Abstract
Background
The coronavirus disease (COVID-19) pandemic affects medical care worldwide, including patients with inflammatory bowel disease (IBD). Thus, we aimed to assess its impact on health care provision, fear of infection, adherence to medical treatment, and compliance with preventative instructions in children and adolescents with IBD.
Methods
A cross-sectional telephonic survey using a Likert scale-based questionnaire was conducted among all pediatric patients with IBD from a single tertiary medical center.
Results
A total of 244 pediatric patients with IBD were included in the study, reporting a high rate of fear of severe COVID-19 infection due to IBD or IBD medications (198, 81.1%). Most of the patients obeyed the Ministry of Health instructions (228, 93.4%), while almost 50% took additional protective measures including avoidance of school and complete lockdown. Concerns regarding the attendance of regular clinics (116, 47.5%) and emergency room in case of IBD exacerbation (178, 73%) were frequently reported. Only 7 patients (2.9%) changed or discontinued their IBD treatment due to COVID-19.
Conclusion
We noted several distinct features of the COVID-19 pandemic effect on pediatric patients with IBD including a high rate of fear of severe COVID-19 infection, fear of attending necessary medical facilities, and high rate of avoidance of social activities.
Impact
Pediatric patients with IBD have a high rate of fear of severe COVID-19 infection, fear of attending necessary medical facilities, and a high rate of avoidance of social activities.
Medication adherence rate in pediatric patients with IBD during the pandemic is similar to the adherence rate among adults with IBD.
Almost 50% of pediatric patients with IBD took additional protective measures including avoidance of school and voluntary lockdown during the COVID-19 pandemic.
Introduction
The novel coronavirus disease (COVID-19) is rapidly spreading, striking millions of people worldwide. The disease, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was announced as a global pandemic by the World Health Organization (WHO) on March 2020, following an outbreak, which initiated in China on December 2019.1
In order to control the virus transmission, the Israeli authorities implemented wide-scale social distancing measures including schools shut-down, traffic and travel restrictions, discontinuation of nonessential work and commerce, and a complete national curfew during national holidays.2 The further gradual easing of these restrictions was followed including the reopening of kindergartens and schools on May 17th.
Medical care provision was changed during the COVID-19 pandemic, using more telemedicine-based practice as guided by the Center of Disease Control and Prevention (CDC).3 These changes affected all patients with chronic diseases, including patients with inflammatory bowel disease (IBD), who experienced changes in standard management, with less frequent outpatient visits.
Patients with IBD were not shown to be more susceptible to severe COVID-19 unless treated with high-dose corticosteroids4 and the pediatric IBD Porto Group of the European Society of Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) recommended to continue medical treatments including biologic agents in pediatric patients with IBD.5 Accordingly, treating physicians of patients with pediatric IBD were instructed by the Israeli Society of Paediatric Gastroenterology, Hepatology, and Nutrition (ISPGHAN) to adopt a non-interruption strategy of IBD medical treatment and to recommend attendance of kindergartens and schools once approved for the general population by the Israeli Ministry of Health (MOH).
We aimed to assess the effect of the COVID-19 pandemic on changes in health care provision, fear of infection, a continuation of medical therapies, and adherence to MOH instructions in pediatric patients with IBD.
Methods
A cross-sectional study based on a structured telephone interview was conducted among all pediatric IBD patients treated in the Institute of Gastroenterology, Nutrition and Liver Diseases in Schneider Children’s Medical Center of Israel. Inclusion criteria were: patients between the ages of 0–18 years with an established diagnosis of IBD. Enrollment occurred between May 31st and July 9th, 2020.
Data collection included demographic data, diagnosis, and current treatment. The survey questionnaire was designed especially for this study and included 13 questions on the behavior and treatment adherence of the patients: 8 questions with a 5-point Likert-scale score, four closed-ended questions and one open-ended question regarding the impact of the COVID-19 pandemic. The survey was answered exclusively by one of the patients’ parents in children younger than 10 years, while children older than 10 years old could answer the survey with their parents.
