Key points.
-
•
For accurate cerebral perfusion pressure calculation, both intracranial pressure (ICP) and MAP transducers should be zeroed at the level of the external auditory meatus.
-
•
Multiple invasive and non-invasive imaging techniques are available for cerebral blood flow measurements.
-
•
The lactate/pyruvate ratio generated via microdialysis is a useful marker of cerebral ischaemia in conjunction with ICP and tissue oxygenation (PtiO2), which is itself a useful marker for tissue hypoxia.
-
•
Multimodality cerebral monitoring can provide individualised targets for management.
Learning objectives.
By reading this article, you should be able to:
-
•
Describe the methods for measuring intracranial pressure (ICP) and identify the components of a normal ICP trace.
-
•
Discuss the available methods and clinical applications of cerebral tissue oxygenation monitoring.
-
•
Explain the underlying physical principles and indications for cerebral blood flow measurement.
Monitoring the brain after traumatic injury, subarachnoid haemorrhage, and neurosurgery plays a crucial role in guiding management, optimising cerebral function, and prevention of secondary brain injury. This article aims to outline some of the scientific principles and clinical applications of different monitoring modalities.
Monitoring intracranial pressure
Intracranial pressure
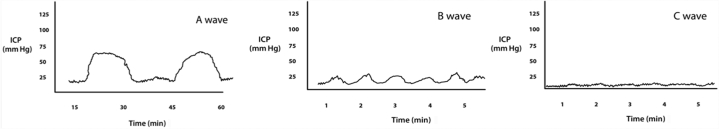
The cerebrospinal fluid acts as a dynamic pressure system. Pressure can be measured directly from the lateral ventricle via a lumbar puncture, lumbar drain, or an intra-parenchymal sensor. Intracranial pressure (ICP) has physiological values of 3–4 mm Hg up to 1 yr, and 10–15 mm Hg in adults. Higher values correspond to intracranial hypertension. The normal ICP trace is pulsatile, reflecting cardiac and respiratory cycles. The cardiac component has three peaks: the P1 (percussion wave) correlating with arterial pulsation, P2 (tidal wave) generated by both arterial pulsation and resistance from intracranial parenchyma, and P3 (dicrotic wave) reflecting closure of the aortic valve. The respiratory component of the waveform is generated by the changes in intrathoracic pressure caused by respiration. As intracranial compliance decreases, pathological waves start to appear. Lundberg described three types of pressure waves: A, B, and C (Table 1; Fig. 1). However, this classification is no longer considered to be useful clinically. In modern clinical practice, the emphasis on recognition and treatment of increased ICP means that plateau waves (Lundberg A waves: an ICP of 50–100 mm Hg for 5–20 min) are rarely seen.
Table 1.
Lundberg waves: variations in the intracranial pressure waveform
| Types of ICP wave |
|---|
|
A waves: pathological, plateau shaped, amplitude 50–100 mm Hg, last 5–20 min, suggestive of low brain compliance B waves: rhythmic oscillations, amplitude <50 mm Hg, occur every 1–2 min, seen in patients undergoing mechanical ventilation, less useful clinically, suggestive of low brain compliance C waves: rhythmic oscillations, amplitude <20 mm Hg, occur every 4–8 min, synchronous with spontaneous variations in arterial blood pressure, non-pathological |
Fig 1.
Lundberg CSF pressure waves A, B, and C. Note the different timescales for each.
Monitoring of ICP is useful in a range of pathologies, including traumatic brain injury (TBI), hydrocephalus, stroke, and encephalopathy. It can be measured using devices inserted into the ventricle, brain parenchyma, and subdural or sub-arachnoid spaces. An intraventricular catheter is the gold standard method. This provides a global measurement of ICP, but also allows in vivo calibration, therapeutic drainage of CSF, and administration of intrathecal drugs. However, intraventricular catheters can be a source of infection, and placement may be difficult in patients with small ventricles or cerebral oedema. Intra-parenchymal catheters are used more commonly. These micro-transducer or fibreoptic tipped systems are placed via a cranial access device or via a small burr hole into the subdural space. Although less invasive and considered accurate, they tend to measure local pressure and may show drift with time.
