Abstract
Posterior reversible encephalopathy cases are increasingly being reported in patients affected by COVID-19, but the largest series so far only includes 4 patients. We present a series of 6 patients diagnosed with PRES during COVID-19 hospitalized in 5 Centers in Lombardia, Italy. 5 out of the 6 patients required intensive care assistence and seizures developed at weaning from assisted ventilation. 3 out of 6 patients underwent cerebrospinal fluid analysis which was normal in all cases, with negative PCR for Sars-CoV-2 genome search. PRES occurrence may be less rare than supposed in COVID-19 patients and a high suspicion index is warranted for prompt diagnosis and treatment.
Keywords: COVID-19, PRES, Seizures
Highlights
-
•
Posterior reversible encephalopathy syndrome is increasingly being reported in COVID-19 patients.
-
•
Weaning from assisted ventilation may be a critical moment in seizure development.
-
•
No evidence of viral genome in the cerebrospinal fluid in this cohort
1. Introduction
Since Hinchey's classical first description of 15 PRES cases [1], numerous other reports have been reported in the literature, but only few papers have been published so far concerning PRES patients in the course of Covid-19 infection, with the largest series including only 4 patients [2] and still few reports [3] concerning neuroradiological peculiarities of brain imaging in this context are published
We report a series of 6 COVID-19 patients developing PRES, from the same geographical region. Moreover, in the present paper we take advantage of the description of these clinical cases to formulate etiopathogenetic considerations and we also propose the use of a prophylactic therapy with an anti-epileptic treatment in what we identified as a delicate transition from forced ventilation to restoration of normal breathing.
All patients reported in this publication were diagnosed by neurological departments located in different hospitals in the Lombardy Region, the most densely populated (approximately 10.000.000 inhabitants) in Italy and one of the most productive and most developed areas of the entire European Union, but also unfortunately the Region in which the covid-19 pandemic was more dramatic with a very significant number of deaths.
The clinical symptomatology of PRES is known, the most significant symptoms in our 6 cases (summarized together with treatment and outcome in Table 1) include alterations in consciousness up to coma, arterial hypertension or significant blood pressure (BP) fluctuations, either focal or generalized epileptic seizures until status epilepticus which continues to represent a potential risk factor for death, visual disturbances ranging from homonymous hemianopsia and to other visual field deficits, up to cortical blindness.
Table 1.
Summary of the main findings in patients 1–6.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| Sex/age | M/54 | F/63 | M/64 | F/64 | M/68 | F/57 |
| Assisted ventilation | Yes | Yes | Yes | Yes | Yes | No |
| ICU | Yes | Yes | Yes | Yes | Yes | No |
| Antibiotics | Ceftriaxone Azithromycin |
Piperacillin Tazobactam |
Ceftriaxone Azithromycin |
Ceftriaxone | No | Levofloxacin |
| Hydroxychloroquine | No | Yes | No | Yes | Yes | Yes |
| Antiretroviral | Lopinavir/ritonavir | Lopinavir/ritonavir | Ritonavir/Darunavir | Darunavir/Cobicistat | Lopinavir/Ritonavir | No |
| Seizures | Yes Partial onset+generalization |
Yes Partial onset+generalization |
Yes Partial onset+generalization |
No | No | Yes Partial onset+generalization |
| Visual field defect | Yes | Yes | Yes | Yes | Yes | Yes |
| Reduced responsiveness | No | Yes | Yes | Yes | Yes | No |
| Headache | No | No | Yes | No | Yes | No |
| Poorly controlled blood pressure | Yes | Yes | No | Yes | Yes | Yes |
| Outcome at dismissal | Right homonymous hemianopsia | Full recovery | Full recovery | Full recovery | Partial recovery | Full recovery |
2. Case 1
A 54-year-old male patient presented in the Emergency Room (ER) for fever and dyspnea started 10 days before. A chest X-ray showed bilateral ground glass opacification (GGO), and the SARS-CoV-2 swab resulted positive. He was first ventilated with CPAP, then transferred to the ICU and treated with invasive ventilation, together with lopinavir/ritonavir, azithromycin and ceftriaxone. The course was complicated by acute renal failure following dialysis treatment, and by episodes of atrial fibrillation treated with pharmacological cardioversion. Following clinical improvement, he was transferred to the medical ward, where he developed a secondarily generalized seizure and subsequent poorly controlled blood pressure values.
