospitals and public health leaders contend with increasing COVID-19 cases through the winter months, an extended examination of ED utilization is essential to mitigating additional harms of the pandemic.
Goals of This Investigation
We used a national emergency medicine clinical quality registry with aggregated electronic health record data to describe more recent and comprehensive trends in ED visitation overall and for select emergency conditions.
Materials and Methods
Study Design and Setting
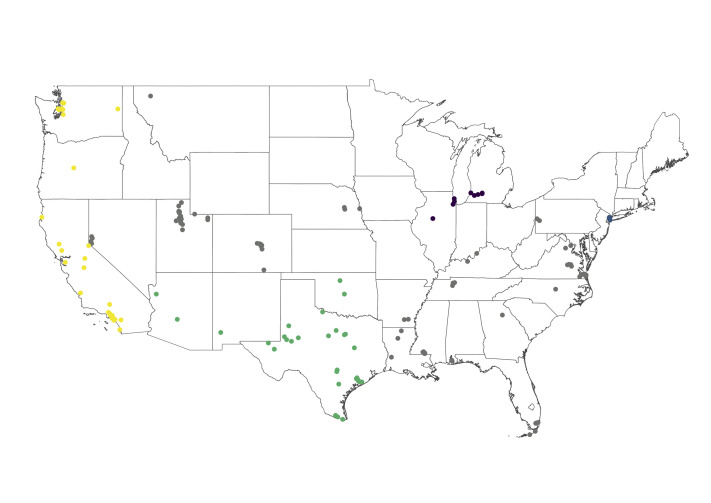
Data were drawn from the Clinical Emergency Department Registry,7 a Centers for Medicare & Medicaid Services Qualified Clinical Data Registry of ED visits maintained by the American College of Emergency Physicians (ACEP) with voluntary participation from EDs nationwide. The analysis sample included 164 ED sites across 35 states (Figure E1, available online at http://www.annemergmed.com/) participating in the registry with complete data from January 2019 through November 15, 2020, with 4 regions of the United States well represented in the sample and identified for subgroup analysis: the Northeast (New York, New Jersey, Connecticut, and Massachusetts), the Midwest (Michigan, Illinois, Iowa, and Ohio), the Southwest (Arizona, New Mexico, Utah, Texas, and Oklahoma), and the West Coast (California, Oregon, and Washington). These data were supplemented with publicly available data on daily active COVID-19 cases per 1,000 population from the University of Maryland COVID-19 Impact Analysis Platform.8
Methods of Measurement
Overall ED visit counts, as well as select emergency conditions, were tabulated. Conditions were identified among International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) with the Clinical Classifications Software Refined tool (version 2020.2; Health Cost and Utilization Project, Rockville, MD), which combines ICD-10-CM codes into clinically meaningful groups.9 This work focused on acute myocardial infarction (CIR009), cerebrovascular accident (CIR020), cardiac arrest/ventricular fibrillation (CIR018), and venous thromboembolism (CIR013 and CIR033). These were chosen to specifically represent clinical scenarios in which timely emergency care is essential, and for which alternative sites of care are unlikely to be appropriate. The daily active COVID-19 cases for the surrounding metropolitan statistical area of each ED were tabulated alongside these daily ED visit data.
Primary Data Analysis
We tabulated total ED visits, as well as select emergency conditions, by month. We plotted biweekly counts and nonparametric smoothed curves generated with a locally weighted scatterplot smoothing (bandwidth 0.18). This method computes a least squares regression for each data point, using nearby points, while applying greater statistical weight to closer points.10 For total visits, summed select emergency conditions, and each emergency condition individually, we plotted these biweekly counts from January 2019 through November 15, 2020.
To characterize changes in the monthly incidence of ED visits during 2020 compared with the 2019 baseline, we estimated Poisson models for the outcome monthly visit count, and entered each month as an indicator variable, in which the 2019 data were the reference category. We reported the raw visit counts with the associated incident rate ratios (IRRs) with 95% confidence intervals (CIs). In addition, to provide a characterization of visits for these emergency conditions changed relative to the overall visit count, we report the percentage of total visits that were for each select emergency condition. The IRR is the ratio of monthly ED visit incident rates compared with the reference category (in this case, all of 2019).
