Small iatrogenic gastrointestinal perforation can be treated successfully using endoscopy.1 However, a large perforation (>3 cm) typically requires surgery.2 With the availability of newer clipping and suturing devices, endoscopic closure of large defects may be considered.3, 4, 5, 6, 7 The technique includes (1) accurate delineation of the perforation site, (2) drainage of fluid collections or infected cavities before closure to prevent wound breakdown, (3) inspection of the surrounding tissue quality to determine the type of endoscopic therapy, (4) assessment of the endoscopic treatment integrity to ensure complete closure, and finally (5) early enteral nutrition initiation for adequate would healing.8 Herein, we describe a case of delayed endoscopic closure of giant gastric perforation by using multiple over-the-scope clips.
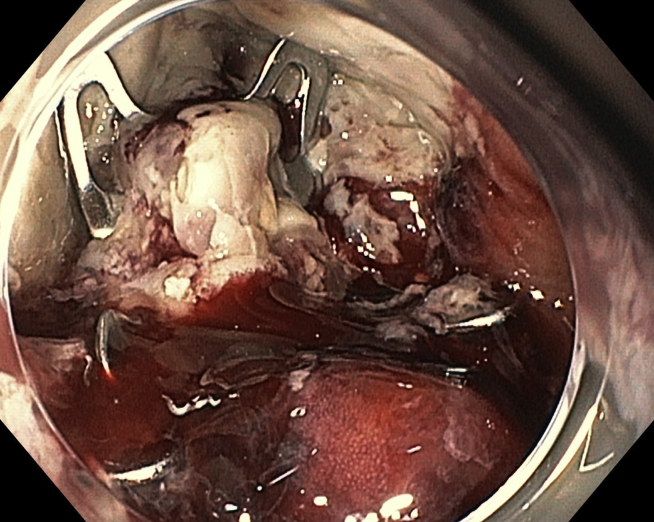
A 72-year-old man underwent an EGD for evaluation of hematemesis. He had Child’s B alcoholic liver cirrhosis and severe pulmonary hypertension. A large bleeding mass was seen in the distal esophagus and cardia (Fig. 1). While we sprayed hemostatic powder on the cardia in a retroflexed position, the patient moved abruptly and developed severe abdominal distention and acute respiratory failure. An abdominal radiograph showed a large pneumoperitoneum (Fig. 2).
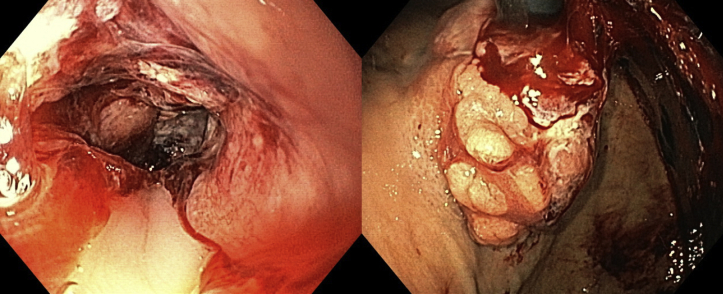
Figure 1.
A large bleeding lesion was seen in the distal esophagus and extending to the cardia.
Figure 2.
Abdominal radiograph showed a large pneumoperitoneum that developed during spraying of hemostasis powder.
The patient declined further evaluation and surgery and was treated conservatively with intravenous antibiotics and nothing by mouth. Over the next 2 days, he remained stable, although the abdominal distention persisted. A CT scan performed on day 3 showed a significant defect in the anterior wall of the stomach separate from the mass and no perigastric fluid collection (Fig. 3). Given that there was no other alternative treatment, an endoscopic closure was performed. Herein, we describe the technique adopted for endoscopic treatment.