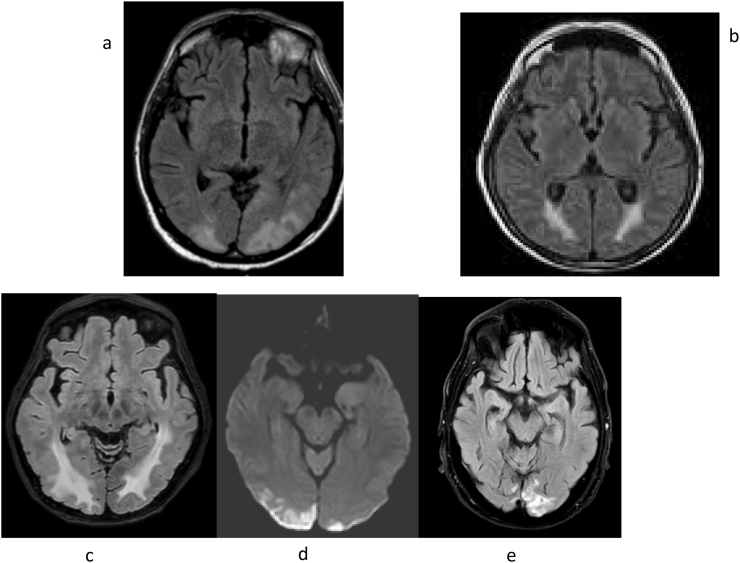
Brain CT scan revealed areas of subcortical hypodensity in both occipital regions, with greater expression on the left. The EEG presented slow dominant theta-delta band activity with bilateral diffusion, however without abnormalities with paroxysmal significance. Brain MRI was consistent with a diagnosis of PRES (Fig. 1a).
Fig. 1.
FLAIR sequences of brain MRI.
At dismissal, the patient was alert, cooperative, with right homonymous hemianopsia and a slight hypotonic tetraparesis compatible with a critical illness polyneuropathy (CIP).
3. Case 2
A 63-year-old female patient presented in ER after a week of fever, cough and myalgias unresponsive to symptomatic therapies. Chest X-ray showed bilateral GGO with consolidation at bases and the pharyngeal swab was positive for SARS-Cov2. Despite treatment with antiviral therapy (lopinavir/ritonavir), hydroxychloroquine, antibiotic therapy (piperacillin/tazobactam) and antithrombotic prophylaxis with low-molecular weight heparin (LMWH), her condition worsened and she was admitted to ICU for invasive ventilation. She also needed hemodynamic support and she underwent immunomodulatory therapy with interleukin-1 antagonist with benefit. She was extubated, but two days later she presented a partial motor seizure with clonic movements of her left side of the face and then in the left hemisome, followed by generalized seizures and epileptic status confirmed by EEG. She was treated with phenytoin, diazepam and levetiracetam, with clinical response and EEG normalization. A first brain CT scan and a subsequent brain MRI (Fig. 1 b) revealed a picture consistent with PRES. Search for SARS-Cov-2 on CSF was negative. The brain MRI performed three weeks later showed a marked improvement, confirming the diagnosis of PRES. The patient is now asymptomatic and had no more epileptic seizures.
4. Case 3
A 64-year-old male was hospitalized after a week of fever unresponsive to antipyretic drugs. The chest X-ray showed GGO. The SARS-CoV-2 swab resulted positive. He was treated with antibiotics and antiretroviral therapy. He first required CPAP treatment, then he needed mechanical ventilation for twenty-three days. After withdrawal of sedation, the patient presented a focal seizure with head and eyes turned to the right, then he became unresponsive and he presented a tetraparesis with normal deep tendon reflexes and absence of other pathological reflexes. EEG confirmed a non-convulsive epileptic status. CSF test for SAR-CoV-2 was negative. Brain MRI showed diffuse white matter hypodense alterations in both hemispheres with symmetrical distribution, mainly affecting the occipital lobes; these lesions did not present contrast-enhancement; few hemosiderin spots suggestive for small hemorrhages were also present. Follow-up MRI was normal, further supporting PRES diagnosis, and clinical recovery was complete.