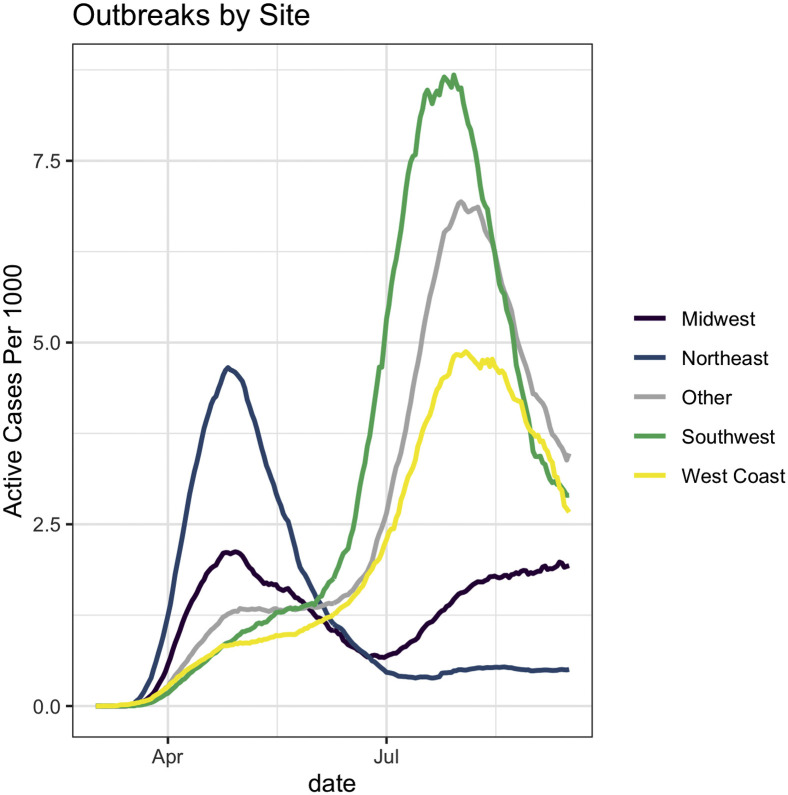
We sorted EDs into the 4 separate regions of the United States well represented in the sample (the Northeast, Midwest, Southwest, and West Coast, as stated earlier), and plotted the average daily active COVID-19 cases per 1,000 population in those regions, as well as for all other sites not contained in those regions (Figure E2, available online at http://www.annemergmed.com/). We summarized total visit counts, summed select emergency condition counts with IRRs, and percentages of total visits that were for summed select emergency conditions, plotted by regions of interest. All analyses were conducted with R software (version 4.0.2; R Foundation) and Stata (version 15; StataCorp, College Station, TX).
Results
Our sample included 164 EDs across 35 states, with median visit rate in 2019 of 31,283 (interquartile range 16,521 to 46,046). Table 1 shows the summed visit counts, monthly IRRs, and proportions, by condition. Figure 1 depicts biweekly total ED visit counts, as well as biweekly ED visit counts for select emergency conditions. Overall ED visits and ED visits for select emergency conditions decreased in March and April 2020. In January, there were 553,078 ED visits in the overall sample, and this decreased to a nadir of 280,609 visits in April, consistent with the Centers for Disease Control and Prevention report.1 By the first half of November, overall ED visits had partially returned to baseline, with 23% less than the 2019 average (IRR 0.77 [95% CI 0.76 to 0.78]).
Table 1.
