Abstract
Three types of cardiac outpouchings are encountered on cardiovascular imaging: diverticula, aneurysms and pseudoaneurysms. The underlying physiology, imaging findings, risk of rupture, and optimal treatment varies for each and a correct diagnosis is critical. We report a case of a rare, incidentally discovered right ventricular aneurysm that was characterized by transthoracic echocardiogram, computed tomography, and cardiac MRI. The types of cardiac outpouchings are reviewed, and we discuss the selection of imaging modality, keys to distinguishing the outpouchings, and management strategies.
Keywords: Right ventricular aneurysm, Cardiac aneurysm, Incidental findings, Computed tomography, Cardiac MRI, Transthoracic echocardiogram
Introduction
Healthy heart tissue consists of three layers. The thin innermost layer, the endocardium, underlies and nourishes the contractile myocardial layer, which is in turn enclosed by the fibrous pericardium [1]. Congenital defects or injury in one or more layers of the wall can lead to a cardiac outpouching. There are three types of cardiac ventricle outpouchings: diverticula, aneurysms, and pseudoaneurysms. While all types may cause no symptoms, patients can present with palpitations, arrythmias, chest pain, dyspnea, and, rarely, sudden death from rupture [2,3]. The key differences between these types of outpouchings are their contractility and extent of involvement of the cardiac wall. These features also determine the respective imaging appearance and clinical significance.
Cardiac diverticula and aneurysms both contain all three layers of the cardiac wall and may be distinguished by their contractility; the former contract with the rest of the ventricle, while the latter do not [2]. However, for both diverticula and aneurysms, the presence of an intact myocardial layer greatly reduces the risk of free wall rupture. Both are typically congenital, although aneurysms rarely develop after traumatic injury [4]. Ventricular diverticula are usually associated with a congenital anomaly and other extracardiac malformations, and thus are often detected early in life and may require surgical repaired if cardiac function is impaired. Congenital ventricular aneurysms are extremely rare, with approximately 800 reported cases. Most affect the left ventricle with only 20 reported cases of right ventricular aneurysms. About 70% of ventricular aneurysms are associated with congenital anomalies and are usually identified early in life [4]. However, they can also occur in isolation and escape detection until later in life. Diverticula are most common at the ventricular apices, while aneurysms can be found at either the apex or the inferior aspect of the heart [4]. They must be carefully distinguished from pseudoaneurysms, the most serious type of outpouching [5].
Pseudoaneurysms are ruptures of the cardiac wall from trauma or ischemia, typically located in the inferior cardiac wall, and are contained only by pericardium or scar tissue [3]. Pseudoaneurysms lack myocardium and balloon outwards from increased ventricular pressure during systole, making them prone to catastrophic rupture unless they are promptly identified and surgically repaired. Therefore, accurate diagnosis of cardiac outpouchings is critical so that appropriate treatment is pursued. To highlight the importance of correctly identifying cardiac outpouchings and review the pertinent imaging examination and findings, we report a case of an incidentally detected, rare right ventricular aneurysm discovered on abdominal computed tomography (CT).
Case report
55-year-old male with long-standing, stable palpitations, anxiety, and fibromyalgia but no history of cardiac intervention presented with epigastric pain. Contrast-enhanced abdominal CT showed a 2-cm cardiac outpouching communicating with the apex of the right ventricle, isoattenuating with intraventricular blood (Figs. 1A and B). A similar anomaly was retrospectively noted identified on an abdominal CT obtained six years earlier. His ECG was normal, and Holter monitor showed normal sinus rhythm with sinus tachycardia and rare atrial and ventricular ectopy. A transthoracic echocardiogram (TTE) was obtained to better characterize the finding. While suboptimal windows precluded identification on the initial interpretation of the study, retrospective review confirmed a 1.6-cm aneurysm at the right ventricular apex without contractions (Fig. 2). As the outpouching was not seen initially on TTE, cardiac magnetic resonance imaging (MRI) was performed, confirmed the 1.6 × 1.8 cm hypokinetic right ventricular aneurysm (Fig. 3, Supplementary Video 1). Given the stability of the aneurysm, surgical resection was deferred, and the patient elected not to pursue treatment for arrythmia.
