Abstract
Chronic intestinal pseudo-obstruction (CIPO) is a severe form of gastrointestinal dysmotility (often due to derangement of the innervation and/or smooth muscle and/or interstitial cells of Cajal) with recurrent episodes of intestinal sub-occlusion. We describe a clinical setting and radiological features of CIPO in an 11-year-old girl with periodic relapses. Our attention was focused firstly on surgical causes, leading to a delay in the diagnosis; thus, is important detecting equivocal symptoms and considering the possible correlation to the CIPO for an early diagnosis and related prevention of acute episodes improving prognosis and quality of life of pediatric patients.
Keywords: Chronic intestinal pseudo-obstruction, Plain abdominal radiographs, Entero-Magnetic Resonance, Entero-Computed Tomography
Introduction
Chronic intestinal pseudo-obstruction (CIPO) is a rare and severe functional digestive syndrome, characterized by a disorder of gut propulsive motility affecting the structure and/or function of components of the intestinal neuromusculature that mimics a mechanical obstruction [1], [2], [3], [4]. It was first described in 1958 by Dudley et al. who reported 13 patients with bowel occlusion's symptoms. Patients underwent exploratory laparotomies, which failed to identify an occlusive lesion [5].
CIPO can affect both adults and children, and should be considered as a separate entity in infants or children. Indeed, the most frequent types in the pediatric population are the congenital and primary forms [6].
Because of its complexity and heterogeneity, CIPO is often misdiagnosed or recognized only in late stages when acute complications may occur.
There are no pathognomonic clinical and radiological findings of CIPO [7].
Case presentation
An 11 years old female child referred to the pediatric emergency room for abdominal pain with alternating constipation and diarrhea.
Her parents reported a 2 years’ history of postprandial abdominal pain, associated with meteorism, nausea, sporadic vomiting and alternating constipation and diarrhea. Her weight was lower than third percentile (26.5 kg), normal height (147 cm) and low body mass index (12.2 kg/m2).
An abdomen X-ray showed a fecal impaction along the length of the colon that was treated with a fecal softener.
In the last 2 months, she complained of abdominal pain, sialorrhea, aerophagia, nausea, meteorism, and nocturnal vomiting. According to these symptoms, she underwent a brain MRI to rule out central causes of vomiting.
According to the clinical picture of an acute abdomen, abdominal radiographs and computed tomography (CT) were performed, showing evident signs of intestinal obstruction. Her symptoms improved without surgery and so she continued follow-up and used antibiotic therapy when needed.
A few months later, a new acute episode of abdominal pain and vomiting occurred; in blood exams protein C reactive, erythrocyte sedimentation rate and procalcitonin were in normal range. Plain radiograph and CT showed (Figs. 1 and 2) a dilated small intestinal bowel, esophageal (33 mm) and bladder distension (Figs. 3 and 4), and she underwent abdominal surgery.
Fig. 1.
Plain radiograph. (A) Dilated small bowel loops on supine radiograph. (B) Multiple air and/or fluid levels on erect radiograph.
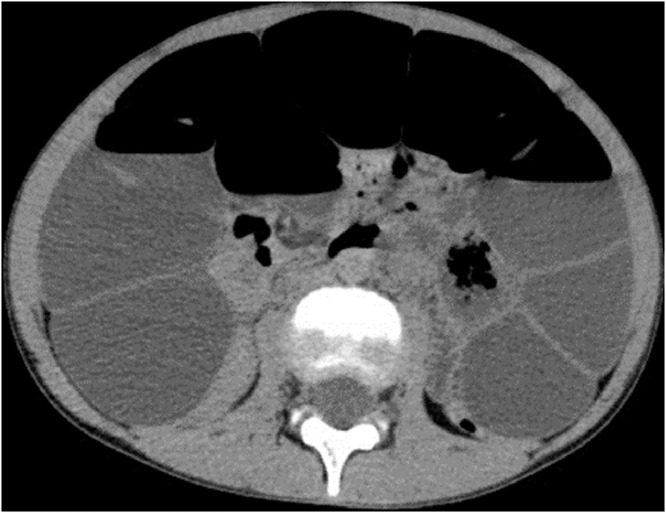
Fig. 2.
Dilated loops of small bowel on abdomen CT.
Fig. 3.

Esophageal ectasia on chest CT.
Fig. 4.

Bladder distension on abdominal CT.
Surgical treatment confirmed a massive distension of small bowel associated with colonic volvulus without ischemic signs (Fig. 5).
Fig. 5.
Massive distension of small bowel without ischemic signs at exploratory laparotomy.
During the exploration, an ileum decompression was performed.
Fluoroscopic study was performed to complete the diagnostic evaluation and evidenced a slow ileal transit time.
Based on the clinical history, radiological signs and acute events, CIPO disease was suspected and she was referred to CIPO Center in Rome.
To improve her quality of life and symptoms, she started parenteral nutrition and a follow-up using a fluoroscopic study with pellets (Fig. 6).
