Learning objectives.
By reading this article, you should be able to:
-
•
Discuss peripartum events that are associated with the development of postpartum posttraumatic stress disorder (PTSD).
-
•
Implement plans for management of anaesthesia for patients with PTSD.
-
•
Identify risk factors contributing to the development of postpartum PTSD.
-
•
Describe the impact of psychological birth trauma on future generations.
Key points.
-
•
Antenatal risk factors, such as PTSD, childhood sexual abuse and fear of childbirth predispose patients to the development of postpartum PTSD.
-
•
A subjective negative appraisal of childbirth is one of the strongest predictors for the development of postpartum PTSD.
-
•
Anaesthetic complications have been associated with postpartum PTSD.
-
•
Patients with a history of childhood sexual abuse present with unique needs in the peripartum period.
-
•
A traumatic birth experience can have negative physical and psychological effects on maternal, fetal and neonatal health.
Trauma has been defined as an event that overwhelms one's ability to maintain a sense of control, to assign meaning to the experience and to maintain connection with others. Psychological trauma that manifests any time in the peripartum period can have significant implications for maternal, fetal and neonatal health. Up to 44% of women perceive their childbirth experience as traumatic.1 The prevalence of postpartum posttraumatic stress disorder (PTSD) in community populations is estimated at 4%, and as high as 18.5% among high-risk groups.2 Some women present with an antenatal history of PTSD. Pre-existing PTSD occurs in approximately 8% of pregnant patients and is often complex and difficult to treat.3
PTSD is classified according to the Diagnostic and Statistical Manual of Mental Disorders as a trauma and stress-related disorder that includes several specific diagnostic criteria:4
-
(i)
Exposure to a traumatic event;
-
(ii)
a specific number of symptoms from each of the categories of re-experiencing, avoidance and arousal;
-
(iii)
negative cognitions and mood;
-
(iv)
duration of longer than 1 month;
-
(v)
symptom-related distress or functional impairment.
Childbirth has only recently been recognised by perinatal psychiatrists as a triggering event fulfilling the PTSD exposure criteria. This enabled the proper identification of peripartum patients with PTSD and stimulated research focusing on prevention strategies, identification of risk factors and potential treatment interventions. Unfortunately, inconsistencies among definitions and measurements of traumatic stress (full compared with partial or subsyndromal PTSD) have challenged interpretation and generalised application of the available data. Furthermore, the topic of peripartum PTSD—although widely recognised in nursing, midwifery and psychological journals—has yet to be well described in clinical obstetric and anaesthesia journals.
This review examines all pertinent literature on this topic and focuses on several aspects of peripartum PTSD, notably: predisposing risk factors for the development of a traumatic birth experience and risk factors for the development of PTSD after a traumatic birth; intrapartum precipitating events associated with the development of postpartum PTSD; the impact of a traumatic birth and postpartum PTSD on maternal and neonatal physical and psychological health; and possible management strategies that can be used at any time across the peripartum period.
Clinical scenario.
Jade, a nulliparous woman, presented for an induction of labour at 39 weeks. She prepared a birth plan with her birth companion and communicated with her obstetrician that she wanted minimal interventions. Contrary to her preferences, she underwent a prolonged induction with misoprostol, a Foley bulb, oxytocin and rupture of membranes. After 36 h of labour, Jade requested epidural analgesia, and although she requested that no students perform the regional block, a trainee attempted and had difficulties. The second provider was successful. Over the next several hours she called out at least twice stating that her contractions were painful. Interventions were not completely effective in addressing the inadequacies of her epidural analgesia. Jade went for a non-urgent Caesarean section after a failed 3-day induction, and despite communicating to the team that she felt pain when they tested the block, they started the surgery. The anaesthesia team did not appreciate her perceived level of pain and failed to provide effective alternative anaesthetic options until after the delivery of her baby. Her subjective negative appraisal of the overall birth experience, the lack of effective communication with providers and severe intraoperative pain all contributed to the development of postpartum PTSD.
Intrapartum traumatic birth experiences
Postpartum PTSD occurs in approximately 4% of postpartum patients overall.2 Several intrapartum events have been associated with an increased risk for the development of PTSD. Awareness of these factors will facilitate identification of PTSD and possibly early intervention. A traumatic event is defined as an actual or perceived threat of death or serious injury to oneself or others4 and may not always match a provider's perception of an event. Differentiating between physical trauma and what is perceived by the patient as traumatic is an essential step in mitigating further psychological harm.
