Learning objectives.
By reading this article, you should be able to:
-
•
Identify that the placebo response is ubiquitous in interactions between patients and clinicians and that it can be cued positively to enhance the therapeutic effect of treatments.
-
•
Describe the psychological or neurobiological mechanisms, and appreciate that individual responses vary widely, can be significant in magnitude, and can be negative (nocebo).
-
•
Discuss the research agenda, including scrutiny of the placebo effect in research, more recent research on placebo mechanisms, and translation of the effect in clinical practice.
-
•
Explain that as clinicians, we are part of the patient's context—what we say and how we behave interact with an individual's learned history to influence the outcomes of treatment.
Key points.
-
•
It is unethical to knowingly deceive a patient into believing they are receiving an active treatment whilst offering them an inactive one.
-
•
A placebo effect is likely ubiquitous in healthcare: it cannot be avoided and should be allowed for.
-
•
A number of factors relevant to both research and clinical practice (e.g. natural history, regression to the mean, and sources of bias) may be mistaken for an individual's response to the specifically active component of treatment, or placebo response to treatment.
-
•
The mechanisms underpinning placebo can be used positively to enhance the overall treatment effect in any given context.
-
•
The mechanisms are complex and include neurobiological and distinctly psychological mechanisms for which there may be a unifying psychobiological theory.
A placebo is an inert treatment that is not designed to have any therapeutic value, such as inert tablets or injections, sham surgery, and other procedures with no therapeutic value. Placebos are widely used in clinical research to provide control arms when evaluating the effects of drugs and other interventions. In a clinical context, knowingly administering an inert treatment without the patient's explicit consent would be unethical, although the practice was widespread in the history of medicine until the first half of the 20th century as an accepted therapeutic strategy. Factors relevant to placebo mechanisms can also result in therapeutic advantage when active treatments are delivered non-deceptively. The focus of this article is the usefulness of such responses in practice, which has been most widely researched in clinical and experimental pain settings.
A very early allusion to contextual (not explicitly therapeutic) factors important to treatment success was from ancient Chinese medicine—The Yellow Emperor's Inner Classic (Huang Di Nei Jing) from the first century BCE: ‘If a patient does not consent to therapy [acupuncture] with positive engagement, the physician should not proceed as the therapy will not succeed’.1 This statement suggests an appreciation that contextual factors are relevant to treatment success, which increased in Western literature through the 19th and 20th centuries. In Henry Beecher's milestone 1955 paper, ‘The powerful placebo’, the placebo groups of 15 placebo-controlled trials were examined, and it was concluded that this effect—averaging approximately 35% of patients—was attributable to placebo. Although methodology and conclusion have since been questioned, the ubiquity and significance of placebo effects in trials, and clinical practice, are now established.2
Definitions
The terms placebo effect and placebo response are often used interchangeably. However, it is important to differentiate the two.
Placebo response is the response observed in the placebo arm of a research trial. In a clinical setting, it is a positive response noted in or described by a patient, which is not attributable to the active treatment itself.
In contrast, placebo effect is the difference in the presence or severity of symptoms between the placebo group and an untreated control arm, and therefore controls for other factors, such as natural history of the condition.3
The nocebo effect has also been described, and is the negative counterpart of the placebo effect. Examples include adverse effects or worsening of symptoms not directly caused by a treatment, when compared with an untreated control arm. It has been studied to a lesser extent than the placebo effect, largely because of ethical considerations.
Other phenomena misattributed to a placebo effect in research and clinical practice
In research, the response magnitude in the placebo group is in fact an observed difference involving true placebo effect and a number of quite distinct and important factors, which, if not recognised, overestimate the magnitude of the placebo effect. Similarly, clinical responses to treatment may be related to a number of these same factors. Whilst there is a ready appreciation of the need to control for these effects in research, it would equally serve the clinician to be aware that such factors may be influencing apparent treatment responses.
Regression to the mean
Regression to the mean describes a phenomenon whereby if a fluctuating variable is extreme when first measured (e.g. pain severity), then it is likely to be closer to the mean on repeated measurement. When patients present to healthcare professionals, receive treatment, or are recruited into trials, symptoms are generally likely to be more severe. Natural random fluctuation in symptoms may be wrongly ascribed to placebo or to treatment.