Fig. 6.

Slow ileal transit time at fluoroscopic study associated with gastrectasis and distension of some ileal loops.
Discussion
CIPO is a rare and debilitating disease characterized by a severe disorder of gut motility without an occluding lesion.
Because there is not a diagnostic work-up, pathognomonic clinical or radiological finding of CIPO, it is often misdiagnosed or unrecognized until advanced stages [7].
CIPO diagnosis is based on clinical and radiological valuation.
Half of the patients become symptomatic within the first month of life and 80% within 1 year [8], [9], [10], [11].
The main symptoms are dysphagia, abdominal distension, pain, vomiting, constipation or diarrhea.
It should be suspected in newborns, infants or children with [12]:
-
Prenatal diagnosis of enlarged bladder or megacystis.
-
Persistent and/or recurrent obstructive symptoms, without an occlusive lesion, after exclusion of Hirschsprung disease, hypothyroidism and celiac disease.
-
Persistent vomiting or intestinal obstruction after Ladd procedure to correct malrotation [13].
-
Symptoms of intestinal obstruction combined to ptosis, deafness and abnormal cardiac rhythm or function.
The role of surgery in CIPO has been debated for years.
Decompression of distended GI segments is an important treatment both in adults and children [7].
Radiological findings
Radiographic examinations could be fundamental for screening and prevention of an acute episode of CIPO.
Plain abdominal radiographs should be used as the first screening tools in all patients with suspected CIPO. It usually identifies the traditional findings of bowel obstruction including dilated bowel loops with or without fluid levels [7].
At follow-up, abdominal ultrasound and fluoroscopic studies may be useful in all patients with a suspect of CIPO to exclude malrotation and organic lesions occluding the gut. It uses Water-soluble contrast solutions or pellets to avoid complications related to barium concretions [12].
Entero-Magnetic Resonance Imaging is preferred to entero-CT in the pediatric population, because is an accurate and radiation free-method [12].
Cine-MRI is an emerging particular sequence of MRI which has been proposed for assessing and monitoring gastrointestinal motility in newborns, infants or children [14,15].
During the acute phase, Entero-CT is the first-choice exam. Although Entero-CT should not be a first-choice exam in children due to the massive radiation dose, it is very accurate to detect intra or extra-luminal causes of mechanical occlusion and intestinal adhesions [7,12].
Thapar and colleagues in 2018, highlighted the importance to perform excretory urograms in children affected by CIPO due to the possible involvement of the urinary tract, described between 36% and 71 % of the cases [8].
The most frequent prenatal sign is the megacystis and it is described in about 20% of the cases [9,11].
Conclusions
The most serious cases of the CIPO spectrum are those involving pediatric patients with prenatal evidence of multi-visceral dilatation (eg, digestive and urinary system) often characterized by inability to tolerate enteral feeding with consequent severe prognosis [7]. About it, some reports indicated that 10%-25% of children with CIPO died before adulthood in the past quarter-century [11], [16] and 1 nationwide review in Japan of 2014 reported that about 10% of patients were dependent on total parental nutrition [17]. Thus, early diagnosis of exclusion is crucial.
Several months were needed before of the correct diagnosis during which the girl had CIPO exacerbations and our attention was focused on surgical causes of intestinal obstruction. For this reason, our case report could be useful for detecting equivocal symptoms and considering the possible correlation to the CIPO.
The description of this clinical report could be useful in the daily practice for screening and early diagnosis of the disease, underlining the appropriate radiological methods to do when a child presented occlusion symptoms, also to prevent acute episodes and potential complications.
Authors’ contributions
RT, CV, CQ and IS conceptualized the work and developed a strategy of research. RT and CQ collected the evidence from the literature and screened upon CV, MCL, GND, NT and IS's suggestions. The authors reviewed the manuscript and approved the final version. All the authors contributed in writing.
Patient consent
Patient privacy was maintained. Consent has been obtained for the radiological procedures performed. The images are anonymized from which the individual cannot be identified. These do not contain any identifying marks and are not accompanied by text that might identify the individual concerned.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Acknowledgments: No funding received for this work. we thank to our patient and family.