Obstetric complications have been noted in numerous studies to increase a patient's risk for developing PTSD.4, 5, 6, 7 Operative birth (assisted vaginal delivery with forceps or a vacuum or Caesarean section), obstetric emergencies and infant complications, and medical interventions are all significant predictors of postpartum PTSD.5,6,9 One prospective study examined the responses of emergency teams to obstetric crises and found that these processes, although intended to improve a patient's safety, may increase the risk for postpartum acute stress disorder or PTSD.10 A separate review found a potential relationship between severe maternal morbidity, especially severe pre-eclampsia, and PTSD symptoms.11 In the majority of recent studies, a patient's negative subjective experience of childbirth has consistently emerged as a critical predictor of PTSD. The authors of one particular study concluded that the perceived severity of an event is more important in predicting PTSD than the objective stressor severity itself.8 Other intrapartum factors such as minimal support during labour and delivery;5,6,9 loss of control and fear of childbirth;8 pain experienced during the birth; and anxiety and inherent coping strategies9 are all significant predictors of the development of postpartum PTSD. Intimate partner violence (IPV) during pregnancy, if considered under the category of past trauma (separate from sexual trauma), has been addressed in multiple studies and has surfaced as another risk factor.3,5,8 Anaesthesia providers are in key positions to identify many of these events and facilitate early referral to mental health specialists to hopefully mitigate adverse consequences of perinatal PTSD.
Postpartum haemorrhage (PPH) may contribute to postpartum PTSD. Obstetric haemorrhage is a recognised cause of physical maternal morbidity and mortality worldwide. However, there are few quality studies exploring the possible effect of severe maternal haemorrhage on maternal emotional and psychological health. The California Maternal Quality Care Collaborative (CMQCC) has recognised the risk for emotional trauma and published recommendations (CMQCC Task Force, Stanford California, USA,Toolkit Version 2.0) based primarily on patient narratives discussing perceptions and experiences surrounding a PPH. A recent review article examined the existing literature on the associations between PPH and PTSD, and between emergency peripartum hysterectomy (EPH) and PTSD.12 Only seven articles were included, and a meta-analysis could not be performed because of the heterogeneity of studies. The authors concluded that there may be an association between PPH and PTSD, and EPH and PTSD; but, these associations must be interpreted with caution because of the small number of quality studies. One qualitative study examined patients' experiences after EPH, and—although not structured to assess specifically for PTSD—provides important insight into the emotional needs of these patients.13 Seven major themes were identified after an EPH: (i) fear; (ii) pain; (iii) the need for information; (iv) numbness (emotional); (v) the need for compassion, attentiveness and sensitivity; (vi) bonding; and (vii) separation from infants. The authors also found that psychological upset occurred after the event, and symptoms of severe emotional upset were often delayed beyond 3 months. ICU admission is a possible consequence of a severe PPH or EPH, and the authors noted that although ICU admission in the general population is a known risk for PTSD, it is unclear if it increases the risk for postpartum PTSD after a PPH or EPH. Regardless of the clinical outcome of a PPH, it is recommended, in accordance with NICE (National Institute for Health and Care Excellence) guidelines, that signs and symptoms of PTSD after any severe maternal morbidity ‘should be monitored over time to ensure timely and effective mental health treatment’.11
The relationship between early pregnancy loss (EPL)—miscarriage and ectopic pregnancy—and the development of posttraumatic stress has also been examined.14 The authors conducted a prospective pilot study using surveys to assess PTSD and anxiety and depression at 1, 3 and 9 months after an EPL. They found that 39% of their study participants met criteria for probable moderate–severe PTSD at 3 months, and that 20% met the criteria for moderate–severe anxiety compared with controls. Interestingly, they also found higher levels of PTSD symptoms in women who experienced an ectopic pregnancy vs those with a miscarriage. Such a high incidence of probable PTSD in this high-risk cohort supports the recognition of EPL as a risk factor and possible point for intervention to mitigate the development and symptom severity of PTSD.
