Abstract
Context
The literature agrees on the impact of post-traumatic stress symptoms in parents of seriously ill children but there is less clarity about the real extent and gender differences of this psychopathological risk. The recent Covid-19 outbreak highlighted new burdens for researchers on Post Traumatic Stress Disorder (PTSD) and clear evidence-based knowledge on this issue is timely needed.
Objective
In this review, we present a synthesis of the updated evidence on PTSD rates in parents of children with severe diseases.
We also aim to try to understand if research in this field has been refined over time with the long-term intent to better face the new challenges of Covid-19 in the paediatric field.
Data sources
The PubMed database was searched.
Study selection
Studies were included if they assessed PTSD in parents of children diagnosed with physical illnesses.
Data extraction
Of 240 studies, 4 were included.
Results
Analysis of the 4 studies revealed 2 studies with PTSD rates around 20% and in line with previous best-evidence. All 4 studies tried to provide more data on fathers, however, all the studies present the lack of a control group.
Limitations
The limited number of studies, which also differ widely in the methodology used.
Conclusions
Methodological errors evidenced in all the 4 studies limit their reliability, making the understanding of the paediatric caregiver’s concern regarding PTSD still difficult. More sound research is needed.
Keywords: PTSD, Severe diseases, Caregivers, Parents, COVID19
Introduction
State of the art
Post-Traumatic Stress Disorder (PTSD) in parents of children with severe physical illnesses represents a public mental health concern that has received increasing attention over the past decade [1–6]. Indeed, PTSD is associated with substantial morbidity, diminished quality of life, high levels of medical utilization, and high economic costs, besides an important burden on the child’s care [7–12].
The most recent edition of the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychological Association, [APA], 2013) [13] first recognized PTSD as a possible mental health sequelae to severe acute and chronic illness experiences both in patients and family members [14].
Since its first appearance in the IIIrd edition of the DSM [15], the PTSD classification, in fact, did not include the illness of a child as a traumatic event for the development of the disorder, but increasing attention has subsequently been paid to the topic in the literature, allowing its inclusion nowadays among traumatic events [13, 16].
In particular, the scientific literature addressed this phenomenon in two meta-analyses, one in 200917 and one published in February 2019 [17]. The 2009 meta-analysis included sixteen studies, showing pooled PTSD prevalence rates of 19.6% in mothers, 11.6% in fathers, and 22.8% in parents. Furthermore, the pooled prevalence ratio for the four studies reporting comparison healthy groups was 4.2. Notably, in families of children with cancer, the proportion of PTSD was about 4 times higher than it was in families with healthy children [18].
These results were what stimulated the great increase of observational studies on this topic and, together with the numerous studies also carried out on other populations of traumatized subjects [19–23], contributed to determining the changes observed in the DSM-5 regarding the traumatic event characteristics. In the DSM-5 criterion A (Trauma), more attention was given to the relevance of indirect exposure to stressor events experienced by a loved one, stating that exposure to an illness that involves the actual or threatened death of a child could be a traumatic event that can lead to PTSD [13].
The DSM-5 specifies the need for the event to be violent or accidental (sudden medical catastrophe), focalizing more on the urgency and abruptness of the perceived threat rather than on its severity. This concept modifies and narrows the possibilities with respect to the previous DSM-IV-TR [16] that only required learning that one’s child had a life-threatening disease. In line with the previous DSM-IV indications, studies on this issue were mainly on cancer diseases and, to a lesser extent, on traumatic accidents. It has only been in the last few years that other diseases have emerged [24–29].
In order to advance the scientific literature on parental PTSD of the last few years, the 2019 meta-analysis could rely on around ten papers providing epidemiologically more sound results [17].
The authors first screened and highlighted 290 studies on this topic in which the most represented disease was still cancer with 159 papers, then 36 studies were on burns, 17 on diabetes, 12 heart disease, 5 epilepsy, 4 asthma, cleft lip and/or palate and phenylketonuria, 2 on HIV infection, sickle-cell disease, spina bifida, and food allergy; finally, 41 studies focussed on other infectious diseases, but at least a quarter of them were of poor quality.