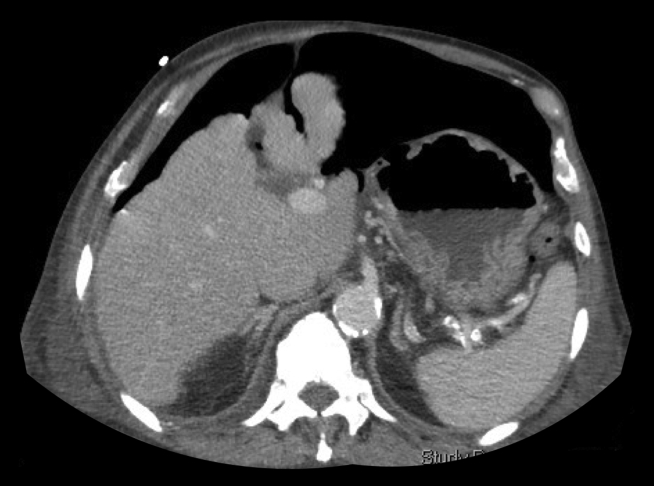
Figure 3.
CT scan of the abdomen showed a large gaping defect in the anterior midgastric wall. The defect did not extend into the bleeding mass.
First, we evacuated the pneumoperitoneum using an angiocatheter (Fig. 4). The angiocatheter was left in situ to prevent further gas accumulation and minimize air embolism risk during the procedure. We used carbon dioxide for insufflation. Second, we assessed the morphology of the perforation and irrigated it thoroughly using saline solution (Fig. 5) to prevent abscess formation. Third, we refreshed the perforation edges using argon plasma coagulation (Forced Coag-60 W). We frequently suctioned the stomach and decompressed the abdomen. Finally, we used the principle of double-layer surgical suture technique. We closed the muscle layer first, followed by approximating the mucosa defect (Fig. 6). Using a twin grasper, we approximated the gaping edges of the muscularis propria and pulled it inside the over-the-scope clip (medium sized atraumatic clip 17.5 mm) before clipping (Fig. 7).
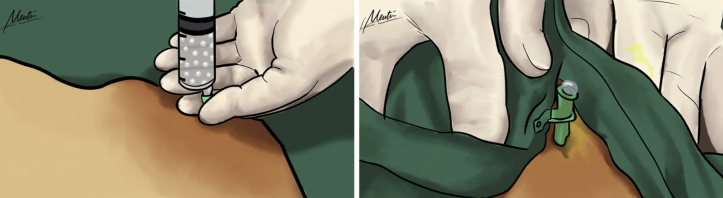
Figure 4.
A saline-solution-filled syringe attached to an angiocatheter was inserted into the sterile abdominal wall to evacuate the pneumoperitoneum before endoscopy.
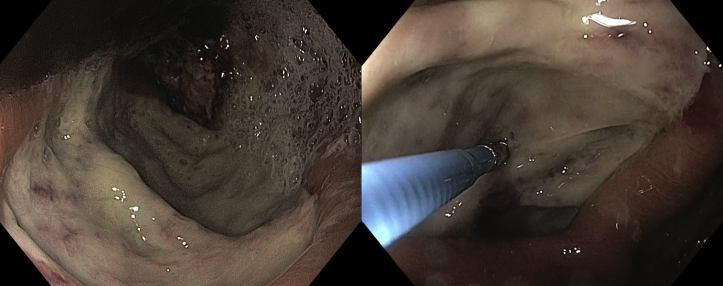
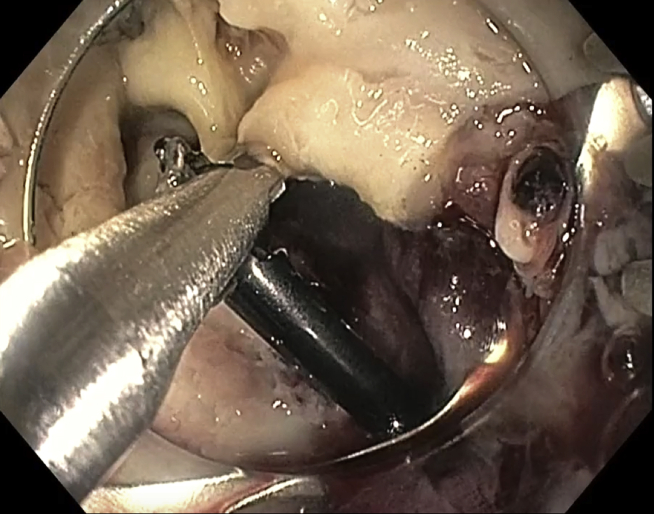
Figure 5.