Intracranial pressure monitoring allows the early detection of an expanding lesion and the calculation of cerebral perfusion pressure (CPP). It has become standard of care in the management of TBI. The Brain Trauma Foundation (BTF) recommends continuous ICP monitoring in the management of all patients with severe TBI to reduce the in-hospital and 2 week mortality after injury. Treatment of an ICP >22 mm Hg is also recommended, as values above this level are associated with increased mortality.1 However, there remains a lack of Class 1 evidence that ICP-guided therapy improves outcomes. A trial performed in South America found no difference in 3–6 month outcomes in patients with severe TBI whose care was guided by ICP monitoring compared with those whose care was based on imaging and clinical examination.2 However, this study had a number of limitations. Differences in patient care, both before hospital admission and after hospital discharge, were not reported, and its applicability to routine practice in developed countries has been questioned. The consensus opinion remains that ICP monitoring remains the standard of care in TBI, as a prospective randomised trial will be impossible.
Cerebral perfusion pressure
Cerebral perfusion pressure is calculated by the following equation: CPP=MAP–ICP. For accurate calculation of CPP, the transducers measuring both MAP and ICP should be zeroed at the level of the foramen of Monro (external auditory meatus).3 The primary goal of an adequate CPP is to maintain cerebral blood flow (CBF) and tissue oxygenation, and its manipulation has become central to the management of TBI. Current guidelines, for survival and favourable outcomes, target a CPP between 60 and 70 mm Hg. However, the minimum optimal CPP threshold is unclear and may depend upon the patient's capacity for cerebral autoregulation. An individualised target CPP for each patient has been proposed.
Cerebrovascular pressure reactivity
Cerebrovascular pressure reactivity is a key component of cerebral autoregulation and is frequently impaired in brain injury. A pressure reactivity index (PRx) can be calculated as a moving correlation coefficient between consecutive values for ICP and arterial blood pressure (ABP) averaged over a defined time. A positive PRx suggests disturbed reactivity of cerebral vasculature or impaired autoregulation. A negative value, where ABP is negatively correlated with ICP, reflects normal autoregulation. It has been suggested that PRx be used to define individual CPP targets in TBI. However, although PRx has been shown to correlate with outcome in some studies, there is currently not enough prospective evidence for its routine use in clinical practice.4
Monitoring cerebral oxygenation
Jugular venous oxygen saturation
Jugular venous oxygen saturation (SjvO2) gives an assessment of global oxygenation and the adequacy of CBF. A catheter is inserted by retrograde cannulation of the internal jugular vein and advanced into the jugular bulb. It should be placed on the side of worst pathology or on the dominant side for venous drainage. Dominance is determined by compression of each internal jugular vein separately and observing for the greatest change in ICP. If no dominance is seen, the right side tends to be used. The catheter tip should lie level with the C1/C2 disc and the position confirmed on a lateral cervical spine X-ray. If the tip is in the wrong position, significant error may result from admixture with extracranial blood. Additional complications include subclinical thrombosis and those associated with central venous cannulation. Measurements can be taken intermittently using serial sampling. Spectrophotometric catheters enable continuous measurement.
SjvO2 reflects the balance between the oxygen supply (CBF, SpO2) and demand (Table 2). Normal SjvO2 is between 55% and 75%. Values below this suggest hypoperfusion with oxygen demand exceeding supply. Cerebral ischaemia is present when SjvO2 is <55%, but cannot be assumed to be absent at higher values. High SjvO2 values indicate hyperaemia or reduced metabolic demand. Most studies are in severe TBI where it has been used to guide interventions, such as the use of hyperventilation. However, SjvO2 provides limited information in patients with focal ischaemia. Positioning problems, clot formation on the catheter, and poor sampling technique also affect accuracy.5
Table 2.