Surprisingly, the results evidenced parents’ PTSD rates of 18.9%, which is perfectly in line with the results of Cabizuca et al.. Nevertheless, 14,891 subjects out of the total sample of 30,068 in Pinquart’s study was represented by parents of children with cancer, generalizing this epidemiological data at risk of bias, and contributing to the difficulty in addressing real epidemiological PTSD rates of parents of sick children in general [17].
However, it can be assumed that the prevalence rates of PTSD reported in this sub-population of traumatized individuals are higher than those reported by epidemiological studies in the general population, with prevalence rates as high as 6.8% in the United States [30] and similar rates reported in European cohorts [31, 32].
Notably, percentages of traumatic stress symptoms, while not meeting the diagnostic criteria for PTSD, were particularly evidenced in parents of children with epilepsy, diabetes, sickle cell disease, heart disease, and cancer. Contrary to expectations, parents of children with a fatal disease, such as incurable cancer or HIV infection/AIDS, did not report the highest levels of post-traumatic stress symptoms, indicating that the objective features of the traumatic event may be less important for the development of traumatic stress symptoms than the individual’s subjective experience of the event. Pinquart’s results also confirmed that the common literature recognized pre-traumatic risk factors for PTSD such as female gender and low social resources, as well the general decline of the disease over time [17].
Considering that the recent outbreak of the COVID-19 pandemic will dramatically lead to a surge of post-traumatic stress symptoms in different groups of people in the future and some evidence for this has already emerged [33], it is important to ensure the most up-to-date evidence on PTSD in all fields of research. In addition to this, even if symptoms of COVID-19 disease are usually mild in children, the high risk of infectiousness for other family members may worsen the emotional impact and the traumatic burden for parents who have to deal with with the COVID-19 infection of their children [34].
Objectives
The present update will summarize last year’s literature published since the 2019 meta-analysis [17] on PTSD and post-traumatic stress symptoms related to having a child with severe illness. A particular focus on possible gender differences between mothers and fathers will be also addressed.
Considering the fact that over a 10-year period, the articles published on this subject showed a tenfold increase, we assumed that a significant number of articles may have been published in the last year.
The main aim in exploring these further studies is to aspire to compiling real epidemiological data on parent’s PTSD with regard to ill children. A further aim is to observe if they address the literature gaps highlighted in previous findings: the majority of the studies were on cancer, included predominantly maternal samples and a very small number had a control group.
With this aim in mind, we have selected 4 main areas of interests, in particular: parents’ PTSD rates, disease type, number of fathers compared to mothers and control groups.
Our goal is to try to understand if research in this field has been refined over time with the long-term intent to help parents better deal with the psychological challenges of having a child infected with SARS-CoV-2 (COVID-19).
Method
Search strategy
Since Pinquart’s meta-analysis included studies until April 2018, we conducted a Medline/PubMed search of published studies between May 2018 and April 2020.
Our digital search strategy involved the co-presence in the title of the keyword “PTSD” with at least one of the following three-word combinations: “parents” and/or “mothers” and/or “fathers”, excluding all studies dealing with other psychological aspects or concerning other mental disorders such as depression, anxiety, etc.
Other web-based databases, as well as unpublished studies, were excluded from the search. Reference sections of the identified papers were eventually checked for additional studies.
Study selection
We included only English language papers that met the following main inclusion criteria: the study assessed PTSD in parents of children diagnosed with physical illnesses.
Eligibility was determined using an approach based on The Grading of Recommendations, Assessment, Development and Evaluation (GRADE) to assess the quality and strength of the evidence.
The selected studies were addressed using a specific “Data Collection Form (DCF)” comprising: N° of parents of children with chronic physical illness; N° of mothers: N° of fathers; type of illness; type of study; time since diagnosis; parental age; parental couple paired for one child (same index traumatic event); child’s age at the time of diagnosis; time since diagnosis; PTSD rates divided by gender.