5. Case 4
A 64-year-old female patient, hospitalized after 10 days of fever and breathing difficulties, was treated at home with antibiotics. At hospital admission she had fever (39 °C) and dyspnea, and neurological examination was normal. Chest x-ray showed GGO in the right basal region, and the nasopharyngeal swab was positive for SARS-CoV-2. Antiviral therapy associated with hydroxychloroquine was started. Due to hypoxia which occurred 24 h later, she was transferred to the ICU, sedated and subjected to mechanical ventilation. After 23 days of ICU admission, the bronchial aspirate for SARS-CoV-2 turned negative. Two days later, after sedation withdrawal she was drowsy with an altered mental status and she complained of blurred vision. Brain CT and MRI (Fig. 1c) were consistent with PRES, with a subsequent haemorrhagic component and improvement at follow-up. The patient became alert again, oriented with normalization of the visual function. This case report was reported in a previous publication [4].
6. Case 5
A 68-year-old male was admitted to the infectious disease department of the Hospital of Gravedona, after eight days of dyspnea and fever, and he had a positive swab for SARS-CoV-2. Oxygen-therapy with CPAP was immediately initiated due to breathing difficulties but worsening of respiratory conditions necessitated a transfer of the patient to ICU and a treatment with invasive ventilation; the patient was treated with hydorxychloroquine and lopinavir/ritonavir. Upon awakening there was a good recovery of alertness and cognitive functions, however the patient complained of visual disturbances in the right visual field and difficulty in walking due to the marked reduction of muscle tone. MRI (Fig. 1d) was consistent with PRES. There was subsequently a progressive improvement of the visual disturbances.
7. Case 6
A 57 years-old female was hospitalized for fever and mild dyspnea and a positive swab test for SARS-CoV-2. Chest x-ray showed no active lesions. In the following days, low-flow oxygen therapy was needed and a treatment with levofloxacin and hydroxychloroquine started. On day-9, the patient suddenly had an aversive seizure with head and eyes turned to the right associated with aphasia. A generalized seizure followed shortly, and it was treated with diazepam iv.
Brain MRI was consistent with PRES (Fig. 1e). In the following days a global aphasia, and frontal neurological symptoms and signs with fatuity and disinhibition appeared; she recovered from aphasia, but she started to complain of visual disturbances in the left hemifield, as well as of rare visual hallucinations. CSF examination showed a slight increase of protein and normal cells, and a negative search for SARS-CoV-2. In the following weeks, she did a full recovery both clinically and in brain imaging.
8. Discussion
Our case series of 6 patients has been collected through reporting by 5 neurology/ICU units in Lombardy with cases occurring during the peak of the epidemic in our region; thus, the number of PRES cases is overall low; the lack of sound epidemiological data on PRES incidence in a pre-COVID era makes it impossible to conclude for an increased risk of developing this syndrome in the context of COVID-19 infection.
CSF data of our three patients who underwent the spinal tap (cases 2, 3 and 6) were substantially normal; of note, PCR search for Sars-Cov-2 genome was negative in all cases; this highlights that PRES in these cases is likely not related to direct viral invasion in the CNS and CSF.
Blood pressure fluctuations are the most relevant factor in PRES pathogenesis; a number of other conditions/treatments have also been reported in association with this syndrome, including hyodroxychloroquine treatment [5]; this drug was administered in 4 of our 6 patients.
In COVID-19 patients, PRES lesions may in some cases present with haemorrhagic features [3,6]; endothelial dysfunction may be relevant in this context [7].
