Abstract
The world is presently infected by the biological fever of COVID-19 caused by SARS-CoV-2 virus. The present study is mainly related to the airborne transmission of novel coronavirus through airway. Similarly, our mother planet is suffering from drastic effects of air pollution. There are sufficient probabilities or evidences proven for contagious virus transmission through polluted airborne-pathway in formed aerosol molecules. The pathways and sources of spread are detailed along with the best possible green control technologies or ideas to hinder further transmission. The combined effects of such root causes and unwanted outcomes are similar in nature leading to acute cardiac arrest of our planet. To maintain environmental sustainability, the prior future of such emerging unknown biological hazardous air emissions is to be thoroughly researched. So it is high time to deal with the future of hazardous air pollution and work on its preventive measures. The lifetime of such an airborne virus continues for several hours, thus imposing severe threat even during post-lockdown phase. The world waits eagerly for the development of successful vaccination or medication but the possible outcome is quite uncertain in terms of equivalent economy distribution and biomedical availability. Thus, risk assessments are to be carried out even during the post-vaccination period with proper environmental surveillance and monitoring. The skilled techniques of disinfection, sanitization, and other viable wayouts are to be modified with time, place, and prevailing climatic conditions, handling the pandemic efficiently. A healthy atmosphere makes the earth a better place to dwell, ensuring its future lifecycle.
Abbreviations: COVID-19, coronavirus disease, 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; WHO, World Health Organization; CoV, Coronavirus; 2019-nCoV, 2019 novel coronavirus; CSG, Coronavirus Study Group; ICTV, International Committee on Taxonomy of Viruses; ACE2, angiotensin-converting enzyme 2; MERS-CoV, Middle-East Respiratory Syndrome coronavirus; NFKB, nuclear factor kappa-light-chain-enhancer of activated B cells; PM, particulate matter; NRF2, nuclear factor erythroid 2-related factor 2; ROS, reactive oxygen species; API, air pollution index; COCOREC, Collaborative Study COVID Recurrence; VOC, volatile organic compound; FCVS, filtered containment venting systems; EPA, Environmental Protection Agency; ASTM, American Society for Testing and Materials; ISO, International organization of Standardization; NAAQS, National Ambient Air Quality Standard; ANN, artificial neural network; IoT, Internet of Things; BCG, Bacillus Calmette Guérin; USEPA, United States Environmental Protection Agency; HEME, High-Efficiency Mist Eliminator; IHD, Ischemic Heart Disease; ALRI, Acute Lower Respiratory Infections; COPD, Chronic Obstructive Pulmonary Disorder; UVGI, Ultraviolet Germicidal Irradiation
Keywords: SARS-CoV-2, Novel coronavirus, Airborne virus, Pathways of transmission, Aerosol or particulate matter, Prevention and control measures, Dispersion
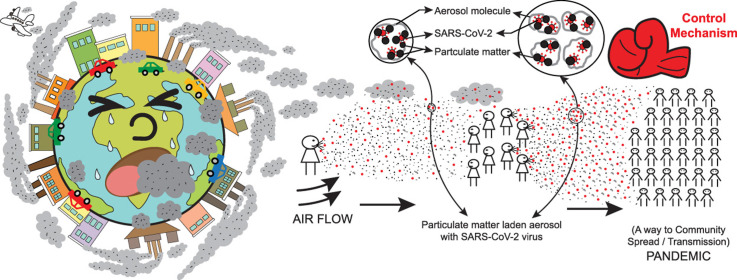
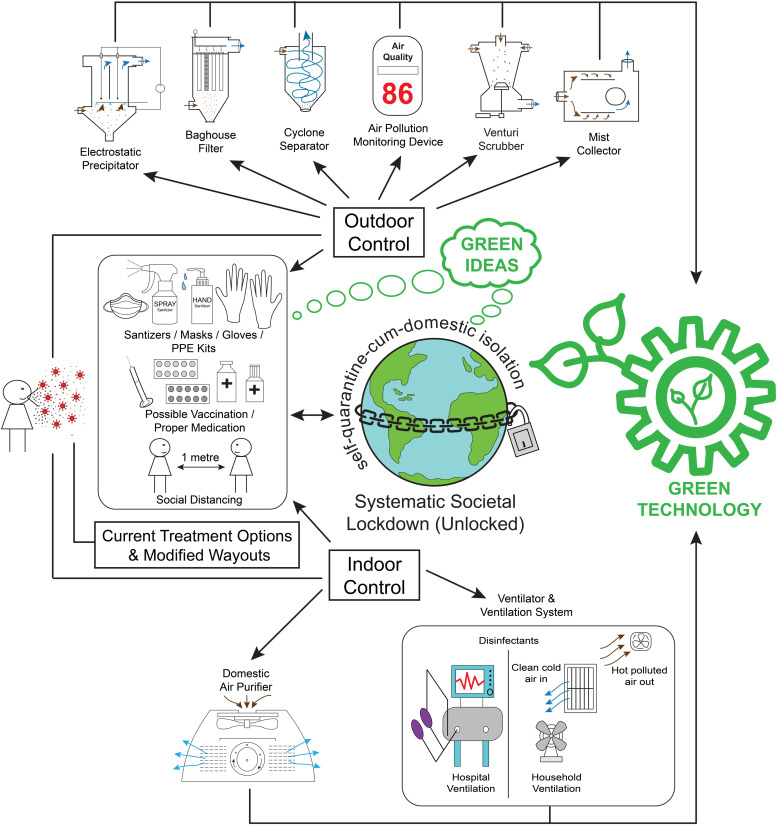
Graphical Abstract
1. Introduction
Coronavirus disease, 2019 (COVID-19) is presently one of the main growing concerns over mankind for the last few months of 2020. The effects of coronavirus are highly devastating with time over the human environment and ecology, resulting in a huge global environmental transition. The spread of COVID-19 by SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus was initially originated from a specific city of China named Wuhan. Gradually, due to human intervention and contact, the disease started transmitting in the global platform from one nation to another. At present times, it is one of the main causes of the global pandemic thus changing the environmental scenario in different geographical and climatic conditions. As it is referred to the severe acute respiratory syndrome, it is directly associated with airborne transmission. Previously, it is proved that such viral transmission is prone to several acute respiratory problems when it is present in the aerosol form [1]. According to WHO (World Health Organization) guidelines, there are various modes of viral transmission related to SARS-CoV-2. The modes of viral transmission are generally categorized into 3 types, which are stated as airborne transmission, direct contact transmission (i.e., that generally gets directly transferred via direct contact with the contaminated surface), which is also referred to as fomite transmission, and droplet transmission (i.e. transmits in form of large respiratory droplets) [2]. Droplet transmission occurs when two persons are in close contact with each other (within 1 m), and the respiratory droplets accordingly get transferred in the form of an aerosol. The infectious droplet can transmit to human eyes, nose, and mouth when they are exposed to such contagious respiratory droplets [3]. This particular respiratory syndrome is associated or results in the development of several chronic or acute disorders like fever, dry cough, breathing problems, pneumonia, dyspnea which may finally lead to respiratory failure or death [4]. Ambient air pollution caused due to PM2.5 is a global environmental issue because it is categorized under one of the primary atmospheric hazards leading to vascular inflammation, oxidative stress, severity in cardiovascular conditions, improper vasomotor responses, etc [5]. Continuous exposure to PM2.5 has a dangerous impact on the fast progression of cancer, fibrotic diseases having in vivo, and in vitro effects on various pulmonary cells [6]. Fine particulate aerosol matter in the ambient atmosphere is an indirect means of respiration which involves the pro-inflammation and oxidation mechanism within the human body [7]. According to a particular study done in the United States, it is being found that 63% of air samples were tested positive. Moreover, the air in several patient rooms, hospital lawns as well as the ambient atmosphere near hospital arenas in Nebraska, USA contains a viral load of 2.9 copies/L [8]. New Delhi, Mumbai in India as well as several cities of India and China are some of the most polluted cities in the world. It is found those population and pollution indexes are connected equivalently which combinedly poses a severe threat over the present pandemic situation in the world [9]. In terms of PM2.5 and NOX, New Delhi is the second most polluted city in the world. At the same point of time, it is a leading city in terms of COVID-19 infection [9]. These toxic contaminants are two primary outdoor pollutants responsible for drastic health impacts on mankind [10]. It is being found that hazardous air pollutants like sulfur, nitrogen dioxide, particulate matter lead to significant health impacts over human biology through socio-economic pathways thus affecting the anthropogenic ecosystem. Prolonged exposure to particulate dust actually harms the climate scenario globally [11]. In general, it is always to be kept in mind that all kinds of severe respiratory cardiovascular diseases are combined effects of viral infections and air hazards [12]. Considering the health point of view, the earth has undergone a huge transformation thus changing the human lifestyle accordingly.
1.1. What is SARS-CoV-2 or novel coronavirus?
Coronavirus (CoV) is an enveloped, single-stranded, positive-sense RNA virus ( Fig. 1(A)), where a long polycistronic mRNA is produced, that codes for several proteins [13]. It is named for its solar-corona-like appearance due to its surface spikes of 9–12 nm long [14]. The virus was called 2019 novel coronavirus (2019-nCoV), that was first found in a sample of broncho-alveolar lavage fluid of a patient, later identified as a new RNA virus strain from the family Coronaviridae, and was confirmed as the cause of a novel coronavirus infected pneumonia (NCIP) [15], occurred in Wuhan, Hubei province, China [16]. Due to the close genetic similarity (89.1% nucleotide similarity) of its viral genome (29,903 nucleotides) [17] with SARS-like CoVs, that has previously been found in BatCov RaTG13, isolated from bats [18], it was changed to SARS-CoV-2 (severe acute respiratory syndrome coronavirus-2) by the Coronavirus Study Group (CSG) of International Committee on Taxonomy of Viruses (ICTV) [19], [20]. Shortly, thereafter, WHO named this disease caused by coronavirus COVID-19 (coronavirus disease, 2019) [21]. Taxonomically, SARS-CoV-2 or novel coronavirus belongs to the order Nidovirales, suborder Cornidovirineae, family Coronaviridae, subfamily Orthocoronavirinae, genus Betacoronavirus (lineage B), subgenus Sarbecovirus, and the species severe acute respiratory syndrome-related coronavirus [22]. SARS-CoV-2 expresses four major protein on its envelope (Fig. 1(A)), one of which is the spike protein (S), that binds to human angiotensin-converting enzyme 2 (ACE2) receptors and mediates subsequent viral entry into the host cell [23], [24]. A membrane glycoprotein, named ACE2, is usually expressed within the kidney, endothelium, lungs, and heart; and plays a vital role in the cardiovascular and immune systems [25], [26]. The SARS-CoV-2 binds to its host cell, especially the alveolar epithelial cells, via the ACE-2 receptors, infects the lower respiratory tract (Fig. 1(B)), and thereby induces the secretion of inflammatory cytokines into the epithelial cells, resulting in the disruption of the epithelial-endothelial barrier and leading to multi-organ damage [27], [28].
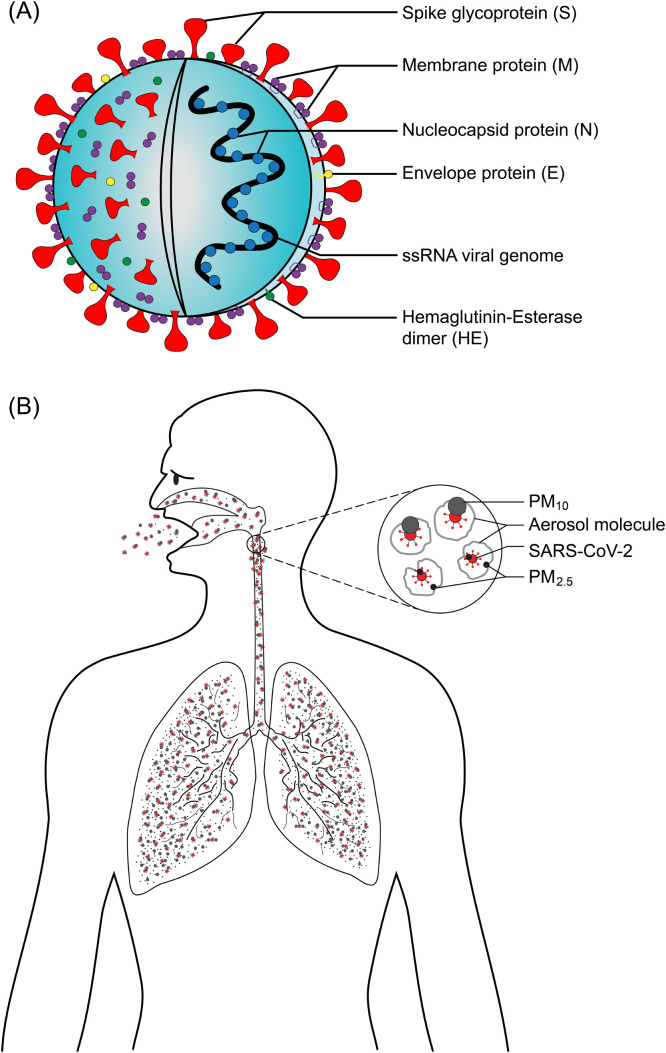
Fig. 1.
SARS-CoV-2 virus and its effect of transmission through aerosol particulates over human biology. (A) Biological structure and schematic diagram of SARS-CoV-2 virus. (B) Viral load adhered to the surface of aerosol particulates severely affecting human respiratory tract and system.
While the entire science community is focusing on airborne transmission of the COVID virus, it is also quite necessary to locate the probable hotspot zones for atmospheric pollution and the ways to control it. Air pollution due to gaseous matter/particulate emission can occur in our environment on an indoor as well as outdoor scale. Past literature survey accordingly shows the fact that several viruses related to respiratory syndromes like SARS-CoV, MERS-CoV (Middle-East Respiratory Syndrome coronavirus), influenza virus, respiratory syncytial virus (causes bronchitis in infants) are all air-borne in nature having both short-range and long-range transmission possibilities [29]. Due to the effect of continuous exposure to air pollution and particulate emission, it is clearly understood that the diseases associated with serious respiratory trouble like asthma, respiratory inflammation, bronchitis, pneumonia, lung impairment, ischemic heart disorder, etc. can further lead to death or rapid increase of mortality rate [30]. It is being reported that the USA, India, China, Chile, Brazil, Mexico, European countries are some of the leading countries that are hugely affected by particulate matter and gaseous pollutants like NO2, SO2, CO2, etc. Several pieces of evidence have been found that Washington DC is being severely affected by particulate matter which further leads to infection due to the influenza virus and other airborne diseases [31]. The United States urban areas turn out to be one of the prime areas for high particulate pollution (PM2.5) leading to severe cardiovascular or respiratory diseases thus increasing the cases of the rate of mortality [32], [33]. New York City in the United States is prone to high exposure to PM2.5, O3, and SO2 which leads to a dangerous respiratory disorder like Asthma [34], [35]. Similarly, from the above evidences, it is quite clear that the infection of COVID-19 is someway directly associated with the contamination of the ambient atmosphere through air pollution. It is being observed that important populous metropolitan cities in the world get simultaneously affected associated with a coronavirus and airborne transmission of particulate matter or aerosol. The rate of mortality and the rate of positive COVID cases are also associated and linked with the above-discussed factors at the same point of time.
This specific review research paper is mainly dealing with the connection between ambient air pollution or particulate emission and the spread of the SARS-CoV-2 virus through air medium in a global way. In addition to that, the paper also focuses on the preventive measures and technologies that can be implemented to reduce the aerosol or solid particulate emission to further control the pandemic efficiently for both indoor as well as outdoor environment context. On the other hand, this manuscript uniquely notifies a thorough discussion relating to the future risk of COVID-19 during the post-COVID period even after vaccination.
1.2. Root cause and source of ambient air pollution
Ambient air pollution is one of the important growing concerns in the present scenario. Industrial revolution and globalization have impacted hugely over the present civilization for the last few decades. The world health organization (WHO) states that the primary air pollutants include SOX, NOX, CO2, CO, ozone, particulate matter like PM2.5, PM10. Exposure of humans and animals to particulate matter leads to several diseases related to respiratory syndromes. Particulate matter mainly comprises PM2.5 and PM10. Now the path or the trajectory of airborne transmission can be classified into indoor and outdoor forms of transmission [30]. According to a particular study done in China, it is proved that meteorological conditions are prone to air pollution during the winter months as the dilution in pollution effects is minimum due to the fact of dispersion, compared to the other seasonal months [36]. So, it is quite well understood from the fact that indoor, as well as outdoor habitats, are equally affected during the winter months due to airborne transmission. Moreover, according to several scientific communities, anthropogenic emission also leads to severe particulate emission or transmission of air pollutants via atmospheric pathways [37]. A complete connection or link between atmospheric hazards (SO2, CO, NO2, O2, O3, PM2.5, and PM10) and novel coronavirus have been reported by some of the Chinese group of scientists [38]. A report by WHO defines that in 2015 almost 92% of the entire world population is dwelling over the air quality guidelines which should be restricted beyond 10 μg/m3. It is also being observed that densely populated cities in any part of the world are getting prone to such a high level of particulate emission with time. It is being keenly observed and studied that almost 86% of the population in one of the most densely populated zones of southeastern nations of Asia (i.e. India, China, Bangladesh, Pakistan, etc.) are severely affected by PM2.5 emission all ranging above 75 μg/m3. Air pollution counts to be one of the main causes of mortality on our planet [39], [40], [41]. Several previous studies proved that industries like cement industries, fly ash generating plants, sponge iron plants, steel plants, and hydrocarbon industries agricultural biomass burning (stubble burning), transportation or traffic system, power generation plants ( Fig. 2) are one of the primary source of pollutants like SO2, CO2, CO, NOX, etc. since the last two decades or so [32], [42]. The main contribution of outdoor pollution, which is one of the transmission pathways for airborne transmission, turns out to be one of the fatal causes of doubling premature mortality by 2050. The carbonaceous compounds emitted from the particulate emissions are one of the vital causes of toxicity in the ambient atmosphere of the outdoor environment of the USA, Russia, South-Eastern Asia [32]. The process of burning fossil fuel also resulted in huge emissions of NO2 in the atmosphere thus reducing the air quality [43]. It is been observed that due to the effect of prolonged monsoon in sub-tropical countries, humidity is one of the governing parameters that decide the fate of prevailing climatic conditions [44]. The presence of moisture in the ambient atmosphere or humid air is directly associated with aerosol formation [45]. As shown in (Fig. 1(B)), a humid climate increases an added probability of particulate aerosol formation with the SARS-CoV-2 virus adhered to its surface due to viral dispersion, thus resulting in human mortality related to acute respiratory failure. So, these facts accordingly state that subtropical countries like India, China, Bangladesh, and other parts of south-eastern Asia may face possible risks associated with the fatal infection of the novel coronavirus. Some of the primary health outcomes related to household or outdoor air pollution are ischemic heart disease (IHD), acute lower respiratory infections (ALRI), chronic obstructive pulmonary disorder (COPD), lung cancer, etc. [46].
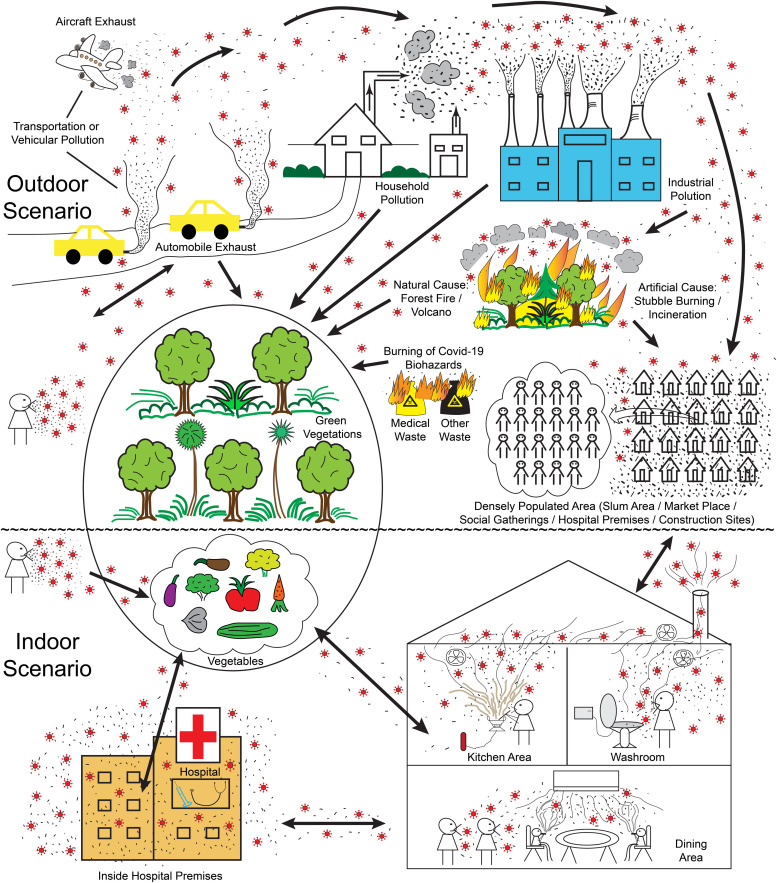
Fig. 2.
Sources and pathways of transmission of novel coronavirus through several routes of air medium containing solid particulate matters, gaseous hazards in form of aerosol leading to indoor in-house air pollution and outdoor ambient air pollution are depicted.
