Key Points
Question
Is implementation of national initiatives associated with improvement in disparities between White and Black patients in the use of surgical procedures in the US?
Findings
In this case-control study using national inpatient data from 2012 to 2017, racial disparities in the use of surgical procedures persisted for all 9 analyzed procedures and worsened for 3 of the analyzed procedures. These disparities were evident regardless of US census division, hospital teaching status, or patient insurance status.
Meaning
Despite the largest national initiative to date aimed at improving racial disparities, these disparities appear to persist and, in some cases, have worsened, highlighting the need for renewed initiatives to improve health care equality.
Abstract
Importance
The largest US federal action plan to date for reducing racial disparities in health care was implemented in 2011 and continues today. It is not known whether this program, along with other initiatives, is associated with a decrease in racial disparities in the use of major surgical procedures in the US.
Objective
To analyze whether national initiatives are associated with improvement in racial disparities between White and Black patients in the use of surgical procedures in the US.
Design, Setting, and Participants
In this case-control study, the national rates of use for 9 major surgical procedures previously shown to have racial disparities in rates of performance between White and Black adult patients (including angioplasty, spinal fusion, carotid endarterectomy, appendectomy, colorectal resection, coronary artery bypass grafting, total hip arthroplasty, total knee arthroplasty, and heart valve replacement) were analyzed from January 1, 2012, through December 31, 2017. Data analysis was conducted from May 1 to June 30, 2020. Population- and sex-adjusted procedural rates during the study period were examined and standardized based on all-payer insurance status. Racial changes were further analyzed by US census division and hospital teaching status for 4 selected procedures: coronary artery bypass grafting, carotid endarterectomy, total hip arthroplasty, and heart valve replacement.
Main Outcomes and Measures
Population- and race-adjusted procedural rates by year, US census division, hospital teaching status, and insurance status.
Results
This study included national inpatient data from 2012 to 2017. In 2012, the national
incidence rate of all 9 major surgical procedures was higher in White than in Black individuals.
For example, the incidence rate of total knee arthroplasty in 2012 for White males was 184.8 per 100 000 persons and for Black males was 79.8 per 100 000 persons. By 2017, these racial disparities persisted for all 9 procedures analyzed. For example, the incidence rate of total knee arthroplasty in 2017 for White males was 220.5 per 100 000 persons and for Black males was 95.6 per 100 000 persons. Although the disparity gap between White and Black patients narrowed for angioplasty (−20.1 per 100 000 persons in males, −4.2 per 100 000 persons in females), spinal fusion (−7.7 per 100 000 persons in males, −15.0 per 100 000 persons in females), carotid endarterectomy (−4.3 per 100 000 persons in males, −4.6 per 100 000 persons in females), appendectomy (−12.3 per 100 000 persons in males, −12.2 per 100 000 persons in females), and colorectal resection (−9.0 per 100 000 persons in males, −12.7 per 100 000 persons in females), the disparity remained constant for coronary artery bypass grafting and widened for 3 procedures, total hip arthroplasty (11.6 per 100 000 persons in males, 20.8 per 100 000 in females), total knee arthroplasty (19.9 per 100 000 persons in males, 12.0 per 100 000 persons in females), and heart valve replacement(12.4 per 100 000 persons in males, 9.2 per 100 000 persons in females). In 2017, racial differences persisted in all US census divisions and in both urban teaching and urban nonteaching hospitals. When rates were adjusted based on insurance status, Black patients with Medicare, Medicaid, and private insurance underwent lower rates of all procedures analyzed compared with White patients. For example, rate of spinal fusion in Black patients was 70.2% of the rate in White patients with Medicare, 56.5% to that of White patients with Medicaid, and 61.2% to that of White patients with private insurance.
Conclusions and Relevance
Results of this study suggest that despite national initiatives, racial disparities have persisted for all analyzed procedures and worsened for one-third of the analyzed procedures. These disparities were evident regardless of US census division, hospital teaching status, or insurance status. Renewed initiatives to help diminish racial disparities and improve health care equality are warranted.
This case-control study examines changes in racial disparity between Black and White patients in the rates of common surgical procedures conducted in the US between 2012 and 2017.
Introduction
Racial disparities in the delivery of health care in the US have been reported in multiple areas of medicine and in various surgical fields.1,2,3,4,5 Lower rates of preventive treatments and worse clinical outcomes after surgery have been shown for racial and ethnic minorities.6,7,8,9,10,11,12,13,14 Rates of use of multiple surgical procedures have been reported to be lower among racial and ethnic minorities than in White patients.1,4,5 Several reasons for these disparities have been proposed, including decreased access to care along with other social and systemic factors.6,15,16,17,18,19,20,21,22 Furthermore, a national US survey conducted in 2017 noted that approximately 22% of Black adults avoided seeking medical care out of fear of discrimination.23
Numerous national initiatives have been implemented to help eliminate racial disparities in health care.24,25,26,27 The Institute of Medicine released a 2010 report showing little progress in the reduction of racial disparities in medicine.28 In 2011, the US Department of Health and Human Services (HHS) launched the largest federally based action plan to date aimed at improving health care equality for all races and ethnicities.27 This action plan was designed to help streamline policy efforts and government programs to reduce disparities among racial and ethnic minorities by assessing resource allocation, increasing the availability of data to improve minority population health, providing incentives for quality care of minority populations, and assessing improvement in disparities over time.27 Subsequent policy changes and programs have also been developed, including a detailed guide for achieving health care equality from the Institute for Healthcare Improvement, referring to racial inequalities as a “forgotten aim.”28 The extent to which these initiatives have led to subsequent improvement in or elimination of the racial gap of surgical use in the US is not known. Specifically, to our knowledge, no recent studies analyzing changes in racial disparity using national, all-payer samples examining a broad group of surgical procedures exist since the period of implementation of the HHS action plan.