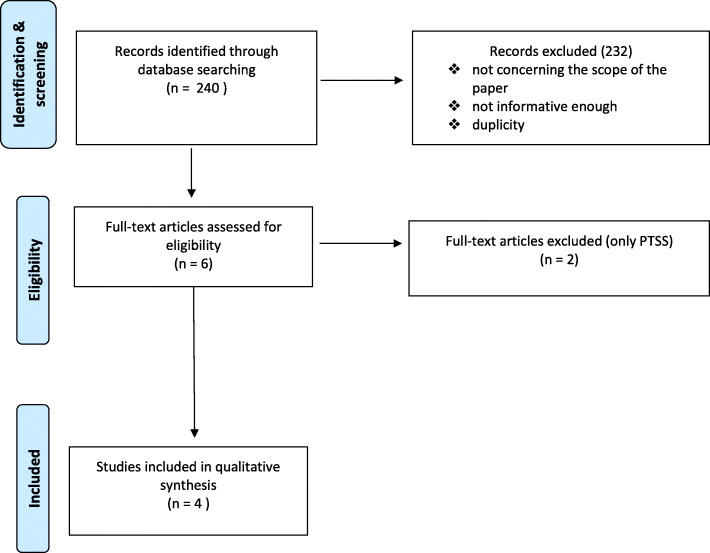
The DCF was filled in separately by two different authors (CB and VP) and checked by a third author (MC). The decisions for inclusion or exclusion are summarized in a flow chart according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) recommendations (Fig. 1). Due to the high degree of heterogeneity between studies, we were unable to undertake a formal meta-analysis.
Fig. 1.
PRISMA Flow chart of study selection process
Results
Study selection
The Medline/Pubmed search retrieved 240 results. We then excluded titles with the following features: a) not concerning the scope of the paper; b) not informative enough; c) duplicity.
Seven studies were thus selected as potentially relevant after screening of titles and abstracts. Among them, we identified 5 cross-section observational studies and 1 review. The latter was eventually discarded because it included studies described in Pinquart’s meta-analysis and the other 2 studies were ruled out because they explored Post-Traumatic Stress Symptoms (PTSS) and not PTSD diagnosis. In the end, four studies were included in this review. The corresponding authors were contacted to supply the information missing from the articles.
Characteristics of the included studies
The characteristics of the included studies are summarized in Table 1.
Table 1.
Key characteristics of the included studies
| Study | Month, year | Type of study | Child disease | Time since diagnosis/event (years) | Total sample (N) | Mothers | Fathers | Parent couple | ^Child Age (years) |
PTSD (%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| °Mean [SD] or median [IQR] | N | °(age) Mean [SD] or median [R] | *Psych fam. (%) | N | °(age) Mean [SD] or median [R]° | *Psych fam (%) | °Mean [SD] or median [R]° | |||||||
| Carmassi et al., | Feb, 2019 | Cross sectional | Epilepsy | > 1 month | 199 | 134 | 42.3 [27–60] | 17.2% | 65 | 45.9 [29–60] | 18.5% | 44 | 0–18 |
♀ 19.5% ♂ 8.1% |
| Werner et 'al., | May, 2019 | Cross sectional | Cardiac device | 6.3 [0.4–17.9] | 126 | 69 | 42 [28.0–60.0] | – | 57 | 44 [28.0–68.0] | – | – | 4.9 [4.4] |
♀ 1% ♂ 0% |
| Lehman et al., | Jan, 2020 |
Longitudinal T0 / T1 (6 months) |
Stroke |
♀ 0.70 [0.33–1.25] ♂ 0.58 [0.34–1.25] |
81 | 54 | 36.2 [23.8–56.0] | – | 27 | 38.4 [34.7–41.3] | – | 23 | 1.58 [0.92–10.92] |
♀ 28% ♂ 15% |
| Schecter et al., | Feb, 2020 | Cross sectional | NICU infants | 1 | 91 | – | – | – | – | – | – | – |
< 1 > 1 |
♀ 17% ♂ 9% |
° SD:Standard deviation/ R:Range/ IQR:Interquartile Range
^Child age at the time of diagnosis/*Parents’ psychiatric family history
A total of 4 studies provided data on 409 parents of children with physical illnesses. Among them, 3 papers reported ages and divided the samples by gender, with a total of 257 mothers (mean age 40.9 years) and 149 fathers (mean age 43.73 years). The physical problems of the children involved were different: 2 papers reported on neurological events, namely epilepsy and stroke, 1 on heart diseases needing implantation of a cardiac rhythm device, and 1 on infants experiencing the intensive care unit.
