Abstract
Undocumented immigrants have disproportionately suffered during the novel coronavirus disease 2019 (COVID-19) pandemic due to factors including limited medical access and financial insecurity, which can exacerbate pandemic-associated distress. Psychological outcomes for immigrant outpatients were assessed after transition to telepsychiatry in March 2020. Mental health was assessed with Patient Health Questionnaire (PHQ-2) and Generalized Anxiety Disorder (GAD-2) inventories, a novel coronavirus-specific survey, and the Kessler Psychological Distress Scale (K10+). Feedback on telepsychiatry sessions and access to non-clinical resources were also gathered, after which multivariable linear regression modeling identified psychosocial factors underlying changes in distress levels. 48.57% and 45.71% of participants reported worsened anxiety and depression levels due to the pandemic, respectively. From March to April, PHQ-2 and GAD-2 scores significantly increased by 0.81 and 0.63 points, respectively. The average total psychological distress score was 23.8, with 60% of scores reflecting serious mental illness. Factors that most influenced K10+ scores included a pre-existing depressive disorder, food insecurity, and comfort during telepsychiatry visits. 93.75% of participants believed access to remote psychiatry helped their mental health during COVID-19. The negative impact of COVID-19 on mental health in vulnerable populations stems from medical and psychosocial factors such as pre-existing psychiatric conditions and unmet essential needs.
Keywords: COVID-19, Mental health, Telepsychiatry, Vulnerable populations, Anxiety, Depression, Distress
1. Introduction
The sweeping effects of the COVID-19 pandemic have led to increased levels of psychological distress and psychiatric symptoms worldwide (Fitzpatrick et al., 2020; Ozamiz-Etxebarria et al., 2020; Ettman et al., 2020; Sønderskov et al., 2020; Wang et al., 2020). While necessary stay-at-home and social distancing orders have slowed spread of the disease (Davies et al., 2020; Tian et al., 2020), they have also produced substantial socio-economic fallout highlighted by devastating job losses and an increased demand for unemployment benefits (Bureau of Labor Statistics, 2020). Because job loss and financial instability are associated with adverse psychological outcomes, the COVID-19 pandemic presents a scenario in which unprecedented numbers of people are at increased risk for psychological distress.
The psychological impact of the COVID-19 pandemic may be compounded among populations already affected by psychosocial factors that place them at heightened psychiatric risk, including poverty and undocumented immigration status (Garcini et al., 2016; Cabral et al., 2020). Difficulties with employment and/or finances are frequently reported as factors that lead to negative psychological outcomes among immigrant populations (Tang et al., 2007), and financial stress has been associated with heightened psychiatric risk (Ezzy, 1993). Therefore, exacerbation of social disparities and disproportionate job loss among low-income families during the COVID-19 pandemic may place undocumented immigrant populations at particularly high risk for adverse psychological impacts (Cénat et al., 2020). Furthermore, existing literature suggests that impoverished, immigrant, and minority communities are already at risk of increased incidence and worsened severity of COVID-19 (Finch and Hernandez Finch, 2020; Maroko et al., 2020). When coupled with the aforementioned levels of psychiatric distress encountered by COVID-19-striken communities, these risk factors suggest a high predisposition to negative mental health outcomes in undocumented immigrant populations. As sparse literature exists on the mental health outcomes of immigrants in a resource-limited pandemic environment, our group set out to characterize the psychological impact of the pandemic on Hispanic psychiatric outpatients in East Harlem, while also elucidating socioeconomic variables that might influence their mental health under such stressful conditions. We hypothesized that increased health risks and financial restrictions would lead to worsened depression, anxiety, and distress.
The following observational study highlights changes in levels of anxiety and depression in a vulnerable outpatient population due to the COVID-19 pandemic through longitudinal PHQ-2 and GAD-2 tracking, a novel coronavirus-specific mental healthcare survey, and the Kessler Psychological Distress Scale K10+. Surveys on telepsychiatry feedback and access to necessities were performed in order to validate this treatment model for future states of emergency and to identify socioeconomic factors that may further exacerbate negative impacts on mental health. Given that no quantitative literature exists on the mental health outcomes of COVID-19 among undocumented immigrants, our results provide the first systematic investigation of pandemic-related mental health care for this population. Using a variety of measures, we found evidence of acute psychological distress and exacerbation of psychiatric symptoms. Furthermore, data collected from feedback surveys and subsequent integrated analyses shed light on factors associated with differential psychological distress among our patient population.
2. Methods
2.1. Research setting and patient population
The East Harlem Health Outreach Partnership (EHHOP) is a free medical clinic that currently serves over 300 members of the East Harlem community in the Manhattan borough of New York City (Liberman et al., 2011). In order to qualify for care at EHHOP, individuals must demonstrate ineligibility to receive health insurance under current policies. This criterion can be met by lacking residency documentation. The EHHOP Mental Health Clinic (MHC) serves 58 patients, with dedicated attending residents and physicians, in-clinic pharmaceutical dispensing, and referral capabilities to legal and social service teams (Mann et al., 2019; Warburton et al., 2019).
At the start of the study period (March 2020), patients actively receiving in-person counseling, psychotherapy, and/or psychopharmaceutical treatment from the MHC were transitioned to telepsychiatry in order to reduce the risk of SARS-CoV-2 infection. Patients maintained the same care regimens and providers for their telehealth visits. All clinic visits during the pandemic happened over telephone, with the exception of video-based intake psychiatric assessments (n=2; WhatsApp). However, all data captured for this study was post-intake and therefore over the telephone. After the transition, patients were contacted via telephone regarding participation in mental health surveys; participation was optional, and patients were informed that decision to participate would in no way impact the status of their care. Demographic information on participants, including gender, age, ethnicity, and psychiatric diagnoses, was aggregated via retrospective chart review. Psychiatric diagnoses were grouped under the categories of “depressive disorder” (includes diagnoses of major depressive disorder, persistent depressive disorder, nonspecific depressive disorder, complex grief/persistent complex bereavement disorder), “anxiety disorder” (includes diagnoses of generalized anxiety disorder, somatic symptom disorder, panic disorder, social anxiety disorder, other anxiety disorder), “post-traumatic stress disorder”, “alcohol use disorder”, and “adjustment disorder”.
This study was approved by the institutional review board at the Icahn School of Medicine at Mount Sinai (HS#: 20–01114 | GCO#1: 20–2148 ISMMS). A certificate of confidentiality was secured from the National Institutes of Health to ensure the protection of privileged information received from immigrants involved in this study.
2.2. Mental health surveys
2.2.1. PHQ-2 & GAD-2
The PHQ-2 and GAD-2 questionnaires are well-validated, abridged methods of monitoring depression and anxiety, respectively (Löwe et al., 2005; Plummer et al., 2016). Other groups have previously validated the administration of these or similar inventories in non-clinical environments (Donker et al., 2011; Bell et al., 2015; Tran et al., 2019), with further evidence supporting their remote use in migrant populations (Kerkenaar et al., 2013). These questions were asked via telephone in Spanish by either native Spanish-speaking providers or translated from English by professional Spanish translators (PSTs) as a screening method during visit-scheduling calls or at the beginning of appointment sessions in March and April. For both PHQ-2 and GAD-2, we considered a score of 3 or above as a “positive” screening result (Kroenke et al., 2003; Plummer et al., 2016). If a patient had more than one assessment per month, they were averaged together.
