Key points.
-
•
Knee joint arthroplasty is associated with significant postoperative pain, which may delay recovery and prolong hospital stay.
-
•
Pre-emptive and multimodal approaches to postoperative analgesia enhance recovery after knee joint arthroplasty.
-
•
Regional anaesthesia offers significant advantages in patients undergoing knee joint arthroplasty.
-
•
Novel regional anaesthetic techniques have been introduced as part of a multimodal analgesia programme after knee joint arthroplasty.
-
•
Further studies are required to determine the combination of regional anaesthetic techniques that provides optimal analgesia after knee joint arthroplasty.
Primary total knee joint arthroplasty (TKA) is among the most frequent procedures performed by orthopaedic surgeons. Despite excellent surgical outcomes, recovery after TKA remains a significant challenge for patients. Pain after orthopaedic surgery is often considered particularly difficult to manage, with up to half of patients reporting significant pain immediately after TKA. This may have a detrimental impact on postoperative recovery by delaying early mobilization and prolonging hospital stay. However, severe postoperative pain is also associated with significant complications including myocardial ischaemia, decreased pulmonary function, increased risk of infection, and the development of chronic pain. Postoperative pain may also affect the mental status of elderly patients, causing delirium or an anxiety disorder. The introduction of specific pathways of care including enhanced recovery programmes (ERPs) has delivered continuous improvement in preoperative, intraoperative, and postoperative outcomes (Fig. 1). Together with advances in pain control and early mobilization, ERPs have also significantly reduced the length of hospital stay (LOS) for patients undergoing TKA. The purpose of this review is to describe traditional and novel analgesic options within ERPs.
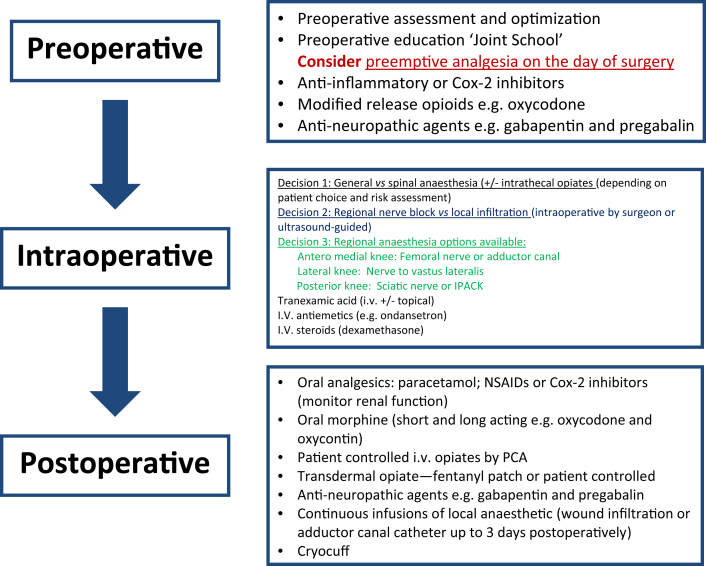
Fig 1.
Preoperative, intraoperative and postoperative pathways for patients undergoing knee joint arthroplasty.
Innervation of the knee
The neural innervation of the knee joint is complex and follows Hilton's Law which states that a joint is innervated by the articular branches of the muscles which move the joint. The articular nerves are derived from the femoral, obturator, tibial, common peroneal, and recurrent peroneal nerves. The femoral nerve, through its saphenous branch and also via its branches to the vastus medialis, intermedius, and lateralis muscles, supplies the suprapatellar recess, the patellar periosteum, and the anteromedial and anterolateral portions of the joint capsule. The medial, lateral, and posterior aspects of the joint capsule, the infrapatellar fat pad, tibial periosteum, and the superior tibio-fibular joint are supplied by the tibial nerve. The common peroneal nerve supplies the anterolateral portion of the capsule, the infrapatellar fat pad, and the tibial periosteum. The tibial periosteum, tibial tuberosity, infrapatellar fat pad, and the superior tibio-fibular joint are supplied by the recurrent peroneal nerve. The obturator nerve supplies the superior part of the posteromedial capsule and the anteromedial aspect of the capsule. Cutaneous innervation of the anterior aspect of the knee is supplied by the femoral nerve. The obturator nerve supplies the skin on the medial aspect of the knee in less than 40% of patients.
Independent predictors of severe postoperative pain after TKA
Independent predictors of moderate to severe postoperative pain after TKA include higher preoperative pain scores, depression, and younger age.1 These predictors may prove valuable in the development of a risk stratification tool for postoperative pain and the selection of an appropriate pain management strategy.
The multimodal approach to pain management
Chemical mediators including prostaglandins (PGE2) and bradykinin are released at the site of tissue injury. These chemical mediators stimulate nociceptors whose afferent fibres enter the spinal cord via the dorsal root ganglion and are propagated by central n-methyl-d-aspartate receptors in the spinal cord via the spinothalamic tract to the brain. The concept of multimodal analgesia relies on understanding these neurohumeral interactions and achieving postoperative analgesia by using a combination of drugs or modalities which inhibit this complex pathway at multiple sites and reduce the requirement for, and side-effects of, individual drugs or therapies.