Two studies specifically involved younger children, with a mean age of 1.58 years [35] and around one year old [36]. The other two studies involved parents whose children presented the event at a mean age of 4.9 years [37] and children followed by paediatricians at any age (0–18 years) [38].
Two studies collected data from 6 months to one year after the diagnosis/event of the child’s disease [35, 36]; whereas one paper reported results collected at a mean time of 6.3 years after the event (Werner) [37], and another one showed data gathered generally a month after the diagnosis of the child’s disease, as required for DSM-5 PTSD diagnosis [38].
Only one study reported psychiatric familiar history in 15.6% of subjects (17.2% among mothers and 18.5% among fathers) [38].
Noteworthy, two studies showed quite homogeneous results, with rates of PTSD ranging from 17 to 19.5% among mothers and from 8.1 to 9% among fathers [36, 38], whereas the parents of patients who experienced a stroke showed a higher prevalence of PTSD (28% of mothers and 15% of fathers) [35]. Surprisingly, Werner et al. [37] reported much lower rates, since only one mother and no fathers had a diagnosis of a PTSD related to the implantation of a cardiac rhythm device in their children.
Discussion
The present review summarizes and discusses the latest evidence regarding PTSD in parents of ill children in order to have updated data in real-time in a period in which scientific research in the field of PTSD needs to be implemented and epidemiological data are necessary.
The Covid-19 outbreak is indeed a public health emergency of international concern and poses a challenge to psychological resilience [33, 39–42]. Research data are needed to develop evidence-driven strategies to reduce adverse psychological impacts and psychiatric symptoms during the epidemic.
Two studies out of four present matching PTSD rates and in line with Pinquart’s meta-analysis [36, 38]. These results corroborate the epidemiological power of the prevalence rates elaborated by Pinquart. There is insufficient data to understand why the other two studies differ so much. One hypothesis would depend on the time between the traumatic clinical event and the parents’ PTSD assessment. Indeed, the study with the higher prevalence rates [35] has the shortest range of time since diagnosis (less than 1 year) and the study with very low rates [37] has a rather long time (almost 7 years) since diagnosis. It is possible that a period of 6.3 years offered sufficient time to recover and to develop resilience [7, 43, 44].
Nevertheless, rates of around 20% turn on a psycho-social alarm on pediatric caregivers and suggest the need for increasing multidisciplinary approaches to pediatric diseases. Social and clinical interventions should be planned by clinician teams together with psychologists and psychiatrists with sufficient expertise on various diseases to enable them to respond effectively to the peculiar needs and situations of pediatric caregivers.
Which was the impact of previous best evidence in guiding the research in this field in the last year?
Answering this issue is fundamental to highlight useful directions to target scientific research on pediatric caregivers PTSD from this point on.
To the best of our knowledge, this is the first review on this subject that tries to analyse the impact of previous best evidence in refining subsequent research.
Methodological errors evidenced in all four studies limit their reliability, making the understanding of the pediatric caregiver’s concern regarding PTSD still difficult.
In this regard, none of the available papers included a control group which is necessary to increase the robustness of these types of studies. This observation makes us question researchers’ ability or possibility to apply evidence in practice [45]. Two different speculative reasons could be difficulty activating broad protocols that require two different study samples or a general difficulty detecting all the information on best evidence that the literature can provide.
On the other hand, all four studies were not on cancer diseases so we can, therefore, affirm that, in this case, the main meta-analysis take-home message has been received, which is that many other diseases can have a damaging effect on parents, leading them to develop real symptomatic pictures of post-traumatic stress disorder. Furthermore, the total number of fathers involved in the studies has significantly increased. This is very important in the perspective of gender medicine both in preventive and clinical terms since mothers and fathers present many differences in the response to stress.