As an effect of all these above discussed sources and causes, the air quality is degrading day by day thus resulting in more and more mortality due to human intervention. Accordingly, it has been scientifically documented that due to the hazardous effect of particulate emission or gaseous pollution, the death rate is almost double that due to the effect of other casualties or accidents [47], [48]. It is also one of the nodal causes leading to several comorbidities, respiratory syndromes [49]. Presently, we are going to discuss more the modes of air pollution that will be affecting the ecology and environment, thus hampering sustainability in the following two ways.
1.2.1. Interior domestic scenario (associated with indoor airborne particulate)/indoor transmission
The form of airborne transmission mainly occurred via viral-contaminated particulate aerosol. The emission of the transmission is primarily composed of human expiration and speech-related matters, thus degrading the atmospheric ecology. The possibilities of viral transmission are mainly through respiratory pathways [50]. There are variable contributions from each route which are quite difficult to predict. The above discussion can be classified into direct and indirect contact for further spread of infection. Direct contact occurs between the infection host and the individual prone to infection whereas the indirect way of transmission can be imparted by means of an object or surface that get contaminated by viral load, known as a fomite [7]. Without the need for direct contact, there are two distinct ways of transmission via airborne pathways. The first mode is via large (> 5 µm in diameter) virus-laden droplets released by infected individuals via a cough or sneeze; the second mode is when a susceptible individual inhales small virus-laden aerosol (< 5 µm in diameter) released during respiration or vocalism [51]. The spread of large droplets is rapidly hindered because of air resistivity and they are eliminated due to a dry form of deposition via the settling effect of gravitation [52]. The small virus-laden particles are somewhat connected with human respiratory discards which could sustain in an ambient atmosphere for several hours [53]. In general, the size of any virus-laden aerosol, as well as the virus itself, accounts to < 5 µm diameter. The indoor air containing inhalable fine particulate matter (< 2.5 µm in diameter) imposes higher or greater risk of infection within confined space like hallways, rooms, restaurants, classroom complexes, etc [54]. Since the size of the coronavirus is small in diameter (having an average size of 0.1 µm), it can easily adhere to the fine dust particles (PM2.5) leading to chronic as well as acute respiratory disorder or syndrome [55]. Moreover, the higher presence of inhalable fine or ultrafine particles in the indoor environment can easily pass through the nostrils or mouth interface finally affecting the lungs or deep respiratory tract. PM2.5 is hugely generated thus diminishing the indoor air quality due to several human activities or interventions such as smoking, fireplace, burning incenses, cooking, fuel combustion on heating, outdoor penetration or ventilation, within confined space of transport vehicles, etc [56]. Although PM10 is also present in the indoor environment, the risk or the probability of infection via PM2.5 is comparatively at a higher level because of its higher surface area within a particular control volume. The winds or turbulent eddies can be one of the primary mediums for transportation and dispersion of such infected respiratory emissions [57].
Other important factors that are needed to be considered are the in-effect aerosol concentration, and the virus-laden aerosol of various sizes within the air medium, the biochemical property of aerosol, the sustainability of the virus within the aerosol, and the lowest concentration of effective viral particles required for possible infection due to inspiration. In a laboratory environment, the half-life of SARS-CoV-2 in aerosol form counts to be 1 h [58], [59]. In a different context, such as variable meteorological factors (temperature, ultraviolet radiation, relative humidity) related to outdoor environmental conditions, the half-life of the virus can be accordingly degraded [60], [61].
The particular concentration of air particulate matter is varying between 108 particles/m3 and 1011 particles/m3 in hugely populated and domestic polluted places by considering the specific air volume during the process of respiration (0.5–1.5 m3/h) [62]. The aerodynamics aerosolization of COVID-19 is quite well justified in closed domestic pathways like hospital premises, medical isolation homes, etc [63], [64]. Another important indoor arena that needs to be considered is the school and classroom premises. Several adverse health effects are noticed among the children and adults within the education hub due to various air hazards [65]. As a result of these consequences, during the post-lockdown phase, all educational institutions including schools and colleges need to adopt several preventive measures against such health hazards. All such preventive measures are discussed in detail in the latter part of the review. Thus, the above data prove that the indoor form of viral transmission is quite significant in terms of population and pollution.
As discussed earlier, the inside atmosphere of the hospital premises counts to be one of the prime zones representing poor air quality including improper air conditioning-cum-mechanical ventilation, insufficient exchange of available oxygen within the indoor arena, as shown in (Fig. 2). Some of the important parameters that govern indoor air pollution are discussed as follows. The most possible activities related to the spread of coronavirus through air emissions are smoking, cooking, activities associated with religious spots inside the domestic hub, gaseous emissions from toilet complexes and fireplaces, etc. They mainly include the infection source is restricted and confined places, subsequent dispersion of the formed aerosol molecules caused due to air turbulence and maximized dilution, the climatic condition which makes the virus stable, and the best favorable domain for its future existence. The isolation rooms, safe home, home quarantine units, or patient’s self-care unit show the enormous presence of infected viral RNA in the contagious indoor environments [66].
The above fact proves that the biological virus adhered over the particulate surface can easily transmit through an indoor airborne pathway, also quite clearly depicted in (Fig. 2). The sample of aerosol shows a massive concentration of SARS-CoV-2 virus inside patient care units having toilet facilities of 19 copies/m3 and 18–42 copies/m3 in medical staff areas containing personal protective equipment composed of discard stuff within two specific hospital arenas of Wuhan, China [64]. The size of the fine particles ranges between (0.2–1) µm which is quite stable in air for several hours as compared to the coarser fractions that impose a direct threat for indirect transmission of viral load through the airway. The fomite way of transmission bears an enhanced risk as the particles get deposited over the surface in the indoor environment [7]. The risk of the contagious spread of virus-bearing aerosol molecules is even more as compared to the outdoor environment in some contexts [32]. A broader spectrum of research is still left to be investigated related to the phenomenon of aerosolization of coronavirus and virus of its kind during regular activities of inspiration or expiration (i.e. respiration), sneezing, coughing, speech in the indoor or outdoor environment [51], [52], [67]. The biological or the physicochemical properties of the virus, the specific rate of infectivity as well as the lifetime of such bioaerosol needs to be properly studied.
The risk associated with the mass spread of infection can be quite efficiently handled by periodic atmospheric ventilation, surface decontamination by advanced techniques of disinfection and sanitization. Thus, future research should not only focus on the investigation of airborne transmission, both indoors and outdoors but also on the physical/chemical/biological/toxicological/virological properties of virus-laden bioaerosol particles. All of these factors properly adjusted for a wide number of potential confounders for infection mediated by SARS-CoV-2, as listed in Table 1.
Table 1.
List of pollutants responsible for airborne transmission of SAR-CoV-2.
| Name of the pollutant | Source | Effects | Refs. |
|---|---|---|---|
| Large virus-laden aerosol (> 5 µm) | Coughing/sneezing | They remain a shorter time in the air and mostly deposited on gravitational settling | [51] |
| Small virus-laden aerosol (< 5 µm) | Respiration/speech | They remain in the air for a longer time and eventually dispersed by winds | [51] |
| They are quickly dispersed and re-circulated in restricted places with poor ventilation (hospitals, quarantine zones, dining area, kitchen area, washroom) | [8] | ||
| VOCs (xylene, toluene) | Oil industry, Fuel-based vehicles | Causes long-term health effects like asthma, nasal tumors, tracheal, bronchial and lung cancer, leukemia | [72], [73], [239] |
| Particulate matters (PM2.5 & PM10) | Industries, stubble burning, transportation, power plants, construction sites, coke oven battery, fly ash and cement dust | Causes carcinogenic effect to human lungs and respiratory system by penetrating the alveolar epithelium | [111], [145], [240] |
| CO | Automobile and transport exhaust | Toxicity leads to the reduction of hemoglobin in human blood | [111], [145] |
| CO2 | Household and greenhouse gaseous emission | Related to particulate emission (PM10, PM2.5) and causes respiratory system imbalance | [11], [42], [80], [241] |
| SOX, H2S | Acid production plant, primary industrial hazard | ||
| NOX, NH3 | Burning of agricultural wastes, incineration of municipal solid waste, research laboratory usage, gaseous emission from anaerobic digestor, septic tank, toilet complex | Causes respiratory tract infection and red blood cell deformability | [11], [43], [111], [242] |
1.2.2. Exterior hotspot zones (associated with ambient atmospheric particulate or gaseous emissions)/outdoor transmission
The universe is suffering from outdoor air pollution for the last century. The deadly effects of particulate emission are majorly affecting the urban lands with very high population density for the last few decades. In this particular global study, we are going to review several pathways of outdoor airborne transmission which is further related to the fast spread of SARS-CoV-2 in form of aerosol or particulate transmission. Here we will be focusing on the real-time source of outdoor air particulate emissions.
Countries like China, India, and some other parts of South-Eastern Asia are some of the prime hotspots related to the industrial sources of pollution. The fatal effects of long term exposure of specific particulates emitted from several industries, traffic, or vehicular transportation lead to several medical disorders [68]. The hydrocarbon industries are one of the major hotspots for atmospheric outdoor pollution emitting a 20% or even higher fraction of volatile organic compounds (VOCs) into our open environment. VOCs are generally classified as carcinogens, irritants having toxic effects on human health in various outdoor, as well as indoor conditions. Exposure to inhalable VOCs leads to fatal lung disorder causing pulmonary dysfunction like asthma, in several climatic conditions [69], [70], [71]. Emission of aromatic hydrocarbon fractions includes xylene, toluene, etc. from several anthropogenic sources like the oil industry, fuel-based automobiles, crude oil extraction units, vehicles, etc. It is experimentally found out that the emission sources vary on basis of location, sources, and concentration of the pollutants [72], [73], [74], [75]. Particulate matters are directly associated with the aerosol and they mainly originated in the outdoor environment where they get linked up with the atmospheric cloud formation (Fig. 2). Accordingly, the particulates in the form of an aerosol, improve their lifecycle by diminishing the global air quality and exhibiting the process of precipitation, lightning, cloud formation, etc. thus creating a global impact on the environment [76], [77], [78]. It is also found that even in coke production in coal industries, cove oven batteries of the steel industries turn out to be one of the primary sources of unknown particulate matters. Coke oven gaseous outlets have vast toxic and carcinogenic effects over life forms. These particular zones are demarcated as hotspot zone for air pollution as local residents face lots of issues related to the unpleasant smell, fumes, odor, smoke, SO2, and dust emissions [79]. The percentage of carbon accounts for 34% of the entire composition of the particulate matter within the automobile exhaust. Carbon-containing aerosol is also present in air pollution sources like industrial emissions, aircraft exhaust, tire dust, automobile exhaust, diesel exhaust, etc. in form of particulate matter [80], as depicted in (Fig. 2) particular study was done in 1982 showcases the fact that some of the primary emission sources are directly connected to the combustion of fuel, coal, oil and refuse. At the same point in time, they are even associated with marine aerosol, soil dust, motor vehicle emission, etc. [81]. Burning of the agricultural wastes or stubble burning also counts as one of the significant sources of primary gaseous pollutants. This mainly leads to be the important factors playing for global climate change in terms of temperature rise, global warming, etc. causing overall environmental change [46].
A remarkable study has pointed out the direct association between the spread of the COVID virus and particulate emission [38], showing a direct correlation between how air pressure and wind speed are directly connected with the dispersion of atmospheric pollutants in form of aerosol emitted from various sources. So, it is clearly and scientifically proven from the above fact that outdoor air transmission is directly associated with several key factors affecting our mother earth like wind speed, relative humidity, temperature, and air pressure. A distributed lag non-linear model helps in finding a complete linkup between people getting hospitalized due to respiratory syndrome and the spread of PM2.5 or PM10 [82]. The primary cause of fear lies in one of the studies done by [59] which shows that COVID-19 is one kind of respiratory syndrome and the SARS-COV-2 remains stable in outdoor atmospheric air for several hours. Moreover, as we know the spread of the disease or infection can occur in an indirect manner, where the atmosphere acts as a medium for transmission.
In the outdoor scenario, the transmission of infection occurs via droplets or aerosol routes where the aerosol adhering fine particulates can disperse in the ambient atmosphere and accordingly can sustain for several hours or distances. In the later part of the transmission, it is noted the inhaled virus now affects the human being having comorbidity or respiration problem from beforehand causing the dry cough, high fever, etc. [83]. It is scientifically shown that the settling velocity of such airborne particles is very low in any prevailing atmospheric condition which accounts for (2.8 × 10−5 m/s–1.4 × 10−4 m/s). In outdoor atmospheric conditions, the typical velocity of the wind or air is about ~ 1 m/s horizontally and ~ 0.1 m/s vertically. As a result of prolonged mixing in the air due to the effect of viral dispersion and presence of moisture in the ambient air, the residence time of virus bearing aerosol or particulate matter bound aerosol accounts for several hours to settle down, in accordance with the prevailing climatic conditions [75], [84], [85].
Population mobility and density of population are also one of the significant reasons for the regular spread and infection of such a novel virus in the outdoor environment [86]. Emissions from traffic and vehicles account for about 31% of the entire primary level of organic particulate matter. Wood burning, coal combustion for cooking, thermal industry primary input contributes to about 10% of entire PM emissions in the globe (Fig. 2), which is even more effective during the winter months [75], [87], [88]. It is being keenly observed that in the troposphere, due to the effect of aerosol nucleation and diverse climatic condition, new particle formation takes place accounting for about 50% of total aerosol production in the outdoor environment. The major part of research related to environmental study reveals that a huge fraction of particulate matter is originated from the new particle formation [89], [90].
Another important area which can also be denoted as a prime source of virus spread in outdoor context is burning or incineration of biomedical waste hazard as shown in (Fig. 2). This actually leads to a huge spread of viral load via air medium during the incomplete process of combustion or incineration of biomedical waste. One of the main concerns is the mass generation of COVID waste from hospital arenas, quarantine houses, or isolation wards to the outdoor environment in form of medical waste or miscellaneous or other waste which is even hazardous in nature [91]. The previous evidences have been found that incineration of municipal solid waste or biomedical waste leads to the large production of particulate dust matters associated with toxic organics like dioxin ash compounds or furan thus further degrading the endocrine system or immune system of the human lifecycle [91], [92], [93]. In general, the byproduct formed due to the incineration of municipal solid waste which may even contain biomedical wastes leads to the large production of hazardous pollutants. This accordingly relates to a higher release of hazardous or toxic air pollutants degrading the human life form [94].
The scientific community should give more and more focus on the source of outdoor environment pollution which is directly associated with the widespread of the COVID-19 virus. The ultrafine or fine particulates referred to as PM2.5, bearing particle diameter less than 2.5 µm, holds higher surface area which is quite capable of damaging the cellular DNA of the human lifecycle. Moreover, it is studied over the years that the finer particles are prone to greater damage over the environment as compared to the larger particles [95], [96], [97]. A report by the World Health Organization showed that over 8 lakh death were encountered by 2005 due to the worst outdoor air quality [98]. A list of possible pollutants that are responsible for airborne transmission of SARS-CoV-2 is entered in Table 1.
1.3. Pathways/routes of leading airborne transmission of particulate matter and SARS-CoV-2 virus in the natural environment (indoor cum outdoor)
In this specific section, we are about to discuss the routes of airborne transmission of air pollutants cum COVID-19 virus. (Fig. 2) details us about all possible pathways of transmission related to the specified virus spread in various routes including indoor as well as outdoor modes of transmission. This figure makes us aware that even after proper trial and vaccination of COVID-19 or after its availability in the open market, we should be quite aware of the consequences during the post-COVID scenario. We should ensure that the post-COVID effect should not hamper the human lifecycle. (Fig. 2) shows all the possible ways or modes of transmission for both airborne particulates as well as the potentially dangerous coronavirus in both the outdoor and indoor contexts. The outdoor mode and source of transmission tell us the most probable pathways of the spread of the virus which imposes a threat to the human life forms. They include densely populated places of mass or social gathering, hospital premises, slum areas, market places, hallways, industrial zones, massive effects transportation or vehicular pollution, household pollution, forest fires (natural/artificial), natural volcanoes, burning of agricultural (stubble burning) wastes, burning of bio-medical wastes, etc. (Fig. 2). On the other hand, the indoor pathways or source of transmission includes inside pollution domestic household premises like cooking, smoking, infectious gas emitted in form of aerosol from the bathroom complexes or sanitary areas, normal breathing or respiration (inspiration or expiration), dining/drawing room areas, inside hospital premises (more number of people in confined spaces), etc. (Fig. 2).
As mentioned in brief, we have already discussed in detail all possible pathways in the previous section on basis of the indoor house and outdoor airborne pollution in several entities relating to coronavirus spread. A particular model development shows that the amount of greenhouse gas emissions including higher fractions of CO2 release due to land conversion or agricultural expansion which could dramatically change the global environmental conditions [99]. It is being predicted that the CO2 emissions will increase 5 times than the present times by 2100 [100]. This might be one of the primary causes of the additional spread of any virus through the airway thus infecting human sustainability gradually.
It is well known that pathways of transmission are occurred by both nose and mouth (Fig. 1(B)). It can also be occurred by man to man transmission (Fig. 2). The spike protein (S) present on the surface of SARS-CoV-2 mainly characterizes the virus, which primarily binds with the ACE2 receptor contained in the cells. By the conversion of angiotensin 2, an anti-inflammatory molecule, into angiotensin 1–7, ACE2 helps in the regulation of blood pressure [101]. Age is one of the prime factors that lead to imbalance and instability in blood pressure. Accordingly, ACE2 receptors are expressed at a greater amount in the human biological system which is directly associated with the aging effect. This increased expression of these receptors leads to an increase in the targets that allow access to the SARS-CoV-2 virus [102]. To reduce the severity caused due to the damage of the lung having root cause as hyperoxia, ACE2 needs to be activated. Several scientific pieces of evidence have been notified where the previous result of respiratory organ damage is occurred by further inhibition of oxidative stress and inflammatory response. The pathway of the inflammatory response can be inhibited by ACE2, thus inhibiting the intracellular signal of NFKB (nuclear factor kappa-light-chain-enhancer of activated B cells). The pathway of the anti-inflammatory response can be further activated by NRF2 (nuclear factor erythroid 2-related factor 2) which acts as a protective protocol to combat ROS (reactive oxygen species) [103]. As a result of all these physiological processes, there is an increase in the number of ACE2 receptors which further leads to the possibility of infection via SARS-CoV-2 and its related virus. In addition to it, when SARS-CoV-2 is bound to ACE2, the activity of the receptor gets blocked accordingly. This results in destroying the immune system of human physiology due to inflammation and further progressing towards premature deaths caused by SARS-CoV-2. Polluted air contains high levels of different particulate matter and gaseous pollutants. Prolonged exposure to particulate emission by PM2.5, PM10 results in triggering of inflammation, oxidative stress. In addition to that, particulate emission also exaggerates the bimodal pathways related to the responses of NRF2 and NFKB [104].
The significance of ACE2 is mainly related to the activation of NRF2 (anti-inflammatory pathway) and the deactivation of NFKB (inflammatory pathway). This is done to ignore the response of deregulated inflammation. On binding with ACE2, SARS-CoV-2 changes the mechanism. In accordance with the exposure to PM2.5, over-expression of ACE2 is observed, which finally increases the probability of SARS-CoV-2 infection. Thus, ACE2 is the key receptor molecule for virus entry [102].
1.4. Combined effects and risk factors related to air pollution and SARS-CoV-2 over the global environment
Acute respiratory syndrome can be occurred by both air pollution and SARS-CoV-2. Exposure to particulate matter induces various acute and chronic lung infections, thus leading to an inflammation risk along with an increase in the high level of cytokine [105], [106]. After attacking ACE2 receptors, SARS-CoV-2 further increases the inflammation, leading to multi-organ damage, causing death.
There is a correlation in a positive way between PM exposure and virus infections in the respiratory tract infection due to viral load. Due to the smaller dimensions of PMs, they can be inhaled easily. A large number of PMs can be inhaled due to repeated inhalation, causing damage to the lung. The PM exposure for the long term induces complete systematic damage [107]. At the same point of time, it is also very much necessary to address the synergistic effect of both virus-laden PM and virus-laden gaseous pollutants. Particular research carried out by a group of scientists in China, shows clearly that the combined effect of both virus-laden PM and gaseous pollutants can be even more drastic on basis of toxicity, and its hazardous effect. Influenza virus and other viruses of its kind can easily combine with PM and SO2 gas, PM and NOx, PM and O3 through aerosol mode, which accordingly results in several acute diseases like influenza virus diseases, COVID-19, tuberculosis, ischemic heart disease, stroke, etc [108]. In fact, the synergistic effect of both PM and gaseous pollutants singly is only harmful, so it is well understood that when the viral infection factor gets associated with it, it is even more lethal and prone to infection. It is quite important to bridge the gap between air pollution and the spread of viral infection which is mainly being studied and reviewed in this paper. The high-end exposure to prolonged air pollution and the spread of novel corona combinedly increases the rate of mortality due to its root cause. The regions with high air pollution index (API) showed double the chances of death as compared to the areas with a low API index [109]. The compromised cells will be invaded by respiratory viruses, pathogens when the subjects to infection are exposed to PM for a prolonged time. It is being observed that both in humans as well as experimental models, PM exposure affecting the lungs occurs via two mechanisms. Firstly, pollutant exposure induces the generation of free radicals inducing oxidative stress, causing damage to the cells. Secondly, the immune cell activation is due to PM induction and thus leading to further inflammation [110].
