Abstract
Background and purpose
Several studies have investigated multi leaf collimator (MLC) leaf design. We performed a systematic review and meta-analysis of those studies to compare the impact of MLC leaf width used for different radiotherapy techniques.
Materials and methods
We decided to focus on 2.5, 3.0 and 5.0 mm leaf width MLCs as it appeared to be the most contentious area from literature. We adopted Cochrane and PRISMA guidelines and computed the association between MLC leaf width and conformity index (CI) across the selected studies as pooled mean difference (PMD) with 95% confidence interval.
Results
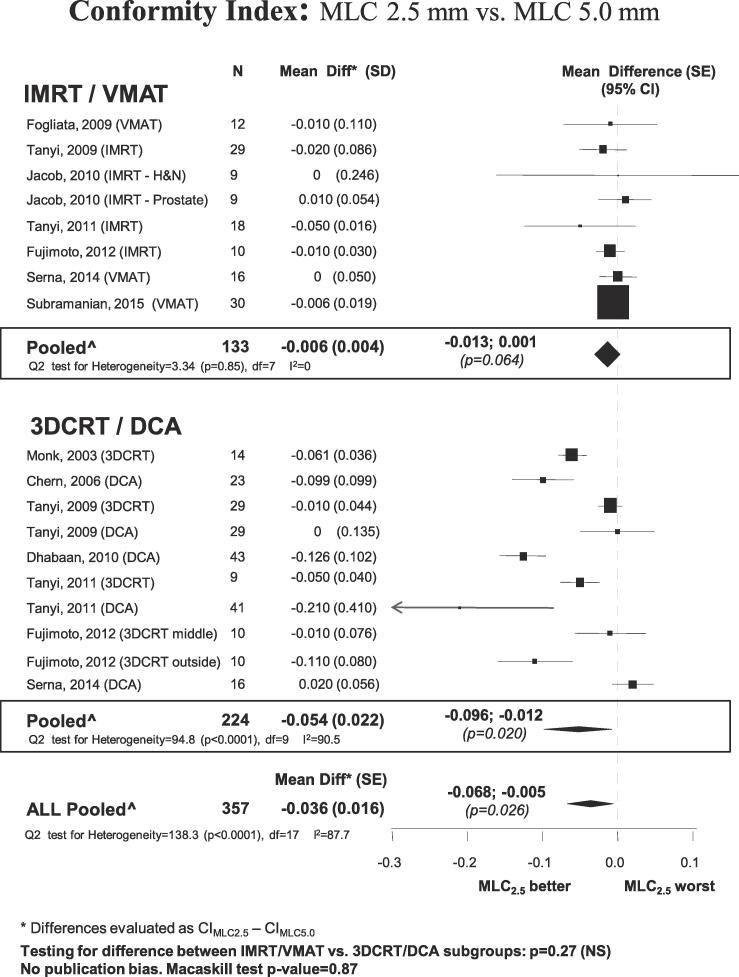
A total of 43 papers were selected from the literature search, of which ten compare MLC leaf width of 2.5 mm or 3.0 mm (MLC2.5 mm) versus 5.0 mm (MLC5 mm) in terms of CI. There was a slight, but significant, difference between MLC2.5 mm and MLC5 mm in favor of the former (mean difference −0.036; 95% confidence interval: −0.068 to −0.005). A subgroup analysis was performed by comparing techniques (intensity modulated radiation therapy vs conformal). In the intensity modulated radiation therapy (IMRT) subgroup, the difference between MLC2.5 mm and MLC5 mm appeared to be negligible (mean difference: −0.006; 95% confidence interval: −0.013 to 0.001) and not significantly different from zero. In the subgroup of studies which used conformal techniques, there was a significant difference between MLC2.5 mm and MLC5 mm (mean difference: −0.054; 95% confidence interval: −0.096 to −0.012).
Conclusions
Introduction of IMRT produced comparable target coverage (CI) between 2.5 or 5.0 mm leaf width MLCs.
