Abstract
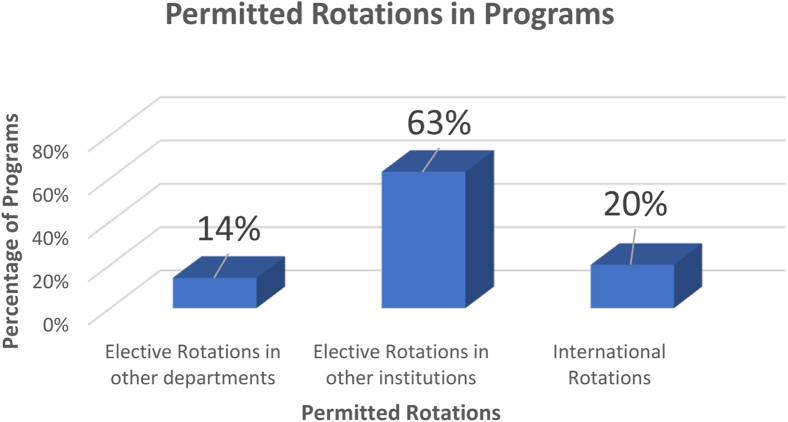
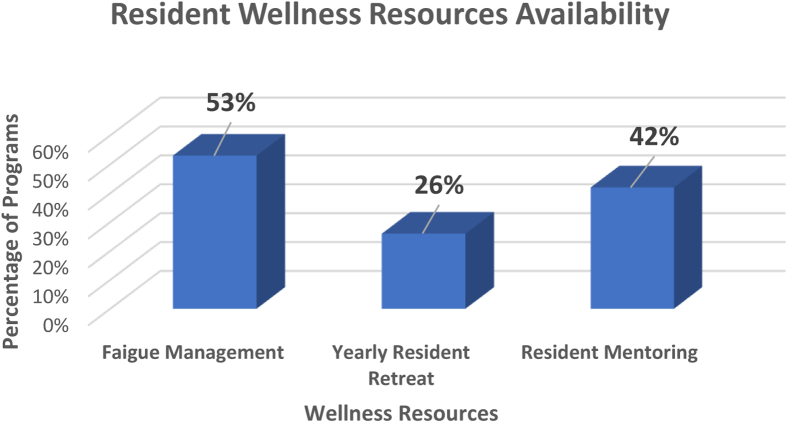
The purpose of this research was to evaluate the variations in research, education, and wellness resources for residents among radiation oncology (RO) residency programs across the United States. A list of accredited programs for the academic year 2018 to 2019 was collected using the Accreditation Council for Graduate Medical Education website. Individual residency program websites were used as the primary source of the data, and the Fellowship Residency Electronic Interactive Data Access System website complemented any missing data. We collected data on dedicated research time, resident rotations, wellness resources, and salary information. Excel 2013 was used for analysis. Information from the 94 Accreditation Council for Graduate Medical Education accredited RO residency programs during the academic year 2018 to 2019 was collected. Seventy-five (80%) programs reported the duration of dedicated research time on their websites. At least 6 months are allowed in 48 (51%) programs, and 27 (29%) programs report that dedicated research time is negotiable. Outstandingly, 20 (21%) programs allow 1 year of dedicated research time, and the median dedicated research time is 9 months. From our study, only 13 (14%) residency programs allow residents to rotate in other departments of the same institution. Fifty-nine (63%) programs allow away rotations at other institutions (external electives). An international rotation is permitted only in 19 (20%) programs. Wellness resoursces specifically fatigue managment, resident retreat and resident mentoring programs were available in 53%, 26% and 42% of programs, respectively. The salary information is obtainable for 63 institutions, and the yearly compensation ranges between $51,000 and $78,000. Moonlighting is allowed only in 28 (30%) programs. Our study found that major variations exist among RO residency programs in the United States regarding research, education, and wellness resources for residents.
Introduction
Residency is the time for education and training, during which a medical student transforms into a capable physician. Having a basic standard for residency programs is very important for the residents to get trained in a more or less similar fashion, which will ensure a similar standard of patient care across the nation once they enter into practice. The Accreditation Council for Graduate Medical Education (ACGME) is responsible for setting the standards for residency programs across the country. ACGME makes sure the necessary criteria are met across the training programs through program reviews, resident surveys, and site visits.
There is a great deal of importance given to the research scholarship activity during residency.1, 2, 3 There has been an increased discussion about fellowship programs in recent years,4 but the data are not available regarding other educational resources like resident elective rotations.