2.2.2. COVID-19 Mental Health Survey
We designed a novel COVID-19-specific survey in order to identify changes in mental health directly attributable to the pandemic. This tool measures pandemic-related changes in anxiety and depression levels, acquaintance with individuals that tested positive for the virus, belief that an acquaintance is infected without having had viral testing, fear of contracting coronavirus, and perception of access to appropriate healthcare resources in case of infection (Appendix A). The survey questions were designed on a Likert scale and delivered to participants once in April or May via telephone by a native Spanish speaker.
2.2.3. Kessler Psychological Distress Scale – K10+
The Kessler Psychological Distress Scales are well validated measures of clinically significant, non-specific distress that are used to screen for serious mental illness (Kessler et al., 2003). They have been translated into Spanish and validated in several Central and South American countries (Kessler et al., 2010). These scales have been used for standardized mental health assessments in migrant populations (Dallo et al., 2013; Bekteshi and van Hook, 2015), and for measurements of distress during disease outbreaks (Taylor et al., 2008) as with COVID-19 in Italy (Moccia et al., 2020). We administered the K10+, which offers the additional advantage of assessing impairment in daily functioning. Scores range from 10–50. A score of ≥20 represent serious mental illness, with subcategories of “mild” (20–24), “moderate” (25–29), and “severe” (30+) (Andrews and Slade, 2001; Kessler et al., 2002). We provided the K10+ to our patient population once in May via telephone by a native Spanish speaker.
2.2.4. Telepsychiatry Feedback Survey
We modified previously published migrant-focused telepsychiatry feedback surveys (Mucic, 2008, 2010) to better understand the impact of telepsychiatry availability on pandemic-induced changes in anxiety and depression levels, as well as to receive feedback on levels of comfort, safety, and expressivity during telepsychiatry sessions (Appendix B). The survey questions were designed on a Likert scale and delivered to participants once in April or May via telephone by a native Spanish speaker or English speaker with a PST.
2.2.5. Access to Necessities Survey
Considering the lack of stimulus support and health insurance for our patient population, we designed a brief survey with dichotomous (Yes/No) questions assessing participants’ coronavirus-related difficulties with paying rent and utilities, receiving income, receiving medical attention, and obtaining food and/or medication (Appendix C). This survey was delivered once in May by a native Spanish speaker via telephone.
2.3. Statistics
All analyses were performed in R Studio version 1.3. Paired t-tests were used for the repeated measures assessment of PHQ-2 and GAD-2 from March to April, and McNemar Chi-Square tests with continuity correction measured changes in the proportion of participants with positive PHQ-2 or GAD-2 results during that time. Relationships between categorical variables, including survey responses, were analyzed with Pearson's Chi-Square (χ2) tests; because of our study's small sample size, all tests employed Monte Carlo simulation with 2,000 replicates. Strength of linear relationships between continuous variables was measured with Pearson's product moment correlation. Potential differences in K10+ scores among multiple groups of participants were examined with one-way analysis of variation (ANOVA) with Tukey post-hoc tests. Multivariable linear regression was employed to assess the impact of various demographic, psychosocial, and clinical factors on total psychological distress scores. Variable selection for the final regression model was performed utilizing Akaike information criterion (AIC) (Akaike, 1973, 1974). For all statistical tests, p<0.05 was considered significant.inf
3. Results
3.1. Demographics
A total of 48 patients at the MHC were effectively transitioned to telepsychiatry between February and March of 2020. One patient was not transitioned due to an inability to be reached via telephone. Two patients declined to be included in the study prior to survey administration. As surveys were administered at staggered times over the months of April and May, the availability of participants to answer surveys varied due to many patients being unreachable via telephone during specific survey administration time periods. Demographic data for the participants who responded to each survey are detailed in Table 1. The surveyed population was 100% Hispanic, and 74–80% of respondents were female across the different survey assessments. “Depressive Disorder” was the most prevalent disorder across all survey groups, followed by “Anxiety Disorder” and “Post-traumatic Stress Disorder”. The largest age group was 40–49 years-old, representing slightly less than half of all participants in all survey groups.
Table 1.
Participant Demographics. This table provides a breakdown of the patient sample by gender, age, ethnicity, and pre-existing psychiatric diagnosis. Sample sizes are unweighted, with 28–35 participants completing each survey tool. “Depressive Disorder” includes major depressive disorder, persistent depressive disorder, nonspecific depressive disorders, and complex grief/persistent complex bereavement disorder; “Anxiety Disorder” includes generalized anxiety disorder, somatic symptom disorder, panic disorder, social anxiety disorder, and other anxiety disorders.
| PHQ-2 N (%) | GAD-2 N (%) | COV1D-19 Mental Health Survey N (%) | K10+ N (%) | Access to Necessities Survey N (%) | Telepsychiatry Feedback Survey N (%) | |
|---|---|---|---|---|---|---|
| Total | 28 (100%) | 30 (100%) | 35 (100%) | 34 (100%) | 34 (100%) | 32 (100%) |
| Gender | ||||||
| Male | 7 (25%) | 6 (20%) | 9 (26%) | 8 (24%) | 8 (24%) | 8 (25%) |
| Female | 21 (75%) | 24 (80%) | 26 (74%) | 26 (76%) | 26 (76%) | 24 (75%) |
| Age | ||||||
| 20–29 | 1 (4%) | 1 (3%) | 2 (6%) | 2 (6%) | 2 (6%) | 1 (3%) |
| 30–39 | 6 (21%) | 5 (17%) | 6 (17%) | 5 (15%) | 5 (15%) | 6 (19%) |
| 40–49 | 13 (46%) | 14 (47%) | 17 (49%) | 14 (41%) | 15 (44%) | 15 (47%) |
| 50–59 | 5 (18%) | 6 (20%) | 6 (17%) | 8 (24%) | 8 (24%) | 7 (22%) |
| 60–69 | 2 (7%) | 3 (10%) | 3 (9%) | 3 (9%) | 2 (6%) | 3 (9%) |
| 70–79 | 1 (4%) | 1 (3%) | 1 (3%) | 2 (6%) | 2 (6%) | 0 (0%) |
| Ethnicity | ||||||
| Hispanic | 28 (100%) | 30 (100%) | 35 (100%) | 34 (100%) | 34 (100%) | 32 (100%) |
| Diagnosis | ||||||
| Depressive Disorder | 12 (43%) | 13 (43%) | 14 (40%) | 13 (38%) | 14 (41%) | 14 (44%) |
| Anxiety Disorder | 10 (36%) | 11 (37%) | 10 (29%) | 10 (29%) | 11 (32%) | 11 (34%) |
| Post-traumatic Stress Disorder | 5 (18%) | 6 (20%) | 8 (23%) | 9 (26%) | 8 (24%) | 9 (28%) |
| Alcohol Use Disorder | 4 (14%) | 3 (10%) | 4 (11%) | 3 (9%) | 3 (9%) | 4 (13%) |
| Adjustment Disorder | 2 (7%) | 3 (10%) | 5 (14%) | 4 (12%) | 4 (12%) | 4 (13%) |
3.2. Impact of COVID-19 on mental health
3.2.1. PHQ-2 & GAD-2
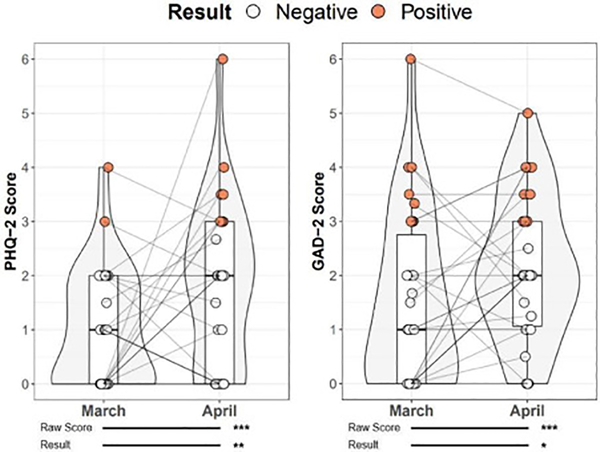
To determine if depressive and anxiety symptoms worsened over time during the COVID-19 pandemic, we examined longitudinal scores from PHQ-2 and GAD-2, respectively. PHQ-2 data was available for 28 participants in the months of both March and April, while GAD-2 data was available for 30 participants. Paired t-testing revealed that PHQ-2 scores increased by an average of 0.81 points per patient from March to April (95% CI: 0.057–1.05, t=7.01, df=27, p<0.0001; Fig. 1). Similarly, GAD-2 scores increased by an average of 0.63 points per patient from March to April (95% CI: 0.40–0.85, df=29, t=5.79, p<0.0001; Fig. 1). We next explored whether the proportion of participants meeting the threshold for a positive result on both measures changed between the months of March and April. We found a significant difference between the proportion of participants who had positive scores on the PHQ-2 in March (2 patients; 7.14%) and April (8 patients; 28.57%) (McNemar with continuity correction, χ2=8.5, p=0.004; Fig. 1). A similar increase in the proportion of participants with positive GAD-2 scores was seen between March (8 patients; 26.67%) and April (10 patients; 33.33%) (χ2=3.78, p=0.05; Fig. 1). Of note, we hypothesize that a substantial portion of patients scored below the “positive” threshold despite having diagnoses of depressive and/or anxiety disorders due to regular psychotherapy and/or pharmacotherapy treatment. Potential causes of these score elevations could include a reduction in the efficacy of remote therapy and substantial pandemic-related stress. Thus, COVID-19-specific and telepsychiatry feedback surveys were implemented.
