Ultrasound is used in medicine for imaging, therapy and for measurement of blood velocity. The use of this low energy, non-ionising waveform means that ultrasound exposures are thought to be less hazardous than other imaging modalities, though mild local tissue heating occurs with absorption of ultrasound energy.
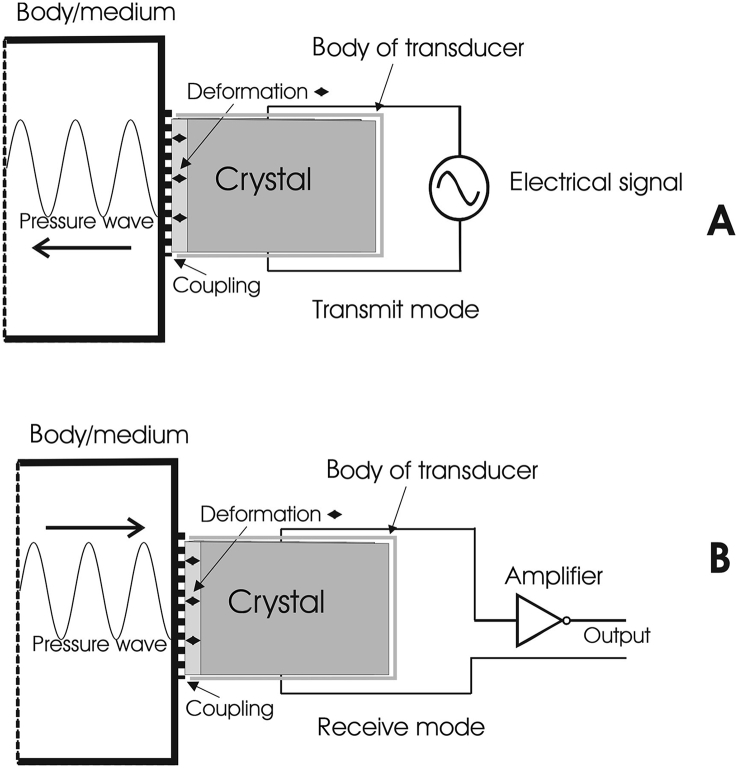
Ultrasonic vibration is defined as being in the bandwidth of 20 kHz to the MHz range, above human hearing ability. An ultrasound probe or transducer consists of a piezoelectric crystal, which mechanically generates and transmits a vibrating pressure wave in a tissue in response to an alternating electrical input (Fig 1A). Conversely, it also transduces an alternating electrical output in response to a vibrating pressure wave input from the tissue. Hence, the piezoelectric crystal can be used both to transmit a pressure wave and to detect a reflected wave (Fig 1B).
Fig. 1.
(A) Generation and transmission of an ultrasound pressure wave from a piezoelectric crystal using an alternating electrical signal input. (B) Reception and detection of a reflected ultrasound pressure wave by a piezoelectric crystal, which generates an electrical signal output (Supplementary material).
The reflection of the ultrasound wave at the interface between two tissues of different densities, or at tissue-fluid (air) interfaces, produces a diagnostic image. The same piezoelectric crystal is usually used as the receiver, with the transmission mode switched off. The reflected pressure changes coupled to the transducer induce electrical signals (Fig 1B), which are processed and displayed to produce an image; this is known as B (‘brightness’) mode. A real-time 2-D image is produced, sometimes using multiple probes arranged in a linear fashion, each transmitting a pulsed wave of ultrasound before electronically gated switching to the receiving mode occurs. This pulsing allows each reflected wave to be associated with its own transmitted wave. Multiple ultrasound probe arrays and their signal processing electronics are designed to create, detect and display changing images with changes in probe position, so that the full image is created with all components at the correct distance from the probe. Moving objects within the scan field can be seen, and additional information about the extent of motion along the line of a single beam can be obtained by more rapid sampling of the M (‘motion’) mode.
If c is the wave propagation velocity, then c=f λ, where f is the wave transmission frequency and λ is its wavelength. Ultrasound velocity in a biological tissue, and the attenuation of the wave amplitude, vary depending on which tissue it is travelling through. In soft tissues the wave velocity is between 1460 and 1630 m s−1, whereas in bone it is 2700–4100 m s−1. Attenuation increases with wave frequency and bone attenuates the waveform about 10 times as much as soft tissue. The greatest penetration is achieved with the lowest frequency, but this gives poor resolution of detail, while the converse holds for high frequency waves. A compromise is to use a frequency high enough that will give good resolution, and low enough to ensure adequate penetration of the tissues being investigated. For example, a frequency of 3 MHz is normally used to visualised the kidneys, while 20 MHz is used to visualise intracorporeal devices inserted by the anaesthetist, such as needles and catheters.