Continuous variables are presented as mean ± standard deviation for normally distributed variables and as median with interquartile range (IQR) for abnormally distributed variables. Categorical variables are presented as frequency and percentage.
Categorical variables were compared using the chi-square test. p-values < 0.05 were considered statistically significant.
Ethical considerations
The study protocol was approved by the local Institutional Review Board. Parents of all subjects gave informed consent to participate in the survey.
Results
Out of a total of 253 pediatric patients with IBD, eligible according to the inclusion criteria, 9 patients refused to take part in the survey leaving a total of 244 patients who participated in the study. The cohort characteristics are depicted in Table 1. The study population included 117 (48%) females with a median age of 15.3 (IQR 12.6–17.1) years. Crohn’s disease (CD) was diagnosed among 170 (69.7%) patients, Ulcerative colitis (UC) among 67 (27.5%) patients and 7 (2.8%) patients had IBD-unclassified. Median disease duration was 3.5 (IQR = 1.5–5.5) years. The survey questions and results are presented in Table 2.
Table 1.
Cohort characteristics.
| Sex, female (n, %) | 117 (48%) |
| Age, years (median, IQR) | 15.3 (12.6–17.1) |
| Disease duration, years (median, IQR) | 3.5 (1.5–5.5) |
| Diagnosis (n, %) | |
| CD | 170 (70%) |
| UC | 67 (27%) |
| IBD-U | 7 (3%) |
| Treatment (n, %) | |
| 5-ASA monotherapy | 52 (21.3%) |
| 5-ASA with steroids | 4 (1.6%) |
| Steroids | 2 (0.8%) |
| Nutritional treatment | 6 (2.5%) |
| Thiopurines monotherapy | 14 (5.7%) |
| MTX monotherapy | 6 (2.5%) |
| Infliximab | 35 (14.3%) |
| Adalimumab | 75 (30.7%) |
| Vedolizumab | 5 (2.1%) |
| Ustekinumab | 14 (5.7%) |
| Biologics with immunomodulator | 14 (5.7%) |
| Other | 5 (2.1%) |
| No treatment | 12 (4.9%) |
CD Crohn’s disease, UC ulcerative colitis, IBD-U IBD-unclassified, IQR interquartile range, 5-ASA 5-aminosalicylic acid, MTX Methotrexate.
Table 2.
Survey results summary.
| Significant worsening | Worsening | No change | Improvement | Significant Improvement | |
| 1 | 2 | 3 | 4 | 5 | |
| Was there a change in healthcare provision due to COVID-19 pandemic? | 7 (2.9%) | 36 (14.8%) | 169 (69.3%) | 31 (12.7%) | 1 (0.4%) |
| Was there a change in your gastroenterologist availability due to COVID-19 pandemic? | 2 (0.8%) | 21 (8.6%) | 181 (74.2%) | 36 (14.8%) | 4 (1.6%) |
| To a very significant extent | To a significant extent | To a medium extent | To a minor extent | Not at all | |
| 1 | 2 | 3 | 4 | 5 | |
| Are you afraid of a severe COVID-19 infection due to your illness or your IBD medications? | 57 (23.4%) | 53 (21.7%) | 46 (18.9%) | 42 (17.2%) | 46 (18.9%) |
| Do you feel a need for emotional support due to COVID-19 pandemic? | 8 (3.3%) | 20 (8.2%) | 33 (13.5%) | 34 (13.9%) | 149 (61.1%) |
| Do you obey the MOH restrictions and guidance? | 173 (70.9%) | 55 (22.5%) | 13 (5.3%) | 2 (0.8%) | 1 (0.4%) |
| Very Afraid | Afraid | Neutral | Not afraid | Not at all | |
| 1 | 2 | 3 | 4 | 5 | |
| Are you afraid to attend the gastroenterology Institute during the COVID-19 Pandemic? | 29 (11.9%) | 87 (35.7%) | 30 (12.3%) | 72 (29.5%) | 26 (10.7%) |