The purpose of this study was to analyze trends over time in racial disparities in patients undergoing major surgical procedures in the US and examine whether the gap in surgical use between White and Black patients has widened or narrowed since the development of new national initiatives to reduce these disparities. In addition, we sought to analyze whether racial differences exist based on geographic factors, hospital teaching status, or insurance type. We hypothesized that, despite national initiatives and health policy changes, persistent racial disparities would exist throughout the study period for the analyzed surgical procedures regardless of geographic division, hospital teaching status, or insurance status.
Methods
Data Source
The National Inpatient Sample (NIS), developed by the Agency for Healthcare Research and Quality as part of the Healthcare Cost and Utilization Project, is the largest all-payer database for inpatient hospital admissions in the US and has been released annually from 1988 through 2017.29 The NIS collects demographic information, such as age, sex, and race, as well as clinical information on the type of procedure and comorbidities. The NIS uses data from more than 35 million hospitalizations to provide national estimates of inpatient admissions and redesigned its hospital sampling method to improve these estimates starting in 2012.29 To study data years with the same sampling and weighting methods, we selected January 1, 2012, as the start of the study and ended on December 31, 2017, which is the most recent year published. Data analysis was performed from May 1 to June 30, 2020. This study did not require review by the Johns Hopkins Institutional Review Board because it was not human subjects research and data were deidentified and are publicly available. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for case-control studies.
Patient Selection
Consistent with previous reports, we selected major surgical procedures from various specialties that are commonly performed, expensive, associated with high rates of disease or death, and have been shown to have racial disparities in their use.1,2,3,4,5 Selected procedures included percutaneous transluminal coronary angioplasty; spinal fusion; coronary artery bypass grafting (CABG); carotid endarterectomy; total hip arthroplasty (THA), excluding diagnoses of hip fracture, dislocation, or revision; total knee arthroplasty (TKA); heart valve replacement; appendectomy; and colorectal resection. Procedures were identified using clinical classification software from the Healthcare Cost and Utilization Project designed for categorizing International Classification of Diseases (ICD) codes into categories for research purposes and longitudinal analyses.30
Statistical Analysis
National estimates of each surgical procedure were calculated for White, Black, Hispanic, and Asian patients. Race- and sex-adjusted incidence for each procedure were calculated using race-specific US Census population data for each year (eTable 1 in the Supplement).31 The difference in rates of use for the procedures between White and Black patients was analyzed from 2012 to 2017 to assess for widening or narrowing of the gap between the races. In addition, we selected 4 procedures: CABG, carotid endarterectomy, THA, and heart valve replacement, to illustrate national changes in use between White, Black, Hispanic, and Asian patients from 2012 to 2017. We chose these 4 procedures because they are common and represent both orthopedic and cardiovascular conditions, consistent with previous reports.1,2,3,4,5 Regional differences were assessed by calculating race-adjusted use rates by US census division and were compared between urban teaching hospitals and urban nonteaching hospitals. We specifically analyzed urban hospitals since this would limit confounding from differences in population demographic characteristics in rural hospital settings. Procedures were analyzed by patient insurance type and split into 3 groups: Medicare, Medicaid, and private insurance. Total enrollees for each insurance type by race were obtained from US census data and race-adjusted procedural incidence rates were compared between White and Black patients.32 As in previous reports, we focused our analysis on disparities between White and Black patients because these groups provide a benchmark of overall changes in health care disparities, but also provide analysis for Hispanic and Asian patients (eTable 1 in the Supplement). Demographic data and characteristics of the study population were collected (eTable 2 in the Supplement). Overall, 4.9% of the surgical cases analyzed in the study had missing race data and were not included in the final analysis. Data were analyzed using SPSS, version 23.0, software (IBM Corp).
Results
The race-adjusted procedural incidence was higher for White than Black patients for every procedure analyzed at every time point in the study, for both men and women. For example, the incidence rate of total knee arthroplasty in 2012 for White males was 184.8 per 100 000 persons and for Black males was 79.8 per 100 000 persons. By 2017, these racial disparities persisted for all 9 procedures analyzed. For example, the incidence rate of total knee arthroplasty in 2017 for White males was 220.5 per 100 000 persons and for Black males was 95.6 per 100 000 persons. The difference between use for White and Black patients from 2012 to 2017 narrowed for 5 procedures including angioplasty (−20.1 per 100 000 persons in males, −4.2 per 100 000 persons in females), spinal fusion (−7.7 per 100 000 persons in males, −15.0 per 100 000 persons in females), carotid endarterectomy (−4.3 per 100 000 persons in males, −4.6 per 100 000 persons in females), appendectomy (−12.3 per 100 000 persons in males, −12.2 per 100 000 persons in females), and colorectal resection (−9.0 per 100 000 persons in males, −12.7 per 100 000 persons in females), the disparity remained constant for coronary artery bypass grafting and widened for 3 procedures, total hip arthroplasty (11.6 per 100 000 persons in males, 20.8 per 100 000 in females), total knee arthroplasty (19.9 per 100 000 persons in males, 12.0 per 100 000 persons in females), and heart valve replacement(12.4 per 100 000 persons in males, 9.2 per 100 000 persons in females). This finding was true for both men and women (Table 1).