A large perforation was seen in the anterior wall of the stomach. After cleaning with saline solution, the integrity of the muscularis propria was assessed using a closed biopsy forceps before clipping.
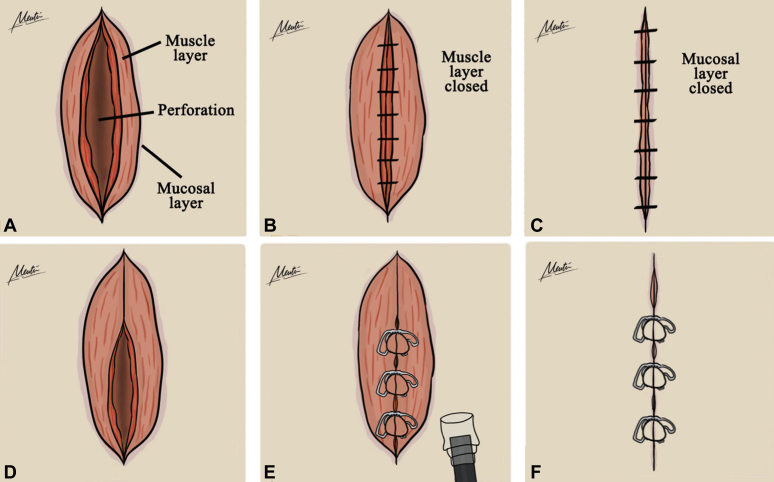
Figure 6.
A, We closed the perforation by adopting the double-layer surgical suture technique. B, In this technique, the inner muscle layer is sutured and closed first. C, The mucosa and submucosa are then approximated. D and E, The same principle was followed with over-the-scope clip application. The muscle layer was closed with over-the-scope clips immediately next to each other. F, The gaping mucosa was then approximated together with additional over-the-scope clips.
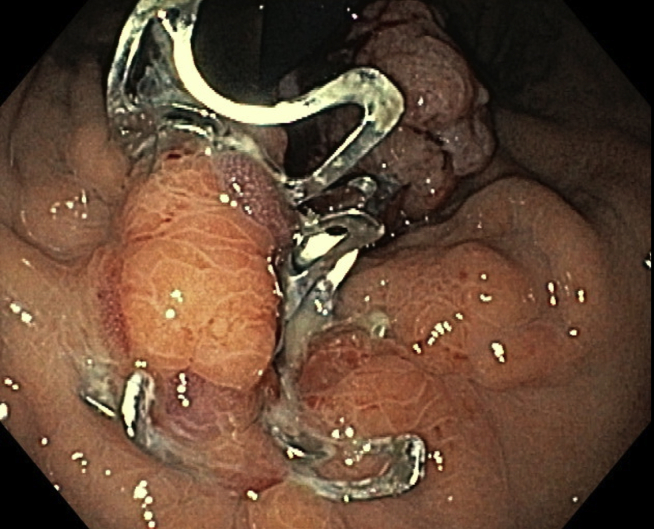
Figure 7.
After freshening the edges with argon plasma coagulation, using a twin grasper, the gaping edges were pulled inside a 17.5-mm atraumatic over-the-scope clip cap before clip deployment.
Using 2 clips, we approximated the muscular defect. We then similarly closed the mucosa using 2 more clips. Each clip was placed immediately next to the previous clip. After closure (Fig. 8), we did not observe any air leak and removed the angiocatheter. Finally, we placed a nasojejunal tube to improve nutrition and promote wound healing. The follow-up radiograph showed resolution of pneumoperitoneum, and water-soluble contrast study showed no leak (Fig. 9). Endoscopy performed at 1 month showed complete epithelization around the clips (Fig. 10). Biopsy specimens obtained from the mass and the follow-up scans showed locally advanced poorly differentiated adenocarcinoma. The patient declined surgery or chemotherapy and was treated conservatively. He died a few months later.
Figure 8.
The perforation was closed after placing 4 over-the-scope clips in a double-layered suture fashion.