Factors affecting jugular venous oxygen saturation (SjvO2)
| Low SjvO2 | High SjvO2 |
|---|---|
| Reduction in oxygen delivery | Reduced cerebral oxygen consumption |
| Raised ICP | Coma |
| Reduced CBF | Hypothermia |
| Hypoxia | Cerebral infarction |
| Profound hypocarbia | |
| Increased cerebral oxygen demand | Increased oxygen delivery |
| Seizures | Hypercapnia |
| Pyrexia | Vasodilation |
Near-infrared spectroscopy
Near-infrared spectroscopy (NIRS) is a non-invasive bedside monitor of regional cerebral oxygenation. Light waves in the near-infrared range (700–1000 nm) are able to penetrate the skin, bone, and brain tissues relatively easily. The main chromophores present in the brain are oxygenated haemoglobin (HbO2), deoxygenated haemoglobin (Hb), and cytochrome aa3 (Cytox), all of which have different absorption spectra. Infrared light is shone through the surface layers of the brain. The light is reflected, redirected, scattered, and absorbed by different tissues with absorption dependent upon the oxygenation status, and the emergent light is sensed by detectors. Changes in the concentration of the near-infrared light can be quantified using reflectance spectroscopy based on the modified Beer–Lambert law.
NIRS has been used clinically to monitor patients with TBI and as an intraoperative monitor in patients undergoing cardiac surgery and carotid endarterectomy. The normal range of cerebral regional oxygen saturation (rSO2) is reported to be 60–75%, but there is a marked variability between NIRS devices. Other factors that reduce reliability include extracranial contamination and interference by ambient light. Ultrasound-tagged NIRS, combining NIRS and ultrasound, has been proposed as a potential improvement, as it aims to selectively detect the signal originating from changes in light passing through the grey matter. Stocchetti and colleagues used two devices to detect the absence of CBF in brain-dead patients. The devices tested both showed higher values of CBF in brain-dead patients than in healthy volunteers. They conclude that further refinements are required before NIRS can be considered reliable.6
Brain tissue oxygenation
Directly monitoring brain tissue oxygen is possible by introducing small flexible micro-catheters placed directly into the brain parenchyma in the area of interest. Different devices are available commercially. The most commonly used is the Licox® sensor (Integra, Mielkendorf, Germany), which measures tissue oxygenation (PtiO2) via a polarographic technique based on the Clark electrode. This consists of a membrane covering an aqueous potassium hydroxide electrolyte solution and two metallic electrodes (a silver anode and a gold cathode). The greater the partial pressure of oxygen is, the greater the diffusion of oxygen is through the membrane, where it is electrochemically reduced at the cathode. The number of oxygen molecules reduced at the cathode is reflected by changes in voltage. As this process is temperature dependent, a temperature probe corrects for variations in tissue temperature. Measurement is limited to the immediate area. Positioning in an area of ischaemia or haematoma will give misleading results. The Neurotrend™ device (Codman, Raynham/Massachusetts, USA) used optical luminescence to measure PtiO2, PtiCO2, pH, and temperature, but is no longer available. A newer device (Raumedic Neurovent-PTO™, RAUMEDIC, Helmbrechts, Germany), also using luminescence, is available, which measures PtiO2, ICP, and temperature. Compared with Licox®, higher PtiO2 values have been noted, which are thought to be a result of different sampling sizes of the probes. Licox® has a larger sensing surface area, which provides more consistent and reproducible measurements.
PtiO2 varies with changes in oxygenation and CBF. Most clinical experience is in patients with severe TBI, and data from this population have allowed the identification of baseline values, including PtiO2 20–35 mm Hg, PtiCO2 40–70 mm Hg, and pH 7.05–7.25.7 A consensus opinion of thresholds for ischaemia has also been deemed as PtiO2 <15–20 mm Hg: a threshold at which intervention should be considered. However, none of these values have yet been proven and are dependent on the underlying pathology. There have been encouraging results from ICP/CPP and PtiO2-guided interventions in patients with severe TBI. Although part of the BTF guidance, there is currently insufficient evidence to mandate its use. The Brain Oxygen Optimization in Severe TBI, Phase 3 trial is underway, which aims to address this question.
Monitoring CBF
Transcranial Doppler and transcranial colour-coded duplex
Transcranial Doppler (TCD) provides a non-invasive method for indirect measurement of CBF. Using a 2 MHz probe and pulsed-wave Doppler, flow velocities (FVs) can be measured in the intracranial arteries via insonation windows. It uses the Doppler effect, whereby the observed frequency of a signal increases as the source moves towards the observer. The velocity of blood flow is directly related to the change in transmitted frequency of a sound wave, which is then incorporated in the Doppler equation:
where V=velocity, c=speed of wave, θ=angle of blood flow relative to the probe, Ft=frequency of transmitted wave, and FD=Doppler shift frequency.