Preoperative period
Patient education
TKA is a major surgical procedure that can be both physically and psychologically stressful for patients. Preoperative education is considered helpful in alleviating a patient's fears about the procedure, providing information about possible outcomes in an accessible format, gaining informed consent, and increasing patient satisfaction. The content of the education programme may include details regarding the surgical procedure and rehabilitation period, the expected benefits of the procedure, and pain management options available. Delivery of the education programme may be improved through personal interviews or presentation sessions and the use of educational media such as videos at ‘joint schools'. Preoperative education has been shown to have a modest beneficial effect on preoperative anxiety. There is, however, little evidence that its use improves postoperative outcomes in patients undergoing TKA, particularly with respect to pain, function, and LOS. There may be some beneficial effects when preoperative education is targeted at those patients most in need of support, including those who have limited social support structures.
Pre-emptive analgesia
An important aspect of pain management following TKA is the pre-emptive use of analgesics. Damage to tissues has been shown to provoke an increased reaction to noxious stimuli both peripherally, by reducing the threshold of nociceptive afferent nerve terminals, and centrally, by augmenting the excitability of second-order sensory neurons in the spinal cord. The concept of pre-emptive analgesia, the administration of analgesics prior to a painful stimulus, aims to prevent the establishment of central sensitization and amplification of postoperative pain. However, pre-emptive analgesia may by itself be too narrow a term and is being increasing viewed as one component of ‘preventative analgesia' which includes preoperative, intraoperative, and postoperative phases.2
The preoperative oral administration of opioids may be helpful for managing pain and reducing postoperative opioid requirements. In patients undergoing TKA, the pre-emptive use of opioids a few hours preoperatively has been shown to improve pain control and accelerate functional recovery.3 However, the preoperative administration of opioids is not commonly included in current ER pathways in order to avoid side-effects including sedation, dysphoria, and postoperative nausea and vomiting.
Pre-emptive administration of non-steroidal anti-inflammatory drugs (NSAIDs) including ketorolac and ibuprofen up to 2 hours preoperatively has been shown to reduce postoperative pain scores, opioid requirements and postoperative nausea.4 The primary site of action of NSAIDs is in the periphery, where they inhibit prostaglandin synthesis and stimulation of nociceptors. However, the use of NSAIDs is often limited due to potential side-effects including a decrease in platelet aggregation and increase in bleeding time, postoperative renal impairment, and impaired wound healing. NSAIDs may therefore be sometimes discontinued for at least 48 hours preoperatively according to surgical preference. Cyclo-oxygenase-2 inhibitors offer selective inhibition of prostaglandin synthesis, thereby reducing bleeding and gastric side-effects observed with non-specific NSAIDS. While preoperative administration of NSAIDs can improve postoperative pain and reduce the consumption of opioid analgesics after TKA, concerns regarding the potential increased risk of cardiovascular side-effects, including heart failure, have limited their use.5
Neuropathic pain is a complex phenomenon and may be recognized in up to 12% of patients following TKA.6 Pregabalin, an anticonvulsant medication, and its predecessor gabapentin, both gabapentinoids, are derivatives of the inhibitory neurotransmitter γ-aminobutyric acid which blocks α2δ subunit-containing voltage-dependent calcium channels. The beneficial effect of pre-emptive administration of pregabalin and gabapentin, an unlicensed use, in the context of knee surgery remains unclear. In one study the administration of gabapentin to patients 1 hour before undergoing knee surgery significantly improved postoperative analgesia and range of knee motion.7 However, further research is required in order to fully establish the optimum dosing schedule and the risks of preoperative gabapentinoid administration including sedation, headache, and visual disturbances. These side-effects may limit their usefulness in some patients, particularly the elderly with deranged renal function and those already receiving polypharmacy.
Intraoperative period
Regional versus general anaesthesia
Many reports over the past two decades have attempted to compare the risks and benefits of regional and general anaesthesia in different patient populations. Although not all studies agree, regional anaesthesia is associated with a reduction in major postoperative complications in a wide variety of surgical patients, with some of the greatest reductions seen in the orthopaedic population. These complications have included deep venous thrombosis, pulmonary embolism, blood transfusion requirements, pneumonia, and respiratory depression.8 There is some evidence to suggest that regional compared to general anaesthesia may be associated with a small but statistically significant reduction in 30-day mortality in patients undergoing TKA, while other studies have not confirmed these findings.9 LOS after TKA may also be reduced in patients receiving regional anaesthesia.
Neuraxial anaesthesia
One of the challenges in spinal anaesthesia is optimal titration of local anaesthetic (LA) to provide sufficient anaesthesia during surgery while avoiding a dosage that is too low and results in the need for supplemental intravenous opioids or conversion to general anaesthesia. Recently 5 mg intrathecal isobaric bupivacaine has been shown to provide adequate anaesthesia for up to an average surgical time of 66 minutes.10 However, this low dose of intrathecal bupivacaine is not standard practice. In combination with femoral nerve block (FNB) and/or sciatic nerve block (SNB) 5 mg intrathecal bupivacaine facilitates earlier recovery room discharge as well as reducing the incidence of urinary retention.10
Some agents may be co-administered with LAs in an attempt to enhance the quality of neural blockade. Commonly used agents have included vasoconstrictors (epinephrine), opioids (diamorphine, morphine, or fentanyl) and α-2 receptor agonists (clonidine). The use of such additives, however, introduces the possibility of additional side-effects. The evidence supporting the use of intrathecal morphine for TKA is not as compelling as that for hip arthroplasty and the optimum dose has yet to be conclusively identified. Large doses of 200–500 μg morphine have been shown to reduce postoperative analgesic requirements, but are associated with an increased incidence of side-effects. Urinary retention is a common problem after spinal anaesthesia, with an incidence of 23% across the surgical specialities increasing further with the use of hydrophilic neuraxial opioids. While moderate doses of intrathecal opioids (100 μg) have a long track record of safety, their use increases the incidence of pruritus and risks respiratory depression.