Figure 1.
Change in PHQ-2 and GAD-2 Scores During the Early Months of the COVID-19 Pandemic. N=28 and N=30 participants completed the PHQ-2 and GAD-2, respectively, in both March and April. Comparison of PHQ-2 and GAD-2 raw scores (PHQ-2 95% CI: 0.057–1.05, t=7.01, df=27, p<0.0001; GAD-2 95% CI: 0.40–0.85, df=29, t=5.79, p<0.0001) and positive test thresholds between March and April (PHQ-2 McNemar with continuity correction, χ2=8.5, p=0.004; GAD-2 χ2=3.78, p=0.05).
3.2.2. COVID-19 Mental Health Survey
35 participants completed the COVID-19 Mental Health Survey (Table 2). 17 (48.57%) and 16 (45.71%) respondents reported increased levels of anxiety and depression due to COVID-19, respectively. While only 2 (5.71%) participants reported decreased anxiety during the pandemic, 8 (22.86%) reported a decrease in depression levels. A substantial number of participants reported no change in anxiety and depression levels (16 (45.71%) and 11 (31.43%), respectively). 21 (60.00%) participants stated that they knew an individual who tested positive for coronavirus, and 10 (28.57%) reported suspecting that an acquaintance had been infected who had not yet been tested. 20 (57.14%) participants reported being worried about contracting coronavirus. Only 2 (5.71%) participants reported perceiving a lack of access to medical care should they become infected, 10 (28.57%) believed they did have adequate access to healthcare, and 23 (65.71%) were unsure.
Table 2.
COVID-19 Mental Health Survey Responses. 35 participants completed this survey. This survey included script recommendations (see Appendix A).
| Q1. How would you rate your level of anxiety due to the coronavirus pandemic? My level of anxiety is... | Much lower than normal | Somewhat lower than normal | The same as normal | Somewhat higher than normal | Much higher than normal |
| N (%) | 1 (2.86%) | 1 (2.86%) | 16 (45.71%) | 12 (34.29%) | 5 (14.29%) |
| Q2. How would you rate your level of depression due to the coronavirus pandemic? My level of depression is... | Much lower than normal | Somewhat lower than normal | The same as normal | Somewhat higher than normal | Much higher than normal |
| N (%) | 1 (2.86%) | 7(20.00%) | 11 (31.43%%) | 12 (34.29%) | 4 (11.43%) |
| Q3. Do you know someone who tested positive for coronavirus? | No | Yes, someone 1 am acquainted with | Yes, someone I am close to but do not live with | Yes, someone 1 live with | |
| N (%) | 14 (40.00%) | 8 (22.86%) | 9 (25.71%) | 4 (11.43%) | |
| Q4. Do you know someone who you think has coronavirus, but has not been able to be tested? | No | Yes, someone 1 am acquainted with | Yes, someone 1 am close to but do not live with | Yes, someone 1 live with | |
| N (%) | 25 (71.43%) | 2 (5.71%) | 6 (17.14%) | 2 (5.71%) | |
| Q5. Please tell us your level of agreement with the following statement: “1 worry about getting coronavirus.” | Strongly disagree | Disagree | Neutral | Agree | Strongly agree |
| N (%) | 0 (0.00%) | 7 (20.00%) | 8 (22.86%) | 14 (40.00%) | 6 (17.14%) |
| Q6. If you think you had coronavirus, do you think you would have access to the appropriate healthcare resources for treatment? | Yes | No | 1 am not sure | ||
| N (%) | 10 (28.57%) | 2 (5.71%) | 23 (65.71%) |
The overarching goal of the COVID-19 Mental Health Survey was to more clearly define changes in perceived levels of anxiety and depression in our patient population due to various pandemic factors, such as infection status of acquaintances or fear of contracting the virus. First, we determined that pandemic-related changes in anxiety and depression levels were directly related. Participants who reported a “much higher” level of anxiety due to coronavirus were more likely to feel that their level of depression was “much higher” as well (χ2=94.40, p=0.0005), with similar direct relationships for “somewhat higher”-“somewhat higher” and “much lower”-“much lower” (Supplementary Table 1.A). Furthermore, we found that lack of acquaintance with someone who was infected with coronavirus led to a higher likelihood of reporting “about the same” level of depression (χ2=67.66, p=0.0005), while living with an infected individual was strongly related to “much higher” levels of depression (Supplementary Table 1.B). We found a similar correspondence between knowing someone who tested positive for coronavirus and self-reported levels of anxiety (χ2=52.23, p=0.0005) (Supplementary Table 1.C). If participants suspected that an untested individual who was “living with” them had coronavirus, they were more likely to report “much higher” levels of anxiety (χ2=30.63, p=0.001) and depression (χ2=32.74, p=0.003) (Supplementary Tables 2.D and 2.E). Finally, we found that individuals were more likely to “strongly agree” that they were worried about getting coronavirus if they had “much higher” depression (χ2=65.58, p=0.0005) or anxiety (χ2=56.58, p=0.0005) levels due to the pandemic; “neutral” concern about contracting coronavirus meant a higher likelihood of reporting “about the same” levels of depression or anxiety during the pandemic (Supplementary Tables 2.F and 2.G). Regarding perceived access to medical care, those who believed they did have access were more likely to report that their levels of depression were “somewhat lower” (χ2=31.76, p=0.0005) (Supplementary Table 1.H). The belief that one would not have access to the appropriate healthcare resources was not strongly associated with responses to questions about pandemic-related changes to levels of anxiety (χ2=19.67, p=0.08) (Supplementary Table 1.I). However, those who agreed that they were worried about contracting coronavirus were less likely to believe they would have access to the appropriate healthcare resources (χ2=34.33, p=0.0005), while those who disagreed were more likely to believe they did have access (Supplementary Table 1.J).