| Are you afraid to attend the ER in case of IBD exacerbation during the COVID-19 pandemic? | 84 (34.4%) | 94 (38.5%) | 13 (5.3%) | 43 (17.6%) | 10 (4.1%) |
| Not at all | Not enough | Sufficiently | Updated | Very updated | |
| 1 | 2 | 3 | 4 | 5 | |
| Do you feel informed about the effect of COVID-19 on patients with IBD? | 87 (35.7%) | 47 (19.3%) | 41 (16.8%) | 49 (20.1%) | 20 (8.2%) |
| Yes | No | ||||
| Have you taken protective measures, in addition to the measures recommended by the MOH? | 120 (49.2%) | 124 (50.8%) | |||
| Did you stop or change your treatment because of the COVID-19 pandemic? | 7 (2.9%) | 237 (97.1%) | |||
| Did you consider stopping or changing your treatment due to the COVID-19 pandemic? | 22 (9 %) | 222 (91%) | |||
| Have you refrained from going to the pharmacy in order to purchase your medications during the COVID-19 pandemic? | 28 (11.5%) | 215 (88.5%) | |||
IBD inflammatory bowel disease, MOH Ministry of Health, ER emergency room, COVID-19 coronavirus disease 2019.
Most patients (169, 69.3%) did not feel any difference in health services provision during the COVID-19 pandemic while 43 (17.6%) noted a deterioration, and 32 (13.1%) noted improvement. The majority of patients (181, 74.2%) reported that there was no change in their gastroenterologist availability whereas 40 (16.4%) patients reported an improvement in treating gastroenterologist availability during the COVID-19 pandemic.
Fear of severe COVID-19 infection due to IBD or IBD medications was reported by 198 (81.1%) patients, with 110 (45.1%) being very concerned about obtaining a severe COVID-19 infection.
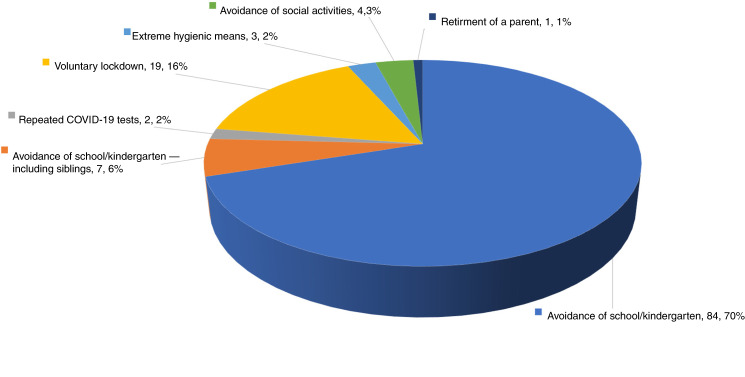
A total of 228 (93.4%) patients reported that they strictly obeyed the MOH guidance. Additional protective measures were taken by 120 (49.2%) patients. The most common measure was complete avoidance of school or kindergarten despite approval of attendance by the MOH, which was taken by 91 (37.3%) patients. Voluntary lockdown (including avoidance of school attendance, social contacts, and staying at home) was implemented by 19 (7.8%) patients and in 4 cases the lockdown included all family members. Other protective measures included: avoidance of school attendance by siblings (7, 2.9%), avoidance of social contacts (4, 1.6%), frequent disinfection measures (3, 1.2%), repeated COVID-19 PCR tests (2, 0.8%), and parental retiring from work (1, 0.4%) (Fig. 1).
Fig. 1. Additional protective measures among pediatric patients with IBD.
The proportions of patients taking additional protective measures appear in different colors.
The majority of patients (134, 54.9%) reported that they were not adequately informed about the potential effect of COVID-19 on patients with IBD.
A subgroup of patients (116, 47.5%) reported that they are not comfortable attending regular clinics during the COVID-19 outbreak, while 84 (34.4%) patients missed their clinic visit. A higher proportion of patients (178, 73%) declared a concern to attend the emergency room (ER) in case of IBD exacerbation. Avoidance of pharmacy visits was reported by 28 (11.5%) patients.