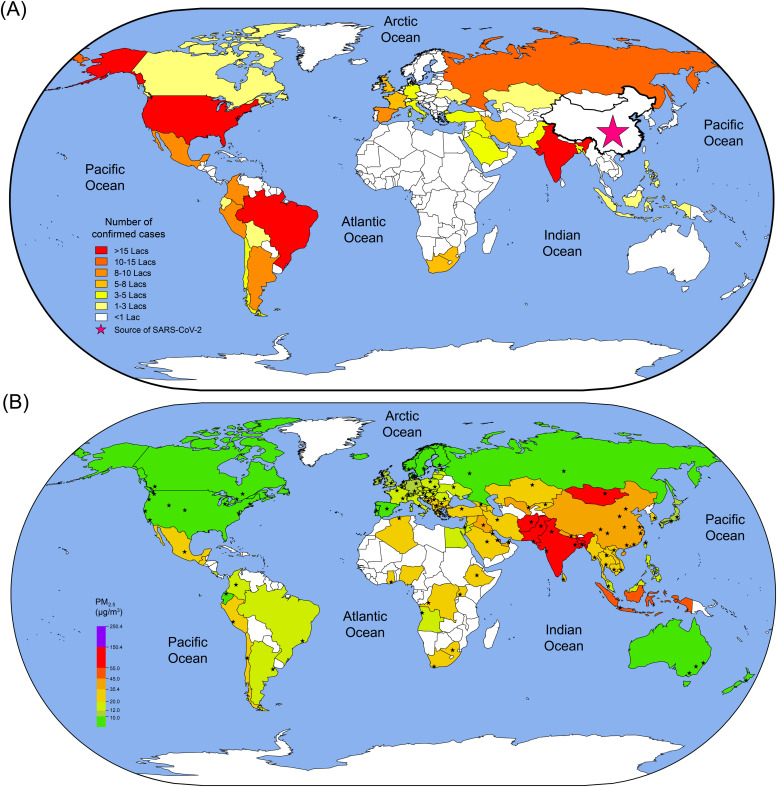
COVID-19 is already a fatal disease, plus, based on 2019–20 data provided by the World Health Organization and World Air Quality Report in ( Fig. 3), the current status of air pollution is dreadful. The higher limits of atmospheric pollution for the last few decades have made the issue of the human population prone to COVID-19 (long-term exposition) and the virus sensitivity, which is connected to the high level of particulate emission in the period during the time of virus origination (short-term exposition). The chronic or the acute effect related to particulate emission includes frequent hospitalizations and rate of mortality. This accordingly affects the cardiovascular and respiratory systems, leading to various issues, pathological infections including carcinoma [111]. Acute respiratory diseases are the main effect of the ambient air pollutants thus leading to premature deaths over the level of two million annually worldwide [112]. This is high time for all of us to be aware of the present scenario and be extra careful; otherwise, the situation will worsen.
Fig. 3.
Global overview of the spread of SARS-CoV-2 infection and ambient air pollution. (A) Map depicts the number of confirmed COVID-19 cases by country. (B) Map represents country-wise average PM2.5 exposure (µg/m3), as calculated from available city data and weighted by population. The data is shown here as of Oct. 15th, 2020 from the WHO [244] and World Air Quality Index (AQI) report of 2019–20 [245], [246].
To decrease the number of new infections and fatalities during the COVID-19 pandemic, a strict lockdown had been imposed. A particular study by the reputed publication house of Cell Press shows the shivering probability of an increased rate of COVID-19 fatalities or mortalities in the United States due to the root cause of air pollution [113]. Since the USA has been one of the leading nations for CO2 emissions in the world for the last few decades, so it is quite necessary to address the combined risks related to hazardous gaseous pollutants adhered to corona molecules immediately [114]. On 19 March 2020, an interim report has been issued by the World Health Organization stating when and how to proceed with the lifting of the deconfinement policies [115], [116]. But, in the post-lockdown scenario, re-allowing the mobility of a large number of populations might increase the risks of new infections and fatalities [117]. In the absence of a vaccine or effective antiviral treatments, recurring epidemic waves may occur and lockdown with longer times may lead to more delay of returning waves. Consequently, the rate of air pollution will again be triggered to its previous condition. Therefore, the situation might worsen, since the infection scenario of COVID-19 is getting worse day by day. Since the genetic variants and high genetic mutations of SARS-CoV-2 isolated from different regions and population densities are different, therefore its potential impact is unknown to be estimated. The countries like India, the USA, Brazil, South Africa, and Russia, the number of cases is increasing, as shown in (Fig. 3). As of October 15, 2020, the total number of confirmed cases is 38.4 million, out of which 1.09 million people are deceased [118]. This indicates that the novel virus-like corona can sustain even future times.
The effect of the corona is the highest in India, due to its population density, which is already mentioned in (Fig. 2). Also, from both the maps shown in (Fig. 3), it has been observed that the highly populated areas are affected the most. Due to the population, a huge number of aerosols are formed as a result of inhalation and exhalation. From the effect of pollution, a large number of particulate matter or gaseous pollutants are formed. Together, population and pollution generate a huge number of particulate matters covered by aerosol. Additionally, SARS-CoV-2 combines with aerosols and particulate matter, and a large number of this combination are inhaled. Therefore, population, air pollution, and COVID-19 – the combined effects will be dangerous and lead to a greater number of fatalities in near future.
1.5. Future of novel coronavirus or possible risk and danger associated with the post-COVID-19 scenario (till or even after vaccination)
It is quite important to study matters related to the future posing threat during the post-COVID time. It has to be taken under full consideration that what all factors might play a significant role during after effect of the COVID-19 virus. Moreover, several groups of scientists and researchers have deeply studied the fact that the COVID-19 virus has drastically mutated over the past few months and will be changing its characteristics more in this due course of time.
This particular virus or pandemic is quite unique from the past form of diseases because the initial stage of the virus was very weak in nature. Accordingly, with time, this specific virus has genetically mutated itself and can survive in any critical atmospheric condition or extreme environment. This particular genetic drift helps the virus to spread quickly over time and on the other hand, and the much-awaited vaccination also depends on several trials which would take a lot of time to normalize the situation. In addition to that, the vaccine should be developed or implemented on basis of the current modified and genetically mutated virus rather not the initial one which might fail the vaccination [119], [120]. The development of vaccination is a time-consuming process as it is based on several human clinical trials [119]. Medical history proves that for the last few months several patients were re-infected by the acute respiratory syndrome of COVID-19 for a consecutive time which proves that the virus gets reactivated in the same biological system thus degrading the immune system of an individual [121]. Moreover, it is quite difficult to predict the complete clearance of second-time reoccurrence or re-infection possibilities within human biology. It mainly depends on several cell-mediated factors associated with the new surge of the COVID-19 virus. It is medically proven that the remaining of the viral RNA (ribonucleic acid) is detected in the respiratory samples even after 6 weeks of cure [122]. It is also clinically proven that due to prolonged use of antibiotics or drugs, the immune system of that particular individual degrades with time, which triggers the reactivation of the COVID virus rather than working over its complete clearance or impairment [123], [124]. It is being observed that a specific study on COCOREC (Collaborative Study COVID Recurrence) says that there is a huge probability of the COVID-19 patient getting affected for a second time even after 21 days of the first onset. It is also noticed that the reactivation or recurrence of the virus including all kinds of clinical data and virological history of the patient. The reactivated virus acts as asymptomatic in nature posing more risk to the human environment thus making it more unpredictable. The rate of reactivation of the novel COVID-19 virus depends upon factors like virological factors, the status of host and variants, or the level of suppression of the immune system of an individual [125].
A particular re-infection study was done and implemented over a group of rhesus monkeys. Initially, four of them got infected with SARS-CoV-2. All of them confirmed recovery but two out of them got re-infected with the virus after confirmed recovery. They didn't even showcase any kind of sign or symptoms of the recurrence of the disease [126]. There are several medical evidences published in the general bulletin that proved that recurrence or second wave of coronavirus has already started. This will actually impose huge prolonged health effects on mankind having devastated outcomes of virus outbreak for another few years to come [127]. In the present as well as in the future scenario, it is found that the generation of biomedical waste related to infectious COVID-19 biohazards will be a huge problem to handle. There are several techniques to control or reduce the volume of such solid waste such as incineration using an advanced associated technique of high temperate pyrolysis or microwave heating [91]. On the other hand, it is observed that these devices produce highly toxic organic fractions of dioxin particulates or unburnt viral load in the ambient atmosphere thus leading to further airborne-transmission of toxic particulate dust cum infection [92]. To handle such a nuisance, several air pollution control devices are being proposed to monitor and reduce the drastic effect of pollution. The proposed devices which may operate efficiently and critical limits of gaseous emissions are dry, semi-dry, or wet scrubber, fabric filters, bag filters, electrostatic precipitators, cyclone separators, etc. [93]. These devices are discussed in detail in the latter part of the study in the controlling or prevention section of airborne transmission. Particular research in Portugal details us that this kind of RNA virus is very difficult to be completely eradicated. Due to the capability of the high rate of mutation and compatibility at extreme climatic conditions, it holds the characteristics of antigenic variability thus weakening the immune system of an individual making him or her prone to infection. In the case of transmission of this virus, it mainly transmits through mucosal membranes and accordingly causes multiple infections in several individuals of a specific community. In addition to the above-discussed hypothesis and clinical evidences, a huge amount of genetic diversity is found in such novel viruses which can even lead to carcinogenic effects over human organs due to the further cause of infections [128]. It is also studied that if the viral load of infection is too high or if the diverse variety of the virus is present, then accordingly it results in reactivation of the dangerous virus despite the implementation of various antiviral therapy [125], [129]. One important research study says that the pandemic situation can continue until the end of 2024–25 in various modes. The resurgence of novel coronavirus is possible and can transform into the form of an influenza pandemic thus leading to enter the regular circulation stage among humans. It can transmit in the form of betacoronavirus in accordance with the annual, biennial, or occasional cum periodic outbreaks [130]. Moreover, a recent study and analysis done by the scientific community of Spain also published in the ELPAIS Society Reports have shown that even maintaining the social distancing norms, avoiding public gatherings, wearing masks will not be enough to prevent us from the risk of contagion or spread of infection. In addition to that in the upcoming winter months, the continuous ventilation will be quite uncomfortable leading to the high risk of infection within confined spaces. The prolonged exposure to such a highly infectious virus can be even more dangerous and cannot be prevented by basic control measures [54]. In the present or the future post-lockdown period, the world is and will be encountering a higher risk of getting infected because of the reopening of bars, restaurants, cinema halls, theater complexes, educational hubs containing confined classroom complexes, etc. As because the deadly virus can easily transmit in form of aerosol or particulate matter even due to the common human activities of breathing, speaking, and shouting, the immediate resumption of such confined indoor hall complexes should be avoided, proper ventilation cum air circulation avoiding recirculation should be adopted, etc. [54].
We are completely unaware of the future of seasonal and environmental factors playing an important role in the spread of novel corona. So, it becomes too difficult standing on the present times to predict the post-recovery and the immune system development in the entire globe. The above discussion proves that the future spread and existence of coronavirus as a post-pandemic depends on the effect of seasonal change, short to the long verse of immunity, and amount of cross-immunity factor [130]. In order to handle the cases of COVID in a much more efficient way, the social distancing norms and regulations including contact tracing and quarantine modules should be followed until proper health care services with critical care units are properly developed in all parts of the world by 2022 [131]. Moreover, the development of vaccines will be a prolonged process as the process imposes several challenges because it will take almost 8 months to 1 year to successfully accomplish all stages of clinical trials like 1st, 2nd, 3rd stages [132], [133]. It will be really difficult to get the appropriate full-length protein, which might be responsible for some medical adverse effects causing further lung complications. In addition to that, the period of potential immunity after vaccination is also not clear [133]. In addition to these above documentations, there is some news bulletin published by WHO and some other news reports which clearly state that no vaccine for COVID-19 will work properly in the upcoming future [134]. A fair process of global vaccination should be implemented to prevent mal piracy of vaccines. We have to keep in mind that initially, the developed vaccine will not reach equivalently to every individual of the world at the same point in time. The vaccination may affect different biological systems differently staying in different parts of the planet. At the same point of time, we have to remember that the mass production of vaccines has never been done before for the entire globe at the same time [133]. Therefore, failure of clinical trials and implementation of successful vaccines, scaling up for mass production or commercialization, or equivalent distribution throughout every part of the globe will be a huge problem at the initial phase, which is quite expected. On the other hand, some of the reputed journals have also reported full ambiguity about the success and efficiency of first vaccine implementation. So accordingly, it is suggested to have mass production of doses of vaccination for complete eradication of the pandemic situation [135]. One of the important guidelines for decreasing the timeline of successful vaccine production for emerging infectious disease (EID) is to quickly find out the route or pathway of transmission (air or water) of SARS-CoV-2 [136].
So here in this specific research model or review article, we have tried our level best to make every individual aware of the most probable way outs and the danger related to the transmission pathways of the COVID-19 virus.
2. Probable engineered technologies for control of aerosol cum particulate matter & gaseous emissions from ambient atmosphere
The implementation of several engineered devices for control of air pollution will be most effective for the eradication of such COVID-19 virus from the ambient atmosphere. Various methodologies have been used to date for reducing the effect of particulate emissions. We have classified the control mechanism on basis of outdoor and indoor transmission of the target virus and fine particulate matter (PM2.5). The proposed devices related to the control of SARS-CoV-2 based on indoor and outdoor transmission are discussed below.
2.1. Control mechanisms for indoor transmission
Indoor house air pollution is also one of the main concerns of the 21st century. The particular section of the study mainly deals with the control mechanisms associated with the control of indoor particulate or aerosol emission in the in-house domestic environment. The kitchen or cooking space within a house is considered as one of the prime hotspots for carbon emission due to the cause of the burning of several materials or edible oils. Moreover, during the winter months or in cold countries, the household fireplace also counts to be a prime source of pollution. Several activities of human beings like smoking, coughing, air pollution inside the bathroom complex, etc. are considered as the main source of aerosol formation or generation of smoke dust and harmful gaseous components. Thus, there is an urgent necessity to curtail down the air pollution level to reduce the aerosol formation which finally leads to a high chance of spread of SARS-CoV-2 adhering to the surface of aerosol and particulate matter. The probable or possible solutions to such problems are listed below.
2.1.1. Household air purifier
The present era is seeing a huge application of indoor air purifying system. There are several types of indoor air purifiers. The ionization air purifier is mainly applicable for the mass removal of aerosol from the indoor atmospheric condition. It is being observed that it has a specific capability of removing aerosol particulate matter related to respiration ranging less than 2.5 µm or ultrafine particles having a size less than 0.1 µm. This specific kind of air purifier works in association with the ventilation system and helps in removing the unsaturated format of volatile organic compound (VOC) [137]. The real-time indoor air monitoring within the human breathing zone, as well as the reduction of respirable aerosol, leads to minimal exposure to dust particles, aeroallergens, airborne viruses, and bacteria (microorganisms) due to mass usage of various ionic air purifiers. This advanced model of indoor air purification device is considered as one of the best technologies for collecting almost 100% of air particulate matter having a size of (0.3–3) μm within residence time of 10–12 h, whereas 90% removal within 5–6 h only [138]. The emerging threats of bioterrorism lead to several outbreaks of such pandemics in the present century which rises the present need for proper indoor air cleaning or maintaining pure air quality by using several air monitoring and cleaning system like the domestic air purifier [138]. As it is clearly and scientifically proven that coronavirus can live in aerosol particles for multiple hours [59]. Moreover, several pieces of evidence have been found that this kind of novel virus can be widely spread through air medium up to 4 m in the hospital premises [64], [139]. This kind of virus can vastly distribute via bio-aerosol coming out from human exhalation [140]. So keeping the above facts in mind, household indoor air purifiers are really important to be installed to minimize the risk of infection due to exposure to particulate matter and virus-laden aerosol as shown in ( Fig. 4). These kinds of air purifiers generally help in the process of disinfection, filtration of exhaust particles, and local pollutants for further combating the novel virus during the crisis period of such a pandemic. The air purifier is one of the most efficient green technology for household air purification within the confinements of the house arena [141].
Fig. 4.
Preventive control measures to combat airborne transmission of novel coronavirus through air medium. Environmentally sustainable green technologies to fight against outdoor and indoor mode of particulate aerosol transmission are shown. Conventional cum modified wayouts for particulate matter (aerosol) collection are depicted.
2.1.2. Ventilator & ventilation system
The ventilation unit or system is mainly applicable for maintaining clean air circulation within the indoor house from the outdoor environment mechanically [2]. When humidity or the presence of moisture is there inside the indoor environment, it leads to fungal growth or particulate house dust thus leading to respiratory problems in humans. Domestic ventilation is somewhat different from a hospital or artificial ventilation. The ventilation system reduces respiratory hazards by increasing the rate of ventilation [142]. The process of house ventilation also helps in controlling the dangerous disease of asthma and allergies caused due to home dust particulates. This specific mechanical heat recovery ventilation system is capable of reducing the in-house relative humidity [143]. An advanced indoor ventilation system was designed containing a dielectric barrier discharge methodology and a UV-photo catalyst filter for advanced removal of gaseous pollutants and particulate dust. Almost ~ 80% of average removal was achieved within 5 h [144]. We already know that one of the prime issues of a high-rise building is improper air circulation and due to stack emission i.e. gaseous pollutants or particulate dust exposure, it provides an unhealthy atmosphere to the indoor air quality [144]. The in-house ventilation is required because of several household activities in our daily lives like cooking, smoking, etc. (Fig. 4). The harmful gas of carbon monoxide (CO) is generated inside the house environment due to the burning of cigarettes and smoke generated out of it, leading to particulate matter ranging between (0.05–1) μm. So it is very important to monitor and control indoor air quality cum pollution by increasing the rate of ventilation thus decreasing the rate of smoke generation [145], [146]. Some of the significant precautionary measures related to airborne transmission of infectious COVID-19 virus related to natural ventilation are maximizing the rate of ventilation, giving enough provision to natural ventilation, reducing recirculation of indoor air [147]. The hospital ventilation is also category indoor house ventilation which is extensively used to provide life support to serious patients suffering from the acute respiratory syndrome, used in hospital emergency, general ward, clinical areas [148], [149], [150], [151]. The turbulent air ventilation system is applied in the operating theater of the surgical area of the hospital premises to reduce bacterial contamination mainly affecting the patient’s skin, mucous membranes, etc. [152]. Since it is being scientifically proven, that COVID-19 has a half-life of more than an hour and even several days or in general any of the airborne pathogens can remain stable in ambient atmosphere, so it is very essential to bar the spread of this specific infectious disease [2], [59], [153], [154]. The artificial or mechanical ventilation constitutes mechanically providing the ventilated air via several operations of heating, ventilating, and air conditioning which is also referred to as the HVAC system. This system is dedicated to controlling the temperature factors, airflow, or distribution factors, and the vital factor of relative humidity which allows the ventilation system to operate in extreme climatic conditions. The recirculation mode makes the system more energy efficient but it is to be kept in mind that recirculation of air should be always associated with the disinfection process to eradicate each and every chance of airborne infection [2]. So, from the above evidence, it is being quite efficiently proved that ventilation (both mechanical/natural) support along with the disinfection process is very much required to control the indoor air quality and save the community from the spread of such an infectious novel virus.
The discussions in the above section detail us about the probable control technologies available for reducing the airborne emission of aerosol particulates along with the novel coronavirus within a short and confined environment of human living or survival, which is clearly depicted in (Fig. 4). When our home or interior or domestic atmosphere gets protected first from severe exposure of infections, then only it is possible to prevent the exterior environment from contamination in a slow and gradual process.
2.2. Control mechanisms for outdoor transmission
In this particular section, we will be mainly focusing on the exterior environment pollution controlling devices that have been benefitting mankind for the last few decades. These devices are considered as one of the prime devices for reducing the limits of ambient air pollution due to particulate, aerosol and gaseous emissions. The proposed devices discussed below can be implemented for controlling the aerosol emission primarily, further reducing the risk associated with viral transmission. They are detailed as follows.
2.2.1. Scrubbing technology
Scrubbers are one of the basic devices used for controlling air pollution limits shown in (Fig. 4). This is also a conventional mechanism used for removing fine dust particulate matter ranging from PM2.5 to PM10. Scientists have observed that highly efficient removal of fly ash particles accounting for 99.91% in an aqueous medium is achieved. The mechanism of the self-primed venturi scrubber also proves to be low cost and can be used for the target compound removal within a short retention time. This particular device is quite compatible with human use and at the same point of time, it works quite energy-efficiently than the conventional system [155]. This has been experimentally proved almost two decades ago that self-primed venturi scrubber works quite efficiently for aerosol collection [156]. This kind of mechanism is most ideal for separating the aerosol or fine dust particles from the cleaner gas. The device works in a self-regulatory mode as a variant of a wet scrubber when connected in series. It superbly removes the particulate matter adhered to aerosol from the industrial outlet. All kinds of filtered containment venting systems (FCVS) are applicable for quick control of aerosol matter from the polluted gas stream. In the year 2012, it has been said that the venturi system out any FCVS is the most advanced device for controlling dust particulates and aerosol ranging from (0.1–300) μm [157]. The dust removal efficiency of 99.5% is achieved at a high airflow rate or gas velocity of 220 m/s having an initial dust concentration of (0.1–1) g/m3 [158]. The absorption of gaseous pollutants and dust particulates at a comparatively lower pressure drop proves that the venturi scrubber reduces the work or energy duty of the device accordingly [159]. One investigation in 2020 shows that out of all the wet scrubbing technology, venturi scrubbing technology turns out to be one of the best cleaning devices. This category of a device generally works over the elimination of aerosol in the range of (0.1–100) μm including gaseous matters like CO2, SO2, CO, I2, acid vapors, PM2.5, PM10, etc. [160]. The above technological mechanisms also prove that this kind of device will be quite useful for the removal of viruses adhering aerosol particulates at the same point of time in a much efficient way out.