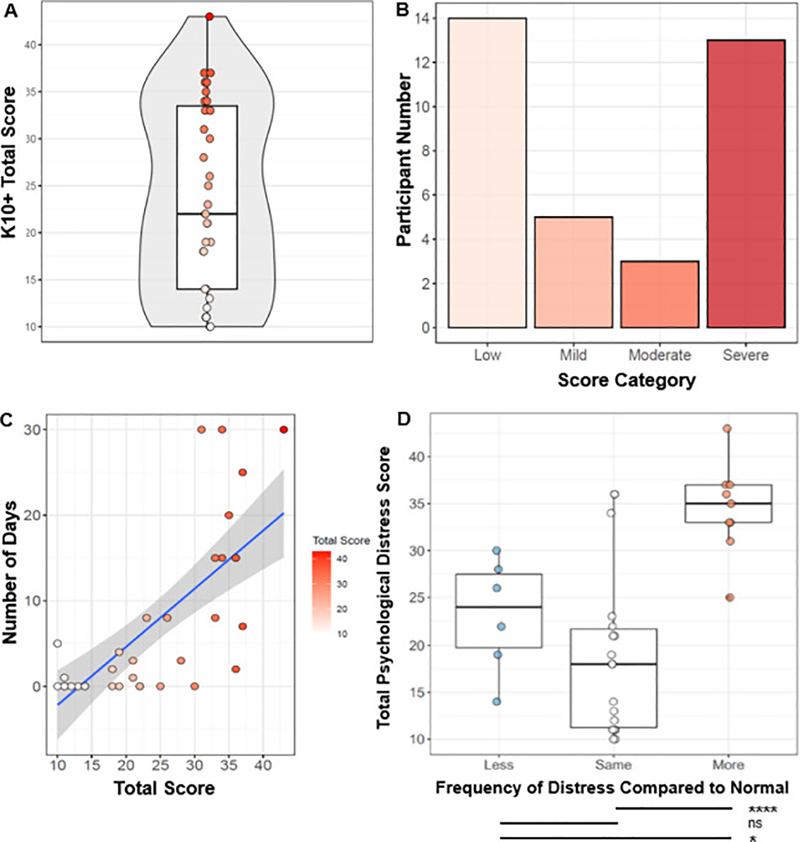
3.2.3. Kessler Psychological Distress Scale K10+
A total of 35 participants completed the K10+. Scores ranged from 10 to 43 and had a mean of 23.8 and a median of 22.0 (Fig. 2.A). 14 (40.00%) participants scored <20 and were considered “Low Risk”; 5 (14.29%) scored in the “Mild” range of 20–24; 3 (8.57%) scored in the “Moderate” range of 25–29; and finally, 13 (37.14%) scored in the “Severe” range of 30+ (Fig. 2.B). On Question 3 (Q3), which asks about the number of days in the past 30 days that participants were unable to work or carry out normal activities, answers ranged from 0 to 30 and had a mean of 7.2 and a median of 3.0. We found a significant, positive correlation between the number of days unable to work or carry out normal activities and total distress scores (Pearson's product moment correlation, r=0.71, p<0.0001; Fig. 2.C). We then grouped responses to Question 2 (Q2), which asks participants about the frequency of the feelings assessed in Question 1 (Q1) in comparison to what is usual for them, into “More Frequent”, “About the Same”, and “Less Frequent” and tested whether total distress scores varied by participants’ perceptions of the frequency of those feelings relative to what is usual for them. There was a significant difference in total psychological distress scores among different perceived frequencies of distress relative to what is usual for the patient by one-way ANOVA (F(2,28)=15.99, p<0.0001) (Fig. 2.D). A Tukey post-hoc test revealed that those who responded that their feelings of distress in the past 30 days were “More Frequent” than usual had total distress scores that were 16.1 points higher on average than those who responded “About the Same” (p<0.0001) and 11.3 points higher on average than those who responded “Less Frequent” (p=0.02). There were no differences in total distress scores between those who responded “About the Same” and “Less Frequent” (p=0.32). This suggests that those experiencing higher levels of distress were more likely to experience these elevated levels of distress more frequently than usual in the past 30 days, consistent with the hypothesis that the COVID-19 pandemic may be leading to exacerbated distress in our patient population.
Figure 2.
Summary of Key Psychological Distress Survey Findings. N=35 participants completed the K10+ survey. A) The median psychological distress score was a 22.0, with individual scores ranging from 10–43. B) Participant response tranches were as follows: 14 (40%) participants were considered “Low Risk” (score<20); 5 (14.29%) “Mild” (score=20–24); 3 (8.57%) “Moderate” (score=25–29); 13 (37.14%) “Severe” (score>29). C) Correlation between responses to Q3 and K10+ psychological distress scores (r2 = 0.71, p<0.0001). D) Comparison between K10+ psychological distress scores and frequency of distress (one-way ANOVA (F(2,28)=15.99, p<0.0001) (*p<0.05, ****p<0.0001).
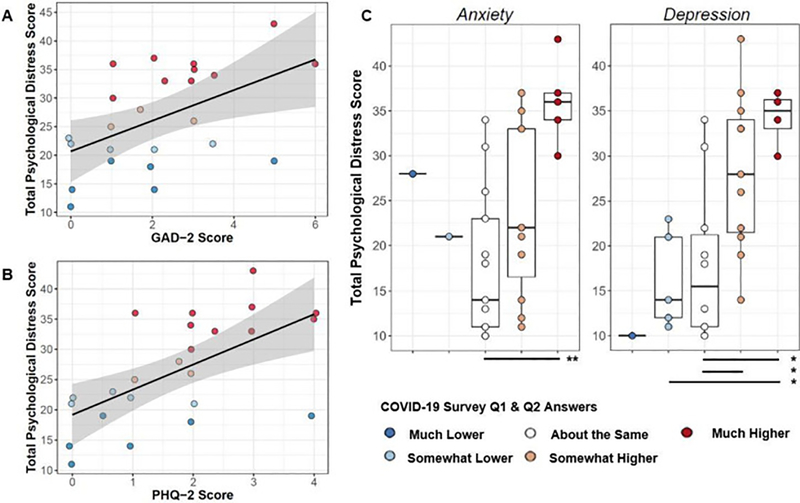
When examining K10+ scores along with GAD-2 and PHQ-2 data from the 30 days prior to K10+ administration (April-May), we found a significant correlation between GAD-2 (r=0.51; p=0.01; Fig. 3.A) and PHQ-2 (r=0.61; p=0.001; Fig. 3.B) and total K10+ scores. Consistent with prior literature (Van Heyningen et al., 2018; Staples et al., 2019), those with positive GAD-2 screens (score of 3 or greater) had total psychological distress scores that were 8.91 points (95% CI: 2.45–15.40) points higher than those with a negative GAD-2 screen (31.70 versus 22.79, t=2.87, df=20.45, p=0.009). Similarly, those with positive PHQ-2 screens (score of 3 or higher) had total psychological distress scores that were 10.18 points (95% CI: 2.94–17.43) higher than those with a negative PHQ-2 screen (33.71 versus 23.53, t=3.08, df=11.49, p=0.01). Furthermore, we found that PHQ-2 scores differed significantly among the total psychological distress categories of low risk, mild, moderate, and severe (one-way ANOVA: F(3,20)=4.165, p=0.02); GAD-2 scores did not differ significantly among distress categorizations (one-way ANOVA: F(3,20)=1.587, p=0.2). Overall, this evidence suggests that the combination of standardized psychological distress tools, longitudinal anxiety and depression inventories (i.e. GAD-2 & PHQ-2), and novel situation-specific surveys allow for a comprehensive and validated strategy for event-specific mental health gauging.