The benefits of epidural analgesia and surgical outcomes have been well documented in the literature. However, epidural analgesia has a significant failure rate and requires more intensive nursing vigilance including high dependency admission to manage hypotension. Combined with the potential for adverse effects including urinary retention, pruritus, hypotension, and motor blockade, epidural anaesthesia may delay recovery after TKA and is often regarded as incompatible with ERPs.
Peripheral nerve blocks
FNB, sometimes in combination with SNB, has traditionally been undertaken to provide analgesia after TKA. In the context of ERPs, the advantages of FNB are limited by quadriceps paresis which hinders postoperative physiotherapy and immediate functional recovery, in addition to increasing the risk of falls. SNB when added to FNB improves pain relief, but foot drop may further impair mobilization. There is now an increasing desire to undertake regional anaesthetic techniques which provide adequate analgesia and reduce morphine consumption without delaying postoperative physiotherapy and rehabilitation.
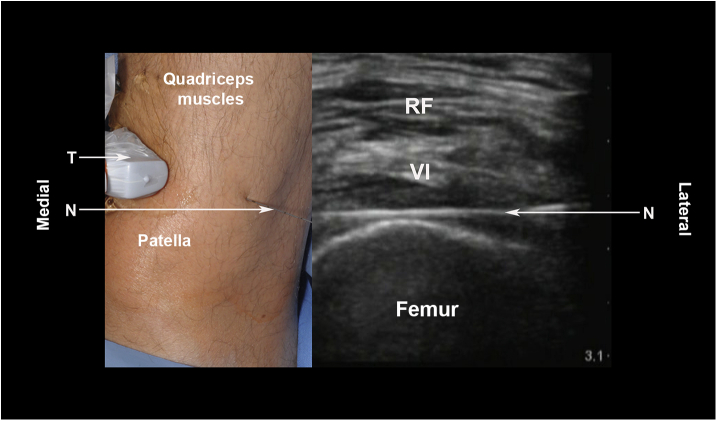
In recent years, there has been a resurgence of interest in the adductor canal block (ACB) as a viable alternative to FNBs within ERPs for knee arthroplasty.11 The adductor canal is a pyramidal, musculoaponeurotic tunnel from the apex of the femoral triangle to the adductor hiatus, running between the vastus medialis muscle anterolaterally and the adductor longus and adductor magnus muscles posteromedially. It is roofed in its entire length by the vastoadductor membrane (Fig. 2). The contents of the adductor canal include the superficial artery and vein, saphenous nerve, the nerve to vastus medialis, the posterior branch of the obturator nerve, and in some cases, the medial cutaneous nerve and the anterior branch of the obturator nerve. The ACB was first described in 1993 as a landmark-based technique dependent on palpation of the sartorius muscle and loss of resistance as the block needle pierced the vastoadductor membrane overlying the adductor canal.12 Recent interest in ultrasonography has reignited interest in the ACB as an ultrasound-guided technique (Fig. 2; Video 1).
Fig 2.
Ultrasound-guided adductor canal block. AL: Adductor longus muscle; LA: Local anaesthetic; RA: Reverberation artefact; SFA: Superficial femoral artery; SM: Sartorius muscle; SN: Saphenous nerve; VAM: Vastoadductor membrane; VM: Vastus medialis muscle. The unlabelled arrows indicate the block needle.
The following are the Supplementary data related to this article:
Ultrasound-guided ACB (USG-ACB) is associated with significantly less analgesic consumption after TKA than placebo alone. Most studies comparing USG-ACB and FNB have reported similar effects of the two blocks on postoperative analgesic consumption and pain scores after knee surgery. However, the ability to ambulate and maintain quadriceps strength after TKA favours USG-ACB, while FNB is associated with postoperative quadriceps paresis, delayed mobilization, and increased LOS.13 Controversy continues to exist as to the optimal level in the thigh at which to perform the USG-ACB. Whereas some clinicians advocate a distal approach, current evidence suggests that an approach at the mid-femoral level does not impair motor function and may allow for a more reliable block. Cephalad spread of LA within the adductor canal reaching the more proximal femoral motor nerve branches within the femoral triangle is rare, but may place the patient at risk of quadriceps paresis. Distal spread of LA into the popliteal fossa has been reported in association with foot drop secondary to anaesthesia of the sciatic nerve. Spread of LA outside the vastoadductor membrane may result in myositis, which is a rare event but may cause progressive and profound weakness of the quadriceps muscles which normally resolves over the ensuing months.
The innervation of the knee is complex, with contributions from both the lumbar and sacral plexuses. However, LA placed within the adductor canal will only anaesthetize nerves supplying structures on the medial aspect of the knee. The benefit of ACB can best be understood when it is viewed as part a multimodal analgesic regime using a number of analgesic modalities, which together will provide superior analgesia and enhance functional recovery after TKA, while limiting the adverse effects of a single drug or procedure alone.