2.2.2. Cyclone separation technology
The cyclone separator or hydro-cyclones are also quite efficient devices for solid particle removal (Fig. 4). A present study two years back reveals that while the cyclone separator is combined with a cartridge filter, it helps in maximum dust collection in minimal time. The swirling motion within a hydro-cyclone helps the particles to attach to the minute surface of the cartridge filter and accordingly makes the device highly efficient for 99.11% removal [161]. Fu et al. [162] show that hydro-cyclone technology makes a mark of 98.3% removal of dust particulate by reducing the air pollution level to a higher fraction as compared to the conventional cyclone systems. This novel inter-particle cyclone removes fine particles of size 15.7 µm and inlet concentration of 2000 mg/L which proves it to be quite a smart device for the removal of ultra-fine particles thus maintaining the environmental norms and regulation. Axial flow cyclone separator is also capable of collecting and segregating ultra-fine particles in a relatively better way in a specified vacuum condition [163]. The radial velocity and the centripetal force help the particles to rotate at a particular rpm, swirls over the inner trajectory, and separates the entrained fine particulate matter producing a cleaner stream of gas [164]. Several decades ago, it has been established that hydro-cyclones count to be one of the finest technologies for controlling, collecting, and separating dust particulate matter, and aerosol from the ambient atmosphere. Moreover, some of the primary or basic mechanisms involved in solid particulate removal are defined as inertial impaction, atomization, gravity settling, diffusion, electrostatics, interception, sieving, etc. [165]. Due to the induced inertia force acting inside the cyclone separator, the particle collection efficiency increases which make it capable of removing the diesel suite particulate matter from the automobile or transportation sector i.e. outdoor transmission [166]. Several US patents have also been filed in respect of cycle separator or hydro-cyclones for removal of several dust particulates and efficient aerosol removal from the ambient outdoor atmosphere via low-cost methodologies.
2.2.3. Electrostatic precipitator
The process of precipitation of particulates in terms of electrostatics or within a highly developed electrical charge field for enhanced collection of foreign particles [167], as shown in (Fig. 4). In the industrial sectors and power plants, wet electrostatic precipitator has been used for decades for control of particulate emission (sub-micron particles) of PM2.5 and PM10 [168]. Electrostatic precipitation follows the following mechanism and science behind the phenomenon [169];
-
•
Electrical discharge occurs at a high voltage for the collection of highly electrically charged fine dust particles.
-
•
Due to the opposite charge of attraction, the particulates attach to each other and finally get separated on basis of gravitational force.
-
•
The electrostatic force of attraction also helps to clean the surface of the electrodes stacked with dust matters.
We know that the process of coal combustion in any steel plant or thermal power plant is one of the main sources of air pollution due to carbon sources. An electrostatic precipitator is used in such plants to remove almost 99% of coal fly ash emitted into the ambient air in Japan [170]. Wet precipitators are enormously used for collecting the fine solid particulate matters, acid aerosols, and re-entrained particles. A novel approach has been made by the University of Ohio to develop a membrane to address the problem of corrosion in metal plates, to achieve a better removal percentage in electrostatic precipitators [171]. It is well experimentally proven that hydrocarbon particulates likely the diesel particulate matter (20–50 nm) causing adverse effect over the respiratory system, imposing carcinogenic compound of human biology was quite easily removed to > 90% in an energy-efficient way out [172]. In 2017, a particular study has shown that an electrostatic precipitator working at a high-temperature condition is highly capable of collecting the re-entrainment particles associated with high carbon fly ash to about 99.2%, using the conditioning medium as CaCO3 powder [173].
2.2.4. Baghouse filter
This particular type of filter contains minimal mechanical parts consisting of various kinds of collectors made of metallic or fiber materials. Blended fibers are used to design the filters containing minute pore size for advanced filtering of fine dust matters thus allowing the clean stream of gas to pass down the bag meteorology (Fig. 4). The simple mechanism of vigorous shaking and due to the effect of gravitation, pulse jet, sonic, or passing reverse air, accordingly allows the dust effluent particles to stay back within the interiors of the bag [174]. The gas cleaning efficiency of the baghouse filter in a coal-fired power plant, which is mainly made of a fabric filter, is also over 99% as mentioned by [174]. A particular study over air pollution controlling devices was undergone to keenly observe the pollution index or emission status over Asian countries. The experimental study shows that the baghouse filter quite efficiently removes 99.3% of average particulate matter (fly ash or other particulates) from the effluent flue gas. The bag filter performed much better than the wet scrubber having a clean outlet gas stream concentration of only 0.55 ± 1.28 mg/Nm3 (inlet concentration of 76.6 ± 32.7 mg/Nm3) having a filtration speed of 2 m/min at 108 °C [175]. The fibrous technology including the use of nanofiber materials inside the baghouse filter increases the removal efficiency and makes the system compatible for sustainable for human use. The fibrous filter model also inherits the antimicrobial property for fighting against any aerosol transmitted virus like swine flu, SARS, influenza, other acute respiratory syndromes, etc. present in the ambient atmosphere [174], [176]. According to the Environmental Protection Agency (EPA), on basis of verification testing protocol used by the American Society for Testing and Materials (ASTM)-Method D6830-02 and International organization of Standardization (ISO)-Method 11057, the pulse jet baghouse filter was approved and tested successfully for the removal of PM2.5. According to the norms and regulations were given by EPA and National Ambient Air Quality Standard (NAAQS) for particulate emissions, the fabric filter baghouse could successfully achieve and pass through all the verification standard testing protocols for filtration of particulate emissions (PM2.5, SO2, NOX, etc.) and control performances [177]. A dual baghouse filter system along with adsorbent injection is capable of removing several toxic compounds like dioxin from flue gas effluent having the highest removal of 99.8% to date [178].
2.2.5. Mist separator/spray mechanism/aerosol separator
Mist Separators or aerosol separators are one of the prime devices for particulate matter separation from different phases shown in (Fig. 4). The oil mist or other format of aerosol components leading to high gaseous emissions or air pollution from the outlet of the automobile engine section is mainly controlled by mist separator unit accounting to > 80% [179]. Mist eliminators are used extensively for the separation of liquid molecules from gaseous bulk. This technology indirectly helps in aerosol separation from gaseous matter. Wave plate mist eliminator is another category of aerosol separation system which works efficiently for this specified purpose [180]. Electrostatic mist eliminator is another variant of conventional mist eliminator where removal of particulate matter above 5 µm accounted for > 80% whereas the PM10 removal accounts for about 60% using the flow rate of 4 m/s. It consists of a discharge plate/electrode, collection plate, aerosol spectrometer, etc as its main components which increase the collection efficiency of particulate matters resembling the design prospect of an electrostatic precipitator [181]. The mist eliminators have extensive implications and implementations in any of the acid regulation or acid production plants namely sulfuric acid plants. The mist eliminators work in collaboration with the electrostatic precipitator. The mist eliminators are generally installed in the units like drying tower, SO2 purification unit, absorption towers, etc. [182], [183], [184]. Giffin et al. [185] investigated that high-efficiency mist eliminators (HEME) are mainly used for the removal of solid and liquid aerosols, humid fractions of particle sizes from 20 nm to 20 µm.
The spray mechanisms are generally used or associated with particle removal methodology to get an enhanced removal rate in a short period. All the above-mentioned devices are directly or indirectly associated with the spray system. Moreover, spray units are being installed within a prilled tower or wet scrubber to reduce the emissions of urea or PM2.5 [186]. The application of electro-spray in a spay tower helps in removing the particulate matter < 5 µm having a ratio of liquid to the gas flow rate of 41–84% for an average particle diameter of 0.3 µm [187]. One of the scientific research articles shows that by adopting the spray mechanism, the rain shower model is developed for sustainable and low-cost removal of CO2 and PM2.5 [188]. Thus, this technology is quite well efficient in removing the associated greenhouse gases from the ambient atmosphere. A specific kind of desulphurization wash tower was installed for absorbing NO and NO2 in the desulphurization mechanism for achieving > 95% removal having 50 min of experimental residence time [189]. The spay tower has high thermal stability up to 370 °C having nanofiber air filters which result in the highest removal of PM2.5 [190].
2.2.6. Air pollution monitoring unit
In the present times, real-time monitoring of particulate aerosol data is very much required to keep the environment under complete sustainability as portrayed in (Fig. 4). The particulate matters are directly associated with health hazards and acute respiratory syndrome thus causing respiratory mortality or morbidity [191]. Air monitoring stations are present in several parts of the planet, in the main metropolis to keep a track of the air quality standards. Several low-cost sensors or portable devices are incorporated to study and observe the mass of the particulate matter of varying sizes. To study the characteristics of data of the aerosol particle measurements, the particle assessment provides the spatial resolution and temporal data [192]. In order to develop different kinds of pollution monitoring devices, a machine algorithm along with a case sensitive artificial neural network (ANN) and two variants of the model are mainly used namely univariate and multivariate. This specific model efficiently can monitor data related to SO2, O3, NO2, PM, etc in high air pollution zones [193]. The Shinyei PPD42NS is an efficient device doped with aerosol particle seizer mainly used for particle counting. This particular device is modeled specifically for monitoring and measuring the concentration of PM2.5 having an upper concentration measuring limit of 800 μg/m3 and a lower measuring limit of 1 μg/m3 [194]. The everyday living of human beings is generally controlled in many ways via a wireless sensory network system. Several internet platforms using WiFi modules work via a novel technique developed by the Internet of Things (IoT). This is a specific smart and portable device that gives alarms or warnings when the air quality is very poor by using the sensory signaling systems. Accordingly, the system also allows us to determine and predict the future data of air quality, the pollution route, or pathway on basis of air quality index [195]. A highly sensitive air particulate matter PM2.5 detector was designed specifically for monitoring the everyday exposure to PM2.5 in the ambient air of an industrial park or densely populated zone. This particular device is highly capable of capturing and detecting particulate matter PM2.5 ranging between 6.64 and 55.12 μg/m3 having the output frequency between 0.63 and 4.03 MHz with a sensitivity of 70.287 kHz/(μg/m3) [196]. The air pollution monitoring process is quite important or significant to understand the health of our ambient atmosphere, which makes the human civilization much compatible with the understanding of the system and its easy use along with sustainable living.
2.3. Post purification or best possible associated disinfection process
It is very important to associate a feasible process of disinfection either as a post purification technology or as a technology which can be associated along with the different control mechanism discussed in the above sections in details. It is always to be kept in mind that whether it is an outdoor or indoor control process, a particular disinfection methodology should be associated with it to assure zero percentage of pathogen discharge to certain our environmental sustainability. Several forms of disinfectant dosing or treatment processes can be preferred as a post-treatment mechanism.
All the above-mentioned devices primarily remove particulate aerosol, which at the first stage reduces the high probability of spread of airborne particulate matters or gaseous pollutants from the ambient atmosphere. Then accordingly it if some fractions of viral aerosol still remain, then an associated disinfectant dosing or technique is self-sufficient for the complete removal of pathogenic or viral aerosol. Several technologies like wet scrubbers, cyclone separators, electrostatic precipitators, etc, can be used as pretreatment mechanisms for maximum removal of particulates or gaseous effluents. For example, if we consider any of the wet scrubbing technologies, then the scrubbing liquid used there can be thoroughly mixed with some fractions of disinfectant dosing leading to complete removal of pathogenic aerosol or virus. On the other hand, a separate disinfection technique can also be installed as a feasible post-treatment option. Similarly, some of the other removal methods can also be associated with disinfection methods for the efficient removal of virus-laden air pollutants.
Here we are discussing some feasible or best possible associated disinfection technologies which can fit best to the above-discussed control prototypes. A unique localized ultraviolet waveband C efficiently removes some selected virus or bacterial load or a pathogen-laden aerosol like deadly Coronavirus, Ebola virus, Avian influenza virus, etc [197]. Some of the researches prove that in the case of indoor air pollution control, air purifiers should be installed with separate or self-associated disinfection to combat local viruses within confined spaces to prevent further secondary contamination [141]. The continuous ultraviolet germicidal irradiation (UVGI) or the pulsed UVGI can be used for controlling infectious bioaerosol or virus-laden airstreams to a higher extent. Moreover, the documentation also shows that pulsed UVGI can further treat the remaining viral load from cyclone samplers or membrane filters and completely eradicate it with no further environmental disposal [198]. Vacuum-based ultraviolet photocatalysis is associated with an indoor air purifier which efficiently removes airborne pathogens or viruses accounting for 90% having short retention time [199]. The plasma air sterilizer can be installed within or associated with any air monitoring device or air pollution controlling device to sterilize the effect of any virus-laden aerosol as well as a sampling of specific SARS-CoV-2 virus within hospital arenas [200]. The combined effect of chemical disinfection (using sodium hypochlorite, hydrogen peroxide, and peracetic acid in proper proportions) and ultraviolet irradiation are capable of complete inactivation of harmful virus, bacterial or microbial reduction, etc [201]. The conventional disinfection using combined effects of free chlorine, chlorine dioxide, peracetic acid dosing were used to prevent cross-contamination of pathogenic load in any wash water streams [202].
Above conventional or modified disinfection processes discussed in this particular section are considered quite cost-effective and efficient in terms of complete deactivation of pathogens, viruses, bacterial or microbial loads of all kinds. This kind of disinfection technique can be associated with any of the probable control mechanisms, which can address the complete handling of virus-laden aerosol and its related issues with zero disposal to maintain environmental sustainability.
All the devices mentioned in the above section shown in (Fig. 4) contribute immensely to controlling and monitoring the air pollution or particulate matter in the form of aerosol throughout the entire environment and ambient atmosphere. The above-proposed devices can operate successfully thus fulfilling the aim of our research. The post-removal of aerosol cum particulate matter will accordingly eliminate the target virus at the same time. All the processes should follow a disinfection methodology which will enact and address the minimal remaining viral load as a better post technology. Therefore, these controlling devices will be quite effective in controlling the spread of coronavirus thus hindering the situation of the pandemic. As we know that the root cause of the spread of this deadly virus is also airborne, so it is quite essential to control the spread of nuisance through the air media in a sustainable and low-cost methodology. This actually makes our planet a safer place to address all the factors leading to the present scenario of global environmental change. A list of preventive measures for the control of airborne transmission of SARS-CoV-2 is summarized in Table 2.
Table 2.
Preventive measures for the control of airborne transmission of SARS-CoV-2.
| Mode of control | Probable preventive measures | Proposed mechanism of prevention related to airborne transmission of SARS-CoV-2 | Refs. |
|---|---|---|---|
| Indoor (followed by the process of final disinfection) | Household Air Purifier | Removes VOCs, aerosol particulate matter having a size of (0.3–3) μm | [137], [138] |
| Ventilator & Ventilation System | Removes home dust particulates of size (0.05–1) μm | [146] | |
| Outdoor (followed by the process of final disinfection) | Scrubbing Technology | Eliminates fine dust particulate matter ranging from PM2.5 to PM10 | [160] |
| Cyclone Separation Technology | Removes solid ultra-fine particles | [162] | |
| Electrostatic Precipitator | Precipitates PM2.5 and PM10 by applying an electric field | [168] | |
| Baghouse Filter | Removes SO2 and dust particles | [177], [243] | |
| Eliminates NOX and dust particles | [177], [243] | ||
| Removes dioxin and particulates | [178] | ||
| Mist/Aerosol Separator | Separates aerosol and liquid molecules from gaseous bulk | [180], [185] | |
| Air Pollution Monitoring Unit | Real-time monitoring of particulate aerosol data | [193] | |
| Conventional wayouts | Vaccination & Proper Medication | Boosts the immune system | [203] |
| Use of Masks, Face Shields, Gloves, PPE kits, Soaps, Sanitizers | Reduces the probability of viral transmission through aerosol or air particulate matter | [218], [220], [221] | |
| Systematic Societal Lockdown | Controls NO2 and CO2 emissions and prevents the spread of coronavirus in air medium | [228], [237] | |
| Social Distancing | Prevents the transmission of the virus to stop further infection | [9], [234] |
2.4. Conventional or modified wayouts for prevention of airborne transmission of SARS-CoV-2 or novel coronavirus
We seldom come across such a situation of pandemic or epidemic in a particular century. The entire planet has already experienced such typical conditions in the past centuries. Presently, the human civilization is facing a drastic change in everyday lifestyle. Accordingly, it is a time-taking process to make the human accustomed to such a critical pandemic scenario. So, some conventional wayouts related to prevention has been going on for the last millennium and needs to be modified to make life easier for mankind. In this section, we will be mainly throwing light on those prevention methodologies. They are listed as follows.
2.4.1. Vaccination & proper medication
This category of medical implementation is mainly one format of a conventional controlling mechanism developed by the human race several hundred years ago. Now presently, several modifications have been brought on basis of change in immune system factors of human beings and several other climatic/environmental causes. Since now the present century in the present year is highly suffering from the adverse effects of the COVID-19 virus, so it is very necessary to develop the vaccination for the present pandemic as depicted in (Fig. 4). One of the prime vaccinations that can work efficiently to combat against such a virus is bacillus Calmette–Guérin (BCG). A particular study shows that BCG vaccination is advised by the medical association which can fight against the severity of COVID-19. This vaccination also experimentally proves a 10.4% reduction in COVID mortality [203]. Over the last decade or century, there has been an urgent necessity for the development of vaccination for several epidemics or pandemic disorders like the Zika virus, Ebola virus, Cholera, Small Pox, H1N1 Influenza virus, Spanish Flu, etc. Moreover, the process of vaccine development is not the same for every disorder or epidemic, or pandemic [133]. Another important prospect of a cure for such a deadly virus counts to be a proper drug supply and medication facility for each and every individual of the human race. Some of the possible remedies which could be applicable for fighting against coronavirus are antiviral wayouts like therapeutic antibiotics, the dosage of cytokines and medicines, development of advanced vaccination, etc. [204]. Some of the modified ways of treating the SARS-CoV-2 virus also includes unique technology and therapy related to plasma treatment. This particular virus is attenuated in nature and pathogenicity is difficult to understand. We are quite aware that the entire world is quite concerned about COVID-19 solid waste generated as a biomedical hazard. In order to reduce the huge mass fraction (almost 95% reduction in the volume of waste) of biomedical waste generated, local municipalities are working on the advanced mode of incineration followed by thermal disinfection. The two ways of thermal techniques applied are high-temperature pyrolysis (540–1093) °C, and medium temperature microwave heating (177–540) °C [91], [205], [206]. The high-temperature pyrolysis at 1093 °C is mainly used to overcome the problem of incomplete combustion and complete destruction of toxic substances like dioxin fly ash or viral residues [205]. At last steam sterilization and autoclave, techniques are preferred for the final disinfection of COVID waste [205]. Some other useful techniques used for the disinfection of COVID wastes are chemical disinfection (using vaporized NaOCl, ClO2, H2O2) which quite efficiently kills all forms of airborne virus and bacteria [91], [207], [208]. On the other hand, the symptoms of coronavirus resemble that of common influenza virus-like common cough and cold, respiratory problems, etc. [209]. So, it is very required to work on the advancement of vaccination and medication for COVID-19. The WHO (World Health Organization) has denoted several candidates for vaccination like the health workers or volunteers initially infecting them with infectious RNA and accordingly the process of protein spike technology can be implemented on basis of human safe trials via different phases [210], [211]. The effect of clinical modification also resulted in productive results related to the cure of the disease. These included the use of glucocorticoids for developing the immune system of the patient. Moreover, the use of several medications including beta-blockers, antiplatelet, statin, insulin, oral hypoglycemic agents, etc. used for treating cardiovascular diseases as well as treating the symptoms of COVID-19 [212]. A special kind of antiviral drug to combat the influenza virus named Favilavir in Japan is now being applied for the advanced treatment of COVID-19 in China. In addition to that, the use of hydroxychloroquine and chloroquine was conventionally used for the treatment of malaria and arthritis. Presently they have been modified and used along with azithromycin during the pulmonary and inflammatory phase for the treatment of coronavirus which is under the study and investigation of the US Food and Drug Administration. In China, the use of Tocilizumab, Anakinra, Baricitinib, Eculizumab, Emapalumab lopinavir/ritonavir, and Heparin has been clinically approved for the severity of COVID-19 cases during the anti-inflammatory phases as a therapeutic wayout [213], [214]. The Remdesivir is also another potential antiviral drug against SARS-CoV-2 which has a promising in-vitro drug activity against the target virus [215]. The natural products derived from medicinal plants also inherit some special antiviral effects over COVID-19. The viral 3-chymotrypsin-like cysteine protease also referred to as 3CLpro is a special kind of anti-viral phytochemical drug which enzymatically controls the further mutation or replication of coronavirus and finally hinders the progressive life cycle [216], [217]. The above literature proves the most possible conventional and modified treatment options which are feasible in nature and can be implementable for treatment of the specific pandemic.
