Abstract
Since March 2020, the world has been fighting a global pandemic caused by a new coronavirus SARS-CoV-2 (COVID-19). SARS-CoV-2 is responsible for severe acute respiratory syndrome, an airway disease that can be severe and fatal in a percentage of cases. Patients with severe COVID-19 can develop extrapulmonary lesions, with renal, hepatic, cardiac, neurological, and tissue involvement that can cause further severe complications. On December 21, 2021, the European Medicines Agency (EMA) authorized the marketing of the first COVID-19 vaccine. However, several randomized trials are ongoing to find effective, safe, and widely available treatments. The most severe stages of COVID-19 infection are characterized by a multi-system inflammatory state induced by a cytokine storm causing multi-organ injury. Epidemiologic evidence has shown that glucocorticoids (GCs), particularly dexamethasone, are used in severe, hospitalized patients with COVID-19 with good therapeutic benefit. COVID-19 can also damage the endothelial system, causing microcirculatory disturbances and consequently leading to functional organ disorders. The combination of endothelial dysfunction with a generalized inflammatory state may contribute to the general pro-coagulative state described in patients with COVID-19 with increased risk of venous and arterial occlusions. The aim of this article is to describe the therapeutic utility of GCs in stabilizing the vascular endothelial barrier in COVID-19 infection. Indeed, we believe that the stabilization of the endothelial barrier and the anti-inflammatory effect of GCs could be the main effect underlying the therapeutic efficacy in COVID-19 patients.
Keywords: Desametasone, COVID-19, SARS-CoV-2, Pandemic, Inflammatory
Introduction
Aim of this article
The aim of this article is to describe the therapeutic utility of GCs in stabilizing the vascular endothelial barrier in COVID-19 infection. The stabilization of the endothelial barrier and the anti-inflammatory effect of GCs could be the main effect underlying the therapeutic efficacy in COVID-19 patients.
The global pandemic COVID-19
Since the beginning of the SARS-CoV-2 coronavirus outbreak in Wuhan China in November 2019, COVID-19 has rapidly spread around the world. In March 2020, the WHO declared a global pandemic status caused by COVID-19 (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.)
Covid-19, viral infection
Clinical manifestations
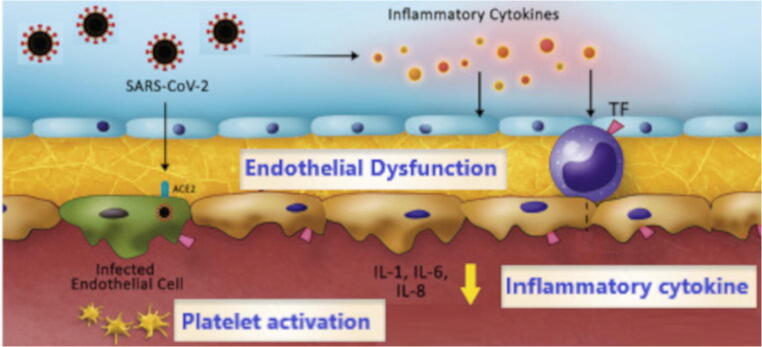
SARS-CoV-2 virus is transmitted from human to human (Li et al., 2020,b). In most cases, the incubation period is approximately 5 days after exposure; in some cases, it can last up to 15 days. The infection in a good percentage of cases may have a totally asymptomatic or mildly symptomatic course. The most common symptoms are cough and dyspnea, myalgia and fatigue, and olfactory disturbances. Epidemiologic evidence shows that fever is present in approximately 90% of patients hospitalized with COVID-19. A percentage of COVID-19-positive patients presents gastrointestinal symptoms such as nausea and diarrhea (Chen et al. 2020). In a percentage of patients, SARS-CoV-2 infection can cause several serious complications: acute respiratory distress syndrome (ARDS) is the major complication in COVID-19-positive patients. Bilateral interstitial pneumonia appears to be the most frequent severe manifestation of infection characterized by cough and dyspnea (Fu et al. 2020). However, in addition to the respiratory system, other organs, particularly the cardiovascular system, may also be affected. Epidemiological data report cases of acute cardiac injury from COVID-19. Thromboembolic complications, including pulmonary embolism, have also been reported. Some cases report hepatic injury (Struyf et al. 2020). Lesions of the lungs and other organs such as the heart or liver appear to be caused by direct or indirect damage from the virus (Chung et al. 2020). SARS-CoV-2 uses the entry receptor ACE-2 to penetrate host cells (Li et al. 2020a; Vitiello and Ferrara 2020a,b), the latter being expressed in several tissues, at the level of type II pneumocytes, cardiac