Keywords: Multi leaf collimators, Treatment planning system, Intensity modulated radiation therapy, Systematic review, Meta-analysis
1. Introduction
The multi leaf collimator (MLC) is one of the most critical components for the delivery of radiation oncology treatments using a linear accelerator [1]. Since the clinical introduction of MLCs in the early 1990s, several treatment planning system (TPS) and theoretical studies were conducted in order to attempt to determine the optimal MLC leaf design, in terms of target coverage and organ sparing [2], [3], [4], [5], [6], [7]. These studies were based on TPS simulations and assessment of typical dose distribution parameters (such as conformity index, homogeneity index, dose volume histograms, tumor control probability, normal tissue complication probability, etc.).
There are many design characteristics in each MLC, such as leaf width, leaf tip design (single focus, double focus, not focused), tongue and groove presence, distance from the patient and leakage, to name a few. All of these characteristics may affect conformity to target and dose to surrounding structures. All papers found in a preliminary search focused on MLC leaf width as the main design parameter of interest, which suggests that authors of these papers consider this to be the biggest contributing factor to the ability to conform to the target and spare normal tissues [2], [3], [4], [5], [6], [7]. Therefore, “MLC leaf width” was used as a search keyword and the remaining part of this analysis focused on this characteristic.
Jacob et al. [2] concluded that three collimator leaf thicknesses studied (10, 5 and 2.5 mm) were equally suitable for conformal coverage of the target volume and sparing of organs at risk (OARs) when using intensity modulated radiation therapy (IMRT). Wang et al. [3] concluded that a 4 mm MLC improved prostate planning target volume (PTV) dose coverage over a conventional 10 mm MLC in the treatment of prostate cancer using 6 MV for IMRT. With similar findings to Wang et al., but in contradiction to Jacob et al., Fujomoto et al. [4] demonstrated that the dose conformity of the PTV improved and the dose to bladder and rectum decreased for 3D conformal radiation therapy (3DCRT) and IMRT of prostate cancer using a 2.5 mm MLC compared to a 5 mm MLC.
Jin et al. [5] performed a study on cranial lesions and concluded that, for the DCA technique, there were significant dosimetric differences between different MLCs in terms of conformity indices. However, for the intensity modulated radiosurgery (IMRS)/IMRT technique, there was no significant difference of conformity index and target coverage between the 3 and 5 mm MLCs. Serna et al. [6] performed a study on brain lesions and showed a variation in conformity index of below 0.5% for volumetric modulated arc therapy (VMAT) and 3% for 3D-DCA, independent of the PTV volume. Therefore, for the VMAT technique, there was no significant improvement in conformation through the use of an MLC leaf width of 2.5 mm for small volumes. In contradiction with some of the above mentioned studies, Nill et al. [7] concluded that an improved PTV coverage and conformity was obtained for a 2.75 mm add-on MLC compared to the internal 4 mm MLC when using IMRT.
For the above mentioned studies, we noticed that there was no uniform agreement on the benefit of smaller leaf width. The difference seemed to be more evident for smaller lesions but, in some situations, it was reduced by the utilization of VMAT or IMRT techniques [6]. This lack of agreement, and the possibility that inverse planning techniques could have reduced the gap, triggered this study.
Since a good number of articles exist on the matter, we believed that a critical/systematic review had the potential to provide a good level of scientific evidence. The purpose of this analysis was to collect and group the existing literature concerning MLC leaf width and to determine if and what conclusions could be deduced. The focus was to determine if MLCs with different leaf width performed better in terms of target coverage and, if so, under what conditions. In general, smaller targets were considered the most challenging [2], [3], [4], [5], [6], [7] and so we decided to focus on leaf widths of 5 mm or less.
2. Material and methods
In this review, the overall structure of the Cochrane analysis [8] or, in general, common rules identified as important in a systematic review according to PRISMA [9], [10] guidelines, were adopted, as follows.