Natural history
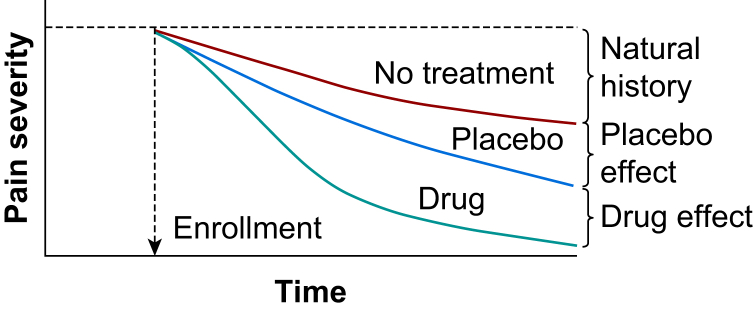
The natural history of some symptoms is such that they are likely to resolve over time. If the natural history of the symptoms matches that of the study period, then it may appear that the symptoms of patients in the placebo group have improved as a result of placebo or treatment (Fig. 1).
Fig 1.
(Used with permission from fig. 27.1, p. 363, Wall and Melzack's Textbook of Pain, 6th Edn., 2013, ISBN: 9780702040597). At the time of enrolment (the clinical corollary of which is the new patient assessment), pain severity is at its highest. Over time, even with no treatment, pain levels may reduce (natural history and perhaps regression to the mean). With treatment (drug or any treatment), the pain reduces to a greater degree, in part because of the ‘intrinsic’ treatment effect, and partly from the placebo effect.
Additional treatments
Patients may receive additional treatments that are difficult to control for. This is especially the case when treatments are integrated, for example in an interdisciplinary pain clinic setting.
Response bias: patients
Social factors may influence the reporting of outcomes from trials. Patients who believe they are receiving treatment may over-report improvements in symptoms. There may be a clinical corollary: patients may also over-report symptoms at initial consultation to expedite treatment or gain access to what is perceived to be a more effective treatment.
Reporting bias
Reporting bias from clinicians or investigators may lead to bias in any study. Blinding aims to limit this bias. However, double blinding is not possible in some study designs, and in a clinical paradigm, clinician belief/expectation affects a patient's response.
Hawthorne effect
The Hawthorne effect describes the process by which the mere fact of observing subjects within a trial may change the behaviour of the subjects.
Mechanisms underpinning placebo effects
Psychological and neurobiological mechanisms influencing the placebo effect are complex, and it appears that there is not one singular pathway, but many different effects and mechanisms.
Psychological mechanisms
There have been two main schools of thought in relation to the psychological mechanisms of the placebo effect. These are conditioning and expectancy.
Conditioning
The conditioning hypothesis suggests that placebo responses result from automatic, unconscious pairing of stimuli via Pavlovian conditioning. An individual may experience a reduction in pain (unconditioned response) after an analgesic intervention, such as an injection (neutral stimulus) containing an analgesic agent (unconditioned stimulus). The pairing of the injection and a reduction in pain may lead the injection (conditioned stimulus) to result into a reduction in pain (conditioned response) without the presence of the original analgesic agent.
Expectancy
Expectancy theories of placebo consider the conscious expectation of a situation to impact the individual's responses within that context. Expectations are formed from prior experience; for example, previous positive experiences of visiting a doctor could lead to an expectation of further positive experiences. Social learning, such as responses to authority, others' experiences of healthcare, or how likely we are to experience positive outcomes, could all influence placebo responses according to expectancy theory.