Discontinuation or change of treatment was considered by 22 (9%) patients whereas only 7 (2.9%) changed or discontinued their IBD medications due to COVID-19. Among patients who discontinued treatment 2 (0.8%) patients stopped anti-TNF therapy, 2 (0.8%) patients discontinued 5-ASA treatment, 2 patients (0.8%) stopped antibiotic therapy and 1 (0.4%) patient discontinued exclusive enteral nutrition treatment.
No significant statistical difference was found comparing patients with UC to patients with CD (data not shown), except for a higher proportion of patients with CD who reported being informed about COVID-19 effect on patients with IBD (70.2% vs. 34.4%, p = 0.03). No significant statistical difference was found comparing patients treated with biologic agents and patients treated with immunomodulators (with or without steroids).
Comparing patients in primary school and younger (n = 110) to those in high school (n = 134), younger patients tended to take more additional protective measures: 63 (57.3%) patients versus 57 (42.5%), respectively (p = 0.02). No other statistically significant differences were found between these groups (data not shown). No significant statistical difference was found comparing young adults at the age of 18 (n = 26), who answered the survey by themselves, to younger patients who filled the survey with a parent (n = 218), except for the difference in obeying MOH restrictions and fear of attending ER. Young adults stated less frequently that they strictly obeyed the MOH restrictions and guidance: 15 (57.7%) vs. 158 (72.5%), whereas a higher proportion of young adults stated that they obeyed the MOH restrictions and guidance only to a medium extent (4 (15.7%) vs. 9 (4.1%), p = 0.01). Young adults stated more frequently that they were not afraid at all to attend the ER during the COVID-19 pandemic (5 (19.2%) vs. 5 (2.3%), p < 0.01).
Discussion
In this study, we present the effect of the COVID-19 pandemic on more than 240 pediatric patients with IBD. Some degree of fear of severe SARS-CoV-2 infection was reported by the majority of patients corresponding to a high proportion of patients feeling uninformed about the possible effect of COVID-19 on IBD. In contrast, only 27% of adult patients with IBD in Germany reported that they are afraid that their medications will worsen COVID-19 infection.6 In a global survey among adult patients with IBD 30% believed that IBD diagnosis predisposes to an increased risk of COVID-19 infection while 64% of patients stated that immunosuppressive medications were associated with a higher risk of infection.7 The higher proportion of pediatric patients concerned about severe COVID-19 infection presented in our study may reflect parental anxiety or merely lack of information.
COVID-19 pandemic had a major impact on the management of patients with chronic diseases, shifting toward telemedicine.8 As our institute adopted this strategy, partially filling the gap in patients’ care, it was reasonable to find that most patients did not feel any change in health care provision. Despite the inability to perform a physical examination,9 telemedicine should be considered as a feasible option for patients with IBD as it can provide acceptable medical care and even has the potential to improve compliance and diminish the loss of follow-up. The COVID-19 pandemic may serve as a window of opportunity for integrating telemedicine in pediatric IBD practice.
Concerns about visiting outpatient clinics and ER during the outbreak were reported by most of the patients in our cohort. These findings are concerning, particularly in view of recent reports describing delayed medical treatment in common medical conditions during the COVID-19 pandemic.10 Efforts should be invested in conveying the message that the risk of delaying essential medical treatment outweighs the small risk of contracting the virus in a controlled environment. Reassurance and education measures should be employed to counteract fear from attending medical services such as ER, specifically in parents of young patients.
Additional protective measures were taken by almost 50% of patients in our cohort, mostly staying at home despite the re-opening of schools and kindergartens. Unnecessary isolation of children who are not at increased risk of the severe disease might have a detrimental impact on a child’s healthcare and wellbeing, emphasizing the need for patient’s guidance and reassurance by all treating disciplines. Those additional measures were more common among younger patients suggesting a significant psychological effect of COVID-19 on parents of young children. On the other hand, young adults with IBD should be encouraged to obey MOH restrictions and guidance, as a higher proportion of those patients stated that they did not fully comply with MOH regulations.