Table 1. Comparison of Population-Adjusted Incidence Rates of Surgical Procedures per 100 000 Persons in the US .
| Variable | 2012 | 2017 | Change in differencea | ||||
|---|---|---|---|---|---|---|---|
| White | Black | Difference | White | Black | Difference | ||
| Men | |||||||
| Angioplasty | 227.1 | 134.5 | 92.6 | 202.8 | 130.3 | 72.5 | −20.1 |
| Spinal fusion | 139.6 | 87.8 | 51.8 | 141.4 | 97.3 | 44.1 | −7.7 |
| CABG | 97.8 | 40.8 | 57.0 | 98.6 | 42.3 | 56.3 | −0.7 |
| Carotid endarterectomy | 38.0 | 10.0 | 28.0 | 40.5 | 16.8 | 23.7 | −4.3 |
| THA | 98.4 | 52.9 | 45.5 | 131.7 | 74.6 | 57.1 | 11.6 |
| TKA | 184.8 | 79.8 | 105.1 | 220.5 | 95.6 | 124.9 | 19.9 |
| Valve replacement | 48.3 | 20.3 | 27.9 | 70.0 | 29.6 | 40.4 | 12.4 |
| Appendectomy | 76.7 | 57.8 | 18.9 | 46.7 | 40.1 | 6.6 | −12.3 |
| Colorectal resection | 90.6 | 68.7 | 21.9 | 59.0 | 46.0 | 12.9 | −9.0 |
| Women | |||||||
| Angioplasty | 105.9 | 97.4 | 8.6 | 94.3 | 89.9 | 4.3 | −4.2 |
| Spinal fusion | 158.1 | 96.5 | 61.6 | 152.5 | 105.9 | 46.6 | −15.0 |
| CABG | 33.9 | 26.9 | 7.0 | 30.6 | 24.7 | 5.9 | −1.1 |
| Carotid endarterectomy | 26.8 | 9.8 | 17.0 | 28.6 | 16.2 | 12.4 | −4.6 |
| THA | 118.2 | 60.0 | 58.2 | 160.6 | 81.6 | 79.0 | 20.8 |
| TKA | 277.9 | 185.7 | 92.2 | 322.7 | 218.5 | 104.2 | 12.0 |
| Valve replacement | 30.7 | 18.8 | 11.9 | 46.4 | 25.3 | 21.1 | 9.2 |
| Appendectomy | 75.5 | 55.8 | 19.8 | 48.3 | 40.8 | 7.5 | −12.2 |
| Colorectal resection | 103.8 | 73.4 | 30.4 | 66.4 | 48.7 | 17.7 | −12.7 |
Abbreviations: CABG, coronary artery bypass grafting; THA, total hip arthroplasty; TKA, total knee arthroplasty.
Change in difference between 2012 and 2017. A negative value indicates narrowing of the gap between White and Black individuals; a positive value indicates widening of the gap.
When analyzing CABG, carotid endarterectomy, THA, and heart valve replacement specifically, the rate of CABG remained relatively constant over time, with White patients having nearly double the race-adjusted incidence per 100 000 persons (65.5 in 2012, 64.2 in 2017) during each year compared with Black (33.5 in 2012, 33.1 in 2017), Hispanic (22.8 in 2012, 26.0 in 2017), and Asian (28.9 in 2012, 33.6 in 2017) patients. There was an overall increasing incidence of carotid endarterectomy, THA, and heart valve replacement from 2012 to 2017, but the incidence for White patients increased more than the incidence for Black, Hispanic, and Asian patients (Figure 1). For example, the incidence of THA in White patients increased from 108.4 per 100 000 persons in 2012 to 146.3 per 100 000 persons in 2017 while the incidence of THA in Black patients only increased from 56.6 per 100 000 person in 2012 to 78.2 per 100 000 persons in 2017 (Figure 1).