Anaesthesia-related factors
It is widely recognised that awareness under general anaesthesia contributes to the development of PTSD. However, there is scant research addressing specific anaesthesia-related causes of postpartum PTSD. One study specifically examined the role of anaesthetic complications as an independent variable in the development of PTSD.7 The authors found that anaesthetic complications were significant predictors of postpartum PTSD and PTSD profile (clinically significant PTSD symptomatology but not meeting full criteria). The types of complications examined were severe nausea and vomiting; failed spinal/epidural anaesthesia leading to intraoperative pain requiring rescue medications; unintentional dural puncture followed by severe postpartum postdural puncture headache; traumatic needle insertion with pain, residual cutaneous haematoma or both; and neurological injuries (central or lower extremity motor and sensory dysfunction linked to regional anaesthesia.) Interestingly, the type of anaesthesia (general vs regional); the amount of anaesthesia information given before, during or after the procedure; and the training level of anaesthesia provider was not significant in predicting acute PTSD or a PTSD profile in the postpartum period.
Pain in labour has been identified in several studies as a significant predictor of PTSD.9 Although pain is almost universally inherent to the birthing process and not a specific anaesthesia-related cause of psychological trauma, the pain of childbirth has many implications for the anaesthesia provider. One study examined if the use of epidural analgesia for the management of labour pain could decrease the incidence of postpartum depression (PPD) and found that its use was associated with a decreased risk.15 One important limitation in this study was that no assessment for the presence of depression was done before birth, therefore complicating postpartum analysis. Although the authors did not assess specifically for PTSD risk, several associations can be made as PPD and PTSD are frequently comorbidities in the postpartum period.5 A recent article examined the contribution of percent improvement of pain (PIP) on PPD.16 The authors concluded that the extent of pain relief provided by epidural analgesia predicts lower PPD scores, although the clinical significance of labour analgesia on PPD needs to be more clearly defined.
The management of anaesthesia for pregnant patients with pre-existing PTSD is also not well defined in the literature, and evidence-based recommendations are lacking. One case report described the anaesthetic management of a non-obstetric patient who had developed PTSD from intraoperative awareness in a previous surgery.17 A successful, non-triggering anaesthetic for the subsequent surgery was the result of preoperative shared decision-making with the patient, cautious use of benzodiazepines, regional anaesthesia and consistent conversation between the patient and the anaesthetist to keep the patient oriented to the present moment. Another paper discussed perioperative implications of PTSD in the general population and suggested the following as part of the anaesthetic plan: focus on managing comorbidities including cardiovascular disease and mental health issues; multimodal pain strategies; avoidance of anaesthetic drugs that may negatively interact with medications used for PTSD; establishment of trust with the entire operating team; calm, slow and quiet approaches to the patient; and cautious use of benzodiazepines.18 Equally as important, they mention asking about fears or potential triggers without extensive discussion about the trauma itself. This concept is supported in other qualitative studies.19
Other anaesthesia-related themes have been elucidated from qualitative narratives. These interviews provide valuable information about real clinical experiences that often cannot be captured through quantitative analysis.19,20 Factors that influence a patient's overall subjective birth experience include wanting control over the exposure of their bodies, fear of restraints and oxygen masks in the operating theatre, nausea and vomiting, and separation from loved ones for procedures. Negative language and perceived lack of support from medical personnel have also been mentioned as stressors. One qualitative study examining women's perceptions showed that even in emergency situations women had clear memories of what their providers said, and women felt ‘more positive about their care when they were given an explanation by health professionals… and a rationale for their medical procedure’.21 Positive feelings were strengthened if the women were involved in shared decision-making about their care. Conversely, if women felt ‘isolated, ignored, treated inadequately, impersonally or unequally, or not listened to’, they recalled feeling more distressed and frustrated. These negative emotions compounded the overall negative appraisal of the birth experience. Thus, addressing the emotional needs of patients early in the experience via compassionate and respectful communication may help to mitigate a negative birth experience and decrease the subsequent risk for the development of PTSD.6,8 Examples of compassionate and respectful communication include acknowledging the patient's experience and emotions, minimising harsh and loud stimuli and communicating with a calm voice, maintaining a focus on her experience and avoiding sidebar discussions with other staff members, inquiring about her emotional state frequently, providing her with facts about what is happening, and involving her and her significant other (if appropriate) in the decision-making process as much as possible (CMQCC Task Force, Stanford California, USA, Toolkit Version 2.0).