Local infiltration
Local infiltration analgesia (LIA) for TKA was first described by Bianconi and colleagues14 and has gained popularity as an additional tool in the multimodal management of pain. The rationale behind LIA is based on an understanding of the neuroanatomy of the knee joint. The density of nerve endings is not homogenous throughout the knee joint, but areas including the suprapatellar fat pad, collateral ligaments, meniscular capsule attachments, and the periosteum are particularly densely innervated. Therefore, successful LIA is dependent on accurate placement of LA rather than random disposition. LIA has been demonstrated to be equivalent to epidural anaesthesia with respect to postoperative analgesia, but superior in terms of improved mobilizsation and LOS.15 A recent meta-analysis showed no significant pain difference in pain intensity or opioid consumption in patients receiving an FNB or LIA for TKA. FNB was associated with reduced pain on movement, while LIA preserves quadriceps function in the immediate postoperative period, which may be beneficial for early functional recovery. The LIA injectate varies between institutions and multiple synergistic preparations have been described, but most tend to include LA (usually ropivacaine 2 mg ml−1 or levobupivacaine 1.5 mg ml−1), epinephrine, ketorolac and/or clonidine. In the setting of significant renal disease, ketorolac is often withheld and is used in a reduced dose in patients over 75 yr of age, those with a history of peptic ulcer disease and/or if the creatinine clearance is less than 30 ml min−1. Complications of LIA are rare but include damage to the neurovascular structures, particularly of the posterior knee, and injury to the peroneal nerve laterally. Additionally, the medications themselves may have adverse effects including allergy, cardiotoxicity, and renal dysfunction. However, with careful injection technique and consideration of the patient's comorbidities, LIA remains a safe and effective option for postoperative analgesia after TKA.
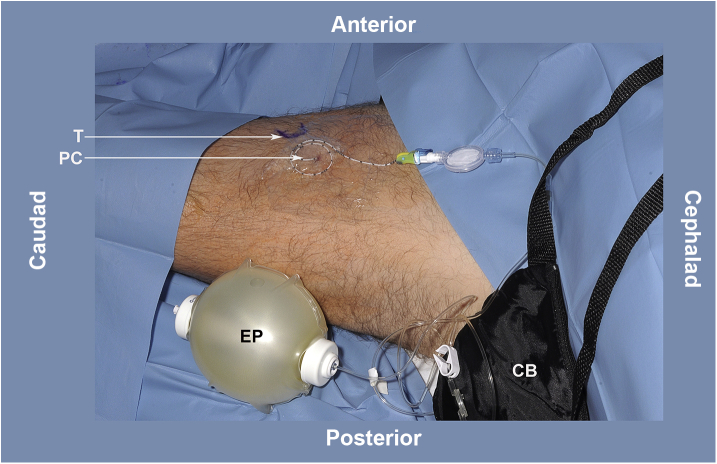
Ultrasound-guided local infiltration (USG-LIA) and periarticular injection of the knee joint has also been described (Fig. 3; Video 2).16 From a conceptual point of view, USG-LIA can be considered as a ring block performed above the knee. USG-LIA is a safe technique which provides excellent analgesia after TKA, while permitting early mobilization. A similar advanced technique of periarticular injection, as part of a motor sparing knee block, involves identifying the genicular branches deep to vastus medialis and lateralis at the level of the femoral epicondyles, with the inferior genicular branch located medial to the tibial plateau adjacent to the genicular vessels.17
Fig 3.
Ultrasound-guided local infiltration. N: Needle; RF: Rectus femoris muscle; T: Transducer (linear, high frequency); VI: Vastus intermedius muscle.
The following are the Supplementary data related to this article:
Novel regional anaesthesia techniques
As the trend moves away from FNB and SNB to provide analgesia after TKA, novel regional anaesthetic techniques have been developed or proposed as part of the multimodal pain management programme. Traditionally, SNBs have been undertaken to provide analgesia of the posterior aspect of the knee after TKA. The innervation of the posterior aspect of the knee is in part derived from the popliteal nerve plexus which ramifies around the genicular vasculature in the popliteal fossa. The popliteal nerve plexus is formed from the tibial nerve and the posterior branch of the obturator nerve. Recently, the infiltration of the interspace between the popliteal artery and the capsule of the posterior knee (IPACK) block has been introduced as an alternative to SNBs (Fig. 4; Video 3).18 The IPACK block is postulated to provide posterior knee analgesia through blockade of terminal branches innervating the posterior knee capsule, while sparing the tibial and peroneal nerves. The risk of neural and vascular injury exists during the IPACK block due to the presence of the popliteal vessels and tibial and peroneal nerves near the posterior capsule. While further studies are required to establish their benefit and safety profile, IPACK blocks may represent a significant advance in providing analgesia to the posterior aspect of the knee after TKA.
Fig 4.
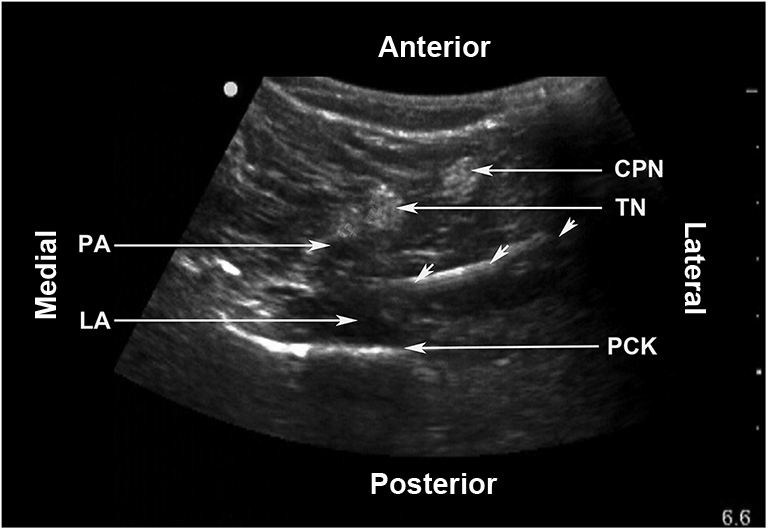
IPACK Block. CPN: Common peroneal nerve; LA: Local anaesthetic; PA: Popliteal artery; PCK: Posterior capsule of the knee; TN: Tibial nerve. The unlabelled arrows indicate the needle.