2.4.2. Use of accessories (mask, face shield, gloves, soaps, sanitizers, disinfectant spray) against COVID-19
The process of usage of accessories to fight against such deadly virus infection which is even present in the ambient atmosphere is reported as the usage of mask, gloves, face shield (Fig. 4). The specific usage of a mask or face shield reduces the probability of viral transmission through aerosol or air particulate matter or even in densely populated zones [218]. Moreover, wearing a mask or face cover will prevent an individual from the spread of infection as well as prevent him or her from self-contamination via means of air in form of a respiratory droplet or aerosol i.e. from community transmission. At the same point of time number of evidences have been scientifically reported that the number of corona cases was reduced by the constant usage of such precautionary accessories [219]. According to WHO guidelines, several preventive measures like the use of masks or face shield, PPE kits, maintaining hand hygiene by using sanitizers, soaps to stop the transmission of coronavirus in an airborne way through aerosol or direct transmission via direct contact [220], [221], [222], [223]. The three main variants of masks used throughout the world related to protection against ambient pollution as well as coronavirus adhered over the aerosol surface are the N95 mask, cloth cum woven mask, and surgical mask. It is also studied that in addition to liquid disinfection or sanitization (by hand soaps/hand sanitizers), other forms of disinfection strategies like heat, radiation, etc. have been adopted as the second line of defense against infection. Environmental sustainability is also another important perspective that has to be kept in mind while designing or manufacturing the PPE (Personal Protection Equipment) kits including masks, face shields, gloves, etc. [224]. A particular study also shows that the disinfection technology and hand hygiene associated with infection in the hospital premises can be reduced to a large extent. Moreover, lots of evidences or proof have been found that the process of aerosolization through coughing or sneezing leads to the transmission of the disease in the form of intubation or extubation as described by the British Association of Urological Medicines [225]. The effective ways of sanitization are very much effective in reducing the aerosol transmission from a highly crowded area with high population density. The process of sanitization also includes disinfection and sterilization of toilet complexes, market places, hospital and medical premises, crowded public areas having several asymptomatic carriers, where complete evidences were found related to aerosol transmission. Since the aerosol matter can transmit in form of total suspended particles via air medium, or can even transmit via direct contact in form of the deposition so it is very essential to wear a mask, gloves, or PPE kit to prevent an individual from further infection [64], [225], [226]. The alcohol-based hand sanitizers are strongly recommended by WHO for maintaining hygiene to combat the spread of infection. They are mainly being prepared from alcohol-based (> 60% alcohol) ethyl alcohol, isopropyl alcohol, glycerol, hydrogen peroxide (mild/low concentration < 3%) in different proportions. At the same point, we have to think about environmental sustainability and lethal toxicity concerns too [227]. On basis of regulations or norms given by the WHO and US Environmental Protection Agency (USEPA), the production of alcohol-based sanitizers or disinfection sprays are to be mass-produced to prevent life forms in all ways. These are one kind of frontline defense and prevention methods to fight against any airborne transmission or direct contact transmission of the virus as well as air pollutants in the ambient atmosphere.
2.4.3. Systematic societal lockdown and social distancing
In 2020, we the citizens of our planet are going through a tough phase of our life related to the infection source and spread of the COVID virus. So, we have to find out some strategies which will further hinder the process of airborne transmission in various pathways. Since the process of development of vaccination or proper medication is still under extensive research, so systematic lockdown and social distancing norms are to be adopted to bar the deadly effect due to the spread of coronavirus in the air medium shown in (Fig. 4). The prime source and cause of air pollution are due to several activities due to human intervention like urbanization, industrialization, burning of fossil fuel. It is quite well understood that the extended lockdown and rules of social distancing will not only stop or reduce the effects of air pollution but also quite effective in handling the critical airborne transmission of COVID-19 [228], [229]. Societal lockdown is one of the modified wayouts to control NO2 and CO2 emissions related to ambient air pollution. Moreover, during the societal lockdown, except for the emergency services all other modes of portability are completely stopped which minimizes human activities leading to air pollution [228]. A particular study in the US shows that even in presence of 15% air pollutants or fine particulate matter (PM2.5 & PM10), death has proportionally increased. In addition to that, several countries like Italy, the USA, the Philippines, Denmark, Chile, Brazil, Mexico, and Peru have proven the fact that COVID-19 infection has a direct link with air pollution or morbidity [229], [230], [231]. So accordingly it proves that systematic societal lockdown or wearing a mask or maintaining social distance etc. proves to be quite effective and has a positive effect on lifeforms and the environment [229], [232]. The process of gradual or systematic lockdown till mass availability of vaccination leads to temporary (> 40%) reduction of CO2 and NO2 thus enhancing the air quality and health status related to respiratory diseases. Due to initial prolonged lockdown or stage-wise lockdown, the primary source of carbon emissions from the exhaust of fossil fuel, industrial outlets, and vehicular air pollution [229], [233] is reduced. Moreover, in the outer environment air pollution, social distancing is one of the best modes of prevention strategies to defeat the COVID-19 virus spread via air medium [234]. In order to prevent an individual from any mode of airborne transmission, it is very essential to maintain a safe distance of 1–2 m between the infection host and receiver (i.e. avoid direct contact between each other) or social distancing norms should be adopted or work from home during lockdown [235]. Finally, we have to keep in mind that during the ongoing unlock phase or post-COVID lockdown phase, every individual should follow the following steps to curtail the airborne transmission of coronavirus or possibly spread via any other modes of transmission. The ongoing lockdown throughout all parts of the world is actually preventing our mother earth from the curse of air pollution thus presenting or reviving into a sustainable environment [9], [236]. In addition to that, systematic societal lockdown helps in stopping the further spread of coronavirus through air medium thus improvising the global air quality. Moreover, it reduces the consumption of extra duty of electricity to curtail the cost of running the industries or other unnecessary factory units, unnecessary usage of motor vehicles or transportation, or petrochemical oil consumption [9], [237]. They are maintaining social distancing, self-quarantine mode, restrict all format of public gathering, etc. to stop the further infection risk [238]. Moreover, it is very much required to implement all the above preventive measures to tactically handle all difficult situations at various times during such a devastating pandemic.
Therefore, we have to keep in mind that usages of the above accessories have to be essentially used to protect mankind from further infections from the deadly coronavirus. It is also to be kept in mind that the above mentioned advanced or modified or conventional ways should be implemented in an environmentally sustainable manner that should not create any nuisance or complexity among all life forms. The overall environmental transformation should be taken in a positive manner addressing all of its limitations for the betterment of 21st-century civilization.
3. Conclusion
The entire research paper mainly discusses and illustrates the source, root cause of the spread of coronavirus via an atmospheric medium. The above-discussed sources and root causes lead to a drastic change in global environmental climatic conditions. It also describes the best possible preventive measures to stop further transmission of the airborne virus through an aerosol form. At the same point of time, it too reminds and alerts mankind about the future threats that it may pose during the post-COVID times. The probability of vast and fast spread of infection, related health hazards through particulate matter cum aerosol is quite evidential through indoor as well as outdoor environmental routes. Several probable engineered protocols or green technology are demonstrated in detail to understand the mechanism of removal or control or systematic monitoring of air pollutants and viral loads. The world has been previously facing such tough times related to viral attacks even in the past during the pandemic situations of the Spanish Flu, Small Pox, Cholera, SARS-CoV-1, and Influenza Virus. So it is very important to study our atmospheric routes of transmission or probable sites or sources of infection and accordingly look forward to stopping them permanently by using innovative techniques. Even after the installation of such advanced or modified controlling devices (wet or venturi scrubbers, electrostatic precipitator, baghouse filter, mist or spray collectors, in-house air purifier, advanced ventilation systems, etc.), some research gaps will still be present to address in the near future. The post-treatment mechanism might work much better if the disinfection process can be incorporated for efficiently addressing all the probability of further infection spread.
So accordingly, in addition to engineered devices of control, some conventional and modified wayouts like self-isolation, social distancing, systematic societal lockdown, development of safe homes or quarantine centers use of medical accessories (like masks, PPE kits, gloves, face shield, etc.) and disinfection or proper sanitization must be continued to be implemented even after the post-vaccination or advanced medication period. It is being clearly observed that the population is directly associated with the pollution scenario. The minimization of population load needs to be addressed within confinement areas using social distancing norms according to WHO.
The use of the above discussed environment sustainable technologies or green wayouts will not only protect every individual from viral cum pollution threats but also gift us a better quality of living.
3.1. Future scope of study
We have to look forward to investigate the future prospect of the present study of research. It is not only the fact of the future of COVID-19 or SARS-CoV-2, but also any other biological virus in the upcoming times. We have learned a lot from the present pandemic situation. We have to keep in mind the problems that we have faced in the present times. The entire science community should encourage more research related to virology as well as environmental air pollution research. Moreover, we should be competent enough or should mainly focus on the detection of such an unknown virus in future times. The climatic condition of the entire world is changing year-wise. Due to the effect of global warming or the emission of greenhouse gases, the overall temperature of the mother planet is increasing day by day. As a result, the glaciated zones including the polar belts are melting thus increasing the water level leading to humidification or natural evaporation. These facts prove the factors affecting global environmental change. As a result of unwanted humidification and viral dispersion, a large amount of aerosol formation takes place, which actually entrains all kinds of solid particulate matter or gaseous emissions due to the man-made cause of industrialization or other air pollution sources. On the other hand, unknown forms of viruses, as well as bacteria, have an advanced capability of adaptation or genetic mutation under any circumstances or extreme environmental climatic conditions. The above reasons discussed in brief leads to several airborne viral transmissions via aerosol adhered particulate matter or gaseous pollutants.
The entire globe is struggling to fight against novel coronavirus. The processes of prevention against both air pollution as well as virus attacks are more or less equal in nature. So we have to adapt the best possible advanced technologies to combat such pollutants or novel viruses. The development of the natural immune system should be looked over in detail so that human biology should be prepared in advance to fight against it. It takes a lot amount of time to develop a vaccination for an unknown virus or disease. More amount of emphasis should be given on the development of proper natural medication, advanced disinfection techniques to such critical hours quickly in the future rather than giving more stress over the development of artificial medication having lots of side effects or complexities. Modified air pollution controlling or monitoring devices should be installed during the pandemic situation to reduce the drastic effect and fatality rate on mankind. Since the diseases are generally contagious in nature, we have to improvise the facility of hospitalization, increase the number of isolation care units or self-quarantine or safe home units. The process of stepwise systematic lockdown, wearing of mask, gloves, face shields, using sanitizers, adopting self-distancing norms should be implemented all-time to protect any individual from the spread of such a deadly virus through the air medium. The pathways or routes of viral transmission through air medium should be demarcated from beforehand so that the viral loads in aerosol form may be killed on a mass basis regionally. All modes of clinical trials for future vaccination have to be updated or modelled within a short span of time. In addition to it, the number of everyday testing has to be increased for the particular virus infection, so that a greater number of patients can be cured at a faster rate. The proper medication as well as the possible vaccination should be equivalently distributed throughout all parts of the world before any form of mal-piracy could take place. During any pandemic situation, everyone should be quite concerned about the huge production of biohazards. Several preventive measures should be considered for the efficient handling of such disease. At last, virology departments should be uniquely established in every hospital or nursing home along with air purification and ventilation units to get clean purified air throughout the surroundings. The scientific societies have to think in a more cost-effective and environmentally sustainable manner to efficiently handle the problems to prevent our mother earth, and its life-forms from any novel infections or pollution effects to hit the globe in the future times to come.
Funding information
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Authors are thankfully acknowledging the supports and facilities extended by IIT Kharagpur for this work.
Biographies

Subhrajit Mukherjee is presently working as a Senior Research Fellow (SRF) or Doctoral Research Scholar at the Environmental or Industrial Pollution Control Laboratory at the Department of Chemical Engineering in IIT Kharagpur. He has previously completed his Master of Technology (M. Tech.) from the same department at the Multiphase Fluid Flow Laboratory in IIT Kharagpur and was mainly involved in the specific research related to process intensification and two-phase flow in milli-channels. Initially, he has completed his Bachelor of Technology (B. Tech.) in Chemical Engineering from West Bengal University of Technology (WBUT). His present research area is mainly focused or associated with air pollution control cum monitoring, management of hazardous materials, advancement in scrubbing technologies, recycling cum reutilization of wastes at a low cost, etc. He has published several remarkable research outputs in form of conference papers as well as peer-reviewed journals in the above specific fields. He acts as a life member and life associate member of prestigious academic professional bodies like the Indian Institute of Chemical Engineers (IICHE), International Environment Forum (IEF), Institution of Engineers (IEI), International Association of Engineers (IAEng), and many more.

Soumendu Boral presently works as a Ph.D. Research Scholar (SRF) at the Structural Biology & Protein Engineering Laboratory at the School of Bioscience in IIT Kharagpur. He carries research in the areas of protein engineering, biochemistry, and structural biology, with a major focus on engineering a novel functional split enzyme for pharmaceutical and biotechnological applications. In this related field, he has produced some outstanding research works published in international journals and conferences. He has accomplished his Master of Science (M.Sc.) in Biotechnology from IIT Roorkee with a broad field of research focused on biophysics and biochemistry using biophysical techniques. Previously, he had completed his Bachelor of Science (B.Sc.) in Microbiology from St. Xavier's College, Kolkata.

Hammad Siddiqi is currently working as a Senior Research Fellow (SRF) at the Department of Chemical Engineering in IIT Kharagpur and pursuing a Ph.D. He had completed his Master of Technology (M. Tech.) from IIT Kharagpur and Bachelor of Technology (B. Tech.) from Aligarh Muslim University (AMU) in Chemical Engineering. His research is broadly focused on alternate energy generation from waste. Specifically, he is working on Experimental and Mathematical studies on the Pyrolysis of biomass. Additionally, his research interests include wastewater treatment and industrial pollution control. He has several noble research outcomes in terms of research articles and international conferences published in top-tier peer-reviewed journals.

Asmita Mishra does innovative research in the broad field of energy and the environment. She has completed her Bachelor of Technology (B. Tech.) in Chemical Engineering from IGIT Sarang. In the next phase, she has done her Master of Technology (M. Tech.) from the Department of Chemical Engineering having specialization in bioprocess engineering at Jadavpur University. During the present times, she is involved in the specific research field of energy recovery, waste management, etc, at the Department of Chemical Engineering in IIT Kharagpur. Previously, she used to work in the associated fields of biofuel production during her masters. She has published numerous conference proceedings as well as research articles in the international journals of high fame.

Bhim Charan Meikap is a distinguished professor and present Head of the Department (HOD) of Chemical Engineering at IIT Kharagpur. He holds vast expertise and experience in the field of industrial pollution control for the last two decades or so. He has published nearly 200 international journals. He has accomplished his masters and Ph.D. from IIT Kharagpur. He acts as a visiting professor in several highly recognized foreign universities like Curtin University in Australia, University of Kwazulu-Natal (UKZN) in South Africa, and Henan Polytechnic University in China. He is also associated with the joint collaborative research project with the University of Edinburgh in the UK. His broad area of research includes fluidization, coal beneficiation, CO2 capture, solid waste management, and environmental pollution monitoring cum control. He has received several distinguished awards throughout his entire lifetime. Moreover, he is associated with several professional and academic bodies and is selected as a fellow by the prestigious Royal Society of Chemistry and the Institution of Engineers. He has been serving as the member and life member of the higher academic societies like the Indian Institute of Chemical Engineers (IICHE), American Institute of Chemical Engineers (AICHE), Institution of Chemical Engineers (IChemE, UK), International Water Association (IWA, UK), Indian Institute of Metals, Canadian Institute of Chemical Engineers and many more. He is on the editorial board of several top tier peer-reviewed journals like Journal of Fluids, South African Journal of Chemical Engineering, WSEAS Transaction of Fluid Mechanics, Environmental Science & Engineering Technology, etc. He is directly involved as the principal investigator in several significant consultancies and sponsored research projects for critical problem solving related to the betterment of mankind. He has successfully guided and supervised around 20 Ph.D. research scholars during their doctoral studies.
Editor: Dr. Zhang Xiwang
References
- 1.Morawska L., Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ. Int. 2020;139 doi: 10.1016/j.envint.2020.105730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morawska L., Tang J.W., Bahnfleth W., Bluyssen P.M., Boerstra A., Buonanno G., Cao J., Dancer S., Floto A., Franchimon F., Haworth C., Hogeling J., Isaxon C., Jimenez J.L., Kurnitski J., Li Y., Loomans M., Marks G., Marr L.C., Mazzarella L., Melikov A.K., Miller S., Milton D.K., Nazaroff W., Nielsen P.V., Noakes C., Peccia J., Querol X., Sekhar C., Seppänen O., Tanabe S., Tellier R., Tham K.W., Wargocki P., Wierzbicka A., Yao M. How can airborne transmission of COVID-19 indoors be minimised? Environ. Int. 2020;142 doi: 10.1016/j.envint.2020.105832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization, Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations, Scientific Brief, 2020, pp. 1–3. 〈 10.1056/NEJMoa2001316.5〉. [DOI]
- 4.Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shkirkova K., Lamorie-Foote K., Connor M., Patel A., Barisano G., Baertsch H., Liu Q., Morgan T.E., Sioutas C., Mack W.J. Effects of ambient particulate matter on vascular tissue: a review. J. Toxicol. Environ. Health Part B. 2020;23:319–350. doi: 10.1080/10937404.2020.1822971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cochard M., Ledoux F., Landkocz Y. Atmospheric fine particulate matter and epithelial mesenchymal transition in pulmonary cells: state of the art and critical review of the in vitro studies. J. Toxicol. Environ. Health Part B. 2020;23:293–318. doi: 10.1080/10937404.2020.1816238. [DOI] [PubMed] [Google Scholar]
- 7.Contini D., Costabile F. Does air pollution influence COVID-19 outbreaks? Atmosphere. 2020;11:377. doi: 10.3390/atmos11040377. [DOI] [Google Scholar]
- 8.Santarpia J.L., Rivera D.N., Herrera V.L., Morwitzer M.J., Creager H.M., Santarpia G.W., Crown K.K., Brett-Major D.M., Schnaubelt E.R., Broadhurst M.J., Lawler J.V., Reid S.P., Lowe J.J. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci. Rep. 2020;10:12732. doi: 10.1038/s41598-020-69286-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shehzad K., Sarfraz M., Shah S.G.M. The impact of COVID-19 as a necessary evil on air pollution in India during the lockdown. Environ. Pollut. 2020;266 doi: 10.1016/j.envpol.2020.115080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Costa S., Ferreira J., Silveira C., Costa C., Lopes D., Relvas H., Borrego C., Roebeling P., Miranda A.I., Paulo Teixeira J. Integrating health on air quality assessment—review report on health risks of two major european outdoor air pollutants: PM and NO 2. J. Toxicol. Environ. Health Part B. 2014;17:307–340. doi: 10.1080/10937404.2014.946164. [DOI] [PubMed] [Google Scholar]
- 11.Rao S., Klimont Z., Smith S.J., Van Dingenen R., Dentener F., Bouwman L., Riahi K., Amann M., Bodirsky B.L., van Vuuren D.P., Aleluia Reis L., Calvin K., Drouet L., Fricko O., Fujimori S., Gernaat D., Havlik P., Harmsen M., Hasegawa T., Heyes C., Hilaire J., Luderer G., Masui T., Stehfest E., Strefler J., van der Sluis S., Tavoni M. Future air pollution in the shared socio-economic pathways. Glob. Environ. Change. 2017;42:346–358. doi: 10.1016/j.gloenvcha.2016.05.012. [DOI] [Google Scholar]
- 12.Domingo J.L., Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ. Res. 2020;187 doi: 10.1016/j.envres.2020.109650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cui J., Li F., Shi Z.-L. Origin and evolution of pathogenic coronaviruses. Nat. Rev. Microbiol. 2019;17:181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wei Q., Wang Y., Ma J., Han J., Jiang M., Zhao L., Ye F., Song J., Liu B., Wu L., Tan W., Wu G., Gao G.F., Liu J. Description of the first strain of 2019-nCoV, C-Tan-nCoV Wuhan strain — National Pathogen Resource Center, China, 2020. China CDC Wkly. 2020;2:81–82. doi: 10.46234/ccdcw2020.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., Zhao Y., Li Y., Wang X., Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020;323:1061. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu F., Zhao S., Yu B., Chen Y.-M., Wang W., Song Z.-G., Hu Y., Tao Z.-W., Tian J.-H., Pei Y.-Y., Yuan M.-L., Zhang Y.-L., Dai F.-H., Liu Y., Wang Q.-M., Zheng J.-J., Xu L., Holmes E.C., Zhang Y.-Z. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lai C.-C., Shih T.-P., Ko W.-C., Tang H.-J., Hsueh P.-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55 doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dhama K., Sharun K., Tiwari R., Dadar M., Malik Y.S., Singh K.P., Chaicumpa W. COVID-19, an emerging coronavirus infection: advances and prospects in designing and developing vaccines, immunotherapeutics, and therapeutics. Hum. Vaccin. Immunother. 2020;16:1232–1238. doi: 10.1080/21645515.2020.1735227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gorbalenya A.E., Baker S.C., Baric R.S., de Groot R.J., Drosten C., Gulyaeva A.A., Haagmans B.L., Lauber C., Leontovich A.M., Neuman B.W., Penzar D., Perlman S., Poon L.L.M., Samborskiy D.V., Sidorov I.A., Sola I., Ziebuhr J. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020;5:536–544. doi: 10.1038/s41564-020-0695-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization (WHO), WHO Director-General’s Remarks at the Media Briefing on 2019-nCoV, World Health Organization, 11 February 2020. 〈https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020〉. (Accessed 10 October 2020).