References
- 1.Stanghellini V, Camilleri M, Malagelada JR. Chronic idiopathic intestinal pseudoobstruction: clinical and intestinal manometric findings. Gut. 1987;28:5–12. doi: 10.1136/gut.28.1.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stanghellini V, Cogliandro RF, De Giorgio R, Barbara G, Morselli-Labate AM, Cogliandro L. Natural history of chronic idiopathic intestinal pseudo-obstruction in adults: a single center study. Clin Gastroent Hepatol. 2005;3:449–458. doi: 10.1016/s1542-3565(04)00675-5. [DOI] [PubMed] [Google Scholar]
- 3.Stanghellini V, Cogliandro RF, De Giorgio R, Barbara G, Salvioli B, Corinaldesi R. Chronic intestinal pseudo-obstruction: manifestations, natural history and management. Neurogastroenterol Motil. 2007;19:440–452. doi: 10.1111/j.1365-2982.2007.00902.x. [DOI] [PubMed] [Google Scholar]
- 4.Amiot A, Cazals-Hatem D, Joly F, Lavergne-Slove A, Peuchmaur M, Bouhnik Y. The role of immunohistochemistry in idiopathic chronic intestinal pseudoobstruction (CIPO): a case-control study. Am J Surg Pathol. 2009;33:749–758. doi: 10.1097/PAS.0b013e31819b381a. [DOI] [PubMed] [Google Scholar]
- 5.Byrne WJ, Cipel L, Euler AR, Halpin TC, Ament ME. Chronic idiopathic intestinal pseudo-obstruction syndrome in children–clinical characteristics and prognosis. J Pediatr. 1977;90:585–589. doi: 10.1016/s0022-3476(77)80371-5. [DOI] [PubMed] [Google Scholar]
- 6.Dudley HA, Sinclair IS, McLaren IF, McNair TJ, Newsam JE. Intestinal pseudo-obstruction. J R Coll Surg Edinb. 1958;3:206–217. [PubMed] [Google Scholar]
- 7.Di Nardo G, Di Lorenzo C, Lauro A, Stanghellini V, Thapar N, Karunaratne TB. Chronic intestinal pseudo-obstruction in children and adults: diagnosis and therapeutic options. Neurogastroenterol Motil. 2016:1–13. doi: 10.1111/nmo.12945. Epub 2016 Sep 29. [DOI] [PubMed] [Google Scholar]
- 8.Mousa H, Hyman PE, Cocjin J, Flores AF, Di Lorenzo C. Long-term outcome of congenitalintestinal pseudoobstruction. Dig Dis Sci. 2002;47:2298–2305. doi: 10.1023/a:1020199614102. [DOI] [PubMed] [Google Scholar]
- 9.Heneyke S, Smith VV, Spitz L, Milla PJ. Chronic intestinal pseudoobstruction: treatment and long term follow up of 44 patients. Arch Dis Child. 1999;81:21–27. doi: 10.1136/adc.81.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vargas JH, Sachs P, Ament ME., Chronic intestinal pseudo-obstruction syndrome in pediatrics Results of a national survey by members of the North American Society of Pediatric Gastroenterology and Nutrition. J Pediatr Gastroenterol Nutr. 1988;7:323–332. [PubMed] [Google Scholar]
- 11.Faure C, Goulet O, Ategbo S, Breton A, Tounian P, Ginies JL. Chronic intestinal pseudoobstruction syndrome: clinical analysis, outcome, and prognosis in 105 children. French-Speaking Group of Pediatric Gastroenterology. Dig Dis Sci. 1999;44:953–959. doi: 10.1023/a:1026656513463. [DOI] [PubMed] [Google Scholar]
- 12.Thapar N, Saliakellis E, Benninga MA, Borrelli O, Curry J, Faure C. Paediatric intestinal pseudo-obstruction: evidence and consensus-based recommendations from an ESPGHAN-Led Expert Group. JPGN. 2018;66:991–1019. doi: 10.1097/MPG.0000000000001982. [DOI] [PubMed] [Google Scholar]
- 13.Devane SP, Coombes R, Smith VV, Bisset WM, Booth IW, Lake BD. Persistent gastrointestinal symptoms after correction of malrotation. Arch Dis Child. 1992;67:218–221. doi: 10.1136/adc.67.2.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ohkubo H, Kessoku T, Fuyuki A, Iida H, Inamori M, Fujii T. Assessment of small bowel motility in patients with chronic intestinal pseudo obstruction using cine-MRI. Am J Gastroenterol. 2013;108:1130–1139. doi: 10.1038/ajg.2013.57. [DOI] [PubMed] [Google Scholar]
- 15.Menys A, Butt S, Emmanuel A, Plumb AA, Fikree A, Knowles C. Comparative quantitative assessment of global small bowel motility using magnetic resonance imaging in chronic intestinal pseudo-obstruction and healthy controls. Neurogastroenterol Motil. 2016;28:376–383. doi: 10.1111/nmo.12735. Epub 2015 Dec 10. [DOI] [PubMed] [Google Scholar]
- 16.Mousa H, Hyman PE, Cocjin J, Flores AF, Di Lorenzo C. Long-term outcome of congenital intestinal pseudo-obstruction. Dig Dis Sci. 2002;47:2298–2305. doi: 10.1023/A:1020199614102. [DOI] [PubMed] [Google Scholar]
- 17.Muto M, Matsufuji H, Tomomasa T, Nakajima A, Kawahara H, Shinobu I. Pediatric chronic intestinal pseudo-obstruction is a rare, serious, and intractable disease: a report of a nationwide survey in Japan. J Pediatr Surg Int. 2014;49:1799–1803. doi: 10.1016/j.jpedsurg.2014.09.025. [DOI] [PubMed] [Google Scholar]