The main limitation of this work is the analysis of a limited number of studies, which also differ widely in the methodology.
Conclusions
More sound research is needed to deal with the psychopathological issue of PTSD in pediatric caregivers in a preventive and gender-targeted perspective.
Acknowledgements
The authors would like to thank Wendy Doherty, lecturer of University of Pisa, for the English language revision.
Abbreviations
- PTSD
(Post-Traumatic Stress Disorder)
- DSM
(Diagnostical and Statistical Manual of Mental Disorders).
- APA
(American Psychiatric Association).
- COVID-19
(Coronavirus disease 2019).
- GRADE
(Grading of Recommendations, Assessment, Development and Evaluation).
- DCF
(Data Collection Form).
- PRISMA
(Preferred Reporting Items for Systematic reviews and Meta-Analyses).
- PTSS
(Post-Traumatic Stress Symptoms).
Authors’ contributions
All authors contributed in researching and reading all the literature used to write this review. The author(s) read and approved the final manuscript.
Authors’ information
P. Striano has served on a scientific advisory board for the Italian Agency of the Drug (AIFA); has received honoraria from GW pharma, Kolfarma s.r.l., and Eisai Inc.; and has received research support from the Italian Ministry of Health and Fondazione San Paolo. All the other authors do not report conflict of interest. This work was developed within the framework of the DINOGMI Department of Excellence of MIUR 2018–2022 (legge 232 del 2016). The other authors have indicated they have no financial relationships relevant to this article to disclose.
Funding
No external funding for this manuscript.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Davydow DS, Richardson LP, Zatzick DF, et al. Psychiatric morbidity in pediatric critical illness survivors: a comprehensive review of the literature. Arch Pediatr Adolesc Med. 2010;164(4):377–385. doi: 10.1001/archpediatrics.2010.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stuber ML, Meeske KA, Krull KR, et al. Prevalence and predictors of posttraumatic stress disorder in adult survivors of childhood cancer. Pediatrics. 2010;125(5):e1124–e1134. doi: 10.1542/peds.2009-2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gunjur A. PTSD in parents after childhood cancer. Lancet Oncol. 2015;16(7):e320. doi: 10.1016/S1470-2045(15)00043-1. [DOI] [PubMed] [Google Scholar]
- 4.Muscara F, McCarthy MC, Woolf C, et al. Early psychological reactions in parents of children with a life threatening illness within a pediatric hospital setting. Eur Psychiatry. 2015;30(5):555561. doi: 10.1016/j.eurpsy.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Carmassi C, Corsi M, Gesi C, et al. DSM-5 criteria for PTSD in parents of pediatric patients with epilepsy: What are the changes with respect to DSM-IV-TR? Epilepsy Behav. 2017; 70(Pt A):97–103. doi: 10.1016/j.yebeh.2017.02.025. [DOI] [PubMed]
- 6.Carmassi C, Corsi M, Bertelloni CA, et al. Mothers and fathers of children with epilepsy: gender differences in post-traumatic stress symptoms and correlations with mood spectrum symptoms. Neuropsychiatr Dis Treat. 2018;14:1371–1379. doi: 10.2147/NDT.S158249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61(Suppl5):4–12;discussion 13–4. [PubMed]
- 9.Brunello N, Davidson JR, Deahl M, et al. Posttraumatic stress disorder: diagnosis and epidemiology, comorbidity and social consequences, biology and treatment. Neuropsychobiology. 2001;43(3):150–162. doi: 10.1159/000054884. [DOI] [PubMed] [Google Scholar]
- 10.Dell’Osso L, Stratta P, Conversano C, et al. Lifetime mania is related to post-traumatic stress symptoms in high school students exposed to the 2009 L'Aquila earthquake. Compr Psychiatry. 2014;55(2):357–362. doi: 10.1016/j.comppsych.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 11.Asselmann E, Wittchen HU, Lieb R, et al. The role of behavioral inhibition and parenting for an unfavorable emotional trauma response and PTSD. Acta Psychiatr Scand. 2015;131(4):279–289. doi: 10.1111/acps.12316. [DOI] [PubMed] [Google Scholar]
- 12.Muzik M, Morelen D, Hruschak J, et al. Psychopathology and parenting: an examination of perceived and observed parenting in mothers with depression and PTSD. J Affect Disord. 2017;207:242–250. doi: 10.1016/j.jad.2016.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- 14.Alonzo AA. The experience of chronic illness and post-traumatic stress disorder: the consequences of cumulative adversity. Soc Sci Med. 2000;50(10):1475–1484. doi: 10.1016/s0277-9536(99)00399-8. [DOI] [PubMed] [Google Scholar]
- 15.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3. Arlington, VA: Author; 1980. [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed., text rev. Washington, DC: Author; 2000.