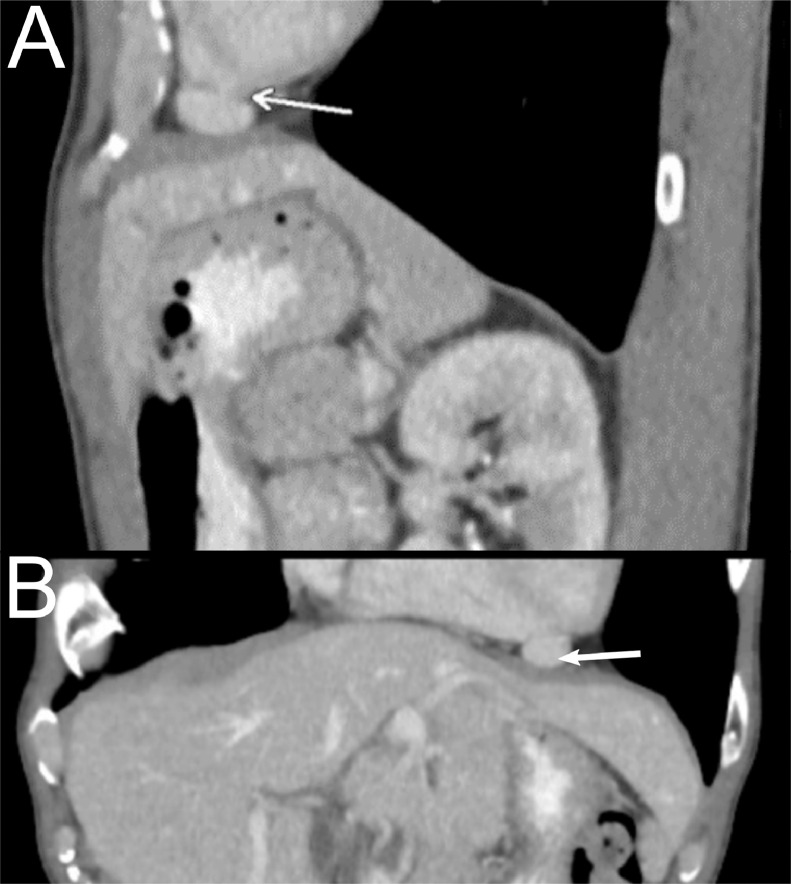
Fig. 1.
Incidental detection of a right ventricular outpouching on abdominal CT. Sagittal (A) and coronal (B) reformatted abdominal CT images show a 2-cm right ventricular outpouching (arrows) isoattenuating with blood within the adjacent right ventricle.
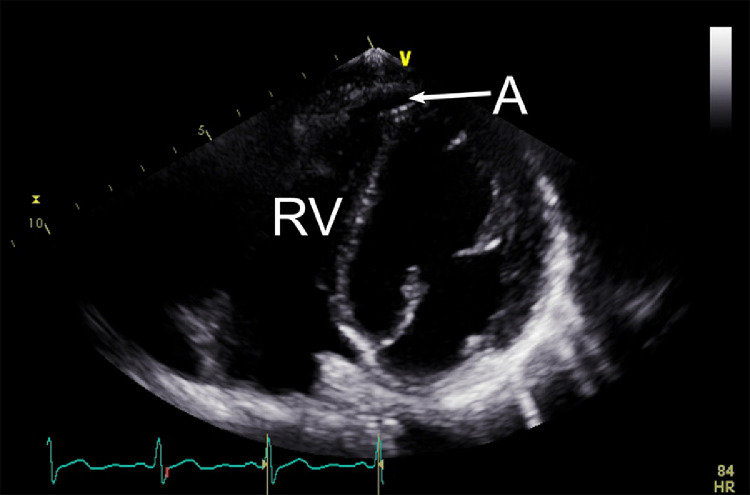
Fig. 2.