The following are the Supplementary data related to this article:
The nerve to vastus lateralis (NVL) is a branch of the femoral nerve. The most distal branches of NVL divide into a varying number of filaments which innervate the anterolateral portion of the joint capsule, reaching as far as the lateral edge of the patella. The distal division of NVL is commonly encountered during anterolateral thigh flap dissection.19 Harvesting of the distal branch of NVL during this procedure is, however, not associated with functional impairment of the lower extremity. Placement of LA around the distal NVL seems an enticing option for reducing sensation from the anterolateral aspect of the knee while also preserving motor function after TKA. Using ultrasound guidance, NVL is found lateral to the descending branch of the lateral circumflex femoral artery between the rectus femoris and VL muscles along a line between the anterior superior iliac spine and the lateral aspect of the patella corresponding to the lateral intermuscular septum (Fig. 5).
Fig 5.
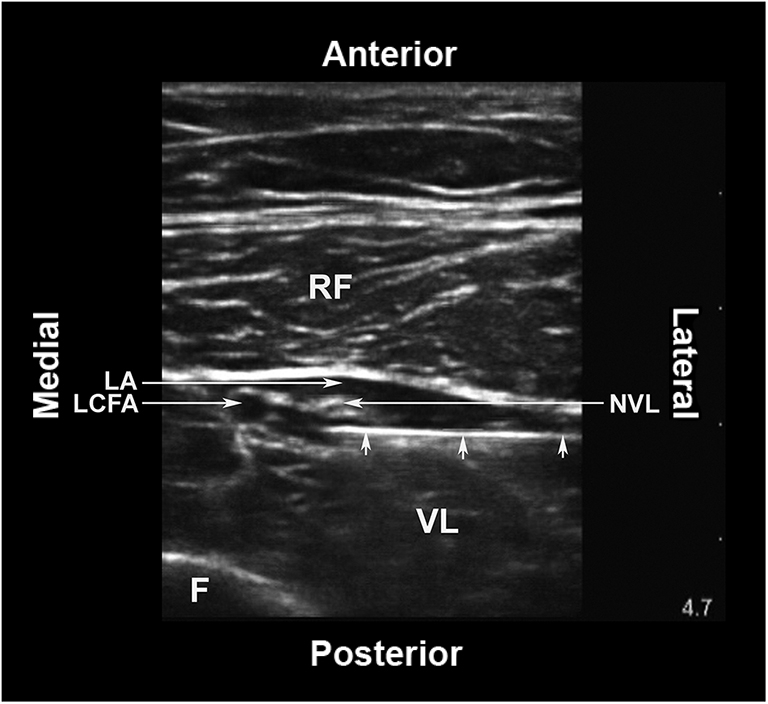
The distal branch of nerve to vastus lateralis in the thigh. F: Femur; LA: Local anaesthetic; LCFA: Descending branch of the lateral circumflex femoral artery; NVL: Nerve to vastus lateralis muscle; RF: Rectus femoris muscle; VL: Vastus lateralis muscle. The small unlabelled arrows indicate the block needle.
Pharmacological adjuvants
The analgesic and anti-inflammatory benefits of glucocorticoids are well established. Dexamethasone is a potent, long-acting glucocorticoid which has been extensively used in the perioperative setting. The preoperative administration of i.v. dexamethasone has been shown to reduce levels of acute phase reactants such as C-reactive protein and interleukin-6 after TKA.20 However, concerns regarding potential side-effects, including increased risk of deep wound infections, have often prevented glucocorticoids from being regularly included in the perioperative protocols for TKA. Nevertheless, randomized trials have confirmed that low dose glucocorticoids are safe and effective in reducing postoperative pain, enhancing mobility, and reducing LOS after TKA.
Knee haematoma after TKA often results in considerable pain after TKA. Postsurgical haemorrhage has additional significant consequences, including acute anaemia, potentially resulting in blood transfusion and prolonged LOS. Tranexamic acid (TXA) is a relatively inexpensive synthetic derivative of the amino acid lysine which prevents the degradation of fibrin by reversibly inhibiting the lysine-binding site on plasminogen. TXA has been shown to be safe and effective in reducing bleeding and haematoma formation after TKA. The optimal dose, timing, and route of TXA administration are still unclear, but current evidence suggests that postoperative blood loss and knee haematoma are significantly reduced when TXA is administered both topically and i.v. rather than by the i.v. alone. This reduction in postoperative knee haematoma and associated pain aids mobility, reduces LOS, and improves patient satisfaction.
Postoperative period
Surgical pain following TKA can be extremely intense during the immediate postoperative period. Multimodal analgesia is essential to maximize pain relief and minimize side-effects while maintaining rehabilitation and patient satisfaction. Communication between surgeons, anaesthetists, nursing staff, physiotherapists, and the acute pain team is essential in this regard.