2020 Monthly ED visit counts and IRRs in the Clinical Emergency Department Registry.
| Measure | Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov (Through Nov 15th) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total visits | |||||||||||
| Visits | 553,078 | 506,075 | 441,460 | 280,609 | 341,509 | 381,777 | 436,761 | 421,469 | 409,321 | 420,955 | 188,179 |
| IRR (95% CI) | 1.06 (1.06–1.06) | 0.97 (0.97–0.97) | 0.84 (0.84–0.85) | 0.54 (0.53–0.54) | 0.65 (0.65–0.66) | 0.73 (0.73–0.73) | 0.84 (0.83–0.84) | 0.81 (0.8–0.81) | 0.78 (0.78–0.79) | 0.81 (0.8–0.81) | 0.77 (0.76–0.78) |
| MI | |||||||||||
| Visits | 2,834 | 2,680 | 2,300 | 1,939 | 2,280 | 2,256 | 2,262 | 2,513 | 2,468 | 2,625 | 1,190 |
| IRR (95% CI) | 1 (0.97–1.04) | 0.95 (0.91–0.99) | 0.81 (0.78–0.85) | 0.69 (0.66–0.72) | 0.81 (0.77–0.84) | 0.8 (0.77–0.83) | 0.8 (0.77–0.84) | 0.89 (0.85–0.93) | 0.87 (0.84–0.91) | 0.93 (0.89–0.97) | 0.9 (0.87–0.94) |
| Percentage | 0.51 | 0.53 | 0.52 | 0.69 | 0.67 | 0.59 | 0.52 | 0.60 | 0.60 | 0.62 | 0.63 |
| CVA | |||||||||||
| Visits | 2,158 | 2,088 | 1,909 | 1,678 | 1,818 | 1,903 | 1,982 | 1,995 | 1,933 | 2,005 | 937 |
| IRR (95% CI) | 0.98 (0.93–1.02) | 0.94 (0.9–0.99) | 0.86 (0.82–0.9) | 0.76 (0.72–0.8) | 0.82 (0.78–0.86) | 0.86 (0.82–0.9) | 0.9 (0.86–0.94) | 0.9 (0.86–0.94) | 0.87 (0.83–0.91) | 0.91 (0.87–0.95) | 0.91 (0.87–0.95) |
| Percentage | 0.39 | 0.41 | 0.43 | 0.60 | 0.53 | 0.50 | 0.45 | 0.47 | 0.47 | 0.48 | 0.50 |
| Arrest | |||||||||||
| Visits | 1,015 | 1,040 | 1,083 | 985 | 881 | 915 | 993 | 938 | 858 | 911 | 377 |
| IRR (95% CI) | 1.01 (0.94–1.07) | 1.03 (0.97–1.1) | 1.07 (1.01–1.14) | 0.98 (0.92–1.04) | 0.87 (0.82–0.94) | 0.91 (0.85–0.97) | 0.99 (0.92–1.05) | 0.93 (0.87–0.99) | 0.85 (0.79–0.91) | 0.9 (0.85–0.97) | 0.88 (0.85–0.92) |
| Percentage | 0.18 | 0.21 | 0.25 | 0.35 | 0.26 | 0.24 | 0.23 | 0.22 | 0.21 | 0.22 | 0.20 |
| VTE | |||||||||||
| Visits | 3,075 | 2,786 | 2,311 | 1,955 | 2,395 | 2,487 | 2,652 | 2,792 | 2,712 | 2,883 | 1,247 |
| IRR (95% CI) | 1.02 (0.98–1.05) | 0.92 (0.89–0.96) | 0.76 (0.73–0.8) | 0.65 (0.62–0.68) | 0.79 (0.76–0.82) | 0.82 (0.79–0.86) | 0.88 (0.84–0.91) | 0.92 (0.89–0.96) | 0.9 (0.86–0.93) | 0.95 (0.92–0.99) | 0.8 (0.75–0.86) |
| Percentage | 0.56 | 0.55 | 0.52 | 0.70 | 0.70 | 0.65 | 0.61 | 0.66 | 0.66 | 0.68 | 0.66 |
MI, Myocardial infarction; CVA, cerebrovascular accident; VTE, venous thromboembolism.