cells, liver cholangiocytes, and endothelial cells. In the most severe stages of COVID-19 infection, a “cytokine cascade”(Vitiello et al. 2020a; Ferrara et al. 2020a) is generated, responsible for multi-system inflammation leading to organ injury (Ferrara et al. 2020b). As mentioned above, a percentage of COVID-19-infected patients show lesions of the cardiovascular system (Clerkin et al. 2020; Vitiello and Ferrara 2020c). Although the exact pathophysiological mechanism of cardiovascular injury in COVID-19 remains to be elucidated, there are multiple possible causes, including acute ischemic injury due to coronary artery obstruction, inflammatory myocardial edema, endotheliitis, and tissue edema due to a dysregulated and systemic immune/inflammatory response (Varga et al. 2020). Neurological damage is also associated with COVID-19 infection; binding of SARS-CoV-2 spike proteins to brain endothelial cells can result in loss of the blood-brain barrier, potentially causing the neurological symptoms associated with COVID-19. Evidence suggests that loss of vascular function and tissue edema play an important role in COVID-19 organ damage. First, there is invasion of endothelial cells (ECs) by the virus; second, there is generalized inflammation. The resulting endotheliitis is characterized by endothelial cell dysfunction. Endothelial dysfunction causes a systemic condition in which the endothelium loses its physiological and functional properties, such as vasodilation, fibrinolysis, and antiplatelet. This endothelium might explain the cardiovascular complications from COVID-19 (Teuwen et al. 2020). Furthermore, the decrease in ACE-2 in the more severe stages of infection leads to an increase in angiotensin 2 (Ang II) and activation of the kinin-kallikrein system (KKS) and increased vascular permeability. Endothelial dysfunction may be responsible for tissue edema and thrombosis formation (Fig. 1). The efficacy against inflammation and endothelial damage may be the main explanation for the efficacy of synthetic glucocorticoids (GCs) in patients with severe COVID-19. On December 21, 2021, the European Medicines Agency (EMA) granted marketing authorization for the first COVID-19 vaccine in people 16 years of age and older. To date, there are no direct antivirals against SARS-CoV-2, and therapeutic treatments are experimental (Who 2020; Vitiello et al. 2020a,b; Vitello and Ferrara 2021; Ferrara 2020).
Fig. 1.
The substances produced by the endothelium are vasoactive compounds, growth factors, mediators of inflammation, adhesion molecules, proteins of the hemostatic system. Through this wide range of compounds the endothelium intervenes in the control of vascular homeostasis, inflammation, immunity, hemostasis and performs a number of important metabolic functions The invasion of endothelial cells (EC) by the virus and the release of inflammatory cytokines cause inflammation of the endothelium. The resulting endotheliitis is characterized by endothelial cell dysfunction. Endothelial dysfunction causes a systemic condition in which the endothelium loses its physiological and functional properties, such as vasodilation, fibrinolysis, and antiplatelet. This induced endotheliitis may be responsible for tissue edema and the risk of thrombosis leading to organ damage in the COVID-19 patient
Normal endothelial function
Endothelial tissue is the cell monolayer that lines the inner surface of blood vessels. In response to stimuli, the endothelium releases factors that regulate vasomotor function, inflammatory processes (e.g., neutrophil recruitment), angiogenesis, and hemostasis. Factors that modulate vascular tone (Daiber et al. 2017) are classified as endothelium-derived relaxation factors (EDRFs), including nitric oxide (NO), prostacyclin (PGI2), and endothelium-derived hyperpolarizing factor (EDHF), and endothelium-derived contraction factors (EDCFs), including angiotensin II, endothelin-1, and vasoconstrictor prostanoids. Impairment of NO synthesis in endothelial dysfunction is responsible for excess vasoconstriction with increased vessel tone as well as decreased anti-aggregative activity.