Analgesic therapy
Opioids have traditionally remained an integral part of most postoperative analgesic protocols after TKA, and i.v. patient-controlled analgesia (IVPCA) has a number of advantages. It is immediate, effective, and tailored to individual needs, particularly in those patients with chronic pain. However, the use of a bulky IVPCA pump may impede patient activity and participation in physical therapy within an ERP. Oral administration of opioids is an alternative strategy and can include a combination of long- and short-acting drugs. However, this strategy relies upon drug administration in a timely and pre-emptive manner within a busy ward environment. Transdermal PCA is a novel approach for delivering opioids to the postoperative patient without the need for venous access and external infusion pumps which limits mobilization. The fentanyl transdermal system utilizes iontophoresis technology and is composed of two units, namely the hydrogel drug and the electronic controller. Transdermal fentanyl PCA is licenced for the management of moderate to severe postoperative pain and has been shown to be as effective as IVPCA with greater ease of use, but is limited by a slower onset time.21 All opioids are associated with a number of side-effects including sedation, respiratory depression, and nausea and vomiting, which impair postoperative recovery. A further concern for patients and physicians is the potential for development of opiate tolerance and addiction. Therefore, additional strategies to reduce morphine consumption are often employed within the multimodal analgesic programme. The simplest approach is the use of paracetamol combined with a short course of NSAIDs and careful titration of opioid analgesics. Paracetamol is a popular adjuvant to opioids as part of a multimodal analgesia regime in the acute postoperative period. Paracetamol is a centrally acting, non-opioid, non-NSAID analgesic and is a safe, effective, and well-tolerated component of the postoperative multimodal analgesic regimen. It has an opioid-sparing effect and is better tolerated in the elderly and high-risk patients after TKA. NSAIDs are also commonly used as a component of multimodal analgesia in the postoperative period to reduce opioid requirements. Postoperative NSAID administration improves outcomes after orthopaedic surgery, including reduced pain scores and enhanced functional recovery. However, the increased risk of bleeding, cardiovascular, and renal complications needs to be balanced with the benefits of NSAID administration after TKA.
Continuous LA infusions
Single injections of LA have a limited duration and ways of preventing rebound pain need to be considered. Intermittent injections and continuous infusions of LA through intra-articular catheters have been used successfully in a number of centres after TKA. The evidence for the use of either intermittent doses or continuous infusion remains equivocal. Additives to the LA infiltration include NSAIDs and epinephrine to prevent drug reabsorption and extend the duration of analgesia. However, concerns regarding infection have limited the use of intra-articular catheters.
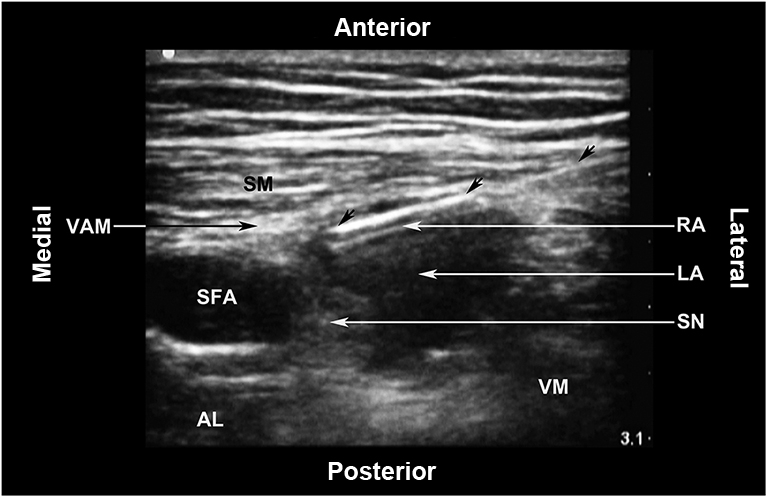
Continuous ACBs are a feasible analgesic modality after TKA, reducing opioid consumption in the first 48 hours after surgery, when compared to placebo (Fig. 6; Video 4). Other outcomes, including quadriceps strength, distance ambulated, and pain scores, all show benefit from continuous ACBs after TKA, while adverse effects are minimal. The use of elastomeric pumps offers a safe and simple alternative to electronic devices, allowing the patient to be mobilized, while delivering a continuous infusion of LA (Fig. 7).
Fig 6.
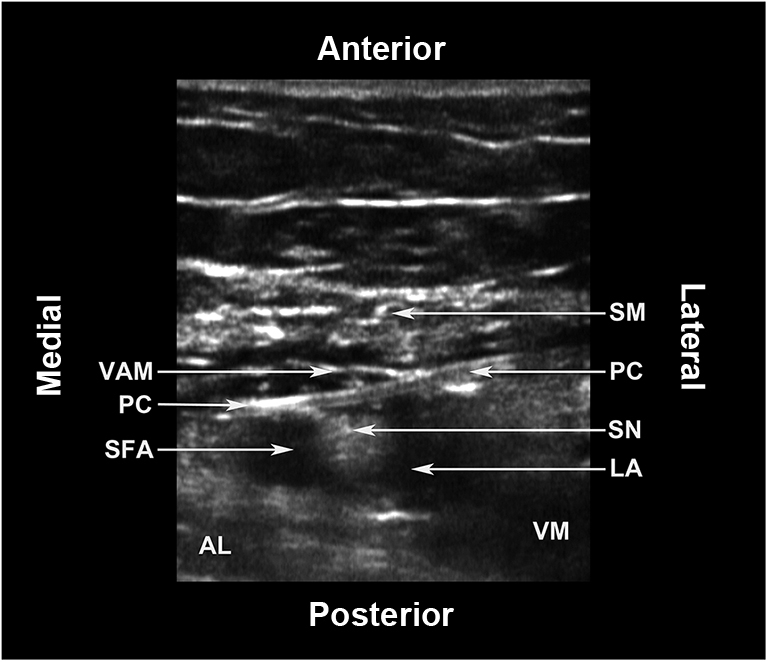
The adductor canal catheter. AL: Adductor longus muscle; LA: Local anaesthetic; PC: Perineural catheter; SFA: Superficial femoral artery; SM: Sartorius muscle; SN: Saphenous nerve; VAM: Vastoadductor membrane; VM: Vastus medialis muscle.