Synthesis
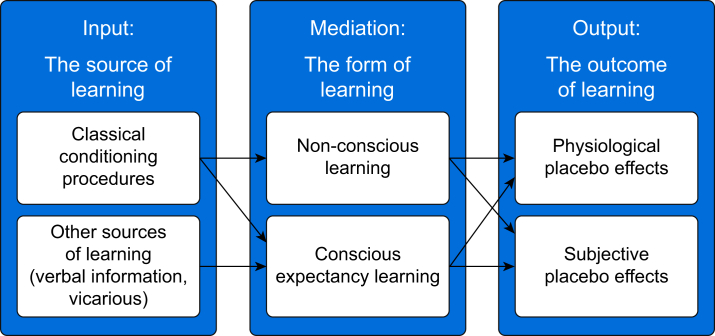
Previous research has suggested two distinct schools of thought regarding psychological mechanisms underpinning placebo effects. More recent debate has questioned whether they are mutually distinct mechanisms. Stewart-Williams and Podd proposed a model in which conditioning and expectancy theories complement and interact to produce an effect (Fig. 2).4 Within this combined model, individual differences can influence a general process upon which the response is underpinned (i.e. how our conscious experience can influence our unconscious physiological responses). Viewing the placebo response as a product of prior learning, expectation, and unconscious physiological conditioning helps clinicians and researchers to consider the placebo effect more in line with the prevailing models of chronic pain, which have grown from Engel's 1977 biopsychosocial model. A synthesis of conditioning and expectation theories also complements work conducted on pain matrix conceptualisations of pain perception by Tiemann and colleagues, which have been shown to rely on top-down and bottom-up processing to modulate pain perception, and Miller and Kaptchuk's model of contextual healing.5,6
Fig 2.
Stewart-Williams and Podd's (2004) combined model of placebo response.4
The placebo response is a function of the psychosocial interaction of the patient with the context surrounding a treatment. Indeed, such is the assumed impact of context upon placebo responses that Miller and Kaptchuk argued for the term ‘contextual healing’ to be used.6 The term contextual healing assumes that the context the patient finds themselves within (clinical environment, cognitive and affective communication of the clinician, the administration ritual, and the patient's cognitive and affective histories) can influence the magnitude of the placebo response.
These contextual factors have been examined in a study of placebo acupuncture. Patients with irritable bowel syndrome were allocated to no treatment; sham acupuncture alone; or sham acupuncture with ‘augmented ‘interaction involving warmth, attention, and confidence.7 Over 3 weeks, 28% of patients in the no treatment group reported ‘adequate reduction ‘in symptoms, compared with 44% in the sham acupuncture group and 62% of patients in the sham acupuncture with augmented interaction. This study indicates that components of the placebo effect can be incrementally added as a graded escalation of component factors. However, it is not clear if the overall effect is simply additive, or factors inherent in patients’ responses are dynamically interactive.
The context and strength of expectations associated with giving a placebo infusion were studied in a 2001 study of patients who had undergone a thoracotomy and were receiving a combination of buprenorphine analgesia as required and a saline infusion. The first group was told that the infusion was inert, the second group was told that the infusion may or may not contain a powerful painkiller, and the third group was told that the infusion contained a powerful painkiller. All groups recorded the same degree of relief. The third group who was told the saline infusion was an analgesic drug used 33% less buprenorphine than the control group, whilst the second group used 20% less. The expectation of analgesia, reinforced by verbal cues given, influenced the requirement for analgesics.8
The clinician may also be influencing the placebo effect in subtle ways not recognised overtly by either the patient or the clinician. In a study examining the effects of clinician expectations, patients in two groups received placebo, opioid analgesic, or naloxone. However, in one group, the clinicians believed no patients would receive an opioid.9 The placebo response in this group was reduced compared with the second group, indicating that clinician expectations were affecting the placebo response.
Clinician interaction style can influence an individual's response to treatment. Positive consultation styles have been found to be associated with the resolution of physical symptoms compared with negative consultation styles.10 In addition, we consider phenomena, such as ‘white coat syndrome’, when thinking about how clinicians can influence a patient's behaviour dependent upon non-verbal communication or even dress code.