Figure 1. National Population-Adjusted Rates of Analyzed Surgical Procedures by Procedure.
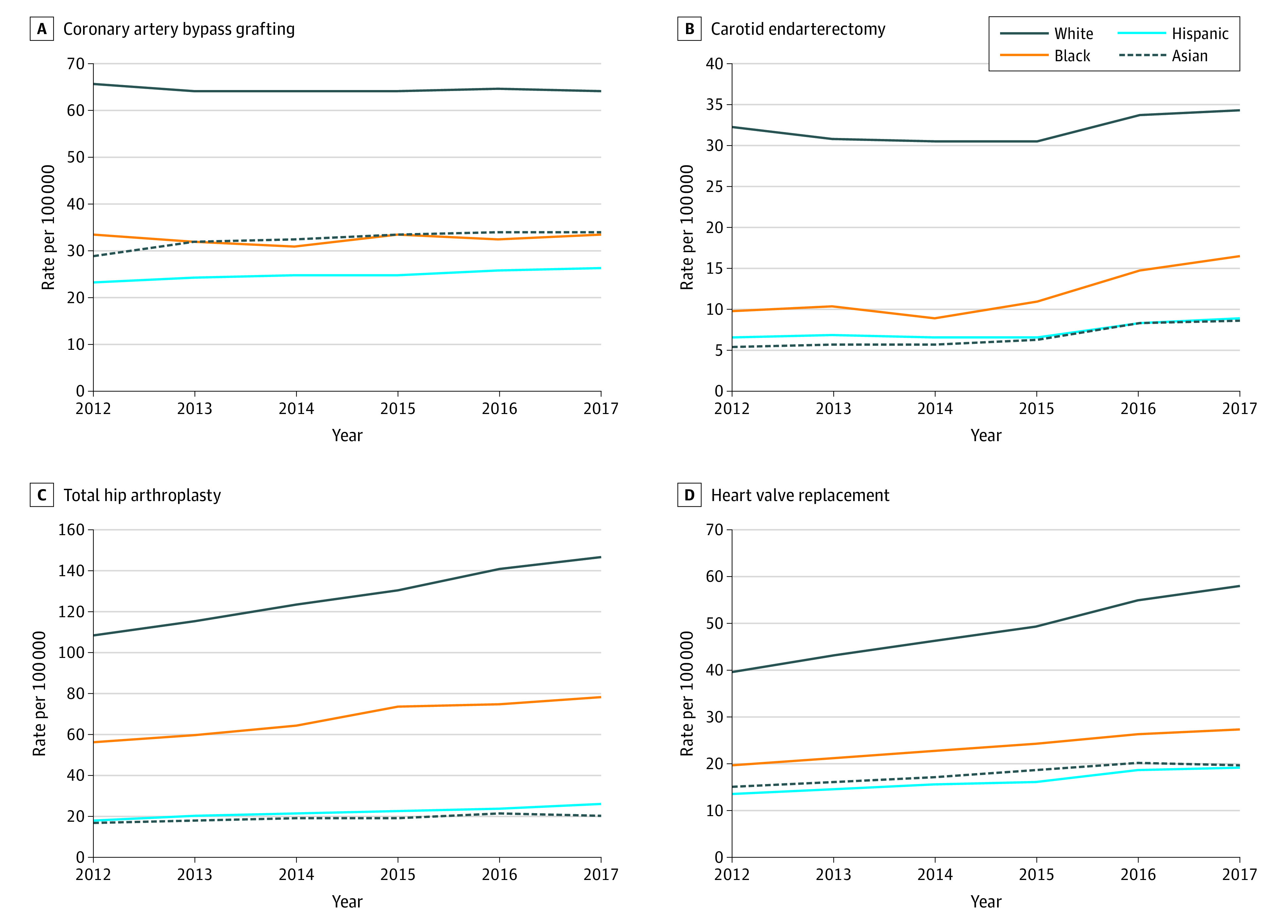
Rates per 100 000 of the US population from 2012 to 2017 of coronary artery bypass grafting (A), carotid endarterectomy (B), total hip arthroplasty (C), and heart valve replacement (D).
In analysis of the race-adjusted incidence of CABG, carotid endarterectomy, THA, and heart valve replacement by US census division, comparing urban teaching hospitals with urban nonteaching hospitals, incidence rates were higher for White than Black patients for every procedure in every US census division. For example, in urban nonteaching hospitals in the East North Central census division, the rate of CABG in White patients was 14.8 per 100 000 while the rate in Black patients was 3.1 per 100 000 in 2017. Although greater differences between White and Black patients were shown in urban nonteaching hospitals, similar changes were observed in urban teaching hospitals. For example, in urban teaching hospitals in the New England census division, the rate of CABG in White patients was 55.7 per 100 000 while the rate in Black patients was 22.4 per 100 000 in 2017. (Figure 2).
Figure 2. National Population-Adjusted Rates of Analyzed Surgical Procedures by US Census Division and Hospital Teaching Status.
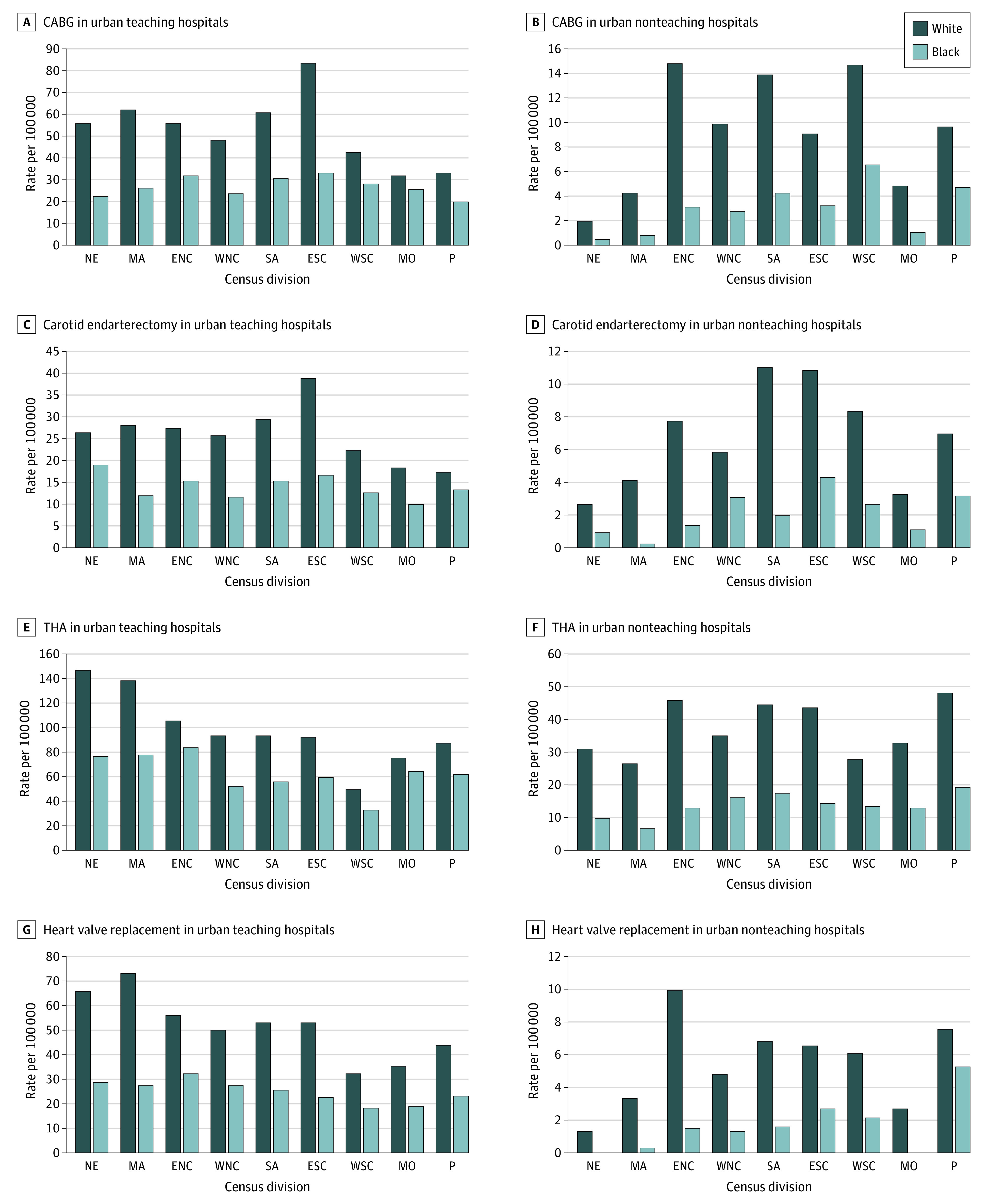
Rates per 100 000 of the US population in 2017 by urban hospital teaching status and US census division for coronary artery bypass grafting (CABG) (A and B), carotid endarterectomy (C and D), total hip arthroplasty (THA) (E and F), and heart valve replacement (G and H). ENC indicates East North Central; ESC, East South Central; MA, Mid-Atlantic; MO, Mountain; NE, New England; P, Pacific; SA, South Atlantic; WNC, West North Central, and WSC, West South Central.
Race-adjusted incidence per 100 000 enrollees was calculated for each surgical procedure using race-based enrollment for each payment system (Medicare, Medicaid, and private insurance) as the denominator. Within all Medicare enrollees, the race-adjusted incidence was higher for White than Black patients for all procedures analyzed (eg, 81.7% higher incidence of appendectomy in White patients compared with Black patients). Among all Medicaid enrollees, the race-adjusted incidence was higher for White than Black patients for all procedures (eg, 74.4% higher for THA). Among all private insurance enrollees (using total private insurance enrollees by race as the denominator), White patients had nearly double the incidence of all surgical procedures analyzed compared with Black patients (eg, 68.3% higher for colorectal resection) (Table 2).