Fig 7.
Continuous adductor canal infusion. CB: Carry bag for the elastomeric pump; EP: Elastomeric pump containing local anaesthetic; PC: Perineural catheter; T: Transducer position for inserting the catheter.
The following are the Supplementary data related to this article:
Gabapentin
The role of gabapentin in the postoperative period remains unclear and there is no strong evidence to support the routine use of gabapentinoids in the management of acute pain following TKA. Gabapentinoids are associated with a small, but clinically insignificant, reduction in postoperative opioid consumption. Furthermore, there is no evidence that the postoperative use of gabapentinoids improves function or decreases the incidence of chronic pain at 3 months in patients after TKA.
Cryocuff
A cryocuff is an ice-filled cuff that can be applied to the knee to provide both cooling and pressure to the arthroplasty site. Theoretically, this may provide cryoanalgesia, prevent LA absorption, reduce inflammation or swelling, and provide physical support to the joint. Cryotherapy is not associated with any serious adverse events and may slightly reduce the amount of blood loss and pain in addition to improving range of movement in the first 1–2 weeks after TKA.22
Future directions
Multimodal analgesia offers many benefits to patients undergoing joint arthroplasty. Although opioids remain an integral part of most postoperative analgesic regimes, novel techniques that reduce opioid requirements and related side-effects have the potential to enhance postoperative recovery and improve patient satisfaction after TKA. Techniques for controlling postoperative pain after lower extremity joint reconstruction have advanced significantly in recent years. Recent work has shown a combination of LIA and ACB to provide improved analgesia than LIA alone.23 However, further studies are required to determine which combination of regional anaesthetic techniques provides optimal analgesia and reduces opioid consumption after TKA while minimizing side effects.
While we await the development of a selective LA that can preferentially anaesthetize sensory nerves while sparing motor nerves, we need to improve the profile of non-selective LAs in the perioperative management of pain. Recent attempts to increase the duration of LA action include liposomal bupivacaine, which is as of yet unavailable in the UK. This preparation of bupivacaine, which is loaded within multivesicular liposomes, increases the duration of LA action by slow release from the liposomes. Liposomal bupivacaine has been shown to be effective in treating postoperative pain when used via local infiltration, compared to placebo with a prolonged duration of action, predictable kinetics, opioid sparing effects, and an acceptable side-effect profile. However, further studies are required to establish the safety and efficacy of liposomal bupivacaine for use via the intrathecal, epidural, and perineural routes.
Declaration of interest
None declared.
MCQs
The associated MCQs (to support CME/CPD activity) can be accessed at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Rob O'Donnell MBChB MSc FRCA is a trainee anaesthetist in the West of Scotland School of Anaesthesia and an Honorary Clinical Lecturer at the University of Glasgow.
John Dolan BSc (Hons) MSc (Pain) PhD MBChB FFARCSI EDRA PgCert (Clin US) is a Consultant Anaesthetist at with special interests in regional anaesthesia, clinical ultrasound, orthopaedic anaesthesia and enhanced recovery. He is a tutor for the MSc course in regional anaesthesia, University of East Anglia.
Matrix codes: 1D02, 2E01, 3A09
Supplementary material
Supplementary data related to this article can be found online at https://doi.org/10.1016/j.bjae.2017.11.003.