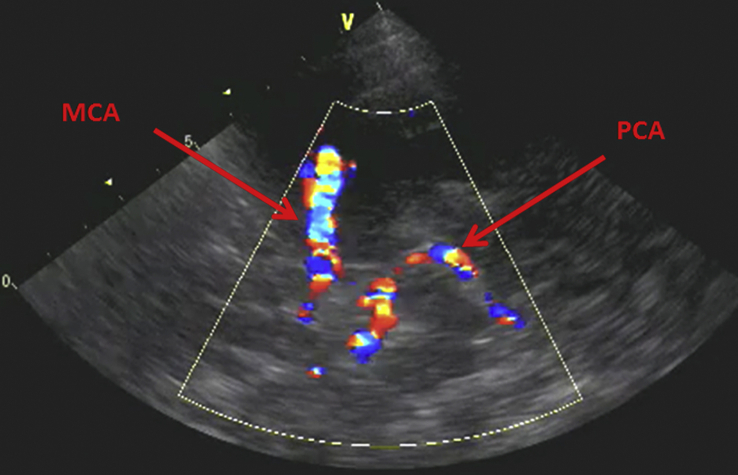
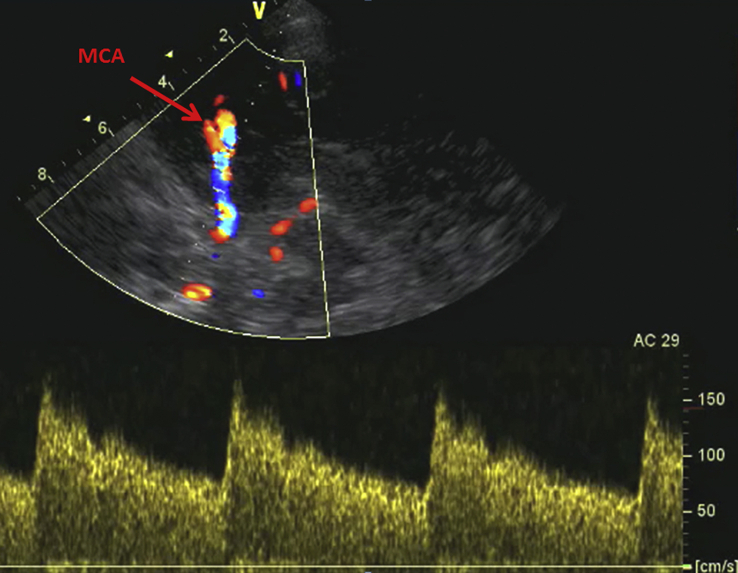
The mean FV correlates to changes in CBF provided that the diameter of the blood vessel and the angle of insonation both remain constant. The middle cerebral artery (MCA) is the most commonly insonated through the transtemporal window, which also allows insonation of anterior and posterior cerebral arteries (see Table 3). The transorbital window allows insonation of the ophthalmic artery and carotid circulation, whereas the distal vertebral and basilar arteries are accessed via the transforaminal window. Transcranial colour-coded duplex (TCCD) combines the pulsed-wave Doppler with real-time imaging to provide the capability for more accurate measurements (Fig 2, Fig 3).
Table 3.
Depth ranges and normal flow velocities (FV)
| Insonation window | Depth range (mm) | FV mean range (cm s−1) | |
|---|---|---|---|
| Middle cerebral artery | Transtemporal | 30–65 | 43–77 |
| Anterior cerebral artery | Transtemporal | 65–75 | 39–61 |
| Posterior cerebral artery | Transtemporal | 55–80 | 29–49 |
| Vertebral artery | Transforaminal | 60–95 | 27–47 |
| Basilar artery | Transforaminal | 90–120 | 31–51 |
| Ophthalmic artery | Transorbital | 35–55 | 16–26 |
| Internal carotid artery (extracranial) | Submandibular | 35–80 | 28–45 |
Fig 2.
TCCD image showing middle and posterior cerebral arteries [MCA and PCA] as insonated via the trans-temporal window at an approximate depth of 50–60 mm.