Antepartum factors
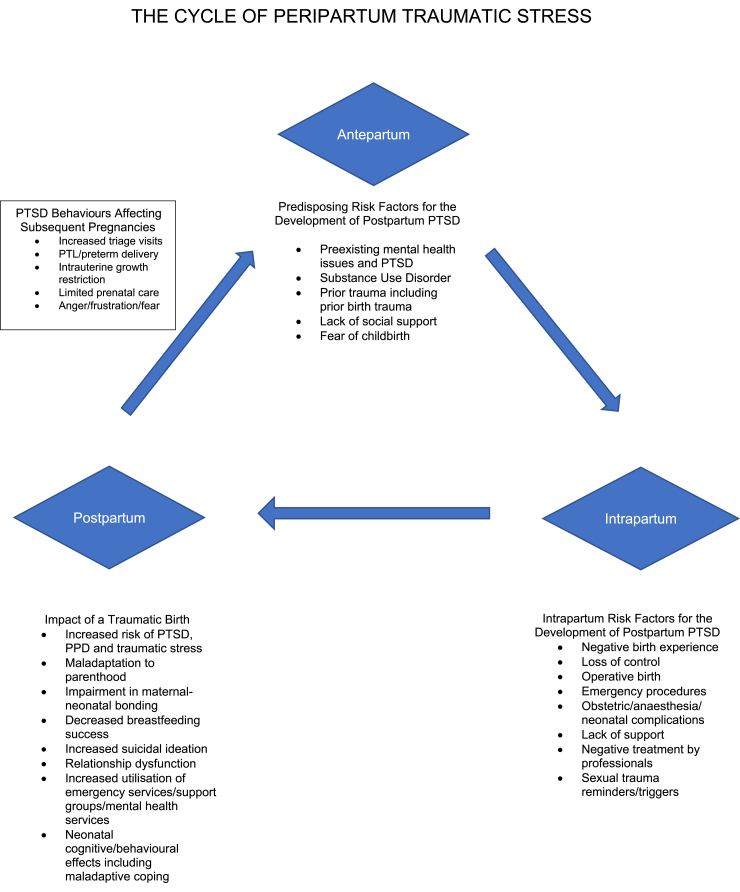
A significant number of women will present to labour and delivery with a pre-existing diagnosis of PTSD.3 This disorder can have profound effects on the physical and psychological health of pregnant women, and as a result of the chronic neurophysiological changes that occur because of unresolved traumatic stress, can even have impacts on the pregnancy, labour and delivery itself (Fig. 1).
Fig 1.
Cycle of peripartum traumatic stress. This figure illustrates the impact of antepartum risks and intrapartum factors on the development of postpartum PTSD. It also shows how postpartum PTSD and the behaviours associated with it can impact a woman's subsequent pregnancies and offspring.
The association between PTSD and preterm delivery (PTD) has been made by several authors. One prospective study establishes a possible association between pre-existing PTSD and PTD between 34 and 37 weeks of gestation.22 The authors found a stronger association between minor depressive disorder and low birth weight. Other research demonstrated an almost four-fold increased risk of PTD in patients with coexisting PTSD and major depressive episodes.23 A suggested mechanism for this phenomenon includes dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis that results in increases in maternal and fetal cortisol. The increase in fetal cortisol then stimulates the fetal adrenal gland to secrete oestriol, which is postulated to influence factors responsible for the initiation of labour. Furthermore, the authors theorised that chronic stress states lead to an increase in adrenaline (epinephrine) and noradrenaline (norepinephrine) concentrations contributing to chronic vasoconstriction, increased uterine artery resistance and the development of fetal growth restriction and preeclampsia, both of which are associated with PTD. The authors also mentioned other stress-related effects including decreases in immune function and risk of bacterial vaginosis resulting in PTD. Although not directly linked to PTD, sleep disturbances and alterations in eating patterns caused by chronic stress can create suboptimal conditions for pregnancy.23
PTSD as the result of prior sexual trauma deserves special consideration because of the intrinsic and extrinsic triggers that can occur during the perinatal period. These triggers are often reminiscent of their previous trauma. Patients with a history of childhood sexual abuse (CSA) or any other form of sexual assault (i.e. military sexual trauma, human trafficking, mass rape in conflict areas) may experience flashbacks or dissociate during pelvic examinations and develop avoidance behaviours resulting in minimal or no prenatal care. Other psychopathology can also occur, such as anxiety and depression in the perinatal period, and negative coping skills such as substance use disorders.24 Symptoms related to hyperarousal can manifest as irritability with caregivers, outright anger, or distrust. Patients may request that no male healthcare providers are involved, may present with extensive birth plans in an attempt to maintain some level of control, request a quiet environment or alternative lighting, clothing or smells so as to avoid associations with the original trauma.3,22 Unresolved trauma from CSA is associated with an increased risk of a traumatic birth experience9 and postpartum PTSD.3,6,8 In one qualitative study, the authors identified several themes elucidating the needs of this population including the need for a trusting relationship before disclosure of past trauma, clear explanations of why procedures are being done, significant anxiety about being exposed, the use of language that is not reminiscent of their trauma, and acceptance and communication of their birth plans with all caregivers.19 Identifying this population in the antenatal period and understanding their unique needs allows for the creation of specialised care plans. Suggested options for management of a patient with peripartum PTSD are outlined in Table 1.