Table 2. National Race-Adjusted Incidence Rates of Surgical Procedures by Insurance Type per 100 000 Enrollees in the US in 2017.
| Variable | Medicare | Medicaid | Private insurance | ||||||
|---|---|---|---|---|---|---|---|---|---|
| White | Black | Difference, %a | White | Black | Difference, %a | White | Black | Difference, %a | |
| Total enrollees, million | 41.9 | 6.0 | NA | 26.7 | 12.5 | NA | 143.2 | 24.0 | NA |
| Adjusted incidence (per 100 000 enrollees) | |||||||||
| Angioplasty | 465.2 | 369.2 | 79.4 | 93.7 | 59.1 | 63.2 | 72.2 | 44.5 | 61.6 |
| Spinal fusion | 373.5 | 262.3 | 70.2 | 101.8 | 57.5 | 56.5 | 95.0 | 58.2 | 61.2 |
| CABG | 213.4 | 117.5 | 55.0 | 32.6 | 14.9 | 45.7 | 31.4 | 15.6 | 49.7 |
| Carotid endarterectomy | 143.0 | 67.1 | 46.9 | 12.7 | 7.4 | 58.2 | 10.7 | 5.8 | 54.2 |
| THA | 456.6 | 231.3 | 50.7 | 50.7 | 37.7 | 74.4 | 90.7 | 50.7 | 55.9 |
| TKA | 904.2 | 550.2 | 60.8 | 77.3 | 52.3 | 67.7 | 154.0 | 93.7 | 60.8 |
| Valve replacement | 224.4 | 100.0 | 44.5 | 26.7 | 17.1 | 64.1 | 21.8 | 10.7 | 49.3 |
| Appendectomy | 60.6 | 49.5 | 81.7 | 62.9 | 42.9 | 68.2 | 41.7 | 24.8 | 59.5 |
| Colorectal resection | 180.7 | 140.2 | 77.6 | 39.9 | 27.8 | 69.6 | 38.9 | 26.6 | 68.3 |
Abbreviations: CABG, coronary-artery bypass grafting; NA, not applicable; THA, total hip arthroplasty; TKA, total knee arthroplasty.
Difference in rate of use in Black patients divided by rate of use in White patients.
Discussion
This study noted persistent racial disparities in patients undergoing major surgical procedures in the US. The race-adjusted incidence of every procedure analyzed was higher for White than Black patients at all time points of the study period. The difference in race-adjusted procedure incidence between White and Black patients narrowed for 5 procedures, remained constant for 1 procedure, and widened for 3 procedures from 2012 to 2017. These racial differences were also observed across all census divisions and in urban teaching hospitals and urban nonteaching hospitals. Adjusted incidence by payer status showed that Black patients underwent surgery at nearly half the rate of White patients for every procedure analyzed for Medicare, Medicaid, and private insurance enrollees.