- 22.Chan J.F.-W., Kok K.-H., Zhu Z., Chu H., To K.K.-W., Yuan S., Yuen K.-Y. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg. Microbes Infect. 2020;9:221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xu X., Chen P., Wang J., Feng J., Zhou H., Li X., Zhong W., Hao P. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci. China Life Sci. 2020 doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kirchdoerfer R.N., Cottrell C.A., Wang N., Pallesen J., Yassine H.M., Turner H.L., Corbett K.S., Graham B.S., McLellan J.S., Ward A.B. Pre-fusion structure of a human coronavirus spike protein. Nature. 2016;531:118–121. doi: 10.1038/nature17200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tikellis C., Thomas M.C. Angiotensin-converting enzyme 2 (ACE2) is a key modulator of the renin angiotensin system in health and disease. Int. J. Pept. 2012;2012:1–8. doi: 10.1155/2012/256294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zheng Y.-Y., Ma Y.-T., Zhang J.-Y., Xie X. COVID-19 and the cardiovascular system. Nat. Rev. Cardiol. 2020;17:259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jiang F., Deng L., Zhang L., Cai Y., Cheung C.W., Xia Z. Review of the clinical characteristics of coronavirus disease 2019 (COVID-19) J. Gen. Intern. Med. 2020;35:1545–1549. doi: 10.1007/s11606-020-05762-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Matheson N.J., Lehner P.J. How does SARS-CoV-2 cause COVID-19? Science. 2020;369:510–511. doi: 10.1126/science.abc6156. (80-.) [DOI] [PubMed] [Google Scholar]
- 29.Kim S.-H., Chang S.Y., Sung M., Park J.H., Bin Kim H., Lee H., Choi J.-P., Choi W.S., Min J.-Y. Extensive viable Middle East respiratory syndrome (MERS) coronavirus contamination in air and surrounding environment in MERS isolation wards. Clin. Infect. Dis. 2016;63:363–369. doi: 10.1093/cid/ciw239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization, Ambient Air Pollution: A Global Assessment of Exposure and Burden of Disease, World Health Organization, 2016. 〈https://www.who.int/phe/publications/air-pollution-global-assessment/en/〉. (Accessed 20 October 2020).
- 31.Somayaji R., Neradilek M.B., Szpiro A.A., Lofy K.H., Jackson M.L., Goss C.H., Duchin J.S., Neuzil K.M., Ortiz J.R. Effects of air pollution and other environmental exposures on estimates of severe influenza illness, Washington, USA. Emerg. Infect. Dis. 2020;26 doi: 10.3201/eid2605.190599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lelieveld J., Evans J.S., Fnais M., Giannadaki D., Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature. 2015;525:367–371. doi: 10.1038/nature15371. [DOI] [PubMed] [Google Scholar]
- 33.Pope C.A., Ezzati M., Cannon J.B., Allen R.T., Jerrett M., Burnett R.T. Mortality risk and PM2.5 air pollution in the USA: an analysis of a national prospective cohort. Air Qual. Atmos. Health. 2018;11:245–252. doi: 10.1007/s11869-017-0535-3. [DOI] [Google Scholar]
- 34.Gorai A., Tuluri F., Tchounwou P. A GIS based approach for assessing the association between air pollution and asthma in New York State, USA. Int. J. Environ. Res. Public Health. 2014;11:4845–4869. doi: 10.3390/ijerph110504845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shmool J.L.C., Kubzansky L.D., Dotson Newman O., Spengler J., Shepard P., Clougherty J.E. Social stressors and air pollution across New York City communities: a spatial approach for assessing correlations among multiple exposures. Environ. Health. 2014;13:91. doi: 10.1186/1476-069X-13-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yang J., Ji Z., Kang S., Zhang Q., Chen X., Lee S.-Y. Spatiotemporal variations of air pollutants in western China and their relationship to meteorological factors and emission sources. Environ. Pollut. 2019;254 doi: 10.1016/j.envpol.2019.07.120. [DOI] [PubMed] [Google Scholar]
- 37.Wang P., Chen K., Zhu S., Wang P., Zhang H. Severe air pollution events not avoided by reduced anthropogenic activities during COVID-19 outbreak. Resour. Conserv. Recycl. 2020;158 doi: 10.1016/j.resconrec.2020.104814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maji K.J., Dikshit A.K., Arora M., Deshpande A. Estimating premature mortality attributable to PM2.5 exposure and benefit of air pollution control policies in China for 2020. Sci. Total Environ. 2018;612:683–693. doi: 10.1016/j.scitotenv.2017.08.254. [DOI] [PubMed] [Google Scholar]
- 40.Health Effects Institute, State of Global Air 2017: A Special Report on Global Exposure to Air Pollution and Its Disease Burden, Climate and Clean Air Coalition, 2017. 〈https://ccacoalition.org/en/resources/state-global-air-2017-special-report-global-exposure-air-pollution-and-its-disease-burden〉. (Accessed 30 September 2020).
- 41.Health Effects Institute, State of Global Air, 2019. 〈https://www.stateofglobalair.org/report〉. (Accessed 10 October 2020).
- 42.Lei Y., Zhang Q., Nielsen C., He K. An inventory of primary air pollutants and CO2 emissions from cement production in China, 1990–2020. Atmos. Environ. 2011;45:147–154. doi: 10.1016/j.atmosenv.2010.09.034. [DOI] [Google Scholar]
- 43.He L., Zhang S., Hu J., Li Z., Zheng X., Cao Y., Xu G., Yan M., Wu Y. On-road emission measurements of reactive nitrogen compounds from heavy-duty diesel trucks in China. Environ. Pollut. 2020;262 doi: 10.1016/j.envpol.2020.114280. [DOI] [PubMed] [Google Scholar]
- 44.Zhang Z., Chan J.C.L., Ding Y. Characteristics, evolution and mechanisms of the summer monsoon onset over Southeast Asia. Int. J. Climatol. 2004;24:1461–1482. doi: 10.1002/joc.1082. [DOI] [Google Scholar]
- 45.Lepeule J., Litonjua A.A., Gasparrini A., Koutrakis P., Sparrow D., Vokonas P.S., Schwartz J. Lung function association with outdoor temperature and relative humidity and its interaction with air pollution in the elderly. Environ. Res. 2018;165:110–117. doi: 10.1016/j.envres.2018.03.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rao S., Pachauri S., Dentener F., Kinney P., Klimont Z., Riahi K., Schoepp W. Better air for better health: forging synergies in policies for energy access, climate change and air pollution. Glob. Environ. Change. 2013;23:1122–1130. doi: 10.1016/j.gloenvcha.2013.05.003. [DOI] [Google Scholar]
- 47.Cohen A.J., Brauer M., Burnett R., Anderson H.R., Frostad J., Estep K., Balakrishnan K., Brunekreef B., Dandona L., Dandona R., Feigin V., Freedman G., Hubbell B., Jobling A., Kan H., Knibbs L., Liu Y., Martin R., Morawska L., Pope C.A., Shin H., Straif K., Shaddick G., Thomas M., van Dingenen R., van Donkelaar A., Vos T., Murray C.J.L., Forouzanfar M.H. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. Lancet. 2017;389:1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dutheil F., Baker J.S., Navel V. COVID-19 as a factor influencing air pollution? Environ. Pollut. 2020;263 doi: 10.1016/j.envpol.2020.114466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brauer M. How much, how long, what, and where: air pollution exposure assessment for epidemiologic studies of respiratory disease. Proc. Am. Thorac. Soc. 2010;7:111–115. doi: 10.1513/pats.200908-093RM. [DOI] [PubMed] [Google Scholar]
- 50.Tellier R., Li Y., Cowling B.J., Tang J.W. Recognition of aerosol transmission of infectious agents: a commentary. BMC Infect. Dis. 2019;19:101. doi: 10.1186/s12879-019-3707-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Asadi S., Wexler A.S., Cappa C.D., Barreda S., Bouvier N.M., Ristenpart W.D. Aerosol emission and superemission during human speech increase with voice loudness. Sci. Rep. 2019;9:2348. doi: 10.1038/s41598-019-38808-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dhand R., Li J. Coughs and sneezes: their role in transmission of respiratory viral infections, including SARS-CoV-2. Am. J. Respir. Crit. Care Med. 2020;202:651–659. doi: 10.1164/rccm.202004-1263PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stadnytskyi V., Bax C.E., Bax A., Anfinrud P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc. Natl. Acad. Sci. 2020;117:11875–11877. doi: 10.1073/pnas.2006874117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.ELPAIS, Aerosol Transmission of Coronavirus, Soc. ELPAIS, 2020. 〈https://english.elpais.com/society/2020-10-28/a-room-a-bar-and-a-class-how-the-coronavirus-is-spread-through-the-air.html?s=09〉. (Accessed 30 October 2020).
- 55.Bar-On Y.M., Flamholz A., Phillips R., Milo R. SARS-CoV-2 (COVID-19) by the numbers. elife. 2020;9 doi: 10.7554/eLife.57309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li Z., Wen Q., Zhang R. Sources, health effects and control strategies of indoor fine particulate matter (PM2.5): a review. Sci. Total Environ. 2017;586:610–622. doi: 10.1016/j.scitotenv.2017.02.029. [DOI] [PubMed] [Google Scholar]
- 57.Chennakesavulu K., Reddy G.R. The effect of latitude and PM2.5 on spreading of SARS-CoV-2 in tropical and temperate zone countries. Environ. Pollut. 2020;266 doi: 10.1016/j.envpol.2020.115176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020 doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., de Wit E., Munster V.J. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020;382:1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Appl. Environ. Microbiol. 2010;76:2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Walker C.M., Ko G. Effect of ultraviolet germicidal irradiation on viral aerosols. Environ. Sci. Technol. 2007;41:5460–5465. doi: 10.1021/es070056u. [DOI] [PubMed] [Google Scholar]
- 62.Fiore A.M., Naik V., Spracklen D.V., Steiner A., Unger N., Prather M., Bergmann D., Cameron-Smith P.J., Cionni I., Collins W.J., Dalsøren S., Eyring V., Folberth G.A., Ginoux P., Horowitz L.W., Josse B., Lamarque J.-F., MacKenzie I.A., Nagashima T., O’Connor F.M., Righi M., Rumbold S.T., Shindell D.T., Skeie R.B., Sudo K., Szopa S., Takemura T., Zeng G. Global air quality and climate. Chem. Soc. Rev. 2012;41:6663. doi: 10.1039/c2cs35095e. [DOI] [PubMed] [Google Scholar]
- 63.Kohanski M.A., Lo L.J., Waring M.S. Review of indoor aerosol generation, transport, and control in the context of COVID‐19. Int. Forum Allergy Rhinol. 2020;10:1173–1179. doi: 10.1002/alr.22661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu Y., Ning Z., Chen Y., Guo M., Liu Y., Gali N.K., Sun L., Duan Y., Cai J., Westerdahl D., Liu X., Xu K., Ho K., Kan H., Fu Q., Lan K. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature. 2020;582:557–560. doi: 10.1038/s41586-020-2271-3. [DOI] [PubMed] [Google Scholar]
- 65.Annesi-Maesano I., Baiz N., Banerjee S., Rudnai P., Rive S., The SINPHONIE Group Indoor air quality and sources in schools and related health effects. J. Toxicol. Environ. Health Part B. 2013;16:491–550. doi: 10.1080/10937404.2013.853609. [DOI] [PubMed] [Google Scholar]
- 66.Santarpia J.L., Rivera D.N., Herrera V.L., Morwitzer M.J., Creager H.M., Santarpia G.W., Crown K.K., Brett-Major D.M., Schnaubelt E.R., Broadhurst M.J., Lawler J.V., Reid S.P., Lowe J.J. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci. Rep. 2020;10:12732. doi: 10.1038/s41598-020-69286-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jones R.M., Brosseau L.M. Aerosol transmission of infectious disease. J. Occup. Environ. Med. 2015;57:501–508. doi: 10.1097/JOM.0000000000000448. [DOI] [PubMed] [Google Scholar]
- 68.Hennig F., Fuks K., Moebus S., Weinmayr G., Memmesheimer M., Jakobs H., Bröcker-Preuss M., Führer-Sakel D., Möhlenkamp S., Erbel R., Jöckel K.-H., Hoffmann B. Association between source-specific particulate matter air pollution and hs-CRP: local traffic and industrial emissions. Environ. Health Perspect. 2014;122:703–710. doi: 10.1289/ehp.1307081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Zhao Q., Li Y., Chai X., Xu L., Zhang L., Ning P., Huang J., Tian S. Interaction of inhalable volatile organic compounds and pulmonary surfactant: potential hazards of VOCs exposure to lung. J. Hazard. Mater. 2019;369:512–520. doi: 10.1016/j.jhazmat.2019.01.104. [DOI] [PubMed] [Google Scholar]
- 70.Paciência I., Madureira J., Rufo J., Moreira A., de E., Fernandes O. A systematic review of evidence and implications of spatial and seasonal variations of volatile organic compounds (VOC) in indoor human environments. J. Toxicol. Environ. Health Part B. 2016;19:47–64. doi: 10.1080/10937404.2015.1134371. [DOI] [PubMed] [Google Scholar]
- 71.Mohamad Nor N., Lau L.C., Lee K.T., Mohamed A.R. Synthesis of activated carbon from lignocellulosic biomass and its applications in air pollution control—a review. J. Environ. Chem. Eng. 2013;1:658–666. doi: 10.1016/j.jece.2013.09.017. [DOI] [Google Scholar]
- 72.Guo S., Hu M., Zamora M.L., Peng J., Shang D., Zheng J., Du Z., Wu Z., Shao M., Zeng L., Molina M.J., Zhang R. Elucidating severe urban haze formation in China. Proc. Natl. Acad. Sci. 2014;111:17373–17378. doi: 10.1073/pnas.1419604111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fortner E.C., Zheng J., Zhang R., Berk Knighton W., Volkamer R.M., Sheehy P., Molina L., André M. Measurements of volatile organic compounds using proton transfer reaction – mass spectrometry during the MILAGRO 2006 campaign. Atmos. Chem. Phys. 2009;9:467–481. doi: 10.5194/acp-9-467-2009. [DOI] [Google Scholar]
- 74.Wang M., Zhu T., Zheng J., Zhang R.Y., Zhang S.Q., Xie X.X., Han Y.Q., Li Y. Use of a mobile laboratory to evaluate changes in on-road air pollutants during the Beijing 2008 Summer Olympics. Atmos. Chem. Phys. 2009;9:8247–8263. doi: 10.5194/acp-9-8247-2009. [DOI] [Google Scholar]
- 75.Zhang R., Wang G., Guo S., Zamora M.L., Ying Q., Lin Y., Wang W., Hu M., Wang Y. Formation of urban fine particulate matter. Chem. Rev. 2015;115:3803–3855. doi: 10.1021/acs.chemrev.5b00067. [DOI] [PubMed] [Google Scholar]
- 76.Stocker T.F., Qin D., Plattner G.K., Tignor M.M.B., Allen S.K., Boschung J., Nauels A., Xia Y., Bex V., Midgley P.M. Cambridge University Press; Cambridge: 2014. Climate Change 2013 – The Physical Science Basis. [DOI] [Google Scholar]
- 77.Fan J., Zhang R., Li G., Tao W.K., Li X. Simulations of cumulus clouds using a spectral microphysics cloud-resolving model. J. Geophys. Res. 2007;112 doi: 10.1029/2006JD007688. [DOI] [Google Scholar]
- 78.Wang Y., Wan Q., Meng W., Liao F., Tan H., Zhang R. Long-term impacts of aerosols on precipitation and lightning over the Pearl River Delta megacity area in China. Atmos. Chem. Phys. 2011 doi: 10.5194/acp-11-12421-2011. [DOI] [Google Scholar]
- 79.Bhopal R.S., Phillimore P., Moffatt S., Foy C. Is living near a coking works harmful to health? A study of industrial air pollution. J. Epidemiol. Community Health. 1994;48:237–247. doi: 10.1136/jech.48.3.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Friedlander S.K. Chemical element balances and identification of air pollution sources. Environ. Sci. Technol. 1973;7:235–240. doi: 10.1021/es60075a005. [DOI] [PubMed] [Google Scholar]
- 81.Kowalczyk G.S., Gordon G.E., Rheingrover S.W. Identification of atmospheric particulate sources in Washington, D.C. using chemical element balances. Environ. Sci. Technol. 1982;16:79–90. doi: 10.1021/es00096a005. [DOI] [Google Scholar]
- 82.Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zhang R., Li Y., Zhang A.L., Wang Y., Molina M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc. Natl. Acad. Sci. 2020;117:14857–14863. doi: 10.1073/pnas.2009637117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.An Z., Huang R.-J., Zhang R., Tie X., Li G., Cao J., Zhou W., Shi Z., Han Y., Gu Z., Ji Y. Severe haze in northern China: a synergy of anthropogenic emissions and atmospheric processes. Proc. Natl. Acad. Sci. 2019;116:8657–8666. doi: 10.1073/pnas.1900125116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bousquet P., Ciais P., Miller J.B., Dlugokencky E.J., Hauglustaine D.A., Prigent C., Van der Werf G.R., Peylin P., Brunke E.-G., Carouge C., Langenfelds R.L., Lathière J., Papa F., Ramonet M., Schmidt M., Steele L.P., Tyler S.C., White J. Contribution of anthropogenic and natural sources to atmospheric methane variability. Nature. 2006;443:439–443. doi: 10.1038/nature05132. [DOI] [PubMed] [Google Scholar]
- 86.Kraemer M.U.G., Yang C.-H., Gutierrez B., Wu C.-H., Klein B., Pigott D.M., du Plessis L., Faria N.R., Li R., Hanage W.P., Brownstein J.S., Layan M., Vespignani A., Tian H., Dye C., Pybus O.G., Scarpino S.V. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368:493–497. doi: 10.1126/science.abb4218. (80-.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang Q., Shao M., Zhang Y., Wei Y., Hu M., Guo S. Source apportionment of fine organic aerosols in Beijing. Atmos. Chem. Phys. 2009;9:8573–8585. doi: 10.5194/acp-9-8573-2009. [DOI] [Google Scholar]
- 88.Zhang Q., Wang S., Zhu P., Wang Z., Zhang G. Full-scale simulation of flow field in ammonia-based wet flue gas desulfurization double tower. J. Energy Inst. 2018;91:619–629. doi: 10.1016/j.joei.2017.02.010. [DOI] [Google Scholar]
- 89.Zhang R. Getting to the critical nucleus of aerosol formation. Science. 2010;328:1366–1367. doi: 10.1126/science.1189732. (80-.) [DOI] [PubMed] [Google Scholar]
- 90.Zhang R., Khalizov A., Wang L., Hu M., Xu W. Nucleation and growth of nanoparticles in the atmosphere. Chem. Rev. 2012;112:1957–2011. doi: 10.1021/cr2001756. [DOI] [PubMed] [Google Scholar]
- 91.Ilyas S., Srivastava R.R., Kim H. Disinfection technology and strategies for COVID-19 hospital and bio-medical waste management. Sci. Total Environ. 2020;749 doi: 10.1016/j.scitotenv.2020.141652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.He P., Zhang H., Zhang C., Lee D. Characteristics of air pollution control residues of MSW incineration plant in Shanghai. J. Hazard. Mater. 2004;116:229–237. doi: 10.1016/j.jhazmat.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 93.Quina M.J., Bordado J.C., Quinta-Ferreira R.M. Treatment and use of air pollution control residues from MSW incineration: an overview. Waste Manag. 2008;28:2097–2121. doi: 10.1016/j.wasman.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 94.Quina M.J., Bordado J.C.M., Quinta-Ferreira R.M. Chemical stabilization of air pollution control residues from municipal solid waste incineration. J. Hazard. Mater. 2010;179:382–392. doi: 10.1016/j.jhazmat.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 95.Kreyling W.G., Semmler M., Möller W. Dosimetry and toxicology of ultrafine particles. J. Aerosol Med. 2004;17:140–152. doi: 10.1089/0894268041457147. [DOI] [PubMed] [Google Scholar]
- 96.Araujo J.A., Barajas B., Kleinman M., Wang X., Bennett B.J., Gong K.W., Navab M., Harkema J., Sioutas C., Lusis A.J., Nel A.E. Ambient particulate pollutants in the ultrafine range promote early atherosclerosis and systemic oxidative stress. Circ. Res. 2008;102:589–596. doi: 10.1161/CIRCRESAHA.107.164970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Schlesinger R.B., Kunzli N., Hidy G.M., Gotschi T., Jerrett M. The health relevance of ambient particulate matter characteristics: coherence of toxicological and epidemiological inferences. Inhal. Toxicol. 2006;18:95–125. doi: 10.1080/08958370500306016. [DOI] [PubMed] [Google Scholar]
- 98.World Health Organization (WHO), WHO Air Quality Guidelines Global Update 2005 Report on a Working Group Meeting Bonn, Germany, World Health Organization, 18–20 October 2005. 〈https://www.euro.who.int/__data/assets/pdf_file/0008/147851/E87950.pdf〉. (Accessed 15 October 2020).