Search words were determined in advance. Searches were performed using PubMed (https://www.ncbi.nlm.nih.gov/pubmed), with search keywords “MLC leaf width”. Further papers were found using Google Scholar (https://scholar.google.com). In addition, all citations in the originally found papers were checked to identify the existence of any new papers. From the group formed by the above described search, all relevant publications relating to the subject matter (MLC comparison) were selected. Published peer-reviewed papers were chosen based on the simple criterion of being a comparison study between different MLC types in terms of conformity index. The data included in the selected publications were collected and the necessary statistical data (such as averages and standard deviations) were either used directly or calculated. If they could not be calculated, then the paper was not included in the review. Posters and presentations were not considered because they were not subjected to a peer review approach and, therefore, they have an uncertain level of evidence, in agreement with PRISMA guidelines. The last search was performed on 31st December 2015. No early cut-off date was determined. No subsequent papers relating to small leaf width comparison was found until end of February 2017. Two people, working independently, were involved in the selection process. Theoretical studies were included only if they produced data that could be used for the purposes of this study, such as standard deviations. Phantom studies were excluded because they were not thought to be representative of real clinical conditions.
It was decided to treat MLC leaf width of 2.5 mm or 3.0 mm as one subgroup, MLC2.5 mm, and MLC of leaf width 5.0 mm as the other subgroup, MLC5 mm. This was partly to increase the number of qualifying papers, but it was also judged that any difference between 2.5 mm and 3.0 mm would be much smaller than between the two subgroups MLC2.5 mm and MLC5 mm. In order to perform the analysis, it was necessary to reformulate the results from each of the papers into a common format. The statistical values chosen to estimate the pooled MLC effect were the mean difference (Diff) and its standard error [SE(Diff)]. To calculate them we used the method described in the Supplementary data.
The association between MLCs and conformity index reduction across the selected studies was then computed as pooled mean difference (PMD) with 95% confidence interval. The PMD was considered statistically significant if the 95% confidence interval did not include zero. PMD was estimated by pooling the study-specific estimates using random effect models [11], fitted using statistical analysis system (SAS) (proc Mixed) with a maximum likelihood estimate. These models provided estimates adjusted for the potential correlation within studies, as well as the heterogeneity between studies.
The homogeneity of the effect across studies was assessed by using the large sample test based on Cochrane’s Q statistics, which are distributed approximately as χ2 statistics. A p-value <0.10 was used to indicate lack of homogeneity between effects. I2 statistics were also provided to quantify the percentage of total variation across studies that was attributable to heterogeneity rather than to chance [12]. The method of Macaskill et al. was used to assess publication bias [13]. This consists of a funnel-plot regression of the PMD on the sample size, weighted by the inverse of the variance.
A subgroup analysis was also performed to evaluate eventual differences between techniques. This was also triggered by the finding of Carosi et al. [14] and Serna et al. [6]. In particular, a comparison between MLC2.5 mm and MLC5 mm was performed in the subgroup of studies where IMRT or VMAT was used. Similarly, the same analysis was performed for the subgroup of studies that adopted 3DCRT or DCA. The hypothesis was that IMRT techniques reduce, or even annul, any differences between MLC2.5 mm and MLC5 mm, in terms of conformity index. In contrast, differences were expected in the subgroup of studies that adopted 3DCRT or DCA.
3. Results
From the literature search, 148 papers were found initially and 43 were selected according to the selection guidelines highlighted in the material and methods section (see Supplementary material for list of studies). Of these, ten papers compared MLCs with leaf widths of 2.5 mm or 3 mm versus 5 mm, in terms of conformity index, and were included in the final analysis (Table 1).
Table 1.