Racial disparities in patients undergoing surgery have been reported in various settings and patient groups.1,2,3,4,5,6,7,8,9,10,11,12,13,14 Jha et al1 analyzed Medicare beneficiaries and showed similar results to what we noted, only in an older, more homogeneous population. The authors used Medicare data from 1992 to 2001 and compared differences in White and Black patients. Similarly, Schoenfeld et al4 used Medicare data to investigate racial differences of surgery use in Medicare Accountable Care Organizations and showed persistent differences before and after implementation of Accountable Care Organizations. We expanded on the results of previous studies by (1) analyzing nationally representative data and providing national incidence rates for several procedures, (2) analyzing differences in private insurance and Medicaid payers, in addition to Medicare beneficiaries, (3) examining differences by census division and hospital teaching status, and (4) providing updated data through 2017, which overlaps the implementation of the largest federal initiative to date aimed at reducing health care disparities.27 In the present study, we noted apparently persistent differences in national rates of surgery use between White and Black patients, with Black patients consistently undergoing lower rates of surgery in every analysis at every time point through 2017.
The findings of the present study are concerning particularly because racial disparities in health care have been widely known since the 1990s and reported extensively in the literature. Many national initiatives have been implemented to ameliorate and reduce these differences in health care inequality. The Healthy People 2010 Final Review highlighted racial and ethnic health disparities from the decade before its publication.33 Following release of this report, the US Department of Health and Human Services Action Plan to Reduce Racial and Ethnic Health Disparities (HHS Disparities Action Plan) was first published in April 2011.27 The HHS Disparities Action plan is the most comprehensive federal program to date aimed at eliminating racial disparities in health care and helps to coordinate policy efforts to lessen health care inequality in the US. Major HHS implementation and policy changes occurred from 2011 to 2014, which coincides with the early period of this study.34 Despite this ambitious and well-organized effort, the results of this study suggest that further action and renewed initiative are needed.
There were other notable national health reform undertakings that occurred during the period of this study. The Affordable Care Act insurance expansions included provisions for increasing the age limit for dependents covered under their parents’ insurance plans, the creation of health insurance exchanges or Marketplaces for those without employer-sponsored insurance coverage, an individual mandate for coverage, and coverage for individuals with preexisting conditions. In addition, a 2012 Supreme Court ruling expanded state Medicaid for adults with low income regardless of disability status, which increased the number of Medicaid recipients by more than 10 million from 2013 to 2019.35 Several new Medicare programs also were implemented during this study period. The Hospital Readmissions Reduction Program, which provides incentives for quality of care by decreasing payments for readmissions, was implemented in 2012 and the Medicare Bundled Payments for Care Improvement initiative was implemented in 2013. Although the Affordable Care Act provisions and Medicaid expansions were not specifically geared toward reducing racial disparities in health care, the results of the present study may also be interpreted in the context of these overall health care reforms.
The findings illustrated in this study show worsening changes in the area of THA and TKA, which are among the most widely used surgeries in the US and are rapidly increasing in incidence.36 A report by Amen et al36 showed persistent racial differences in THA and TKA through 2015, with a tapering or leveling off of the disparity gap. The present study expands on those findings by including more recent data and complementing the results with census division, hospital characteristics, and payer status analyses. The findings of the present study suggest that the racial disparities are worsening in every category with no indication of improvement through 2017. Total joint arthroplasty is an important area of investigation into racial differences particularly because there is a well-established lack of a biological reason for these differences. Black individuals experience osteoarthritis at a prevalence equal to or greater than that of White individuals, yet this study and others observed persistent and, in this case, worsening racial disparities in the surgical management of hip and knee osteoarthritis.37,38 This occurrence is apparent despite initiatives by the American Academy of Orthopaedic Surgeons and other groups to reduce or eliminate these disparities.24,25
Several of the aforementioned studies along with others have demonstrated racial differences in surgical use for Medicare beneficiaries.1,4,5 This study appears to support these results and suggests persistence of this trend through 2017. In addition, the present study noted that these racial differences appear to persist in other groups, such as those with Medicaid and private insurance. In patients enrolled in Medicaid, the rate of surgical use for Black patients was nearly half that of White patients when race-adjusted rates based on the number of national enrollees were analyzed. These findings are in agreement with previous studies that have reported decreased access to care in patients enrolled in Medicaid.39
Explanations for the disproportionate difference in surgical use between different racial and ethnic groups have been proposed and studied. It is unlikely that racial differences in the rates of the surgeries analyzed in this study are due to differences in disease burden or biological reasons, but rather are multifactorial and likely due to various social and systemic influences.6,15,16,17,18,19,20,21,22 Variations in physician recommendations, socioeconomic factors, cultural beliefs, mistrust of the health care system, risk averseness to newer procedures, and physicians’ implicit bias have been reported as factors contributing to racial disparities in health care.6,15,16,17,18,19,20,21,22 In addition, decreased access to care associated with factors such as socioeconomic status, insurance status, geography, and possibly increasing medical subspecialization, may all play a role in health care disparities.39,40 In a 2017 Robert Wood Johnson Foundation survey, one-third of Black adults reported experiencing racial discrimination when visiting a physician and 22% avoided seeking care out of fear of racial discrimination.23 This poll, although published in 2017 during the final year of data collection in this study, is likely reflective of earlier beliefs and may still have influenced racial disparities before, during, and after the study period presented herein.