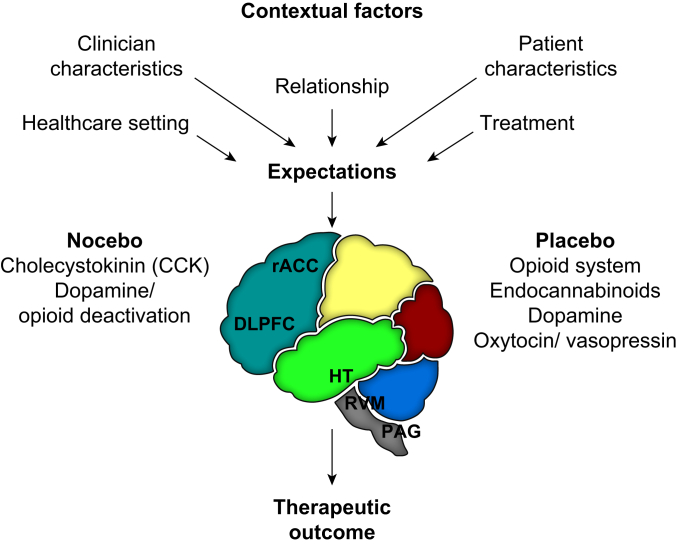
In consideration of various factors that influence the placebo response, the evidence suggests that the context and environment interact with the individual's physiology, as depicted in Figure 3.11
Fig 3.
Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain, adapted with permission from Rossettini and colleagues (2018).11 DLPFC, dorsolateral prefrontal cortex; HT, hypothalamus; PAG, periaqueductal grey; rACC, rostral anterior cingulate cortex; RVM, rostral ventromedial medulla.
Neurobiological mechanisms of placebo and nocebo
Placebo
The neurobiology of the placebo effect was first demonstrated in 1978 when it was shown that giving the opioid antagonist naloxone could block the placebo response, indicating the involvement of endogenous opioids.12 Subsequently, their role was shown to differ depending on the context, in which the placebo response was induced. In an experimental model of pain, naloxone blocked the placebo response related to expectation and conditioning with opioids. When the placebo response was induced with non-opioid conditioning using an NSAID, this response was naloxone insensitive.13
Cholecystokinin (CCK) has known anti-endogenous opioid actions. Administration of the CCK antagonist proglumide was found to enhance placebo analgesia. Opioid-induced placebo analgesic response appears to be mediated by a balance between endogenous opioids and CCK.14
In an experimental pain study, subjects were conditioned either with morphine or ketorolac during experimental arm tourniquet pain. The placebo response in the ketorolac group was blocked by the administration of the CB1 receptor antagonist rimonabant, which had no effect in the morphine group, indicating that the placebo response to the NSAID was mediated by the endocannabinoid system.15
Other neurotransmitters that have been found to be involved in the placebo effect include dopamine, oxytocin, and vasopressin. In patients with Parkinson's disease, increases in endogenous dopamine release in response to placebo administration were observed, comparable with those of therapeutic doses of levodopa or apomorphine.16 In addition, vasopressin has been found to enhance the expectation-induced placebo analgesia effects on experimental pain in women, but not in men.17 The influence of oxytocin on the placebo effect has yielded conflicting results, with some evidence of enhancement of placebo effects on experimental pain response in male volunteers.18
Nocebo
Cholecystokinin secretion and dopamine inhibition have been shown to play a role in the nocebo hyperalgesia response and activation of the hypothalamic–pituitary–adrenal (HPA) responses with increased plasma adrenocorticotropic hormone and cortisol. Nocebo hyperalgesia and HPA responses are antagonised by the anxiolytic drug diazepam, whereas the CCK antagonist proglumide blocks nocebo hyperalgesia without affecting HPA activity.19 Functional neuroimaging has shown involvement of areas of the brain involved with anticipatory anxiety, for which the clinical correlate may be fear avoidance, and in the commonly observed scenario when the patient flinches or withdraws before touch or palpation in the expectation of pain.20
Neuroanatomy
Neuroimaging studies have indicated involvement of the dorsolateral prefrontal cortex, rostral anterior cingulate cortex, hypothalamus, rostral ventromedial medulla, and periaqueductal grey in modulating the placebo effect both in terms of observed neuronal activity, but also in reported levels of pain after administration of naloxone.21 The neural circuitry implicated in this study is hypothesised to be demonstrating both top-down and bottom-up processing.
Placebo effects in clinical settings
Placebo effects are ubiquitous in pragmatic clinical settings and are of relevance to clinical outcomes, particularly in the context of acute and chronic pain. These effects depend on factors related to the treatment, the patient, and the clinician. The complex dynamic interaction of these factors is what determines the eventual direction and magnitude of placebo response in any given patient, within a specific context.