Resident wellness and prevention of burnout has become an essential objective of ACGME in recent years.5 ACGME has been implementing restrictions in duty hours to improve resident wellness,6,7 but variations in resident wellness recourses may exist among radiation oncology (RO) residency programs.
The purpose of this research was to evaluate the variations in research, education, and wellness resources for residents among RO residency programs across the United States.
Methods and Materials
A list of accredited programs for the academic year 2018 to 2019 was collected using the ACGME website (www.acgme.org). Individual residency program websites were used as the primary source of data, and the Fellowship Residency Electronic Interactive Data Access System website (www.freida.ama-assn.org) complemented the missing data. We collected data on dedicated research time, resident rotations, wellness resources, and salary information. Excel 2013 was used for analysis.
Results
Information was obtained from 94 RO residency programs, which were ACGME accredited during the academic year 2018 to 2019.
Research
Of 94 programs, 75 (80%) reported the duration of dedicated research time on their websites. At least 6 months are allowed in 48 (51%) programs, and 27 (29%) programs reported that the dedicated research time is negotiable. Outstandingly, 20 (21.28%) programs allow 1 year of dedicated research time, and the median dedicated research time is 9 months.
Elective rotations
Elective rotations outside the primary department or the primary training institutions help the residents improve their clinical skills and perspectives. From our study, only 13 (14%) residency programs reported allow residents to rotate in other departments of the same institution. Fifty-nine (63%) programs allow away rotations at other institutions (external electives). An international rotation is permitted only in 19 (20%) programs (Fig 1).
Figure 1.
Permitted elective rotations for radiation oncology residents across the residency programs.
Wellness resources
Resident burnout and wellness are 2 areas where ACGME and individual residency programs focus, to improve the residency experience. We evaluated the availability of wellness resources, as presented in the RO program websites, and found that there are many variations across the programs (Fig 2). Fatigue management training is available in 50 (53%) programs. Twenty-four (26%) programs routinely organize resident retreats yearly. Thirty-nine (42%) programs reported that they have resident mentoring programs.
Figure 2.
Availability of resident wellness resources across radiation oncology residency programs in the United States.
Financial wellness is an integral part of resident wellness, and we evaluated the resident salary information across the programs. The salary information was obtainable for 63 institutions, and the yearly compensation ranges between $51,000 to $78,000. Moonlighting is allowed only in 28 (30%) programs.
Discussion
We found a significant variation in the protected research time for residents, with 51% of programs allowing up to 6 months of research and only 21% of programs allowing up to 1 year of research. Studies have found a steady increase in research activity among contemporary RO residents compared with the mid-2000s.2 In a recent survey study among Canadian RO residency programs, 66% of the residents and 20% of program directors reported a lack of protected research time as a barrier for research activity.3 The differences in dedicated research time will have a significant difference in research productivity among the residents of various programs.1,8
There have been some discussions about elective rotations for medical students in RO to prepare them to be the right candidate for matching into RO residency.9 We found a limited number of scholarly activities regarding training elective rotation in related specialties like radiology.10 Our research found that only 14% of programs allow the residents to rotate in other departments of the same institution. Surprisingly, 59 (63%) programs allow away rotations in an RO department at other institutions. There has been an increased interest in global RO recently.11,12 Twenty percent of residency programs allow international rotation, and these rotations may help prepare the resident for a global health career.13
Resident wellness and burnout have come to the spotlight in the last 2 decades,5 and ACGME has been implementing restrictions in duty hours to improve resident wellness.6,7 Despite these interventions, burnout continues to be prevalent among the resident community.14 Recent research among the RO residents in North America has revealed a high prevalence of resident burn out, reporting up to 33% among American residents and 42% among Canadian residents.15,16 In a recent survey study among female RO residents, noticeably, only 5% did not report any symptoms of burnout.17 Despite the significant need for interventions to improve resident wellness, we found that only 53% and 26% of residency programs have fatigue management programs and resident retreats, respectively. Resident burnout is an area that will need urgent intervention among RO trainees.