Fig 3.
MCA Doppler waveform, demonstrating a flow velocity (cm s−1) waveform using the pulsed-wave Doppler mode.
Transcranial Doppler is used primarily to monitor for vasospasm after subarachnoid haemorrhage. It can predict angiographic spasm with good sensitivity and specificity, increased further by the use of TCCD and inclusion of the Lindegaard index. Values of mean FV in the MCA values >120 cm s−1 coupled with a Lindegaard index 3–6 are highly indicative of vasospasm.8 The Lindegaard index is the ratio of the mean FV in the MCA to the mean FV in the internal carotid artery measured through the submandibular window.
Other clinical applications of TCD include the following:
-
(i)
detection of microemboli
-
(ii)
intraoperative monitoring during carotid surgery
-
(iii)
estimation of ICP through monitoring changes in pulsatility index (PI)
(PI=FV systolic–FV diastolic/FV mean)
An online educational video on the performance of TCD examination can be found at https://vimeo.com/176611066.
Imaging methods
CT perfusion
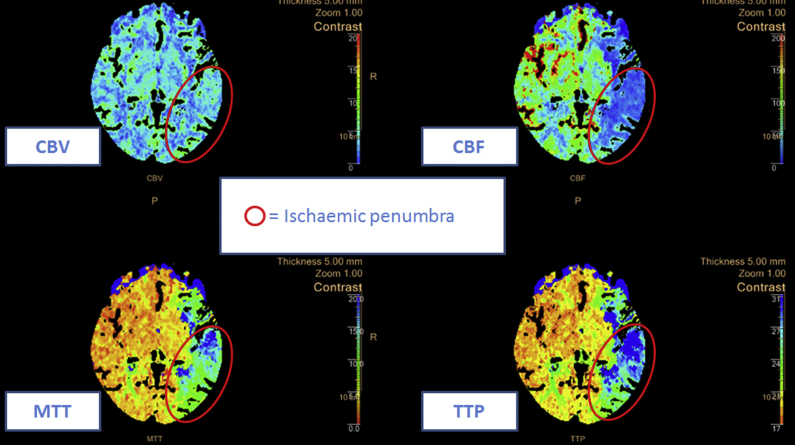
CT perfusion is widely used to assess CBF, particularly in patients presenting with acute stroke and subarachnoid haemorrhage, to identify potentially reversible cerebral hypoperfusion (ischaemic penumbra) and differentiate these areas with infarcted areas of the brain. It can be rapidly performed using a spiral CT scanner with images analysed by commercially available software to produce perfusion maps. Iodinated contrast is injected intravenously and multiple slices taken at the level of the basal ganglia to visualise all vascular territories (anterior, middle, and posterior cerebral arteries); however, this repetitive imaging of the brain tissue produces high doses of radiation for the patient. Calculations are made for mean transit time (MTT), measured in seconds and representing the average length of time a certain volume of blood spends in the cerebral arterial circulation, and cerebral blood volume (CBV), measured in millilitres of blood per 100 g of brain tissue and representing the total volume of blood in the cerebral arterial and venous systems per cerebral tissue volume. CBF is measured in millilitres of blood per 100 g of brain tissue per minute, and is related to CBV and MTT by the central volume principle, whereby CBF=CBV/MTT. CT perfusion maps are most commonly interpreted by visual inspection; in the example of acute stroke, the ischaemic penumbra is identified as the area with increased MTT, reduced or diminished CBF, but with preserved CBV because of blood supplied from the collateral circulation (Fig. 4).
Fig 4.
CT perfusion image in acute stroke demonstrating a left MCA territory mismatch with preserved CBV, but reduced CBF and increased MTT (note the colour-coded key next to each slice), indicating the ischaemic penumbra marked in red.