Placebo mechanistic studies are usually carried out in healthy volunteers, but clinical studies revealing placebo effects in patients have included numerous pain conditions, including acute postoperative pain, headache, neuropathic pain, low back pain, and irritable bowel syndrome.
Placebo effects on drug treatment
The important study (also referred to in the section on psychological mechanisms) in patients after thoracotomy indicates the importance of positive verbal cues on improving analgesic outcomes. Whilst inert treatment given with deceptive intent is unethical in clinical practice, other studies by the same authors demonstrated that non-deceptive overt delivery of analgesia, given with positive verbal cues, was superior in reducing pain compared with hidden administration, confirming that patient expectation may be positively modified to improve analgesia.22
It is probable that positive (although importantly, ethically, accurate) information about medication may improve its effectiveness.
A qualitative study on patient use of medication as prescribed found that whilst patients were pragmatic rather than idealistic in using a wide range of prescribed medication, past medication experiences and relationships with healthcare providers were particularly influential, which appear to be consistent with recurring themes of experience and expectation, and of practical utility in optimising analgesic use in pain clinic and community settings.23
The clinic environment itself may have relevance to both nocebo and placebo effects—or potentially individual patient responses—as these can be influenced by social learning or contagion, with evidence that vicarious experience is a factor.24
Placebo effects in a pain management programme
A pain management programme (PMP) is a group intervention for chronic pain that has been embedded in clinical practice. Many PMPs are based on models, such as cognitive behaviour therapy or acceptance and commitment therapy, and as such aim to promote a supportive psychotherapeutic context. Treatment complexity explains an absence of research on placebo in this area. Positive contextual factors, such as interpersonal peer interactions and repeated positive experiences of a PMP, would theoretically have a beneficial impact upon patients in addition to the educational materials presented at the groups.
Placebo effects on X-ray-guided interventions
The ubiquity of the placebo effect on procedures is recognised in clinical practice guidelines. Studies examining responses to facet joint injections and medial branch blocks (MBBs) have used saline injections as a control. These injections are designed as a placebo intervention (albeit one that involves needle puncture and injection of saline). Some patients receiving saline injections do report pain relief, and in one study, 32% of such patients reported greater than 50% pain relief after the injection of saline.25 Guidelines for the investigation of lumbar facetogenic pain suggest that MBBs resulting in 80% pain relief should be repeated in putatively positive responders, before radio-frequency neurotomy, with reported false-positive rates of MBBs between 25% and 41%, which may be a placebo response.26
It is likely that placebo responses are present in all needle-based pain interventions.
Individual factors
Not all individuals display response to placebo. This can in part be explained by individual physiological differences, but also to psychological factors, as discussed earlier. Several studies have looked to identify particular psychological characteristics, which give insight into how an individual would respond to placebo. Corsi and Colloca found that placebo responses were negatively correlated with anxiety severity and pain.27 They also reviewed other research that suggested that placebo was associated with optimism, suggestibility, empathy, openness to experience, and somatic focus, whilst nocebo was associated with pessimism, anxiety, and catastrophising. Whilst in a clinical setting it would be impractical to administer a battery of psychometric tests to each individual, it is important to consider how psychological factors can influence the response to treatment and how these factors could be incorporated into ‘treatment as usual’ within a clinical setting.
Conclusions: clinical usefulness of the placebo effect
Placebo effects are many and varied, and have particular significance in the treatment of pain. Whilst the administration of a placebo as a deceptive and sole treatment is appropriately limited by ethical considerations, the same mechanisms underlying placebo effects apply to the administration of active treatments in pragmatic clinical settings.
The context surrounding the administration of all treatments is very important. Comparisons of open with hidden administration of drugs have shown that treatment is more effective when given openly with the patient expecting an effect. Expectation, both on the part of the patient and the clinician, influences the context, as does conditioning (prior experience), consultation style, and many other factors surrounding the treatment.
This highlights the attention we should pay to the context surrounding the treatments we give. Since it is demonstrated that placebo effects exist in routine clinical care as a result of therapeutic rituals, the doctor–patient relationship, and psychosocial context, it is appropriate and advisable to maximise these effects. The importance of this placebo component of treatment, even when no ‘placebo’ is administered, should not be underestimated and should be exploited for the benefit of the patient.