- 99.Suh S., Johnson J.A., Tambjerg L., Sim S., Broeckx-Smith S., Reyes W., Chaplin-Kramer R. Closing yield gap is crucial to avoid potential surge in global carbon emissions. Glob. Environ. Change. 2020;63 doi: 10.1016/j.gloenvcha.2020.102100. [DOI] [Google Scholar]
- 100.Riahi K., van Vuuren D.P., Kriegler E., Edmonds J., O’Neill B.C., Fujimori S., Bauer N., Calvin K., Dellink R., Fricko O., Lutz W., Popp A., Cuaresma J.C., KC S., Leimbach M., Jiang L., Kram T., Rao S., Emmerling J., Ebi K., Hasegawa T., Havlik P., Humpenöder F., Da Silva L.A., Smith S., Stehfest E., Bosetti V., Eom J., Gernaat D., Masui T., Rogelj J., Strefler J., Drouet L., Krey V., Luderer G., Harmsen M., Takahashi K., Baumstark L., Doelman J.C., Kainuma M., Klimont Z., Marangoni G., Lotze-Campen H., Obersteiner M., Tabeau A., Tavoni M. The shared socioeconomic pathways and their energy, land use, and greenhouse gas emissions implications: an overview. Glob. Environ. Change. 2017;42:153–168. doi: 10.1016/j.gloenvcha.2016.05.009. [DOI] [Google Scholar]
- 101.Hayashi N., Yamamoto K., Ohishi M., Tatara Y., Takeya Y., Shiota A., Oguro R., Iwamoto Y., Takeda M., Rakugi H. The counterregulating role of ACE2 and ACE2-mediated angiotensin 1–7 signaling against angiotensin II stimulation in vascular cells. Hypertens. Res. 2010;33:1182–1185. doi: 10.1038/hr.2010.147. [DOI] [PubMed] [Google Scholar]
- 102.Comunian S., Dongo D., Milani C., Palestini P. Air pollution and COVID-19: the role of particulate matter in the spread and increase of COVID-19’s morbidity and mortality. IJERPH. 2020;17:4487. doi: 10.3390/ijerph17124487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Fang Y., Gao F., Liu Z. Angiotensin-converting enzyme 2 attenuates inflammatory response and oxidative stress in hyperoxic lung injury by regulating NF-κB and Nrf2 pathways. QJM Int. J. Med. 2019;112:914–924. doi: 10.1093/qjmed/hcz206. [DOI] [PubMed] [Google Scholar]
- 104.Leclercq B., Kluza J., Antherieu S., Sotty J., Alleman L.Y., Perdrix E., Loyens A., Coddeville P., Lo Guidice J.-M., Marchetti P., Garçon G. Air pollution-derived PM2.5 impairs mitochondrial function in healthy and chronic obstructive pulmonary diseased human bronchial epithelial cells. Environ. Pollut. 2018;243:1434–1449. doi: 10.1016/j.envpol.2018.09.062. [DOI] [PubMed] [Google Scholar]
- 105.Farina F., Sancini G., Battaglia C., Tinaglia V., Mantecca P., Camatini M., Palestini P. Milano summer particulate matter (PM10) triggers lung inflammation and extra pulmonary adverse events in mice. PLoS One. 2013;8 doi: 10.1371/journal.pone.0056636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Palestini P. Health risk assessment for air pollutants: lung inflammation and extra pulmonary adverse events are correlated to particulate matter size, origin and season of collection. Toxicol. Lett. 2016;259:S9. doi: 10.1016/j.toxlet.2016.07.703. [DOI] [Google Scholar]
- 107.Ciencewicki J., Jaspers I. Air pollution and respiratory viral infection. Inhal. Toxicol. 2007;19:1135–1146. doi: 10.1080/08958370701665434. [DOI] [PubMed] [Google Scholar]
- 108.Ma Q., Qi Y., Shan Q., Liu S., He H. Understanding the knowledge gaps between air pollution controls and health impacts including pathogen epidemic. Environ. Res. 2020;189 doi: 10.1016/j.envres.2020.109949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Cui Y., Zhang Z.-F., Froines J., Zhao J., Wang H., Yu S.-Z., Detels R. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environ. Health. 2003;2:15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mantecca P., Sancini G., Moschini E., Farina F., Gualtieri M., Rohr A., Miserocchi G., Palestini P., Camatini M. Lung toxicity induced by intratracheal instillation of size-fractionated tire particles. Toxicol. Lett. 2009;189:206–214. doi: 10.1016/j.toxlet.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 111.Kampa M., Castanas E. Human health effects of air pollution. Environ. Pollut. 2008;151:362–367. doi: 10.1016/j.envpol.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 112.Di Q., Wang Y., Zanobetti A., Wang Y., Koutrakis P., Choirat C., Dominici F., Schwartz J.D. Air pollution and mortality in the medicare population. N. Engl. J. Med. 2017;376:2513–2522. doi: 10.1056/NEJMoa1702747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Liang D., Shi L., Zhao J., Liu P., Sarnat J.A., Gao S., Schwartz J., Liu Y., Ebelt S.T., Scovronick N., Chang H.H. Urban air pollution may enhance COVID-19 case-fatality and mortality rates in the United States. Innovation. 2020;1 doi: 10.1016/j.xinn.2020.100047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Rayner S. Prospects for CO2 emissions reduction policy in the USA. Glob. Environ. Change. 1993;3:12–31. doi: 10.1016/0959-3780(93)90012-A. [DOI] [Google Scholar]
- 115.Tian H., Liu Y., Li Y., Wu C.-H., Chen B., Kraemer M.U.G., Li B., Cai J., Xu B., Yang Q., Wang B., Yang P., Cui Y., Song Y., Zheng P., Wang Q., Bjornstad O.N., Yang R., Grenfell B.T., Pybus O.G., Dye C. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368:638–642. doi: 10.1126/science.abb6105. (80-.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.World Health Organization (WHO), Considerations for Quarantine of Individuals in the Context of Containment for Coronavirus Disease (COVID-19): Interim Guidance, World Health Organization, 19 March 2020. 〈https://apps.who.int/iris/handle/10665/331299〉. (Accessed 15 October 2020).
- 117.López L., Rodó X. The end of social confinement and COVID-19 re-emergence risk. Nat. Hum. Behav. 2020;4:746–755. doi: 10.1038/s41562-020-0908-8. [DOI] [PubMed] [Google Scholar]
- 118.World Health Organization, Coronavirus Disease (COVID-19) Pandemic, World Health Organization, 2020. 〈https://www.who.int/emergencies/diseases/novel-coronavirus-2019〉. (Accessed 15 October 2020).
- 119.Armengaud J., Delaunay-Moisan A., Thuret J., van Anken E., Acosta-Alvear D., Aragón T., Arias C., Blondel M., Braakman I., Collet J., Courcol R., Danchin A., Deleuze J., Lavigne J., Lucas S., Michiels T., Moore E.R.B., Nixon-Abell J., Rossello-Mora R., Shi Z., Siccardi A.G., Sitia R., Tillett D., Timmis K.N., Toledano M.B., van der Sluijs P., Vicenzi E. The importance of naturally attenuated SARS-CoV-2in the fight against COVID-19. Environ. Microbiol. 2020;22:1997–2000. doi: 10.1111/1462-2920.15039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Grubaugh N.D., Petrone M.E., Holmes E.C. We shouldn’t worry when a virus mutates during disease outbreaks. Nat. Microbiol. 2020;5:529–530. doi: 10.1038/s41564-020-0690-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Batisse D., Benech N., Botelho-Nevers E., Bouiller K., Collarino R., Conrad A., Gallay L., Goehringer F., Gousseff M., Joseph D.C., Lemaignen A., Lescure F.-X., Levy B., Mahevas M., Penot P., Pozzetto B., Salmon D., Slama D., Vignier N., Wyplosz B. Clinical recurrences of COVID-19 symptoms after recovery: viral relapse, reinfection or inflammatory rebound? J. Infect. 2020 doi: 10.1016/j.jinf.2020.06.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Xiao A.T., Tong Y.X., Zhang S. Profile of RT-PCR for SARS-CoV-2: a preliminary study from 56 COVID-19 patients. Clin. Infect. Dis. 2020;71:2249–2251. doi: 10.1093/cid/ciaa460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Ling Y., Xu S.-B., Lin Y.-X., Tian D., Zhu Z.-Q., Dai F.-H., Wu F., Song Z.-G., Huang W., Chen J., Hu B.-J., Wang S., Mao E.-Q., Zhu L., Zhang W.-H., Lu H.-Z. Persistence and clearance of viral RNA in 2019 novel coronavirus disease rehabilitation patients. Chin. Med. J. (Engl.) 2020;133:1039–1043. doi: 10.1097/CM9.0000000000000774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Carmo A., Pereira‐Vaz J., Mota V., Mendes A., Morais C., Silva A.C., Camilo E., Pinto C.S., Cunha E., Pereira J., Coucelo M., Martinho P., Correia L., Marques G., Araújo L., Rodrigues F. Clearance and persistence of SARS‐CoV‐2 RNA in patients with COVID‐19. J. Med. Virol. 2020 doi: 10.1002/jmv.26103. jmv.26103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ye G., Pan Z., Pan Y., Deng Q., Chen L., Li J., Li Y., Wang X. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. J. Infect. 2020;80:e14–e17. doi: 10.1016/j.jinf.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ota M. Will we see protection or reinfection in COVID-19? Nat. Rev. Immunol. 2020;20:351. doi: 10.1038/s41577-020-0316-3. 351–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.V. Rambaran, Coronavirus Could Have A Deadlier Second Wave Later This Year, CDC Director Warns, Fox News, 2020. 〈https://www.foxnews.com/health/coronavirus-could-have-deadlier-second-wave-later-this-year-cdc-director-warns〉. (Accessed 20 September 2020).
- 128.Alpalhão M., Ferreira J.A., Filipe P. Persistent SARS-CoV-2 infection and the risk for cancer. Med. Hypotheses. 2020;143 doi: 10.1016/j.mehy.2020.109882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z., Yu J., Kang M., Song Y., Xia J., Guo Q., Song T., He J., Yen H.-L., Peiris M., Wu J. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N. Engl. J. Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kissler S.M., Tedijanto C., Goldstein E., Grad Y.H., Lipsitch M. Projecting the transmission dynamics of SARS-CoV-2 through the postpandemic period. Science. 2020;368:860–868. doi: 10.1126/science.abb5793. (80-.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ferguson N.M., Laydon D., Nedjati-Gilani G., Imai N., Ainslie K., Baguelin M., Bhatia S., Boonyasiri A., Cucunubá Z., Cuomo-Dannenburg G., Dighe A., Dorigatti I., Fu H., Gaythorpe K., Green W., Hamlet A., Hinsley W., Okell L.C., Van Elsland S., Thompson H., Verity R., Volz E., Wang H., Wang Y., Gt Walker P., Walters C., Winskill P., Whittaker C., Donnelly C.A., Riley S., Ghani A.C. Impact of Non-Pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality and Healthcare Demand. Imperial.Ac.Uk; 2020. [DOI] [Google Scholar]
- 132.Koirala A., Joo Y.J., Khatami A., Chiu C., Britton P.N. Vaccines for COVID-19: the current state of play. Paediatr. Respir. Rev. 2020 doi: 10.1016/j.prrv.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lurie N., Saville M., Hatchett R., Halton J. Developing covid-19 vaccines at pandemic speed. N. Engl. J. Med. 2020;382:1969–1973. doi: 10.1056/NEJMp2005630. [DOI] [PubMed] [Google Scholar]
- 134.IANS Report, No Guarantee Any Covid Vaccine in Development Will Work: WHO Chief, Times of India, 2020. 〈https://timesofindia.indiatimes.com/world/rest-of-world/no-guarantee-any-covid-vaccine-in-development-will-work-who-chief/articleshow/78277449.cms#:~:text=GENEVA%3A〉. World Health Organisation (WHO, now in development will work). (Accessed 25 September 2020).
- 135.Berkley S. COVID-19 needs a big science approach. Science. 2020;367:1407. doi: 10.1126/science.abb8654. 1407–1407. [DOI] [PubMed] [Google Scholar]
- 136.Billington J., Deschamps I., Erck S.C., Gerberding J.L., Hanon E., Ivol S., Shiver J.W., Spencer J.A., Van Hoof J. Developing vaccines for SARS-CoV-2 and future epidemics and pandemics: applying lessons from past outbreaks. Health Secur. 2020;18:241–249. doi: 10.1089/hs.2020.0043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Alshawa A., Russell A.R., Nizkorodov S.A. Kinetic analysis of competition between aerosol particle removal and generation by ionization air purifiers. Environ. Sci. Technol. 2007;41:2498–2504. doi: 10.1021/es061760y. [DOI] [PubMed] [Google Scholar]
- 138.Grinshpun S.A., Mainelis G., Trunov M., Adhikari A., Reponen T., Willeke K. Evaluation of ionic air purifiers for reducing aerosol exposure in confined indoor spaces. Indoor Air. 2005;15:235–245. doi: 10.1111/j.1600-0668.2005.00364.x. [DOI] [PubMed] [Google Scholar]
- 139.Guo Z.-D., Wang Z.-Y., Zhang S.-F., Li X., Li L., Li C., Cui Y., Fu R.-B., Dong Y.-Z., Chi X.-Y., Zhang M.-Y., Liu K., Cao C., Liu B., Zhang K., Gao Y.-W., Lu B., Chen W. Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg. Infect. Dis. 2020;26:1583–1591. doi: 10.3201/eid2607.200885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.National Research Council . National Academies Press; Washington, D.C.: 2020. Rapid Expert Consultation on the Possibility of Bioaerosol Spread of SARS-CoV-2 for the COVID-19 Pandemic (April 1, 2020) [DOI] [Google Scholar]
- 141.Zhao B., Liu Y., Chen C. Air purifiers: a supplementary measure to remove airborne SARS-CoV-2. Build. Environ. 2020;177 doi: 10.1016/j.buildenv.2020.106918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Davies M., Ucci M., McCarthy M., Oreszczyn T., Ridley I., Mumovic D., Singh J., Pretlove S. A review of evidence linking ventilation rates in dwellings and respiratory health – a focus on house dust mites and mould. Int. J. Vent. 2004 doi: 10.1080/14733315.2004.11683911. [DOI] [Google Scholar]
- 143.Wright G.R., Howieson S., McSharry C., McMahon A.D., Chaudhuri R., Thompson J., Donnelly I., Brooks R.G., Lawson A., Jolly L., McAlpine L., King E.M., Chapman M.D., Wood S., Thomson N.C. Effect of improved home ventilation on asthma control and house dust mite allergen levels. Allergy. 2009;64:1671–1680. doi: 10.1111/j.1398-9995.2009.02098.x. [DOI] [PubMed] [Google Scholar]
- 144.Park J.H., Byeon J.H., Yoon K.Y., Hwang J. Lab-scale test of a ventilation system including a dielectric barrier discharger and UV-photocatalyst filters for simultaneous removal of gaseous and particulate contaminants. Indoor Air. 2007;18:44–50. doi: 10.1111/j.1600-0668.2007.00503.x. [DOI] [PubMed] [Google Scholar]
- 145.Leaderer B.P., Cain W.S., Isseroff R., Berglund L.G. Ventilation requirements in buildings-II. Particulate matter and carbon monoxide from cigarette smoking. Atmos. Environ. 1984;18:99–106. doi: 10.1016/0004-6981(84)90232-4. [DOI] [Google Scholar]
- 146.Seidenberg A.B., Orlan E.N., Travers M.J., Sutfin E.L. Air quality and presence of air ventilation systems inside waterpipe cafés in North Carolina. Tob. Control. 2019;28:356–358. doi: 10.1136/tobaccocontrol-2018-054361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Qian H., Zheng X. Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J. Thorac. Dis. 2018;10:S2295–S2304. doi: 10.21037/jtd.2018.01.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sornboot J., Aekplakorn W., Ramasoota P., Bualert S., Tumwasorn S., Jiamjarasrangsi W. Detection of airborne Mycobacterium tuberculosis complex in high-risk areas of health care facilities in Thailand. Int. J. Tuberc. Lung Dis. 2019;23:465–473. doi: 10.5588/ijtld.18.0218. [DOI] [PubMed] [Google Scholar]
- 149.Rule A.M., Apau O., Ahrenholz S.H., Brueck S.E., Lindsley W.G., de Perio M.A., Noti J.D., Shaffer R.E., Rothman R., Grigorovitch A., Noorbakhsh B., Beezhold D.H., Yorio P.L., Perl T.M., Fisher E.M. Healthcare personnel exposure in an emergency department during influenza season. PLoS One. 2018;13 doi: 10.1371/journal.pone.0203223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Jo S., Hong J., Lee S.-E., Ki M., Choi B.Y., Sung M. Airflow analysis of Pyeongtaek St Mary's Hospital during hospitalization of the first Middle East respiratory syndrome patient in Korea. R. Soc. Open Sci. 2019;6 doi: 10.1098/rsos.181164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Kulkarni H., Smith C.M., Lee D.D.H., Hirst R.A., Easton A.J., O’Callaghan C. Evidence of respiratory syncytial virus spread by aerosol time to revisit infection control strategies? Am. J. Respir. Crit. Care Med. 2016;194:308–316. doi: 10.1164/rccm.201509-1833OC. [DOI] [PubMed] [Google Scholar]
- 152.Pasquarella C., Sansebastiano G.E., Ferretti S., Saccani E., Fanti M., Moscato U., Giannetti G., Fornia S., Cortellini P., Vitali P., Signorelli C. A mobile laminar airflow unit to reduce air bacterial contamination at surgical area in a conventionally ventilated operating theatre. J. Hosp. Infect. 2007;66:313–319. doi: 10.1016/j.jhin.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 153.Marr L.C., Tang J.W., Van Mullekom J., Lakdawala S.S. Mechanistic insights into the effect of humidity on airborne influenza virus survival, transmission and incidence. J. R. Soc. Interface. 2019;16 doi: 10.1098/rsif.2018.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Brown J.R., Tang J.W., Pankhurst L., Klein N., Gant V., Lai K.M., McCauley J., Breuer J. Influenza virus survival in aerosols and estimates of viable virus loss resulting from aerosolization and air-sampling. J. Hosp. Infect. 2015;91:278–281. doi: 10.1016/j.jhin.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 155.Bal M., Siddiqi H., Mukherjee S., Meikap B.C. Design of self priming venturi scrubber for the simultaneous abatement of HCl gas and particulate matter from the flue gas. Chem. Eng. Res. Des. 2019;150:311–319. doi: 10.1016/j.cherd.2019.08.005. [DOI] [Google Scholar]
- 156.Lehner M. Aerosol separation efficiency of a venturi scrubber working in self-priming mode. Aerosol Sci. Technol. 1998;28:389–402. doi: 10.1080/02786829808965533. [DOI] [Google Scholar]
- 157.Lee J., Jung W.Y., Lee H.C., Kim G.T., Lee D.Y. Experimental study on aerosol scrubbing efficiency of self-priming venturi scrubber submerged in water pool. Ann. Nucl. Energy. 2018;114:571–585. doi: 10.1016/j.anucene.2017.12.052. [DOI] [Google Scholar]
- 158.Ali M., Yan C., Sun Z., Wang J., Gu H. CFD simulation of dust particle removal efficiency of a venturi scrubber in CFX. Nucl. Eng. Des. 2013;256:169–177. doi: 10.1016/j.nucengdes.2012.12.013. [DOI] [Google Scholar]
- 159.Mi T., Yu X.M. Dust removal and desulphurization in a novel venturi scrubber. Chem. Eng. Process. Process Intensif. 2012;62:159–167. doi: 10.1016/j.cep.2012.07.010. [DOI] [Google Scholar]
- 160.Ali S., Waheed K., Qureshi K., Irfan N., Ahmed M., Siddique W., Farooq A. Experimental investigation of aerosols removal efficiency through self-priming venturi scrubber. Nucl. Eng. Technol. 2020;52:2230–2237. doi: 10.1016/j.net.2020.03.019. [DOI] [Google Scholar]
- 161.Xie B., Li S., Jin H., Hu S., Wang F., Zhou F. Analysis of the performance of a novel dust collector combining cyclone separator and cartridge filter. Powder Technol. 2018;339:695–701. doi: 10.1016/j.powtec.2018.07.103. [DOI] [Google Scholar]
- 162.Fu P.-B., Wang F., Yang X.-J., Ma L., Cui X., Wang H.-L. Inlet particle-sorting cyclone for the enhancement of PM 2.5 separation. Environ. Sci. Technol. 2017;51:1587–1594. doi: 10.1021/acs.est.6b04418. [DOI] [PubMed] [Google Scholar]
- 163.Hsu Y.-D., Chein H.M., Chen T.M., Tsai C.-J. Axial flow cyclone for segregation and collection of ultrafine particles: theoretical and experimental study. Environ. Sci. Technol. 2005;39:1299–1308. doi: 10.1021/es0491735. [DOI] [PubMed] [Google Scholar]
- 164.Mukhopadhyay N., Chakrabarti R.K., Bose P.K. A new theoretical approach of designing cyclone separator for controlling diesel soot particulate emission. SAE Tech. Pap. 2006 doi: 10.4271/2006-01-1978. [DOI] [Google Scholar]
- 165.Darcovich K., Jonasson K.A., Capes C.E. Developments in the control of fine particulate air emissions. Adv. Powder Technol. 1997;8:179–215. doi: 10.1016/S0921-8831(08)60463-X. [DOI] [Google Scholar]
- 166.Bose P.K., Roy K., Mukhopadhya N., Chakraborty R.K. Improved theoretical modeling of a cyclone separator as a diesel soot particulate emission arrester. Int. J. Automot. Technol. 2010;11:1–10. doi: 10.1007/s12239-010-0001-9. [DOI] [Google Scholar]
- 167.Saiyasitpanich P., Keener T.C., Khang S.J., Lu M. Removal of diesel particulate matter (DPM) in a tubular wet electrostatic precipitator. J. Electrost. 2007;65:618–624. doi: 10.1016/j.elstat.2007.01.005. [DOI] [Google Scholar]
- 168.R. Altman, G. Offen, W. Buckley, I. Ray, c, Power Eng., Barrington, Illinois, 2001.