Details of Studies comparing small leaf width MLCs that comply with inclusion criteria.
| Author | Year | Conflict of interest/funding | Country | N of patients | Comparison | Formula CI calculation^ | Anatomical site | Technique | Statistics |
|---|---|---|---|---|---|---|---|---|---|
| Monk | 2003 | UK | 14 | 3 vs 5 mm | CI_B | Brain | 3DRCT | Individual patient data | |
| Chern | 2006 | USA | 23 | 3 vs 5 mm | NCI | Brain | DCA | Mean (SD) per group; t-test avail | |
| Fogliata | 2009 | Varian | Switzerland | 12 | 2.5 vs 5 mm | CI_P | Brain | VMAT | Mean (SD) per group; no t-test |
| Tanyi | 2009 | USA | 29 | 2.5 vs 5 mm | NCI | Lung | IMRT, 3DRCT, DCA | Mean (SD) per group; t-test avail | |
| Dhabaan | 2010 | USA | 43 | 2.5 vs 5 mm | CI_B | Brain | DCA | Individual patient data | |
| Jacob | 2011 | Germany | 9 | 2.5 vs 5 mm | PITV | H&N, Prostate | IMRT | Mean (95% CI) per group | |
| Tanyi | 2011 | Varian | USA | 68* | 2.5 vs 5 mm | NCI | Brain | IMRT, 3DRCT, DCA | Mean diff (SD) |
| Fujimoto | 2012 | Japan | 10 | 3 vs 5 mm | PITV | Prostate | IMRT, 3DRCT | Mean (SD) per group; no t-test | |
| Serna | 2014 | Spain | 16 | 2.5 vs 5 mm | CI_P | Brain | VMAT, DCA | Mean (SD) per group; no t-test | |
| Subramanian | 2015 | India | 30 | 2.5 vs 5 mm | PITV | Lung | VMAT | Mean (SD) per group; t-test avail |
CI_B: Brainscan; CI_P: Paddick; NCI: Nakamura; CI_B: RTOG guideline. ^Feuvret et al. (Int. J. Radiation Oncology Biol. Phys, 2006: 333–342) and Ohtakara et al. (Br J Radiol, 2012:e223-e228).
Lesions.
Three of the ten selected studies (Monk et al., Chern et al. and Fujimoto et al.) compared 3 mm leaf width versus 5.0 mm, while the others compared 2.5 mm leaf width versus 5.0 mm.
In total, 357 cases from those ten papers were included in the main analysis.
The conformity index of MLC2.5 mm for the whole group was slightly, but significantly, better compared to MLC5 mm. The pooled mean difference was −0.036 with a 95% confidence interval ranging between −0.068 and −0.005 (p = 0.026).
In the IMRT/VMAT subgroup, the difference between MLC2.5 mm and MLC5 mm appeared to be negligible (mean difference: −0.006; 95% confidence interval: −0.013 to 0.001) and not significantly different from zero (p = 0.064). In contrast, in the subgroup of studies that used conformal 3DCRT/DCA techniques, MLC2.5 mm results were significantly different to MLC5 mm (mean difference: −0.054; 95% confidence interval: −0.096 to −0.012; p = 0.02). This is shown graphically by a forest plot in Fig. 1.
Fig. 1.
Study analysis results.
Within the IMRT/VMAT subgroup, there was a substantial homogeneity between studies. In the 3DCRT/DCA subgroup, in contrast, the heterogeneity remained quite large. However, all studies but one (Serna et al.) showed greater conformity for MLC2.5 mm.
Table 1 shows the main study characteristics.
4. Discussion
A systematic review of TPS studies, relating to treatment quality using different MLC leaf widths, was performed. For the purposes of this analysis, we focused on a specific index (CI) but, in theory, the analysis could be extended to include other quality index parameters. In our analysis, we highlighted that the IMRT/VMAT subgroup showed no evidence of difference in target coverage (CI) between 2.5 mm and 5.0 mm MLCs, unlike the 3DCRT/DCA subgroup, in which leaf width affected the target coverage.