Table 1.
Management strategies. This table summarises suggested management strategies for the pregnant patient with PTSD at different points during the peripartum period. †Trauma-informed care practices in healthcare recognise the impact trauma has on individuals and work to promote a culture of safety to prevent retraumatising patients in the medical care setting.
| Antepartum | Identify those patients with increased risk for the development of PTSD |
| Develop individualised care plans | |
| Multidisciplinary planning | |
| Establishment of expectations | |
| Identification of trauma reminders | |
| Identify need for psychotherapy | |
| Strengthen interpersonal relationships | |
| Intrapartum | Optimise pain management (per patient request) |
| Trauma-informed care practices† | |
| Minimise separation from support person/partner | |
| Adherence to care plan | |
| Collaborative decision-making | |
| Use coping skills to minimise the impact of trauma reminders | |
| Postpartum (for any traumatic birth experience) | Acknowledgement of traumatic event, grief/loss, or both |
| Follow-up obstetric care regularly over the first year (even if the patient appears asymptomatic) | |
| Process traumatic experience as desired via compassionate and respectful communication | |
| Offer referral for emotional and psychological support |
In patients without a pre-existing diagnosis of PTSD, several other antenatal risk factors may increase vulnerability to the development of postpartum PTSD. These include a lack of social support,8,9 maternal mental health conditions such as depression and anxiety, fear of childbirth and other trauma exposures such as previous birth trauma and IPV.8
Trauma-informed care
The context in which trauma is managed and interventions are used that contribute to outcomes is referred to as ‘trauma-informed care’. What a trauma-informed care approach would look like for obstetric anaesthesia providers has not been formally established. The Substance Abuse and Mental Health Service Administration (SAMHSA) defines trauma-informed care with four ‘R’s’: a programme, organisation or system that realises the widespread impact of trauma and understands potential paths for recovery; recognises the signs and symptoms of trauma in clients, families, staff and others involved with the system; and responds by fully integrating knowledge about trauma into policies, procedures and practices, and seeks to actively resist retraumatisation.25
By superimposing these principles onto what has been learned from existing research, a proposed trauma-informed care practice for obstetric anaesthesia providers might include the following:
-
(i)
Realise that a significant proportion of women are survivors of trauma and that their previous trauma can negatively impact their current childbirth experience.
-
(ii)
Recognise established risk factors and identify vulnerable populations early in pregnancy; plan for consultation in a high-risk obstetric anaesthesia clinic to facilitate shared decision-making and development of mutually acceptable care plans that address fears and triggers; recognise acute stress reactions during labour and delivery and establish a plan for the pharmacological and non-pharmacological management of these.
-
(iii)
Respond and resist retraumatisation by vigilantly confirming efficacy of neuraxial analgesia and anaesthesia, minimising physical trauma with needle insertion, offering effective patient-focused communication, allowing the significant other to remain with the patient when possible, providing transparency and education if complications arise and referring early to mental health specialists.