Our research found that residents' annual salary ranged between $51,000 and $78,000, consistent with a previous report.18 We believe that financial wellness is an integral part of resident wellness, and financial pressure has been found to increase resident burnout and negatively affect professionalism.19 To make matters worse, medical residents and fellows have low financial literacy and high debt.20 There are reported attempts to improve financial literacy by implementing a curriculum in personal finance,21 but these opportunities are not widely available.22 There have been some discussions about the importance of personal finance in the RO community in recent years.23,24
Although mentorship is widely believed to have an essential role in career development, our study found that only 42% of residency programs have a formal mentorship program. Dhami et al25 identified a lack of mentorship as a “critical unmet need” through a survey study among RO residents. Even though 85% of residents reported that mentorship plays a critical role in residency training, only 53% had a current mentor.25 They also reported that programs with a higher number of faculty and residents (>10) are more likely to have a formal mentorship program (88% vs 44%). The residents in a structured mentoring program reported being satisfied with the experience. Barry et al26 and Osborn et al17 had reported that female RO residents prefer to have women ROs as their mentor and noted having difficulty finding a mentor. American College of Radiation Oncology and the American Society for Radiation Oncology have implemented resident mentoring programs to mitigate this gap in mentorship.27,28 However, lack of mentorship continues to be a problem, and action needs to be taken to improve the training experience.
We acknowledge that our study has several limitations. We collected the data primarily from the program websites. Program websites are limited as they are neither comprehensive nor up to date.29 We have also noticed occasional discrepancies within the websites between the departmental page and the residency page during our data collection.
Conclusions
Our study found that major variations exist among RO residency programs in the United States with regards to research, education, and wellness resources for residents. Further interventions are warranted to improve these variations among residency programs.
Acknowledgments
Jenna M. Kahn, MD, Oregon Health & Science University (OHSU), Portland, Oregon and Rahul Tendulkar, MD, Cleveland Clinic Hospital, Cleveland, Ohio.
Footnotes
Sources of support: This work had no specific funding.
Disclosures: none.
References
- 1.Morgan P.B., Sopka D.M., Kathpal M. First author research productivity of united states radiation oncology residents: 2002-2007. Int J Radiat Oncol Biol Phys. 2009;74:1567–1572. doi: 10.1016/j.ijrobp.2008.10.022. [DOI] [PubMed] [Google Scholar]
- 2.Verma V., Burt L., Gimotty P.A. Contemporary trends in radiation oncology resident research. Int J Radiat Oncol Biol Phys. 2016;96:915–918. doi: 10.1016/j.ijrobp.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Dahn H.M., Best L., Bowes D. Attitudes towards research during residency training: A survey of canadian radiation oncology residents and program directors. J Cancer Educ. 2019;34 doi: 10.1007/s13187-019-01565-8. [DOI] [PubMed] [Google Scholar]
- 4.Mohamad O., Meyer J.J. Recent trends in radiation oncology fellowship training in the united states. Int J Radiat Oncol Biol Phys. 2017;99:539–540. doi: 10.1016/j.ijrobp.2017.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Raj K.S. Well-being in residency: A systematic review. J Grad Med Educ. 2016;8:674–684. doi: 10.4300/JGME-D-15-00764.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Philibert I., Friedmann P., Williams W.T. New requirements for resident duty hours. JAMA. 2002;288:1112–1114. doi: 10.1001/jama.288.9.1112. [DOI] [PubMed] [Google Scholar]
- 7.Nasca T.J., Day S.H., Amis E.S. The new recommendations on duty hours from the acgme task force. N Engl J Med. 2010;363:e3. doi: 10.1056/NEJMsb1005800. [DOI] [PubMed] [Google Scholar]
- 8.Gutovich J.M., Den R.B., Werner-Wasik M. Predictors of radiation oncology resident research productivity. J Am Coll Radiol. 2013;10:185–189. doi: 10.1016/j.jacr.2012.06.036. [DOI] [PubMed] [Google Scholar]
- 9.Jang S., Rosenberg S.A., Hullet C. Value of elective radiation oncology rotations: How many is too many? Int J Radiat Oncol Biol Phys. 2018;100:558–559. doi: 10.1016/j.ijrobp.2017.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matalon S.A., Howard S.A., Abrams M.J. Assessment of radiology training during radiation oncology residency. J Cancer Educ. 2018;34 doi: 10.1007/s13187-018-1357-1. [DOI] [PubMed] [Google Scholar]