It is important to offer the ‘right’ treatment—that is, the one(s) most likely to ‘work’—early, as this increases the chances of therapy being successful. Debate has historically presented two opposing underlying mechanisms that govern the placebo effect. However, recent thinking has pointed to a synthesis of conditioning and expectation models, which allows us to consider a person's physiological response in the context of their learned history. Therefore, therapeutic effectiveness may be further enhanced by clinicians who consider the individual and environmental contexts that patients find themselves within, and use the conditioning and expectation effects that we are all subject to when engaging in therapeutic encounters.
Declaration of interests
The authors declare that they have no conflicts of interest.
MCQs
The associated MCQs (to support CME/CPD activity) are accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Nick Plunkett FRCA FFPMANZCA FFPMRCA is a consultant in anaesthesia and pain medicine. In addition to a long-standing commitment to education in pain medicine, Dr Plunkett has an interest in understanding the influence of psychological factors on the presentation of pain conditions to improve interdisciplinary clinical management.
Joel Perfitt FRCA FFPMRCA is a consultant in anaesthesia and pain medicine with an interest in the assessment of acute and chronic pain, their management, and interventional techniques.
Steve Jones DClinPsy MSc BSc is a senior clinical psychologist with an established interest in investigating the overlap between physical and mental health. He has researched in chronic pain, cystic fibrosis, and eating difficulties focusing on how our perceptions of the world and our context can influence our physical and psychological experiences.
Matrix codes: 1D01, 2E01, 3E00
References
- 1.Kong J., Kaptchuk T.J., Polich G. Expectancy and treatment interactions: a dissociation between acupuncture analgesia and expectancy evoked placebo analgesia. Neuroimage. 2009;45:940–949. doi: 10.1016/j.neuroimage.2008.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kienle G.S., Kiene H. The powerful placebo effect: fact or fiction? J Clin Epidemiol. 1997;50:1311–1318. doi: 10.1016/s0895-4356(97)00203-5. [DOI] [PubMed] [Google Scholar]
- 3.Vase L., Skyt I., Hall K.T. Placebo, nocebo, and neuropathic pain. Pain. 2016;157(Suppl. I):S98–S105. doi: 10.1097/j.pain.0000000000000445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stewart-Williams S., Podd J. The placebo effect: dissolving the expectancy versus conditioning debate. Psychol Bull. 2004;130:324–340. doi: 10.1037/0033-2909.130.2.324. [DOI] [PubMed] [Google Scholar]
- 5.Tiemann L., May E.S., Postornio M. Differential neurophysiological correlates of bottom-up and top-down modulations of pain. Pain. 2015;156:289–296. doi: 10.1097/01.j.pain.0000460309.94442.44. [DOI] [PubMed] [Google Scholar]
- 6.Miller F.G., Kaptchuk T.J. The power of context: reconceptualising the placebo effect. J R Soc Med. 2008;101:222–225. doi: 10.1258/jrsm.2008.070466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaptchuk T.J., Kelley J.M., Conboy L.A. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008;336:999–1003. doi: 10.1136/bmj.39524.439618.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pollo A., Amanzio M., Arslanian A., Casadio C., Maggi G., Benedetti F. Response expectancies in placebo analgesia and their clinical relevance. Pain. 2001;93:77–84. doi: 10.1016/S0304-3959(01)00296-2. [DOI] [PubMed] [Google Scholar]
- 9.Gracely R.H., Dubner R., Deeter W.R., Wolskee P.J. Clinicians’ expectations influence placebo analgesia. Lancet. 1985;1:43. doi: 10.1016/s0140-6736(85)90984-5. [DOI] [PubMed] [Google Scholar]