References
- 1.Rakel B.A., Blodgett N.P., Zimmermann M.B. Predictors of postoperative movement and resting pain following total knee replacement. Pain. 2012;153:2192–2203. doi: 10.1016/j.pain.2012.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vadivelu N., Mitra S., Schermer E., Kodumudi V., Kaye A.D., Urman R.D. Preventative analgesia for postoperative pain control: a broader concept. Local Reg Anesth. 2014;7:17–22. doi: 10.2147/LRA.S62160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cheville A., Chen A., Oster G., McGarry L., Narcessian E. A randomized trial of controlled-release oxycodone during inpatient rehabilitation following unilateral total knee arthroplasty. J Bone Joint Surg Am. 2001;83:572–576. doi: 10.2106/00004623-200104000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Comfort V.K., Code W.F., Rooney M.E., Yip R.W. Naproxen premedication reduces postoperative tubal ligation pain. Can J Anaesth. 1992;4:349–352. doi: 10.1007/BF03009045. [DOI] [PubMed] [Google Scholar]
- 5.Bally M., Nandini D., Rich B. Risk of acute myocardial infarction with NSAIDs in real world use: Bayesian meta-analysis of individual patient data. Br Med J. 2017;357 doi: 10.1136/bmj.j1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harden R.N., Bruehl S., Stanos S. Prospective examination of pain-related and psychological predictors of CRPS-like phenomena following total knee arthroplasty: a preliminary study. Pain. 2003;106:393–400. doi: 10.1016/j.pain.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Menigaux C., Adam F., Guignard B., Sessler D.I., Chauvin M. Preoperative gabapentin decreases anxiety and improves early functional recovery from knee surgery. Anesth Analg. 2005;100:1394–1399. doi: 10.1213/01.ANE.0000152010.74739.B8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith L.M., Cozowicz C., Uda Y., Memtsoudis S.G., Barrington M.J. Neuraxial and combined neuraxial/general anesthesia compared to general Anesthesia for major truncal and lower limb surgery: A systematic review and meta-analysis. Anesth Analg. 2017;125:1931–1945. doi: 10.1213/ANE.0000000000002069. [DOI] [PubMed] [Google Scholar]
- 9.Perlas A., Chan V.W.S., Beattie S. Anesthesia technique and mortality after total hip or knee arthroplasty. A retrospective, propensity score–matched cohort study. Anesthesiology. 2016;125:724–731. doi: 10.1097/ALN.0000000000001248. [DOI] [PubMed] [Google Scholar]
- 10.Awad I.T., Cheung J.J., Al-Allaq Y., Conroy P.H., McCartney C.J. Low-dose spinal bupivacaine for total knee arthroplasty facilitates recovery room discharge: a randomized controlled trial. Can J Anaesth. 2013;60:259–265. doi: 10.1007/s12630-012-9867-5. [DOI] [PubMed] [Google Scholar]
- 11.Jiang X., Wang Q., Wu C., Tian W. Analgesic efficacy of adductor canal block in total knee arthroplasty: A meta-analysis and systematic review. Orthop Surg. 2016;8:294–300. doi: 10.1111/os.12268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van der Wal M., Lang S.A., Yip R.W. Transsartorial approach for saphenous nerve block. Can J Anaesth. 1993;40:542–546. doi: 10.1007/BF03009739. [DOI] [PubMed] [Google Scholar]
- 13.Abdallah F.W., Whelan D.B., Chan V.W. Adductor canal block provides noninferior analgesia and superior quadriceps strength compared with femoral nerve block in anterior cruciate ligament reconstruction. Anesthesiology. 2016;124:1053–1064. doi: 10.1097/ALN.0000000000001045. [DOI] [PubMed] [Google Scholar]
- 14.Bianconi M., Ferraro L., Traina G.C. Pharmacokinetics and efficacy of ropivacaine continuous wound instillation after joint replacement surgery. Br J Anaesth. 2003;91:830–835. doi: 10.1093/bja/aeg277. [DOI] [PubMed] [Google Scholar]
- 15.Andersen K.V., Bak M., Christensen B.V., Harazuk J., Pedersen N.A., Søballe K. A randomized, controlled trial comparing local infiltration analgesia with epidural infusion for total knee arthroplasty. Acta Orthop. 2010;81:606–610. doi: 10.3109/17453674.2010.519165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sinha S., Abrams J., Vellanky S., Arumugam S. 41st Annual regional anesthesiology and acute pain medicine meeting. American Society Regional Anaesthesia; 2006. Safety of anesthesiologist-administered ultrasound-guided infiltration analgesia with liposomal bupivacaine compared to femoral-tibial nerve block in total knee arthroplasty patients.http://epostersonline.com/asra_RA16/node/880 Available from: [Google Scholar]
- 17.Egeler C., Jayakumar A., Ford S. Motor-sparing knee block–description of a new technique. Anaesthesia. 2013;68:542–543. doi: 10.1111/anae.12233. [DOI] [PubMed] [Google Scholar]
- 18.Gururva Reddy A.V., Jangale A., Reddy R.C., Sagi M., Gaikwad A., Reddy A. To compare effect of combined block of ACB with IPACK and ACB alone on total knee replacement in immediate postoperative rehabilitation. Int J Orthop Sci. 2017;3:141–145. [Google Scholar]
- 19.Song Y.G., Chen G.Z., Song Y.I. The free thigh flap: A new free flap concept based on the septocutaneous artery. Br J Plast Surg. 1984;37:149–159. doi: 10.1016/0007-1226(84)90002-x. [DOI] [PubMed] [Google Scholar]
- 20.Smith C., Erasmus P.J., Myburgh K.H. Endocrine and immune effects of dexamethasone in unilateral total knee replacement. J Int Med Res. 2006;34:603–611. doi: 10.1177/147323000603400605. [DOI] [PubMed] [Google Scholar]
- 21.Ground S., Hall J., Spacek A., Hoppenbrouwers M., Richarz, Bonnet F. Iontophoretic transdermal system using fentanyl compared with patient-controlled intravenous analgesia using morphine for postoperative pain management. Br J Anesth. 2007;98:806–815. doi: 10.1093/bja/aem102. [DOI] [PubMed] [Google Scholar]
- 22.Adie S., Kwan A., Naylor J.M., Harris I.A., Mittal R. Cryotherapy following total knee replacement. Cochrane Database Syst Rev. 2012;9 doi: 10.1002/14651858.CD007911.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Andersen H.L., Gyrn J., Møller L., Christensen B., Zaric D. Continuous saphenous nerve block as supplement to single-dose local infiltration analgesia for postoperative pain management after total knee arthroplasty. Reg Anesth Pain Med. 2013;38:106–111. doi: 10.1097/AAP.0b013e31827900a9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.