Limitations
There are several limitations of this study. Although we report differences in the race- and population-adjusted national incidence of surgical procedures, we cannot determine whether these differences are due to overuse by White patients or underuse by Black patients. The NIS, like any database, is subject to coding error and there is a possibility of diagnosis coding error when switching from ICD-9 to ICD-10 during the 2015 data year. However, coding error is more likely to affect comorbidity and diagnosis data rather than single procedure coding, and we do not report on comorbidity data.41 In addition, the analysis focused on 2012 and 2017 and not specifically on the 2015 data year. Furthermore, any coding error would likely be evenly distributed over races and would not affect the racial differences that were analyzed in this study. Although we provide findings from the comparison of urban teaching and urban nonteaching hospitals, the NIS does not allow for identification of specific hospitals or determination of the proportion of racial or ethnic minorities treated at a given hospital. Furthermore, we cannot evaluate or compare clinical outcomes or follow-up data after surgery between groups since the NIS does not collect this information. One strength of the NIS is that it provides a nationally representative, all-payer sample that can be used to analyze changes that cannot be examined with smaller patient cohorts.
Conclusions
The results of this study suggest that racial disparities persist in the use of major surgical procedures in the US, with Black patients undergoing surgery at lower rates than White patients. These differences were apparent for all procedures analyzed, in all census divisions, and in both teaching and nonteaching urban hospital settings. In addition, racial differences were observed in the Medicare, Medicaid, and private insurance populations. The findings of this study highlight the need for renewed initiatives to diminish racial disparities and improve health care equality.
eTable 1. Gender-Adjusted and Population-Adjusted National Incidence of Surgical Procedures by Race in the United States from 2012 to 2017
eTable 2. Demographic Data and Characteristics of the Study Population
References
- 1.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353(7):683-691. doi: 10.1056/NEJMsa050672 [DOI] [PubMed] [Google Scholar]
- 2.Goodman SM, Parks ML, McHugh K, et al. Disparities in outcomes for African Americans and Whites undergoing total knee arthroplasty: a systematic literature review. J Rheumatol. 2016;43(4):765-770. doi: 10.3899/jrheum.150950 [DOI] [PubMed] [Google Scholar]
- 3.Schoenfeld AJ, Tipirneni R, Nelson JH, Carpenter JE, Iwashyna TJ. The influence of race and ethnicity on complications and mortality after orthopedic surgery: a systematic review of the literature. Med Care. 2014;52(9):842-851. doi: 10.1097/MLR.0000000000000177 [DOI] [PubMed] [Google Scholar]
- 4.Schoenfeld AJ, Sturgeon DJ, Dimick JB, et al. Disparities in rates of surgical intervention among racial and ethnic minorities in Medicare accountable care organizations. Ann Surg. 2019;269(3):459-464. doi: 10.1097/SLA.0000000000002695 [DOI] [PubMed] [Google Scholar]
- 5.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349(14):1350-1359. doi: 10.1056/NEJMsa021569 [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine . Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press; 2003. [PubMed] [Google Scholar]
- 7.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE III. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945-949. doi: 10.1001/archsurg.143.10.945 [DOI] [PubMed] [Google Scholar]
- 8.Mehtsun WT, Figueroa JF, Zheng J, Orav EJ, Jha AK. Racial disparities in surgical mortality: the gap appears to have narrowed. Health Aff (Millwood). 2017;36(6):1057-1064. doi: 10.1377/hlthaff.2017.0061 [DOI] [PubMed] [Google Scholar]
- 9.Cooper GS, Yuan Z, Landefeld CS, Rimm AA. Surgery for colorectal cancer: race-related differences in rates and survival among Medicare beneficiaries. Am J Public Health. 1996;86(4):582-586. doi: 10.2105/AJPH.86.4.582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lucas FL, Stukel TA, Morris AM, Siewers AE, Birkmeyer JD. Race and surgical mortality in the United States. Ann Surg. 2006;243(2):281-286. doi: 10.1097/01.sla.0000197560.92456.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morris AM, Billingsley KG, Baxter NN, Baldwin LM. Racial disparities in rectal cancer treatment: a population-based analysis. Arch Surg. 2004;139(2):151-155. doi: 10.1001/archsurg.139.2.151 [DOI] [PubMed] [Google Scholar]
- 12.Rangrass G, Ghaferi AA, Dimick JB. Explaining racial disparities in outcomes after cardiac surgery: the role of hospital quality. JAMA Surg. 2014;149(3):223-227. doi: 10.1001/jamasurg.2013.4041 [DOI] [PubMed] [Google Scholar]
- 13.Schoenfeld AJ, Sieg RN, Li G, Bader JO, Belmont PJ Jr, Bono CM. Outcomes after spine surgery among racial/ethnic minorities: a meta-analysis of the literature. Spine J. 2011;11(5):381-388. doi: 10.1016/j.spinee.2011.03.013 [DOI] [PubMed] [Google Scholar]
- 14.Sultan DH, Gishe J, Hanciles A, Comins MM, Norris CM. Minority use of a National Cancer Institute–designated comprehensive cancer center and non-specialty hospitals in two Florida regions. J Racial Ethn Health Disparities. 2015;2(3):373-384. doi: 10.1007/s40615-015-0084-0 [DOI] [PubMed] [Google Scholar]
- 15.Cox ED, Nackers KA, Young HN, Moreno MA, Levy JF, Mangione-Smith RM. Influence of race and socioeconomic status on engagement in pediatric primary care. Patient Educ Couns. 2012;87(3):319-326. doi: 10.1016/j.pec.2011.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Variation in perceptions of treatment and self-care practices in elderly with osteoarthritis: a comparison between African American and White patients. Arthritis Rheum. 2001;45(4):340-345. doi: [DOI] [PubMed] [Google Scholar]