Figure 3.
Inter-inventory Comparisons of Participant Mental Health Outcomes. A) Correlation between psychological distress scores and GAD-2 scores (r2 = 0.61; p = 0.001). B) Correlation between K10+ psychological distress scores and PHQ-2 scores (r2 = 0.51; p = 0.01). For A and B, color of individual data point corresponds to magnitude of psychological distress score. C) Comparison between K10+ psychological distress scores and COVID-19 Mental Health Survey Q1 (Anxiety) and Q2 (Depression) (Q1 one-way ANOVA F(4,27)=5.146, p=0.003; Q2 F(4,27)=4.545, p=0.006) (*p<0.05, **p<0.001).
We next sought to explore relationships between responses to our COVID-19 survey assessing pandemic-specific aspects of distress and the more general psychological distress measured by the K10+. A total of 32 participants completed both surveys. A one-way ANOVA revealed a significant relationship between total psychological distress scores and responses to Q1 of our COVID-19 survey asking about levels of anxiety due to the pandemic (F(4,27)=5.146, p=0.003; Fig. 3.C). Tukey post-hoc analysis indicated that those who responded that their anxiety was “Much Higher” due to the pandemic had total psychological distress scores that were 18.31 points higher on average than those who responded that their anxiety was “About the Same” (p=0.001) and 12.45 points higher on average than those who responded that their anxiety was “Somewhat Higher” due to the pandemic (p=0.05); no other differences were found. Similarly, we found a significant relationship between responses to Q2 of the COVID-19 survey,(self-reported degree of depression exacerbation due to the pandemic) and total psychological distress scores (one-way ANOVA F(4,27)=4.545, p=0.006). Tukey post-hoc analysis revealed that those who indicated “Much Higher” levels of depression due to the pandemic had total psychological distress scores that were 16.35 points higher on average than those who said that their depression was “About the Same” (p=0.02).
3.3. Patient perception of telepsychiatry transition
32 participants completed the telepsychiatry feedback survey. 30 (93.75%) participants agreed or strongly agreed that the availability of remote psychiatry during the COVID-19 pandemic helped them manage their overall mental health. 28 (87.50%) and 27 (84.38%) of participants felt that remote psychiatry helped them manage their levels of anxiety and depression, respectively. Those who reported the availability of telepsychiatry helped them manage their overall mental health during the pandemic were also likely to report that it helped them manage their depression (χ2=54.81, p=0.002, Supplementary Table 1.K), and anxiety levels (χ2=40.96, p=0.005; Supplementary Table 1.L). Similar direct relationships existed for neutral and negative responses to Q1–3 (Supplementary Tables 2.K and 2.L).
Several factors can jeopardize participants’ level of comfort and safety during telepsychiatry sessions, including, but not limited to, a preference for in-person sessions, hesitation regarding use of remote, third-party translators, or concerns over lack of confidentiality, many of which can be avoided with in-person clinical sessions (Shore et al., 2006; Mucic, 2010; Chakrabarti, 2015). Accordingly, we next sought to examine the relationship between participants’ level of comfort, safety, and how much they felt they could express in telepsychiatry sessions compared to on-site visits. We first tested the correspondence between levels of safety and comfort during telepsychiatry sessions; as expected, there was a relationship between levels of safety and comfort (χ2=40.7, p=0.02), with those who felt safer with telepsychiatry visits also feeling more comfortable, and vice-versa (Supplementary Table 1.M). Furthermore, a significant relationship was found between levels of safety and the extent to which participants’ felt they could express themselves compared to on-site visits (χ2=49.9, p=0.001). Inspection of the residuals revealed the expected relationships between participants’ level of safety during telepsychiatry visits and how much they felt they could express in those visits compared to on-site visits. Those who felt safer during telepsychiatry visits also felt that they could express more during those visits than they could during on-site visits, and vice-versa (Supplementary Table 1.N). A Chi-square test of independence found a similar relationship between how comfortable participants felt with telepsychiatry visits and how much they felt they could express during those visits, albeit at trend-level significance (χ2=33.1, p=0.07), with the residuals indicating that those who felt more comfortable with telepsychiatry visits also felt that they could express “Somewhat More” during those visits (Supplementary Table 1.O). Finally, we sought to determine the relationship between participants’ levels of safety, comfort, degree of expression, and perceived benefits of telepsychiatry on their mental health. A Chi-Square test of independence indicated an association between reported feelings of safety during telepsychiatry sessions and how much they felt the sessions helped them manage their overall mental health (χ2=29.32, p=0.02), such that those who felt safer during telepsychiatry sessions were more likely to report that they helped manage their mental health, and vice versa (Supplementary Table 1.P).
3.4. Changes in essential patient needs
34 participants completed our Access to Necessities Survey. All participants reported difficulty accessing at least one of the essential needs since the beginning of the COVID-19 pandemic. The essential need for which the most participants reported difficulty accessing was Rent/Housing (n=31, 91.18%), followed by Income (n=30, 88.24%), Food (n=23, 67.65%), Utilities (n=17, 50.00%), Healthcare Access (n=14, 41.18%), and Medications (n=9, 26.47%). These findings emphasize the severity of social insecurity among undocumented immigrants during states of emergency, particularly without situational government stimulus support.
3.5. Clinical and psychosocial factors associated with psychological distress
A variety of demographic, clinical, and psychosocial factors influence the degree of distress experienced by individuals in the face of adversity. To better understand the potential contribution of these factors to the severity of psychological distress experienced in this outpatient psychiatric sample, we performed a multivariable linear regression analysis with total psychological distress scores as the response variable. We selected age, gender, pre-existing psychiatric diagnoses, COVID-19-related need for assistance with basic life necessities (Access to Necessities Survey), knowing someone with confirmed or suspected COVID-19, perceived access to healthcare, and participants’ comfort with telepsychiatry treatment sessions one month prior (questions 4–6 on our Telepsychiatry Feedback Survey) as potential predictor variables. An Akaike Information Criterion (AIC) stepwise model selection algorithm (Akaike, 1973, 1974) indicated that a combination of 1) a pre-existing depressive disorder, 2) food insecurity, and 3) level of expression during telepsychiatry visits together explained 40.11% of the variance in total psychological distress scores (F(6,19)=3.79, adjusted R2=0.4011, p=0.012). Of note, examination of the regression coefficients revealed that a diagnosis of a depressive disorder (p=0.017) and food insecurity (p=0.020) increased predicted psychological distress, while patient report of expressing “The Same” amount in their telepsychiatry sessions as they do in on-site sessions decreased predicted psychological distress (p=0.023) (Table 4).
Table 4.