Of note, the distinction between cases of haemorrhagic PRES and recently described patterns of diffuse leukoencephalopathy with microbleeds in COVID-19 patients with persistent confusion and lethargy [8] is not straightforward and might reflect a continuum of alterations involving both the endothelium and the white matter.
It is still not known whether PRES incidence has been substantially increasing in the pandemic; an anecdotal report by Kishfy, Casasola and others at Mount Aubum Hospital in Cambridge, MA, USA [9] described 2 cases in a week as compared with a previous mean of 1.4 cases/yr.
In 4 of our patients, the most critical time for the occurrence of seizures for the patient was represented by the transition from oxygen therapy to the return to a normal breathing. Most of the patients first presented a partial motor seizure, followed by one or more generalized seizures, in cases 2 and 4 then ending up in a status epilepticus. It is possible that the restoration of normal cerebral oxygenation has led to an epileptogenic irritative activity on the cortex not differently from what happens deliberately with hyperpnea during EEG recording. However, case 6 was not subjected to assisted ventilation.
Credit author statement
I declare that all the co-authors have provided relevant contribution for the writing of this article and that thay agree with the submission.
References
- 1.Hinchey J., Chavez C., Appignani B., Breen J. A reversible posterior Leuckoencephalopathy syndrome. N Engl J Med. 1996;334:494–500. doi: 10.1056/NEJM199602223340803. [DOI] [PubMed] [Google Scholar]
- 2.Parauda S.C., Gao V., Gewirtz A.N., Parikh N.S., Merkler A.E., Lantos J., White A., Leifer D., Navi B.B., Segal A.Z. Posterior reversible encephalopathy syndrome in patients with COVID-19. J Neurol Sci. 2020;416:117019. doi: 10.1016/j.jns.2020.117019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conte G., Avignone S., Carbonara M., Meneri M., Ortolano F., Cinnante C., Triulzi F. COVID-19-Associated PRES-like Encephalopathy with Perivascular Gadolinium Enhancement. AJNR Am. J. Neuroradiol. 2020 Aug 13 doi: 10.3174/ajnr.A6762. (Online ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Princiotta Cariddi L., Tabaee Damavandi P., Carimati F., Banfi P., Clemenzi A., Marelli M., Giorgianni A., Vinacci G., Mauri M., Versino M. Reversible encephalopathy syndrome (PRES) in a COVID-19 patient. J Neurol. 2020 Nov;267(11):3157–3160. doi: 10.1007/s00415-020-10001-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gatla N., Annapureddy N., Sequeira M., Jully M. Posterior reversibile encephalopathy syndrome in systemic lupus erythematosus. J Clin Rheumatol. 2013;19(6):334–340. doi: 10.1097/RHU.0b013e3182a21ffd. [DOI] [PubMed] [Google Scholar]
- 6.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19-associated acute Hemorragic necrotizing encephalopathy: CT and MRI features. Radiology. 2020 Aug;296(2):E119–E120. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blecharz-Lang K.G., Wagner J., Fries A., Nieminen-Kelha M., Rosner J., Schneider U.C. Vajkoczy p interleukin 6-mediated endothelial barrier disturbances can be attenuated by blockade of the il6 receptors expressed in brain microvascular endothelial cells. Transl Stroke Res. 2018 Dec;9(6):631–642. doi: 10.1007/s12975-018-0614-2. [DOI] [PubMed] [Google Scholar]
- 8.Radmanesh A., Derman Y., Lui Y., Raz E., Loh J., Hagiwara M., Borja M., Zan E., Fatterpekar G. COVID-19-associated diffuse leukoencephalopathy and microhaemorrhages. Radiology. 2020 Oct;297(1):E223–E227. doi: 10.1148/radiol.2020202040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kishfy L., Casarola M., Banankhan P., Parvez A., Jan Y.J., Shenoy A.M., Thomson C., Abdel Razek A. Posterior Reversible Encephalopathy Syndrome (PRES) as a neurological association in severe Covid-19. J Neurol Sci. 2020;(Jul 15):414. doi: 10.1016/j.jns.2020.116943. [DOI] [PMC free article] [PubMed] [Google Scholar]