Only a minority of patients reported that they considered changing or discontinue IBD medications, and even a lower percentage actually did so. These findings are similar to recent reports in adults with IBD in whom about 4% of medication discontinuation was observed.6,7 Despite the high treatment adherence, these findings should not be ignored, as a cessation of treatment may have significant implications on disease control and potential complications.
Our study has several limitations including the lack of a control group, which did not allow a comparison with other pediatric populations, and interviewing only one parent, preventing a full perspective for each case.
In conclusion, we found several distinct features of the COVID-19 pandemic effect on pediatric patients with IBD including a high rate of fear of severe COVID-19 infection, fear of attending necessary medical facilities, and a high rate of avoidance of social activities. Our findings emphasize the importance of providing patients with the most updated information, not only regarding their chronic condition but also regarding the effect of global medical issues on their disease and treatment, particularly during a time of the global pandemic. Establishing open patient-physician communication may motivate patients to raise questions regarding their concerns, enabling physicians to address these issues prior to a decline in medical adherence. We believe that patients’ feelings and behaviors can be improved by reassurance and pro-active patient education.
Author contributions
L.D. and A.A. conceptualized and designed the study; I.O., M.M., and R.S. participated in designing the study. L.D., R.N., and D.B.O. participated in the acquisition of data and analysis and interpretation of data. A.A. and L.D. drafted the manuscript. All authors critically revised the manuscript and approved the final version.
Competing interests
The authors declare no competing interests.
Consent statement
The study protocol was approved by the local Institutional Review Board. Parents of all subjects gave informed consent to participate in the survey.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO. Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed 6 Jul 2020.
- 2.Leshem E, Afek A, Kreiss Y. Buying time with COVID-19 outbreak response, Israel. Emerg. Infect. Dis. 2020;26:2251–2253. doi: 10.3201/eid2609.201476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CDC. What to do if you are sick. https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when-sick.html. Accessed 6 Jul 2020.
- 4.Monteleone G, Ardizzone S. Are patients with inflammatory bowel disease at increased risk for Covid-19 infection? J. Crohns Colitis. 2020;14:1334–1336. doi: 10.1093/ecco-jcc/jjaa061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turner D, et al. Corona virus disease 2019 and paediatric inflammatory bowel diseases: global experience and provisional guidance (March 2020) from the Paediatric IBD Porto Group of European Society of Paediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2020;70:727–733. doi: 10.1097/MPG.0000000000002729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grunert, P. C., Reuken, P. A., Stallhofer, J., Teich, N., & Stallmach, A. Inflammatory Bowel Disease in the COVID-19 Pandemic: the Patients’ Perspective. Journal of Crohn’s and Colitis. jjaa126, 10.1093/ecco-jcc/jjaa126 (2020). [DOI] [PMC free article] [PubMed]
- 7.D’Amico F, Rahier J-F, Leone S, Peyrin-Biroulet L, Danese S. Views of patients with inflammatory bowel disease on the COVID-19 pandemic: a global survey. Lancet Gastroenterol. Hepatol. 2020;5:631–632. doi: 10.1016/S2468-1253(20)30151-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hong Z, et al. Telemedicine during the COVID-19 pandemic: experiences from Western China. J. Med. Internet Res. 2020;22:e19577. doi: 10.2196/19577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hjelm NM. Benefits and drawbacks of telemedicine. J. Telemed. Telecare. 2005;11:60–70. doi: 10.1258/1357633053499886. [DOI] [PubMed] [Google Scholar]
- 10.Snapiri O, et al. Delayed diagnosis of paediatric appendicitis during the COVID-19 pandemic. Acta Paediatr. 2020;109:1672–1676. doi: 10.1111/apa.15376. [DOI] [PMC free article] [PubMed] [Google Scholar]