Summary Statistics of Multivariable Linear Regression Model. A model consisting of pre-existing diagnosis of a depressive disorder, presence of COVID-19-related food insecurity, and participants’ feedback about the degree to which they could express themselves during telepsychiatry sessions together explained 40.11% of the variance in Kessler Psychological Distress Scale K10+ total scores. As shown in the model coefficients, pre-existing diagnosis of depressive disorder and food insecurity increased predicted distress score, while perception of being able to express “about the same” during telepsychiatry sessions as during on-site sessions decreased the predicted score.
| Model Summary | |||||
| R | R2 | Adjusted R2 | Std. Error of the Estimate | F | Significance |
| 0.7381 | 0.5448 | 0.4011 | 7.501 | 3.79 | 0.01187 |
| Coefficients | |||||
| Step | Beta | Std. Error | t-value | Significance | |
| (Constant) | 20.483 | 5.186 | 3.95 | 0.00086 *** | |
| Depressive Disorder | 8.647 | 3.312 | 2.611 | 0.01717 * | |
| Food Insecurity | 8.71 | 3.433 | 2.537 | 0.02011 * | |
| Expressed the Same | −10.72 | 4.349 | −2.465 | 0.02340 * | |
| Expressed Somewhat Less | −7.746 | 4.753 | −1.63 | 0.1196 | |
| Expressed Somewhat More | −9.984 | 6.604 | −1.512 | 0.14705 | |
| Expressed Substantially Less | 4.871 | 8.811 | 0.553 | 0.58686 |
4. Discussion
The onset of the COVID-19 pandemic was predicted to have a particularly detrimental impact on disadvantaged populations (Druss et al., 2020; Qiu et al., 2020; Ross et al., 2020). Among these populations are low-income immigrants, who are especially vulnerable to public health crises due to factors such as close-quarters living, inadequate financial resources for survival without employment, inaccessibility of public health insurance, and avoidance of healthcare institutions for fear of deportation (Chen et al., 2011; Cook et al., 2017; Page et al., 2020; Ross et al., 2020; Solis et al., 2020). However, no study had empirically assessed if these vulnerabilities materialized in the form of negative mental health outcomes, specifically in undocumented immigrant populations with pre-existing psychiatric disorders. Therefore, our group set out to assess changes in mental health of this sub-population during the COVID-19 pandemic through the use of psychiatric assessment tools, including PHQ-2 and GAD-2, a novel COVID-19 Mental Health Survey, an adapted telepsychiatry feedback survey, and the Kessler Psychological Distress Scale K10+. These surveys were administered for the purpose of this study between March and May 2020 as part of the clinic's shift to a telepsychiatry model.
Our findings reinforce the influence of clinical, psychological, and socioeconomic factors on mental health status during states of emergency. Specifically, we report an overall increase in levels of depression and anxiety directly attributable to the coronavirus pandemicas well as high levels of psychological distress among our population. The latter is noteworthy given a recent report of increased psychological distress among the general U.S. population coinciding with the initial spread of the COVID-19 pandemic (McGinty et al., 2020). We also demonstrated that knowing or suspecting that an acquaintance has coronavirus can directly impact one's mental health. The majority of the studied patient population favored the continued availability of telepsychiatry after the pandemic, and many agreed that telepsychiatry helped them manage their overall mental health and levels of depression and anxiety. However, we found that the positive impact of telepsychiatry was dependent on the comfort, safety, and perceived level of expression during these sessions. Our results suggest that, when considering a population that is highly vulnerable to resource-scarcity and intimate partner violence, telepsychiatry should be considered on a case-by-case basis, as certain participants believed the format negatively impacted their mental health (Prosman et al., 2011; Boserup et al., 2020). The use of telephone sessions as opposed to video consults may have contributed to discomfort, as this communication medium lacks nonverbal communication and thereby may decrease one's sense of interpersonal connection (Luxton et al., 2014).
Our results fall in line with changes that occur in the general population due to traumatic events, such as pandemics (Yu et al., 2005; Taylor et al., 2008; Lau et al., 2010; Goldmann, 2014). However, this study specifically contributes to literature focused on the impact of pandemics on populations with pre-existing psychiatric conditions including major depressive disorder, generalized anxiety disorder, and post-traumatic stress disorder. Through the use of multivariable linear regression, we were able to identify pre-existing depressive disorder and food insecurity as major contributors to psychological distress. Indeed, “dose-dependent” relationships have previously been established between food insecurity and the mental wellbeing of immigrants in high-income countries (Dou et al., 2020). Furthermore, several commentaries have warned about the exacerbation of pre-existing psychiatric conditions by COVID-19, particularly in vulnerable populations with substantial cultural differences (Chatterjee et al., 2020; Druss et al., 2020; Junior et al., 2020; Ross et al., 2020).
Ultimately, historical pandemic literature and new quantitative findings on COVID-19-related effects on mental health emphasize the need for both acute and long-term proliferation of mental health resources, including hot lines and other forms of remote support and free community clinic services. Our group has demonstrated that even the most basic form of telepsychiatry, telephone sessions, can be highly impactful with regards to improving mental health in vulnerable populations.
Study limitations
This study is inherently limited in design due to the urgent need for remote implementation of psychiatric survey tools. Data acquisition from participants was staggered in order to avoid creating additional stress. As a result of this decision, not all participants were accounted for in each survey, limiting cross-analysis between inventories. While our clinic possesses pre-COVID-19 PHQ-9 and GAD-7 historical patient data, this data was collected on-paper during clinic visits. Thus, the historical data was not cross-referenced against PHQ-2 and GAD-2 data gathered by telephone due to potential confounds from the comparison of datasets with variable acquisition methods. This study observed the mental health of a population currently enrolled in outpatient psychiatric care, and therefore these results are not necessarily generalizable to the greater population. While this study involved a small patient sample, similar survey strategies can be used to measure mental health outcomes due to a state of emergency in larger, balanced studies.
Supplementary Material
Table 3.
Telepsychiatry Feedback Survey Responses. 32 participants completed this survey. This survey included script recommendations (see Appendix B).
| Q1. Please tell us your level of agreement with the following statement: “The availability of remote psychiatry has helped me manage my overall mental health.” | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| N (%) | 0 (0.00%) | 1 (3.125%) | 1 (3.125%) | 20 (62.5%) | 10 (31.25%) | |
| Q2. Please tell us your level of agreement with the following statement: “The availability of remote psychiatry has helped me manage my levels of anxiety.” | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| N (%) | 0 (0.00%) | 1 (3.125%) | 3 (9.375%) | 18 (56.25%) | 10 (31.25%) | |
| Q3. Please tell us your level of agreement with the following statement: “The availability of remote psychiatiy has helped me manage my levels of depression.” | Strongly disagree | Disagree | Neutral | Agree | Strongly agree | |
| N (%) | 1 (3.125%) | 1 (3.125%) | 3 (9.375%) | 15 (46.875%) | 12 (37.5%) | |
| Q4. How would you rate your level of comfort during phone therapy appointments compared to in-person therapy appointments? | Very uncomfortable | Somewhat uncomfortable | Did not make a difference | Somewhat more comfortable | Much more comfortable | I am not sure |
| N (%) | 2 (6.25%) | 7 (21.875%) | 15 (46.875%) | 1 (3.125%) | 2 (6.25%) | 5 (15.625%) |
| Q5. How would you rate your level of safety during phone therapy appointments compared to in-person therapy appointments? | Very unsafe | Somewhat unsafe | Did not make a difference | Somewhat safer | Much safer | I am not sure |
| N (%) | 2 (6.25%) | 4 (6.25%) | 14 (43.75%) | 5 (15.625%) | 3 (9.375%) | 4 (12.5%) |
| Q6. How much were you able to express during phone therapy appointments compared to in-person therapy appointments? | I expressed substantially less than I would have wanted to | 1 expressed somewhat less than I would have wanted to | I expressed the amount I usually do | I expressed somewhat more than I usually do | I expressed substantially more than I usually do | I am not sure |
| N (%) | 1 (3.125%) | 7 (21.875%) | 14 (43.75%) | 4(12.5%) | 0 (0.00%) | 6(18.75%) |
| Q7. Would you like remote psychiatiy to remain an option when the EHHOP clinic opens for in-person visits? | Yes | No | I am not sure | No Answer | ||
| N (%) | 26 (81.25%) | 2 (6.25%) | 3 (9.375%) | 1 (3.125%) |
Highlights.