- 10.Thomas K.B. General practice consultations: is there any point in being positive? Br Med J (Clin Res Ed) 1987;294:1200–1202. doi: 10.1136/bmj.294.6581.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rossettini G., Carlino E., Testa M. Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain. BMC Musculoskelet Disord. 2018;19:27. doi: 10.1186/s12891-018-1943-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levine J.D., Gordon N.C., Fields H.L. The mechanisms of placebo analgesia. Lancet. 1978;2:654–657. doi: 10.1016/s0140-6736(78)92762-9. [DOI] [PubMed] [Google Scholar]
- 13.Benedetti F., Mayberg H.S., Wager T.D., Stohler C.S., Zubieta J.K. Neurobiological mechanisms of the placebo effect. J Neurosci. 2005;25:10390–10402. doi: 10.1523/JNEUROSCI.3458-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Benedetti F. The opposite effects of the opiate antagonist naloxone and the cholecystokinin antagonist proglumide on placebo analgesia. Pain. 1996;64:535–543. doi: 10.1016/0304-3959(95)00179-4. [DOI] [PubMed] [Google Scholar]
- 15.Benedetti F., Amanzio M., Rosato R., Blanchard C. Nonopioid placebo analgesia is mediated by CB1 cannabinoid receptors. Nat Med. 2011;17:1228–1230. doi: 10.1038/nm.2435. [DOI] [PubMed] [Google Scholar]
- 16.de la Fuente-Fernandez R., Ruth T.J., Sossi V., Schulzer M., Calne D.B., Stoessl A.J. Expectation and dopamine release: mechanism of the placebo effect in Parkinson’s disease. Science. 2001;293:1164–1166. doi: 10.1126/science.1060937. [DOI] [PubMed] [Google Scholar]
- 17.Colloca L., Pine D.S., Ernst M., Miller F.G., Grillon C. Vasopressin boosts placebo analgesic effects in women: a randomized trial. Biol Psychiatry. 2016;79:794–802. doi: 10.1016/j.biopsych.2015.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kessner S., Sprenger C., Wrobel N., Wiech K., Bingel U. Effect of oxytocin on placebo analgesia: a randomized study. JAMA. 2013;310:1733–1735. doi: 10.1001/jama.2013.277446. [DOI] [PubMed] [Google Scholar]
- 19.Benedetti F., Amanzio M., Vighetti S., Asteggiano G. The biochemical and neuroendocrine bases of the hyperalgesic nocebo effect. J Neurosci. 2006;26:12014–12022. doi: 10.1523/JNEUROSCI.2947-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Finniss D.G., Kaptchuk T.J., Miller F., Benedetti F. Biological, clinical, and ethical advances of placebo effects. Lancet. 2010;375:686–695. doi: 10.1016/S0140-6736(09)61706-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Eippert F., Bingel U., Schoell E.D. Activation of the opioidergic descending pain control system underlies placebo analgesia. Neuron. 2009;63:533–543. doi: 10.1016/j.neuron.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 22.Pollo A., Amanzio M., Arslanian A., Casadio C., Maggi G., Benedetti F. Response expectancies in placebo analgesia and their clinical relevance. Pain. 2001;93:77–84. doi: 10.1016/S0304-3959(01)00296-2. [DOI] [PubMed] [Google Scholar]
- 23.Dolovich L., Nair K., Sellors C., Lohfeld L., Lee A., Levine M. Do patients’ expectations influence their use of medications? Qualitative study. Can Fam Physician. 2008;54:384–393. [PMC free article] [PubMed] [Google Scholar]
- 24.Benedetti F. Placebo effects: from the neurobiological paradigm to translational implications. Neuron. 2014;84:623–637. doi: 10.1016/j.neuron.2014.10.023. [DOI] [PubMed] [Google Scholar]
- 25.Schwarzer A.C., Wang S.C., Bogduk N., McNaught P.J., Laurent R. Prevalence and clinical features of lumbar zygapophysial joint pain: a study in an Australian population with chronic low back pain. Ann Rheum Dis. 1995;54:100–106. doi: 10.1136/ard.54.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bogduk N. On diagnostic blocks for lumbar zygapophysial joint pain. F1000 Med Rep. 2010;2:57. doi: 10.3410/M2-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Corsi N., Colloca L. Placebo and nocebo effects: the advantage of measuring expectations and psychological factors. Front Psychol. 2017;8:308. doi: 10.3389/fpsyg.2017.00308. [DOI] [PMC free article] [PubMed] [Google Scholar]