Impact of postpartum PTSD
The psychological and psychosocial consequences of a traumatic birth experience on maternal well-being are well described, including but not limited to depression, anxiety and panic, suicidal thoughts and relationship difficulties.26 Stressful life events have also been shown to impact the oxytocinergic system, with lower levels of oxytocin prenatally observed in women with higher levels of cumulative stress.27 This is important given the association between lower maternal oxytocin levels with maternal depression, impaired mother–infant bonding and negative parenting behaviours with decreased maternal sensitivity.27 In fact, violence from an intimate partner, pre-existing PTSD and postpartum PTSD have all been shown to have a negative impact on maternal–infant bonding.28,29 The potential for intergenerational transmission of oxytocin deficiency to offspring is another significant implication of maternal trauma and may be part of the explanation of higher rates of behavioural and psychiatric disorders among offspring.27 Although research investigating the impact of perinatal PTSD on child outcomes is limited, evidence suggests postpartum PTSD is associated with low birth weight infants and lower rates of breastfeeding.28
Early referral to mother–baby psychological treatment for women with postpartum PTSD may prevent attachment deficits and limit the negative impact of maternal trauma on future generations. Mother–baby programmes attend to the psychological needs of the mother through provision of trauma-focused psychotherapy and psychoeducation while offering therapeutic interventions that strengthen the mother–infant relationship and promote healthy child development.
The identification of prenatal vulnerability factors, and predisposing factors occurring during labour and delivery, can assist with the identification of women at increased risk for the development of PTSD after childbirth. These factors as mentioned previously can include a woman's subjective level of distress during labour and delivery, instrumental or operative delivery, maternal or infant complications, lack of social support, psychiatric history, prior traumatic experiences, fear of childbirth and poor coping strategies.5,6,30 A woman's subjective experience is one of the most important risk factors for later development of PTSD, highlighting the importance of quality provider interactions and supportive, empathic communication during labour and delivery.6,8 These risk factors should also be considered when designing therapeutic interventions targeting the prevention and reduction of posttraumatic stress symptoms among psychologically vulnerable women, ensuring that services are not limited to women with more objective trauma alone.
Although obstetric care providers are encouraged to screen routinely for a history of sexual trauma during prenatal care, universal screening for PTSD is not routinely carried out postpartum (or antepartum) as it is for depression; this is likely to result in under-recognition of PTSD. The Perinatal PTSD Questionnaire and the Traumatic Event Scale are valid, reliable screening tools designed specifically to measure posttraumatic stress symptoms related to childbirth.7,9 However, neither screening tool measures PTSD according to all DSM-V diagnostic criteria. In addition, the timing and frequency of screening is not well established, and obstetric providers remain hesitant to screen for PTSD when specialised mental health providers may not be readily available.31 One recent article examined trajectories of birth-related PTSD after a traumatic birth experience up to 6 months after childbirth.2 As the authors examined the course of PTSD at various postpartum time points, they realised that the disease does not stay constant, and that different variables could be identified at 4–6 weeks postpartum that were associated with recovery vs chronic trajectories for PTSD. Factors such as severe affective symptoms (anxiety and depression), experiences of further trauma and low levels of satisfaction with healthcare providers were predictive of chronic and delayed PTSD trajectories. This study highlights specific patients that should be followed more closely given their increased risk for chronic PTSD and suggests ongoing screening later into the postpartum period. Although anaesthesia providers may not routinely follow patients beyond 24 h, their assessments on the first postpartum day allow for early identification of high-risk women. Their intimate knowledge of intrapartum events coupled with an understanding of the above risk factors allow for targeted observations for signs of acute stress such as hypersensitivity to stimuli, tearfulness, change in affect, difficulty concentrating or hostility and subsequent referral to appropriate mental health professionals.
Conclusions
Although research is continually emerging in this area, there are still many unanswered questions. Some possible areas of future research include: (i) the development of optimal screening procedures for vulnerability factors, (ii) whether shared decision-making models of care can impact a woman's perception of the birth experience and mitigate the development of PTSD, and (iii) optimal medical and non-medical interventions for the perioperative management of PTSD. The role of pain relief in labour is not completely understood and warrants further study. Nonetheless, there is currently substantial and valuable data to support certain clinical implications.
PTSD in the peripartum period can have devastating effects on maternal, fetal and neonatal health. It is essential that all providers that have any significant role in the care of pregnant women understand the risk factors that may increase vulnerability to a traumatic birth, identify when a traumatic birth may have occurred, and offer appropriate treatment and referrals. The understanding of patient preferences that we have gleaned from qualitative studies should direct our behaviours towards a shared decision-making model of care for those with pre-existing PTSD and universal behaviours that are respectful and supportive. For anaesthesia providers, our expertise in crisis management should also encompass acute emotional crisis management and the acceptance of our role as ‘guardians of psychological safety’ in the operating theatre. We have an opportunity and a responsibility to positively impact a patient's subjective experience of childbirth. If we can assist in providing our patients with a positive birth experience, we may decrease the incidence of PTSD in the postpartum period and its impact on future generations.