Transthoracic echocardiogram of a right ventricular aneurysm. Four chamber view from TTE shows a hypokinetic aneurysm (A) with connection to the right ventricle (RV).
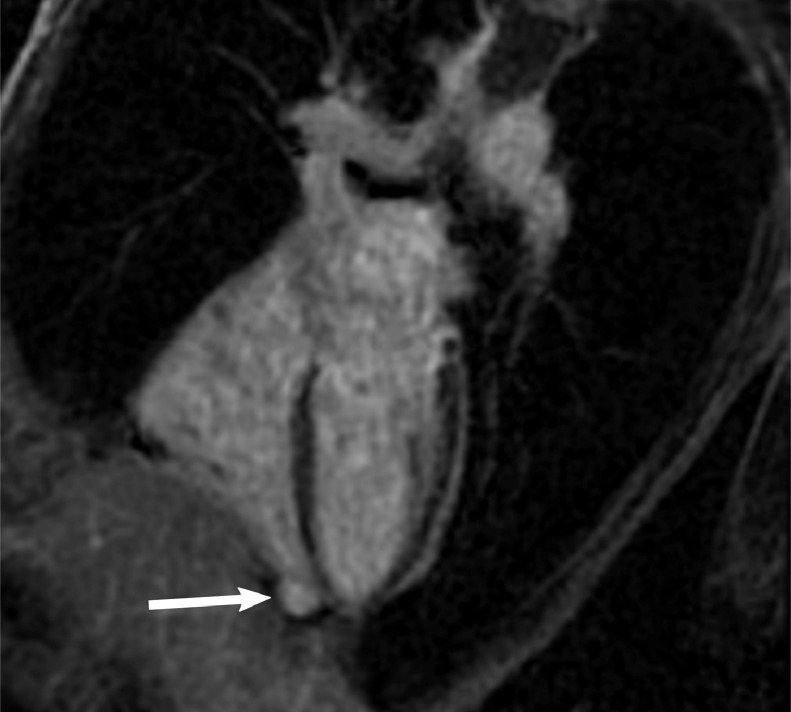
Fig. 3.
Right ventricular aneurysm as seen on cardiac MRI. Horizontal long axis, post-contrast phase sensitive inversion recovery MR image shows small right ventricular apical aneurysm (arrow).
Discussion
Because of the importance of accurate characterization of cardiac outpouchings, selection of imaging modality is crucial. TTE is often obtained first because of relative wide availability and real-time imaging, but accurate diagnosis can be difficult as defect location, body habitus, and variations in examiner skill can all contribute to poor image quality and a missed diagnosis. TTE is less sensitivity than other imaging modalities, as seen in this case, so other methods such as dedicated cardiac CT or MRI should be obtained if a high clinical suspicion remains or a definitive diagnosis cannot be made by TTE alone [6].
Regardless of the imaging modality, several features can help distinguish the different types of ventricular outpouchings. Motion of the outpouching wall during systole is the most helpful. Ventricular diverticula contract with the unaffected cardiac wall, true aneurysms are hypokinetic or akinetic, and pseudoaneurysms paradoxically balloon outwards as ventricular pressure increases during contraction [2]. The size of the neck of the outpouching can also help distinguish pseudoaneurysms from other outpouchings. The initial defect in the cardiac wall leading to pseudoaneurysm formation is almost always small, as larger ruptures are typically lethal. While the outpouching of a pseudoaneurysm expands under pressure from the ventricle, its neck size is fixed by the surrounding intact myocardium. Accordingly, pseudoaneurysm tend to have a narrow neck to maximal aneurysmal diameter ratio [7]. Finally, pseudoaneurysms tend to exhibit delayed pericardial enhancement relative to true aneurysms on gadolinium-enhanced cardiac MRI [8]. Unfortunately, none of these findings is 100% specific, and they must be considered together with the clinical presentation.
