To the Editor:
We read the article entitled “Change in Functional Beta Cell Capacity With Time Following Autologous Islet Transplantation” by Ali et al1 published in May/June 2019 with great interest. The authors described a decline in the function of autologous islet grafts in a longitudinal study of 31 patients after total pancreatectomy and islet autotransplantation (TPIAT) based on BETA-2 scores and mixed meal tolerance testing. Interestingly, this is reported as the first use of BETA-2 for the assessment of islet graft function in the setting of autotransplantation.
However, we would like to respectfully point out that we have previously validated and used the BETA-2 score as a reliable tool to monitor islet graft function in the setting of islet autotransplantation in a report published in November 2018.2 Subsequently, we reported a longitudinal study, which demonstrated stable long-term islet graft function after allotransplantation was made possible with engraftment of an optimal islet mass.3 All patients with long-term insulin independence had BETA-2 scores consistently above 17, despite fluctuations in individual scores above this cutoff. This fluctuation of the BETA-2 score, in the setting of stable optimal islet graft function, is related to transient changes in basal insulin requirement and fasting c-peptide serum levels, which, in turn, are due to changes in insulin sensitivity (resistance) resulting from body weight increase, infection, physical activity, or other factors. For example, when a patient is subjected to a transient stress, insulin resistance increases and prompts islets to secrete more insulin to maintain optimal glucose control. This results in a higher fasting c-peptide serum concentration and ultimately translates into a higher BETA-2 score. After the stressor subsides, less insulin is required and a lower serum c-peptide value results in a reduced calculated BETA-2 score. Thus, fluctuation of a BETA-2 score above 17 does not, ipso facto, reflect a decline of islet graft function.
Intrigued by the findings reported by Ali et al,1 we performed additional analysis of BETA-2 scores over time in our cohort of 22 patients after TPIAT performed for chronic pancreatitis with at least 2-year follow-up. We retrospectively divided patients into 3 groups depending on insulin use and functional graft status according to Igls classification, which we adjusted for autotransplantation2: group 1 — 9 insulin independent patients with optimal Igls outcome; group 2 — 4 patients with good Igls outcome and requiring only long acting insulin or only minimal insulin supplementation with meals; and group 4 — 9 patients with good and marginal Igls outcome and requiring full insulin supplementation in multiple daily doses.2,4 Figure 1A presents BETA-2 scores in group 1 over time. BETA-2 scores fluctuated for each individual patient as in allotransplant patients, but in the range above 15, similar to our previous studies in TPIAT patients.2,3
FIGURE 1.
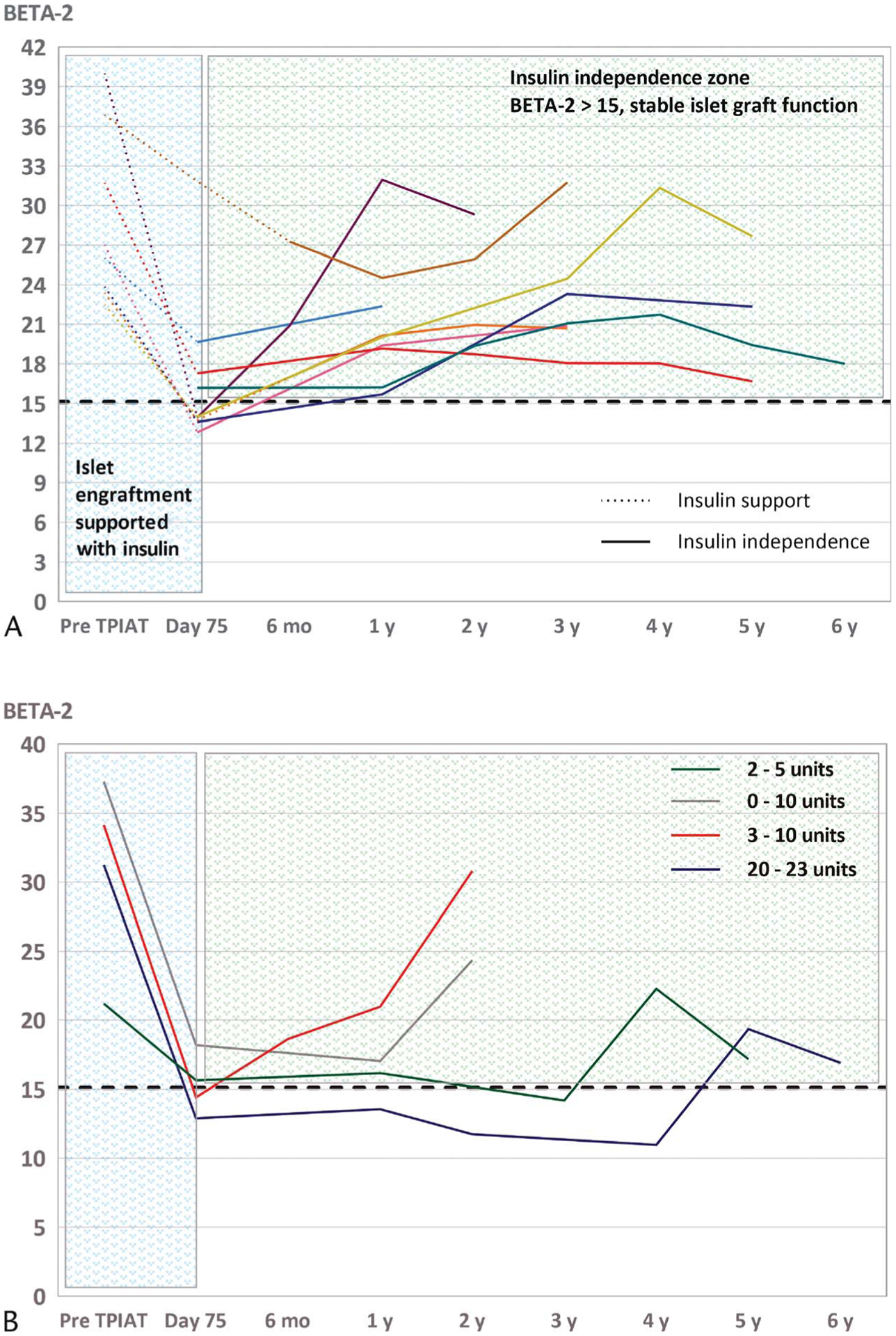
Trends of BETA-2 in patients after TPIAT due to chronic pancreatitis and intractable pain. A, Trends of BETA-2 in group 1 (n = 9) in patients with long-term insulin independence. Patients were supported initially with exogenous insulin (dotted line) to support islet function and optimize conditions for islet engraftment. Afterward, insulin was successfully weaned off maintaining optimal glucose control (continuous line represents insulin independence). In insulin-independent patients, the BETA-2 scores remain above 15 (dashed line) and thus reflect stable islet graft function. Nevertheless, the scores are noted to fluctuate. B, Trends of BETA-2 in group 2 (n = 4) in patients with partial islet graft function and good functional outcomes based on Igls classification.2,4 Patients required minimal insulin support once a day with long-acting insulin or only small doses during their meals. In those patients, BETA-2 scores also remained stable and fluctuated in a range above 10 (dashed line), reflecting stable islet graft function. The legend shows decreasing doses of insulin supplementation for individual patients corresponding to lines with different colors.