- 17.Pinquart M. Posttraumatic Stress Symptoms and Disorders in Parents of Children and Adolescents With Chronic Physical Illnesses: a meta-analysis. J Trauma Stress. 2019;32:88–96. doi: 10.1002/jts.22354. [DOI] [PubMed] [Google Scholar]
- 18.Cabizuca M, Marques-Portella C, Mendlowicz MW, et al. Posttraumatic stress disorder in parents of children with chronic illnesses: a meta-analysis. Health Psychol. 2009;28(3):379–388. doi: 10.1037/a0014512. [DOI] [PubMed] [Google Scholar]
- 19.Schlenger WE, Caddell JM, Ebert L, et al. Psychological reactions to terrorist attacks: findings from the National Study of Americans' reactions to September 11. JAMA. 2002;288(5):581–588. doi: 10.1001/jama.288.5.581. [DOI] [PubMed] [Google Scholar]
- 20.Hashemian F, Khoshnood K, Desai MM, et al. Anxiety, depression, and posttraumatic stress in Iranian survivors of chemical warfare. JAMA. 2006;296(5):560–566. doi: 10.1001/jama.296.5.560. [DOI] [PubMed] [Google Scholar]
- 21.Darves-Bornoz JM, Alonso J, de Girolamo G, et al. Main traumatic events in Europe: PTSD in the European study of the epidemiology of mental disorders survey. J Trauma Stress. 2008;21(5):455462. doi: 10.1002/jts.20357. [DOI] [PubMed] [Google Scholar]
- 22.Lilly MM, Pole N, Best SR, et al. Gender and PTSD: what can we learn from female police officers? J Anxiety Disord. 2009;23(6):767–774. doi: 10.1016/j.janxdis.2009.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dell'Osso L, Carmassi C, Massimetti G, et al. Full and partial PTSD among young adult survivors 10 months after the L'Aquila 2009 earthquake: gender differences. J Affect Disord. 2011;131(1–3):79–83. doi: 10.1016/j.jad.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 24.Coakley RM, Forbes PW, Kelley SD, et al. Family functioning and posttraumatic stress symptoms in youth and their parents after unintentional pediatric injury. J Traum Stress. 2010;23:807–810. doi: 10.1002/jts.20586. [DOI] [PubMed] [Google Scholar]
- 25.Horsch A, McManus F, Kennedy P. Cognitive and non-cognitive factors associated with posttraumatic stress symptoms in mothers of children with type 1 diabetes. Behav Cogn Psychother. 2012;40(4):400–411. doi: 10.1017/S1352465812000112. [DOI] [PubMed] [Google Scholar]
- 26.Forinder U, Claesson L, Szybek K, et al. Exploring the content of post-traumatic stress symptoms among parents after Paediatric stem cell transplant. PLoS One. 2015;10(5):e0126905. doi: 10.1371/journal.pone.0126905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Le Gouëz M, Alvarez L, Rousseau V, et al. Posttraumatic stress reactions in parents of children esophageal atresia. PLoS One. 2016;11(3):e0150760. doi: 10.1371/journal.pone.0150760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dell’Osso L, Corsi M, Gesi C, et al. Adult autism subthreshold Spectrum (AdAS Spectrum) in parents of pediatric patients with epilepsy: correlations with post-traumatic stress symptoms. Compr Psychiatry. 2018;83:25–30. doi: 10.1016/j.comppsych.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 29.Weinstein SM, Pugach O, Rosales G, et al. Family Chaos and asthma control. Pediatrics. 2019;144(2):e20182758. doi: 10.1542/peds.2018-2758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alonso J, Angermeyer MC, Bernert S, et al. Prevalence of mental disorders in Europe: results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;420:21–27. doi: 10.1111/j.1600-0047.