GCs and endothelites COVID-19 induced
Synthetic GCs are glucocorticoid receptors (GCr) agonists and, to a lesser extent, mineralocorticoid receptors (MRs), both of which are members of the nuclear receptor superfamily of ligand-activated transcription factors (Alexander et al. 2008). The main GR responsible for the therapeutic effects of GCs is GRα (Walker 2007). In the vascular system, GRs are expressed by intact arteries, vascular smooth muscle cells, and endothelial cells. Therefore, the conditions suggest for direct modulation of endothelial function by GCs. Evidence from in vitro and ex vivo models suggests that GCs are capable of directly modulating endothelial function. However, their effects appear to differ depending on whether they are used in healthy or in inflammation-associated conditions. Epidemiological evidence has associated treatment with GCs, particularly dexamethasone, with good therapeutic efficacy in COVID-19 patients. In particular, recommendations on the use of GCs for COVID-19 patients are based largely on data from the RECOVERY trial, a large multi-center, randomized, open-label study. This study compared hospitalized patients who received up to 10 days of dexamethasone with those who received the standard of care. Mortality at 28 days was lower among patients who were treated with dexamethasone. This benefit was observed in patients who were mechanically ventilated or required supplemental oxygen at the time of enrollment (Horby et al. 2020). As described, patients with severe COVID-19 may develop a systemic inflammatory response that can lead to lung injury, cardiovascular injury, and neurologic injury. It has been proposed that the potent anti-inflammatory effects of COVID-19 may prevent or mitigate these detrimental effects. In particular, we believe that endothelial damage caused by an abnormal inflammatory response and an unregulated immune system is a major cause of tissue damage that occurs in the most severe stages of infection. The anti-inflammatory properties of GCs are associated with a reduction in the generalized inflammatory state in the severe COVID-19 patient with maintenance of the integrity, function, and normal activity of the endothelium and macro- and microcirculation. However, modulation of the endothelium under conditions of functional integrity and under conditions of inflammation associated with viral infection must be classified. Specifically, the effects of GCs on endothelial function in the physiological condition may lead to impaired endothelial function (Schäfer et al. 2005; Ramzy et al. 2008). The mechanisms involved are decreased vascular NO availability, which is secondary to decreased eNOS (endothelial nitric oxide synthase) activity (Rogers et al. 2002), decreased eNOS gene transcription, increased eNOS degradation (Liu et al. 2009), decreased eNOS protein stability, and decreased levels of tetrahydrobiopterin, a cofactor required for eNOS enzyme activity (Dorrance et al. 2004). In addition to decreasing eNOS activity/expression, GCs have been found to reduce the bioavailability of vascular NO by increasing the production of reactive oxygen species (ROS). Exposure of endothelial cells to dexamethasone increases ROS production by NAD(P)H oxidase and xanthine oxidase, decreases NO production, and increases cytotoxic peroxynitrite (ONOO-) production. Vascular inflammation is manifested in several ways, including increased expression of endothelial cell (EC) adhesion molecules, recruitment of inflammatory cells, cytokine release, and reduced nitric oxide (NO) bioactivity (Ait-Oufella et al. 2010; Lorant et al. 1995). Physiologically, endogenous glucocorticoids exert a permissive role in suppressing local and systemic inflammation. Administration of GCs, such as dexamethasone, is widely used to suppress inflammation, and indicated in autoimmune diseases, although the mechanisms by which they act are not fully understood (Lee and Burckart 1998; Longui 2007). The role of GCs on endothelial function under inflammatory conditions seems different than under physiological conditions. Compelling evidence supports a beneficial vascular effect of GCs in high-grade inflammation associated with septic shock, and this effect is mediated by activation of the endothelial GC receptor (Goodwin et al. 2013, 2014). The mechanisms involved in the beneficial effects of GCs on endothelial cells under inflammatory conditions are likely due to a decrease in endothelial expression of cytokines (IL-6, IL-8), G-CSF, VEGF, endothelin-1, NFκB, arginase 2, and COX-2. The use of GCs may lead to avoidance of microcirculatory disturbances, and consequently functional disturbances of all internal organs may also avoid endothelial dysfunction and generalized inflammatory state by indirectly reducing the general pro-coagulative state described in COVID-19 patients leading to venular and arteriolar occlusions. (Salvador et al. 2014; Lefer et al. 1980; Oakley and Cidlowski 2015).
Conclusions
Epidemiological evidence shows the efficacy of dexamethasone in severe COVID-19 in reducing mortality. We believe that the main anti-COVID-19 effect of GCs is associated, in parallel with known anti-inflammatory activities, with modulation of vascular and endothelial wall inflammation, reducing organ and tissue injury, edema formation, and the risk of arterial and venous occlusion, in the most severe stages of SARS-CoV-2 infection.
Copyright
The authors certify that the manuscript is original, never submitted to other journal for publication before. All authors contributed equally to the manuscript and had the opportunity to revise and approve the final text.
Authors’ contribution
Antonio Vitiello: Conceptualization, writing-original draft, methodology, writing-original draft.
Francesco Ferrara: Writing-review and editing, supervision, validation. The manuscript was written entirely by the authors. All authors made an equal contribution in the development of the paper.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Francesco Ferrara, Email: francesco.ferrara@uslumbria1.it.
Antonio Vitiello, Email: antonio.vitiello2@uslumbria1.it.