Given the rarity of right ventricular aneurysms and diverticula, no specific management guidelines exist, and management is based on information available from the literature on left-sided outpouchings. In adults, arrythmias or chest pain can often be managed medically [2]. Surgical repair can relieve symptoms unresponsive to more conservative therapies or be included in the repair of larger malformations in children. However, with the risk of rupture estimated to be 1.2% per year, the risks of prophylactic surgery should be carefully weighed in otherwise healthy patients [2]. Conversely, the risk of rupture in an untreated pseudoaneurysm is nearly 30% over 4 years, so urgent surgical repair is indicated [9].
In conclusion, ventricular outpouchings are uncommon but important cardiac imaging findings. While distinguishing among the three types can be challenging, proper selection of imaging modality and knowledge of the critical differences can lead to a correct diagnosis and appropriate treatment.
Acknowledgments
A.F.V. was supported by NIH T32 GM008692.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
Patient consent information: https://kb.wisc.edu/hsirbs/18866.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2020.12.066.
Contributor Information
Andrew F. Voter, Email: avoter@wisc.edu.
Jeffrey P. Kanne, Email: jkanne@uwhealth.org.
Anthony D. Kuner, Email: akuner@uwhealth.org.
Lori Mankowski Gettle, Email: lmankowskigettle@uwhealth.org.
Appendix A. Supplementary materials
Supplementary Raw Research Data. This is open data under the CC BY license http://creativecommons.org/licenses/by/4.0/
References
- 1.Jaffar A. Anatomical Structure of the Heart. In: Elmoselhi A, editor. Cardiology: an integrated approach. McGraw-Hill Education; New York, NY: 2017. editor. [Google Scholar]
- 2.Ohlow M-A. Congenital left ventricular aneurysms and diverticula: an entity in search of an identity. J Geriatr Cardiol. 2017;14(12):750–762. doi: 10.11909/j.issn.1671-5411.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frances C, Romero A, Grady D. Left ventricular pseudoaneurysm. J Am Coll Cardiol. 1998;32(3):557–561. doi: 10.1016/s0735-1097(98)00290-3. [DOI] [PubMed] [Google Scholar]
- 4.Ohlow M-A, von Korn H, Lauer B. Characteristics and outcome of congenital left ventricular aneurysm and diverticulum: analysis of 809 cases published since 1816. Int J Cardiol. 2015;185:34–45. doi: 10.1016/j.ijcard.2015.03.050. [DOI] [PubMed] [Google Scholar]
- 5.Yamashiro S, Kuniyoshi Y, Miyagi K, Uezu T, Arakaki K, Koja K. Two cases of ventricular tachycardia with congenital left ventricular malformation in an adult. Ann Thorac Cardiovasc Surg. 2004;10(1):42–46. [PubMed] [Google Scholar]
- 6.Qin JX, Jones M, Shiota T, Greenberg NL, Tsujino H, Firstenberg MS. Validation of real-time three-dimensional echocardiography for quantifying left ventricular volumes in the presence of a left ventricular aneurysm: in vitro and in vivo studies. J Am Coll Cardiol. 2000;36(3):900–907. doi: 10.1016/s0735-1097(00)00793-2. [DOI] [PubMed] [Google Scholar]
- 7.Catherwood E, Mintz GS, Kotler MN, Parry WR, Segal BL. Two-dimensional echocardiographic recognition of left ventricular pseudoaneurysm. Circ. 1980;62(2):294–303. doi: 10.1161/01.cir.62.2.294. [DOI] [PubMed] [Google Scholar]
- 8.Konen E, Merchant N, Gutierrez C, Provost Y, Mickleborough L, Paul NS. True versus false left ventricular aneurysm: differentiation with MR imaging–initial experience. Radiol. 2005;236(1):65–70. doi: 10.1148/radiol.2361031699. [DOI] [PubMed] [Google Scholar]
- 9.Faxon DP, Ryan TJ, Davis KB, McCabe CH, Myers W, Lesperance J. Prognostic significance of angiographically documented left ventricular aneurysm from the Coronary Artery Surgery Study (CASS) Am J Cardiol. 1982;50(1):157–164. doi: 10.1016/0002-9149(82)90023-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Raw Research Data. This is open data under the CC BY license http://creativecommons.org/licenses/by/4.0/