The results of this analysis could be explained by the improved ability of IMRT to achieve conformity of dose distribution to the target. This is because IMRT inherently positions the leaves to achieve a dosimetric criteria, which is also used to judge plan quality, thereby making the MLC leaf width aspect less evident. The findings could be further explained by the fact that IMRT implements an automatic algorithm and, therefore, is less dependent on operator ability and TPS type. This is in line with the findings of Carosi et al. [14] who performed a comparison between 4 mm and 10 mm MLCs and showed that, in 3DCRT, the use of the 4 mm mMLC gave a gain in target conformity and in OARs dose sparing, whereas in IMRT plans there was no advantage. Also Tanyi et al. [15] demonstrated the dosimetric merit of a 2.5 mm leaf width MLC system over a 5 mm leaf width system for stereotactic radiosurgery brain targets with IMRT but showed that conformity index difference between the MLC systems was smaller for IMRT than for 3DCRT and DCA. This was also in line with the studies from Jin et al. [5] and Serna et al. [6].
Since the subject matter was well defined, we believed that the search method described above was effective and very unlikely to present weak points that may occur during a systematic review. Leaf width is known for all commercially available MLCs and the process of determining whether an article should be included or not was very simple and straightforward. Although the studies were not ‘randomized’ per se, all authors performed a comparison using the same patient model, creating plans using the same TPS but with different beam limiting devices (MLCs) and then comparing the results obtained from both plans.
An important aspect to consider was the possible heterogeneity of comparison criteria in the calculation. For example, there was not an agreed formula for conformity index (CI) and authors may have used different methods. However, all collected articles provided a comparison between two systems and, for that comparison, the same method was used. This study compared relative differences, not absolute values. Therefore, for the purposes of this study, the heterogeneity of conformity index formula was not considered to be of particular importance. A detailed summary of the differences between CI definitions has been described (Feuvret et al. [16] and Ohtakara et al. [17]). The selected papers used four different formulae to calculate CI: Brainscan (CI_B) [17], Paddick (CI_P) [18], Nakamura (NCI) [19] and PITV according to Radiation Therapy Oncology Group (RTOG) classifications (PITV) [20].
The difference observed between MLC2.5 mm and MLC5 mm in the 3DCRT/DCA subgroup and the absence of any difference in the IMRT/VMAT group could be explained by the basic difference between the two methods. IMRT/VMAT algorithms optimize the position of the leaves to achieve good conformality i.e. the leaf positions are set such that a dosimetric objective is met, whereas 3DCRT/DCA sets the leaf positions according to geometric algorithms. Therefore, when evaluated against dosimetric criteria (in this case CI), it was reasonable to expect the IMRT/VMAT algorithm to be superior regardless of leaf width or other factors, as also found by others [14], [6].
It was interesting to observe the difference in heterogeneity between the two groups (3DCRT/DCA and IMRT/VMAT). This could be explained by the following reasons:
IMRT/VMAT is designed to achieve, in an automatic manner, the best conformity given the delivery system design, making it less subject to the experience of the operator. 3DCRT/DCA requires a more manual input of parameters (e.g. margins, leaf fit algorithms, such as “touch edge” or “overlap edge”) that can vary from operator to operator or from TPS to TPS. Therefore, a less experienced operator, when performing 3DCRT/DCA planning, may select manual parameters that are not optimal in terms of conformity. Furthermore, IMRT/VMAT is able to achieve higher modulation (i.e. changes in delivery parameters, such as number of beams, leaf positions, beam weights, etc., to leverage all the degrees of freedom of the system) and therefore inherently allows better conformality for all MLC types than 3DCRT/DCA.
We intuitively expected the finer MLC leaf width to produce plans with superior dose conformity and OAR sparing, due to the ability of the MLC to conform more smoothly to the target. This expectation seemed to have a sound basis in history, and probably personal experience, since a difference clearly existed when using geometric techniques, which pre-date the introduction of inverse planning techniques. However, it seemed that the introduction of inverse planning techniques significantly reduced the differential between different MLC types and made that less operator dependent.