Data are drawn from the Clinical Emergency Department Registry, a sample of 164 EDs across 35 states. Total visit counts, together with IRRs (generated by Poisson regression with 2019 as reference category), and percentages (select emergency condition count divided by overall visit count) are reported by month. Conditions were identified by diagnosis codes with Clinical Classification Software Revised. The cardiac arrest category includes ventricular fibrillation.
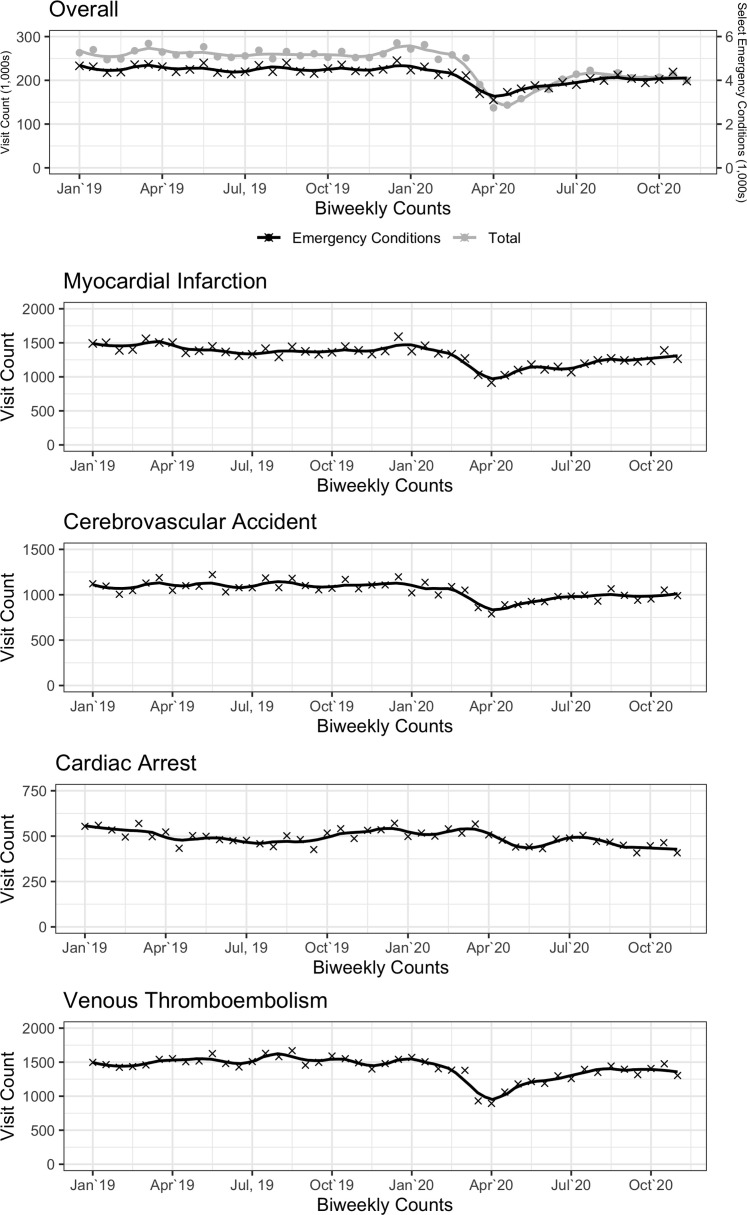
Figure 1.
Total and select emergency condition biweekly ED visit counts. Data are drawn from the Clinical Emergency Department Registry, a sample of 164 EDs across 35 states. This includes the sum of overall ED visits, as well as summed emergency conditions including the following identified by Clinical Classification Software Revised code: myocardial infarction, cerebrovascular accident, cardiac arrest/ventricular fibrillation, and venous thromboembolism. Points are plotted together with smoothed fit curves generated by locally estimated scatterplot smoothing.