Declaration of Interest
The authors declare that they have no conflicts of interest.
MCQs
The associated MCQs (to support CME/CPD activity) will be accessible at www.bjaed.org/cme/home by subscribers to BJA Education.
Biographies
Tracey Vogel MD is a practicing obstetric anaesthetist in Pittsburgh, PA, USA. She completed her anaesthesia training, including a fellowship in obstetric anaesthesia from Stanford University. Dr Vogel is also a certified sexual assault counsellor at Allegheny County's Rape Center PAAR (Pittsburgh Action Against Rape) where she currently volunteers in medical advocacy and education for adult survivors of sexual trauma.
Sarah Homitsky MD is board certified in adult psychiatry, child and adolescent psychiatry from the University of Pittsburgh. Dr Homitsky is the medical director for the Women's Behavioural Health unit at Allegheny Health Network, and specialises in the treatment of mood and anxiety disorders during pregnancy and postpartum.
Matrix codes: 1E03, 2B06, 3B00
References
- 1.de Graaff L.F., Honig A., van Pampus M.G., Stramrood C.A.I. Preventing post-traumatic stress disorder following childbirth and traumatic birth experiences: a systematic review. Acta Obstet Gynecol Scand. 2018;97:648–656. doi: 10.1111/aogs.13291. [DOI] [PubMed] [Google Scholar]
- 2.Dikmen-Yildiz P.D., Ayers S., Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: a systematic review and meta-analysis. J Affect Disord. 2017;208:634–645. doi: 10.1016/j.jad.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 3.Seng J.S., Low L.K., Sperlich M., Ronis D.L., Liberzon I. Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstet Gynecol. 2009;114:839–847. doi: 10.1097/AOG.0b013e3181b8f8a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association . 5th ed. Author; Arlington, VA: 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 5.Ayers S., Bond R., Bertullies S., Wijma K. The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychol Med. 2016;46:1121–1134. doi: 10.1017/S0033291715002706. [DOI] [PubMed] [Google Scholar]
- 6.Andersen L.B., Melvaer L.B., Videbech P., Lamont R.F., Joergensen J.S. Risk factors for developing post-traumatic stress disorder following childbirth: a systematic review. Acta Obstet Gynecol Scand. 2012;91:1261–1272. doi: 10.1111/j.1600-0412.2012.01476.x. [DOI] [PubMed] [Google Scholar]
- 7.Lopez U., Meyer M., Loures V. Post-traumatic stress disorder in parturients delivering by caesarean section and the implication of anaesthesia: a prospective cohort study. Health Qual Life Outcome. 2017;15(1–13):118. doi: 10.1186/s12955-017-0692-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dekel S., Stuebe C., Dishy G. Childbirth induced posttraumatic stress syndrome: a systematic review of prevalence and risk factors. Front Psychol. 2017;8:560. doi: 10.3389/fpsyg.2017.00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Soet J.E., Brack G.A., DiIorio C. Prevalence and predictors of women's experience of psychological trauma during childbirth. Birth. 2003;30:36–46. doi: 10.1046/j.1523-536x.2003.00215.x. [DOI] [PubMed] [Google Scholar]
- 10.Silverstein R.G., Centore M., Pollack A., Barrieau G., Gopalan P., Lim G. Postpartum psychological distress after emergency team response during childbirth. J Psychosom Obstet Gynecol. 2019;40(4):304–310. doi: 10.1080/0167482X.2018.1512095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Futura M., Sandall J., Bick D. A systematic review of the relationship between severe maternal morbidity and post-traumatic stress disorder. BMC Pregnancy Childb. 2012;12:125. doi: 10.1186/1471-2393-12-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zaat T.R., van Steijn M.E., de Haan-Jebbink J.M. Posttraumatic stress disorder related to postpartum haemorrhage: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2018;22:214–220. doi: 10.1016/j.ejogrb.2018.04.012. [DOI] [PubMed] [Google Scholar]
- 13.de la Cruz C.Z., Coulter M., O'Rourke K., Mbah A.K., Salihu H.M. Post-traumatic stress disorder following emergency peripartum hysterectomy. Arch Gynecol Obstet. 2016;294:1–8. doi: 10.1007/s00404-016-4008-y. 2016. [DOI] [PubMed] [Google Scholar]