Other factors that may have contributed to these differences include the leaf modelling or dose grid used during the calculation and inverse planning phase. Similarly, the plans may not have been fully optimized to take full advantage of the smaller leaf width. However, it was assumed that, since the purpose of each one of the collected studies was to determine differences between MLC designs, the parameters and methods must have been carefully evaluated and selected by the authors.
The effect of more complex beam arrangements was not studied as none of the selected papers included this as a factor. This study only covered the conformity index (i.e. the behavior of the high dose region) as there was not enough data for other indicators to reach statistical significance. PRISMA and Cochrane analysis methods could also be applied to treatment planning studies, allowing proper integration of results from different hospitals, different disease sites and planning systems.
The inclusion/exclusion criteria were very simple and straightforward. Very rarely was it necessary to read the body of the article to determine if it was related to an MLC comparison study. One of the small leaf width comparison studies (Jin et al. [5]) was excluded because it provided results in terms of the CI mean ratio (instead of mean difference) and there was no way to recover the original CI mean and pertinent SD. Another study (Hong et al. [21]) was excluded because the data did not derive from humans. With one exception, all articles were in English. Further communication with the authors of the selected studies was not deemed necessary. Publication bias was not present (Macaskill test p-value 0.87). Only two out of ten studies (Tanyi at al. [15] and Fogliata at al. [22]) have disclosed funding. This was not deemed to create a significant bias, although the Tanyi at al. [15] study showed the biggest benefit of the 2.5 mm MLC in the IMRT subgroup.
In conclusion, the performed study indicated that the introduction of IMRT produced comparable target coverage (CI) between 2.5 or 5.0 mm leaf width MLCs.
Conflict of interest statement
Marco Luzzara and Kevin Brown are Elekta AB employees. They have played key roles in the design and dosimetry of several multi leaf collimators including both 2.5 mm and 5 mm leaves. They also hold related patents.
Luigi Santoro has a scientific collaboration with Elekta AB.
Acknowledgments
None.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.phro.2018.03.005.
Contributor Information
Marco Luzzara, Email: marco.luzzara@elekta.com.
Luigi Santoro, Email: luigi.santoro@ieo.it.
Kevin Brown, Email: Kevin.Brown@elekta.com.
Appendix A. Supplementary data
References
- 1.Webb S. Contemporary IMRT: Developing Physics and Clinical Implementation. Series in Med Phys and Biom Eng, Iop.org 2005 ISBN: 0 7503 1004 9 2004.
- 2.Jacob V., Bayer W., Astner S.T., Busch R., Kneschaurek P. A planning comparison of dynamic IMRT for different collimator leaf thicknesses with helical tomotherapy and RapidArc for prostate and head and neck tumors. Strahlenther Onkol. 2010;186:502–510. doi: 10.1007/s00066-010-2124-3. [DOI] [PubMed] [Google Scholar]
- 3.Wang S-C, Wang X, Yin-Bo H, Zhao Y-Q, Tao L, Ping A, et al. A dosimetric comparison of the fixed-beam IMRT plans using different leaf width of multileaf collimators for the intermediate risk prostate cancer. Rad Phys Chem n.d. doi:10.1016/j.radphyschem.2016.07.008.
- 4.Fujimoto S., Ono K., Furukawa K., Kudo T., Akagi Y., Koyama T. Influence of high-definition multileaf collimator for three-dimensional conformal radiotherapy and intensity-modulated radiotherapy of prostate cancer. Nihon Hoshasen Gijutsu Gakkai Zasshi. 2012;68:825–834. doi: 10.6009/jjrt.2012_jsrt_68.7.825. [DOI] [PubMed] [Google Scholar]
- 5.Jin J.-Y., Yin F.-F., Ryu S., Ajlouni M., Kim J.H. Dosimetric study using different leaf-width MLCs for treatment planning of dynamic conformal arcs and intensity-modulated radiosurgery. Med Phys. 2005;32:405–411. doi: 10.1118/1.1842911. [DOI] [PubMed] [Google Scholar]
- 6.Serna A., Puchades V., Mata F., Ramos D., Alcaraz M. Influence of multi-leaf collimator leaf width in radiosurgery via volumetric modulated arc therapy and 3D dynamic conformal arc therapy. Phys Med. 2015 doi: 10.1016/j.ejmp.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Nill S., Tucking T., Munter M.W., Oelfke U. Intensity modulated radiation therapy with multileaf collimators of different leaf widths: a comparison of achievable dose distributions. Radiother Oncol. 2005;75:106–111. doi: 10.1016/j.radonc.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 8.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. The Cochrane Coll, 2011 Available from www.cochrane-Handbook.org 2011.