References
- Ait-Oufella H, Maury E, Lehoux S, Guidet B, Offenstadt G. The endothelium: physiological functions and role in microcirculatory failure during severe sepsis. Intensive Care Med. 2010;36(8):1286–1298. doi: 10.1007/s00134-010-1893-6. [DOI] [PubMed] [Google Scholar]
- Alexander SP, Mathie A, Peters JA (2008) Guide to receptors and channels (GRAC), 3rd edition. Br J Pharmacol. 153 Suppl 2(Suppl 2):S1–209. doi: 10.1038/sj.bjp.0707746 [DOI] [PMC free article] [PubMed]
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J', Yu T, Zhang X, Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung TW, Sridhar S, Zhang AJ. Olfactory dysfunction in coronavirus disease 2019 patients: observational cohort study and systematic review. Open Forum Infect Dis. 2020;7:ofaa199. doi: 10.1093/ofid/ofaa199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, Jain SS, Burkhoff D, Kumaraiah D, Rabbani LR, Schwartz A, Uriel N. COVID-19 and cardiovascular disease. Circulation. 2020;141(20):1648–1655. doi: 10.1161/CIRCULATIONAHA.120.046941. [DOI] [PubMed] [Google Scholar]
- Daiber A, Steven S, Weber A, Shuvaev VV, Muzykantov VR, Laher I, Li H, Lamas S, Münzel T. Targeting vascular (endothelial) dysfunction. Br J Pharmacol. 2017;174(12):1591–1619. doi: 10.1111/bph.13517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorrance AM, Mack EA, Webb RC. Glucocorticoids decrease GTP cyclohydrolase and tetrahydrobiopterin-dependent vasorelaxation through glucocorticoid receptors. J Cardiovasc Pharmacol. 2004;43:8–13. doi: 10.1097/00005344-200401000-00002. [DOI] [PubMed] [Google Scholar]
- Ferrara F. Antirheumatic in SARS-CoV-2: benefit or risk? Italian Journal of Medicine. 2020;14(2):114–115. doi: 10.4081/itjm.2020.1290. [DOI] [Google Scholar]
- Ferrara F, Granata G, Pelliccia C, La Porta R, Vitiello A. The added value of pirfenidone to fight inflammation and fibrotic state induced by SARS-CoV-2 : anti-inflammatory and anti-fibrotic therapy could solve the lung complications of the infection? Eur J Clin Pharmacol. 2020;76(11):1615–1618. doi: 10.1007/s00228-020-02947-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrara F, Porta R, D'Aiuto V, Vitiello A. Remdesivir and COVID-19. Ir J Med Sci. 2020;17:1–2. doi: 10.1007/s11845-020-02401-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrara F, Porta R, Santilli P, D'Aiuto V, Vitiello A. Are multiple sclerosis therapies safe in severe acute respiratory syndrome coronavirus 2 times? Indian J Pharmacol. 2020;52(5):441–442. doi: 10.4103/ijp.IJP_417_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020;80(6):656–665. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin JE, Feng Y, Velazquez H, Sessa WC. Endothelial glucocorticoid receptor is required for protection against sepsis. Proc Natl Acad Sci U S A. 2013;110:306–311. doi: 10.1073/pnas.1210200110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin JE, Feng Y, Velazquez H, Zhou H, Sessa WC. Loss of the endothelial glucocorticoid receptor prevents the therapeutic protection afforded by dexamethasone after LPS. PLoS One. 2014;9:e108126. doi: 10.1371/journal.pone.0108126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L et al. (2020) Dexamethasone in hospitalized patients with Covid-19 - preliminary report. N Engl J Med. NEJMoa2021436. doi: 10.1056/NEJMoa2021436
- Lee JI, Burckart GJ. Nuclear factor kappa B: important transcription factor and therapeutic target. J Clin Pharmacol. 1998;38(11):981–993. doi: 10.1177/009127009803801101. [DOI] [PubMed] [Google Scholar]
- Lefer AM, Crossley K, Grigonis G, Lefer DJ. Mechanism of the beneficial effect of dexamethasone on myocardial cell integrity in acure myocardial ischemia. Basic Res Cardiol. 1980;75(2):328–339. doi: 10.1007/BF01907581. [DOI] [PubMed] [Google Scholar]