- 14.Farren J., Jalmbrant M., Ameye L. Post-traumatic stress, anxiety and depression following miscarriage or ectopic pregnancy: a prospective cohort study. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2016-011864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ding T., Wang D., Qu Y., Chen Q., Zhu S., Zhu S. Epidural labour analgesia is associated with a decreased risk of postpartum depression: a prospective cohort study. Anesth Analg. 2014;119:383–392. doi: 10.1213/ANE.0000000000000107. [DOI] [PubMed] [Google Scholar]
- 16.Lim G., Farrell L.M., Facco F.L., Gold M.S., Wasan A.D. Labor analgesia as a predictor for reduced postpartum depression scores: a retrospective observational study. Anesth Analg. 2018;126:1598–1605. doi: 10.1213/ANE.0000000000002720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mashour G.A., Jiang Y., Osterman J. Perioperative treatment of patients with a history of intraoperative awareness and post-traumatic stress disorder. Anaesthesiology. 2006;104:893–894. doi: 10.1097/00000542-200604000-00044. [DOI] [PubMed] [Google Scholar]
- 18.Wofford K., Hertzberg M., Vacchiano C. The perioperative implications of posttraumatic stress disorder. AANA J. 2012;80:463–470. [PubMed] [Google Scholar]
- 19.Sobel L., O’Rourke-Suchoff D., Holland E. Pregnancy and childbirth after sexual trauma. Patient perspectives and care preferences. Obstet Gynecol. 2018;132:1461–1468. doi: 10.1097/AOG.0000000000002956. [DOI] [PubMed] [Google Scholar]
- 20.Simpkin P., Klaus P. Classic Day Publishing; Seattle, WA: 2004. When survivors give birth. [Google Scholar]
- 21.Futura M., Sandall J., Bick D. Women's perceptions and experiences of severe maternal morbidity — a synthesis of qualitative studies using a meta-ethnographic approach. Midwifery. 2014;30:158–169. doi: 10.1016/j.midw.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 22.Rogal S.S., Poschman K., Belanger K. Effects of posttraumatic stress disorder on pregnancy outcomes. J Affect Disord. 2007;102:137–143. doi: 10.1016/j.jad.2007.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yonkers K.A., Smith M.V., Forray A. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry. 2014;71:897–904. doi: 10.1001/jamapsychiatry.2014.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roller C.G. Moving beyond the pain: women’s responses to the perinatal period after childhood sexual abuse. J Midwifery Womens Health. 2011;56:488–493. doi: 10.1111/j.1542-2011.2011.00051.x. [DOI] [PubMed] [Google Scholar]
- 25.Substance Abuse and Mental Health Services Administration 2014. https://store.samhsa.gov/system/files/sma14-4884.pdf Available from:
- 26.Fenech G., Thomson G. Tormented by ghosts from their past: a meta-synthesis to explore the psychosocial implications of a traumatic birth on maternal well-being. Midwifery. 2014;30:185–193. doi: 10.1016/j.midw.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Toepfer P., Heim C., Entringer S. Oxytocin pathways in the intergenerational transmission of maternal early life stress. Neurosci Biobehav Rev. 2016;73:293–308. doi: 10.1016/j.neubiorev.2016.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cook N., Ayers S., Horsch A. Maternal posttraumatic stress disorder during the perinatal period and child outcomes: a systematic review. J Affect Disord. 2018;225:18–31. doi: 10.1016/j.jad.2017.07.045. [DOI] [PubMed] [Google Scholar]
- 29.Zeitlin D., Colmsee M., Dhanjal T.S. Maternal–fetal bonding: the impact of domestic violence on the bonding process between a mother and child. Arch Womens Ment Health. 1999;2:183–189. [Google Scholar]
- 30.van Heumen M.A., Hollander M.H., van Pampus M.G., van Dillen J., Stramrood C.A.I. Psychosocial predictors of postpartum posttraumatic stress disorder in women with a traumatic childbirth experience. Front Psychiatry. 2018;9:348. doi: 10.3389/fpsyt.2018.00348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ayers S., Wright D.B., Thornton A. Development of a measure of postpartum PTSD: the city birth trauma Scale. Front Psychiatry. 2018;9:409. doi: 10.3389/fpsyt.2018.00409. [DOI] [PMC free article] [PubMed] [Google Scholar]