In addition, we found stable islet graft function in 4 patients who required only minimal insulin supplementation (group 2) (Fig. 1B). Again, BETA-2 scores also fluctuated over time but remained consistently elevated, reflecting stable islet graft function. The remaining patients requiring full insulin supplementation (group 3) had low BETA-2 scores (i.e., below 10). Nevertheless, these patients never completely lost their serum c-peptide despite follow-up times as long as 6 years. BETA-2 scores in the low range reflect blood glucose control mostly related to insulin dose adjustments rather than to β-cell function itself. Therefore, a BETA-2 score might be not the best estimate of β-cell functional capacity in such cases.
Lastly, an unfortunate discrepancy in the precise BETA-2 formula exists in the literature. The original article in which Forbes et al5 derive the BETA-2 score was first published in the Wiley Online Library with an erroneous version of the formula. We have recently notified the publisher of the discrepancy between the online and print versions. Unfortunately, it appears that Ali et al1 cited the online version of the article and used the erroneous formula. The correct BETA-2 score formula is the following:
Fortunately, despite using the erroneous formula, the general interpretation of the results presented by Ali et al1 remains unchanged. Overall, the individual BETA-2 scores are lowered on average by 1 point and thus do not affect the general direction of the trend or the outcomes.
In summary, our work suggests more stable islet graft function in contrast to the experience reported by Ali et al.1 A possible explanation for the conflicting results is that Ali et al1 analyzed mean BETA-2 scores for all patients combined at each time point (see Fig. 2 in Ali et al1), rather than analyzing trends for each patient separately. Furthermore, it seems that many patients did not have BETA-2 scores at each time point (eg, n = 40 at 6 months vs less than n = 17 at subsequent time points), which makes the analysis less reliable.
Of note, we suspect that a slightly higher BETA-2 cutoff for insulin independence after allotransplantation (BETA-2 >17), when compared with autotransplantation (BETA-2 >15), might be related to higher insulin resistance due to immunosuppression.3 The resulting fasting c-peptide serum levels would be higher and would translate into higher BETA-2 scores in allotransplant patients.
In light of these reservations and based on our own findings, we posit that β-cell function may remain stable after islet autotransplantation and plays a very important long-term role in improved glucose control and patient quality of life.6
Acknowledgments
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK P30 DK02059), the Kovler Family Fund, and Dompé Farmaceutici S.p.A.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Ali KF, San Martin VT, Walsh RM, et al. Change in functional beta cell capacity with time following autologous islet transplantation. Pancreas. 2019;48:656–661. [DOI] [PubMed] [Google Scholar]
- 2.Gołębiewska JE, Bachul PJ, Fillman N, et al. Assessment of simple indices based on a single fasting blood sample as a tool to estimate beta-cell function after total pancreatectomy with islet autotransplantation — a prospective study. Transpl Int. 2019;32:280–290. [DOI] [PubMed] [Google Scholar]
- 3.Bachul PJ, Gołębiewska JE, Basto L, et al. BETA-2 score is an early predictor of graft decline and loss of insulin independence after pancreatic islet allotransplantation. Am J Transplant. 2020;20:844–851. [DOI] [PubMed] [Google Scholar]
- 4.Rickels MR, Stock PG, de Koning EJP, et al. Defining outcomes for β-cell replacement therapy in the treatment of diabetes: a consensus report on the Igls criteria from the IPITA/EPITA opinion leaders workshop. Transpl Int. 2018;31: 343–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forbes S, Oram RA, Smith A, et al. Validation of the BETA-2 score: an improved tool to estimate beta cell function after clinical islet transplantation using a single fasting blood sample. Am J Transplant. 2016;16:2704–2713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sutherland DE, Radosevich DM, Bellin MD, et al. Total pancreatectomy and islet autotransplantation for chronic pancreatitis. J Am Coll Surg. 2012;214:409–424; discussion 424–426. [DOI] [PMC free article] [PubMed] [Google Scholar]