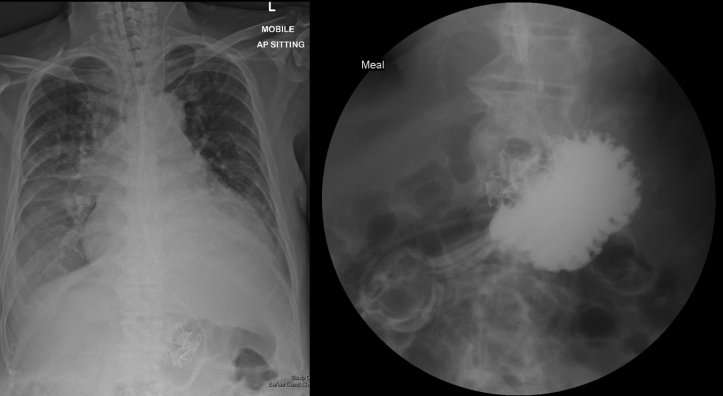
Figure 9.
Follow-up abdominal radiograph showed resolution of the pneumoperitoneum on day 4 after endoscopy, and the water-soluble contrast study showed no leak on day 7.
Figure 10.
Complete epithelialization of the defect with retained over-the-scope clips was seen at endoscopy performed after 1 month.
We have expanded the previous descriptions on the utility of over-the-scope clips to treat gastrointestinal perforation. We have demonstrated the application of multiple over-the-scope clips to close a larger defect (Video 1, available online at www.giejournal.org). Our case was successful for many reasons. The stomach is relatively sterile, and it was likely that the peritoneum was not heavily soiled. This likely prevented wound breakdown and abscess formation. Our immediate nutrition commencement and use of broad-spectrum antibiotics allowed proper wound healing. In this case, we did not use the endoscopic suturing technique because the narrowed distal esophageal lumen would likely have restricted the passage of a suturing device.
Acknowledgment
We thank Ms Meutia Gozali for creating the medical illustrations for this article.
Disclosure
Dr Soetikno is a consultant for Olympus and Fujifilm. All other authors disclosed no financial relationships.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Asokkumar at ravishnkr03@gmail.com.
Supplementary data
Endoscopic closure of iatrogenic large gastric perforation.
References
- 1.Verlaan T., Voermans R.P., van Berge Henegouwen M.I. Endoscopic closure of acute perforations of the GI tract: a systematic review of the literature. Gastrointest Endosc. 2015;82:618–628.e5. doi: 10.1016/j.gie.2015.03.1977. [DOI] [PubMed] [Google Scholar]
- 2.Raju G.S., Saito Y., Matsuda T. Endoscopic management of colonoscopic perforations (with videos) Gastrointest Endosc. 2011;74:1380–1388. doi: 10.1016/j.gie.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Willingham F.F., Buscaglia J.M. Endoscopic management of gastrointestinal leaks and fistulae. Clin Gastroenterol Hepatol. 2015;13:1714–1721. doi: 10.1016/j.cgh.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Ge P.S., Thompson C.C. The use of the overstitch to close perforations and fistulas. Gastrointest Endosc Clin N Am. 2020;30:147–161. doi: 10.1016/j.giec.2019.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kono M., Kanesaka T., Maekawa A. Delayed perforation after gastric endoscopic submucosal dissection can be treated by using over-the-scope clips. Ann Gastroenterol. 2019;32:526. doi: 10.20524/aog.2019.0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piyachaturawat P., Mekaroonkamol P., Rerknimitr R. Use of the over the scope clip to close perforations and fistulas. Gastrointest Endosc Clin N Am. 2020;30:25–39. doi: 10.1016/j.giec.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 7.Angsuwatcharakon P., Prueksapanich P., Kongkam P. Efficacy of the Ovesco clip for closure of endoscope related perforations. Diagn Ther Endosc. 2016;2016:9371878. doi: 10.1155/2016/9371878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baron T.H., Wong Kee, Song L.M. A comprehensive approach to the management of acute endoscopic perforations (with videos) Gastrointest Endosc. 2012;76:838–859. doi: 10.1016/j.gie.2012.04.476. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic closure of iatrogenic large gastric perforation.