- 17.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Differences in expectations of outcome mediate African American/White patient differences in “willingness” to consider joint replacement. Arthritis Rheum. 2002;46(9):2429-2435. doi: 10.1002/art.10494 [DOI] [PubMed] [Google Scholar]
- 18.Kennedy BR, Mathis CC, Woods AK. African Americans and their distrust of the health care system: healthcare for diverse populations. J Cult Divers. 2007;14(2):56-60. [PubMed] [Google Scholar]
- 19.Hausmann LRM, Mor M, Hanusa BH, et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010;25(9):982-988. doi: 10.1007/s11606-010-1399-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504-1510. doi: 10.1007/s11606-013-2441-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whittle J, Conigliaro J, Good CB, Lofgren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. 1993;329(9):621-627. doi: 10.1056/NEJM199308263290907 [DOI] [PubMed] [Google Scholar]
- 22.Constantinescu F, Goucher S, Weinstein A, Fraenkel L. Racial disparities in treatment preferences for rheumatoid arthritis. Med Care. 2009;47(3):350-355. doi: 10.1097/MLR.0b013e31818af829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robert Wood Johnson Foundation : Discrimination in America: experiences and views of African Americans. Published October 2017. Accessed June 15, 2020. https://legacy.npr.org/assets/img/2017/10/23/discriminationpoll-african-americans.pdf
- 24.O’Connor MI, Lavernia CJ, Nelson CL. AAOS/ORS/ABJS musculoskeletal healthcare disparities research symposium: editorial comment: a call to arms—eliminating musculoskeletal healthcare disparities. Clin Orthop Relat Res. 2011;469(7):1805-1808. doi: 10.1007/s11999-011-1884-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Movement Is Life caucus. Movement Is Life: a catalyst for change: addressing musculoskeletal health disparities. 2011. Accessed 2019 Aug 4. https://www.movementislifecaucus.com/wp-content/uploads/Movement-Is-Life-A-Catalyst-For-Change-Proceedings-Report.pdf
- 26.National Institute of Arthritis Musculoskeletal and Skin Diseases . Strategic plan fiscal years 2020-2024. Turning discovery into health. Accessed November 29, 2020. https://www.niams.nih.gov/sites/default/files/pdf/NIAMS-StrategicPlan-2020-2024-v1.pdf
- 27.US Department of Health and Human Services . HHS action plan to reduce racial and ethnic disparities: a nation free of disparities in health and health care. Published April 2011. Accessed June 15, 2020. https://www.minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf
- 28.Wyatt R, Laderman M, Botwinick L, Mate K, Whittington J. Achieving health equity: a guide for health care organizations—IHI white paper. Institute for Healthcare Improvement; 2016.
- 29.Agency for Healthcare Research and Quality. HCUP National Inpatient Sample . NIS overview. Accessed May 1, 2020. https://www.hcup-us.ahrq.gov/nisoverview.jsp
- 30.HCUP Clinical Classifications Software for ICD-10-PCS . Healthcare Cost and Utilization Project (HCUP). 2017. Agency for Healthcare Research and Quality. Accessed June 10, 2020. https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp
- 31.US Census Bureau . Population estimates. Accessed June 15, 2020. https://data.census.gov/cedsci/table?q=United%20States
- 32.Berchick ER, Hood E, Barnett JC. Health insurance coverage in the United States: 2017. Published September 12, 2018. P60-264. Accessed June 15, 2020. https://www.census.gov/library/publications/2018/demo/p60-264.html
- 33.National Center for Health Statistics . Healthy people 2010 final review. Accessed June 15, 2020. https://www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review.pdf
- 34.US Department of Health and Human Services . ASPE report. HHS Action Plan to Reduce Racial and Ethnic Health Disparities Implementation Progress Report. Washington, DC: Office of the Assistant Secretary for Planning and Evaluation. Published November 1, 2015. Accessed June 15, 2020. https://aspe.hhs.gov/basic-report/hhs-action-plan-reduce-racial-and-ethnic-health-disparities-implementation-progress-report-2011-2014
- 35.Allen H, Sommers BD. Medicaid expansion and health: assessing the evidence after 5 years. JAMA. 2019;322(13):1253-1254. doi: 10.1001/jama.2019.12345 [DOI] [PubMed] [Google Scholar]
- 36.Amen TB, Varady NH, Rajaee S, Chen AF. Persistent racial disparities in utilization rates and perioperative metrics in total joint arthroplasty in the US: a comprehensive analysis of trends from 2006 to 2015. J Bone Joint Surg Am. 2020;102(9):811-820. doi: 10.2106/JBJS.19.01194 [DOI] [PubMed] [Google Scholar]
- 37.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34(1):172-180. [PubMed] [Google Scholar]
- 38.Vaughn IA, Terry EL, Bartley EJ, Schaefer N, Fillingim RB. Racial-ethnic differences in osteoarthritis pain and disability: a meta-analysis. J Pain. 2019;20(6):629-644. doi: 10.1016/j.jpain.2018.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hsiang WR, Lukasiewicz A, Gentry M, et al. Medicaid patients have greater difficulty scheduling health care appointments compared with private insurance patients: a meta-analysis. Inquiry. 2019;56:46958019838118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.FitzGerald JD, Soohoo NF, Losina E, Katz JN. Potential impact on patient residence to hospital travel distance and access to care under a policy of preferential referral to high-volume knee replacement hospitals. Arthritis Care Res (Hoboken). 2012;64(6):890-897. doi: 10.1002/acr.21611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khera R, Angraal S, Couch T, et al. Adherence to methodological standards in research using the National Inpatient sample. JAMA. 2017;318(20):2011-2018. doi: 10.1001/jama.2017.17653 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Gender-Adjusted and Population-Adjusted National Incidence of Surgical Procedures by Race in the United States from 2012 to 2017
eTable 2. Demographic Data and Characteristics of the Study Population