Although overall visits decreased by 46% in April, the declines were generally smaller for select emergency conditions than for visits as a whole. In comparison with the 2019 average, monthly visit counts for cardiac arrest and venous thromboembolism were at 12% (IRR 0.88; 95% CI 0.85 to 0.92) and 20% (IRR 0.80; 95% CI 0.75 to 0.86) lower, respectively, in November 2020. ED visits were 10% lower for acute myocardial infarction (IRR 0.90; 95% CI 0.87 to 0.94) and 9% lower for cerebrovascular disease (IRR 0.91; 95% CI 0.87 to 0.95). The percentage of total visits that were for myocardial infarction increased from 0.51% in January 2020 to 0.69% in April 2020. The percentage of total visits with a diagnosis of cardiac arrest increased to 0.35% in April 2020, nearly doubling from 0.18% in January 2020.
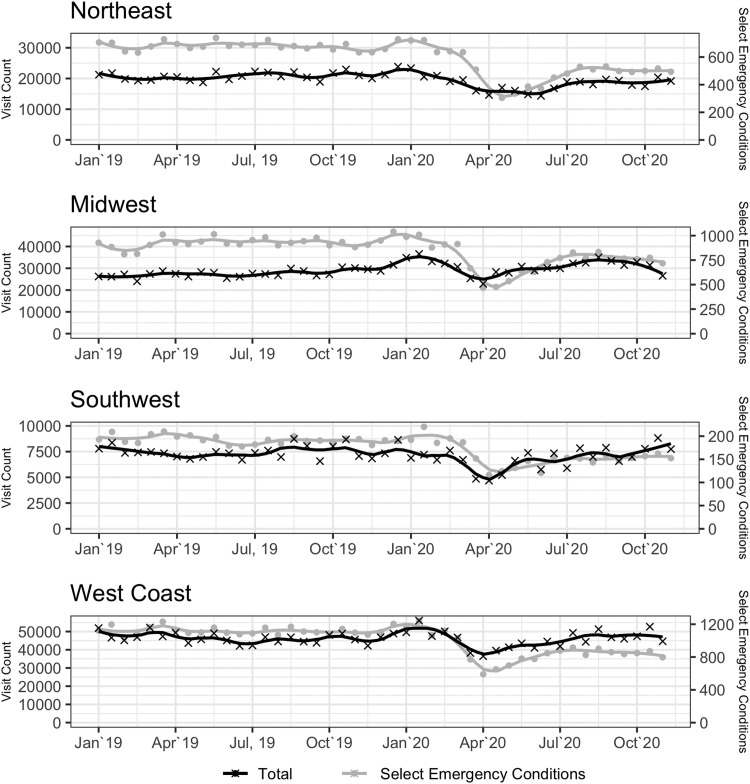
Figure 2 depicts the total and summed select emergency condition visit counts across COVID-19 outbreak regions addressed in the analysis. Despite considerable variation in the trajectory of the COVID-19 outbreak (Figure E2, available online at http://www.annemergmed.com/), the overall pattern of ED visits observed was similar across regions. The Northeast exhibited 35% less visits in April compared with the 2019 average (IRR 0.65; 95% CI 0.62 to 0.68), corresponding to the early peak in COVID-19 cases in New York City and surrounding areas. Similar to the national trend, the proportion of overall ED visits that were for any one of the select high-acuity conditions increased from 1.50% in January to 2.43% in April 2020 in the Northeast, with similar changes in the other geographic regions. Table 2 shows the visit counts and monthly IRRs across different regions of the United States, with varying time trends in COVID-19 outbreaks.
Figure 2.
Total and summed select emergency condition biweekly ED visit counts, by region. Data are drawn from the Clinical Emergency Department Registry, a sample of 164 EDs across 35 states. This includes the sum of overall ED visits, as well as summed emergency conditions including the following identified by Clinical Classification Software Revised code: myocardial infarction, cerebrovascular accident, cardiac arrest/ventricular fibrillation, and venous thromboembolism. Points are plotted together with smoothed fit curves generated by locally estimated scatterplot smoothing.
Table 2.