Undocumented immigrant outpatients showed increased depression and anxiety during COVID-19.
The pandemic was directly associated with increased psychological distress levels.
Telephone-based telepsychiatry helped patients manage their mental health during the pandemic.
Depressive disorders and comfort during telepsychiatry strongly influenced distress levels.
Acknowledgments
Our sincerest gratitude to the medical students, residents, and attendings of the EHHOP clinic for their continued patient care during the coronavirus pandemic, enabling this research. Thank you to Marcela Maria Serafini and Pacific Interpreters for survey scripting and therapy/survey administration Spanish translation services, respectively.
Funding
This work was supported by the National Institutes of Health [NIH T32 GM007280 to RAS, JJF, SKP, and CY] and the Ira W. DeCamp Foundation [Community Health Grant to the EHHOP Clinic], the Atran Foundation [Donation to the EHHOP Clinic], and the American Psychiatric Association [Award for Advancing Minority Health to CK].
Footnotes
Conflicts of Interest
The authors have no conflicts to report.
Appendix. Supplementary materials
References
- Akaike H. Maximum likelihood identification of gaussian autoregressive moving average models. Biometrika, 60 (1973), pp. 255–265. [Google Scholar]
- Akaike H. A New Look at the Statistical Model Identification. IEEE Transactions on Automatic Control, 19 (1974), pp. 716–723. [Google Scholar]
- Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Australian and New Zealand Journal of Public Health, 25 (2001), pp. 494–497. [DOI] [PubMed] [Google Scholar]
- Bekteshi V, van Hook M. Contextual Approach to Acculturative Stress Among Latina Immigrants in the U.S. Journal of Immigrant and Minority Health, 17 (2015), pp. 1401–1411. [DOI] [PubMed] [Google Scholar]
- Bell KR, Brockway JA, Fann JR, Cole WR, De Lore JS, Bush N, Lang AJ, Hart T, Warren M, Dikmen S, Temkin N, Jain S, Raman R, Stein MB. Concussion treatment after combat trauma: Development of a telephone based, problem solving intervention for service members. Contemporary Clinical Trials, 40 (2015), pp. 54–62. [DOI] [PubMed] [Google Scholar]
- Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. American Journal of Emergency Medicine, 91 (2020), pp. 3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. The Unemployment Situation - July 2020. U.S. Department of Labor; (2020), Article USDL-20–1503. [Google Scholar]
- Cabral J, Cuevas AG. Health Inequities Among Latinos/Hispanics: Documentation Status as a Determinant of Health. Journal of Racial and Ethnic Health Disparities. Journal of Racial and Ethnic Health Disparities, 7 (2020), pp. 874–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat JM, Dalexis RD, Kokou-Kpolou CK, Mukunzi JN, Rousseau C. Social inequalities and collateral damages of the COVID-19 pandemic: when basic needs challenge mental health care. International Journal of Public Health, 65 (2020), pp. 717–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrabarti S. Usefulness of telepsychiatry: A critical evaluation of videoconferencing-based approaches. World Journal of Psychiatry, 5 (3) (2015), pp. 286–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee SS. Impact of COVID-19 pandemic on pre-existing mental health problems. Asian Journal of Psychiatry, 51 (2020), Article 102071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen J, Vargas-Bustamante A. Estimating the effects of immigration status on mental health care utilizations in the United States. Journal of Immigrant and Minority Health, 13 (2011), pp. 671–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook B Le, Trinh NH, Li Z, Hou SSY, Progovac AM. Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatric Services, 68 (2017), pp. 9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallo FJ, Kindratt TB, Snell T. Serious psychological distress among non-Hispanic whites in the United States: The importance of nativity status and region of birth. Social Psychiatry and Psychiatric Epidemiology, 48 (2013), pp. 1923–1930. [DOI] [PubMed] [Google Scholar]
- Davies NG, Kucharski AJ, Eggo RM, Gimma A, Edmunds WJ, Jombart T, O’Reilly K, Endo A, Hellewell J, Nightingale ES, Quilty BJ, Jarvis CI, Russell TW, Klepac P, Bosse NI, Funk S, Abbott S, Medley GF, Gibbs H, Pearson CAB, Flasche S, Jit M, Clifford S, Prem K, Diamond C, Emery J, Deol AK, Procter SR, Zandvoort K van, Sun YF, Munday JD, Rosello A, Auzenbergs M, Knight G, Houben RMGJ, Liu Y. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. The Lancet Public Health, 5 (7) (2020), pp. E375–E385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donker T, Straten A van, Marks I, Cuijpers P. Quick and easy self-rating of Generalized Anxiety Disorder: Validity of the Dutch web-based GAD-7, GAD-2 and GAD-SI. Psychiatry Research, 188 (2011), pp. 58–64. [DOI] [PubMed] [Google Scholar]
- Dou N, Mitchell D, Na M. Food Insecurity and Mental Health Status Among Immigrants in High-Income Countries Between 2014–2017. Current Developments in Nutrition, 4 (2) (2020), p. 179–179. [Google Scholar]
- Druss BG. Addressing the COVID-19 Pandemic in Populations with Serious Mental Illness. JAMA Psychiatry, 77 (2020), pp. 891–892. [DOI] [PubMed] [Google Scholar]
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of Depression Symptoms in U.S. Adults Before and During the COVID-19 Pandemic. JAMA Network Open, 3 (9) (2020), Article e2019686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezzy D. Unemployment and mental health: A critical review. Social Science and Medicine, 37 (1993), pp. 41–52. [DOI] [PubMed] [Google Scholar]
- Finch WH, Hernández Finch ME. Poverty and Covid-19: Rates of Incidence and Deaths in the United States During the First 10 Weeks of the Pandemic. Frontiers in Sociology, 5 (2020), pp. 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick KM, Harris C, Drawve G. Living in the midst of fear: Depressive symptomatology among US adults during the COVID-19 pandemic. Depression and Anxiety, 37 (10) (2020), pp. 957–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcini LM, Murray KE, Zhou A, Klonoff EA, Myers MG, Elder JP. Mental Health of Undocumented Immigrant Adults in the United States: A Systematic Review of Methodology and Findings. Journal of Immigrant and Refugee Studies, 14 (2016), pp. 1–25. [Google Scholar]
- Goldmann E, Galea S. Mental Health Consequences of Disasters. Annual Review of Public Health, 35 (2014), pp. 169–183. [DOI] [PubMed] [Google Scholar]