Calculations are also made for time (in seconds) for contrast to peak in brain tissue and to drain away, giving time-to-peak (TTP) and time-to-drain derivations, which are highly sensitive markers for cerebral ischaemia.9
Xenon-enhanced CT
Xenon is a highly lipid soluble inert gas. It readily crosses the blood–brain barrier and is clearly visible on CT scans. After a baseline CT scan, oxygen 100% is inhaled to wash out nitrogen, followed by inhalation of xenon until it equilibrates at a predetermined percentage. Another CT scan is performed and xenon inhalation discontinued. Serial CT scans are then taken and an analysis of xenon washout patterns allows the quantification of CBF through a modification of Kety–Schmidt technique.10
Perfusion-weighted MRI techniques
-
(i)
Arterial spin labelling: This is a non-invasive technique, as no contrast is injected. Protons in the arterial blood water are magnetically labelled by applying a radiofrequency pulse and rendering it an ‘endogenous tracer’. After a time delay called transit time, the tracer will arrive at its destination or region of interest, and at this point, MRI imaging is performed. This is compared to baseline imaging, and cerebral flow maps are produced.
-
(ii)
Dynamic susceptibility contrast-weighted imaging: When the i.v. contrast agent, gadolinium, passes through the cerebral arterial vasculature, it reduces the signal intensity for MRI images. Using this principle, gadolinium is injected, and repeated rapid MRI imaging is performed. When the sequence is analysed, a signal intensity curve is produced from which CBF can be calculated.
Nuclear medicine methods
(i) Positron emission tomography: This uses radioactive-labelled water [15O] H2O injected intravenously then scanned on a tomograph for a 10 min session, with arterial blood sampling to measure radioactivity. The injected [15O] H2O rapidly distributes into the brain tissue proportional to CBF, and then rapidly washes out. CBF is calculated by an analysis of time activity curves generated by the PET scanner.
(ii) Single photon emission computed tomography: This uses radioactive tracers, most commonly γ-emitting technetium 99. This is highly lipophilic, readily crosses the blood–brain barrier, and its distribution is proportional to CBF. It continues to emit γ radiation for some hours, which can be detected by γ cameras to produce a 3D image representing CBF.
Monitoring cerebral metabolism
Microdialysis
Cerebral microdialysis allows the continuous bedside monitoring of changes in local metabolites, which reflects cerebral energy metabolism. It has been used in patients with TBI and subarachnoid haemorrhage, and after surgery. A thin (0.6 mm) coaxial catheter is inserted into the chosen area. This has a dialysis membrane on its outer surface through which low flow rates of perfusate are pumped. The catheter wall allows free diffusion of water and solutes driven by the concentration gradient between the interstitial fluid and the perfusate. The molecular weight of the molecules sampled is limited by the pore size of the dialysis membrane. Micro-dialysate samples are collected about every 60 min to enable the measurement of substances in the cerebral extracellular fluid. The substances routinely analysed are the following:
-
(i)
energy-related metabolites (e.g. glucose, lactate, and pyruvate)
-
(ii)
neurotransmitters (e.g. glutamate and aspartate)
-
(iii)
markers of cellular degradation (e.g. glycerol and potassium)
-
(iv)
exogenous substances (e.g. drugs)
The concentration of these substances measured is not the absolute concentration, but dependent on the degree of equilibration between the interstitial fluid and the perfusate.
Microdialysis is considered useful in patients at risk of cerebral ischaemia or hypoxia. Glucose, lactate, and pyruvate concentrations provide information on cerebral glucose delivery, utilisation, and the contributions of aerobic vs anaerobic metabolism. The metabolic derangements seen in severe brain injury are associated with an elevation of the lactate/pyruvate ratio and reductions in brain glucose. Glycerol is produced from enzymatic degradation of phospholipid membranes after cell death, and increased levels have been found in microdialysis samples after severe TBI. Variations in the concentrations of glutamate and aspartate are also seen, with extremely high levels in secondary cerebral ischaemia and contusions. The lactate/pyruvate ratio is considered a useful marker of impaired cerebral metabolism and enables interventions to be tailored accordingly.7 However, microdialysis is not currently recommended for routine clinical use. As this technique only gives information regarding a small area surrounding the catheter, results must be interpreted in the context of catheter location, other monitors (e.g. ICP), and the clinical condition of the patient. As with any invasive technique, there is the possibility of complications, but these are rare.
Multimodality monitoring
Primary brain injury is characterised by a host of pathophysiological changes not all of which will be detected by individual neuromonitoring devices. Multimodality monitoring involves data integration from various monitoring tools assessing both local and global cerebral oxygenation, haemodynamics, and metabolism.11, 12 Multimodality monitoring provides a more comprehensive view of the patient's status, and enables optimal intervention targets to be set and the best treatment choices made.