2020 Monthly ED visit counts and IRRs, by region, in the Clinical Emergency Department Registry.
| Measure | Jan | Feb | Mar | Apr | May | Jun | Jul | Aug | Sep | Oct | Nov (Through Nov 15th) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Northeast | |||||||||||
| Count | 64,877 | 57,434 | 51,462 | 28,982 | 32,458 | 36,984 | 45,437 | 46,835 | 44,563 | 45,713 | 20,837 |
| IRR (95% CI) | 1.02 (0.98–1.05) | 0.92 (0.89–0.96) | 0.76 (0.73–0.8) | 0.65 (0.62–0.68) | 0.79 (0.76–0.82) | 0.82 (0.79–0.86) | 0.88 (0.84–0.91) | 0.92 (0.89–0.96) | 0.9 (0.86–0.93) | 0.95 (0.92–0.99) | 0.73 (0.72–0.74) |
| Select emergency conditions | |||||||||||
| Count | 976 | 889 | 790 | 703 | 685 | 692 | 841 | 838 | 826 | 841 | 400 |
| IRR (95% CI) | 1.01 (0.94–1.07) | 1.03 (0.97–1.1) | 1.07 (1.01–1.14) | 0.98 (0.92–1.04) | 0.87 (0.82–0.94) | 0.91 (0.85–0.97) | 0.99 (0.92–1.05) | 0.93 (0.87–0.99) | 0.85 (0.79–0.91) | 0.9 (0.85–0.97) | 0.92 (0.86–0.99) |
| Percentage | 1.50 | 1.55 | 1.54 | 2.43 | 2.11 | 1.87 | 1.85 | 1.79 | 1.85 | 1.84 | 1.92 |
| Midwest | |||||||||||
| Count | 89,880 | 80,445 | 71,122 | 42,484 | 52,735 | 61,142 | 71,987 | 72,093 | 69,156 | 69,024 | 30,417 |
| IRR (95% CI) | 1.06 (1.05–1.07) | 0.94 (0.93–0.95) | 0.84 (0.83–0.85) | 0.47 (0.47–0.48) | 0.53 (0.52–0.54) | 0.6 (0.6–0.61) | 0.74 (0.73–0.75) | 0.76 (0.76–0.77) | 0.75 (0.74–0.75) | 0.6 (0.59–0.61) | 0.78 (0.77–0.79) |
| Select emergency conditions | |||||||||||
| Count | 1,587 | 1,452 | 1,245 | 1,137 | 1,304 | 1,315 | 1,383 | 1,502 | 1,441 | 1,430 | 556 |
| IRR (95% CI) | 1.05 (0.99–1.12) | 0.96 (0.9–1.03) | 0.85 (0.79–0.92) | 0.76 (0.7–0.82) | 0.74 (0.68–0.8) | 0.75 (0.69–0.81) | 0.91 (0.85–0.97) | 0.9 (0.84–0.97) | 0.91 (0.85–0.97) | 0.75 (0.7–0.81) | 0.97 (0.91–1.02) |
| Percentage | 1.77 | 1.80 | 1.75 | 2.68 | 2.47 | 2.15 | 1.92 | 2.08 | 2.08 | 2.07 | 1.83 |
| Southwest | |||||||||||
| Count | 18,567 | 17,131 | 15,237 | 10,817 | 12,515 | 12,380 | 13,718 | 13,609 | 13,533 | 14,372 | 6,457 |
| IRR (95% CI) | 1.08 (1.07–1.08) | 0.96 (0.96–0.97) | 0.85 (0.85–0.86) | 0.51 (0.5–0.51) | 0.63 (0.63–0.64) | 0.73 (0.73–0.74) | 0.86 (0.86–0.87) | 0.86 (0.86–0.87) | 0.83 (0.82–0.83) | 0.58 (0.58–0.59) | 0.8 (0.79–0.81) |
| Select emergency conditions | |||||||||||
| Count | 313 | 318 | 257 | 220 | 311 | 291 | 305 | 330 | 301 | 369 | 162 |
| IRR(95% CI) | 1.29 (1.22–1.36) | 1.18 (1.12–1.24) | 1.01 (0.95–1.07) | 0.92 (0.87–0.98) | 1.06 (1–1.12) | 1.07 (1.01–1.13) | 1.12 (1.06–1.19) | 1.22 (1.16–1.28) | 1.16 (1.1–1.22) | 0.75 (0.7–0.8) | 1.04 (0.93–1.16) |
| Percentage | 1.69 | 1.86 | 1.69 | 2.03 | 2.49 | 2.35 | 2.22 | 2.42 | 2.22 | 2.57 | 2.51 |
| West Coast | |||||||||||
| Count | 108,640 | 98,462 | 81,120 | 55,778 | 66,503 | 73,058 | 80,733 | 77,767 | 76,343 | 77,446 | 33,681 |
| IRR (95% CI) | 1.07 (1.06–1.09) | 0.99 (0.98–1.01) | 0.88 (0.87–0.9) | 0.63 (0.61–0.64) | 0.72 (0.71–0.74) | 0.72 (0.7–0.73) | 0.79 (0.78–0.81) | 0.79 (0.77–0.8) | 0.83 (0.82–0.85) | 0.73 (0.72–0.74) | 0.72 (0.71–0.72) |
| Select emergency conditions | |||||||||||