- 169.Parker K.R. Applied Electrostatic Precipitation. Springer; Netherlands, Dordrecht: 1997. Why an electrostatic precipitator? pp. 1–10. [DOI] [Google Scholar]
- 170.Noda N., Makino H. Influence of operating temperature on performance of electrostatic precipitator for pulverized coal combustion boiler. Adv. Powder Technol. 2010;21:495–499. doi: 10.1016/j.apt.2010.04.012. [DOI] [Google Scholar]
- 171.Bayless D.J., Alam M.K., Radcliff R., Caine J. Membrane-based wet electrostatic precipitation. Fuel Process. Technol. 2004;85:781–798. doi: 10.1016/j.fuproc.2003.11.025. [DOI] [Google Scholar]
- 172.Saiyasitpanich P., Keener T.C., Lu M., Khang S.J., Evans D.E. Collection of ultrafine diesel particulate matter (DPM) in cylindrical single-stage wet electrostatic precipitators. Environ. Sci. Technol. 2006;40:7890–7895. doi: 10.1021/es060887k. [DOI] [PubMed] [Google Scholar]
- 173.Zheng C., Shen Z., Chang Q., Su Q., Zhu X., Gao X. Experimental study on electrostatic precipitation of low-resistivity high-carbon fly ash at high temperature. Energy Fuels. 2017;31:6266–6273. doi: 10.1021/acs.energyfuels.7b00107. [DOI] [Google Scholar]
- 174.Yang C. Aerosol filtration application using fibrous media—an industrial perspective. Chin. J. Chem. Eng. 2012;20:1–9. doi: 10.1016/S1004-9541(12)60356-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Lo Y.-Y., Wang I.-C., Lee M.-L., Chou M.-S. Removal of particulates from emissions of joss paper furnaces. Aerosol Air Qual. Res. 2011;11:429–436. doi: 10.4209/aaqr.2011.05.0062. [DOI] [Google Scholar]
- 176.Podgórski A., Bałazy A., Gradoń L. Application of nanofibers to improve the filtration efficiency of the most penetrating aerosol particles in fibrous filters. Chem. Eng. Sci. 2006;61:6804–6815. doi: 10.1016/j.ces.2006.07.022. [DOI] [Google Scholar]
- 177.Pham M., Clark C., McKenna J. The evolution and impact of testing baghouse filter performance. J. Air Waste Manag. Assoc. 2012;62:916–923. doi: 10.1080/10962247.2012.687360. [DOI] [PubMed] [Google Scholar]
- 178.Chi K.H., Chang S.H., Chang M.B. Reduction of dioxin-like compound emissions from a waelz plant with adsorbent injection and a dual baghouse filter system. Environ. Sci. Technol. 2008;42:2111–2117. doi: 10.1021/es702396y. [DOI] [PubMed] [Google Scholar]
- 179.Satoh K., Kawai T., Ishikawa M., Matsuoka T. Development of method for predicting efficiency of oil mist separators. SAE Tech. Pap. 2000 doi: 10.4271/2000-01-1234. [DOI] [Google Scholar]
- 180.Azzopardi B.J., Sanaullah K.S. Re-entrainment in wave-plate mist eliminators. Chem. Eng. Sci. 2002 doi: 10.1016/S0009-2509(02)00270-1. [DOI] [Google Scholar]
- 181.Kim J., Kim H.-J., Han B., Lee S., Lee J., Moon S., Kim Y.-J. Particle removal characteristics of a high-velocity electrostatic mist eliminator. Aerosol Air Qual. Res. 2020 doi: 10.4209/aaqr.2019.12.0648. [DOI] [Google Scholar]
- 182.Kohl A.L., Nielsen R.B. Gas Purification. Elsevier; 1997. Sulfur dioxide removal; pp. 466–669. [DOI] [Google Scholar]
- 183.King M.J., Davenport W.G., Moats M.S. Sulfuric Acid Manufacture. Elsevier; 2013. Minimizing sulfur emissions; pp. 341–348. [DOI] [Google Scholar]
- 184.Zhang Y. Advances in Ultra-Low Emission Control Technologies for Coal-Fired Power Plants. Elsevier; 2019. Fine particles characteristics of ultra-low emission coal-fired power plants; pp. 159–197. [DOI] [Google Scholar]
- 185.Giffin P.K., Parsons M.S., Waggoner C.A. A test stand for the evaluation of high efficiency mist eliminators. Rev. Sci. Instrum. 2012;83 doi: 10.1063/1.4757581. [DOI] [PubMed] [Google Scholar]
- 186.Wang S., Wang J., Song C., Wen J. Numerical investigation on urea particle removal in a spray scrubber using particle capture theory. Chem. Eng. Res. Des. 2019 doi: 10.1016/j.cherd.2019.03.011. [DOI] [Google Scholar]
- 187.Kim H.-G., Kim H.-J., Lee M.-H., Kim J.-H. Experimental study on the enhancement of particle removal efficiency in spray tower scrubber using electrospray. Asian J. Atmos. Environ. 2014;8:89–95. doi: 10.5572/ajae.2014.8.2.089. [DOI] [Google Scholar]
- 188.Chen S.-C., Tang M., Kuehn T.H., Lo C.S., Zhao D., Xie X., Sun J., Cao Q., Pui D.Y.H. Design of a rain-shower based cleaning system for simultaneous PM2.5 removal and CO2 capture of ambient air. Sep. Purif. Technol. 2020;237 doi: 10.1016/j.seppur.2019.116389. [DOI] [Google Scholar]
- 189.Shao J., Yang Y., Whiddon R., Wang Z., Lin F., He Y., Kumar S., Cen K. Investigation of NO removal with ozone deep oxidation in Na2CO3 solution. Energy Fuels. 2019;33:4454–4461. doi: 10.1021/acs.energyfuels.9b00519. [DOI] [Google Scholar]
- 190.Zhang R., Liu C., Hsu P.-C., Zhang C., Liu N., Zhang J., Lee H.R., Lu Y., Qiu Y., Chu S., Cui Y. Nanofiber air filters with high-temperature stability for efficient PM 2.5 removal from the pollution sources. Nano Lett. 2016;16:3642–3649. doi: 10.1021/acs.nanolett.6b00771. [DOI] [PubMed] [Google Scholar]
- 191.Pope C.A., Dockery D.W. Health effects of fine particulate air pollution: lines that connect. J. Air Waste Manag. Assoc. 2006;56:709–742. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- 192.Jovašević-Stojanović M., Bartonova A., Topalović D., Lazović I., Pokrić B., Ristovski Z. On the use of small and cheaper sensors and devices for indicative citizen-based monitoring of respirable particulate matter. Environ. Pollut. 2015;206:696–704. doi: 10.1016/j.envpol.2015.08.035. [DOI] [PubMed] [Google Scholar]
- 193.Bashir Shaban K., Kadri A., Rezk E. Urban air pollution monitoring system with forecasting models. IEEE Sens. J. 2016;16:2598–2606. doi: 10.1109/JSEN.2016.2514378. [DOI] [Google Scholar]
- 194.Austin E., Novosselov I., Seto E., Yost M.G. Laboratory evaluation of the Shinyei PPD42NS low-cost particulate matter sensor. PLoS One. 2015;10 doi: 10.1371/journal.pone.0137789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Dhingra S., Madda R.B., Gandomi A.H., Patan R., Daneshmand M. Internet of things mobile–air pollution monitoring system (IoT-Mobair) IEEE Internet Things J. 2019;6:5577–5584. doi: 10.1109/JIOT.2019.2903821. [DOI] [Google Scholar]
- 196.Chiang C.-T. Design of a high-sensitivity ambient particulate matter 2.5 particle detector for personal exposure monitoring devices. IEEE Sens. J. 2018;18:165–169. doi: 10.1109/JSEN.2017.2768403. [DOI] [Google Scholar]
- 197.Lai A.C.K., Nunayon S.S., Tan T.F., Li W.S. A pilot study on the disinfection efficacy of localized UV on the flushing-generated spread of pathogens. J. Hazard. Mater. 2018 doi: 10.1016/j.jhazmat.2018.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Lin W.E., Mubareka S., Guo Q., Steinhoff A., Scott J.A., Savory E. Pulsed ultraviolet light decontamination of virus-laden airstreams. Aerosol Sci. Technol. 2017;51:554–563. doi: 10.1080/02786826.2017.1280128. [DOI] [Google Scholar]
- 199.Kim J., Jang J. Inactivation of airborne viruses using vacuum ultraviolet photocatalysis for a flow-through indoor air purifier with short irradiation time. Aerosol Sci. Technol. 2018;52:557–566. doi: 10.1080/02786826.2018.1431386. [DOI] [Google Scholar]
- 200.Li Y.H., Fan Y.Z., Jiang L., Wang H.B. Aerosol and environmental surface monitoring for SARS-CoV-2 RNA in a designated hospital for severe COVID-19 patients. Epidemiol. Infect. 2020;148 doi: 10.1017/S0950268820001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Koivunen J., Heinonen-Tanski H. Inactivation of enteric microorganisms with chemical disinfectants, UV irradiation and combined chemical/UV treatments. Water Res. 2005;39:1519–1526. doi: 10.1016/j.watres.2005.01.021. [DOI] [PubMed] [Google Scholar]
- 202.Banach J.L., Sampers I., Van Haute S., van der Fels-Klerx H.J. Effect of disinfectants on preventing the cross-contamination of pathogens in fresh produce washing water. IJERPH. 2015;12:8658–8677. doi: 10.3390/ijerph120808658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Escobar L.E., Molina-Cruz A., Barillas-Mury C. BCG vaccine protection from severe coronavirus disease 2019 (COVID-19) Proc. Natl. Acad. Sci. USA. 2020;117:17720–17726. doi: 10.1073/pnas.2008410117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Liu C., Zhou Q., Li Y., Garner L.V., Watkins S.P., Carter L.J., Smoot J., Gregg A.C., Daniels A.D., Jervey S., Albaiu D. Research and development on therapeutic agents and vaccines for COVID-19 and related human coronavirus diseases. ACS Cent. Sci. 2020;6:315–331. doi: 10.1021/acscentsci.0c00272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Datta P., Mohi G., Chander J. Biomedical waste management in India: critical appraisal. J. Lab. Physicians. 2018 doi: 10.4103/jlp.jlp_89_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Wang J., Shen J., Ye D., Yan X., Zhang Y., Yang W., Li X., Wang J., Zhang L., Pan L. Disinfection technology of hospital wastes and wastewater: suggestions for disinfection strategy during coronavirus disease 2019 (COVID-19) pandemic in China. Environ. Pollut. 2020 doi: 10.1016/j.envpol.2020.114665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Singh N., Tang Y., Ogunseitan O.A. Environmentally sustainable management of used personal protective equipment. Environ. Sci. Technol. 2020;54:8500–8502. doi: 10.1021/acs.est.0c03022. [DOI] [PubMed] [Google Scholar]
- 208.Rowan N.J., Laffey J.G. Challenges and solutions for addressing critical shortage of supply chain for personal and protective equipment (PPE) arising from coronavirus disease (COVID19) pandemic – case study from the Republic of Ireland. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Sun J., Zhuang Z., Zheng J., Li K., Wong R.L.-Y., Liu D., Huang J., He J., Zhu A., Zhao J., Li X., Xi Y., Chen R., Alshukairi A.N., Chen Z., Zhang Z., Chen C., Huang X., Li F., Lai X., Chen D., Wen L., Zhuo J., Zhang Y., Wang Y., Huang S., Dai J., Shi Y., Zheng K., Leidinger M.R., Chen J., Li Y., Zhong N., Meyerholz D.K., McCray P.B., Perlman S., Zhao J. Generation of a broadly useful model for COVID-19 pathogenesis, vaccination, and treatment. Cell. 2020;182:734–743.e5. doi: 10.1016/j.cell.2020.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Cohen J., Kupferschmidt K. Vaccine designers take first shots at COVID-19: two candidate vaccines start trials while dozens more are rushed into development. Science. 2020 doi: 10.1126/science.368.6486.14. (80-.) [DOI] [PubMed] [Google Scholar]
- 211.Cohen J. Vaccine designers take first shots at COVID-19. Science. 2020;368:14–16. doi: 10.1126/science.368.6486.14. (80-.) [DOI] [PubMed] [Google Scholar]
- 212.Mehra M.R., Desai S.S., Kuy S., Henry T.D., Patel A.N. Retraction: cardiovascular disease, drug therapy, and mortality in Covid-19. N. Engl. J. Med. 2020;382:2582. doi: 10.1056/NEJMoa2007621. doi: 10.1056/NEJMoa2007621. 2582–2582. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 213.Abd El-Aziz T.M., Stockand J.D. Recent progress and challenges in drug development against COVID-19 coronavirus (SARS-CoV-2) – an update on the status. Infect. Genet. Evol. 2020;83 doi: 10.1016/j.meegid.2020.104327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Magro G. COVID-19: review on latest available drugs and therapies against SARS-CoV-2. Coagulation and inflammation cross-talking. Virus Res. 2020;286 doi: 10.1016/j.virusres.2020.198070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Sanders J.M., Monogue M.L., Jodlowski T.Z., Cutrell J.B. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. JAMA. 2020 doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 216.Tahir ul Qamar M., Alqahtani S.M., Alamri M.A., Chen L.-L. Structural basis of SARS-CoV-2 3CLpro and anti-COVID-19 drug discovery from medicinal plants. J. Pharm. Anal. 2020;10:313–319. doi: 10.1016/j.jpha.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Mohammad T., Shamsi A., Anwar S., Umair M., Hussain A., Rehman M.T., AlAjmi M.F., Islam A., Hassan M.I. Identification of high-affinity inhibitors of SARS-CoV-2 main protease: towards the development of effective COVID-19 therapy. Virus Res. 2020;288 doi: 10.1016/j.virusres.2020.198102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Li T., Liu Y., Li M., Qian X., Dai S.Y. Mask or no mask for COVID-19: A public health and market study. PLoS One. 2020;15 doi: 10.1371/journal.pone.0237691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Cheng V.C.-C., Wong S.-C., Chuang V.W.-M., So S.Y.-C., Chen J.H.-K., Sridhar S., To K.K.-W., Chan J.F.-W., Hung I.F.-N., Ho P.-L., Yuen K.-Y. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020;81:107–114. doi: 10.1016/j.jinf.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.World Health Organization, Rational Use of Personal Protective Equipment for Coronavirus Disease (COVID-19) and Considerations During Severe Shortages: Interim Guidance, World Health Organization, 6 April 2020. 〈https://apps.who.int/iris/handle/10665/331695〉. (Accessed 30 September 2020).
- 221.World Health Organization, Advice on the Use of Masks in the Community, During Home Care and in Health Care Settings in the Context of the Novel Coronavirus (2019-nCoV) Outbreak: Interim Guidance, World Health Organization, 29 January 2020. 〈https://apps.who.int/iris/handle/10665/330987〉. (Accessed 30 September 2020).
- 222.World Health Organization, Advice on the Use of Masks in the Context of COVID-19: Interim Guidance, World Health Organization, 5 June 2020. 〈https://apps.who.int/iris/handle/10665/332293〉. (Accessed 20 October 2020).
- 223.Clemens K.S., Matkovic J., Faasse K., Geers A.L. Determinants of safety-focused product purchasing in the United States at the beginning of the global COVID-19 pandemic. Saf. Sci. 2020;130 doi: 10.1016/j.ssci.2020.104894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Klemeš J.J., Van Fan Y., Jiang P. The energy and environmental footprints of COVID-19 fighting measures – PPE, disinfection, supply chains. Energy. 2020 doi: 10.1016/j.energy.2020.118701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Jessop Z.M., Dobbs T.D., Ali S.R., Combellack E., Clancy R., Ibrahim N., Jovic T.H., Kaur A.J., Nijran A., O’Neill T.B., Whitaker I.S. Personal protective equipment (PPE) for surgeons during COVID-19 pandemic: a systematic review of availability, usage, and rationing: cutting edge review. Br. J. Surg. 2020 doi: 10.1002/bjs.11750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Yuan L., Zhi N., Yu C., Ming G., Yingle L., Nirmal Kumar G., Li S., Yusen D., Jing C., Dane W., Xinjin L., Kin-fai H., Haidong K., Qingyan F., Ke L. Aerodynamic characteristics and RNA concentration of SARS-CoV-2 aerosol in Wuhan hospitals during COVID-19 outbreak. BioRxiv. 2020 doi: 10.1101/2020.03.08.982637. [DOI] [Google Scholar]
- 227.Mahmood A., Eqan M., Pervez S., Alghamdi H.A., Tabinda A.B., Yasar A., Brindhadevi K., Pugazhendhi A. COVID-19 and frequent use of hand sanitizers; human health and environmental hazards by exposure pathways. Sci. Total Environ. 2020;742 doi: 10.1016/j.scitotenv.2020.140561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Paital B., Das K., Parida S.K. Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Paital B. Nurture to nature via COVID-19, a self-regenerating environmental strategy of environment in global context. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.139088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.EPA, Particulate Matter (PM2.5) Trends, 2020. 〈https://www.epa.gov/air-trends/particulate-matter-pm25-trends〉.
- 231.Kanniah K.D., Kamarul Zaman N.A.F., Kaskaoutis D.G., Latif M.T. COVID-19’s impact on the atmospheric environment in the Southeast Asia region. Sci. Total Environ. 2020;736 doi: 10.1016/j.scitotenv.2020.139658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.D. Child, The Positive Impacts on the Environment Since the Coronavirus Lockdown Began, 2020. 〈https://www.standard.co.uk/news/world/positive-impact-environment-coronavirus-lockdown-a4404751.html〉. (Accessed 24 September 2020).
- 233.J. Watts Climate crisis: in coronavirus lockdown, nature bounces back – but for how long? Guard, 2020. <https://www.theguardian.com/world/2020/apr/09/climate-crisis-amid-coronavirus-lockdown-nature-bounces-back-but-for-how-long>. (Accessed 30 September 2020).
- 234.Cheke R.S., Shinde S., Ambhore J., Adhao V., Cheke D. Coronavirus: hotspot on coronavirus disease 2019 in India. IJMS. 2020;72:29–34. doi: 10.25259/IJMS_33_2020. [DOI] [Google Scholar]
- 235.Almutairi N., Schwartz R.A. COVID‐19 with dermatologic manifestations and implications: an unfolding conundrum. Dermatol. Ther. 2020;33 doi: 10.1111/dth.13544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Kumari P., Toshniwal D. Impact of lockdown measures during COVID-19 on air quality–a case study of India. Int. J. Environ. Health Res. 2020:1–8. doi: 10.1080/09603123.2020.1778646. [DOI] [PubMed] [Google Scholar]
- 237.Muhammad S., Long X., Salman M. COVID-19 pandemic and environmental pollution: a blessing in disguise? Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Kostoff R., Briggs M., Porter A., Aschner M., Spandidos D., Tsatsakis A. [Editorial] COVID‑19: post‑lockdown guidelines. Int. J. Mol. Med. 2020;46:463–466. doi: 10.3892/ijmm.2020.4640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Soni V., Singh P., Shree V., Goel V. Air Pollution and Control. 2018. Effects of VOCs on human health; pp. 119–142. [DOI] [Google Scholar]
- 240.Ghio A.J., Huang Y.-C.T. Exposure to concentrated ambient particles (CAPs): a review. Inhal. Toxicol. 2004;16:53–59. doi: 10.1080/08958370490258390. [DOI] [PubMed] [Google Scholar]
- 241.Yun Y., Gao R., Yue H., Li G., Zhu N., Sang N. Synergistic effects of particulate matter (PM10) and SO2 on human non-small cell lung cancer A549 via ROS-mediated NF-κB activation. J. Environ. Sci. 2015;31:146–153. doi: 10.1016/j.jes.2014.09.041. [DOI] [PubMed] [Google Scholar]
- 242.Bor-Kucukatay M., Wenby R.B., Meiselman H.J., Baskurt O.K. Effects of nitric oxide on red blood cell deformability. Am. J. Physiol. Circ. Physiol. 2003;284:H1577–H1584. doi: 10.1152/ajpheart.00665.2002. [DOI] [PubMed] [Google Scholar]
- 243.Kang Y.S., Kim S.S., Hong S.C. Combined process for removal of SO2, NOx, and particulates to be applied to a 1.6-MWe pulverized coal boiler. J. Ind. Eng. Chem. 2015;30:197–203. doi: 10.1016/j.jiec.2015.05.022. [DOI] [Google Scholar]
- 244.World Health Organization (WHO), WHO Coronavirus Disease (COVID-19) Dashboard, World Health Organization, 2020. 〈https://covid19.who.int/〉. (Accessed 15 October 2020).
- 245.IQAir, World Air Quality Report, 2019. World Air Quality Report, 2020, pp. 1–22. 〈https://www.iqair.com/world-most-polluted-cities/world-air-quality-report-2019-en.pdf〉. (Accessed 15 October 2020).
- 246.IQAir, Air Quality and Pollution City Ranking, IQAir, 2020. 〈https://www.iqair.com/us/world-air-quality-ranking〉. (Accessed 15 October 2020).