- Li G, He X, Zhang L, Ran Q, Wang J, Xiong, et al. Assessing ACE2 expression patterns in lung tissues in the pathogenesis of COVID-19. J Autoimmun. 2020;112:102463. doi: 10.1016/j.jaut.2020.102463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Mladinov D, Pietrusz JL, Usa K, Liang M. Glucocorticoid response elements and 11β-hydroxysteroid dehydrogenases in the regulation of endothelial nitric oxide synthase expression. Cardiovasc Res. 2009;81:140–147. doi: 10.1093/cvr/cvn231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longui CA. Glucocorticoid therapy: minimizing side effects. J Pediatr. 2007;83(5 Suppl):S163–S177. doi: 10.1590/S0021-75572007000700007. [DOI] [PubMed] [Google Scholar]
- Lorant DE, Zimmerman GA, McIntyre TM, Prescott SM. Platelet-activating factor mediates procoagulant activity on the surface of endothelial cells by promoting leukocyte adhesion. Semin Cell Biol. 1995;6(5):295–303. doi: 10.1006/scel.1995.0039. [DOI] [PubMed] [Google Scholar]
- Oakley RH, Cidlowski JA. Glucocorticoid signaling in the heart: a cardiomyocyte perspective. J Steroid Biochem Mol Biol. 2015;153:27–34. doi: 10.1016/j.jsbmb.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramzy D, Tumiati LC, Tepperman E, Sheshgiri R, Jackman J, Badiwala M, Rao V. Dual immunosuppression enhances vasomotor injury: interactive effect between endothelin-1 and nitric oxide bioavailability. J Thorac Cardiovasc Surg. 2008;135:938–944. doi: 10.1016/j.jtcvs.2007.09.075. [DOI] [PubMed] [Google Scholar]
- Rogers KM, Bonar CA, Estrella JL, Yang S. Inhibitory effect of glucocorticoid on coronary artery endothelial function. Am J Physiol Heart Circ Physiol. 2002;283:1922–1928. doi: 10.1152/ajpheart.00364.2002. [DOI] [PubMed] [Google Scholar]
- Salvador E, Shityakov S, Förster C. Glucocorticoids and endothelial cell barrier function. Cell Tissue Res. 2014;355(3):597–605. doi: 10.1007/s00441-013-1762-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schäfer SC, Wallerath T, Closs EI, Schmidt C, Schwarz PM, Förstermann U, Lehr HA. Dexamethasone suppresses eNOS and CAT-1 and induces oxidative stress in mouse resistance arterioles. Am J Physiol Heart Circ Physiol. 2005;288(1):H436–H444. doi: 10.1152/ajpheart.00587.2004. [DOI] [PubMed] [Google Scholar]
- Struyf T, Deeks JJ, Dinnes J, Takwoingi Y, Davenport C, Leeflang MM, et al. Cochrane COVID-19 Diagnostic Test Accuracy Group. Signs and symptoms to determine if a patient presenting in primary care or hospital outpatient settings has COVID-19 disease. Cochrane Database Syst Rev. 2020;7(7):CD013665. doi: 10.1002/14651858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teuwen LA, Geldhof V, Pasut A, Carmeliet P. COVID-19: the vasculature unleashed. Nat Rev Immunol. 2020;20(7):389–391. doi: 10.1038/s41577-020-0343-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitiello A, Ferrara F. Correlation between renin-angiotensin system and severe acute respiratory syndrome coronavirus 2 infection: what do we know? Eur J Pharmacol. 2020;883:173373. doi: 10.1016/j.ejphar.2020.173373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitiello A, Ferrara F. Pharmacological agents to therapeutic treatment of cardiac injury caused by Covid-19. Life Sci. 2020;262:118510. doi: 10.1016/j.lfs.2020.118510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitiello A, Ferrara F. Remdesivir versus ritonavir/lopinavir in COVID-19 patients. Ir J Med Sci. 2020;18:1–2. doi: 10.1007/s11845-020-02440-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitiello A, Ferrara F. Therapeutic strategies for SARS-CoV-2 acting on ACE-2. Eur J Pharm Sci. 2021;156:105579. doi: 10.1016/j.ejps.2020.105579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitiello A, Ferrara F, Pelliccia C, Granata G, La Porta R. Cytokine storm and colchicine potential role in fighting SARS-CoV-2 pneumonia. Italian Journal of Medicine. 2020;14(2):88–94. doi: 10.4081/itjm.2020.124. [DOI] [Google Scholar]
- Vitiello A, La Porta R, Ferrara F (2020b) Sacubitril, valsartan and SARS-CoV-2. BMJ Evid Based Med. bmjebm-2020-111497. doi: 10.1136/bmjebm-2020-111497 [DOI] [PubMed]
- Walker BR. Glucocorticoids and cardiovascular disease. Eur J Endocrinol. 2007;157(5):545–559. doi: 10.1530/EJE-07-0455. [DOI] [PubMed] [Google Scholar]
- World health organization (WHO) https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. [Accessed 30 Nov 2020]