| Count | 2,347 | 2,169 | 1,889 | 1,690 | 1,887 | 1,902 | 2,027 | 2,126 | 2,063 | 2,223 | 941 |
| IRR (95% CI) | 0.94 (0.84–1.05) | 0.95 (0.85–1.07) | 0.77 (0.68–0.87) | 0.66 (0.58–0.76) | 0.93 (0.83–1.05) | 0.87 (0.78–0.98) | 0.92 (0.81–1.03) | 0.99 (0.89–1.11) | 1.11 (1–1.23) | 0.92 (0.82–1.03) | 0.98 (0.93–1.02) |
| Percentage | 2.16 | 2.20 | 2.33 | 3.03 | 2.84 | 2.60 | 2.51 | 2.73 | 2.70 | 2.87 | 2.79 |
Data are drawn from the Clinical Emergency Department Registry, a sample of 164 EDs across 35 states. Total visit counts, together with IRRs (generated by Poisson regression with 2019 as reference category), and percentages (summed select emergency condition count divided by overall visit count) are reported by month. Summed select emergency conditions were identified by diagnosis codes with Clinical Classification Software Revised, and included acute myocardial infarction, cerebrovascular accident, cardiac arrest/ventricular fibrillation, and venous thromboembolism.
Limitations
The findings in this report are subject to several limitations. First, this work cannot empirically address why visit counts changed, and explanations for the reasons behind changes are strictly conjecture. Although the Clinical Emergency Department Registry represents a diverse range of EDs across the country, including a relative focus on smaller, community EDs, the sample has not been validated as nationally representative. Our results should not be interpreted as unbiased estimates of the behavior of ED visit counts nationwide, but rather as a useful starting point for discussion of care seeking and access issues in the pandemic era. Second, diagnostic categories rely on the use of specific codes, and these may not be consistently or reliably applied to ED visits in each case. Third, the present study focused on a specific subset of high-acuity conditions, aimed at targeting those that almost certainly warrant timely care in an ED setting. Broader changes in the mix of presentations and acuity to the nation’s EDs are not addressed in the present analysis. To address the underlying issue—namely, what happened to those patients who would have otherwise presented for stroke or myocardial infarction but did not owing to COVID-19—future work is required. One approach might be to take advantage of especially comprehensive patient-level data (for example, in a large, integrated health system) to follow over time the clinical course of these potential disease entities. An answer to this question will be an essential piece of the puzzle to limit excess mortality in the era of COVID-19.
Discussion
We found that both the total and emergency-condition-specific ED visit counts had not returned to their prepandemic levels by mid-November in this national registry of US EDs. The decline in ED visit counts was larger among overall visits than in the subset of visits for select emergency conditions in this analysis. Although COVID-19’s effect varied significantly over time and across regions of the United States, we did not find significant variation in the pattern of ED visits across regions.