- 9.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gotzsche P.C., Ioannidis J.P.A. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(264–9):W64. doi: 10.1371/journal.pmed1000097. [DOI] [PubMed] [Google Scholar]
- 11.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 12.Higgins J.P.T., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 13.Macaskill P., Walter S.D., Irwig L. A comparison of methods to detect publication bias in meta-analysis. Stat Med. 2001;20:641–654. doi: 10.1002/sim.698. [DOI] [PubMed] [Google Scholar]
- 14.Carosi A., Ingrosso G., Ponti E., Tolu B., Murgia A., di Cristino D. Dosimetric effect of Elekta Beam Modulator micromultileaf in three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for prostate cancer. Med Dosim. 2014;39:180–184. doi: 10.1016/j.meddos.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Tanyi J.A., Kato C.M., Chen Y., Chen Z., Fuss M. Impact of the high-definition multileaf collimator on linear accelerator-based intracranial stereotactic radiosurgery. Br J Radiol. 2011;84:629–638. doi: 10.1259/bjr/19726857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feuvret L., Noel G., Mazeron J.-J., Bey P. Conformity index: a review. Int J Radiat Oncol Biol Phys. 2006;64:333–342. doi: 10.1016/j.ijrobp.2005.09.028. [DOI] [PubMed] [Google Scholar]
- 17.Ohtakara K., Hayashi S., Hoshi H. The relation between various conformity indices and the influence of the target coverage difference in prescription isodose surface on these values in intracranial stereotactic radiosurgery. Br J Radiol. 2012;85:e223–e228. doi: 10.1259/bjr/36606138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paddick I. A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. J Neurosurg. 2000;93(Suppl. 3):219–222. doi: 10.3171/jns.2000.93.supplement. [DOI] [PubMed] [Google Scholar]
- 19.Nakamura J.L., Verhey L.J., Smith V., Petti P.L., Lamborn K.R., Larson D.A. Dose conformity of gamma knife radiosurgery and risk factors for complications. Int J Radiat Oncol Biol Phys. 2001;51:1313–1319. doi: 10.1016/s0360-3016(01)01757-6. [DOI] [PubMed] [Google Scholar]
- 20.Shaw E., Kline R., Gillin M., Souhami L., Hirschfeld A., Dinapoli R. Radiation Therapy Oncology Group: radiosurgery quality assurance guidelines. Int J Radiat Oncol Biol Phys. 1993;27:1231–1239. doi: 10.1016/0360-3016(93)90548-a. [DOI] [PubMed] [Google Scholar]
- 21.Hong C.-S., Ju S.G., Kim M., Kim J.-I., Kim J.M., Suh T.-S. Dosimetric effects of multileaf collimator leaf width on intensity-modulated radiotherapy for head and neck cancer. Med Phys. 2014;41:021712. doi: 10.1118/1.4860155. [DOI] [PubMed] [Google Scholar]
- 22.Fogliata A., Clivio A., Nicolini G., Vanetti E., Cozzi L. Intensity modulation with photons for benign intracranial tumours: a planning comparison of volumetric single arc, helical arc and fixed gantry techniques. Radiother Oncol. 2008;89:254–262. doi: 10.1016/j.radonc.2008.07.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.