- 11.Rodin D., Yap M.L., Grover S. Global health in radiation oncology: The emergence of a new career pathway. Semin Radiat Oncol. 2017;27:118–123. doi: 10.1016/j.semradonc.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 12.Thompson R.F., Grover S. A resident's perspective on global health rotations in radiation oncology. Int J Radiat Oncol Biol Phys. 2015;93:1165–1166. doi: 10.1016/j.ijrobp.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 13.Brown D.W., Einck J., Pawlicki T. The case for elective international residency rotations. Int J Radiat Oncol Biol Phys. 2015;93:963–964. doi: 10.1016/j.ijrobp.2015.08.050. [DOI] [PubMed] [Google Scholar]
- 14.Lin M., Battaglioli N., Melamed M. High prevalence of burnout among us emergency medicine residents: Results from the 2017 national emergency medicine wellness survey. Ann Emerg Med. 2019;74 doi: 10.1016/j.annemergmed.2019.01.037. [DOI] [PubMed] [Google Scholar]
- 15.Ramey S.J., Ahmed A.A., Takita C. Burnout evaluation of radiation residents nationwide: Results of a survey of united states residents. Int J Radiat Oncol Biol Phys. 2017;99:530–538. doi: 10.1016/j.ijrobp.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 16.Dahn H., McGibbon A., Bowes D. Burnout and resiliency in canadian oncology residents: A nationwide resident and program director survey. Pract Radiat Oncol. 2019;9:e118–e125. doi: 10.1016/j.prro.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 17.Osborn V.W., Doke K., Griffith K.A. A survey study of female radiation oncology residents’ experiences to inform change. Int J Radiat Oncol Biol Phys. 2019;104 doi: 10.1016/j.ijrobp.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 18.Doke K., Mohamad O., Royce T.J. Fellowship training programs in radiation oncology: A snapshot from 2005 to 2017. Int J Radiat Oncol Biol Phys. 2019;104:765–772. doi: 10.1016/j.ijrobp.2019.03.013. [DOI] [PubMed] [Google Scholar]
- 19.Mareiniss D.P. Decreasing gme training stress to foster residents' professionalism. Acad Med. 2004;79:825–831. doi: 10.1097/00001888-200409000-00003. [DOI] [PubMed] [Google Scholar]
- 20.Ahmad F.A., White A.J., Hiller K.M. An assessment of residents' and fellows' personal finance literacy: An unmet medical education need. Int J Med Educ. 2017;8:192–204. doi: 10.5116/ijme.5918.ad11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bar-Or Y.D., Fessler H.E., Desai D.A. Implementation of a comprehensive curriculum in personal finance for medical fellows. Cureus. 2018;10 doi: 10.7759/cureus.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bar-Or Y. Empowering physicians with financial literacy. J Med Pract Manage. 2015;31:46–49. [PubMed] [Google Scholar]
- 23.Witek M., Siglin J., Malatesta T. Is financial literacy necessary for radiation oncology residents? Int J Radiat Oncol Biol Phys. 2014;90:986–987. doi: 10.1016/j.ijrobp.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 24.Royce T.J., Davenport K.T., Dahle J.M. A burnout reduction and wellness strategy: Personal financial health for the medical trainee and early career radiation oncologist. Pract Radiat Oncol. 2019;9:231–238. doi: 10.1016/j.prro.2019.02.015. [DOI] [PubMed] [Google Scholar]
- 25.Dhami G., Gao W., Gensheimer M.F. Mentorship programs in radiation oncology residency training programs: A critical unmet need. Int J Radiat Oncol Biol Phys. 2016;94:27–30. doi: 10.1016/j.ijrobp.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 26.Barry P.N., Miller K.H., Ziegler C. Factors affecting gender-based experiences for residents in radiation oncology. Int J Radiat Oncol Biol Phys. 2016;95:1009–1016. doi: 10.1016/j.ijrobp.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 27.Engel S., Lischalk J.W., Barry P. Radiation oncology resident mentorship: Results of a resident-coordinated mentorship program. J Am Coll Radiol. 2017;14:1607–1610. doi: 10.1016/j.jacr.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 28.Holliday E.B., Jagsi R., Thomas C.R. Standing on the shoulders of giants: Results from the radiation oncology academic development and mentorship assessment project (roadmap) Int J Radiat Oncol Biol Phys. 2014;88:18–24. doi: 10.1016/j.ijrobp.2013.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prabhu A.V., Karukonda P., Hansberry D.R. A window to internet-based information seeking of us fourth-year medical students: Are radiation oncology residency program websites comprehensive? Int J Radiat Oncol Biol Phys. 2018;101:789–791. doi: 10.1016/j.ijrobp.2018.04.005. [DOI] [PubMed] [Google Scholar]