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- 32.Carmassi C, Dell'Osso L, Manni C, et al. Frequency of trauma exposure and post-traumatic stress disorder in Italy: analysis from the world mental health survey initiative. J Psychiatr Res. 2014;59:77–84. doi: 10.1016/j.jpsychires.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:112921. doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yuan R, Xu QH, Xia CC, et al. Psychological status of parents of hospitalized children during the COVID-19 epidemic in China. Psychiatry Res. 2020;288:112953. doi: 10.1016/j.psychres.2020.112953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lehman LL, Maletsky K, Beaute J, et al. Prevalence of symptoms of anxiety, depression, and post-traumatic stress disorder in parents and children following pediatric stroke. J Child Neurol. 2020;2020:883073820909617. doi: 10.1177/0883073820909617. [DOI] [PubMed] [Google Scholar]
- 36.Schecter R, Pham T, Hua A, et al. Prevalence and longevity of PTSD symptoms among parents of NICU infants analyzed across gestational age categories. Clin Pediatr. 2020;59(2):163–169. doi: 10.1177/0009922819892046. [DOI] [PubMed] [Google Scholar]
- 37.Werner H, Balmer C, Lehmann P. Posttraumatic stress and health-related quality of life in parents of children with cardiac rhythm devices devices. Qual Life Res. 2019;28:2471–2480. doi: 10.1007/s11136-019-02202-z. [DOI] [PubMed] [Google Scholar]
- 38.Carmassi C, Corsi M, Bertelloni CA, et al. Post-traumatic stress and major depressive disorders in parent caregivers of children with a chronic disorder. Psychiatry Res. 2019;279:195–200. doi: 10.1016/j.psychres.2019.02.062. [DOI] [PubMed] [Google Scholar]
- 39.Araújo FJO, de Lima LSA, Cidade PIM, et al. Impact of Sars-Cov-2 and its reverberation in global higher education and mental health [published online ahead of print, 2020 Apr 12] Psychiatry Res. 2020;288:112977. doi: 10.1016/j.psychres.2020.112977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cleland J Resilience or Resistance: A personal response to COVID-19 [published online ahead of print, 2020 Apr 5]. Med Educ. 2020;10.1111/medu.14170. doi:10.1111/medu.14170. [DOI] [PubMed]
- 41.Holmes EA, O'Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science [published online ahead of print, 2020 Apr 15]. Lancet Psychiatry. 2020;S2215–0366(20)30168–1. doi:10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed]
- 42.Orsini A, Corsi M, Santangelo A, et al. Challenges and management of neurological and psychiatric manifestations in SARS-CoV-2 (COVID-19) patients [published online ahead of print, 2020 Aug 6]. Neurol Sci. 2020;10.1007/s10072-020-04544-w. doi:10.1007/s10072-020-04544-w. [DOI] [PMC free article] [PubMed]
- 43.McFarlane AC. Posttraumatic stress disorder: a model of the longitudinal course and the role of risk factors. J Clin Psychiatry. 2000;61(Suppl 5):15–23. [PubMed] [Google Scholar]
- 44.Perkonigg A, Pfister H, Stein MB, et al. Longitudinal course of posttraumatic stress disorder and posttraumatic stress disorder symptoms in a community sample of adolescents and young adults. Am J Psychiatry. 2005;162(7):1320–1327. doi: 10.1176/appi.ajp.162.7.1320. [DOI] [PubMed] [Google Scholar]
- 45.Barber S, Corsi M, Furukawa TA, et al. Quality and impact of secondary information in promoting evidence-based clinical practice: a cross-sectional study about EBMH. Evidence-Based Mental Health. 2016;19:82–85. doi: 10.1136/eb-2016-102414. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.