Our study extends prior work, with a large sample of EDs across 35 states and a longer duration. The decline in overall ED visit counts may be related to increased use of alternative modes of care (telemedicine) and decreased propensity to seek care. These changes may not be dangerous in the case of low-acuity conditions or clinical syndromes such as headache, for which emergency diagnoses are rare. Such an explanation, though, is not readily available for emergency conditions such as stroke or myocardial infarction, for which time is tissue. Concurrent with spikes in COVID-19 cases, the visit counts for cardiac arrest/ventricular fibrillation were greater than in 2019 in the early period, as well as late summer. That presentations for cardiac arrest/ventricular fibrillation have increased as visits for other high-acuity conditions have decreased provides additional evidence that patients may be delaying care for life-threatening conditions. It is also possible that critically ill patients were more often boarding where COVID-19 outbreaks were large, thus increasing the number of patients arresting in the ED. Furthermore, the consistent patterns found among varied acute medical conditions—myocardial infarction, stroke, and venous thromboembolism—also suggest that patients are avoiding time-sensitive emergency care beyond infectious syndromes.
In conclusion, the decline in ED visits for these time-sensitive emergencies raises the concern that the COVID-19 pandemic may be associated with a detrimental change in care-seeking behavior or access to care. Efforts thus far to encourage individuals with concerning signs and symptoms to seek emergency care may not have been sufficient. Visit counts increased after an initial nadir in April, but through mid-November, there has not been a return to baseline in acute care-seeking behavior as measured by visit counts to our nation’s EDs.
Footnotes
Please see page 85 for the Editor’s Capsule Summary of this article.
Supervising editor: Donald M. Yealy, MD. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
Author contributions: AKV and ATJ conceived the study. ATJ, CR, and SL designed and performed the analysis. AKV, PG, AT, and ML contributed to data acquisition. AKV and ATJ drafted the manuscript, and all authors contributed to the study.
All authors attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist. Dr. Venkatesh reports receiving support through contract HHSM-500-2013-13018I-T0001 modification 000002 from the Centers for Medicare & Medicaid Services, as well as receiving career development support (grant KL2TR001862) from the National Center for Advancing Translational Science and Yale Center for Clinical Investigation and the American Board of Emergency Medicine–National Academy of Medicine Anniversary Fellowship.
A podcast for this article is available at www.annemergmed.com.
Supplementary Data
Figure S1.
Clinical Emergency Department Registry sites in the analysis sample.
Figure S2.
COVID-19 outbreaks by active cases per 1,000 population, across regions.
References
- 1.Hartnett K.P., Kite-Powell A., DeVies J. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75:2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Woolf S.H., Chapman D.A., Sabo R.T. Excess deaths from COVID-19 and other causes, March-April 2020. JAMA. https://jamanetwork.com/journals/jama/fullarticle/2768086 Available at: [DOI] [PMC free article] [PubMed]
- 4.Anderson T.S., Stevens J.P., Pinheiro A. Hospitalizations for emergent medical, surgical, and obstetric conditions in Boston during the COVID-19 pandemic. J Gen Intern Med. 2020;35:3129–3132. doi: 10.1007/s11606-020-06027-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bilinski A., Emanuel E.J. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA. 2020;324:2100–2102. doi: 10.1001/jama.2020.20717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woolf S.H., Chapman D.A., Sabo R.T. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA. https://doi.org/10.1001/jama.2020.19545 [DOI] [PMC free article] [PubMed]
- 7.American College of Emergency Physicians Clinical Emergency Department Registry. https://www.acep.org/cedr/ Available at:
- 8.Maryland Transportation Institute . University of Maryland; College Park, MD: 2020. University of Maryland COVID-19 Impact Analysis Platform.https://data.covid.umd.edu Available at: [Google Scholar]
- 9.Agency for Healthcare Research and Quality Clinical Classification Software Refined (CCSR) for ICD-10-CM diagnoses. Healthcare Cost and Utilization Project. https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp Available at:
- 10.Cleveland W.S. Robust locally weighted regression and smoothing scatterplots. J Am Stat Assoc. 1979;74:829–836. [Google Scholar]