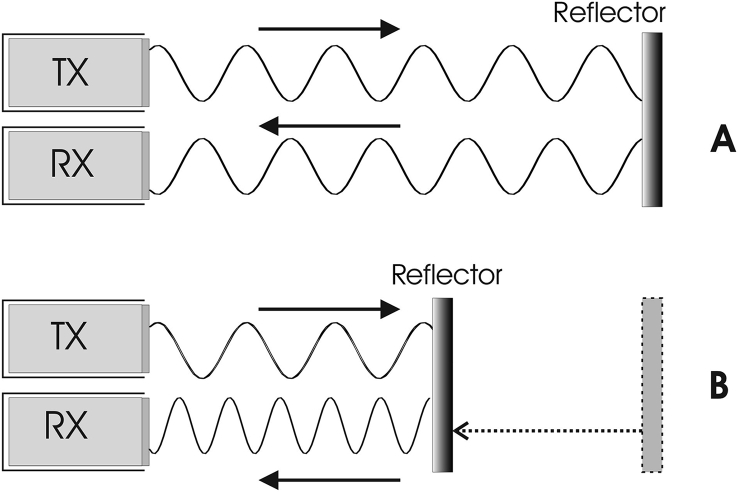
Ultrasound can also be used in Doppler mode. When an ultrasonic wave reflects off a stationary object, the reflected wave has the same frequency as the transmitted wave (Fig 2A). However, when the object (such as a collection of red blood cells) is moving towards the transmitter, it encounters more oscillations per unit time than its stationary equivalent, so the frequency of the reflected wave is apparently increased (Fig 2B). Conversely, when the object is moving away from the ultrasound wave, the frequency of the reflected wave is reduced. This property, the Doppler effect, can be used as a non-invasive technique for measurement of blood velocity within the body, whence flow may be calculated. For a transmitted frequency fT, of wavelength λ, and if the velocity of the wave in the medium is c, fT=c/λ. If the beam hits an object which is moving directly towards the transmitter at velocity v (v<<c), the frequency of the waves arriving at the reflecting boundary (fR) will now appear to be: fR=(c+v)/λ. The reflecting boundary will now act as an ultrasonic wave source, which is moving towards the transmitter at velocity v, and the actual frequency sensed by the transmitter (in receiver mode) will be:
Fig. 2.
(A) When a transmitted (TX) wave is reflected off a stationary object, the reflected wave is received (RX) at the same frequency as the transmitted wave. (B) When the reflecting object is moving towards the transmitted wave, the frequency of the reflected wave increases; this is the Doppler effect (Supplementary material).
The apparent increase in frequency is given by ,
Normally the Doppler beam is applied non-invasively (i.e. not directly facing an oncoming flow of blood), but from outside the blood vessel, say at an angle θ to the long axis of the blood vessel, and the expression for frequency shift becomes:
The frequency difference can be transduced into an audible signal, or used to calculate the velocity of the blood cells.
The greatest accuracy in measuring blood velocity (e.g. to derive cardiac output) is achieved by having the probe aligned as far as is possible with the vessel (e.g. keeping θ to a minimum). Having measured the mean velocity of the blood in a vessel in order to calculate the blood flow, the mean diameter of the vessel must also be measured, and its cross-sectional area calculated; then the blood flow (e.g. cardiac output if the aorta has been visualised) is essentially the velocity times the cross-sectional area. The velocity profile across a vessel may be nearly constant if the blood flow is turbulent near the aortic valve, or parabolic if it is closer to laminar further downstream during at least part of the cardiac cycle, but modern Doppler devices recognise this and calculate the mean velocity.
While some systems use separate transmission and receiving probes to give continuous wave Doppler, others use the same probe to transmit and receive pulsed wave Doppler signals. Although useful for showing specific structures, pulsed wave Doppler is unable to sample at a high enough rate to avoid ‘aliasing’. Aliasing occurs when the velocity of movement, in terms of pulses/second (e.g. of blood flow) is more than half the pulsed Doppler wave sampling rate, and can lead to the direction of flow being misinterpreted. Duplex Doppler uses a normal black and white ultrasound image for the structure being visualised (e.g. the aorta), and switches to colour in Doppler mode to visualise blood flow within, with colour coding corresponding to the magnitude and direction of flow. This allows vessel structure and function to be visualised and quantified.
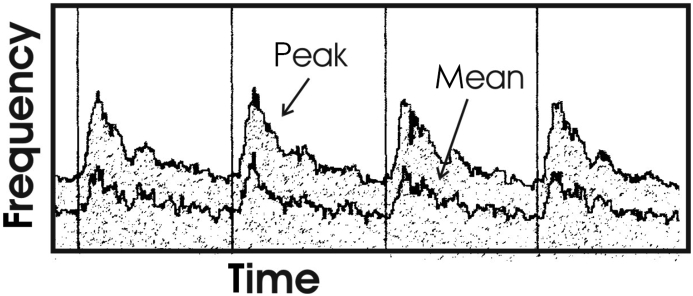
More quantitative information can be deduced from the Doppler power spectrum of the audio signal, or the Doppler frequency shift spectrum. The frequency shift spectrum represents the variation of flow velocity, and the power spectrum within a frequency bandwidth is proportional to the number of blood cells with velocities in that range (Fig 3). The power frequency shift spectrum bears a superficial resemblance to the velocity profile of flow in a vessel. Given that the velocity waveforms in a vessel throughout the cardiac cycle are complex, this sort of analysis gives more information of the severity of arterial or cardiac disease than a single measurement of mean velocity.
Fig. 3.
Doppler frequency shift spectrum for peak and mean blood velocity spectra; the density of grey dots represents the power spectrum within frequency bandwidths (Supplementary material).
Declaration of interest
The author declares that they have no conflict of interest.
Biography
Patrick Magee PhD, FRCA was a consultant anaesthetist at Royal United Hospitals Bath, retiring from clinical practice in 2019. A biomedical engineer before clinical training, he has maintained his links with the engineering community through work with the British Standards Institute, the Royal Academy of Engineering, the Institute of Mechanical Engineers, and the University of Bath. He completed his PhD in biomedical engineering in 2014. He is a past examiner for the Primary FRCA and the European Diploma in Anaesthesiology and has published a book and numerous chapters and papers on physics, clinical measurement and equipment relevant to anaesthetic practice.
Matrix codes: 1A03, 2A04, 3I00
Further reading
- 1.The Physics, Clinical Measurement and Equipment of Anaesthetic Practice. Patrick Magee and Mark Tooley, OUP; 2011. Ch.10. [Google Scholar]