Declaration of interest
The authors declare that they have no conflicts of interest.
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Mazen Elwishi FRCA is a consultant anaesthetist at St George's Hospital with an interest in neuroanaesthesia and anaesthesia for interventional radiology.
Judith Dinsmore FRCA is a consultant anaesthetist at St George's Hospital with a special interest in neuroanaesthesia. She is an examiner for the final FRCA and Joint Committee of Intercollegiate Examiners. She is also the current President of the Neuro Anaesthesia & Critical Care Society of Great Britain and Ireland.
Matrix codes: 1A01, 2A04, 3F00
References
- 1.Brain Trauma Foundation. Guidelines for the management of severe TBI, 4th ed. Available from: https://braintrauma.org/guidelines/guidelines-for-the-management-of-severe-tbi-4th-ed#/. [Accessed 25 May 2018].
- 2.Chestnut R.M., Temkin N., Carney N. A trial of intra-cranial pressure monitoring in traumatic brain injury. N Eng J Med. 2012;367:2471–2481. doi: 10.1056/NEJMoa1207363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas E., (on behalf of NACCS) Czosnyka M., Hutchinson P., (on behalf of SBNS) Calculation of cerebral perfusion pressure in the management of traumatic brain injury: joint position statement by the councils of the Neuroanaesthesia and Critical Care Society of Great Britain and Ireland (NACCS) and the Society of British Neurological Surgeons (SBNS) Br J Anaesth. 2015;115:487–488. doi: 10.1093/bja/aev233. [DOI] [PubMed] [Google Scholar]
- 4.Nordstrom C.-H., Koskinen L.-O., Olivecrona M. Aspects on the physiological and biochemical foundations of neurocritical care. Front Neurol. 2017;8:274. doi: 10.3389/fneur.2017.00274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Roux P., Menon D.K., Citerio G. Consensus summary statement of the international multidisciplinary consensus conference on multimodality monitoring in neurocritical care. A statement for healthcare professionals from the Neurocritical Care Society and the European Society of Intensive Care Medicine. Neurocrit Care. 2014;21(Suppl. 2):1–26. doi: 10.1007/s12028-014-0041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caccioppola A., Caarbonara M., Macri M. Ultrasound-tagged near-infrared spectroscopy does not disclose absent cerebral circulation in brain-dead adults. Br J Anaesth. 2018;121:588–594. doi: 10.1016/j.bja.2018.04.038. [DOI] [PubMed] [Google Scholar]
- 7.Bhatia A., Gupta A.K. Neuromonitoring in the intensive care unit. II. Cerebral oxygenation monitoring and microdialysis. Intensive Care Med. 2007;33:1322–1328. doi: 10.1007/s00134-007-0660-9. [DOI] [PubMed] [Google Scholar]
- 8.Marshall S.A., Nyquist P., Ziai W.C. The role of transcranial Doppler ultrasonography in the diagnosis and management of vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am. 2010;21:291–303. doi: 10.1016/j.nec.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Abels B., Klotz E., Tomandl B.F., Kloska S.P., Lell M.M. Perfusion CT in acute ischemic stroke: a qualitative and quantitative comparison of deconvolution and maximum slope approach. Am J Neuroradiol. 2010;31:1690–1698. doi: 10.3174/ajnr.A2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yonas H., Pindzola R.R., Johnson D.W. Xenon/computed tomography cerebral blood flow and its use in clinical management. Neurosurg Clin N Am. 1996;7:605. [PubMed] [Google Scholar]
- 11.Kirkman M.A., Smith M. Intracranial pressure monitoring, cerebral perfusion pressure estimation, and ICP/CPP-guided therapy: a standard of care or optional extra after brain injury? Br J Anaesth. 2014;1:35–46. doi: 10.1093/bja/aet418. [DOI] [PubMed] [Google Scholar]
- 12.Kirkman M.A., Smith M. Multimodal intracranial monitoring: implications for clinical practice. Anesthesiol Clin. 2012;30:269–287. doi: 10.1016/j.anclin.2012.05.007. [DOI] [PubMed] [Google Scholar]