- Van Heyningen T, Honikman S, Tomlinson M, Field S, Myer L. Comparison of mental health screening tools for detecting antenatal depression and anxiety disorders in South African women. PLoS ONE, 13 (2018), pp. 1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junior J, Moreira M, Pinheiro W, Silva L da, Neto M. The mental health of those whose rights have been taken away: An essay on the mental health of indigenous peoples in the face of the 2019 Coronavirus (2019-nCoV) outbreak. Psychiatry Research, 289 (2020), Article 113094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerkenaar MME, Maier M, Kutalek R, Lagro-Janssen ALM, Risti R, Pichlhofer O. Depression and anxiety among migrants in Austria: A population based study of prevalence and utilization of health care services. Journal of Affective Disorders, 151 (2013), pp. 220–228. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32 (2002), pp. 959–976. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SLT, Manderscheid RW, Walters EE, Zaslavsky AM. Screening for serious mental illness in the general population. Archives of General Psychiatry, 60 (2003), pp. 184–189. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Green JG, Gruber MJ, Sampson NA, Bromet E, Cuitan M, Furukawa TA, Gureje O, Hinkov H, Hu CY, Lara C, Lee S, Mneimneh Z, Myer L, Oakley-Browne M, Posada-Villa Jo, Sagar R, Viana MC, Zaslavsky AM. Screening for serious illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. International Journal of Methods in Psychiatric Research, 19 (2010), pp. 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The patient health questionnaire-2: Validity of a two-item depression screener. Medical Care, 41 (2003), pp. 1284–1292. [DOI] [PubMed] [Google Scholar]
- Lau JTF, Griffiths S, Choi KC, Tsui HY. Avoidance behaviors and negative psychological responses in the general population in the initial stage of the H1N1 pandemic in Hong Kong. BMC Infectious Diseases, 10 (2010), Article 139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberman KM, Meah YS, Chow A, Tornheim J, Rolon O, Thomas DC. Quality of mental health care at a student-run clinic: Care for the uninsured exceeds that of publicly and privately insured populations. Journal of Community Health, 36 (2011), pp. 733–740. [DOI] [PubMed] [Google Scholar]
- Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). Journal of Psychosomatic Research, 58 (2005), pp. 163–171. [DOI] [PubMed] [Google Scholar]
- Luxton D, Pruitt L, Osenbach J. Best Practices for Remote Psychological Assessment via Telehealth Technologies. Professional Psychology: Research and Practice, 45 (2014), pp. 27–35. [Google Scholar]
- Mann CL, Rifkin RA, Nabel EM, Thomas DC, Meah YS, Katz CL. Exploring Antidepressant Adherence at a Student-Run Free Mental Health Clinic. US Community Mental Health Journal, 55 (2019), pp. 57–62. [DOI] [PubMed] [Google Scholar]
- Maroko AR, Nash D, Pavilonis BT. COVID-19 and Inequity: a Comparative Spatial Analysis of New York City and Chicago Hot Spots. Journal of Urban Health, 97 (2020), pp. 461–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty EE, Presskreischer R, Han H. Psychological Distress and Loneliness Reported by US Adults in 2018 and April 2020. JAMA, 324 (1) (2020), pp. 93–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia L, Janiri D, Pepe M, Dattoli L, Molinaro M, Martin V De, Chieffo D, Janiri L, Fiorillo A, Sani G, Nicola M Di. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain, Behavior, and Immunity, 87 (2020), pp. 75–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mucic D. International telepsychiatry: a study of patient acceptability. Journal of Telemedicine and Telecare, 14 (2008), pp. 241–243. [DOI] [PubMed] [Google Scholar]
- Mucic D. Transcultural telepsychiatry and its impact on patient satisfaction. Journal of Telemedicine and Telecare, 16 (2010), pp. 237–242. [DOI] [PubMed] [Google Scholar]
- Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cadernos de Saude Publica, 36 (4) (2020), Article e00054020. [DOI] [PubMed] [Google Scholar]
- Page K, Venkataramani M, Beyrer C, Polk S. Undocumented U.S. Immigrants and Covid-19. New England Journal of Medicine, 382 (2020), Article e62. [DOI] [PubMed] [Google Scholar]
- Plummer F, Manea, Trepel L, McMillan DD. Screening for anxiety disorders with the GAD-7 and GAD-2: A systematic review and diagnostic metaanalysis. General Hospital Psychiatry, 39 (2016), pp. 24–31. [DOI] [PubMed] [Google Scholar]
- Prosman GJ, Jansen SJC, Fo Wong SH Lo, Lagro-Janssen ALM. Prevalence of intimate partner violence among migrant and native women attending general practice and the association between intimate partner violence and depression. Family Practice, 28 (2011), pp. 267–271. [DOI] [PubMed] [Google Scholar]
- Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. General Psychiatry, 33 (2020), pp. 19–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross J, Diaz C, Starrels J. The Disproportionate Burden of COVID-19 for Immigrants in the Bronx, New York. JAMA Internal Medicine, 180 (8) (2020), pp. 1043–1044. [DOI] [PubMed] [Google Scholar]
- Shore JH, Savin D, Novins D, Manson SM. Cultural aspects of telepsychiatry. Journal of Telemedicine and Telecare, 12 (2006), pp. 116–121. [DOI] [PubMed] [Google Scholar]
- Solis J, Franco-Paredes C, Henao-Martínez AF, Krsak M, Zimmer SM. Structural Vulnerability in the U.S. Revealed in Three Waves of COVID-19. The American journal of tropical medicine and hygiene, 103 (2020), pp. 25–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sønderskov KM, Dinesen PT, Santini ZI, Østergaard SD. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatrica, 32 (2020), pp. 226–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staples LG, Dear BF, Gandy M, Fogliati V, Fogliati R, Karin E, Nielssen O, Titov N. Psychometric properties and clinical utility of brief measures of depression, anxiety, and general distress: The PHQ-2, GAD-2, and K-6. General Hospital Psychiatry, 56 (2019), pp. 13–18. [DOI] [PubMed] [Google Scholar]
- Tang TN, Oatley K, Toner BB. Impact of life events and difficulties on the mental health of Chinese immigrant women. Journal of Immigrant and Minority Health, 9 (2007), pp. 281–290. [DOI] [PubMed] [Google Scholar]
- Taylor MR, Agho KE, Stevens GJ, Raphael B. Factors influencing psychological distress during a disease epidemic: Data from Australia's first outbreak of equine influenza. BMC Public Health, 8 (2008), pp. 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H, Liu Y, Li Y, Wu CH, Chen B, Kraemer MUG, Li B, Cai J, Xu B, Yang Q, Wang B, Yang P, Cui Y, Song Y, Zheng P, Wang Q, Bjornstad ON, Yang R, Grenfell BT, Pybus OG, Dye C. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science, 368 (2020), pp. 638–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran HV, Gore JM, Darling CE, Ash AS, Kiefe CI, Goldberg RJ. Clinically significant ventricular arrhythmias and progression of depression and anxiety following an acute coronary syndrome. Journal of Psychosomatic Research, 117 (2019), pp. 54–62. [DOI] [PubMed] [Google Scholar]
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17 (5) (2020), Article 1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warburton A, Serafini R, Shuham B, Leader A, Barazani S, Moser JA, Meah Y. Leveraging NADAC to Steer Drug Formularies in Resource-Limited Clinics. Journal of Scientific Innovation in Medicine, 2 (1) (2019), Article 5. [Google Scholar]
- Yu HYR, Ho SC, So KFE, Lo YL. Short communication: The psychological burden experienced by Hong Kong midlife women during the SARS epidemic. Stress and Health, 21 (2005), pp. 177–184. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.